Urinary incontinence after c section
The Connection Between C-Sections and Urinary Incontinence
Posted on
by Michelle Stepp
Finding out you’re pregnant can be a time that is full of excitement and joy! However, sometimes there may be some topics of concern that may come up along your journey. You might have a pre-existing health condition or a problem arises and your doctor may feel that having a traditional vaginal birth may be too risky. Some serious thoughts and conversations might lie ahead and the topic of delivering your child via c-section could be the safest choice.
What is a C-Section and When is it Needed?
What is a c-section?
Cesarean birth, which is often referred to as a c-section, is a surgical procedure performed by a doctor to deliver a newborn through an incision that is made in the abdomen and uterus. It may be a safer option rather than vaginal birth if the goal is to protect the newborn’s health or if the mother has a medical condition that can affect the pregnancy. A c-section can be either scheduled to coincide with the planned due date or it can be an emergency if the mother or baby’s health is in immediate danger.
What are some medical reasons a c-section may be needed?
A c-section may be the best course of action to take due to potential complications that can make vaginal birth unsafe for the mother and/or her baby. A c-section can be necessary for any of the following reasons:
- The baby is too large for a vaginal birth. A very large baby sometimes simply cannot fit through the vaginal opening without causing significant damage.
- The baby is either sideways or breech (feet first instead of head first) in the womb. The position of the baby in this way can be dangerous as there is a risk that oxygen supply through the umbilical cord could be cut off if the baby gets stuck during delivery.
- The mother has a medical condition such as high blood pressure or diabetes. High blood pressure can be risky during pregnancy due to the stress that is put on the heart.
 When there is a high amount of sugar in the blood, as with diabetes, nerves and blood vessels can be damaged. Both of these medical conditions can make a c-section more favorable for the safety of the mother and her baby.
When there is a high amount of sugar in the blood, as with diabetes, nerves and blood vessels can be damaged. Both of these medical conditions can make a c-section more favorable for the safety of the mother and her baby. - If the mother has had a previous c-section, she is at a greater risk for complications during childbirth. There can be scar tissue buildup after each c-section making another incision more difficult and risk damage to the bladder or bowel.
- The mother might have an infection that could potentially be passed on to the baby during vaginal birth. As a safety precaution, a c-section would be a better choice in this case.
- When there are multiple babies in the womb, a c-section is a wise decision so that no harm is done to either the babies or the mother.
Can a C-Section Cause Incontinence?
Childbirth in itself causes strain and tears on a woman’s body. The uterus starts getting heavier as the infant grows and the surrounding structures begin to stretch and weaken.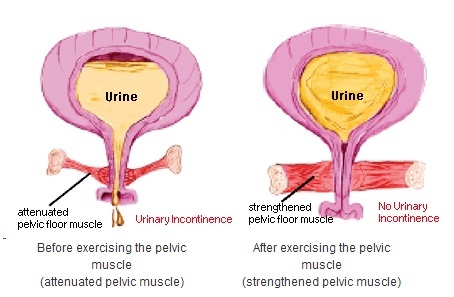 Some women think that having a c-section will prevent them from side effects of vaginal birth like urinary incontinence or fecal incontinence. However, studies have shown that having a c-section doesn’t protect women from suffering from urinary or fecal incontinence. Bladder issues after a c-section are quite common.
Some women think that having a c-section will prevent them from side effects of vaginal birth like urinary incontinence or fecal incontinence. However, studies have shown that having a c-section doesn’t protect women from suffering from urinary or fecal incontinence. Bladder issues after a c-section are quite common.
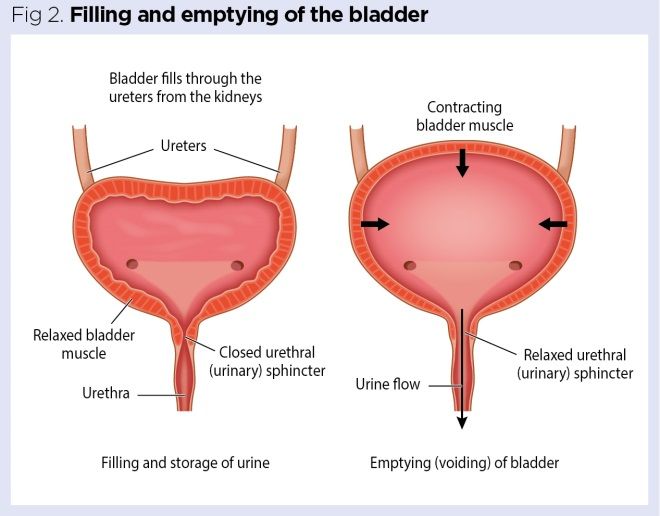
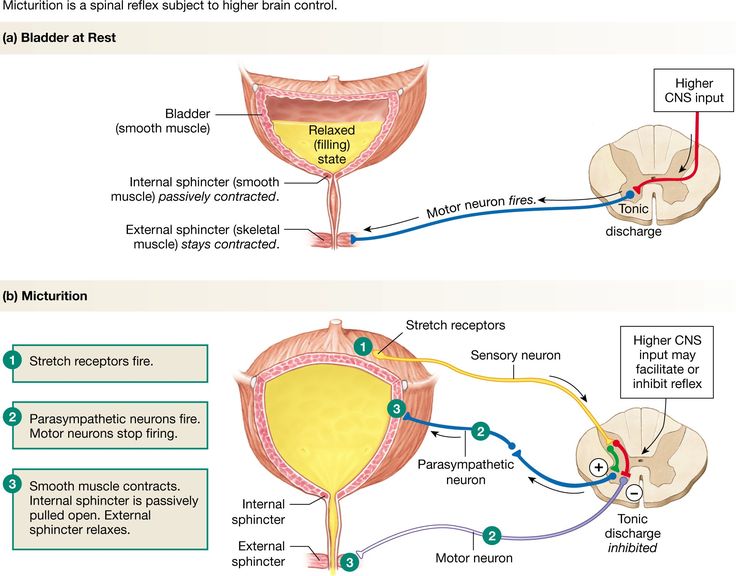
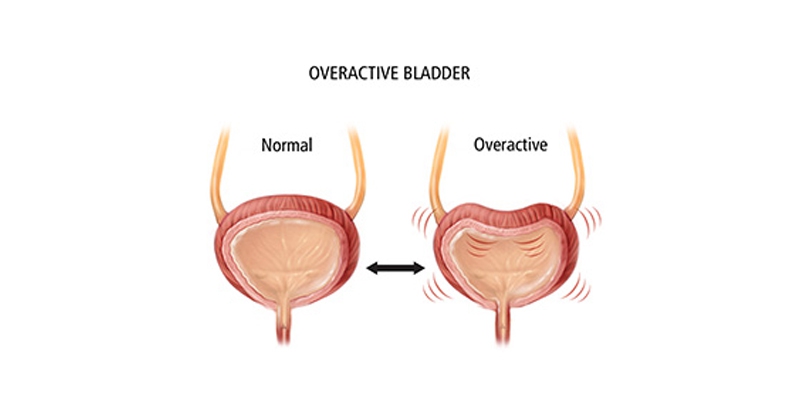
After the abdominal incision is made during a c-section, scar tissue is formed from collagen during the healing process. The collagen fibers of this scar tissue can extend deep into the layers below the skin and create bladder problems. Bladder issues after a c-section such as urinary incontinence can result when this scar tissue attaches to the wall of the bladder. After a woman gives birth, things begin to reduce back down in size, this scar tissue pulls on the bladder making her feel as though she needs to urinate more urgently (urge incontinence) or more often (overactive bladder).
How Long Does Urinary Incontinence from a C-Section Last?
Urinary incontinence from a c-section can take up to six months, or even longer for some women, to get their bladder functioning like normal again.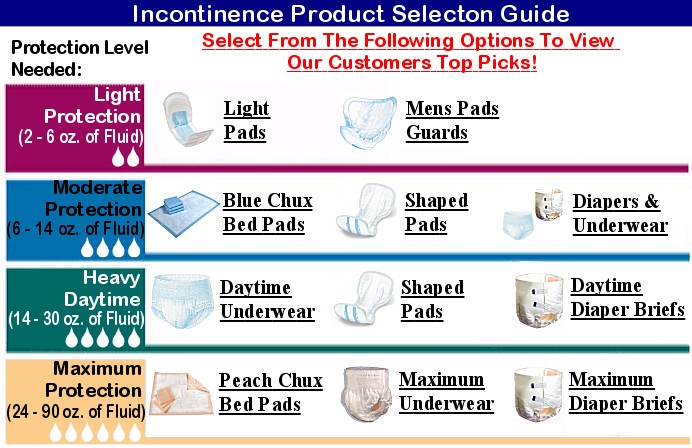 There are several things that a woman can do to help the process along and get it back faster. In the interim, considering the use of incontinence products such as pads, liners, and protective underwear can help women get through the more difficult times.
There are several things that a woman can do to help the process along and get it back faster. In the interim, considering the use of incontinence products such as pads, liners, and protective underwear can help women get through the more difficult times.
How You Can Improve Urinary Incontinence Symptoms from a C-Section
Some of the ways a woman can treat urinary incontinence from a c-section to help her bladder get back to its normal function are:
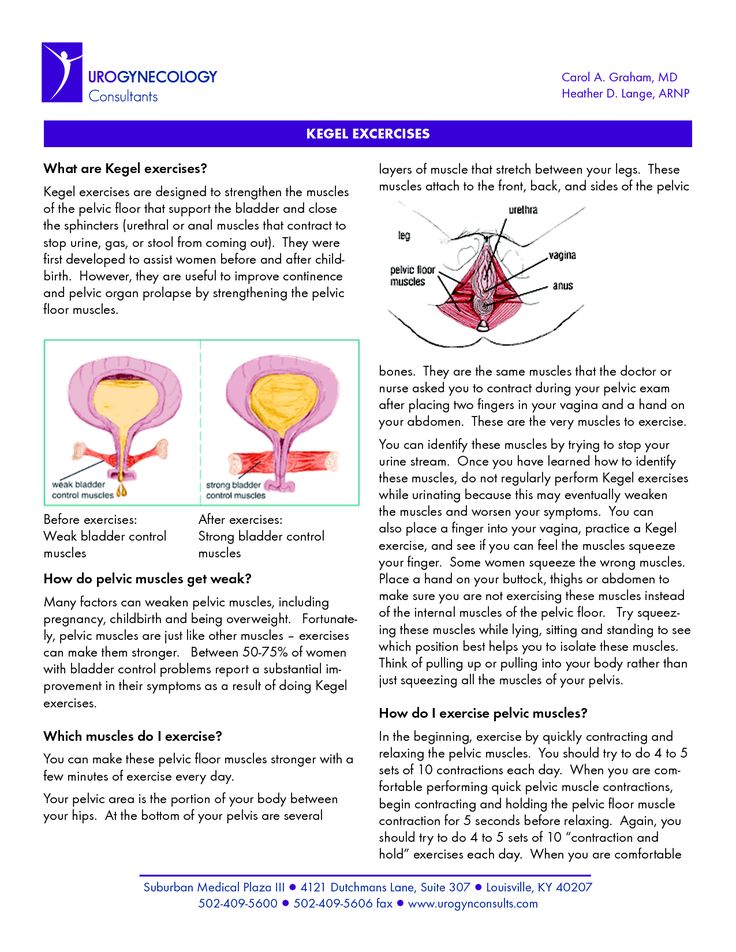
Kegel Exercises
Strengthening the pelvic floor muscles after delivery is an important part of regaining bladder control. The stronger and more elastic these muscles are, the less stress or urge incontinence is experienced. Starting kegel exercises right after childbirth can greatly reduce urinary incontinence symptoms and get you on the path for normal bladder function sooner rather than later.
A Pessary Ring
A pessary ring is a small, soft, silicone vaginal ring that is inserted into the vagina.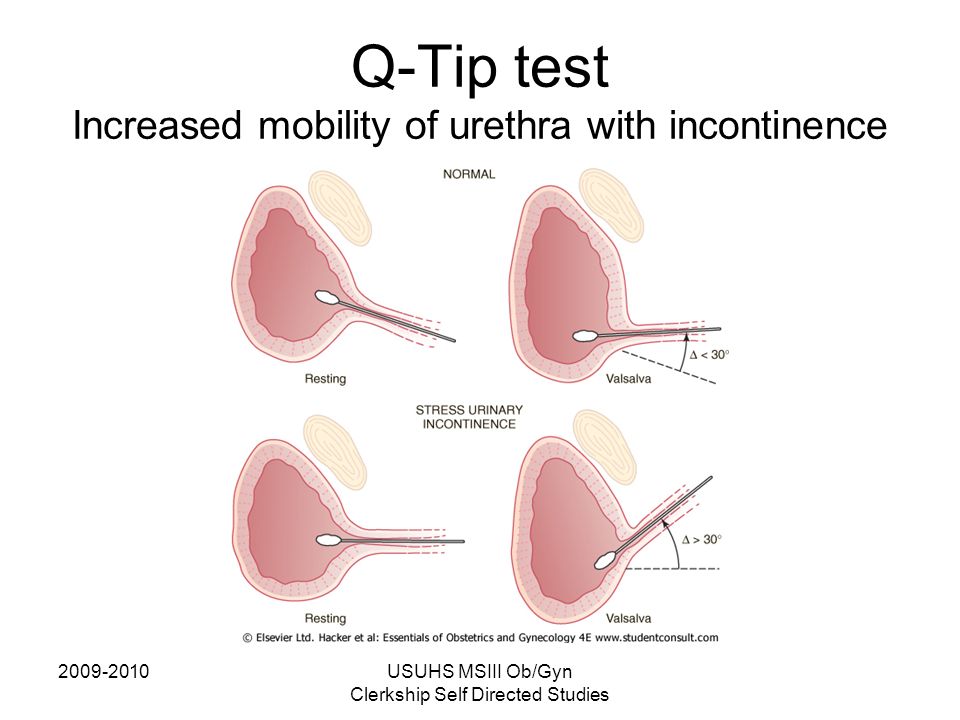 Women who can benefit from a pessary ring are those that have urinary incontinence that seems to be persistent. The pessary ring is placed inside the vagina to act as a “speed bump” for the urethra and left there throughout the day. Some women prefer to use a pessary ring only when they engage in activities, while others put it in place in the morning and remove it in the evening. This device can be very helpful for women experiencing bladder issues after a c-section.
Women who can benefit from a pessary ring are those that have urinary incontinence that seems to be persistent. The pessary ring is placed inside the vagina to act as a “speed bump” for the urethra and left there throughout the day. Some women prefer to use a pessary ring only when they engage in activities, while others put it in place in the morning and remove it in the evening. This device can be very helpful for women experiencing bladder issues after a c-section.
Electrical Stimulation Therapy
By sending mild electrical currents to the muscles in the pelvic floor that are involved in urination, these muscles then contract. By repeating this electrical stimulation pulse, the pelvic floor muscles begin to strengthen, producing a similar effect to what kegel exercises do. A doctor can perform this therapy or the patient can be given a unit to use in the privacy of their own home to help relieve their urinary incontinence symptoms.
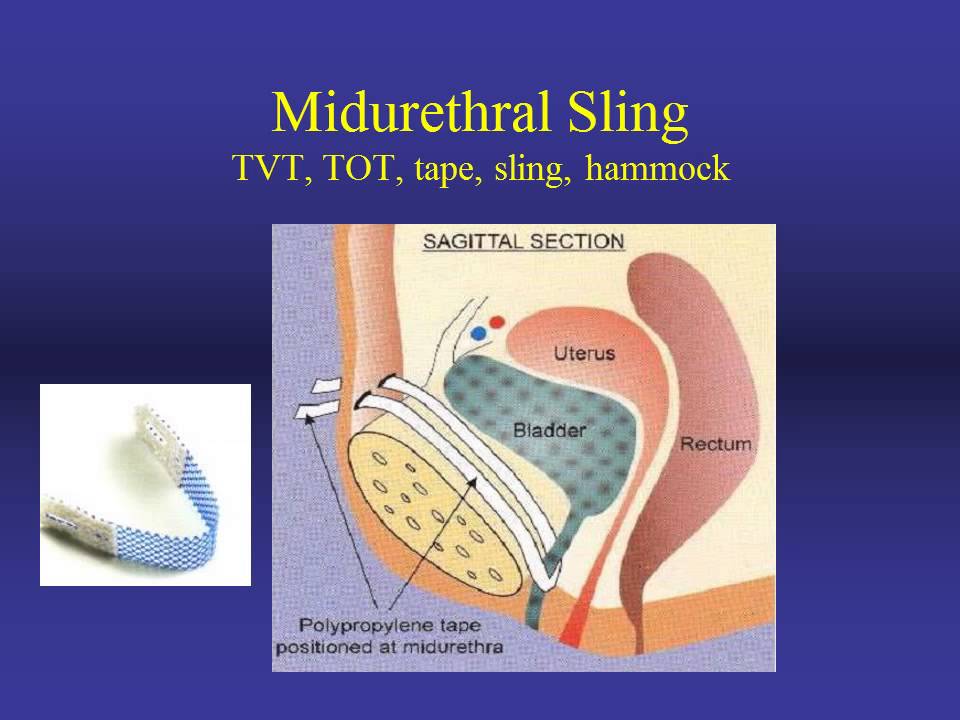
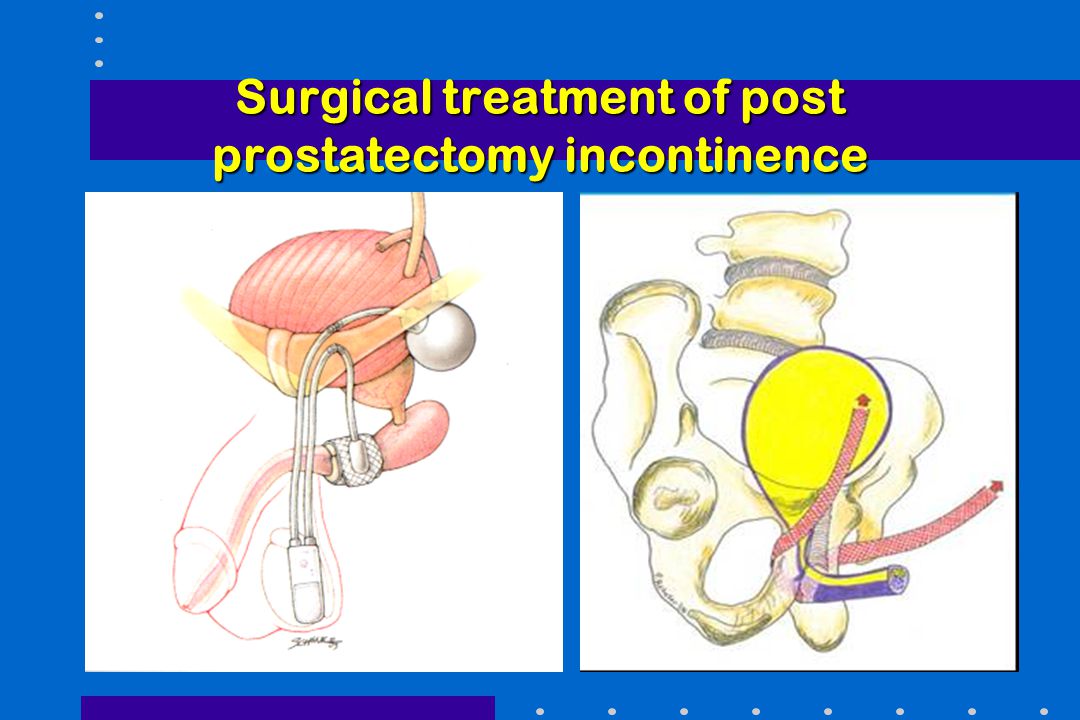
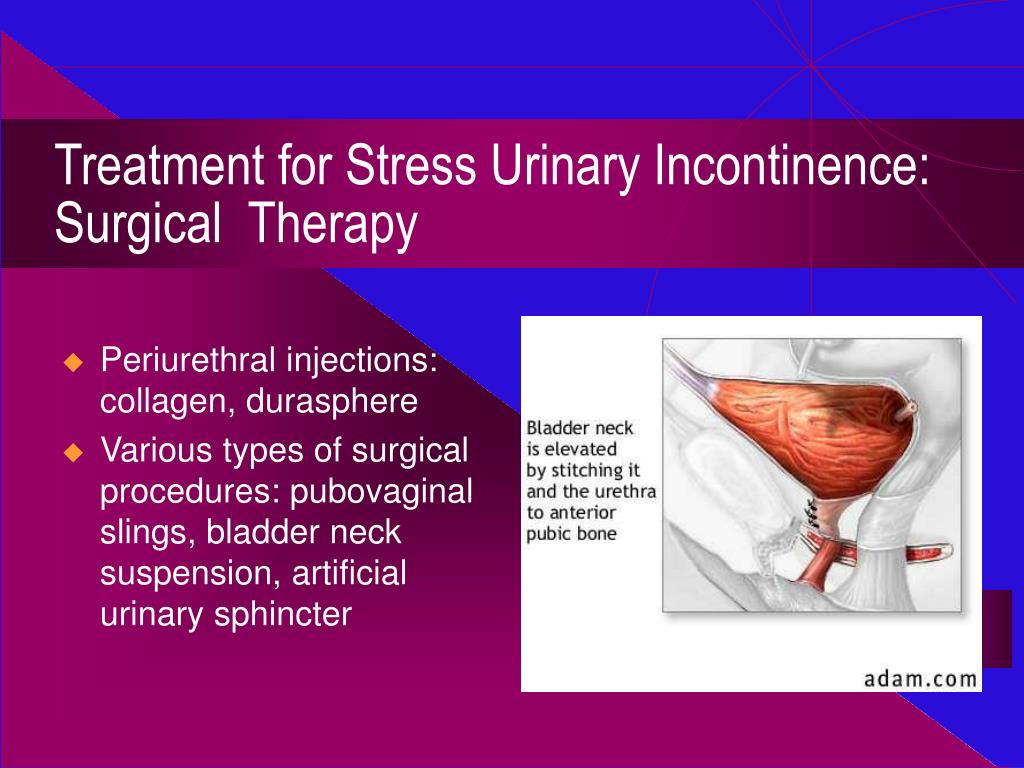
Sling Surgery
One of the most common surgeries for urinary incontinence is sling surgery. In this minimally invasive procedure, the surgeon inserts a U- shaped, mesh sling that permanently lifts and supports the urethra like a hammock. This procedure is quick and important to note that it is also permanent, so women that choose this option should not consider any more pregnancies.
In this minimally invasive procedure, the surgeon inserts a U- shaped, mesh sling that permanently lifts and supports the urethra like a hammock. This procedure is quick and important to note that it is also permanent, so women that choose this option should not consider any more pregnancies.
Lifestyle Changes
There are many lifestyle changes that can also help women with urinary incontinence to regain bladder control. Many of these might be good to try before choosing some of the more permanent options.
- Remain at a healthy weight. Carrying around extra pounds can put pressure on the bladder and lead to urinary incontinence.
- Maintain a healthy diet. Alcohol, caffeine, and spicy foods tend to aggravate the bladder causing it to contract more often, making urine harder to control.
- Stay hydrated. Try to drink the recommended 8 ounces of water each day. Avoiding water as a way to control the number of times you need to use the restroom can result in a urinary tract infection or dehydration.
 Both are not good for a healthy bladder.
Both are not good for a healthy bladder. - Stop smoking. Nicotine causes bladder muscles to spasm and women who smoke also often have a chronic cough. Frequent coughing episodes lead to urinary incontinence because of the pressure continuously put on the bladder.
- Pads, liners, and other incontinence products can help absorb leaks and help with urinary incontinence. There are so many options available to women that are concerned about discreetness and living a dignified lifestyle.
As you can see, there is a connection between c-sections and urinary incontinence but you don’t have to let your bladder control your life. There are many options available to treat bladder issues after a c-section such as urinary incontinence, even if you feel that you have exhausted all other avenues.
For questions about any of the incontinence products we carry to help with urinary or fecal incontinence, give us a call. One of our Personally Delivered Product Experts is happy to help.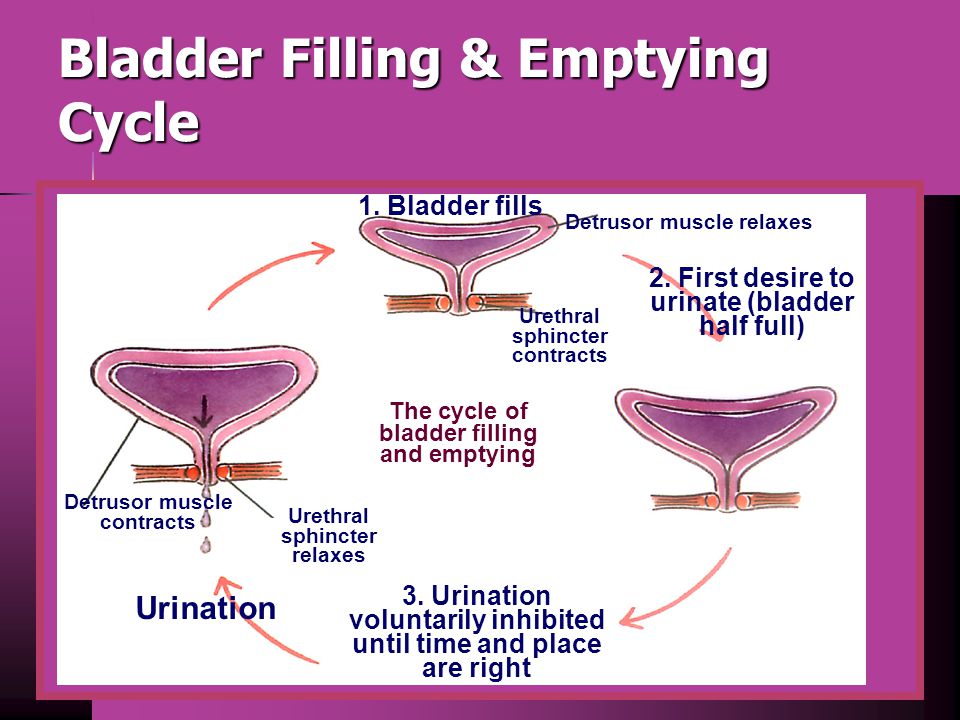
Popular Incontinence Products for Women
Posted in Incontinence ResourcesTagged c-section incontinence, incontinence after c-section, incontinence after giving birth
Urinary incontinence after vaginal delivery or cesarean section
. 2003 Mar 6;348(10):900-7.
doi: 10.1056/NEJMoa021788.
Guri Rortveit 1 , Anne Kjersti Daltveit, Yngvild S Hannestad, Steinar Hunskaar; Norwegian EPINCONT Study
Affiliations
Affiliation
- 1 Epidemiology of Incontinence in the County of Nord-Trøndelag study, Bergen, Norway. [email protected]
- PMID: 12621134
- DOI: 10.
 1056/NEJMoa021788
1056/NEJMoa021788
Free article
Guri Rortveit et al. N Engl J Med. .
Free article
. 2003 Mar 6;348(10):900-7.
doi: 10.1056/NEJMoa021788.
Authors
Guri Rortveit 1 , Anne Kjersti Daltveit, Yngvild S Hannestad, Steinar Hunskaar; Norwegian EPINCONT Study
Affiliation
- 1 Epidemiology of Incontinence in the County of Nord-Trøndelag study, Bergen, Norway. [email protected]
- PMID: 12621134
- DOI: 10.
 1056/NEJMoa021788
1056/NEJMoa021788
Abstract
Background: It is uncertain whether women who deliver by cesarean section have an increased risk of urinary incontinence as compared with nulliparous women and whether women who deliver vaginally have an even higher risk.
Methods: We studied 15,307 women enrolled in the Epidemiology of Incontinence in the County of Nord-Trøndelag (EPINCONT) study, which involved a community-based cohort. The data base for this study was linked to data from the Medical Birth Registry of Norway. We included women who answered questions related to urinary incontinence, were younger than 65 years of age, and had had no deliveries, cesarean sections only, or vaginal deliveries only.
Results: The prevalence of any incontinence was 10.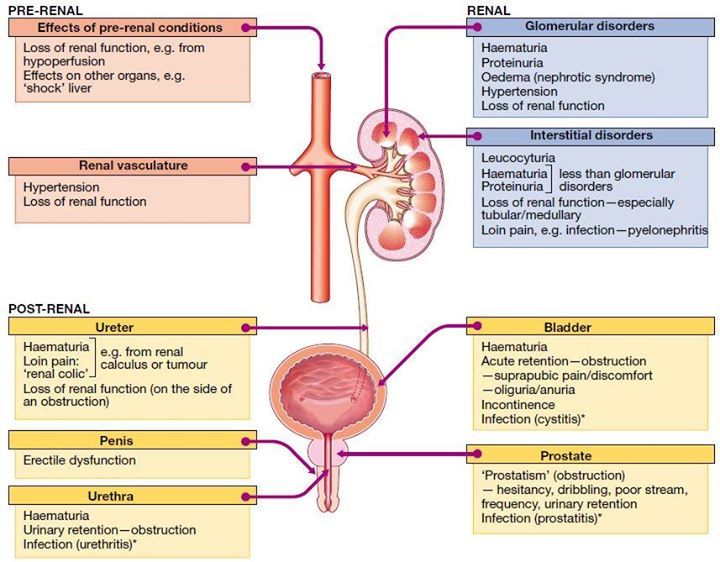 1 percent in the nulliparous group; age-standardized prevalences were 15.9 percent in the cesarean-section group and 21.0 percent in the vaginal-delivery group. Corresponding figures for moderate or severe incontinence were 3.7 percent, 6.2 percent, and 8.7 percent, respectively; figures for stress incontinence were 4.7 percent, 6.9 percent, and 12.2 percent, respectively; figures for urge incontinence were 1.6 percent, 2.2 percent, and 1.8 percent, respectively; and figures for mixed-type incontinence were 3.1 percent, 5.3 percent, and 6.1 percent, respectively. As compared with nulliparous women, women who had cesarean sections had an adjusted odds ratio for any incontinence of 1.5 (95 percent confidence interval, 1.2 to 1.9) and an adjusted odds ratio for moderate or severe incontinence of 1.4 (95 percent confidence interval, 1.0 to 2.1). Only stress and mixed-type incontinence were significantly associated with cesarean sections. The adjusted odds ratio for any incontinence associated with vaginal deliveries as compared with cesarean sections was 1.
1 percent in the nulliparous group; age-standardized prevalences were 15.9 percent in the cesarean-section group and 21.0 percent in the vaginal-delivery group. Corresponding figures for moderate or severe incontinence were 3.7 percent, 6.2 percent, and 8.7 percent, respectively; figures for stress incontinence were 4.7 percent, 6.9 percent, and 12.2 percent, respectively; figures for urge incontinence were 1.6 percent, 2.2 percent, and 1.8 percent, respectively; and figures for mixed-type incontinence were 3.1 percent, 5.3 percent, and 6.1 percent, respectively. As compared with nulliparous women, women who had cesarean sections had an adjusted odds ratio for any incontinence of 1.5 (95 percent confidence interval, 1.2 to 1.9) and an adjusted odds ratio for moderate or severe incontinence of 1.4 (95 percent confidence interval, 1.0 to 2.1). Only stress and mixed-type incontinence were significantly associated with cesarean sections. The adjusted odds ratio for any incontinence associated with vaginal deliveries as compared with cesarean sections was 1. 7 (95 percent confidence interval, 1.3 to 2.1), and the adjusted odds ratio for moderate or severe incontinence was 2.2 (95 percent confidence interval, 1.5 to 3.1). Only stress incontinence (adjusted odds ratio, 2.4; 95 percent confidence interval, 1.7 to 3.2) was associated with the mode of delivery.
7 (95 percent confidence interval, 1.3 to 2.1), and the adjusted odds ratio for moderate or severe incontinence was 2.2 (95 percent confidence interval, 1.5 to 3.1). Only stress incontinence (adjusted odds ratio, 2.4; 95 percent confidence interval, 1.7 to 3.2) was associated with the mode of delivery.
Conclusions: The risk of urinary incontinence is higher among women who have had cesarean sections than among nulliparous women and is even higher among women who have had vaginal deliveries. However, these findings should not be used to justify an increase in the use of cesarean sections.
Copyright 2003 Massachusetts Medical Society
Similar articles
-
[Mode of delivery on urinary incontinence].
Yang X, Zheng H, Liao QP, Tao RX, Fu C, Peng XL, Wang D, Luan YQ.
 Yang X, et al. Zhonghua Fu Chan Ke Za Zhi. 2004 Oct;39(10):662-5. Zhonghua Fu Chan Ke Za Zhi. 2004. PMID: 16144561 Chinese.
Yang X, et al. Zhonghua Fu Chan Ke Za Zhi. 2004 Oct;39(10):662-5. Zhonghua Fu Chan Ke Za Zhi. 2004. PMID: 16144561 Chinese. -
Risk factors for stress, urge or mixed urinary incontinence in Italy.
Parazzini F, Chiaffarino F, Lavezzari M, Giambanco V; VIVA Study Group. Parazzini F, et al. BJOG. 2003 Oct;110(10):927-33. BJOG. 2003. PMID: 14550363
-
The effect of pregnancy and mode of delivery on the prevalence of urinary and fecal incontinence.
McKinnie V, Swift SE, Wang W, Woodman P, O'Boyle A, Kahn M, Valley M, Bland D, Schaffer J. McKinnie V, et al. Am J Obstet Gynecol. 2005 Aug;193(2):512-7; discussion 517-8. doi: 10.1016/j.ajog.2005.03.056. Am J Obstet Gynecol. 2005. PMID: 16098879
-
Female urinary incontinence, from pregnancy to menopause: a review of epidemiological and pathophysiological findings.
Fritel X, Ringa V, Quiboeuf E, Fauconnier A. Fritel X, et al. Acta Obstet Gynecol Scand. 2012 Aug;91(8):901-10. doi: 10.1111/j.1600-0412.2012.01419.x. Epub 2012 May 22. Acta Obstet Gynecol Scand. 2012. PMID: 22497363 Review.
-
Does cesarean section reduce postpartum urinary incontinence? A systematic review.
Press JZ, Klein MC, Kaczorowski J, Liston RM, von Dadelszen P. Press JZ, et al. Birth. 2007 Sep;34(3):228-37. doi: 10.1111/j.1523-536X.2007.00175.x. Birth. 2007. PMID: 17718873 Review.
See all similar articles
Cited by
-
Urinary incontinence and related quality of life among elderly women in Tabas, South Khorasan, Iran.
Najafi Z, Morowatisharifabad MA, Jambarsang S, Rezaeipandari H, Hemayati R.
 Najafi Z, et al. BMC Urol. 2022 Dec 31;22(1):214. doi: 10.1186/s12894-022-01171-9. BMC Urol. 2022. PMID: 36587231 Free PMC article.
Najafi Z, et al. BMC Urol. 2022 Dec 31;22(1):214. doi: 10.1186/s12894-022-01171-9. BMC Urol. 2022. PMID: 36587231 Free PMC article. -
Investigation on prevalence and risk factors associated with genitourinary syndrome of menopause in middle-aged and older women in Beijing community: a cross sectional study.
Zhu Y, Wei J, Yang X, Zhu W, Zhang W. Zhu Y, et al. BMC Womens Health. 2022 Dec 30;22(1):558. doi: 10.1186/s12905-022-02099-w. BMC Womens Health. 2022. PMID: 36585649 Free PMC article. Review.
-
URINARY INCONTINENCE - FROM CHILDHOOD ONWARDS.
Živković D, Franić D, Kojović V. Živković D, et al. Acta Clin Croat. 2022 Mar;61(1):115-123. doi: 10.20471/acc.2022.61.01.14. Acta Clin Croat.
 2022. PMID: 36398081 Free PMC article. Review.
2022. PMID: 36398081 Free PMC article. Review. -
Investigating the Efficacy of an 18-Week Postpartum Rehabilitation and Physical Development Intervention on Occupational Physical Performance and Musculoskeletal Health in UK Servicewomen: Protocol for an Independent Group Study Design.
Elliott-Sale KJ, Bostock EL, Jackson T, Wardle SL, O'Leary TJ, Greeves JP, Sale C. Elliott-Sale KJ, et al. JMIR Res Protoc. 2022 Jun 1;11(6):e32315. doi: 10.2196/32315. JMIR Res Protoc. 2022. PMID: 35648463 Free PMC article.
-
Effects of lateral episiotomy on the emergence of urinary incontinence during the first postpartum year in primiparas: prospective cohort study.
Živković K, Orešković S, Cerovac A, Milošević M, Luetić AT, Prka M, Habek D, Lukanović D, Spagnol G, Živković N.
 Živković K, et al. Prz Menopauzalny. 2021 Dec;20(4):163-169. doi: 10.5114/pm.2021.110956. Epub 2021 Nov 23. Prz Menopauzalny. 2021. PMID: 35069067 Free PMC article.
Živković K, et al. Prz Menopauzalny. 2021 Dec;20(4):163-169. doi: 10.5114/pm.2021.110956. Epub 2021 Nov 23. Prz Menopauzalny. 2021. PMID: 35069067 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Urinary incontinence in women after childbirth
One of the manifestations of pelvic floor dysfunction in women associated with overstretching or tearing of the soft tissues of the pelvis during childbirth. It does not have to be a rapid delivery or delivery of a large fetus. Often this is observed after normal childbirth. I must say that a caesarean section also does not completely relieve a woman from the likelihood of urinary incontinence. Recovery after childbirth can take several months and a long period of urinary incontinence causes a lot of inconvenience.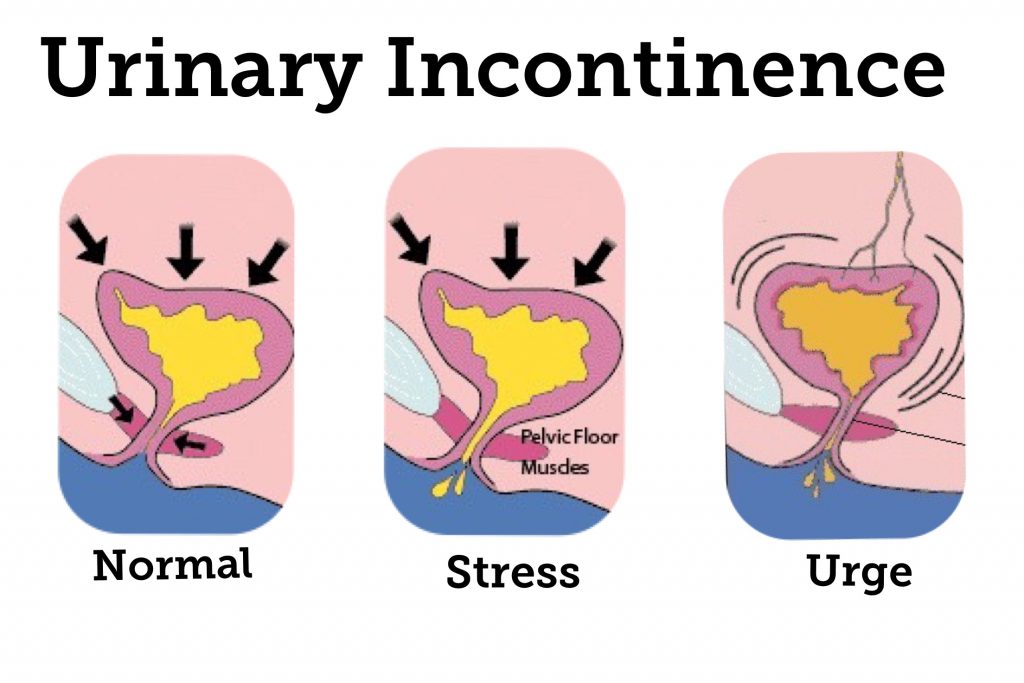 nine0003
nine0003
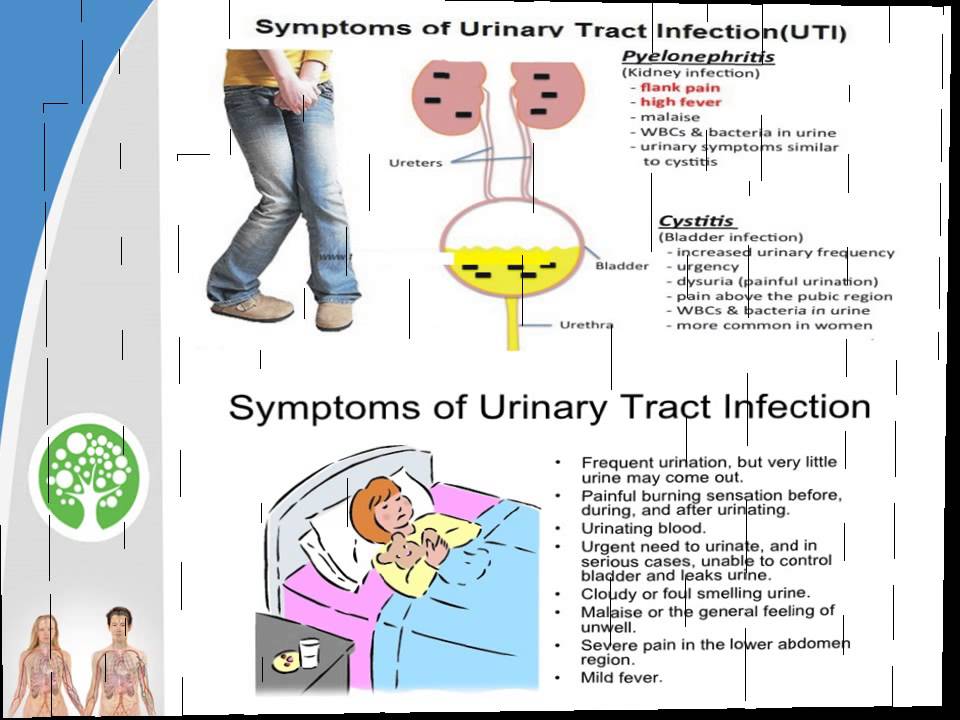
There are several types of postpartum incontinence: Stress incontinence, when Involuntary release of urine occurs when coughing, sneezing, or exercising. Imperative, which occurs with a sudden urge to urinate, and the woman does not have time to react in time. Involuntary, when urine is released little by little throughout the day or continues for some time after emptying the bladder.
Why?
Involuntary excretion of urine occurs as a result of dysfunction of the pelvic floor muscles. During childbirth, they stretch, become less elastic. Various factors can provoke urination disorders: trauma during childbirth, inflammation in the genitourinary tract, and features of the connective tissue that a woman has. nine0003
How to confirm the diagnosis?
Sometimes, in order to find an effective treatment, a gynecological examination, urine analysis and ultrasound examination of the uterus and bladder and measurement of the strength of the pelvic floor muscles with a special device - pneumatic digital perineometer iEASE XFT -0010 are enough.
In complex cases, it is necessary to involve a urologist and additional research methods - cystoscopy, urofluometry, MRI, etc. nine0003
What to do?
If the problem does not disappear within a couple of weeks after childbirth, it must be actively addressed:
After making sure that there is no inflammatory process in the kidneys and bladder, physiotherapy exercises and modern physiotherapy can be used . To enhance the effect, autoplasma therapy has been successfully used recently. Given that most women are breastfeeding, the use of drugs is highly undesirable, and often absolutely contraindicated. If conservative methods are ineffective, options for surgical correction should be considered. Full information on surgical methods of treatment can be obtained at the appointment of a urologist. nine0003 The main thing to understand is that urinary incontinence should not be tolerated - it should be eliminated as soon as possible. Our clinic practices a comprehensive approach to solving the problem of urinary incontinence after childbirth. Come to your first postpartum appointment no later than one month after delivery. If you have problems with urinary incontinence, come early. Diagnosis starts with physical examination, tests, ultrasound and pelvic floor strength measurement perineometer iEASE XFT -0010 . Treatment begins with the correction of disorders identified during the examination, plus elementary methods of Kegel therapeutic exercises. In the process of rehabilitation, the mode of electromyostimulation of the pelvic floor muscles, selected according to the first test, is added, it is possible to use parallel magnetic laser therapy and PRP autoplasma therapy. There are two types of incontinence: in one case it is associated with an irresistible urge (as they say, "did not get to the toilet"), in the other case, involuntary urination occurs with an increase in intra-abdominal pressure during physical exertion, laughter, coughing, sneezing, etc. The problem in most cases is not resolved by itself, causing physical and psychological inconvenience and suffering (the need to walk around with pads and diapers) and reducing the quality of life, including intimate life. They are embarrassed to talk about it, and compared to how many people are prone to this problem, only a few seek help. Often they simply do not know who exactly to turn to - they go to a gynecologist, and to a therapist, and to a neuropathologist, while this should be done comprehensively and always with the participation of a urologist. nine0003 1. Slow contractions: tighten the muscles as if to stop urination, slowly count to three. To relax. Special therapeutic exercises also help to strengthen the muscles of the small pelvis. 1. I.P. lying on your back. We exhale, draw in the stomach, pull the knees to the chest. There is no need to despair: although treatment is not a simple process due to the large number of components involved in the formation of this syndrome, it is very effective. In all cases, it begins with conservative methods: medicines, physiotherapy and, of course, the therapeutic exercises we have already mentioned. Refrain from activities that increase intra-abdominal pressure. If conservative treatment does not help, low-traumatic surgical methods come to the rescue in the form of imposing various types of loops. nine0003 Sometimes an episiotomy is done for the benefit of the baby and mother. Healing is very fast due to tissue matching and a powerful hormonal explosion. The main task of the mother, if she has stitches, is to keep them clean. This, of course, is hygiene (washing twice a day, from front to back, you can use a decoction of chamomile or a weak solution of potassium permanganate) and ensuring oxygen access. Associated with the latter is the ban on underwear and pads, which causes violent protest among women in maternity hospitals. One should not underestimate such an important moment as the normalization of the stool on the third day after childbirth. Defecation does not provoke the divergence of the sutures, on the contrary, this stool retention can lead to trouble, so try to achieve a soft and spontaneous stool by the third day, and upon returning from the hospital, consult a doctor to make sure that the sutures are healing correctly, without divergence and suppuration. nine0003 Immediately after delivery, the uterus should empty well, so turn over, give a vertical load. The return of the tone of the soft tissues of the perineum will also be helped by sexual intercourse, which improves tissue nutrition. Please note: they are allowed when the placental site has been restored in the uterine cavity and there is no longer a risk of inflammation. If you feel pain during intercourse, do not hesitate to tell the doctor about it - he will find out the reason and advise the appropriate position. 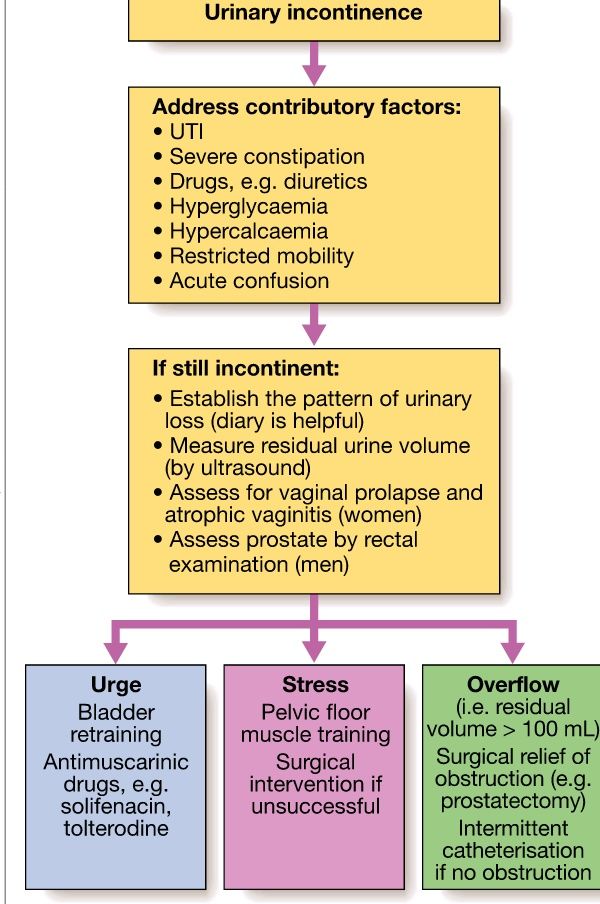
Steps to follow:
Urinary incontinence and other health issues after childbirth - Useful articles
 There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases. nine0003
There may be mixed forms. The symptom of this disease is frequent urination more than 8 times during the day and 2 times at night, pain, leakage of urine and "urgency" - a feeling that urination will begin now. The causes of the disease can be different: inflammatory diseases of the pelvic organs, injuries after childbirth, concomitant neurological, endocrine and other somatic diseases. nine0003 Therapeutic exercise for incontinence
In women after childbirth, disorders of vascular circulation and nervous regulation in the pelvic area are not uncommon. If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions. nine0003
If there was a difficult birth, a large fetus, tears, stitches, then the prevention of incontinence should be started immediately, strengthening and restoring the muscles of the pelvic floor, nervous regulation and blood circulation. It is better, of course, to do this before pregnancy. Kegel exercises not only help to cope with involuntary urination, but also increase voluntary control over sexual reactions. nine0003
2. Contractions: tense and relax these same muscles as quickly as possible.
3. Push-ups: tense the perineum and abdominal muscles.
2. I.P. Same. Alternately raise straight legs and make circular movements out and in with full amplitude. nine0069 3. From the same position while exhaling, pull up the chest with bent knees and clasp them with your hands.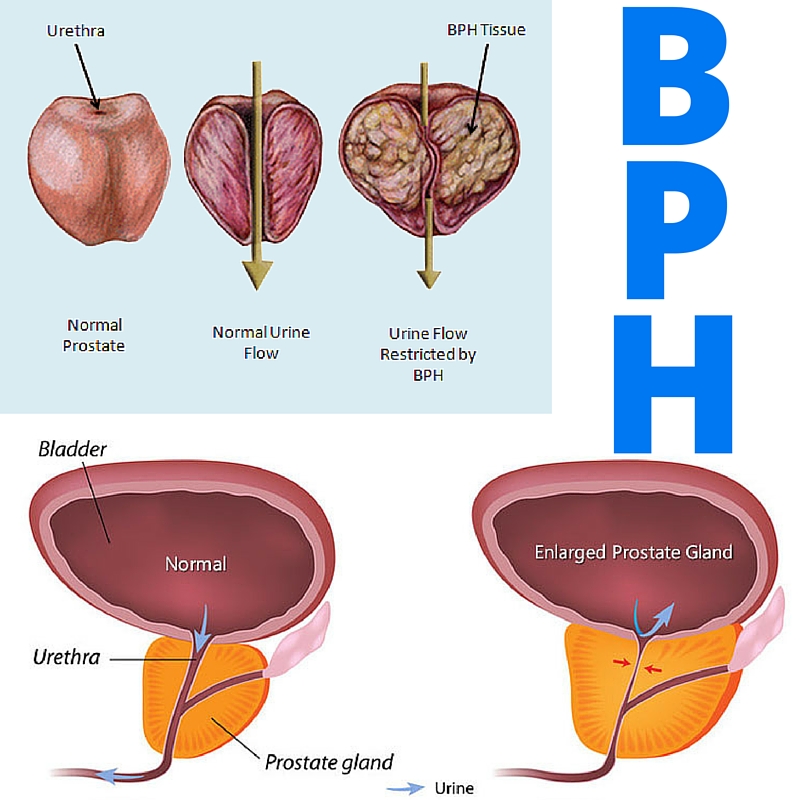
4. Now we raise the upper part of the body and sit down, wrapping our arms around our knees.
5. At the expense of 1-2-3, raise the upper body and one leg, to which we reach with the same hand. We go down to count 4.
6. Knees bent. At the expense of 1-2-3, we raise the pelvis, squeeze the buttocks, retract the anus. On the count of 4, lower the pelvis and relax.
7. From the same position, we lay bent knees to the right and left of the body. nine0069 8. I.P. standing, with support. On the inhale we rise on our toes, on the exhale we squat, holding on to the chair.
9. In the same position, holding on to the support, we roll from toes to heels and back.
10. I.P. On knees. Sit on your heels, stretch your arms up.
11. From the same position, alternately straighten the legs and pull them back. Shoulders-back-leg at the same time form one straight line.
12. Standing on all fours, alternately pull opposite arm and leg: straighten on the count of times, hold 2-3, return to the starting position on the count of 4.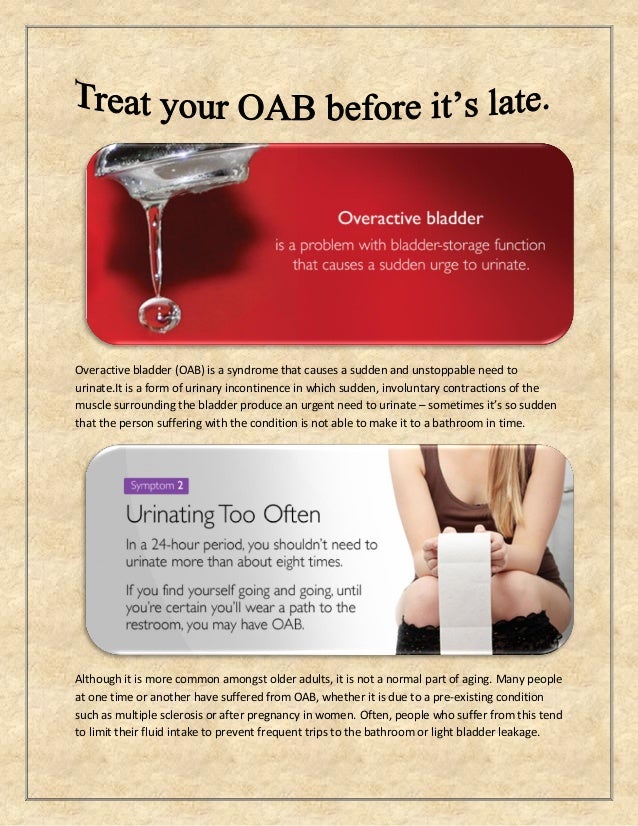 Be careful not to arch your back. nine0069 13. From the same starting position on count 1 stretch one leg back, on count 2-3 take it to the side parallel to the floor, bending at the knee, on count 4 return to the starting position.
Be careful not to arch your back. nine0069 13. From the same starting position on count 1 stretch one leg back, on count 2-3 take it to the side parallel to the floor, bending at the knee, on count 4 return to the starting position.
14. I.P. hands on the belt, one foot is on the chair. We lean forward and reach for the raised leg, bending it at the knee as much as possible. Problems in the perineum
During childbirth, injuries to the soft tissues of the perineum are possible.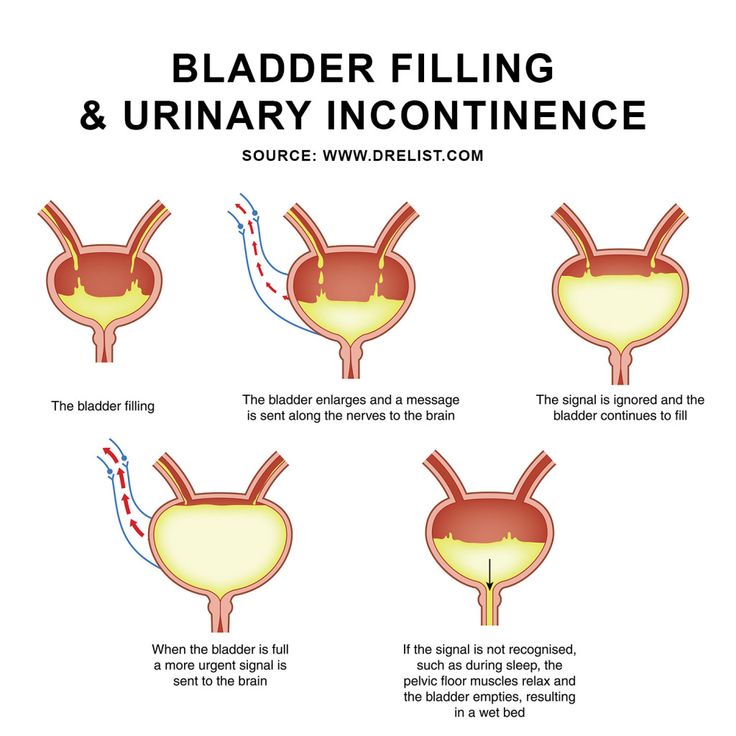 Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life. nine0003
Doctors pay special attention to this, but the woman herself should be engaged in prevention throughout the pregnancy. First of all, this is gymnastics, which prepares the muscles of this area for the birth load. Cure inflammatory processes that reduce the elasticity of the perineum (they include thrush), be careful with nutrition: an excess of sweet and starchy foods, especially in recent months, lead to an increase in the size of the fetus, increasing the risk of trauma, which then backfires problems in sexual life. nine0003 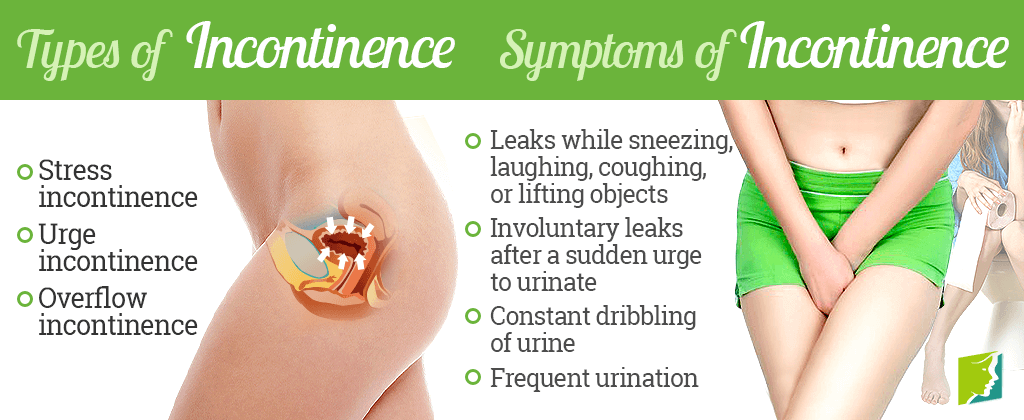
Uterus and vagina
Some women who have recently given birth complain of vaginal gaping, even asking to "sew it up so that it was like before." Bringing the vaginal ring back to normal is really very important, but this process takes some time. During childbirth, the vagina stretches to let the baby through. Closing occurs within six months, which can be accelerated, for example, by the already mentioned Kegel exercise or the mixing-breeding of the legs. nine0003  This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down. nine0003
This will improve blood flow, help her take a central position. Any exercises on the press are possible only after the complete cessation of secretions, otherwise an increase in intra-abdominal pressure increases the risk of resumption of bleeding. You can do it 6-8 weeks after giving birth in a prone position so as not to strain the muscles of the pelvic floor. But sitting in the hospital, especially if you have stitches, is not necessary - it is better to eat while standing, and to feed the baby - lying down. nine0003 Hemorrhoids
Another problem after the birth of a baby is hemorrhoids - a frequent manifestation of varicose veins.