Late pregnancy swelling
Swollen ankles, feet and fingers in pregnancy
It's normal to get some swelling in pregnancy, particularly in your legs, ankles, feet and fingers.
It's often worse at the end of the day and further into your pregnancy.
Swelling that comes on gradually is not usually harmful to you or your baby, but it can be uncomfortable.
A sudden increase in swelling can be a sign of pre-eclampsia, a condition that needs to be monitored as soon as possible.
Non-urgent advice: Call your midwife, GP or labour ward immediately if you have:
- a sudden increase in swelling in your face, hands or feet
- a very bad headache
- problems with your vision, such as blurring or flashing lights in your eyes
- severe pain just below your ribs
- vomiting with any of these symptoms
These could be symptoms of pre-eclampsia, which can lead to serious complications if it's not monitored and treated.
Normal pregnancy swelling
Swelling is caused by your body holding more water than usual when you're pregnant.
Throughout the day the extra water tends to gather in the lowest parts of the body, especially if the weather is hot or you have been standing a lot.
The pressure of your growing womb can also affect the blood flow in your legs. This can cause fluid to build up in your legs, ankles and feet.
What can help to reduce swelling
Try to:
- avoid standing for long periods
- wear comfortable shoes and socks – avoid tight straps or anything that might pinch if your feet swell
- try to rest with your feet up as much as you can
- drink plenty of water – this helps your body get rid of excess water
- exercise – try to take regular walks during the day or doing foot exercises
Foot exercises
You can do foot exercises sitting or standing. They improve blood circulation, reduce swelling in the ankles, and prevent cramp in the calf muscles:
They improve blood circulation, reduce swelling in the ankles, and prevent cramp in the calf muscles:
- bend and stretch your foot up and down 30 times
- rotate each foot in a circle 8 times one way and 8 times the other way
Get more tips on exercising in pregnancy.
Page last reviewed: 10 March 2021
Next review due: 10 March 2024
Swelling during pregnancy | Pregnancy Birth and Baby
beginning of content3-minute read
Listen
Most women get swollen ankles and feet while pregnant. It’s natural to have concerns about swelling since it can be uncomfortable, make your shoes tighter and possibly make you feel embarrassed. Knowing what to look for and how best to manage it can help you stay as comfortable as possible.
Knowing what to look for and how best to manage it can help you stay as comfortable as possible.
Why do women experience swelling during pregnancy?
There are 3 main reasons women experience swelling while pregnant.
- Throughout pregnancy, you produce more blood than usual to help your baby grow.
- As the baby grows, your uterus presses on and slightly blocks the veins that return blood from your legs to your heart.
- Your hormones make the walls of your veins softer, which makes it harder for them to work properly.
For these reasons, your blood tends to pool in your legs. There, a small amount of blood leaks through tiny blood vessels into the tissues and produces the swelling you can see and feel.
Where and when will I get swelling?
The swelling should be only in your feet and ankles. Your fingers might get a little larger — enough to make any rings feel tight — but they shouldn't be obviously swollen.
Your feet and ankles are likely to swell later in the day. This is mainly due to gravity — any extra fluid in your body will sink to your feet and ankles, especially if you spend a lot of time on your feet.
This is mainly due to gravity — any extra fluid in your body will sink to your feet and ankles, especially if you spend a lot of time on your feet.
Swelling is also more likely to happen later in your pregnancy.
Gradual swelling isn't harmful to you or your baby, but it can feel uncomfortable.
How can I reduce swelling?
Some simple things can help you feel more comfortable and can also aid in preventing swelling.
Try to:
- avoid standing for long periods without moving
- wear comfortable shoes (avoid tight straps or anything that might pinch if your feet swell)
- put your feet up as much as you can
- limit salty foods and excessive salt in your diet
- sleep on your left side, which will help blood return to the heart
- exercise regularly by walking or swimming — this helps keep your circulation going
If you need to stand for long periods, try to move around and change position regularly.
Compression stockings can help the blood flow back to the heart and limit how much swelling you get. Massage and reflexology might also help reduce swelling and associated symptoms.
Massage and reflexology might also help reduce swelling and associated symptoms.
Even if your swelling is bothering you, remember to still drink plenty of water. Keeping your fluids up is important to avoid dehydration and stay healthy.
Normal or abnormal swelling?
Most pregnant women have swollen feet and ankles at some point, and this is perfectly normal. However, there are times when swelling could indicate something more serious.
Contact your midwife, doctor or hospital immediately if:
- swelling is there at the start of the day or doesn't go down when you rest
- your face or hands are swollen
- the swelling is more than you have had before
These are warning signs for pre-eclampsia, which is high blood pressure caused by pregnancy. This is a very serious condition both for you and your baby, so call your doctor or midwife as soon as possible. Don't wait for your next regular appointment.
If one leg is more swollen than the other, this could suggest a more serious problem with one of your veins, such as deep vein thrombosis. Again, contact your doctor or midwife as soon as possible.
Again, contact your doctor or midwife as soon as possible.
Most swelling is a normal part of pregnancy and will usually go away after you've given birth. However, if you're concerned about anything, no matter how small or seemingly insignificant, talk to your doctor or midwife.
You can also call Pregnancy, Birth and Baby on 1800 882 436 to talk to a maternal child health nurse.
Sources:
NSW Health (Having a baby), The Royal Women's Hospital (Active pregnancy), The Royal Women's Hospital (Common concerns in early pregnancy), Cochrane (Interventions for varicose veins and leg oedema in pregnancy), King Edward Memorial Hospital (Pregnancy, birth and your baby), Department of Health (Clinical practice guidelines: Pregnancy care), King Edward Memorial Hospital (Minor Symptoms or Disorders in Pregnancy King Edward Memorial Hospital Clinical Guidelines: Obstetrics & Midwifery), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists - Pre-eclampsia and high blood pressure during pregnancy (The Royal Australian and New Zealand College of Obstetricians and Gynaecologists - Pre-eclampsia and high blood pressure during pregnancy)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2020
Back To Top
Related pages
- Common discomforts during pregnancy
- Varicose veins
- Leg cramps during pregnancy
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Colorectal cancer in pregnant women
Oncological diseases are observed in 1 out of 1000 pregnant women [1-3]. The most common such diseases are female genital cancer or breast cancer, melanoma, lymphoma and leukemia. Colorectal cancer (CRC) occurs in 1 in 50,000 pregnant women [1]. There are few data on the combination of CRC and pregnancy in the literature, and there are no specific clinical recommendations. The practical doctor, who faces the task of treating such a patient, often finds himself in a difficult position. We present our own clinical observations. nine0003
The practical doctor, who faces the task of treating such a patient, often finds himself in a difficult position. We present our own clinical observations. nine0003
Patient B., , 38 years old, was admitted to Lapino Clinical Hospital on March 2, 2014 with a diagnosis of pregnancy 23—24 weeks, rectal cancer, cT3NxMx. From the anamnesis it is known that the real pregnancy is the second, the first 12 years ago ended in a timely manner with an operative delivery without complications. Heredity is not burdened, does not suffer from chronic diseases. During pregnancy, the patient noted periodic constipation and small bloody discharge from the rectum during defecation. A sigmoidoscopy was performed at the place of residence, which revealed a tumor of the rectum at a distance of 15-18 cm from the anus. Histological examination of the biopsy revealed a highly differentiated adenocarcinoma. nine0003
Examined at Lapino Clinical Hospital. Pregnancy proceeds without features, corresponds to a period of 24 weeks. Pathological changes in the fetus were not detected. A colonoscopy was performed: when examining 70 cm of the large intestine, no additional formations were found in the intestine. Ultrasound of the uterus revealed a scar and two myomatous nodes measuring 39×22 and 23×16 mm, head presentation of the fetus. An MRI scan diagnosed a tumor of the rectum without signs of invasion into the surrounding structures, no secondary foci were detected. According to laboratory tests, no significant deviations from the norm were revealed. The level of cancer-embryonic antigen is increased to 21 ng/ml. The diagnosis was made: pregnancy 23-24 weeks, highly differentiated adenocarcinoma of the rectum, cT3NxM0. nine0003
Pathological changes in the fetus were not detected. A colonoscopy was performed: when examining 70 cm of the large intestine, no additional formations were found in the intestine. Ultrasound of the uterus revealed a scar and two myomatous nodes measuring 39×22 and 23×16 mm, head presentation of the fetus. An MRI scan diagnosed a tumor of the rectum without signs of invasion into the surrounding structures, no secondary foci were detected. According to laboratory tests, no significant deviations from the norm were revealed. The level of cancer-embryonic antigen is increased to 21 ng/ml. The diagnosis was made: pregnancy 23-24 weeks, highly differentiated adenocarcinoma of the rectum, cT3NxM0. nine0003
The situation was discussed with the patient and her relatives, the nature of the disease and possible complications were explained. The patient expressed a strong desire to continue the pregnancy. A consultation was held consisting of an obstetrician-gynecologist, a surgeon, an oncologist and an anesthesiologist. It was decided to perform surgery in the volume of anterior resection of the rectum with the formation of a colorectal anastomosis and preservation of pregnancy.
It was decided to perform surgery in the volume of anterior resection of the rectum with the formation of a colorectal anastomosis and preservation of pregnancy.
06.03.14 the patient was operated on. An upper median laparotomy was performed due to the large size of the uterus. The uterus was removed from the abdominal cavity. Examination of the abdominal cavity revealed no distant metastases. An exophytic circular tumor with a diameter of 6 cm is detected in the distal third of the sigmoid colon and the rectosigmoid region. There is no invasion of the tumor into the surrounding anatomical structures. An extrafascial anterior resection of the rectum was performed with the formation of a colorectal anastomosis with a stapler. Then bilateral wedge resection of the ovaries was performed. An urgent histological examination did not reveal any atypical cells in the resected ovarian tissue. It was decided to refrain from performing bilateral salpingo-oophrectomy. The laparotomic wound was sutured in layers. nine0003
nine0003
Histological examination of the resected rectum revealed a moderately differentiated ulcerated adenocarcinoma, growing in one of the areas into the mesorectal tissue. There is abscessing of the intestinal wall in the area of tumor growth. No tumor growth was detected in the resection margins. 2 out of 15 lymph nodes have adenocarcinoma metastases. Thus, the stage of the tumor process is defined as IIIB, according to the TNM classification - as pT3pN1cM0.
The postoperative period was uneventful. The patient became active on the 2nd day. On the 3rd day there was an independent chair. Due to the increased tone of the uterus, she received Hemipral for 3 days. She was discharged in a satisfactory condition on the 8th day. In the future, the pregnancy proceeded without complications, ended in operative delivery at the 38th week. A healthy girl was born weighing 2750 g, height 49cm, 8 points on the Apgar scale. The patient was examined one month after delivery: colonoscopy and ultrasound of the abdominal cavity were performed. There were no signs of recurrence of the disease.
There were no signs of recurrence of the disease.
Patient K., , 37 years old, was hospitalized at the Institute of Surgery named after A.V. Vishnevsky on 02.07.14 with a diagnosis of sigmoid colon cancer, cT3NxM0. Heredity is not burdened, does not suffer from chronic diseases. From the anamnesis it is known that on March 10, 2014, her pregnancy ended in operative delivery without complications. This pregnancy is the second, the first 8 years ago ended in a timely manner with childbirth without complications. nine0003
Starting from the first trimester of the last pregnancy, the patient noted constipation and the discharge of unchanged blood from the rectum during defecation, however, the obstetricians-gynecologists who observed her associated this with "hemorrhoids aggravated during pregnancy." After childbirth, these symptoms persisted, which was the reason for contacting a surgeon. An examination has been carried out. A colonoscopy was performed: at a distance of 25 cm from the anus, a loose polypoid formation up to 4 cm in diameter was detected, a biopsy material was taken. Histological examination of the biopsy showed a picture of highly differentiated adenocarcinoma. Computed tomography of the thoracic and abdominal organs with intravenous contrast was performed, a tumor of the sigmoid colon 7.2 cm in diameter was diagnosed, regional lymphadenopathy, no secondary foci were detected. nine0003
Histological examination of the biopsy showed a picture of highly differentiated adenocarcinoma. Computed tomography of the thoracic and abdominal organs with intravenous contrast was performed, a tumor of the sigmoid colon 7.2 cm in diameter was diagnosed, regional lymphadenopathy, no secondary foci were detected. nine0003
04.07 the patient was operated on. A laparoscopic left-sided hemicolectomy was performed with the formation of a transverse rectoanastomosis with a device for applying a mechanical suture. Intraoperatively during the revision of the abdominal cavity, no distant metastases were detected. Macropreparation: circular saucer-shaped tumor 6 cm long. After cutting the tumor, it is seen that it grows into all layers of the intestinal wall and grows into the surrounding tissue in the form of a node with a diameter of 2 cm.
Histological examination shows a moderately differentiated adenocarcinoma of the sigmoid colon, invading all layers of the intestinal wall and growing into the mesenteric tissue. Tumor with minor perifocal inflammation, foci of perineural invasion. In 7 out of 27 lymph nodes examined, tumor metastases of a similar structure were found. Thus, the stage of the tumor process is defined as IIIc, according to the TNM classification - as pT3pN2bcM0.
Tumor with minor perifocal inflammation, foci of perineural invasion. In 7 out of 27 lymph nodes examined, tumor metastases of a similar structure were found. Thus, the stage of the tumor process is defined as IIIc, according to the TNM classification - as pT3pN2bcM0.
The postoperative period was uneventful. On the 2nd day there was an independent chair. She was discharged in a satisfactory condition on the 6th day after the operation. She was referred for adjuvant chemotherapy. At the control examination after 1 month, the patient's condition is satisfactory, the abdomen is soft, painless, physiological functions are not disturbed. The patient is under the supervision of an oncologist at the place of residence, adjuvant chemotherapy is being carried out according to the FOLFOX scheme. nine0003
CRC in combination with pregnancy is a major clinical problem. At a young age, CRC is rare and, as a rule, in patients with a genetic predisposition. However, hereditary forms of cancer, as well as chronic inflammatory bowel disease, are rare in pregnant women with CRC. So, in the study by R. Girard et al. [9], only 4 out of 19 patients had these factors. There have been suggestions about the role of hormones in the occurrence of tumors, the level of which increases during pregnancy. However, in the study by M. Slattery et al. [15], only 1 out of 156 samples of colorectal malignant tumors in pregnant women turned out to be positive for estrogen receptors, and none of them showed positive receptors for progesterone. Single reports have been published on the role of insulin-like growth factor I (IGF I), placental growth factor and pro-angiogenic factors, the level of which increases during pregnancy [10]. Thus, to date, the genesis of CRC in pregnant women has been little studied, and the results of studies conducted in this area raise more questions than they answer. nine0003
So, in the study by R. Girard et al. [9], only 4 out of 19 patients had these factors. There have been suggestions about the role of hormones in the occurrence of tumors, the level of which increases during pregnancy. However, in the study by M. Slattery et al. [15], only 1 out of 156 samples of colorectal malignant tumors in pregnant women turned out to be positive for estrogen receptors, and none of them showed positive receptors for progesterone. Single reports have been published on the role of insulin-like growth factor I (IGF I), placental growth factor and pro-angiogenic factors, the level of which increases during pregnancy [10]. Thus, to date, the genesis of CRC in pregnant women has been little studied, and the results of studies conducted in this area raise more questions than they answer. nine0003
Symptoms of CRC in pregnant women do not differ from the classic symptom complex - abdominal pain, anemia, constipation, rectal bleeding. These manifestations can also occur during normal pregnancy, which leads to late diagnosis [14]. So, in the largest study by M. Bernstein et al. [2], which included 39 patients, according to the Dukes classification, there was no stage A in any observation, stage B was noted in 41%, stage C in 44%, and stage D in 15% of patients.
So, in the largest study by M. Bernstein et al. [2], which included 39 patients, according to the Dukes classification, there was no stage A in any observation, stage B was noted in 41%, stage C in 44%, and stage D in 15% of patients.
Instrumental diagnosis of CRC in pregnant women has a number of features. Performing sigmoidoscopy and partial colonoscopy of the left colon in pregnant women is safe [4]. If it is necessary to examine the right sections of the colon, the procedure should be performed with caution, since the development of inferior vena cava compression syndrome is possible [3]. nine0003
Computed tomography is contraindicated due to the risk of radiation damage to the fetus. The methods of choice are magnetic resonance imaging (MRI) and ultrasound.
Clinical and epidemiological signs of CRC in pregnant women and in the general population are presented in the table.
Clinical and epidemiological signs of colorectal cancer in pregnant women and in the general population
The choice of tactics for the treatment of CRC in combination with pregnancy depends on the stage of the disease and on the gestational age. nine0003
nine0003
When diagnosing CRC during the first half of pregnancy, most sources of literature at the early stages recommend surgery with preservation of pregnancy, in the presence of signs of tumor invasion into neighboring structures or in the presence of distant metastases, termination of pregnancy with subsequent complex treatment. Surgical intervention with preservation of pregnancy in its first half is associated with the risk of fetal death in no more than 3.8% of cases [11]. When diagnosing a tumor in the second half of pregnancy, it is recommended to postpone the operation until the time of delivery, which should occur as early as possible. It is believed that a viable baby can be born after 32 weeks of gestation. The method of delivery does not matter; childbirth is possible both through the natural birth canal and by caesarean section. At the same time, CRC surgery can be combined with a caesarean section or postponed for 1-2 weeks in order to reduce the size of the uterus [13].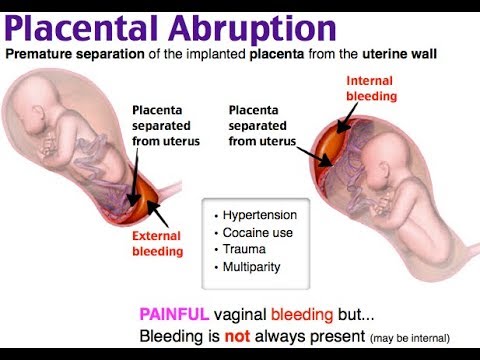 The latter is especially important in low rectal cancer. nine0003
The latter is especially important in low rectal cancer. nine0003
Removal of a tumor with signs of invasion into neighboring structures should be carried out as a single block; if there are signs of tumor invasion into the uterus, hysterectomy is indicated [12].
Most authors recommend performing prophylactic salpingo-oophrectomy due to the high incidence of CRC metastasis in the ovaries in pregnant patients compared with non-pregnant patients (25-30% and 3-8%, respectively) [1, 12]. It is possible to perform a bilateral wedge-shaped resection of the ovaries with an urgent histological examination, based on the results of which a decision is made to remove them. If a decision is made to keep the pregnancy, bilateral salpingo-oophrectomy is not recommended due to the high risk of spontaneous abortion, but wedge resection with urgent histological examination is mandatory [12]. If atypical cells are detected in the resected ovarian tissue, the decision on further tactics should be taken collectively. In the presence of metastatic lesions of the ovaries, the life expectancy of patients is 3–12 months [12]. nine0003
In the presence of metastatic lesions of the ovaries, the life expectancy of patients is 3–12 months [12]. nine0003
Operation in the second half of pregnancy may be associated with severe technical difficulties due to an enlarged uterus, as well as a risk to the fetus with prolonged anesthesia and severe blood loss. In addition, the pressure of the uterus on the inferior vena cava during surgery can lead to the development of compression syndrome of the inferior vena cava. As a prevention of this complication, it is proposed in the literature to place the operating table with an inclination to the left [13].
nine0002 Radiation therapy during pregnancy is contraindicated. Chemotherapy in the first trimester is associated with a high risk of fetal death or malformations and is therefore contraindicated [5]. In case of detection of unresectable CRC in the first trimester, termination of pregnancy with subsequent induction chemotherapy is recommended. In the II and III trimesters, the use of chemotherapy using 5-fluorouracil and leucovorin leads to fetal death or malformations in only 2-6% of cases, although fetal growth retardation or low birth weight is observed in 15-20% of cases [5]. The use of DNA topoisomerase I inhibitors (irinotecan), platinum drugs (oxaliplatin) and targeted drugs (bevacizumab, cetuximab) are traditionally contraindicated in all trimesters of pregnancy. Recently, there have been isolated reports in the literature about the possibility of using irinotecan and oxaliplatin in the II and III trimesters without the development of undesirable effects in the fetus [6, 8]. nine0003
The use of DNA topoisomerase I inhibitors (irinotecan), platinum drugs (oxaliplatin) and targeted drugs (bevacizumab, cetuximab) are traditionally contraindicated in all trimesters of pregnancy. Recently, there have been isolated reports in the literature about the possibility of using irinotecan and oxaliplatin in the II and III trimesters without the development of undesirable effects in the fetus [6, 8]. nine0003 The prognosis for CRC in combination with pregnancy depends on the stage of the disease. In a study by M. Dahling et al. [7], who included 134 pregnant women with CRC, showed no differences in survival rates in the group of patients and in the general population.
Thus, CRC in combination with pregnancy is rare and has certain differences from CRC in the general population. Late diagnosis is due to the fact that the existing symptoms are often not given due importance, this is a serious problem. All pregnant women who complain of rectal bleeding and constipation should be examined by a surgeon and examined with sigmoidoscopy. Currently, in such situations, there are no clear clinical recommendations, and the definition of treatment tactics should be done collegially with the participation of an obstetrician-gynecologist, oncologist, surgeon, anesthetist. The patient should be fully informed about the nature of her disease and possible complications, and her opinion should be decisive. Treatment of CRC in late pregnancy is usually delayed until the time of delivery, which is associated with the risk of developing locally advanced or generalized forms of the disease. The first case presented demonstrates the possibility of successfully performing radical surgery for rectal cancer in late pregnancy with its preservation. nine0003
Currently, in such situations, there are no clear clinical recommendations, and the definition of treatment tactics should be done collegially with the participation of an obstetrician-gynecologist, oncologist, surgeon, anesthetist. The patient should be fully informed about the nature of her disease and possible complications, and her opinion should be decisive. Treatment of CRC in late pregnancy is usually delayed until the time of delivery, which is associated with the risk of developing locally advanced or generalized forms of the disease. The first case presented demonstrates the possibility of successfully performing radical surgery for rectal cancer in late pregnancy with its preservation. nine0003
Treatment of cancer in pregnant patients
REASONS
PAROKONNAYA Anastasia Anatolyevna
Doctor of Medical Sciences, Senior Researcher, Department of Radiosurgery, Research Institute of Clinical and Experimental Radiology, FBSI N.N. N.N. Blokhin” of the Ministry of Health of the Russian Federation
Pregnancy cancer
What types of cancer can occur during pregnancy?
In the first place today, we note the incidence of cervical cancer, melanoma and breast cancer in pregnant women. Further, we are already talking about lymphoproliferative diseases, such as Hodgkin's lymphoma, non-Hodgkin's lymphoma, various types of oncological pathology of the intestine. nine0003
Further, we are already talking about lymphoproliferative diseases, such as Hodgkin's lymphoma, non-Hodgkin's lymphoma, various types of oncological pathology of the intestine. nine0003
But this is a very rare situation, so we still say, first of all, "cervical cancer", "melanoma", "breast cancer". In principle, today these types of cancer in pregnant women have already been learned to be treated quite effectively.
Can pregnancy provoke the development of oncology?
There is a misconception that pregnancy can cause some type of cancer. In fact, pregnancy can accelerate the development of an already existing disease, but it is impossible to provoke some kind of disease to growth. nine0003
Some people think, on the contrary, that pregnancy is such a wonderful condition in which cancer in general
cannot be diagnosed and cannot be established, because this is a sunny state when the whole body of a woman is set to positive, and any oncology is generally unthinkable during this period.
In fact, unfortunately, this is not entirely true. If a woman already had some kind of small tumor, even a few millimeters, then, unfortunately, in some cases, pregnancy can provoke its growth. nine0003
Can IVF cause cancer?
In recent years, we are increasingly talking and hearing that the IVF program and everything related to in vitro fertilization can cause cancer during pregnancy. In my opinion, this is not entirely true.
It is my deep conviction that the IVF program itself and hyperstimulation cannot lead a woman to cancer during pregnancy, because the mechanism is probably different. Probably, unfortunately, women come to the IVF program already having a certain development of the tumor. Let it be minimal, but there is simply no accurate diagnosis during the preparation for the program, firstly. nine0003
Unfortunately, there is no good consultation, for example, by the same mammologist before the IVF program or carrying out extensive diagnostic
measures that would help identify the tumor before starting this program. Therefore, this is how the deployment, the manifestation of the disease, occurs at the moment when in vitro fertilization is performed, and the woman has already, for example, become pregnant.
Therefore, this is how the deployment, the manifestation of the disease, occurs at the moment when in vitro fertilization is performed, and the woman has already, for example, become pregnant.
Therefore, we see and hear more and more about these cases, but in fact, it seems to me that this is not a very clear and precise diagnosis at the stage of preparation for this program. Therefore, it is very important for our fellow reproductive specialists to know and remember that in the modern world, with such a very important event as in vitro fertilization, we must do everything to exclude the possible oncological disease before the program. nine0003
How often can a pregnancy be maintained if cancer is detected?
Of course, at the first visit of a woman with cancer during pregnancy, we must: firstly, assess the stage of the disease. We have the ability to safely diagnose the fetus today. This is the first.
The second, of course, at what stage of pregnancy she came.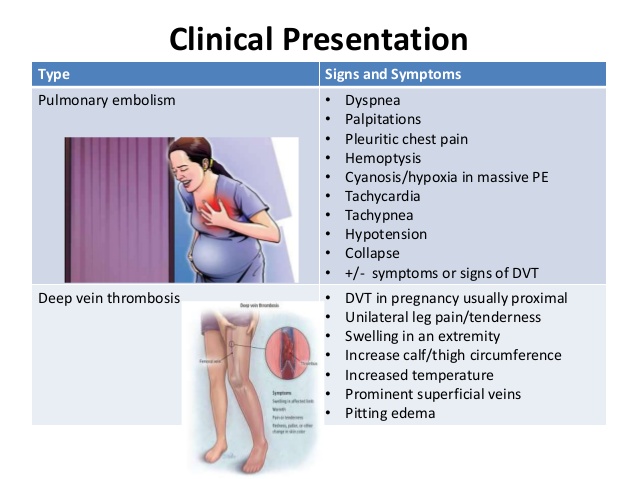 If this is the second or third trimester of pregnancy, we can discuss with the woman the option, for example, of early delivery and the start of treatment after delivery. nine0115 But if a woman comes at the very beginning of her pregnancy, for example, in the first trimester, and she has the fourth stage of cancer, then, unfortunately, in these cases it is sometimes necessary to discuss the option of terminating the pregnancy with her, but this is extremely rare.
If this is the second or third trimester of pregnancy, we can discuss with the woman the option, for example, of early delivery and the start of treatment after delivery. nine0115 But if a woman comes at the very beginning of her pregnancy, for example, in the first trimester, and she has the fourth stage of cancer, then, unfortunately, in these cases it is sometimes necessary to discuss the option of terminating the pregnancy with her, but this is extremely rare.
Again, I repeat that they come far from the first trimester, but usually come in the middle of the second trimester, when it is simply inhuman, in my opinion, to terminate a pregnancy at a period of 24-25 weeks, when the arms, legs, head are already formed - we already have everything. All that remains is to develop this fetus, this child. nine0003
Of course, if the stage is still quite common, and we are talking about saving, immediately saving the life of a woman, we have to discuss abortion with her, but, I say again, this is very rare today, because, again, I repeat: we have learned already treat such women at any time.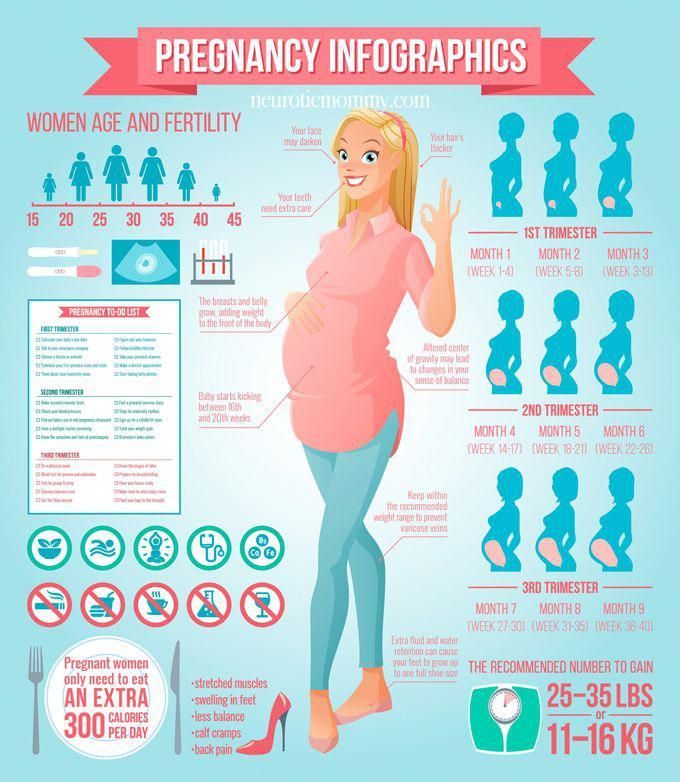
Symptoms and treatment features
What signs and symptoms of breast cancer should alert a pregnant woman?
Oncological disease, unfortunately, of course, depends on the phase or duration of pregnancy with which the patient applied, having this disease. If the patient comes in late pregnancy, and the tumor began to appear, appeared and began to develop somewhere at the beginning of this pregnancy, respectively, by the end of pregnancy, this tumor will reach a large size. This is the first moment. nine0003
The second thing that affects the development of the disease during pregnancy. Unfortunately, I am very sad to talk about this, but I am forced to say this. These are the mistakes of our doctors, who often take, for example, an inflammatory disease, the same mastitis, or some related problems associated with pregnancy, for an accompanying calm pathological process, of course, but not cancer.
The problem here is that these doctors consider it possible to try to treat such patients on their own, not to make a diagnosis in time, not to conduct the minimum oncological examination that we need in order to make a diagnosis on time. nine0003
nine0003
Therefore, first of all, think about the fact that your life and the life of your unborn child are in your hands.
Maybe even apply without a referral, and then, when the initial diagnosis is made, continue or not continue the examination, because, as I said, the processes and treatment are connected, first of all, with the golden time that you spend thinking , doubt, listening to neighbors and an illiterate doctor.
Therefore, first of all, think about the fact that your life and the life of your unborn child are in your hands. nine0122
What influences the development of cancer during pregnancy?
Oncological disease, unfortunately, of course, depends on the phase or duration of pregnancy with which the patient applied, having this disease. If the patient comes in late pregnancy, and the tumor began to appear, appeared and began to develop somewhere at the beginning of this pregnancy, respectively, by the end of pregnancy, this tumor will reach a large size. This is the first moment. nine0003
This is the first moment. nine0003
The second thing that affects the development of the disease during pregnancy. Unfortunately, I am very sad to talk about this, but I am forced to say this. These are the mistakes of our doctors, who often take, for example, an inflammatory disease, the same mastitis, or some related problems associated with pregnancy, for an accompanying calm pathological process, of course, but not cancer.
The problem here is that these doctors consider it possible to try to treat such patients on their own, not to make a diagnosis in time, not to conduct the minimum oncological examination that we need in order to make a diagnosis on time. nine0003
The main problem is that a woman comes not of her own free will, but with a very large tumor. Maybe she would like to come earlier, but the doctor at the place of residence says: “Calm down, everything is fine. Unfortunately, this is a normal condition during pregnancy.” It costs nothing for the doctor to send the patient once again, if he has any doubts, to the oncologist.
This is not a very complicated procedure, and, in fact, not to an oncologist, but at least to a surgeon who is behind your wall, not far from your institution. But this is the problem. nine0003
I must say that this is not only a problem of the regions or some remote cities, maybe from Moscow or St. Petersburg. This is a problem in Moscow too, because recently I had a patient who was treated for 6 months of her pregnancy from lactational mastitis, despite the fact that she had widespread breast cancer, the third stage of the disease with an advanced clinical picture, with damage to the lymph nodes, with altered skin.
In general, even maybe a first-year resident could have already diagnosed cancer, but, nevertheless, the doctor of a respected institution did not consider it necessary to check the diagnosis and carry out some minimum diagnosis. It all ended very badly. The woman gave birth to a child, but she died shortly after she gave birth to a baby. nine0003
Therefore, I say again that, in general, not the pregnancy itself affects the development of the disease, but everything that accompanies this pregnancy: illiteracy of the doctor, late diagnosis, the woman's fear of going to the doctor on time, because she does not want sometimes it’s just to hear terrible, in her opinion, words. The word "cancer" sounds to her, especially against the background of pregnancy, just like a disaster. I must say that there is no need to be afraid, because your life depends, first of all, on the terms of treatment with which you will come to the doctor, a specialist in this direction. nine0003
The word "cancer" sounds to her, especially against the background of pregnancy, just like a disaster. I must say that there is no need to be afraid, because your life depends, first of all, on the terms of treatment with which you will come to the doctor, a specialist in this direction. nine0003
Cancer is not transmitted to a child! Children are born healthy!
Proven in thousands of cancer patients, men and women.
SURVEYS
Anastasia Anatolyevna Parokonnaya
Doctor of Medical Sciences, Senior Researcher, Department of Radiosurgery, Research Institute of Clinical and Experimental Radiology Federal State Budgetary Institution National Research Center of Oncology named after N.N. N.N. Blokhin” of the Ministry of Health of the Russian Federation
What examinations should a pregnant woman undergo to select a treatment? nine0078
When we start examining a pregnant patient, of course, we must consider which diagnostic method is safe for the fetus.
Today, the number of methods that actually harm the unborn child is rather limited. Of course, it is undesirable to perform magnetic resonance imaging, for example, or positron emission tomography, or to take an x-ray of the lower parts of the body where the abdomen is located. But, for example, regular mammography with protection of the abdomen or a regular x-ray of the lungs - we can do these things today in pregnant women if necessary. nine0003
But many types of cancer today are diagnosed quite successfully with the help of, firstly, ultrasound navigation, that is, already on ultrasound, often a great specialist - I emphasize again, ultrasound - sees that this is a malignant pathology, this is the first. The second is that we perform a biopsy of this formation at any stage of pregnancy, get a histology and already understand what we are dealing with, is it cancer or some other disease.
Are special examinations required for such patients? nine0078
Special examinations for pregnant patients are not required.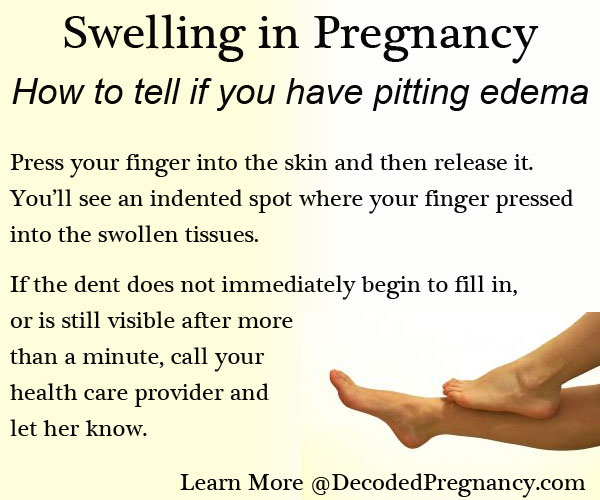 We just need to deliberately, I emphasize again, approach the issue of diagnostics, figure out what is safe at this time, what is desirable, what is not.
We just need to deliberately, I emphasize again, approach the issue of diagnostics, figure out what is safe at this time, what is desirable, what is not.
In the first trimester, unfortunately, some diagnostic procedures are generally undesirable.
Even if magnetic resonance imaging is needed, it is highly undesirable in the first trimester, and you need to think about what options you can use instead of MRI. The same ultrasound sometimes allows you to answer the question whether it is oncology or not. We must again collectively resolve this issue of the safety of a particular diagnostic method at a particular time. nine0003
At what stages is cancer usually detected in pregnant women?
The whole problem here is that we do not detect a tumor in the initial stage in pregnant women. As a rule, pregnant women come to us with advanced stages and in the second or early third trimester, when it is no longer possible and undesirable to terminate the pregnancy, when the tumor has already reached a very large size.
Then we have to think together with obstetricians about which treatment option to select for this woman. nine0115 The percentage of morbidity in pregnant women is, in principle, not very high.
TREATMENT
PAROKONNAYA Anastasia Anatolyevna
Doctor of Medical Sciences, Senior Researcher, Department of Radiosurgery, Research Institute of Clinical and Experimental Radiology, FBSI N.N. N.N. Blokhin” of the Ministry of Health of the Russian Federation
Treatment of cancer in pregnant women
How advanced are modern cancer treatments for pregnant women? nine0078
About twelve years ago in Russia it was absolutely impossible to imagine that you and I would treat a pregnant patient and keep her pregnant, because the approach to such women was absolutely merciless, let's say.
It was believed that the pregnancy should be terminated at any time, as soon as she applied to the hospital with oncological pathology. Sometimes women terminated this pregnancy at 28 - 29 - 30 weeks of pregnancy, without saving the fetus, without resuscitating it, which was impossible in those years. nine0003
Sometimes women terminated this pregnancy at 28 - 29 - 30 weeks of pregnancy, without saving the fetus, without resuscitating it, which was impossible in those years. nine0003
Sometimes women terminated this pregnancy at 28 - 29 - 30 weeks of pregnancy, without saving the fetus, without resuscitating it, which was impossible in those years.
Of course, life's tragedies were behind this. Today we have learned to treat such women without terminating the pregnancy, and this treatment is complete, and it includes all types of assistance - exactly the same that a non-pregnant woman with one or another oncological pathology would receive.
What is the difference between cancer treatment in pregnant women in Russia and abroad? nine0078
Today we can safely say that our level of treatment for this group of patients with pregnancy does not differ from, for example, foreign analogues. Why? Because today we are working directly in such a big connection, in an international working group that today unites 37 centers in Europe, America, today Mexico is also involved in this work, because this working group allows us all to collectively discuss all cases of cancer development during pregnancy and collectively select treatment options. nine0003
nine0003
Among my colleagues are colleagues from Belgium, Israel, from Italy (from the Milan Oncology Center), from the clinic in Leuven, from Frankfurt am Main. The modern capabilities of the Internet allow us today to conduct online consultations that determine the fate of a particular patient. I must say that basically, until today, all our joint decisions have led to the fact that we decided to treat patients without terminating the pregnancy. We have such opportunities.
In Russia, all the methods that we use in the treatment of these patients are exactly the same as in Israel or Italy. We have the same treatment regimens. I must say that these schemes are almost monthly reviewed collegially by us. Once every three months, we gather with our colleagues, we used to gather until recently in one country or another. nine0003
Now this is happening online, at small conferences, and we are discussing what we can offer our pregnant patients today, how to track the health of their children, how, in fact, they will live on, how these children develop. We share our results.
We share our results.
It must be said that in this sense Russia is not in last place, if not in second or third place. Therefore, I think that over the past ten years we have made quite a lot of progress in this direction. nine0003
Is it possible for pregnant women with oncology to be treated in the regions?
Today, of course, federal centers have the greatest experience in treating such pregnant patients. Federal centers, clinical, located in Moscow, St. Petersburg. Most often, women turn to these centers, but today we have the opportunity to treat such women in our regions. Why?
This has become possible because we are developing the issue of telemedicine. Almost every week we consult our colleagues from remote regions on telemedicine, discussing with them the possibilities of treating pregnant women with oncology. We jointly determine which treatment courses are possible, for how long. nine0003
If a woman feels some kind of trouble, if her treating person, for example, an obstetrician, who observes her, suspects that there is an oncological pathology, of course, she should immediately be referred to an oncologist.
First, this is the district oncologist, who should already give a referral - preferably to the federal center, because this is the place, this is the clinic, where there is the greatest experience in managing such patients. This is first.
Secondly, today in the federal centers we have the same international composition of the council. We can connect various institutions of other European or American colleagues and discuss with them. At the level of the district clinic, there will probably not be such opportunities. Therefore, I think that district oncologists should not have any difficulties with referral to the federal center. nine0003
Once again I remind you, our dear patients, that you have the right to be treated in the place you want. You do not have the right to refuse, for example, a referral to a federal clinic or to the clinic that you have chosen for yourself.
Physicians who treat pregnant cancer patients
Surgeons
Oncologists
Geneticists
Obstetricians
Psychologists
Treatment safety
nine0002Do drugs taken by a pregnant woman affect the baby?
Of course, various chemicals affect the fetus. In the first trimester of pregnancy, especially from the 8th to the 15th week of pregnancy, the use of various drugs and medications is undesirable, because there is a laying, the so-called period of organogenesis, when the main organs of the child are laid, and a violation of this process is highly undesirable.
In the first trimester of pregnancy, especially from the 8th to the 15th week of pregnancy, the use of various drugs and medications is undesirable, because there is a laying, the so-called period of organogenesis, when the main organs of the child are laid, and a violation of this process is highly undesirable.
But there are situations when we still have to start treating a woman. Those chemotherapeutic drugs that are in the arsenal of oncologists today, in some cases, can be used starting from 13-14 weeks, that is, this is the second trimester, the beginning of the second trimester. nine0115 In this situation, we first check the fetus for various anomalies. If the fetus is healthy, then the probability that at this
term the drugs that we use today and have proven to be safe will be extremely low. Therefore, different cancers are treated with different drugs.
There are diseases, such as melanoma, that require treatment with drugs that are highly toxic to the fetus. Here, of course, questions arise. Sometimes it is necessary to solve such issues with the use of these medicines really together - at the level of an international council, because the drug is obviously toxic at any time, and we need to think ten times whether it can be used or we can get by, for example, with surgical intervention at this time in a patient . nine0003
Here, of course, questions arise. Sometimes it is necessary to solve such issues with the use of these medicines really together - at the level of an international council, because the drug is obviously toxic at any time, and we need to think ten times whether it can be used or we can get by, for example, with surgical intervention at this time in a patient . nine0003
Does pregnancy treatment or early delivery harm the fetus?
If a woman receives, for example, treatment during pregnancy without terminating this pregnancy, receives certain drugs, certain types of operations are performed on her, in this case, is the fetus and unborn child harmed?
In this case, today we can say with greater certainty that, starting from the second trimester, when we treat these women, there is practically no fetal pathology. nine0003
But what can really harm? May harm early delivery in these children. About 10 years ago, when we just started dealing with this problem, we tried with our fellow obstetricians to give birth to our women as quickly as possible, sent them to give birth somewhere at 32-33-34 weeks of pregnancy, because we wanted to continue as soon as possible treatment. We were afraid that the accumulated complex of therapeutic measures would lead to some kind of illness or pathology in this child.
We were afraid that the accumulated complex of therapeutic measures would lead to some kind of illness or pathology in this child.
It turned out that the chemotherapy itself or the operation itself, which is performed on a woman, does not lead to fetal pathology, but the very early delivery of the baby leads. The babies suffered from early births, they were, as we say, deeply premature: they did not breathe well, they did not hear well, they needed resuscitation. Therefore, today, when we treat these women with modern methods, we are not in a hurry to give birth.
We understand that the treatment is effective, the woman receives it in full, and we can extend it until the normal terms of childbirth, and today both 37 and 38 weeks are considered normal terms. In general, the fetus is born already with a good weight, with good growth and does not suffer from medical manipulations. nine0003
It is not worth postponing the treatment of cancer during pregnancy, if it has been diagnosed. I had examples of women who refused to carry out all therapeutic measures only because they were afraid that those substances, those drugs, those operations that we offer them would be very toxic to the fetus and could destroy it.
I had examples of women who refused to carry out all therapeutic measures only because they were afraid that those substances, those drugs, those operations that we offer them would be very toxic to the fetus and could destroy it.
In fact, today we have a pretty clear idea of what drugs we can use in pregnant women safely enough. Therefore, this should not be a reason to postpone treatment. This will end very badly. nine0003
If a woman observes the development of the disease during the entire period of pregnancy and expects that when the birth comes, she will go to the doctor, unfortunately, you may simply not live to see this period. There have been such cases. They are very tragic. In our practice, thank God, we were able to convince a woman that she needed to be treated immediately. But in other clinics, I know, there were such cases.
How safe is radiation therapy for the unborn child?
If today we are talking about the relative safety of chemotherapy and safe surgical treatment, then, of course, it is not necessary to speak in the affirmative about the safety of radiation therapy. nine0003
nine0003
In Russia, we do not use radiation therapy in pregnant patients, although there are two European centers: in Greece and in Italy, which use radiation therapy in pregnant patients with certain protection, with a lead apron, covering, so to speak, the abdomen with special pads and conducting radiation therapy in the first trimester. Those doctors who perform this
study in these centers are convinced that radiation therapy does not harm the fetus. But today we still don’t have long-term results of these manipulations, and our experience has shown that, in general, today we can still get by with chemotherapeutic drugs rather than radiation therapy. nine0003
But I think that with the development of different methods of radiation therapy, gentle radiation, for example, only the area that is sick, such a directed beam of radiation therapy, we will soon be able to use it in pregnant patients too.
How can the patient help the doctor in the treatment process?
If a woman feels any trouble, for example, in the same breast, do not try to treat herself. She should, of course, contact a doctor for any symptoms. This will be her help to the doctor. The sooner we make a diagnosis, the easier it will be for us to treat later. nine0003
She should, of course, contact a doctor for any symptoms. This will be her help to the doctor. The sooner we make a diagnosis, the easier it will be for us to treat later. nine0003
If treatment is already underway, what kind of assistance is required from our patients? Of course, in time to fulfill all the appointments of the doctor. Finally, what do we demand and ask from our patients after the completion of the treatment? Do not forget about us, because, despite the happiness that they will gain by giving birth to a healthy child -
I emphasize again, against the background of the treatment - some of them relax and decide that this is where the fight against the disease ends.
Unfortunately, the struggle continues, and it continues sometimes not for one year, but for several subsequent years, when these patients must take certain drugs. At the same time, they naturally take care of the baby that is next to them, and sometimes they forget that they were once sick with something. Therefore, over the next 2-3 years, we ask you to still remember us, do not forget us and come to us for examination as needed. nine0003
Therefore, over the next 2-3 years, we ask you to still remember us, do not forget us and come to us for examination as needed. nine0003
How well developed is the treatment regimen for pregnant women with breast cancer?
Breast cancer is one of the most common forms of oncology in pregnant patients, but it must be said that this type of cancer is the most studied, most tested to date and in the localization in which we feel quite confident today with treatment of these patients.
Today, treatment regimens have already been worked out. I must say that we worked out these schemes together with our European colleagues. nine0003
This was done at special consultations, special conferences, where one or another variant and regimen of drug therapy was selected.
Today, drug therapy for breast cancer is well developed. At different stages of pregnancy and different variants and stages, we already clearly know what treatment regimen we can apply to these women.
Features of radioiodine therapy in pregnant women
RUMYANTSEV Pavel Olegovich
MD, oncologist, radiologist, endocrinologist, Deputy Director of the National Research Center for Endocrinology of the Ministry of Health of the Russian Federation, Director of the Institute of Oncoendocrinology
Can pregnant women receive radioiodine therapy?
For pregnant women, radioiodine therapy, as well as radiodiagnosis, as well as radioisotope diagnostics in general, is contraindicated in any way. Nursing - the same. You can contrive and between feedings at some time go through a short diagnostic procedure with the same technetium - it is quickly excreted - but these are rather such exceptions.
Such situations rarely occur, but somewhere you can slip through. But in general, in general, pregnancy and feeding are contraindications for radionuclide diagnostics, radionuclide therapy without exception. nine0003
How does this treatment affect fertility in men and women?
Now the question of the consequences in terms of reproductive function is a question that also often arises for both men and women.
Let's start with women, they are more vulnerable in this regard in all respects, because, in fact, this is the contingent that more often suffers from thyroid diseases, thyroid cancer and thyrotoxicosis.
The second point is that this is a question that is connected precisely with the effect on the female reproductive system, which is more complicated. Of course, there should always be a stipulation. nine0003
In general, radionuclide therapy has been shown to be safe for reproduction, just not within the 6 month period when we impose a moratorium. The quality, success of your pregnancy, the health of the child, and the gestation are not affected in any way by previous radioiodine therapy.
We had girls who gave birth after multiple sessions of radionuclide therapy, there are no problems at all.
In men, the same thing: there is no effect on spermatogenesis.
The only thing is when very high activity is rare, then they can
there are risks for both girls and boys, when very often and very much, reproductive dysfunction. In this situation, it is better to use the so-called assisted reproductive technologies.
In this situation, it is better to use the so-called assisted reproductive technologies.
It is better to take healthy eggs before high-dose, powerful radioiodine therapy and then make sure in terms of the birth of healthy offspring after therapy. Then, no matter what happens, you always have a reserve of eggs, embryos. We have a powerful reproductive department, and we always consult with them, they insure us. But in general, yes, pregnancy is a very important issue for us, it was studied separately and carefully. There is no delayed, remote influence, but radionuclide therapy during pregnancy and feeding is prohibited. nine0003
Today there is a clear statement: if there is no life-threatening condition for the pregnant woman and the fetus, then it is better to postpone the treatment of thyrotoxicosis and thyroid cancer until term, childbirth, after pregnancy. Do not interfere with the process of natural gestation and allow the woman natural or assisted delivery.
Breastfeeding and pregnancy planning
PAROKONNAYA Anastasia Anatolyevna
Doctor of Medical Sciences, Senior Researcher, Department of Radiosurgery, Research Institute of Clinical and Experimental Radiology, FBSI N.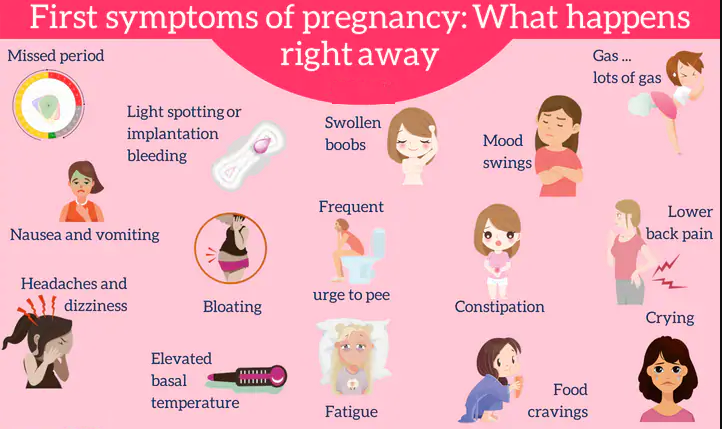 N. N.N. Blokhin” of the Ministry of Health of the Russian Federation
N. N.N. Blokhin” of the Ministry of Health of the Russian Federation
How does treatment affect breastfeeding and childbearing?
Can a woman breastfeed during treatment?
To the question of lactation, for example, of a pregnant patient who underwent cancer treatment after the birth of a child. Is it possible to feed or not a baby who, for example, was born to such a mother? As a rule, mothers continue to be treated with chemotherapy after childbirth. This process takes another 3-4 months.
Therefore, it is probably not worth feeding a child with chemotherapy drugs. Still, he has already suffered enough in the womb, so it makes sense to interrupt lactation, and we do this for our patients. The child is supplemented with special mixtures.
Is breastfeeding possible after cancer treatment?
Once you had a breast disease, for example, you had one mammary gland partially or completely removed, you once received full treatment and now, having agreed with the doctor, you gave birth to this child.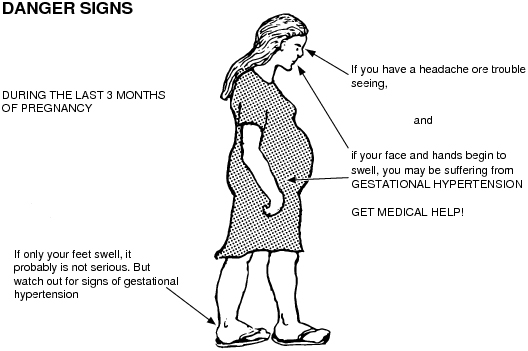 In this case, is it possible to feed him? nine0003
In this case, is it possible to feed him? nine0003
There are no contraindications to lactation in this case. We allow children to be fed. Our women even manage to feed a child for 6 months in the absence of one mammary gland.
Another thing is that lactation is so short, about 6-7 months, no more. Then comes the depletion of the second mammary gland. Even if the resected mammary gland, that is, part of the gland is preserved, lactation is also short-lived, because the radiation therapy carried out leads to the formation of fibrosis in the mammary gland, and there are few healthy milk-producing lobules in the mammary gland. But there are no direct contraindications to such lactation, to feeding the child after the operation. nine0003
When can pregnancy be planned after cancer treatment?
It is possible to plan a subsequent pregnancy after 2-3 years. Why such a period?
Firstly, by this moment the main treatment and chemotherapy, sometimes hormone therapy, are over. True, today hormone therapy lasts up to 5 years, but after 2-3 years we can discuss, for example, its short-term stop. This is the first.
True, today hormone therapy lasts up to 5 years, but after 2-3 years we can discuss, for example, its short-term stop. This is the first.
Second - 2-3 years is, unfortunately, that dangerous period when the disease can return, and it returns with different forms of the disease, with different forms of cancer. This is also biologically inexplicable today, but, nevertheless, for these 2-3 years, a woman should take care, first of all, about herself and come to the examinations on time. nine0003
If this dangerous period is lived through, survived, then we can already discuss issues related to subsequent pregnancy.
Unfortunately, our life today is such that many women at the age of 34-35 do not yet have a child. It is from this age that various oncological diseases begin. A woman approaches the treatment period without having a child, and the possibility of a subsequent pregnancy is questionable.
I must say that today this issue is being resolved positively. Today there are no strict prohibitions on pregnancy after cancer treatment. If a woman feels well, if she is effectively, fruitfully, let's say, treated, if she has
If a woman feels well, if she is effectively, fruitfully, let's say, treated, if she has
a period of remission has come - and we can talk about this, 2-3 years after the completion of treatment - she can discuss with her oncologist the question of a subsequent pregnancy.
Of course, we should discuss each such pregnancy and such a decision with our patient, because if the stage is widespread and there is a long, long-term treatment for more than one year, it is better to wait with pregnancy and not think about it yet. We must deal with the main task - the treatment of the disease.
But if you have the initial stage of the disease, if a sufficiently long period of time has passed, if your menstrual function has been preserved, if you live well in a family, you have a wonderful husband and you are planning a pregnancy, today it is not forbidden to discuss the issue of a subsequent pregnancy with an oncologist. nine0003
There is even evidence that women who have had a subsequent pregnancy and were previously treated for breast cancer have a much higher survival rate than those who did not have this pregnancy.