Uncontrollable vomiting during pregnancy
Severe vomiting in pregnancy - NHS
Sickness in pregnancy (sometimes called morning sickness) is common. Around 8 out of every 10 pregnant women feel sick (nausea), are sick (vomiting) or both during pregnancy. This does not just happen in the morning.
For most women, this improves or stops completely by around weeks 16 to 20, although for some women it can last longer.
Some pregnant women experience very bad nausea and vomiting. They might be sick many times a day and be unable to keep food or drink down, which can impact on their daily life.
This excessive nausea and vomiting is known as hyperemesis gravidarum (HG), and often needs hospital treatment.
Exactly how many pregnant women get HG is not known as some cases may go unreported, but it's thought to be around 1 to 3 in every 100.
If you are being sick frequently and cannot keep food down, tell your midwife or doctor, or contact the hospital as soon as possible. There is a risk you may become dehydrated, and your midwife or doctor can make sure you get the right treatment.
Symptoms of hyperemesis gravidarum
HG is much worse than the normal nausea and vomiting of pregnancy.
Signs and symptoms of HG include:
- prolonged and severe nausea and vomiting
- being dehydrated. Symptoms of dehydration include, feeling thirsty, tired, dizzy or lightheaded, not peeing very much, and having dark yellow and strong-smelling pee
- weight loss
- low blood pressure (hypotension) when standing
Unlike regular pregnancy sickness, HG may not get better by 16 to 20 weeks. It may not clear up completely until the baby is born, although some symptoms may improve at around 20 weeks.
See your GP or midwife if you have severe nausea and vomiting. Getting help early can help you avoid dehydration and weight loss.
Getting help early can help you avoid dehydration and weight loss.
There are other conditions that can cause nausea and vomiting, and your doctor will need to rule these out first.
See the healthtalk.org website for videos and written interviews of women talking about their experiences of hyperemesis gravidarum and how they coped.
What causes hyperemesis gravidarum?
It's not known what causes HG, or why some women get it and others do not. Some experts believe it is linked to the changing hormones in your body that occur during pregnancy.
There is some evidence that it runs in families, so if you have a mother or sister who has had HG in a pregnancy, you may be more likely to get it yourself.
If you have had HG in a previous pregnancy, you are more likely to get it in your next pregnancy than women who have never had it before, so it's worth planning in advance.
Treating hyperemesis gravidarum
There are medicines that can be used in pregnancy, including the first 12 weeks, to help improve the symptoms of HG. These include anti-sickness (anti-emetic) drugs, vitamins (B6 and B12) and steroids, or combinations of these.
You may need to try different types of medicine until you find what works best for you.
You can visit the Bumps website to find out which medicines are safe to use in pregnancy.
If your nausea and vomiting cannot be controlled, you may need to be admitted to hospital. This is so doctors can assess your condition and give you the right treatment to protect the health of you and your baby.
Treatment can include intravenous fluids, which are given directly into a vein through a drip. If you have severe vomiting, the anti-sickness drugs may also need to be given via a vein or a muscle.
The charity Pregnancy Sickness Support has information and tips on coping with nausea and vomiting, including HG.
Will hyperemesis gravidarum harm my baby?
HG can make you feel very unwell, but it's unlikely to harm your baby if treated effectively.
However, if it causes you to lose weight during pregnancy, there is an increased risk that your baby may be born smaller than expected (have a low birthweight).
Other symptoms you may experience
Pregnancy Sickness Support is in touch with many women who have had HG, and who report having some or all of the following symptoms in addition to the main symptoms listed above:
- extremely heightened sense of smell
- excessive saliva production
- headaches and constipation from dehydration
If you experience these symptoms, you are not alone. Many women have them and they will go away when the HG stops or the baby is born.
Many women have them and they will go away when the HG stops or the baby is born.
How you might feel
The nausea and vomiting of HG can impact your life at a time when you were expecting to be enjoying pregnancy and looking forward to the birth of your baby.
It can affect you both emotionally and physically. The symptoms can be hard to cope with. Without treatment HG may also lead to further health complications, such as depression or tears in your oesophagus.
Severe sickness can be exhausting and stop you doing everyday tasks, such as going to work or even getting out of bed.
In addition to feeling very unwell and tired, you might also feel:
- anxious about going out or being too far from home in case you need to vomit
- isolated because you do not know anyone who understands what it's like to have HG
- confused as to why this is happening to you
- unsure about how to cope with the rest of the pregnancy if you continue to feel very ill
If you feel any of these, do not keep it to yourself.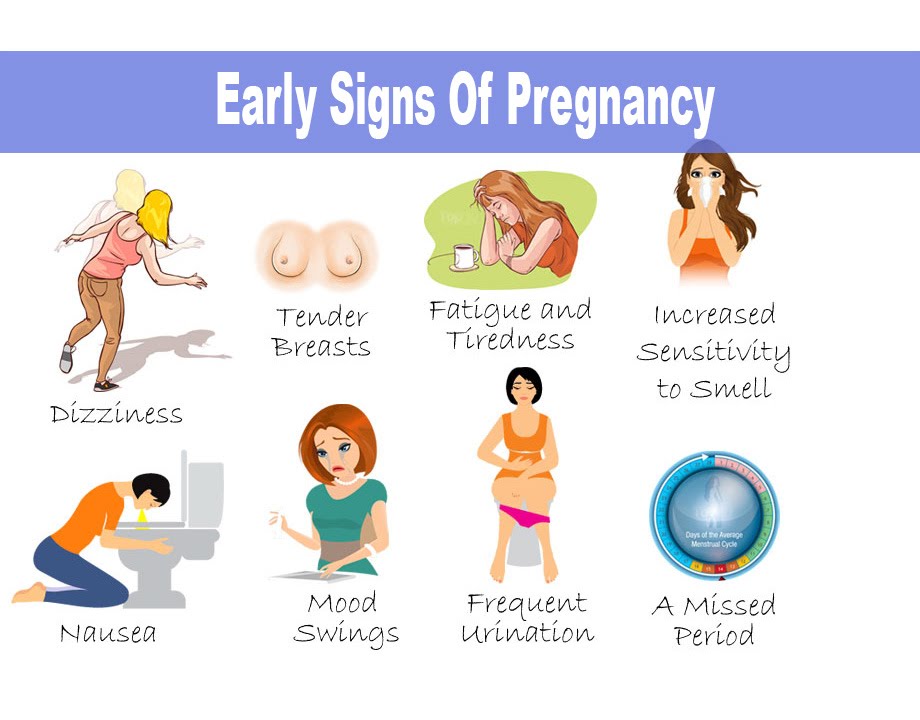 Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
Talk to your midwife or doctor, and explain the impact HG is having on your life and how it is making you feel. You could also talk to your partner, family and friends if you want to.
If you want to talk to someone who has been through HG, you can contact Pregnancy Sickness Support's help section. They have a support network across the UK and can put you in touch with someone who has had HG.
Bear in mind that HG is much worse than regular pregnancy sickness. It is not the result of anything you have or have not done, and you do need treatment and support.
Another pregnancy
If you have had HG before, it's likely you will get it again in another pregnancy.
If you decide on another pregnancy, it can help to plan ahead, such as arranging child care so you can get plenty of rest.
You could try doing things that helped last time.
Talk to your doctor about starting medicine early.
Blood clots and hyperemesis gravidarum
Because HG can cause dehydration, there's also an increased risk of having a blood clot (deep vein thrombosis), although this is rare.
If you are dehydrated and immobile, there is treatment that you can be given to prevent blood clots.
Read more about how to prevent deep vein thrombosis.
Severe vomiting during pregnancy (hyperemesis gravidarum)
Severe vomiting during pregnancy (hyperemesis gravidarum) | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- Hyperemesis gravidarum is a complication of pregnancy in which sufferers experience severe nausea and vomiting.

- It is more severe than morning sickness.
- It can lead to other health problems including dehydration, malnutrition, depression, anxiety and difficulty doing day-to-day tasks.
- Most people with hyperemesis gravidarum need to go to hospital for intravenous (IV) fluids and treatment.
What is hyperemesis gravidarum?
Hyperemesis gravidarum is a complication of pregnancy in which sufferers experience severe nausea and vomiting. It makes eating and drinking difficult and leads to weight loss, malnutrition and dehydration if it is not treated.
How is hyperemesis gravidarum different to morning sickness?
Morning sickness refers to nausea and vomiting in pregnancy, even though it doesn't only occur in the morning. The majority of people who are pregnant have some level of morning sickness.
Hyperemesis gravidarum is more severe, affecting about 1 in 100 people who are pregnant. There isn’t a clear definition as to when morning sickness becomes severe enough to be called hyperemesis gravidarum.
In general, people with morning sickness may feel put off by certain foods, but they can eat and drink and don’t lose much weight. Symptoms come and go and usually improve with dietary changes. Sometimes it may affect your mood and your ability to do your usual daily activities.
People with hyperemesis gravidarum have symptoms that are severe and constant. They have difficulty eating and drinking anything and usually need medicines and intravenous fluids. It often involves having to take time off work and needing help with your daily activities. It may affect your mood and in some cases could cause post-traumatic stress after your baby is born.
Both morning sickness and hyperemesis gravidarum usually start between 4 and 10 weeks of pregnancy and improve by 20 weeks. Some people continue to have symptoms throughout pregnancy.
What symptoms or problems could I have with hyperemesis gravidarum?
The main symptoms of hyperemesis gravidarum are severe nausea and vomiting, difficulty eating and drinking and weight loss. Some people have excessive saliva production.
Some people have excessive saliva production.
Hyperemesis gravidarum can lead to other health problems, such as:
- malnutrition and dehydration
- an imbalance of salts or acid in your body
- kidney damage
- low vitamin levels
- a tear in your oesophagus
- reflux
- constipation
- dental erosion
Other possible effects of hyperemesis gravidarum include:
- depression, anxiety and post-traumatic stress
- breastfeeding difficulties
- relationship problems
- financial problems
- difficulty with daily activities
- reluctance to have more children
How is hyperemesis gravidarum treated?
You should receive treatment from a doctor with special expertise in this area. You’ll be monitored closely, and may need to go to hospital for ongoing care.
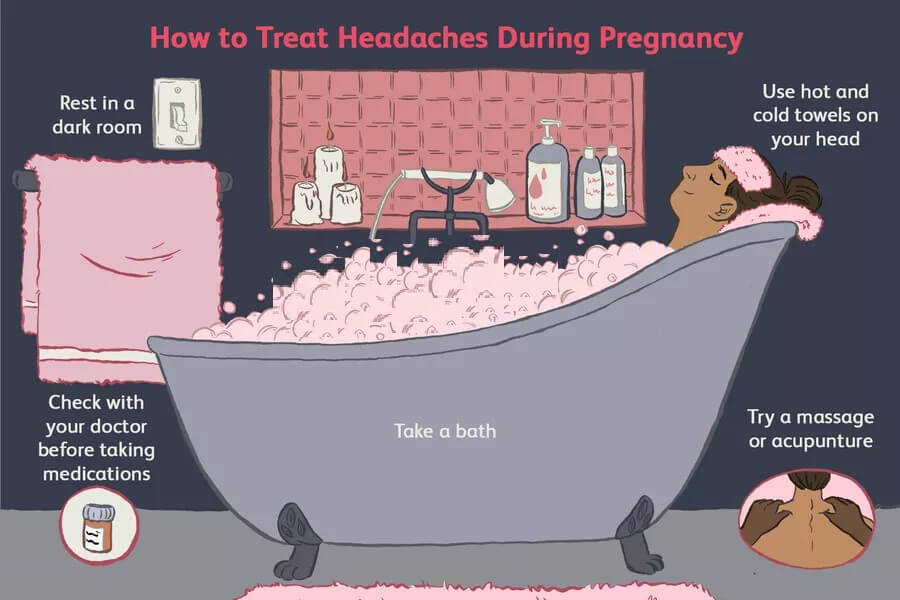
There are many dietary and lifestyle measures that can reduce nausea and vomiting. These are worth trying, but more intensive treatment is usually needed if you suffer from hyperemesis gravidarum.
What treatment will I need?
There are several different medicines available to treat nausea and vomiting. Your symptoms might not disappear completely, but the aim is for you to manage to eat and drink some food or water during the day without vomiting.
Some people find that multivitamins make them feel sick. It’s fine to stop pregnancy multivitamins if this helps, if possible, try to continue taking folate.
If you’ve had hyperemesis gravidarum, in future pregnancies it can help to start taking medicine for nausea and vomiting as early as possible — even before you conceive.
Hydration
Try to drink fluids so you don’t get dehydrated. It can help to sip on a drink containing sugar or electrolytes every 15 minutes, or suck on ice blocks or icypoles.
If you can’t keep food or fluids down, go to your local emergency department. You will need intravenous (IV) fluids, which may help improve nausea and vomiting, and can help keep up your levels of electrolytes.
Nutrition
Try to eat small amounts regularly. Eat any food that you can keep down, as long as it’s safe in pregnancy — don’t worry about eating healthy foods right now.
You might need to see a dietitian. If you have low vitamin levels, you may need supplements.
In extreme cases, if you’re unable to eat, you may need to be fed through a tube. This can cause complications and requires careful monitoring.
Treatment of related conditions
Other treatments may include:
- antacids or other medicines to treat reflux
- laxatives for constipation
- medicines to reduce saliva production
Rinse your mouth out with water after vomiting, to protect your teeth from damage. If you can, add some baking soda to the water you rinse with.
Can hyperemesis gravidarum affect my baby?
If you have hyperemesis gravidarum, your placenta may not be working as it should. This can affect your baby. Your baby may be more likely to be small and to be born early. It’s not clear if you have a higher risk of stillbirth.
It’s not clear if you have a higher risk of stillbirth.
In severe cases, people with hyperemesis gravidarum may choose to have a termination of pregnancy (abortion) if they have tried intensive treatment without relief.
Where can I get support?
If you experience hyperemesis gravidarum, contact Hyperemesis Australia for information and support.
You can also call Pregnancy, Birth and Baby on 1800 882 436 to speak to a maternal child health nurse.
Other sources of support include:
- relatives or friends who may be able to help you with day-to-day tasks or prepare meals for your family
- services such as cleaners and supermarket delivery
- a social worker
- a psychologist or counsellor for help with depression and anxiety
- Perinatal Anxiety & Depression Australia (PANDA)
If you suffer from hyperemesis gravidarum, it’s likely that working will be difficult, talk to your employer about changing to another role, or about taking special parental leave if you need extended time off to take care of yourself.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Society of Obstetric Medicine of Australia and New Zealand (Guideline for the management of nausea and vomiting in pregnancy and hyperemesis gravidarum), Royal Hospital for Women (Hyperemesis gravidarum (HG) and nausea and vomiting in pregnancy (NVP) - management), Hyperemesis Australia (What is HG?), The Royal Hospital for Women (Nausea and vomiting of pregnancy (NVP)), King Edward Memorial Hospital (Looking after yourself), Hyperemesis Australia (House and family), Hyperemesis Australia (Oral hygeine), Hyperemesis Australia (Mental health), Hyperemesis Australia (Diet and nutrition), Hyperemesis Australia (Employment)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: August 2022
Back To Top
Related pages
- Morning sickness
- Healthy diet during pregnancy
Need more information?
Nausea and vomiting in pregnancy and Hyperemesis Gravidarum - Maternal, child and family health
While nausea and vomiting are both common symptoms of early pregnancy, if you are very sick and it’s impacting your normal life, you may have Hyperemesis Gravidarum or HG as it’s often known, which involves excessive nausea and vomiting during pregnancy
Read more on NSW Health website
Pregnancy - morning sickness - Better Health Channel
Morning sickness is typically at its worst early in the day but it can strike at any point during the day or night.
Read more on Better Health Channel website
Morning sickness - MyDr.com.au
Many women experience morning sickness (nausea and vomiting) in early pregnancy, and the symptoms can actually occur at any time of the day or night.
Read more on myDr website
Morning sickness
Morning sickness is a feeling of nausea or the experience of vomiting during pregnancy. Find out why some women get it and what you can do to relieve it.
Read more on Pregnancy, Birth & Baby website
Preventing motion sickness in children - Australian Prescriber
The following general points should be considered when managing children who are prone to motion sickness: As motion sickness induces gastric stasis, it slows drug absorption, so preventing symptoms from occurring is more effective than trying to treat them after symptom onset
Read more on NPS MedicineWise website
Multiple pregnancy (triplets or more)
Learning you're pregnant with triplets or more can be a shock, but overall, most parents find having multiple babies to be a positive experience.
Read more on Pregnancy, Birth & Baby website
Blood tests during pregnancy
Find out more about the blood tests you be offered during your pregnancy. what they test for and when you’ll be offered them.
Read more on Pregnancy, Birth & Baby website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.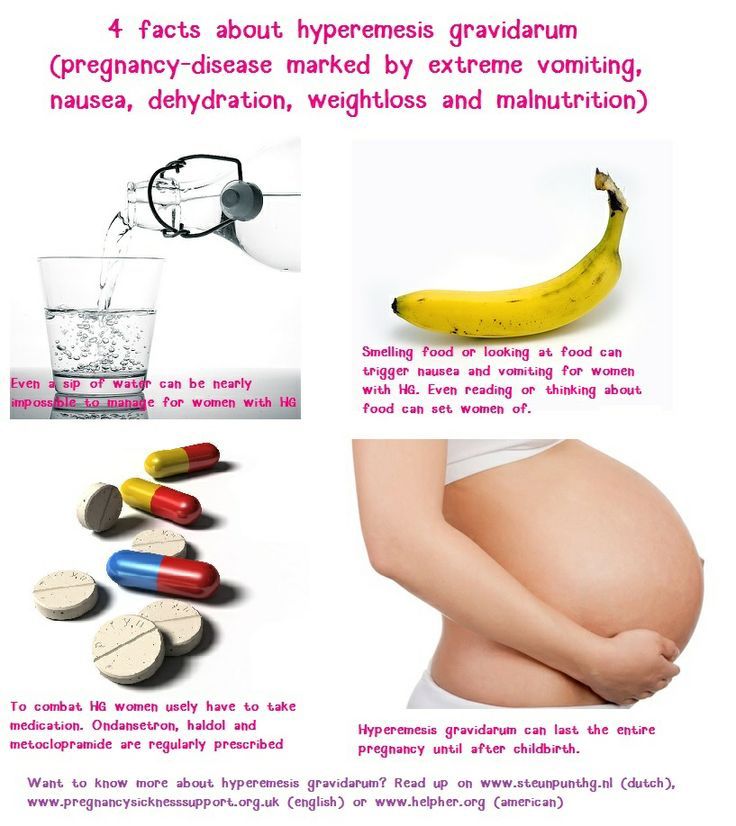
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
More than morning sickness: the problem of uncontrollable pregnancy vomiting
Summary. Combination of genetic factors and hormonal disorders lead to the development of pathology postpartum period. This, based on the results of a new study, was reported by American scientists at the Annual Conference of the Infusion Nurses Society (INS) held in Baltimore, USA.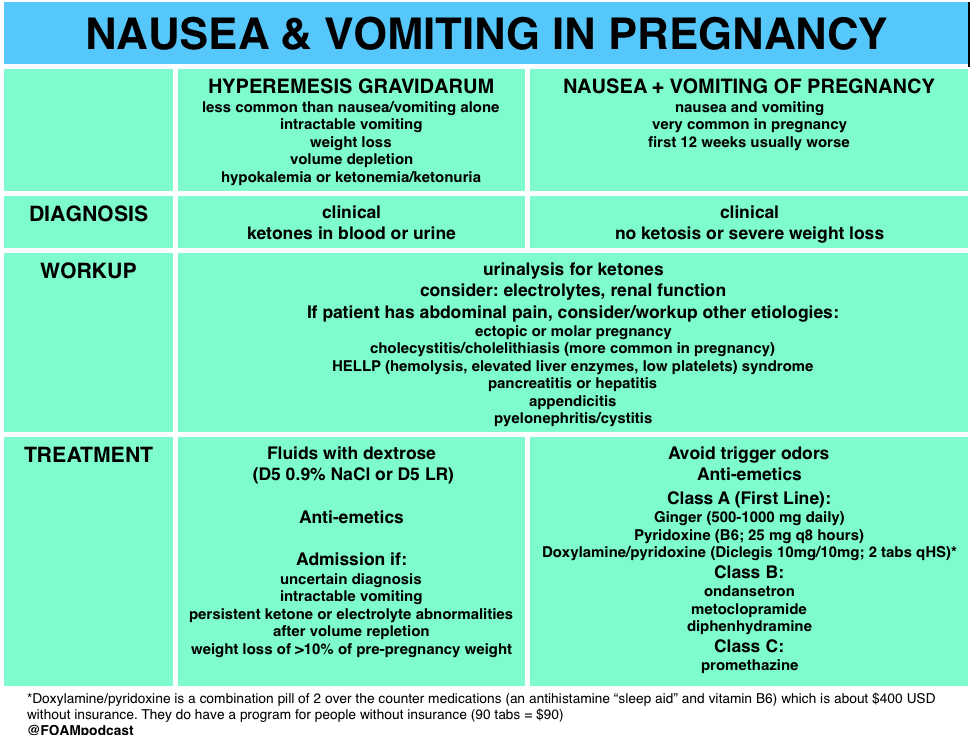 nine0005
nine0005
Persistent vomiting of pregnancy, also called hyperemesis gestationis, is characterized by frequent episodes of vomiting that can lead to exhaustion, unconsciousness, and organ failure. Author Kimber MacGibbon noted that the condition they are studying is poorly diagnosed, and clinicians often do not know how to distinguish it from morning sickness common during pregnancy. At the same time, even in the case of timely recognition of the pathology, the attending physicians often do not know what methods of treatment should be applied. nine0005
The development of complications in mother and child
Symptoms of hyperemesis usually begin around 4-6 weeks of gestation and peak at 11-13 weeks. Nevertheless, in 22% of women, signs of pathology persist throughout pregnancy. The longer the symptoms persist and the more severe they are, the higher the risk of long-term complications for mother and baby.
Babies of mothers with hyperemesis gestation who have not received any medical care may experience neurodevelopmental delays, behavioral problems, and vitamin K deficiency embryopathies. These babies are more likely to be born prematurely and may have intrauterine growth retardation. Timely treatment of intractable vomiting of pregnancy is effective in preventing long-term changes, the researchers say, but healthcare professionals need to be able to diagnose the condition. nine0005
These babies are more likely to be born prematurely and may have intrauterine growth retardation. Timely treatment of intractable vomiting of pregnancy is effective in preventing long-term changes, the researchers say, but healthcare professionals need to be able to diagnose the condition. nine0005
Influence of hormonal changes and genetic factors
Previous studies have shown that women with hyperemesis have elevated levels of the hormone GDF15, which is produced by the placenta. It is this hormone, which also plays a role in appetite control and is associated with the development of cachexia in patients with cancer, and the IGFBP7 gene , according to some experts, are associated with the development of uncontrollable vomiting of pregnant women.
Previously, doctors believed that the main causes of the pathology under study were psychological and hormonal disorders, but in the course of this work, scientists noticed that the genetic characteristics of the patient also play an important role. It is the combination of gene activity IGFBP7 and an increased level of GDF15 leads to the fact that the hormone, acting on the subcortical centers of the cerebral hemispheres, leads to indomitable vomiting.
It is the combination of gene activity IGFBP7 and an increased level of GDF15 leads to the fact that the hormone, acting on the subcortical centers of the cerebral hemispheres, leads to indomitable vomiting.
The authors of the study emphasized that they are interested in finding potential treatments for pregnant women with this pathology that would block any interactions of GDF15 with the brain, however, such work is likely to be carried out only in a few years. At the same time, they noticed that the results obtained in the study of methods for treating cachexia in cancer patients can also be used for the treatment of hyperemesis in pregnant women. nine0005
Subscribe to our Telegram channel, Viber community, Instagram, Facebook page, and Twitter to be the first to receive the latest and most relevant news from the world of medicine.
- Arenschield L. (2019) More than morning sickness: treating hyperemesis gravidarum. Medscape, May 19 (www.
 medscape.com/viewarticle/913199#vp_1).
medscape.com/viewarticle/913199#vp_1).
Yuliya Kotikovich
Nausea and vomiting of pregnant women: the view of an anesthesiologist-resuscitator
Despite the fact that nausea and vomiting are very common during pregnancy, the questions of their etiology and pathogenesis are still open. Head of the Department of Anesthesiology and Resuscitation of the Krasnoyarsk Regional Clinical Center for Maternal and Childhood Protection, Assistant of the Department of Anesthesiology and Resuscitation, IPO KrasSMU named after. Professor V. F. Voyno-Yasenetsky Yuri Raspopin analyzed the literature over the past 10 years in order to study the current state of the problem and determine further research prospects. nine0033
Clinical picture
Nausea and vomiting are the most common symptoms of advanced pregnancy: up to 80% of women experience them. As a rule, they appear on the 4th week of pregnancy and disappear on their own at the 12-14th week. However, about 20% of women continue to experience nausea and vomiting throughout the entire period.
However, about 20% of women continue to experience nausea and vomiting throughout the entire period.
Excessive vomiting of pregnancy is characterized by severe nausea, uncontrollable vomiting that continues until the 22nd week of pregnancy, as defined by the 2016 WHO. As the most severe form, it occurs in 0.3–4% of women. It is one of the most common reasons for hospitalization in early pregnancy. Left untreated or failing, it can lead to maternal morbidity and poor neonatal outcomes. nine0005
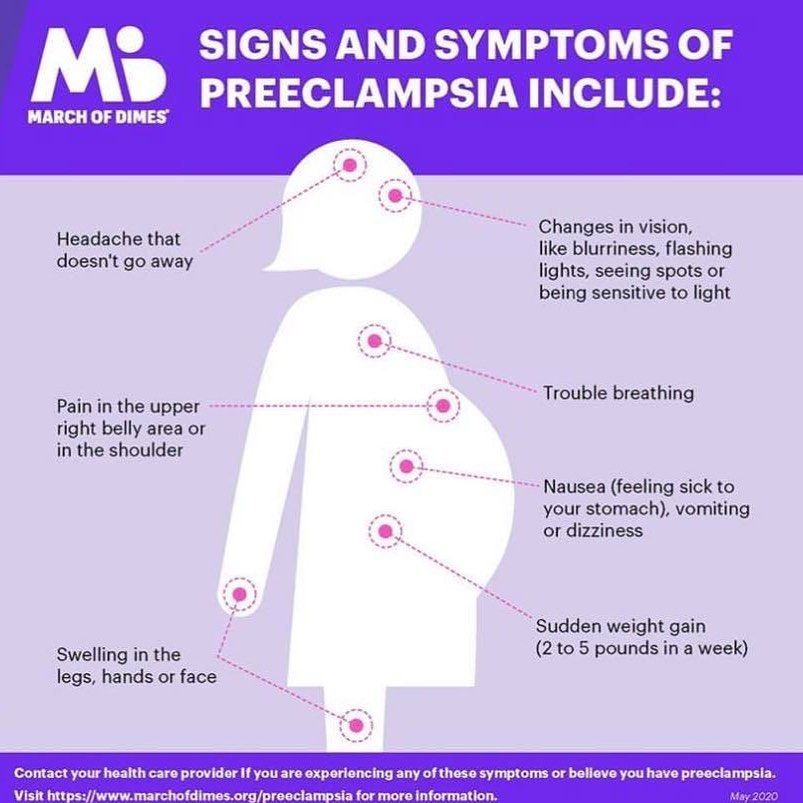
A large population-based cohort study in Sweden over 12 years (1997–2009) of more than 1 million women with excessive pregnancy vomiting found that admission in the 2nd trimester more than doubled the risk of severe preeclampsia, 3 times the risk of placental abruption and 39% the risk of having a fetus with extremely low body weight.
From an economic point of view, the cost of treating and maintaining women with nausea and vomiting of pregnancy is enormous. In 2012, in the United States, the treatment of one such patient cost $47,351, and the annual cost was about $1.7 billion. Of this, the direct cost of treatment takes 60%, the rest is indirect economic losses. And in Canada, for example, the treatment of one patient with nausea and vomiting of pregnancy is 653 Canadian dollars per week. nine0005
In 2012, in the United States, the treatment of one such patient cost $47,351, and the annual cost was about $1.7 billion. Of this, the direct cost of treatment takes 60%, the rest is indirect economic losses. And in Canada, for example, the treatment of one patient with nausea and vomiting of pregnancy is 653 Canadian dollars per week. nine0005
Currently, the world community is switching to ICD-11, which is distinguished by the degree of sophistication. The concept of excessive vomiting of pregnant women is spelled out in it along with mild vomiting of pregnant women, vomiting of pregnant women with metabolic disorders.
In terms of recommendations, 3 documents on this issue were found internationally: the American Society of Obstetricians and Gynecologists for 2018, the Royal College of Obstetricians and Gynecologists of Great Britain and the Society of Obstetricians and Gynecologists of Canada for 2016. nine0005
Risk factors:
- history of nausea and vomiting;
- the presence of nausea and vomiting in close relatives;
- young women under 20;
- nulliparous;
- multiple pregnancy;
- taking oral contraceptives;
- history of miscarriage; nine0034
- motion sickness, migraine;
- ethnic etc.
:strip_icc():format(jpeg)/kly-media-production/medias/2785562/original/028627600_1556001360-shutterstock_1019963743.jpg)
Severity score
A modified PUQE (Pregnancy-Unique Quantification of Emesis and Nausea) scale is used. Patients are asked 3 questions:
Concept difference
There is a fine line between pregnancy nausea and vomiting and excessive pregnancy vomiting. nine0005
Diagnosis
It must be remembered that nausea and vomiting of pregnant women can be both primary and secondary conditions against the background of severe somatic pathology, including hepatitis, pancreatitis, pancreatic necrosis, pyelonephritis, migraine, diabetic ketoacidosis and others.
First of all, it is necessary to carefully collect anamnesis, which is the cornerstone in the diagnosis of this condition. Laboratory and instrumental diagnostics are also helpful. For example, nausea and vomiting of pregnant women is characterized by an increase in liver enzymes up to 300 U / l, as well as bilirubin - up to 40 mg / l. In hepatitis, for comparison, the first indicator increases several thousand times, and the second - more than 40 mg / l. nine0005
In hepatitis, for comparison, the first indicator increases several thousand times, and the second - more than 40 mg / l. nine0005
Screening for ketonuria is now the gold standard in all guidelines. It is often used as an aid in diagnosis, fluid therapy, or admission/discharge decisions for patients. With ketosis as a condition that develops against the background of carbohydrate starvation of cells, fat begins to break down with the formation of a large number of ketone bodies. Accordingly, this is one of the adaptive reactions of the body to the absence of carbohydrates in food, it acts as a certain measure of starvation. Increased metabolic demands during pregnancy, even in the absence of vomiting or poor oral nutrition, are a predisposing factor in the development of ketonuria. nine0005
It should be remembered that nausea and vomiting of pregnancy is characterized by the first appearance before 9 weeks. After that, it is necessary to carry out a differential diagnosis, with which this condition may be associated.
Etiology and pathogenesis
There are several theories of nausea and vomiting of pregnancy, including excessive vomiting. This suggests that this problem has not been fully studied.
The hormonal theory is related to several hormones:
- HCG . This is the time factor. As a rule, the peak of symptoms of nausea and vomiting of pregnant women is observed against the background of an increase in hCG. They also increase in conditions such as multiple pregnancy or female pregnancy, since in such cases the level of hCG is elevated. However, the failure of some studies to show an association between nausea and vomiting and hCG levels may be due to the different biological activity of different isoforms of this hormone. nine0034
- Estrogen . It is also a temporary factor. There are studies that show that nausea and vomiting of pregnancy is common with an increase in estrogen levels, and less often with a decrease.
- Progesterone . Alone or in combination with estrogen at elevated levels, it can cause stomach arrhythmias, resulting in increased nausea and vomiting.
More attention is now being paid to the hormone GDF15, which, like hCG, is produced by the placenta. Its level increases in early pregnancy when symptoms of nausea and vomiting occur. However, several recent studies point to the leading role of GDF15, rather than hCG, in the development of excessive vomiting during pregnancy. It is this hormone that plays a leading role in appetite control and is associated with the development of cachexia in cancer patients by activating the ICFBP17 gene, which is symptomatically similar to excessive vomiting of pregnant women (weight loss, muscle atrophy). nine0005
Another theory is related to serotonin receptors located in the vagus afferent neurons of the gastrointestinal tract and the vomiting center in the brain. It has been proposed because, like progesterone and the hormone GDF15, they play a role in altering GI motility.
The genetic theory is based on a 2016 population cohort study of 1,723 female twins. Genetic predisposition was confirmed in 73%. In 53%, excessive vomiting of pregnant women was observed. And 28% of women reported that their mothers had it, at 19% of cases are in twin sisters.
It is important to pay attention to another theory. She suggests that nausea and vomiting of pregnancy is an evolutionary adaptation to potentially dangerous foods, which is a protective reaction.
Treatment options
Mild (≤6 PUQE)
Non-drug therapy with lifestyle and diet changes. It involves frequent small meals, a high protein and carbohydrate diet, avoiding spicy foods, etc.
Further treatment is based on the exclusion of other causes of nausea and vomiting. At each stage, it is necessary to remember the importance of enteral nutrition, and in case of dehydration, the replacement infusion therapy.
Remember the importance of prevention. There are several studies that have shown that women who took multivitamins during fertilization were less likely to need medical attention and hospitalization if they developed vomiting during pregnancy. The authors suggest that this may have been due to increased levels of vitamin B6. Therefore, there is a standard recommendation: start taking prenatal vitamins a month before pregnancy. nine0005
Rest and restriction of various external irritants (odors, humidity, noise and others) will help relieve the initial signs of nausea and vomiting.
Recommendations include ginger-based preparations (250 mg capsules 4 times a day). You should also consider electrical stimulation, acupressure, acupuncture of the P6 point, which is located on the back of the hand near the wrist. Most studies report the benefits of this stimulation. But there are significant methodological shortcomings. For example, the last 2 large studies have shown no benefit over sham stimulation. nine0005
nine0005
Moderate (PUQE 7-12)
First-line drugs are pyridoxine or its combination with doxylamine. A number of studies have shown the effectiveness of this combination in the treatment of varying degrees of severity of nausea and vomiting during pregnancy. They act on the vestibular pathway of nausea and vomiting by blocking the connection of histamine receptors in the vomiting center with the chemoreceptor trigger zone. Cases of harmful effects on the fetus are not described. However, caution should be exercised when using several antiemetics at the same time, as this may lead to an increased risk of extrapyramidal disorders. nine0005
Diphenhydramine and metoclopramide and ondansetron are recommended as second line.
Severe (13 or more points on the PUQE scale)
Initial treatment includes rehydration, elimination of electrolyte deficiency. In this case, replacement infusion therapy of balanced solutions with the inclusion of thiamine 100 mg daily for 2-3 days is carried out, followed by the introduction of multivitamins.