Urinary retention in pregnancy
Acute Urinary Retention in the First-trimester of Pregnancy: A Case Report
- Article
- Authors etc.
- Metrics
- Figures etc.
Chenyang Dai , Jiali Peng, Rufang Chen
Published: March 11, 2022 (see history)
DOI: 10.7759/cureus.23057
Cite this article as: Dai C, Peng J, Chen R (March 11, 2022) Acute Urinary Retention in the First-trimester of Pregnancy: A Case Report. Cureus 14(3): e23057. doi:10.7759/cureus.23057
Abstract
Acute urinary retention (AUR) is a rare occurrence during pregnancy. If not dealt with in time, it can lead to bladder rupture, miscarriage, or even uterine rupture and other serious consequences that endanger the health of both mother and fetus. Many risk factors have been identified. To better understand the etiology and treatment of urinary retention during pregnancy, we report on one pregnant woman with AUR who presented at 11+1 weeks of gestation due to uterus retroversion.
Introduction
Acute urinary retention (AUR) is defined as a sudden and painful inability to voluntarily void urine [1]. AUR is a rare but serious complication of pregnancy. It can lead to serious consequences, such as acute renal failure, spontaneous abortion, permanent bladder dysfunction, and bladder rupture [2], and occurs more often between 10 and 16 weeks of gestation [3,4]. According to previous reports, AUR occurs in approximately 1 in 3,000 pregnant women and is often associated with uterine incarceration [5]. However, as shown in our report, even without uterine entrapment, retroversion of the uterus itself can cause AUR.
Case Presentation
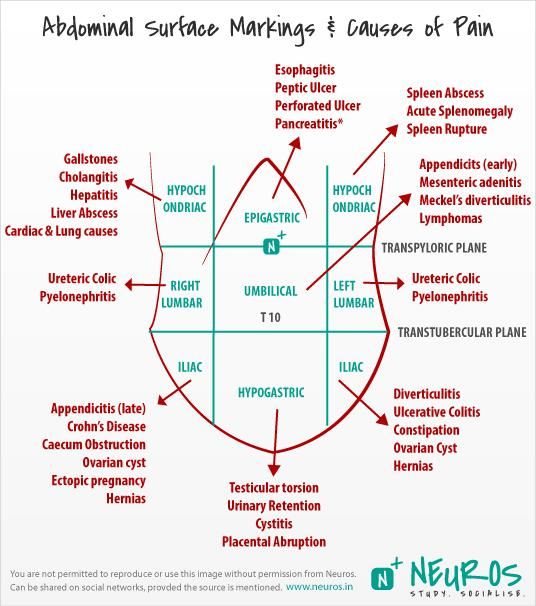
A 32-year-old primigravida was admitted to the Obstetrics Department with AUR at 11+1 weeks of gestation on December 27, 2021. The patient’s pregnancy had been normal until six days ago when she experienced urgency, frequent urination, and nocturia at least 10 times per night, associated with a sensation of incomplete bladder emptying and dysuria.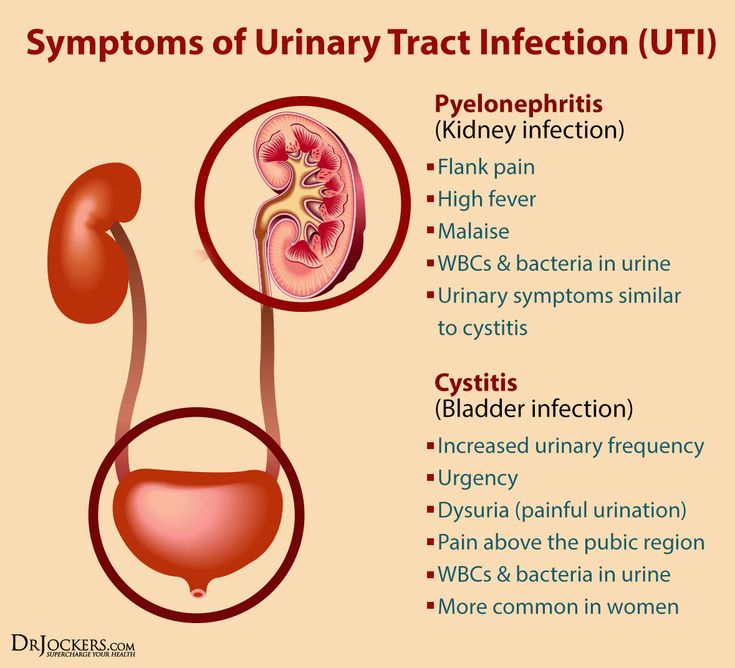 The illness, personal, and family history of this patient were unremarkable. Physical examination showed that a dramatically distended bladder was palpable above the pubic symphysis, and gynecological examination detected fullness in the posterior fornix and anterior displacement of the cervix. On bimanual examination, the retroverted uterus impacted in the pelvis was found. Routine urinalysis and assessment of kidney function (December 27, 2021) were negative. The ultrasound (December 27, 2021) detected a retroverted uterus. A gestational sac was seen in the uterine cavity, and a fetal echo was seen in the sac. The fetal heartbeat is visible. CRL is about 43 mm, and NT is 1.5 mm. The echoes of the uterine wall were uniform, the bilateral ovaries were visible, and no obvious abnormal mass echo was found in the bilateral appendages. The lower rod of the bladder is trapped by the pregnant uterus and contains approximately 427 cm3 urine (Figure 1).
The illness, personal, and family history of this patient were unremarkable. Physical examination showed that a dramatically distended bladder was palpable above the pubic symphysis, and gynecological examination detected fullness in the posterior fornix and anterior displacement of the cervix. On bimanual examination, the retroverted uterus impacted in the pelvis was found. Routine urinalysis and assessment of kidney function (December 27, 2021) were negative. The ultrasound (December 27, 2021) detected a retroverted uterus. A gestational sac was seen in the uterine cavity, and a fetal echo was seen in the sac. The fetal heartbeat is visible. CRL is about 43 mm, and NT is 1.5 mm. The echoes of the uterine wall were uniform, the bilateral ovaries were visible, and no obvious abnormal mass echo was found in the bilateral appendages. The lower rod of the bladder is trapped by the pregnant uterus and contains approximately 427 cm3 urine (Figure 1).
Figure 1: Abdominal ultrasound shows a retroverted uterus and a full bladder.
Abdominal ultrasound shows a retroverted uterus and a full bladder. The left image is the longitudinal section of the probe, and the right image is the transverse section of the probe.
The patient was diagnosed with AUR during pregnancy. The patient experienced rapid relief from her bladder discomfort after being inserted with a urinary catheter, with prompt drainage of 450 ml of clear urine. The catheter was continued indwelled and clipped intermittently five days later to exercise bladder function. Meanwhile, the patient was guided to adopt the knee-chest prone position for 15 min, 3 times a day to improve uterine retroversion (Figure 2). Ultrasound showed no pelvic mass, and the uterine polarity changed significantly seven days later. The patient's symptoms improved significantly, and she was able to void normally and was discharged from the hospital after the indwelling catheter was removed seven days later. The patient was advised to adopt a knee-chest prone position and limit fluid intake before sleep, as before, to prevent an AUR relapse during the next pregnancy. Thereafter, the patient has a regular obstetrics examination in our hospital. Her symptoms did not recur again, and her pregnancy remained uneventful until now.
Thereafter, the patient has a regular obstetrics examination in our hospital. Her symptoms did not recur again, and her pregnancy remained uneventful until now.
Figure 2: Knee-chest prone position.
Discussion
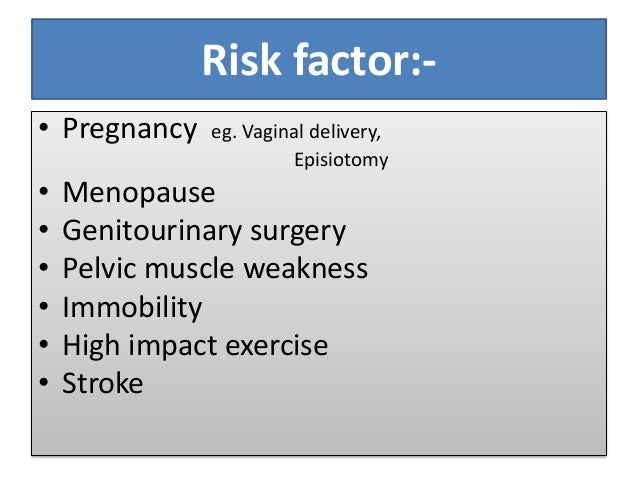
The etiology of AUR can be broadly classified into infectious, pharmacological, neurological, anatomical, myopathic, and functional categories [6]. In addition, as shown by the findings of Chen et al., maternal age >35 years, preterm birth, and first delivery were significantly associated with AUR [7]. While the most studied pathogenesis of AUR in pregnancy is anatomy, this includes endometriosis, pelvic adhesions, congenital malformations of the uterus, fibroids, or anatomical variations in the shape of the pelvis [4]. And interestingly, most cases of AUR are noted to take place in the middle of the night [8]. In the present case, the patient is a primipara, but no other high-risk factors have been found. The proposed mechanism is that, under the action of hormones, the glands in the cervical canal become hyperplasia and hypertrophy, which makes the cervix gradually soften after pregnancy, increasing the chance of uterine retroversion.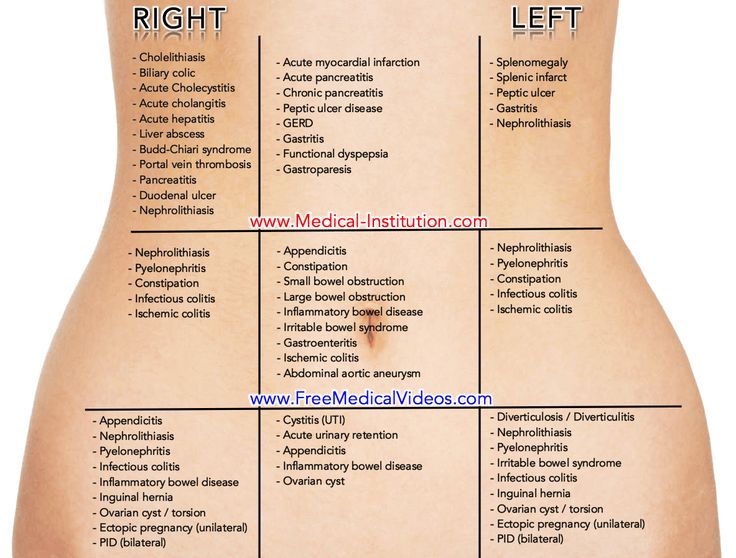 Then the cervix presses against the lower part of the bladder and interferes with urethral drainage without causing deformation or compression of the urethra. This suggests that even without confinement, uterine inversion during pregnancy can cause AUR.
Then the cervix presses against the lower part of the bladder and interferes with urethral drainage without causing deformation or compression of the urethra. This suggests that even without confinement, uterine inversion during pregnancy can cause AUR.
AUR can have a variety of clinical manifestations. According to the available data, the most common symptoms of AUR during pregnancy are urinary incontinence, incomplete urination, vaginal bleeding, miscarriage, painful urination, rectal compression, and constipation [4,9]. However, rare symptoms such as lower extremity swelling, severe hypertension, hydronephrosis, and asymptomatic AUR are easily overlooked during consultation [2,10]. Physical examination findings mainly include a low fundal height for the age of gestation, bladder distension, and palpation of a mass that can induce urgency. It is often difficult to see the cervix on a vaginal exam because it is hidden behind the symphysis pubis [4], as also shown in our case.
There is no simple diagnostic test to determine the cause of urinary retention during pregnancy. Apart from clinical manifestations and physical examination, auxiliary examinations such as ultrasound, magnetic resonance imaging (MRI), and endoscopy are useful tools for the diagnosis of a retroverted gravid uterus and AUR, and the use of sonography as a non-invasive diagnostic tool should be encouraged in a larger group of patients first [11]. In this study, typical signs and symptoms of the genitourinary system helped us to make a preliminary judgment, and an ultrasound image provided final confirmation. MRI can be used in complex cases and as a more accurate test to rule out other possible diagnoses. As Dierickx et al. [12] suggested, MRI was the imaging modality of choice for uterine incarceration, and MRI is recommended prior to manual or colonoscopy-assisted reduction to rule out anterior incarceration. Using cystoscopy as a diagnostic tool, it is recommended to exclude the presence of urinary vegetations, as the cause of AUR in pregnancy is external pressure, and cystoscopy is not very meaningful.
Apart from clinical manifestations and physical examination, auxiliary examinations such as ultrasound, magnetic resonance imaging (MRI), and endoscopy are useful tools for the diagnosis of a retroverted gravid uterus and AUR, and the use of sonography as a non-invasive diagnostic tool should be encouraged in a larger group of patients first [11]. In this study, typical signs and symptoms of the genitourinary system helped us to make a preliminary judgment, and an ultrasound image provided final confirmation. MRI can be used in complex cases and as a more accurate test to rule out other possible diagnoses. As Dierickx et al. [12] suggested, MRI was the imaging modality of choice for uterine incarceration, and MRI is recommended prior to manual or colonoscopy-assisted reduction to rule out anterior incarceration. Using cystoscopy as a diagnostic tool, it is recommended to exclude the presence of urinary vegetations, as the cause of AUR in pregnancy is external pressure, and cystoscopy is not very meaningful.
Bladder decompression by insertion of an indwelling Foley catheter is the preferred method for most clinicians. An indwelling catheter after catheterization is particularly important [13], because the urethral mucosa edema, bladder neck incarceration, and weak bladder contraction caused by the overstuffed bladder and overstretched detrusor muscle can make the patient unable to urinate after extubation. Our study shows that catheter indwelling for seven days can fully drain urine and improve clinical efficiency. With reasonable clinical care, such as daily cleaning of the urethra, instructing the patient to drink more water, and body position changes (knee-chest position; Figure 2), not only does it not increase the chance of urinary tract infection, but also it can relieve the pressure of the retroflexed uterus on the bladder and subside the urethral mucosal edema. Manual reduction during vaginal examination is another resetting method used as a first-line treatment. Use two fingers to gently press on the retroverted uterus at the posterior vaginal fornix and support the rectum with one finger while gently pressing on the suprapubic area of the abdomen [4,14]. Manual reduction is not recommended after 20 weeks of pregnancy as it increases the risk of preterm birth [14]. If the above processing methods fail, invasive surgery, including colonoscopy-assisted repositioning and laparotomy or laparoscopy, may be considered. For a non-incarcerated uterus, it sticks out of the abdomen as pregnancy increases, which naturally relieves pressure on the bladder. For such patients, invasive procedures should be used with caution [11].
Manual reduction is not recommended after 20 weeks of pregnancy as it increases the risk of preterm birth [14]. If the above processing methods fail, invasive surgery, including colonoscopy-assisted repositioning and laparotomy or laparoscopy, may be considered. For a non-incarcerated uterus, it sticks out of the abdomen as pregnancy increases, which naturally relieves pressure on the bladder. For such patients, invasive procedures should be used with caution [11].
Conclusions
AUR is a rare emergency that can occur at any time in pregnancy. Clinicians need to identify and diagnose in a timely manner based on symptoms and signs and combine them with images to quickly find the cause. Early individualized treatments can relieve bladder pressure in time, reset the uterus, and prevent spontaneous abortion and other destructive consequences for the mother and fetus. Close follow-up and patient education are also important for the recurrence of UR. These include limiting fluid intake before bed, avoiding the Valsalva maneuver, turning to a prone position, leaning forward when urinating, seeking immediate medical advice at the earliest warning sign, and more.
References
- Choong S, Emberton M: Acute urinary retention. BJU Int. 2000, 85:186-201. 10.1046/j.1464-410x.2000.00409.x
- Newell SD, Crofts JF, Grant SR: The incarcerated gravid uterus: complications and lessons learned. Obstet Gynecol. 2014, 123:423-7. 10.1097/AOG.0000000000000102
- Suzuki S, Ono S, Satomi M: Recurrence of urinary retention secondary to retroverted gravid uterus. N Am J Med Sci. 2009, 1:54-57.
- Lam K, Suen CF: Stranded under the Prom: impacted gravid uterus presenting as acute urinary retention. BMJ Case Rep. 2015, 2015:10.1136/bcr-2015-211064
- Danis RB, Brannon RK, Pereira N: Acute urinary retention due to a nonincarcerated retroverted gravid uterus. Int Urogynecol J. 2015, 26:453-4. 10.1007/s00192-014-2547-y
- Mevcha A, Drake MJ: Etiology and management of urinary retention in women. Indian J Urol. 2010, 26:230-5. 10.4103/0970-1591.65396
- Chen JS, Chen SC, Lu CL, Yang HY, Wang P, Huang LC, Liu FS: Acute urinary retention during pregnancy--a nationwide population-based cohort study in Taiwan.
 Medicine (Baltimore). 2016, 95:e3265. 10.1097/MD.0000000000003265
Medicine (Baltimore). 2016, 95:e3265. 10.1097/MD.0000000000003265 - Yang JM, Huang WC: Sonographic findings in acute urinary retention secondary to retroverted gravid uterus: pathophysiology and preventive measures. Ultrasound Obstet Gynecol. 2004, 23:490-5. 10.1002/uog.1039
- Shnaekel KL, Wendel MP, Rabie NZ, Magann EF: Incarceration of the gravid uterus. Obstet Gynecol Surv. 2016, 71:613-9. 10.1097/OGX.0000000000000362
- Hsu PC, Yu MH, Wang CY, Wang YK, Wang CK, Su HY: Asymptomatic uterine incarceration at term: successful management of a rare complication in pregnancy. Taiwan J Obstet Gynecol. 2018, 57:745-9. 10.1016/j.tjog.2018.08.025
- Yohannes P: Ultrasound in acute urinary retention and retroverted gravid uterus. Ultrasound Obstet Gynecol. 2004, 23:427. 10.1002/uog.1071
- Dierickx I, Delens F, Backaert T, Pauwels W, Gyselaers W: Case report: incarceration of the gravid uterus: a radiologic and obstetric challenge. J Radiol Case Rep. 2014, 8:28-36. 10.
 3941/jrcr.v8i7.1854
3941/jrcr.v8i7.1854 - Chauleur C, Vulliez L, Seffert P: Acute urine retention in early pregnancy resulting from fibroid incarceration: proposition for management. Fertil Steril. 2008, 90:1198.e7-10. 10.1016/j.fertnstert.2007.10.008
- Zhuang L, Wang XY, Sang Y, Xu J, He XL: Acute urinary retention in the first and second-trimester of pregnancy: Three case reports. World J Clin Cases. 2021, 9:3130-9. 10.12998/wjcc.v9.i13.3130
Acute Urinary Retention in the First-trimester of Pregnancy: A Case Report
Author Information
Chenyang Dai Corresponding Author
Obstetrics and Gynecology Department, The First People's Hospital of Foshan, Foshan, CHN
Jiali Peng
Obstetrics and Gynecology Department, The First People's Hospital of Foshan, Foshan, CHN
Rufang Chen
Obstetrics and Gynecology Department, The First People's Hospital of Foshan, Foshan, CHN
Ethics Statement and Conflict of Interest Disclosures
Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements
Chenyang Dai and Jiali Peng contributed equally to the work and should be considered co-first authors
Article Information
DOI
10.7759/cureus.23057
Cite this article as:
Dai C, Peng J, Chen R (March 11, 2022) Acute Urinary Retention in the First-trimester of Pregnancy: A Case Report. Cureus 14(3): e23057. doi:10.7759/cureus.23057
Cureus 14(3): e23057. doi:10.7759/cureus.23057
Publication history
Peer review began: March 05, 2022
Peer review concluded: March 10, 2022
Published: March 11, 2022
Copyright
© Copyright 2022
Dai et al. This is an open access article distributed under the terms of the Creative Commons Attribution License CC-BY 4.0., which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
License
This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Acute Urinary Retention in the First-trimester of Pregnancy: A Case Report
Figures etc.
Figure 1: Abdominal ultrasound shows a retroverted uterus and a full bladder.
Abdominal ultrasound shows a retroverted uterus and a full bladder. The left image is the longitudinal section of the probe, and the right image is the transverse section of the probe.
Download full-size
Figure 2: Knee-chest prone position.
Download full-size
9.6
RATED BY 3 READERS
CONTRIBUTE RATING
Scholarly Impact Quotient™ (SIQ™) is our unique post-publication peer review rating process. Learn more here.
What's SIQ™?
Scholarly Impact Quotient™ (SIQ™) is our unique post-publication peer review rating process. SIQ™ assesses article importance and quality by embracing the collective intelligence of the Cureus community-at-large. All registered users are invited to contribute to the SIQ™ of any published article. (Authors cannot rate their own articles.)
High ratings should be reserved for work that is truly groundbreaking in its respective field. Anything above 5 should be considered above average. While all registered Cureus users can rate any published article, the opinion of domain experts is weighted appreciably more than that of non-specialists. An article’s SIQ™ will appear alongside the article after being rated twice and is recalculated with each additional rating.
Visit our SIQ™ page to find out more.
Close
Scholarly Impact Quotient™ (SIQ™)
Scholarly Impact Quotient™ (SIQ™) is our unique post-publication peer review rating process. SIQ™ assesses article importance and quality by embracing the collective intelligence of the Cureus community-at-large. All registered users are invited to contribute to the SIQ™ of any published article. (Authors cannot rate their own articles.)
Already have an account? Sign in.
Enter your email address to receive your free PDF download.
Please note that by doing so you agree to be added to our monthly email newsletter distribution list.
ACUTE URINARY RETENTION AS A COMPLICATION OF PREGNANCY: REPORT OF A CASE | JAMA
ACUTE URINARY RETENTION AS A COMPLICATION OF PREGNANCY: REPORT OF A CASE | JAMA | JAMA Network [Skip to Navigation]This Issue
- Download PDF
- Full Text
-
Share
Twitter Facebook Email LinkedIn
- Cite This
- Permissions
Article
July 12, 1952
Maxwell Spring, M.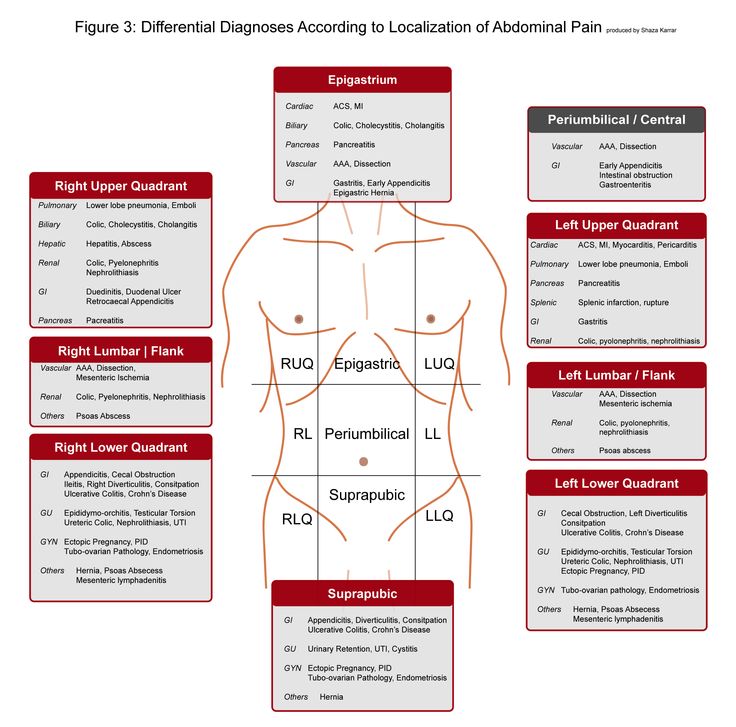 D.; Jesse J. Hymes, M.D.
D.; Jesse J. Hymes, M.D.
Author Affiliations
Bronx, N. Y.
From the Departments of Medicine and Urology, Bronx Hospital, New York.
JAMA. 1952;149(11):1011-1012. doi:10.1001/jama.1952.72930280002009a
Full Text
Abstract
The urinary bladder functions normally during pregnancy; however, when a retroverted uterus is present during the pregnant state, the bladder may not empty properly. Severe uterine retroflexion can result in complete obstruction of the urinary channel. The obstruction is caused by the expanding uterus being securly wedged between the os pubis and the sacrum, with the urethra occluded at the point where pressure is exerted by the cervix.
In the available literature there are three reports of patients who suffered complete urinary retention in pregnancy due to uterine retroflexion: Smellie (1876)1; Crabtree (1942)2; and Burdon, Maurer, and Lich Jr. (1951).3 All of these patients were in the fourth month of pregnancy; the patient reported on in this paper was in the third month. In all four cases the degree of retroflexion was complete, so as to prevent the rise of the uterus out of the true pelvis.
(1951).3 All of these patients were in the fourth month of pregnancy; the patient reported on in this paper was in the third month. In all four cases the degree of retroflexion was complete, so as to prevent the rise of the uterus out of the true pelvis.
Full Text
Add or change institution
- Academic Medicine
- Acid Base, Electrolytes, Fluids
- Allergy and Clinical Immunology
- Anesthesiology
- Anticoagulation
- Art and Images in Psychiatry
- Bleeding and Transfusion
- Cardiology
- Caring for the Critically Ill Patient
- Challenges in Clinical Electrocardiography
- Clinical Challenge
- Clinical Decision Support
- Clinical Implications of Basic Neuroscience
- Clinical Pharmacy and Pharmacology
- Complementary and Alternative Medicine
- Consensus Statements
- Coronavirus (COVID-19)
- Critical Care Medicine
- Cultural Competency
- Dental Medicine
- Dermatology
- Diabetes and Endocrinology
- Diagnostic Test Interpretation
- Diversity, Equity, and Inclusion
- Drug Development
- Electronic Health Records
- Emergency Medicine
- End of Life
- Environmental Health
- Ethics
- Facial Plastic Surgery
- Gastroenterology and Hepatology
- Genetics and Genomics
- Genomics and Precision Health
- Geriatrics
- Global Health
- Guide to Statistics and Methods
- Guidelines
- Hair Disorders
- Health Care Delivery Models
- Health Care Economics, Insurance, Payment
- Health Care Quality
- Health Care Reform
- Health Care Safety
- Health Care Workforce
- Health Disparities
- Health Inequities
- Health Informatics
- Health Policy
- Hematology
- History of Medicine
- Humanities
- Hypertension
- Images in Neurology
- Implementation Science
- Infectious Diseases
- Innovations in Health Care Delivery
- JAMA Infographic
- Law and Medicine
- Leading Change
- Less is More
- LGBTQIA Medicine
- Lifestyle Behaviors
- Medical Coding
- Medical Devices and Equipment
- Medical Education
- Medical Education and Training
- Medical Journals and Publishing
- Melanoma
- Mobile Health and Telemedicine
- Narrative Medicine
- Nephrology
- Neurology
- Neuroscience and Psychiatry
- Notable Notes
- Nursing
- Nutrition
- Nutrition, Obesity, Exercise
- Obesity
- Obstetrics and Gynecology
- Occupational Health
- Oncology
- Ophthalmic Images
- Ophthalmology
- Orthopedics
- Otolaryngology
- Pain Medicine
- Pathology and Laboratory Medicine
- Patient Care
- Patient Information
- Pediatrics
- Performance Improvement
- Performance Measures
- Perioperative Care and Consultation
- Pharmacoeconomics
- Pharmacoepidemiology
- Pharmacogenetics
- Pharmacy and Clinical Pharmacology
- Physical Medicine and Rehabilitation
- Physical Therapy
- Physician Leadership
- Poetry
- Population Health
- Preventive Medicine
- Professional Well-being
- Professionalism
- Psychiatry and Behavioral Health
- Public Health
- Pulmonary Medicine
- Radiology
- Regulatory Agencies
- Research, Methods, Statistics
- Resuscitation
- Rheumatology
- Risk Management
- Scientific Discovery and the Future of Medicine
- Shared Decision Making and Communication
- Sleep Medicine
- Sports Medicine
- Stem Cell Transplantation
- Substance Use and Addiction Medicine
- Surgery
- Surgical Innovation
- Surgical Pearls
- Teachable Moment
- Technology and Finance
- The Art of JAMA
- The Arts and Medicine
- The Rational Clinical Examination
- Tobacco and e-Cigarettes
- Toxicology
- Trauma and Injury
- Treatment Adherence
- Ultrasonography
- Urology
- Users' Guide to the Medical Literature
- Vaccination
- Venous Thromboembolism
- Veterans Health
- Violence
- Women's Health
- Workflow and Process
- Wound Care, Infection, Healing
Save Preferences
Privacy Policy | Terms of Use
Home - Seni
Home - Seni- Seni Club
- Where to buy
- Request a free sample
- Contacts
- Change country
- menu
Urological pads for women with mild to moderate urinary incontinence
More details
Urological pads for women with mild to moderate urinary incontinence
Urological inserts for men with mild to moderate urinary incontinence
More details
Urological inserts for men with mild to moderate urinary incontinence
A wide range of absorbent products for people in need of reliable protection.
More
A wide range of absorbent products for people in need of reliable protection.
Absorbent briefs
Absorbent briefs for active people who need comfortable protection.
More
Absorbent briefs for active people who need comfortable protection.
skin care
Daily skin care products
More details
Cosmetics for daily skin care
A well-chosen product not only ensures the comfort of the person who uses it, but also avoids unnecessary costs.
Find product
It is important to choose the correct size of the product. An incorrectly selected size can lead not only to leakage, but even harm to health. Use the special "form" to select the correct size.
Find size
Seni care products have been helping to properly care for skin that needs especially delicate care for many years. Depending on the purpose, conditions of use and individual characteristics of the skin, seni care cosmetics are conventionally divided into 2 areas: for specialized care and for the care of dry and sensitive skin. Informative packaging design, convenient color identification with special symbols make it easy to choose the right cosmetic product.
Read more
Take care of yourself
The illness of a loved one, whether a child, parent or other family member, changes many aspects of the lives of all those involved.
Read more
seni lady and regular pads
Many women don't know where to start when they experience urinary incontinence.
Read more
MoreThe SeniControl mobile app is a handy tool with which you can easily monitor your urinary incontinence. The application will assess the degree of urinary incontinence and recommend the best urological product that will suit your needs.
Read more
Application available at:
Chronic urinary retention: description of the disease, causes, symptoms, diagnosis and treatment
Chronic urinary retention is the inability to empty the bladder. Symptoms depend on the amount of residual urine and signs of the disease that caused chronic urinary retention.
The large volume of fluid remaining in the bladder is characterized by heaviness in the lower abdomen and shortening of the time between toilet visits. To detect pathology, ultrasound diagnostics of the pelvic organs, urethrocystoscopy and other research methods are used.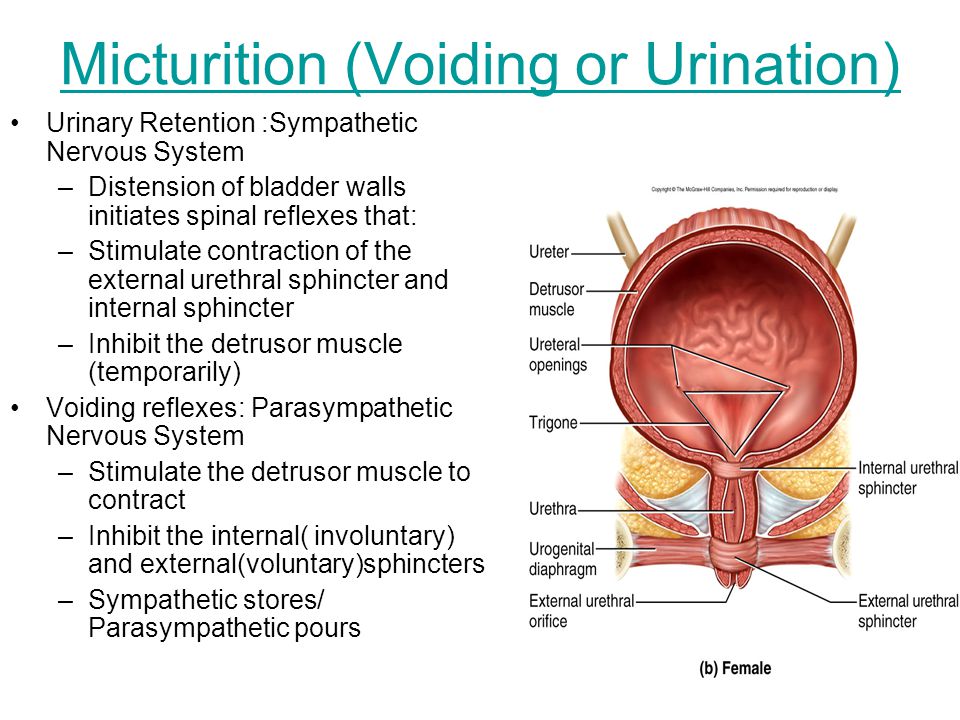
In some cases, chronic urinary retention is due to disorders in the human nervous system. For diagnosis, studies are used to check the functionality of the spinal cord and brain. Along with instrumental methods of examination, the patient is prescribed to take tests.
Urinary retention (ischuria), in most cases, is diagnosed in male patients. The elderly are at risk. The occurrence of chronic urinary retention, which has developed due to disturbances in the functioning of the nervous system, does not depend on the gender of a person. The pathology is treated by a urologist. In the presence of disorders in the nervous system, a neurologist is involved in the treatment.
Symptoms
Chronic urinary incontinence is characterized by the absence of pain. Symptoms of chronic ischuria are expressed as signs of the underlying disease. Patients note a feeling of incomplete release of the bladder from the fluid. Urine excretion occurs in small volumes. In some cases, regular urinary retention leads to bladder overflow. This provokes involuntary leakage of fluid from the urethra.
This provokes involuntary leakage of fluid from the urethra.
Urine changes color and physical characteristics. The liquid becomes saturated in color and acquires an unpleasant odor. In some cases, bloody inclusions are noted in the urine.
It is impossible to independently diagnose chronic urinary retention without the presence of education. If the first symptoms occur, you should contact qualified specialists. The doctor will conduct a series of diagnostic measures. Detection of pathology using modern equipment allows obtaining accurate information about the presence of ischuria and the stage of development of the primary disease. Thanks to this, the specialist can prescribe the most effective treatment for a particular patient.
Causes of occurrence
Chronic urinary retention occurs with the development of various diseases. In some cases, the occurrence of ischuria is possible when taking certain drugs. So tricyclic antidepressants reduce the functionality of the muscular membrane of the bladder.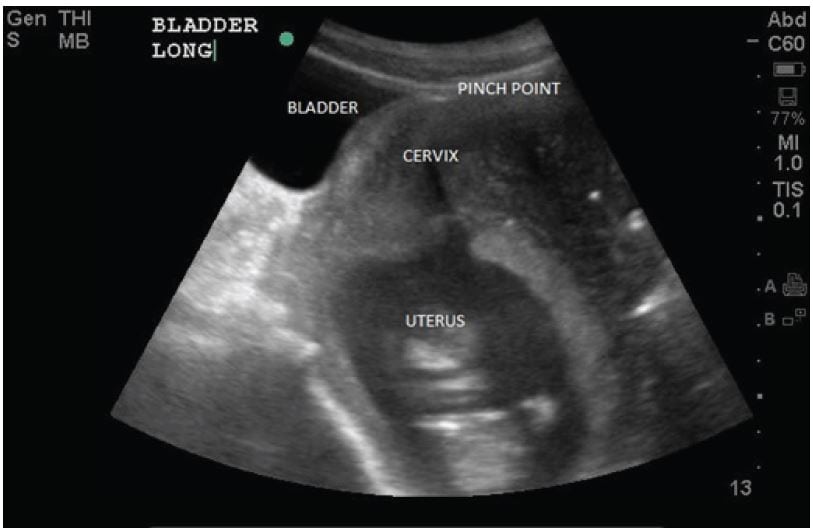 This leads to the accumulation of fluid in the body. In addition, certain drugs can adversely affect the performance of the urinary system.
This leads to the accumulation of fluid in the body. In addition, certain drugs can adversely affect the performance of the urinary system.
In male patients, the occurrence of urinary retention occurs due to the development of sclerosis or prostate cancer. In women, urinary retention is most common, which occurs against the background of prolapse of the pelvic organs. With organ prolapse, the throughput of the urinary tract may decrease. In some cases, ischuria occurs when a benign or malignant neoplasm appears. Chronic urinary retention can occur in women during pregnancy.
The development of foci of inflammation can provoke chronic urinary retention. Pathogenic microorganisms that enter the organs of the urinary system can disrupt its functionality. This leads to systematic incomplete emptying of the bladder. Among the diseases that contribute to the occurrence of chronic urinary retention, note:
-
Cystitis.
-
Balanitis.

-
Urethritis.
-
Prostatitis.
-
Pyelonephritis.
The list of infectious diseases that cause chronic urinary retention does not end there. The development of ischuria is facilitated not only by various infectious diseases of the urinary system, but also by pathologies that provide mechanical resistance to the normal outflow of urine:
-
The presence of stones in the bladder, partially blocking the outflow of fluid.
-
Malignant or benign neoplasm of the prostate.
-
Narrowing of the urethra.
-
Tumor of the urethra, blocking its lumen.
-
Acute form of prostatitis. There is an increase in the size of the prostate. This leads to a partial blockage of the outflow of urine from the bladder.
The last stage of development of phimosis. The disease is observed in men of different ages. Violation of the outflow of urine is due to a lack of tissue of the foreskin. Treatment of the last stage of phimosis is possible only through surgical intervention.
Violation of the outflow of urine is due to a lack of tissue of the foreskin. Treatment of the last stage of phimosis is possible only through surgical intervention.
Often chronic ischuria occurs in patients with neurological diseases. In addition, risk factors include surgical interventions on the pelvic organs. Possible stretching of the muscular membrane of the bladder.
Diagnostics
To identify chronic urinary retention, specialists carry out diagnostic measures. Self-diagnosis is not possible. Delaying a visit to the doctor can lead to the development of various kinds of complications.
The doctor conducts a survey and examination of the patient. The specialist examines the available medical documentation. During the survey, the doctor pays attention to the time interval that has passed since the last urination and to the presence of pain in the lower abdomen.
During the examination, the doctor performs palpation of the lower abdomen.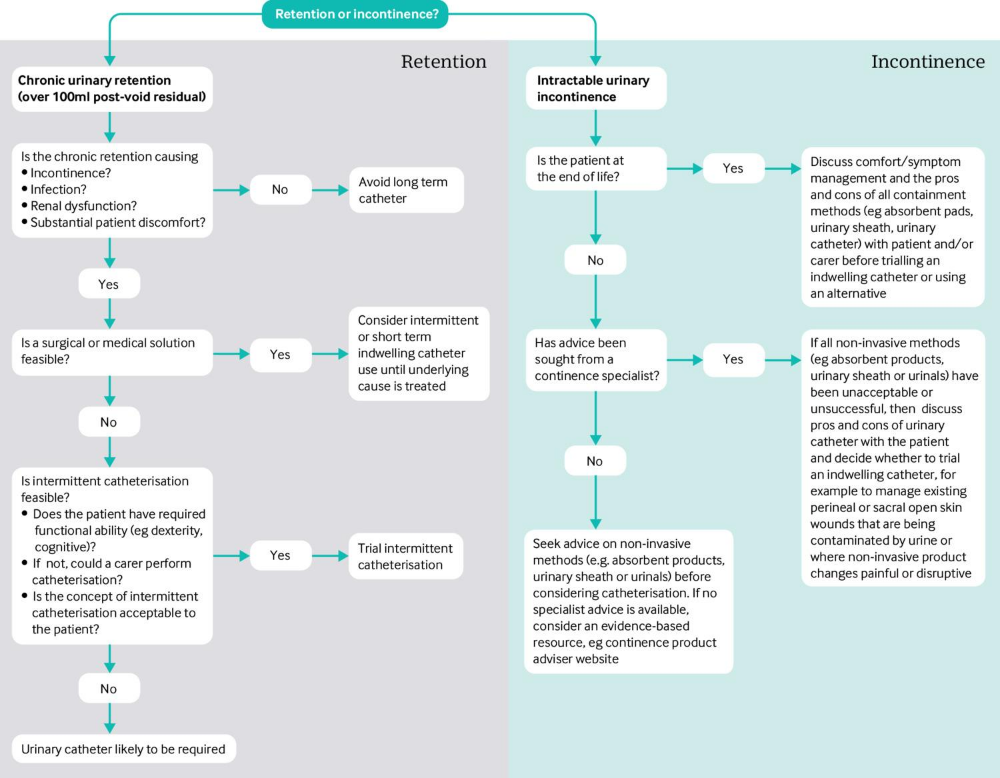 In the presence of residual urine in the bladder, a pronounced increase in the size of the organ is observed. It is important for the doctor to take into account that a small amount of urine output may be associated with a violation of the functionality of the kidneys. In this case, the fluid simply does not fill the bladder. In the presence of this type of pathology, palpation of the bladder will become impossible.
In the presence of residual urine in the bladder, a pronounced increase in the size of the organ is observed. It is important for the doctor to take into account that a small amount of urine output may be associated with a violation of the functionality of the kidneys. In this case, the fluid simply does not fill the bladder. In the presence of this type of pathology, palpation of the bladder will become impossible.
Laboratory research
After the examination, the specialist prescribes laboratory tests. Along with other diagnostic methods, this allows him to more accurately determine the cause of the pathology and take effective measures to eliminate it. The following laboratory tests are assigned:
-
General blood analysis. It is necessary to determine the state of the patient's body. A blood test reveals the presence of an inflammatory process resulting from the accumulation of urine. In the presence of inflammation in the patient's blood, a high level of leukocytes and an increased erythrocyte sedimentation rate are observed.
-
General urine analysis. It is used to determine the violation of the functionality of the organs of the urinary system. With a large volume of fluid in the bladder after emptying, an increased amount of protein and red blood cells is observed in the urine. You can determine the number of bacteria. The fluid at the outlet of the urinary tract is sterile. When collected, a small amount of microorganisms enters it. The level of bacteria exceeding the norm indicates that the infection has entered the organs of the urinary system.
-
Blood chemistry. The doctor pays attention to the indicators of creatinine and urea. Deviation of indicators from the norm may indicate the development of the inflammatory process.
Instrumental diagnosis
If necessary, the doctor prescribes instrumental examinations for the patient. They are performed using specialized medical equipment. The patient is assigned to undergo the following instrumental studies:
-
Ultrasound diagnostics.
 The patient undergoes a study of the bladder, prostate gland, kidneys. Ultrasound allows you to determine the size of internal organs, their echogenicity and identify deviations from the norm. An enlarged prostate gland can lead to urinary problems. Ultrasound examination allows you to determine the presence and size of stones in the kidneys and bladder.
The patient undergoes a study of the bladder, prostate gland, kidneys. Ultrasound allows you to determine the size of internal organs, their echogenicity and identify deviations from the norm. An enlarged prostate gland can lead to urinary problems. Ultrasound examination allows you to determine the presence and size of stones in the kidneys and bladder. -
Cystoscopy. This diagnostic method allows you to visually examine the patient's bladder from the inside. For the study, a specialized cystoscope is used. It is injected into the bladder through the patient's urethra. Cystoscopy is performed under the influence of painkillers. This makes the procedure absolutely painless for the patient. To facilitate the advancement of the cystoscope through the urethra, a gel is used.
-
Retrograde cystography. During the study, a specialized substance is introduced into the patient's bladder. It is opaque to x-rays. After a contrast agent is injected through the urethra, specialists take a series of x-rays.
 So it is possible to obtain information about the location, size of the bladder and urinary canals.
So it is possible to obtain information about the location, size of the bladder and urinary canals.
Gynecological examination
Identification of the causes of chronic urinary retention in female patients can be carried out using a gynecological chair. The gynecologist during the examination determines the presence of prolapse of the pelvic organs. Organ prolapse may partially block the normal excretion of urine from the patient's body. During the examination, the patient is in the supine position. Conducting a gynecological examination reveals not only the prolapse of the pelvic organs, but also the occurrence of malignant or benign formations.
In the process of diagnosis, a disease is detected that has led to the development of chronic urinary retention. In treatment, it is necessary first of all to eliminate the root cause of the pathology. Additionally, the patient may be assigned computed tomography or other examination methods.
Treatment of disease
It is necessary to treat the primary pathology that provoked chronic urinary retention. After the root cause is eliminated, the symptoms disappear, and the outflow of urine returns to normal.
After the root cause is eliminated, the symptoms disappear, and the outflow of urine returns to normal.
Surgery
In some cases, with prolonged stagnation of urine in the pelvic organs, inflammation occurs. This requires immediate treatment and removal of residual fluid from the bladder. Emptying the bladder is possible in two ways.
catheterization. For the procedure, a specialized catheter is used. It is injected into the bladder through the urethra. In order to avoid the entry of pathogenic organisms along the ascending path into the organs of the urinary system, the catheter, the skin at the entrance to the urethra and its mucous membrane are subject to mandatory disinfection.
During the procedure, male patients are in a supine position with legs extended. Women undergo the procedure lying on their backs with their lower limbs apart, bent at the knees.
The doctor disinfects the catheter and the urethral mucosa. After that, a layer of specialized gel is applied to the instrument and into the urethra, which serves to facilitate the procedure. The catheter is inserted into the urethra until the outflow of urine begins through it. The specialist attaches a urinal used to collect fluid to the catheter.
The catheter is inserted into the urethra until the outflow of urine begins through it. The specialist attaches a urinal used to collect fluid to the catheter.
To avoid infection and the development of diseases, the catheter is kept in the bladder for as little time as possible. There are several contraindications to the procedure:
-
Acute form of prostatitis.
-
Significant narrowing of the urethra due to neoplasms, pelvic organ prolapse, or other causes.
-
Rupture of the urethra.
-
Uncontrolled erection not related to the patient's arousal.
Cystostomy
If there is no possibility to carry out catheterization, then surgical intervention is performed through the anterior wall of the abdomen. The puncture is performed using a trocar - a specialized medical instrument.
The patient is in the supine position during the procedure. To avoid pain in the patient, the doctor injects an anesthetic drug. The operation is performed under the influence of local anesthesia. The procedure is carried out in the following order:
The operation is performed under the influence of local anesthesia. The procedure is carried out in the following order:
-
The doctor anesthetizes the area of the operation.
-
At the insertion site of the instrument, the specialist makes an incision in the skin. This facilitates tissue puncture with a trocar.
-
The surgeon pierces the front wall of the abdomen and the bladder with a sharp movement.
-
When piercing, the doctor needs to monitor the depth of insertion of the instrument. Too deep insertion can lead to injury to the opposite wall of the bladder.
-
A catheter is immersed into the trocar tube and sutured to the skin. This is necessary in order to eliminate the risk of spontaneous loss.
After the operation, the fluid from the bladder will be completely removed outside, bypassing the urinary tract. In order to avoid disruption of the functionality of the muscular membrane of the bladder, it is necessary to carry out certain exercises.