Umbilical cord from mom to baby
Umbilical cord care in newborns Information | Mount Sinai
Cord - umbilical; Neonatal care - umbilical cord
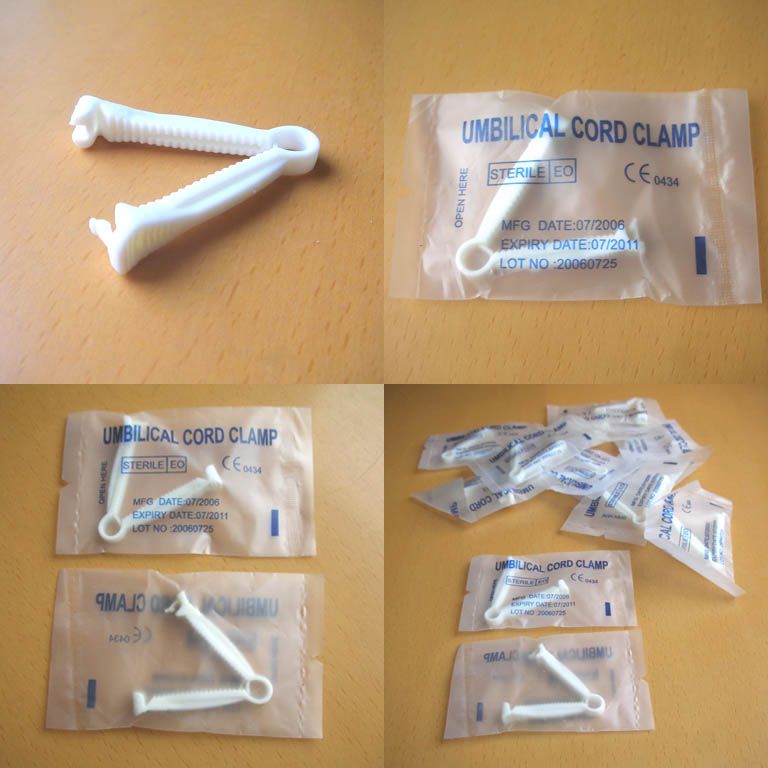
The umbilical cord connects the baby to the mother's placenta. During fetal development in the womb, the umbilical cord is the lifeline to the baby supplying nutrients. After birth, the cord is clamped and cut. Eventually between 1 to 3 weeks the cord will become dry and will naturally fall off. During the time the cord is healing it should be kept as clean and as dry as possible.
A sponge bath is the best way to clean your baby until the umbilical cord falls off. To give a sponge bath, dip a soft cloth in the warm water and wring out the excess. If needed, a mild soap can be used in the water. Wipe the baby's skin gently starting from the area of the baby's head and work your way down to the rest of the body. Pay special attention to the skin creases and diaper area. Rinse your baby with clean warm water and dry him or her completely.
Information
When your baby is born the umbilical cord is cut and there is a stump left. The stump should dry and fall off by the time your baby is 5 to 15 days old. Keep the stump clean with gauze and water only. Sponge bathe the rest of your baby, as well. Do not put your baby in a tub of water until the stump has fallen off.
Let the stump fall off naturally. Do not try to pull it off, even if it is only hanging on by a thread.
Watch the umbilical cord stump for infection. This does not occur often. But if it does, the infection can spread quickly.
Signs of a local infection at the stump include:
- Foul-smelling, yellow drainage from the stump
- Redness, swelling, or tenderness of the skin around the stump
Be aware of signs of a more serious infection. Contact your baby's health care provider immediately if your baby has:
- Poor feeding
- Fever of 100.
 4°F (38°C) or higher
4°F (38°C) or higher - Lethargy
- Floppy, poor muscle tone
If the cord stump is pulled off too soon, it could start actively bleeding, meaning every time you wipe away a drop of blood, another drop appears. If the cord stump continues to bleed, call your baby's provider immediately.
Sometimes, instead of completely drying, the cord will form pink scar tissue called a granuloma. The granuloma drains a light-yellowish fluid. This will most often go away in about a week. If it does not, call your baby's provider.
If your baby's stump has not fallen off in 4 weeks (and more likely much sooner), call you baby's provider. There may be a problem with the baby's anatomy or immune system.
Esper F. Postnatal bacterial infections. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine.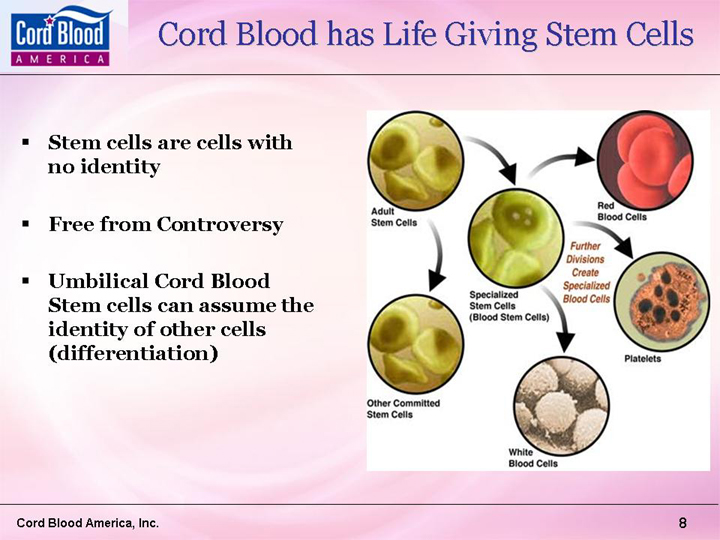 11th ed. Philadelphia, PA: Elsevier; 2020:chap 48.
11th ed. Philadelphia, PA: Elsevier; 2020:chap 48.
Nathan AT. The umbilicus. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 125.
Taylor JA, Wright JA, Woodrum D. Newborn nursery care. In: Gleason CA, Juul SE, eds. Avery's Diseases of the Newborn. 10th ed. Philadelphia, PA: Elsevier; 2018:chap 26.
Wesley SE, Allen E, Bartsch H. Care of the newborn. In: Rakel RE, Rakel DP, eds. Textbook of Family Medicine. 9th ed. Philadelphia, PA: Elsevier; 2016:chap 21.
Last reviewed on: 12/10/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Embryology, Umbilical Cord - StatPearls
Introduction
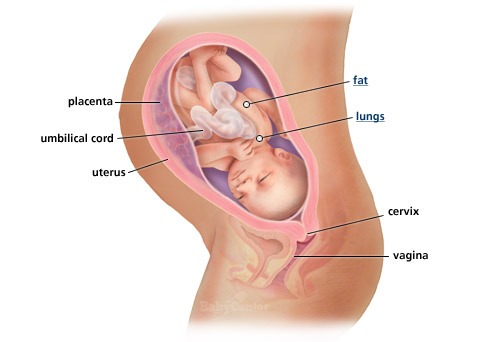
The umbilical cord is the vital connection between the fetus and the placenta.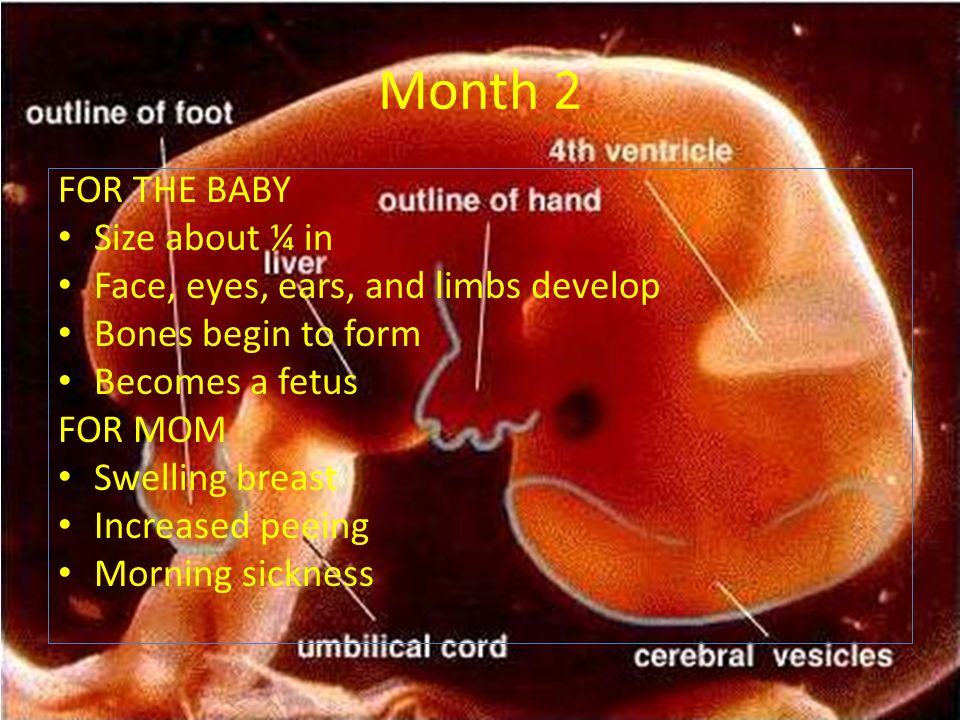 Umbilical cord development begins in the embryologic period around week 3 with the formation of the connecting stalk. By week 7, the umbilical cord has fully formed, composed of the connecting stalk, vitelline duct, and umbilical vessels surrounding the amniotic membrane. The umbilical vessels carry the fetal blood back and forth to the placenta, with the umbilical vein carrying oxygenated blood with nutrients from the placenta to the fetus and the umbilical arteries transporting deoxygenated blood with waste products from the fetus to the placenta. Embryonic structures regress near the end of the first trimester, leaving the umbilical cord composed of two umbilical arteries and one umbilical vein surrounding by a gelatin-like extracellular matrix known as Wharton’s jelly. Elongation of the umbilical cord occurs primarily in the second trimester. The average umbilical cord is 50 to 60 centimeters in length, 2 centimeters in diameter, with up to 40 helical turns. Abnormalities of the umbilical cord can lead to increased morbidity and mortality of the fetus.
Umbilical cord development begins in the embryologic period around week 3 with the formation of the connecting stalk. By week 7, the umbilical cord has fully formed, composed of the connecting stalk, vitelline duct, and umbilical vessels surrounding the amniotic membrane. The umbilical vessels carry the fetal blood back and forth to the placenta, with the umbilical vein carrying oxygenated blood with nutrients from the placenta to the fetus and the umbilical arteries transporting deoxygenated blood with waste products from the fetus to the placenta. Embryonic structures regress near the end of the first trimester, leaving the umbilical cord composed of two umbilical arteries and one umbilical vein surrounding by a gelatin-like extracellular matrix known as Wharton’s jelly. Elongation of the umbilical cord occurs primarily in the second trimester. The average umbilical cord is 50 to 60 centimeters in length, 2 centimeters in diameter, with up to 40 helical turns. Abnormalities of the umbilical cord can lead to increased morbidity and mortality of the fetus.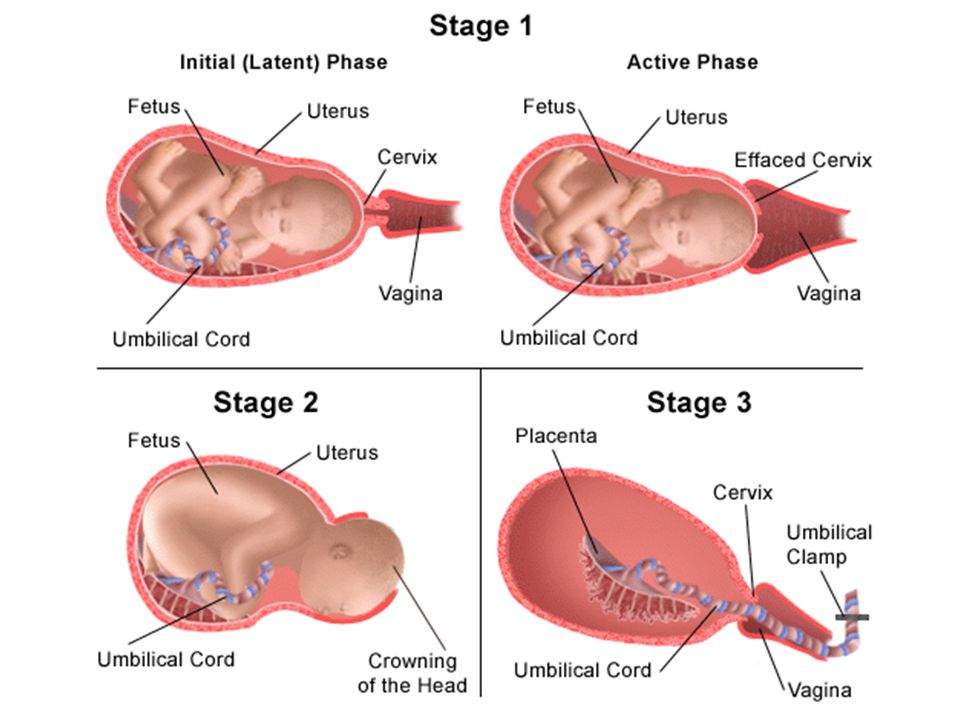
Development
The development of the umbilical cord begins in the third week of embryologic formation. The developing embryo consists of a trilaminar disc attached to the decidua basalis by the connecting stalk, the primitive umbilical cord.[1][2] The connecting stalk is a thick stalk of the extraembryonic membrane extending from the caudal end of the embryo to the center of the developing placenta on the decidua basalis.[3] The process of body folding occurs during week four with rapid growth amnion and embryonic disc compared to the yolk sac. Cranial caudal folding causes approximation of the connecting stalk and yolk sac on the ventral surface of the embryo.[1][2] The amnion expands to cover the entire embryo except for the rudimentary umbilical ring, where the connecting stalk and yolk sac emerge.[1][2] During this time, the allantois, an outpouching of the endodermal hindgut, forms and extends into the connecting stalk.[1][2][4] Between the fourth and eighth weeks, there is an increase in amniotic fluid production, which causes the amniotic cavity to swell and fill the chorionic space.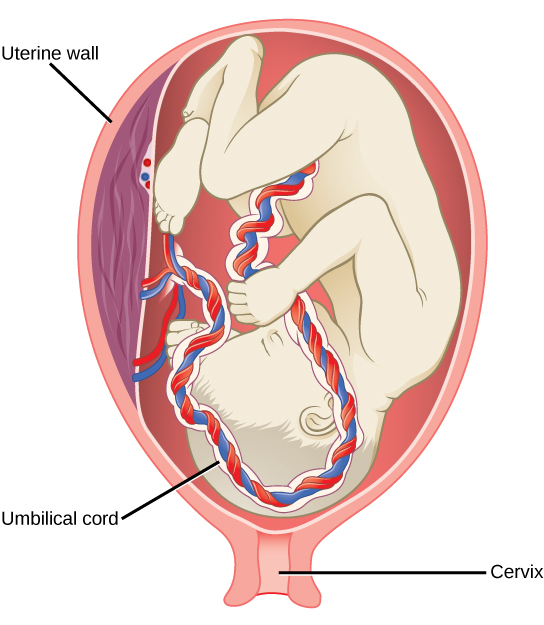 This increase in the amniotic fluid also causes elongation of the connecting stalk, and the yolk sac is compressed down within the connecting stalk to form the omphalomesenteric or vitelline duct.[1][2][5] The expansion of the amniotic cavity causes the amnion and the chorion to come into contact, and the extraembryonic mesoderm covering these two layers fuses. As such, the chorionic cavity disappears, leaving the umbilical cord, the composite of the connecting stalk and vitelline duct surrounded by the amnion, floating in the amniotic fluid.[1][2][4]
This increase in the amniotic fluid also causes elongation of the connecting stalk, and the yolk sac is compressed down within the connecting stalk to form the omphalomesenteric or vitelline duct.[1][2][5] The expansion of the amniotic cavity causes the amnion and the chorion to come into contact, and the extraembryonic mesoderm covering these two layers fuses. As such, the chorionic cavity disappears, leaving the umbilical cord, the composite of the connecting stalk and vitelline duct surrounded by the amnion, floating in the amniotic fluid.[1][2][4]
Starting in week three, endothelial precursor cells in the mesoderm surrounding the allantois coalesce to form small capillaries. Vasculogenesis continues, and by the end of the third week, the capillaries have grown to establish a functional vascular network within the connecting stalk. During the same period, the arterial and venous systems within the embryo are developing. The arterial system is initially established as the paired dorsal aortae from which the aortic arches originate.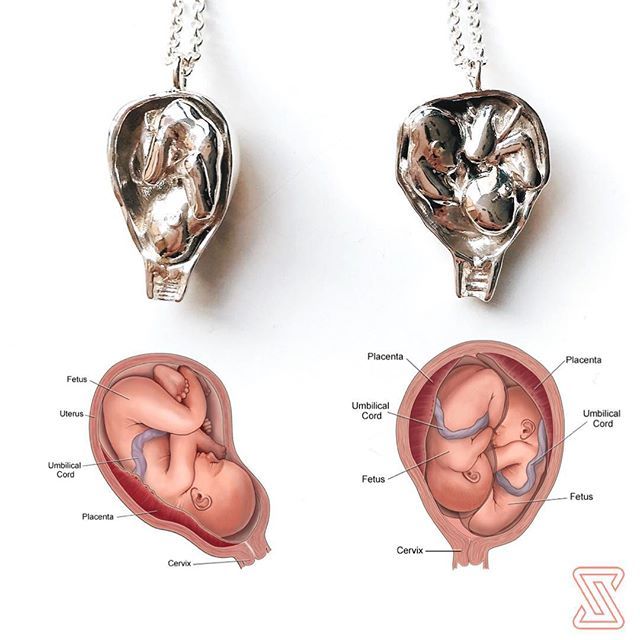 The primitive venous system is initially made up of the umbilical, vitelline, and cardinal systems. Early in the fourth week, two umbilical arteries branch from the paired dorsal aortae to become connected to the vascular network of the umbilical cord.[1] During the fifth week, this connection is obliterated as the umbilical arteries develop their connection to a branch of the fifth pair of lumbar intersegmental arteries that will later become the internal iliac arteries.[1][2][4] The umbilical veins are originally bilateral and drain into the right and left sinus horns of the sinus venosus. The connections of the umbilical veins to the sinus horns regress in the second month with complete regression of the right umbilical vein as the left umbilical vein persists and forms its connection to the ductus venosus within the developing liver.[2][4] With the initiation of fetal heart pumping around week four, the umbilical arteries carry deoxygenated blood to the placenta, and the umbilical vein carries oxygenated blood back to the fetus from the placenta.
The primitive venous system is initially made up of the umbilical, vitelline, and cardinal systems. Early in the fourth week, two umbilical arteries branch from the paired dorsal aortae to become connected to the vascular network of the umbilical cord.[1] During the fifth week, this connection is obliterated as the umbilical arteries develop their connection to a branch of the fifth pair of lumbar intersegmental arteries that will later become the internal iliac arteries.[1][2][4] The umbilical veins are originally bilateral and drain into the right and left sinus horns of the sinus venosus. The connections of the umbilical veins to the sinus horns regress in the second month with complete regression of the right umbilical vein as the left umbilical vein persists and forms its connection to the ductus venosus within the developing liver.[2][4] With the initiation of fetal heart pumping around week four, the umbilical arteries carry deoxygenated blood to the placenta, and the umbilical vein carries oxygenated blood back to the fetus from the placenta. [4]
[4]
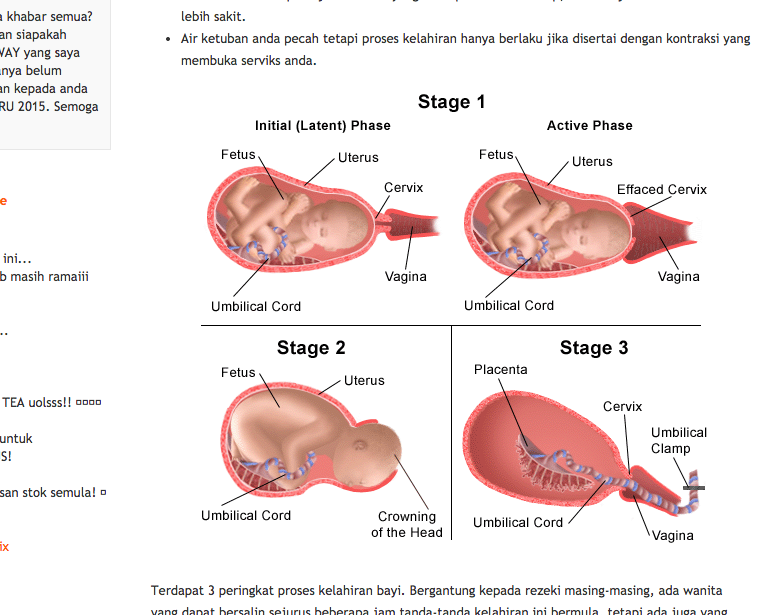
By week seven, the intestines begin to herniate out of the embryo through the umbilical ring and into the umbilical cord.[4][6][2] This physiologic herniation is necessary for proper rotation of the intestines and adequate growth of the fetus to house the expanding intestines.[6] The rapid development of the intestines causes elongation of the umbilical cord.[6] Between weeks ten and twelve, the intestines leave the umbilical cord and return to the abdominal cavity.[4][2][6] During this time, the extraembryonic mesoderm develops a rich extracellular matrix to protect the cord called Wharton’s jelly.[2][7] The umbilical cord continues to elongate during the second trimester with a length comparable to the crown-rump length of the fetus.[1][8] By term, the vitelline duct and allantois have typically completely involuted.[1][5] However, in some cases, remnants of the allantois and vitelline duct can be found in the umbilical cord proximal to the neonate.[2][5] At birth, the cord typically measures an average of 50 to 60 cm in length and 2 cm in diameter with up to 40 helical turns.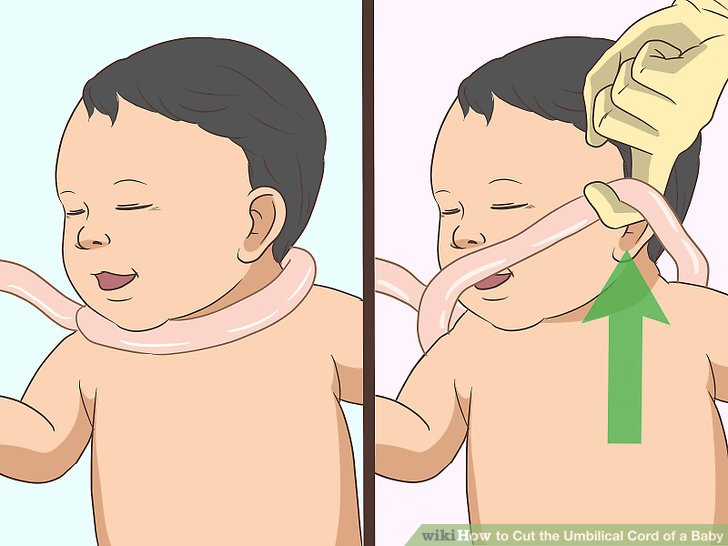 [4][8] After the birth of the neonate, the umbilical cord is clamped and then cut as the neonate now breathes on its own, and the remainder of the umbilical cord is delivered along with the placenta.
[4][8] After the birth of the neonate, the umbilical cord is clamped and then cut as the neonate now breathes on its own, and the remainder of the umbilical cord is delivered along with the placenta.
Cellular
Mesenchymal stem cells found within the Wharton’s jelly of the umbilical cord express c-kit and telomerase activity, consistent with the markers of stem cells.[9][10][11] These cells can be easily extracted after delivery and offer a source of stem cells with fewer ethical considerations than other sources.[7][10] These cells have shown the ability to differentiate into neurons and glia when exposed to specific growth factors.[9] Additionally, these cells may play a role in treating autoimmune disease due to their ability to suppress the secretion of interferon-gamma and transform growth factor-beta1.[10] A more recent study completed on rats showed that transplantation of Wharton’s jelly into the site of traumatic brain injury could reduce the amount of brain damage by reducing brain edema and increasing expression of brain-derived neurotrophic factor.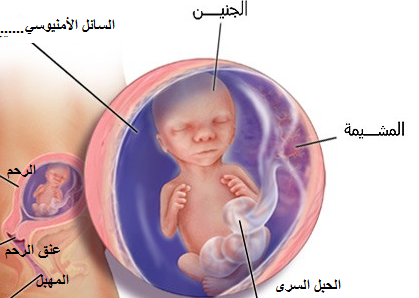 [7] Researchers continue to investigate Wharton’s jelly and mesenchymal stem cells for their potential therapeutic and technological roles.[10][12][13]
[7] Researchers continue to investigate Wharton’s jelly and mesenchymal stem cells for their potential therapeutic and technological roles.[10][12][13]
Biochemical
The Wharton’s jelly of the umbilical cord is a gelatin-like structure rich in proteoglycans, specifically hyaluronic acid and chondroitin sulfate.[11] Hyaluronic acid is present throughout the body in connective and epithelial tissues.[14] It is a disaccharide polymer made of alternating glycosidic bonds between D-glucuronic acid and N-acetyl-D-glucosamine.[14][15] The number of repeats differs between tissues, but hyaluronic acid purified from the umbilical cord is 3,140,000 Da in size.[16] Chondroitin sulfate is a disaccharide consisting of repeats of N-acetylgalactosamine and iduronic acid.[15] Together, these compounds contribute to cellular hydration and the scaffolding of the umbilical cord.[11][15]
Molecular
Wharton’s jelly is the gelatinous extracellular matrix contained within the umbilical cord that serves as protection for the umbilical vessels. [9][17][4] It prevents the umbilical cord from compressing and provides flexibility to allow for fetal movement within the amniotic cavity.[4][17] It originates from the extraembryonic mesoderm and contains proteoglycans, specifically hyaluronic acid and chondroitin sulfate.[11][17][18] As opposed to other tissues in the body, Wharton’s jelly contains no capillaries.[11] When exposed to temperature changes, such as after delivery of the fetus, the structure of Wharton’s jelly collapses, contributing to the physiological clamping of the cord.[19]
[9][17][4] It prevents the umbilical cord from compressing and provides flexibility to allow for fetal movement within the amniotic cavity.[4][17] It originates from the extraembryonic mesoderm and contains proteoglycans, specifically hyaluronic acid and chondroitin sulfate.[11][17][18] As opposed to other tissues in the body, Wharton’s jelly contains no capillaries.[11] When exposed to temperature changes, such as after delivery of the fetus, the structure of Wharton’s jelly collapses, contributing to the physiological clamping of the cord.[19]
Function
The main function of the umbilical cord is to house the umbilical vessels, which circulate blood between the embryo and the placenta. The umbilical arteries and veins are the vital connection carrying blood between the growing fetus and the placenta.[4] Without this connection to the placenta, the fetus would have no way to receive oxygen and other nutrients or filter out carbon dioxide, urea, and other waste products.[4][20] With the expansion of the amniotic cavity and elongation of the umbilical cord, the fetus has ample space for movement and growth. [4][21][17] During this time in utero, Wharton’s jelly protects the umbilical vessels so the fetus can move and turn without compression of its blood supply.[7][17][22]
[4][21][17] During this time in utero, Wharton’s jelly protects the umbilical vessels so the fetus can move and turn without compression of its blood supply.[7][17][22]
Mechanism
The umbilical vein carries fetal blood from the placenta to the fetus, providing the necessary oxygen and nutrients.[4] Normally found at the 12 o'clock position when facing the umbilicus of the fetus, the umbilical vein is recognizable by its thinner wall and larger lumen in comparison to the arteries.[8][23][2] Blood flowing through the umbilical vein enters the fetus through the umbilical ring and passes through ductus venosus before entering the inferior vena cava.[8][23] In return, the two umbilical arteries carry deoxygenated fetal blood containing waste products from the internal iliac arteries back to the placenta.[4][23] The exchange of these materials happens in the intervillous spaces of the placenta between the maternal and fetal blood supplies.[4][20] Wharton's jelly, the gelatin-like extracellular matrix surrounding the umbilical vessels, provides an elastic cushioning resistant to compression and twisting, allowing for continued blood flow with fetal movement. [7][17][21][22][4] There are several hypotheses regarding how the umbilical cord develops its helices, including differential flow through umbilical arteries and twisting of the intestines within the cord. The belief is that adequate coiling contributes to the strength of Wharton's jelly in protecting the umbilical vessels from compression.[4][17]
[7][17][21][22][4] There are several hypotheses regarding how the umbilical cord develops its helices, including differential flow through umbilical arteries and twisting of the intestines within the cord. The belief is that adequate coiling contributes to the strength of Wharton's jelly in protecting the umbilical vessels from compression.[4][17]
After birth, closure of the umbilical arteries initiates by the contraction of circularly arranged smooth muscle within the vascular wall.[19][2] Physiologic closure of the umbilical vein occurs after the umbilical arteries, allowing for prolonged communication and possible transfusion of the remaining placental blood to the neonate.[2][8] The remnants of the umbilical arteries within the neonate become the medial umbilical ligaments, found on the anterior abdominal wall running from the umbilicus inferiorly to the pelvis.[2][19] The remnant of the umbilical vein becomes the ligamentum teres hepatis, which extends superiorly from the umbilicus to connect to the falciform ligament of the liver. [2][8]
[2][8]
Testing
The most useful investigational tool in utero is the ultrasound.[4] It can be useful in the evaluation of fetal anatomy, measuring amniotic fluid levels, watching for fetal movement, and visualizing fetal blood flow. Continuous Doppler ultrasound can visualize the blood flow through the umbilical artery.[4][24][25] This information is then used to create a velocity waveform that can predict the amount of vascular resistance in the placenta.[4] A high placental vascular resistance is associated with intrauterine growth restriction, and the presence of abnormal reverse flow through the umbilical artery can help to determine the need for early delivery.[4][24] When assessing high-risk pregnancies, the evaluation of umbilical artery Doppler velocimetry is utilized to decrease perinatal mortality.[25] Additionally, during high-risk deliveries and in cases of neonatal depression, umbilical cord arterial blood gases should be collected.[23] Umbilical artery pH and gas analysis are the most reliable tests to assess fetal oxygenation and acid-base in the perinatal period directly.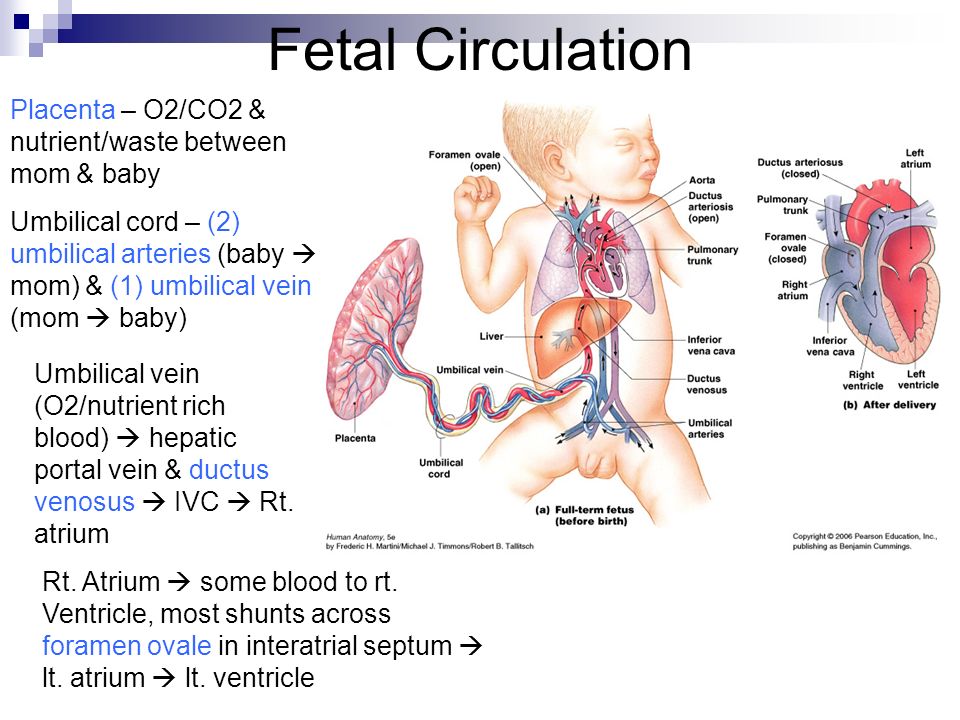 A normal pH and gas analysis at delivery rules out intrapartum asphyxia.[23]
A normal pH and gas analysis at delivery rules out intrapartum asphyxia.[23]
Pathophysiology
A single umbilical artery occurs in less than 1% of all pregnancies due to primary agenesis or secondary atrophy. Over half of these are isolated single umbilical arteries, but the anomaly is also associated with an increased risk of congenital and chromosomal abnormalities. Additionally, a single umbilical artery correlates with prematurity and intrauterine growth restriction.[4][26][27][1][28]
When the umbilical cord inserts near the margin of the placenta instead of the center, it is referred to as marginal cord insertion or battledore placenta; this occurs at a rate of 9% in singleton pregnancies, with an increased rate in twin pregnancies (24 to 33%). Marginal cord insertion is associated with intrauterine growth restriction, preterm labor, and fetal distress.[3][4][28]
Velamentous cord insertion is a type of abnormal insertion occurring in 1 to 2% of pregnancies in which the umbilical vessels begin to spread out before reaching their normal insertion site at the center of the placenta. In this anomaly, the vessels travel separately between the amnion and chorion before reaching the placenta. This area lacks the normal protection by Wharton’s jelly, leaving it susceptible to compression and rupture. Velamentous cord insertion increases the risk of adverse outcomes in the perinatal period due to vasa previa and placental abruption.[3][4][28][29]
In this anomaly, the vessels travel separately between the amnion and chorion before reaching the placenta. This area lacks the normal protection by Wharton’s jelly, leaving it susceptible to compression and rupture. Velamentous cord insertion increases the risk of adverse outcomes in the perinatal period due to vasa previa and placental abruption.[3][4][28][29]
Vasa previa occurs in about 0.04% of pregnancies when fetal vessels are located between the cervix and the fetal presenting part and can result from velamentous cord insertion or vessels traveling between lobes of the placenta. If pregnancy progresses to rupture of membranes, vasa previa presents with the combination of painless vaginal bleeding and fetal heart tones showing signs of distress.[4][29][30][28]
Loss of Wharton’s jelly occurs most commonly near the fetal insertion site but also presents near the placental insertion site. The loss of this protective material leaves the umbilical cord vessels susceptible to compression due to twisting and knotting.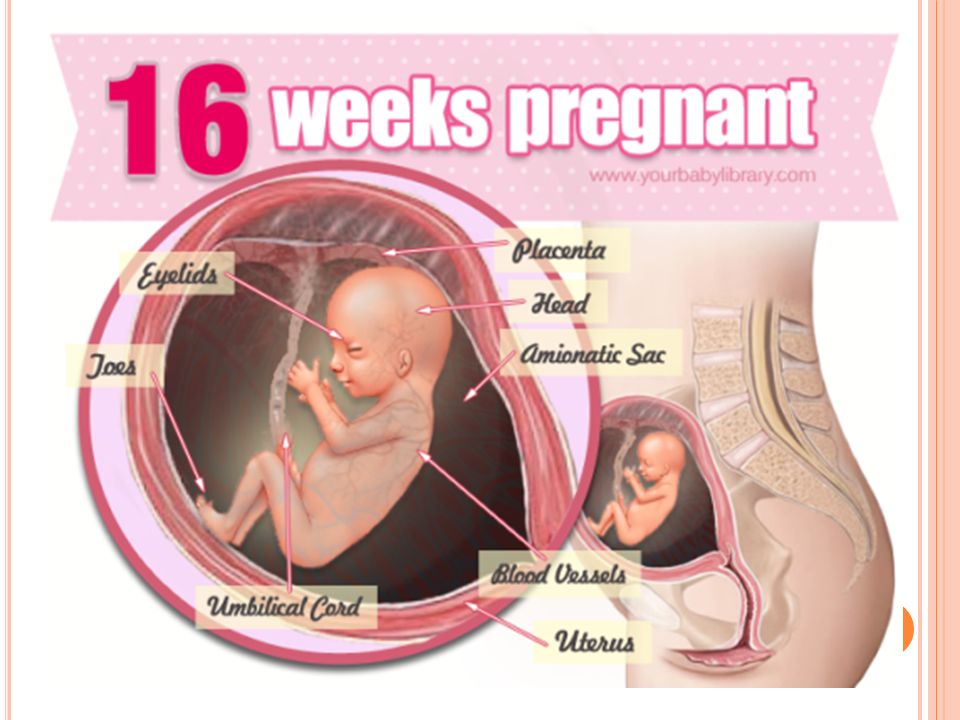 The absence of Wharton’s jelly at any location on the umbilical cord increases the risk of intrauterine fetal demise as well as adverse perinatal outcomes due to compression of vessels during labor. Loss of Wharton’s jelly may be diagnosable before delivery, with a decreased diameter of the umbilical cord visualized by ultrasound.[4][22]
The absence of Wharton’s jelly at any location on the umbilical cord increases the risk of intrauterine fetal demise as well as adverse perinatal outcomes due to compression of vessels during labor. Loss of Wharton’s jelly may be diagnosable before delivery, with a decreased diameter of the umbilical cord visualized by ultrasound.[4][22]
When the vitelline duct fails to regress during the embryonic period completely, it can lead to the formation of an abnormal outpouching of the intestines referred to as a Meckel’s diverticulum. This outpouching persists in about 2% of neonates, usually measures around 2 inches in length, and is typically located in the ileum about 2 feet from the ileocecal valve (following the rule of 2’s). Partial regression of the duct can lead to a vitelline fistula, a fibrous band-like connection between the umbilicus and intestine, or a vitelline cyst, which is an abnormal collection of fluid within the remaining duct. In most cases, these anomalies are asymptomatic, but the abnormal connection is known to increase the risk of internal hernia, volvulus, and intussusception.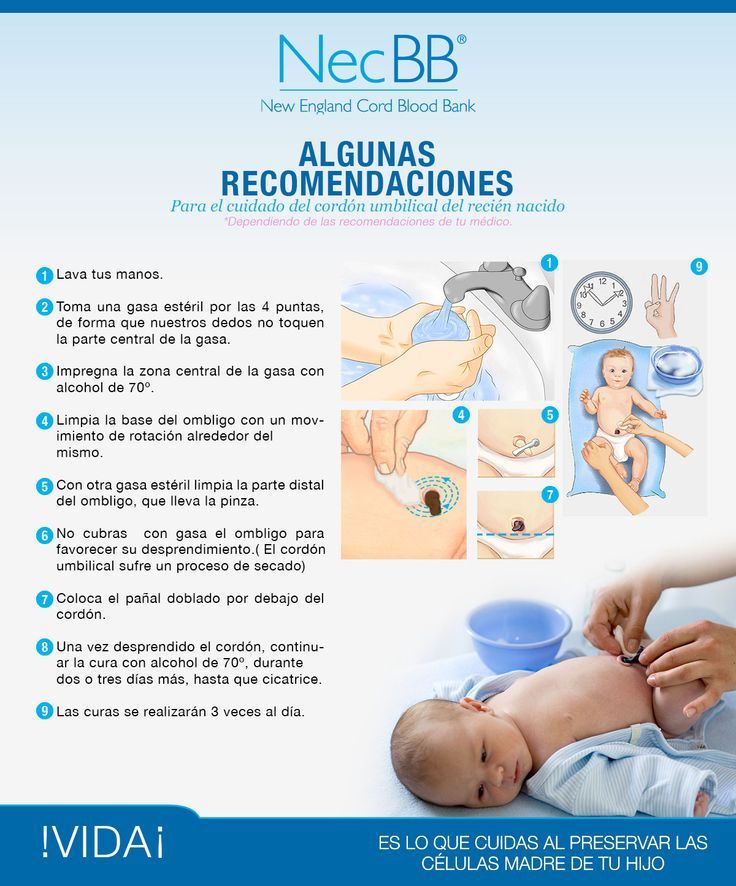 [2][5]
[2][5]
Funisitis is the migration of fetal neutrophils out of the bloodstream and into the umbilical cord. This migration process initiates with the release of neutrophil chemokines, such as interleukin-8 and granulocyte chemotactic protein. Funisitis is most commonly present in the setting of intraamniotic infection, specifically chorioamnionitis, and is part of the fetal inflammatory response syndrome, which indicates a high risk of preterm labor and increased neonatal morbidity. This process is identified microscopically after delivery, but due to the need for mature neutrophils within fetal blood, it is not typically present before 20 weeks of gestation.[31]
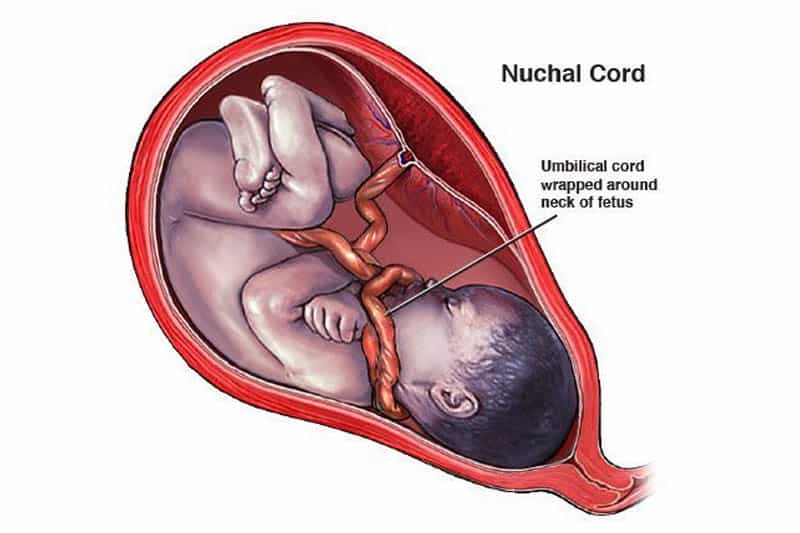
If the umbilical cord becomes too long in utero, there is an increased risk that it can become wound around the fetus or even become tied into a knot due to fetal movement. If the cord becomes wound around the fetal neck, it is referred to as a nuchal cord. The incidence of the nuchal cord is estimated at up to 29% at term, with the incidence increasing relative to gestational age. When the fetus descends during labor, increased torsional forces on the umbilical cord can decrease blood flow through the umbilical vessels and lead to signs of fetal distress and acidosis. When discovered, expedient reduction of the nuchal cord is important to return proper blood flow to the fetus and avoid prolonged asphyxia.[4][17]
When the fetus descends during labor, increased torsional forces on the umbilical cord can decrease blood flow through the umbilical vessels and lead to signs of fetal distress and acidosis. When discovered, expedient reduction of the nuchal cord is important to return proper blood flow to the fetus and avoid prolonged asphyxia.[4][17]
Similarly, knots that form in utero are associated with longer umbilical cords. Loose umbilical knots present no danger to the fetus on their own, but when the knot tightens, the increased compression on the cord initially collapses the thin-walled vein before the thicker-walled arteries. This tightening of the knot can happen in utero and during labor, leading to signs of fetal distress, asphyxia, or even intrauterine fetal demise.[4][17][21]
Additionally, longer umbilical cords are more likely to lie between the cervix and the presenting fetal part during delivery leading to possible umbilical cord prolapse with rupture of membranes. Umbilical cord prolapse is diagnosed by palpation of the umbilical cord within the vagina along with changes in the fetal heart tracing indicating fetal distress, such as recurrent and prolonged decelerations.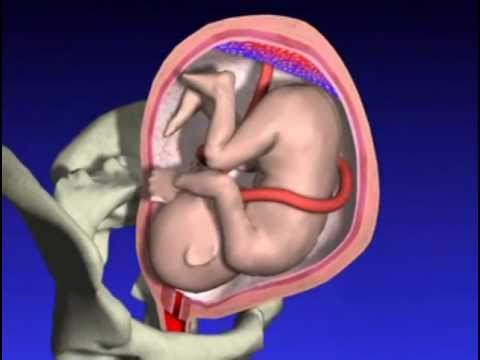 Management of this condition is expedient delivery of the baby, mostly via cesarean section, but operational vaginal delivery may be performed if that is determined to be the faster route.[4][32]
Management of this condition is expedient delivery of the baby, mostly via cesarean section, but operational vaginal delivery may be performed if that is determined to be the faster route.[4][32]
In monochorionic monoamniotic twin gestations, the fetuses share the same amniotic cavity within the uterus leading to possible cord entanglement. Similar to a knotted cord, tightening of the cord entanglement and increasing entanglement can cause compression of fetal vessels leading to intrauterine fetal demise. Cord entanglement can be detected in utero by ultrasound, but studies suggest that prenatal diagnosis has not shown improved neonatal outcomes.[4][28]
Other rare abnormalities include persistent right umbilical vein, umbilical artery aneurysm, umbilical cord cyst, umbilical hemangioma, and umbilical teratoma.[4]
Clinical Significance
The umbilical cord is the vital connection between the fetus and the placenta. Without this connection, the fetus would be unable to receive oxygen and nutrients from the mother or remove carbon dioxide and other waste products. [4] Sonographic analysis of the umbilical cord in the antepartum period is important for the early diagnosis of umbilical abnormalities.[4][2][25] Early recognition of abnormalities, such as velamentous cord insertion and nuchal cord, can improve perinatal outcomes.[4][17][29] Detection of any abnormality early in pregnancy should lead to serial ultrasound examinations to evaluate the patient for any associated complications.[4]
[4] Sonographic analysis of the umbilical cord in the antepartum period is important for the early diagnosis of umbilical abnormalities.[4][2][25] Early recognition of abnormalities, such as velamentous cord insertion and nuchal cord, can improve perinatal outcomes.[4][17][29] Detection of any abnormality early in pregnancy should lead to serial ultrasound examinations to evaluate the patient for any associated complications.[4]
Possible adverse outcomes of umbilical cord abnormalities include intrauterine growth restriction, preterm labor, fetal distress and asphyxia, and even intrauterine fetal demise.[4] After delivery, the portion of the cord remaining attached to the fetus may be useful for intravenous access by umbilical vein catheterization.[2][8] This can be used for transfusions and resuscitation of the neonate while the vessel is still patent, up to 14 days.[8] Additionally, umbilical cord blood has been used as an alternative source for bone marrow transplants since 1988 due to the presence of hematopoietic stem cells. [33] Umbilical cord blood transplantation has successfully helped to cure patients with hematologic diseases through the transplantation of allogeneic hematopoietic stem cells.[33] Furthermore, the therapeutic roles of Wharton’s jelly and the stem cells found within the umbilical cord are still under investigation.[10][12][13]
[33] Umbilical cord blood transplantation has successfully helped to cure patients with hematologic diseases through the transplantation of allogeneic hematopoietic stem cells.[33] Furthermore, the therapeutic roles of Wharton’s jelly and the stem cells found within the umbilical cord are still under investigation.[10][12][13]
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Development of the Fetal membrane and the Placenta, Diagram illustrating a later stage in the development of the umbilical cord, Placental villi, Umbilical cord, Allantois, Heart, Embryo. Contributed by Gray's Anatomy Plates
Figure
Development of the Fetal Membranes and Placenta, Fetus of about eight weeks; enclosed in the amnion, Umbilical cord, Chorionic, Placenta. Contributed by Gray's Anatomy Plates
Figure
Development of Fetal Membranes and Placenta, Fetus in utero; between fifth and sixth months, Umbilical cord, Cervix uteri. Contributed by Gray's Anatomy Plates
Contributed by Gray's Anatomy Plates
Figure
The Branchial Region, Embryo of about six weeks, Umbilical cord, Embryology. Contributed by Gray's Anatomy Plates
Figure
Umbilical cord. Image courtesy S Bhimji MD
References
- 1.
Persutte WH, Hobbins J. Single umbilical artery: a clinical enigma in modern prenatal diagnosis. Ultrasound Obstet Gynecol. 1995 Sep;6(3):216-29. [PubMed: 8521073]
- 2.
Hegazy AA. Anatomy and embryology of umbilicus in newborns: a review and clinical correlations. Front Med. 2016 Sep;10(3):271-7. [PubMed: 27473223]
- 3.
Rathbun KM, Hildebrand JP. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Oct 5, 2022. Placenta Abnormalities. [PubMed: 29083591]
- 4.
Moshiri M, Zaidi SF, Robinson TJ, Bhargava P, Siebert JR, Dubinsky TJ, Katz DS. Comprehensive imaging review of abnormalities of the umbilical cord. Radiographics. 2014 Jan-Feb;34(1):179-96.
 [PubMed: 24428290]
[PubMed: 24428290]- 5.
An J, Zabbo CP. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 26, 2022. Meckel Diverticulum. [PubMed: 29763135]
- 6.
Malone JC, Shah AB. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Feb 10, 2022. Embryology, Midgut. [PubMed: 31985949]
- 7.
Cheng T, Yang B, Li D, Ma S, Tian Y, Qu R, Zhang W, Zhang Y, Hu K, Guan F, Wang J. Wharton's Jelly Transplantation Improves Neurologic Function in a Rat Model of Traumatic Brain Injury. Cell Mol Neurobiol. 2015 Jul;35(5):641-9. [PMC free article: PMC4481175] [PubMed: 25638565]
- 8.
Lewis K, Spirnak PW. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 26, 2022. Umbilical Vein Catheterization. [PubMed: 31751059]
- 9.
Mitchell KE, Weiss ML, Mitchell BM, Martin P, Davis D, Morales L, Helwig B, Beerenstrauch M, Abou-Easa K, Hildreth T, Troyer D, Medicetty S.
 Matrix cells from Wharton's jelly form neurons and glia. Stem Cells. 2003;21(1):50-60. [PubMed: 12529551]
Matrix cells from Wharton's jelly form neurons and glia. Stem Cells. 2003;21(1):50-60. [PubMed: 12529551]- 10.
Zhou C, Yang B, Tian Y, Jiao H, Zheng W, Wang J, Guan F. Immunomodulatory effect of human umbilical cord Wharton's jelly-derived mesenchymal stem cells on lymphocytes. Cell Immunol. 2011;272(1):33-8. [PMC free article: PMC3235326] [PubMed: 22004796]
- 11.
Safari F, Fani N, Eglin D, Alini M, Stoddart MJ, Baghaban Eslaminejad M. Human umbilical cord-derived scaffolds for cartilage tissue engineering. J Biomed Mater Res A. 2019 Aug;107(8):1793-1802. [PubMed: 30983084]
- 12.
Corsello T, Amico G, Corrao S, Anzalone R, Timoneri F, Lo Iacono M, Russo E, Spatola GF, Uzzo ML, Giuffrè M, Caprnda M, Kubatka P, Kruzliak P, Conaldi PG, La Rocca G. Wharton's Jelly Mesenchymal Stromal Cells from Human Umbilical Cord: a Close-up on Immunomodulatory Molecules Featured In Situ and In Vitro. Stem Cell Rev Rep. 2019 Dec;15(6):900-918.
 [PubMed: 31741193]
[PubMed: 31741193]- 13.
Nishida F, Zappa Villar MF, Zanuzzi CN, Sisti MS, Camiña AE, Reggiani PC, Portiansky EL. Intracerebroventricular Delivery of Human Umbilical Cord Mesenchymal Stem Cells as a Promising Therapy for Repairing the Spinal Cord Injury Induced by Kainic Acid. Stem Cell Rev Rep. 2020 Feb;16(1):167-180. [PubMed: 31760626]
- 14.
Walker K, Basehore BM, Goyal A, Zito PM. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 25, 2022. Hyaluronic Acid. [PubMed: 29494047]
- 15.
Casale J, Crane JS. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Mar 27, 2022. Biochemistry, Glycosaminoglycans. [PubMed: 31335015]
- 16.
Saari H, Konttinen YT, Friman C, Sorsa T. Differential effects of reactive oxygen species on native synovial fluid and purified human umbilical cord hyaluronate. Inflammation. 1993 Aug;17(4):403-15. [PubMed: 8406685]
- 17.
Peesay M.
 Nuchal cord and its implications. Matern Health Neonatol Perinatol. 2017;3:28. [PMC free article: PMC5719938] [PubMed: 29234502]
Nuchal cord and its implications. Matern Health Neonatol Perinatol. 2017;3:28. [PMC free article: PMC5719938] [PubMed: 29234502]- 18.
Gupta A, El-Amin SF, Levy HJ, Sze-Tu R, Ibim SE, Maffulli N. Umbilical cord-derived Wharton's jelly for regenerative medicine applications. J Orthop Surg Res. 2020 Feb 13;15(1):49. [PMC free article: PMC7017504] [PubMed: 32054483]
- 19.
Meyer WW, Rumpelt HJ, Yao AC, Lind J. Structure and closure mechanism of the human umbilical artery. Eur J Pediatr. 1978 Jul 19;128(4):247-59. [PubMed: 668732]
- 20.
Kapila V, Chaudhry K. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 25, 2022. Physiology, Placenta. [PubMed: 30855916]
- 21.
Sørnes T. Umbilical cord knots. Acta Obstet Gynecol Scand. 2000 Mar;79(3):157-9. [PubMed: 10716294]
- 22.
Damasceno EB, de Lima PP. Wharton's jelly absence: a possible cause of stillbirth. Autops Case Rep.
 2013 Oct-Dec;3(4):43-47. [PMC free article: PMC5453660] [PubMed: 28584806]
2013 Oct-Dec;3(4):43-47. [PMC free article: PMC5453660] [PubMed: 28584806]- 23.
Thorp JA, Rushing RS. Umbilical cord blood gas analysis. Obstet Gynecol Clin North Am. 1999 Dec;26(4):695-709. [PubMed: 10587963]
- 24.
Fleischer A, Schulman H, Farmakides G, Bracero L, Blattner P, Randolph G. Umbilical artery velocity waveforms and intrauterine growth retardation. Am J Obstet Gynecol. 1985 Feb 15;151(4):502-5. [PubMed: 3976751]
- 25.
Divon MY. Umbilical artery Doppler velocimetry: clinical utility in high-risk pregnancies. Am J Obstet Gynecol. 1996 Jan;174(1 Pt 1):10-4. [PubMed: 8571990]
- 26.
Murphy-Kaulbeck L, Dodds L, Joseph KS, Van den Hof M. Single umbilical artery risk factors and pregnancy outcomes. Obstet Gynecol. 2010 Oct;116(4):843-850. [PubMed: 20859147]
- 27.
Ramesh S, Hariprasath S, Anandan G, Solomon PJ, Vijayakumar V. Single umbilical artery. J Pharm Bioallied Sci. 2015 Apr;7(Suppl 1):S83-4.
 [PMC free article: PMC4439720] [PubMed: 26015760]
[PMC free article: PMC4439720] [PubMed: 26015760]- 28.
Hubinont C, Lewi L, Bernard P, Marbaix E, Debiève F, Jauniaux E. Anomalies of the placenta and umbilical cord in twin gestations. Am J Obstet Gynecol. 2015 Oct;213(4 Suppl):S91-S102. [PubMed: 26428508]
- 29.
Rocha J, Carvalho J, Costa F, Meireles I, do Carmo O. Velamentous cord insertion in a singleton pregnancy: an obscure cause of emergency cesarean-a case report. Case Rep Obstet Gynecol. 2012;2012:308206. [PMC free article: PMC3517836] [PubMed: 23243528]
- 30.
Derbala Y, Grochal F, Jeanty P. Vasa previa. J Prenat Med. 2007 Jan;1(1):2-13. [PMC free article: PMC3309346] [PubMed: 22470817]
- 31.
Kim CJ, Romero R, Chaemsaithong P, Chaiyasit N, Yoon BH, Kim YM. Acute chorioamnionitis and funisitis: definition, pathologic features, and clinical significance. Am J Obstet Gynecol. 2015 Oct;213(4 Suppl):S29-52. [PMC free article: PMC4774647] [PubMed: 26428501]
- 32.
Sayed Ahmed WA, Hamdy MA. Optimal management of umbilical cord prolapse. Int J Womens Health. 2018;10:459-465. [PMC free article: PMC6109652] [PubMed: 30174462]
- 33.
Ballen KK, Gluckman E, Broxmeyer HE. Umbilical cord blood transplantation: the first 25 years and beyond. Blood. 2013 Jul 25;122(4):491-8. [PMC free article: PMC3952633] [PubMed: 23673863]
Umbilical cord: everything you need to know.
06/29/2022
Future parents often know about the umbilical cord (umbilical cord) only that it is clamped after the birth of a child. Meanwhile, the umbilical cord plays an important role in the course of a healthy pregnancy, and the blood and tissues of the umbilical cord are a kind of bio-insurance for the health of your family for many years and even decades in the future.
So, what are the functions of the umbilical cord?
The umbilical cord is a wonderful thread that connects mother and child for 9months of pregnancy.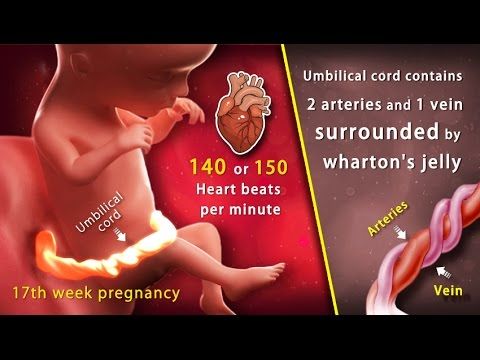 A narrow, tube-like structure, the umbilical cord runs from the belly of the developing embryo to the placenta, delivering oxygen and nutrient-rich blood and removing the baby's waste products. It begins to develop about 5 weeks after conception. As the baby grows, the umbilical cord gets longer and longer, forming a neat coil in the womb, until it reaches its full length (50-60 cm) at about 28 weeks.
A narrow, tube-like structure, the umbilical cord runs from the belly of the developing embryo to the placenta, delivering oxygen and nutrient-rich blood and removing the baby's waste products. It begins to develop about 5 weeks after conception. As the baby grows, the umbilical cord gets longer and longer, forming a neat coil in the womb, until it reaches its full length (50-60 cm) at about 28 weeks.
There are blood vessels inside the umbilical cord: two arteries and one vein. The vessels are located in the thickness of a powerful connective tissue that protects them from possible compression. The vein delivers fresh oxygen and nutrients to the baby through the placenta, which in turn is connected to the mother's bloodstream. The arteries transport the waste products of the child. The path is the same: through the placenta, they enter the mother's bloodstream and are filtered through her kidneys. nine0003
The blood that flows through the umbilical cord is called cord blood. It is a rich source of hematopoietic stem cells. These cells can be harvested and stored for use in more than 80 treatments for diseases including leukemia, lymphomas, metabolic disorders, various anemias, and more.
It is a rich source of hematopoietic stem cells. These cells can be harvested and stored for use in more than 80 treatments for diseases including leukemia, lymphomas, metabolic disorders, various anemias, and more.
The connective tissue that protects the vessels in the umbilical cord is called Wharton's jelly. It is a gelatinous substance composed mainly of collagen. It is Wharton's jelly that allows the umbilical cord to do its job throughout pregnancy, preventing it from contracting or bending. In addition, it is in the connective tissue of the umbilical cord that mesenchymal stem cells (MSCs) are located, which are currently being actively explored as a potential treatment for a wide range of serious diseases. Like cord blood, cord tissue and MSCs can be banked. nine0003
What happens to the umbilical cord after the baby is born?
When a baby is born, the umbilical cord is no longer needed, so it is cut. This process is quick and painless; since the umbilical cord contains no nerves, the baby will not feel anything.
Cords are usually discarded unless the family decides to collect and store cord blood and/or cord tissue from their child. The collection of these biomaterials is quick, easy and low risk, however, the collection needs to be planned in advance for the family: biobanks must be notified of the intention to save blood and tissue, and parents will need to have a cord blood and / or tissue collection kit (most banks recommend purchasing set at least six weeks before the due date). nine0003
CryoCentre LLC works on an all-inclusive basis: when concluding a Contract for stem cell collection, we form and send a set to the maternity hospital specified by the clients. If the place of future birth is not determined, the set is kept at the parents' home in the appropriate conditions determined by the bank.
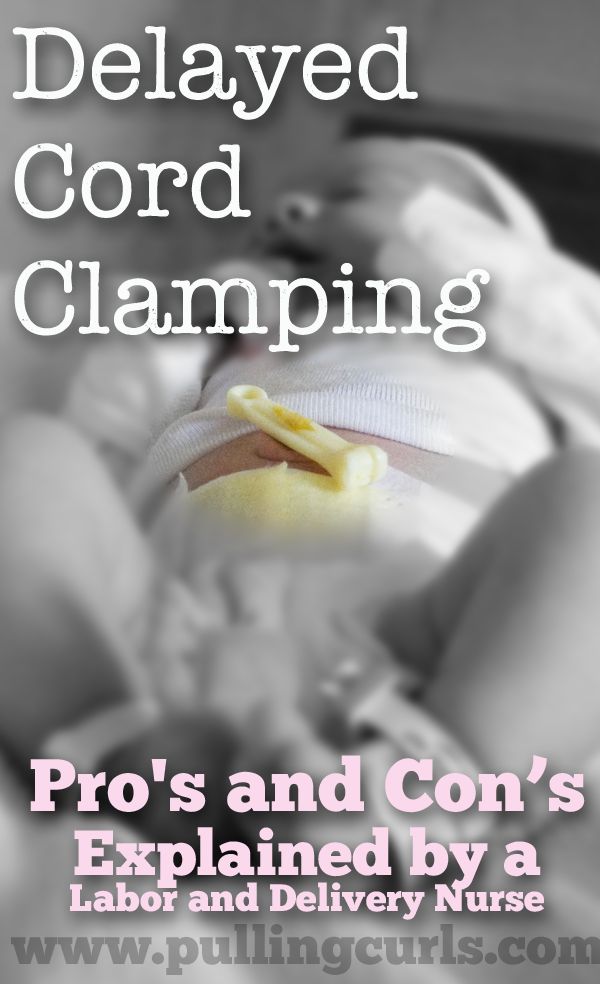
About the pulsation of the umbilical cord.
Delayed cord clamping is 30-60 seconds after the baby is born. This practice is recommended by major medical organizations, including the World Health Organization (WHO). Delayed cord clamping allows more fetal red blood cells from the placenta to pass through the cord into the baby's body, as recommended. This maintains iron stores during the first months of life, reducing the risk of developing iron deficiency anemia. This practice is also believed to promote healthy brain development in the first few years of life. Delayed cord clamping can be performed for both vaginal delivery and caesarean delivery, and is suitable for term and premature babies. It is also fully compatible with newborn cord blood banking. nine0003
Delayed cord clamping allows more fetal red blood cells from the placenta to pass through the cord into the baby's body, as recommended. This maintains iron stores during the first months of life, reducing the risk of developing iron deficiency anemia. This practice is also believed to promote healthy brain development in the first few years of life. Delayed cord clamping can be performed for both vaginal delivery and caesarean delivery, and is suitable for term and premature babies. It is also fully compatible with newborn cord blood banking. nine0003
There is an Indonesian form of childbirth, the so-called "lotus birth". In this case, the umbilical cord is not cut and the baby remains attached to the placenta until two weeks after birth. This practice is not generally accepted and has not been shown to provide any health benefits to infants. The vast majority of medical practitioners advise against doing this, arguing that lotus childbirth is deadly for newborns, as it seriously increases the risk of bacterial infections.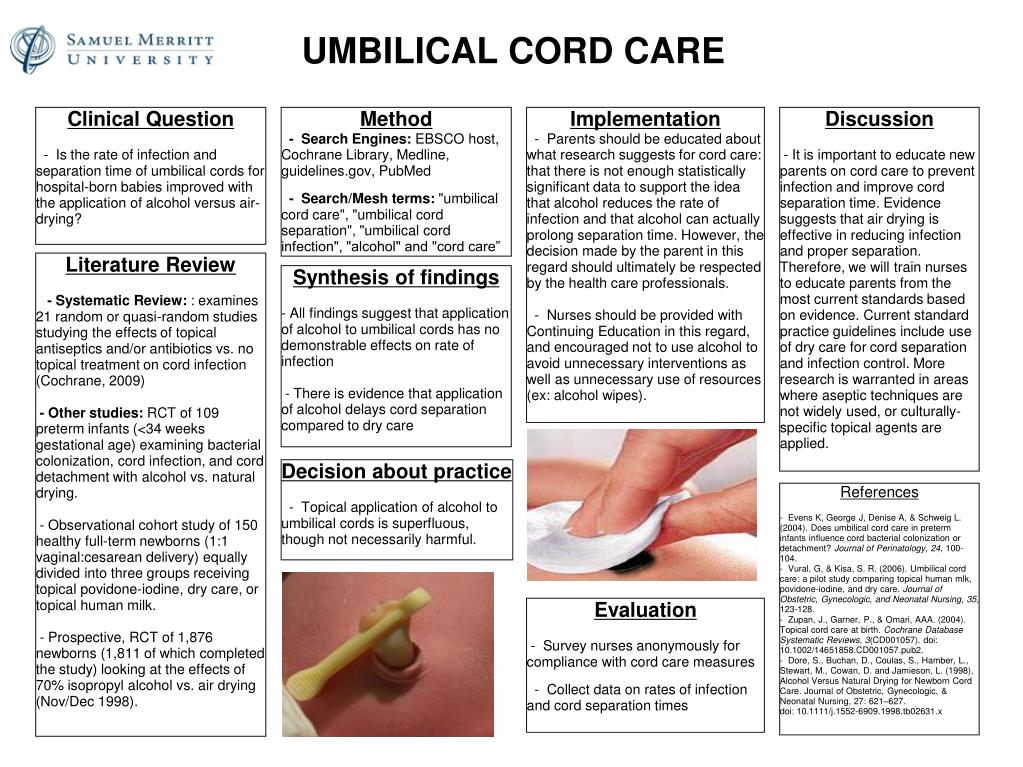 nine0029
nine0029
If you have questions about cord blood and/or cord storage, talk to your doctor, call CryoCentre LLC to make an informed decision for your family's bioinsurance health.
The most important things for expectant mothers to know about the umbilical cord
What can be seen on ultrasonography
The umbilical cord begins to form at the 4th week of pregnancy and is completely formed at the 7th week of pregnancy. During the first state-sponsored screening from the 11th to the 13th week of pregnancy, the placenta is assessed, the number of blood vessels in it is determined, where the placenta is located and how the umbilical cord is attached to it - centrally, at the edge or elsewhere, the place of attachment is assessed of the umbilical cord to the anterior wall of the fetal abdomen - is the umbilical cord pressed into the internal organs of the abdominal cavity (omphalocele), is there any defect in the anterior wall of the fetal abdomen near the place of attachment of the umbilical cord and whether the internal organs protrude outward along it (gastroschisis). It is very important to evaluate the place of attachment of the umbilical cord in twins. The second state-sponsored screening, which takes place between the 20th and 22nd weeks of pregnancy, is assessed for structural changes. nine0003
It is very important to evaluate the place of attachment of the umbilical cord in twins. The second state-sponsored screening, which takes place between the 20th and 22nd weeks of pregnancy, is assessed for structural changes. nine0003
During the first government-sponsored screening from the 11th to 13th week of pregnancy, the umbilical cord is assessed and the number of blood vessels in it is determined, where the placenta is and how the umbilical cord is attached to it.
As the pregnancy progresses, the umbilical cord cannot be traced along its entire length, because some kind of loop may be hidden behind the fetus. In turn, in the third trimester, the doctor may perform an additional examination - Dopplerography, to assess the flow in the umbilical artery, as it indicates the well-being of the fetus. Changes in arterial flow can be observed in cases of fetal growth retardation. If the changes are too great, a decision may be made to allow the pregnancy earlier, as the baby does not have adequate growth conditions in the uterus and it is safer to terminate the pregnancy so that the baby is not harmed.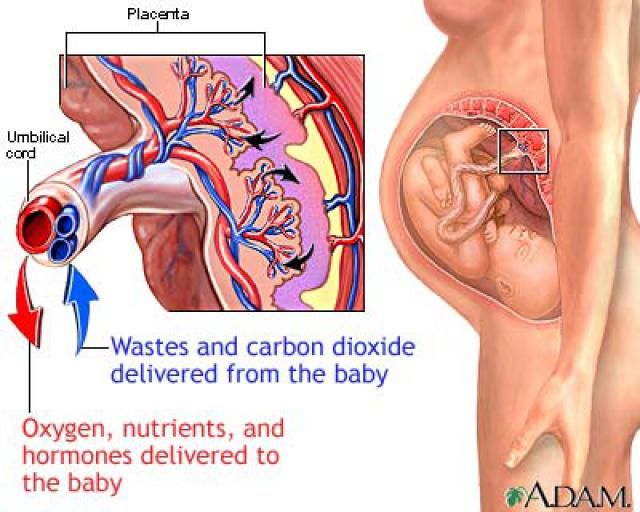 nine0003
nine0003
By evaluating various indicators of the umbilical cord, it is possible to predict the likely developmental problems of the child and, to the extent possible, eliminate them, improving the well-being of the baby in case of pregnancy complications.
Number of blood vessels in the umbilical cord
There are normally three blood vessels in the umbilical cord - one vein, through which nutrients and oxygen are supplied to the child from the placenta, and two arteries that collect metabolic products and fetal processing and transport them to mother's body. nine0003
The umbilical cord may have not three, but two blood vessels - an artery and a vein. This applies to 0.5% of all pregnancies. It can be diagnosed on both the first and second ultrasonographic screening. This is one of the small or soft markers, that is, it additionally draws the doctor's attention to the development of pregnancy and the anatomical structures of the fetus. This does not confirm either a genetic or congenital malformation of the fetus, but the doctor may prescribe additional ultrasonographic studies, and, if necessary, send to an expert doctor to rule out a congenital pathology of the fetus, and also in the third trimester to control the estimated weight of the fetus - does it correspond term of pregnancy. nine0003
nine0003
The baby cannot suffocate in the umbilical cord, because he receives oxygen through the same umbilical cord, and does not inhale through the mouth. The baby begins to breathe through the mouth, taking the first breath.
Although two blood vessels in the umbilical cord are considered pathological, there is no need to worry too much, as the baby can receive nutrients and oxygen from the mother in sufficient quantities.
Umbilical cord length
The average umbilical cord is 50–60 centimeters [1] long and 1.5–2 centimeters in diameter, but can be shorter or longer, up to 100 centimeters. The future mother cannot influence this length in any way, this is determined by genetics, therefore, with each pregnancy, the size of the umbilical cord may be different. nine0003
If the umbilical cord is long, it can wrap around the baby - around the legs, arms, neck or other parts of the body, but even in this situation there is no reason to fear.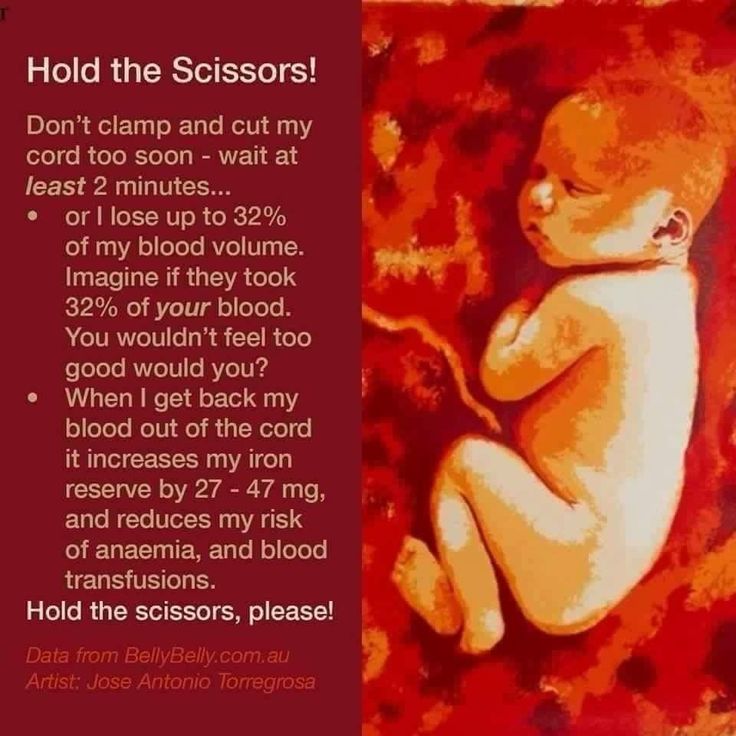 In the same woman, the umbilical cord may be of normal length during one pregnancy, and too short during the next. It has nothing to do with food or physical activity.
In the same woman, the umbilical cord may be of normal length during one pregnancy, and too short during the next. It has nothing to do with food or physical activity.
The baby's umbilical cord is around the neck
Often women, recalling their childbirth, tell with horror that the baby's umbilical cord was wrapped around the neck, which almost strangled him. The child cannot suffocate in the umbilical cord, because he receives oxygen through the same umbilical cord, and does not inhale through the mouth. The baby begins to breathe through the mouth, taking the first breath. If the birth went without complications, it is loud and piercing - the first cry. nine0003
After birth, the baby also does not immediately breathe through the mouth, but continues to receive nutrients and oxygen through the umbilical cord until it is cut.
A quarter of babies are born with the umbilical cord wrapped around the neck or arms, legs, abdomen or other parts of the body.
It must be remembered that the umbilical cord is wrapped around a dynamic process, if the baby's umbilical cord is wrapped, it can also slip and unwind.
If ultrasonography reveals that the umbilical cord is around the neck or other part of the body, then after a few days it may not be there, and in the baby it may be wrapped shortly before delivery. Whether the length, position, or entanglement of the umbilical cord in a woman with a term pregnancy with a cephalic presentation of the fetus will interfere with childbirth is assessed only in the process of childbirth. nine0003
The umbilical cord can also slip off the baby's body during childbirth. Usually the umbilical cord, even if it is twisted, is long enough to allow the baby to freely exit through the birth canal. And during labor pains, it does not shrink easily, because its blood vessels are covered with a dense jelly-like substance.
Advertisement
Advertisement
After the baby was born, the umbilical cord fulfilled its function.
With her cutting, the life of mother and child takes on a new dimension - they are still very connected, but not in a literal sense anymore. nine0003
When the umbilical cord is too short or there are several tight coils around the baby's neck, sometimes during the expulsion period, a slight deviation of the fetal head back between contractions can be observed, there may also be changes in the fetal heart sounds, however, that the umbilical cord is short, it is stated after childbirth. And usually the midwife removes the loop of the umbilical cord from the child's neck so quickly that the mother may not notice this during childbirth.
Since during childbirth the fetus is monitored by recording heart sounds or cardiotocography, noticing changes that may be caused by the location or entanglement of the umbilical cord, the mother will be asked to change her position, the tones will be recorded for a long time. If the baby does not receive enough oxygen and begins to suffer, changes in tones will be significant, and depending on the phase of labor, a decision may be made to allow delivery immediately - to do a caesarean section or instrumental vaginal delivery (with vacuum).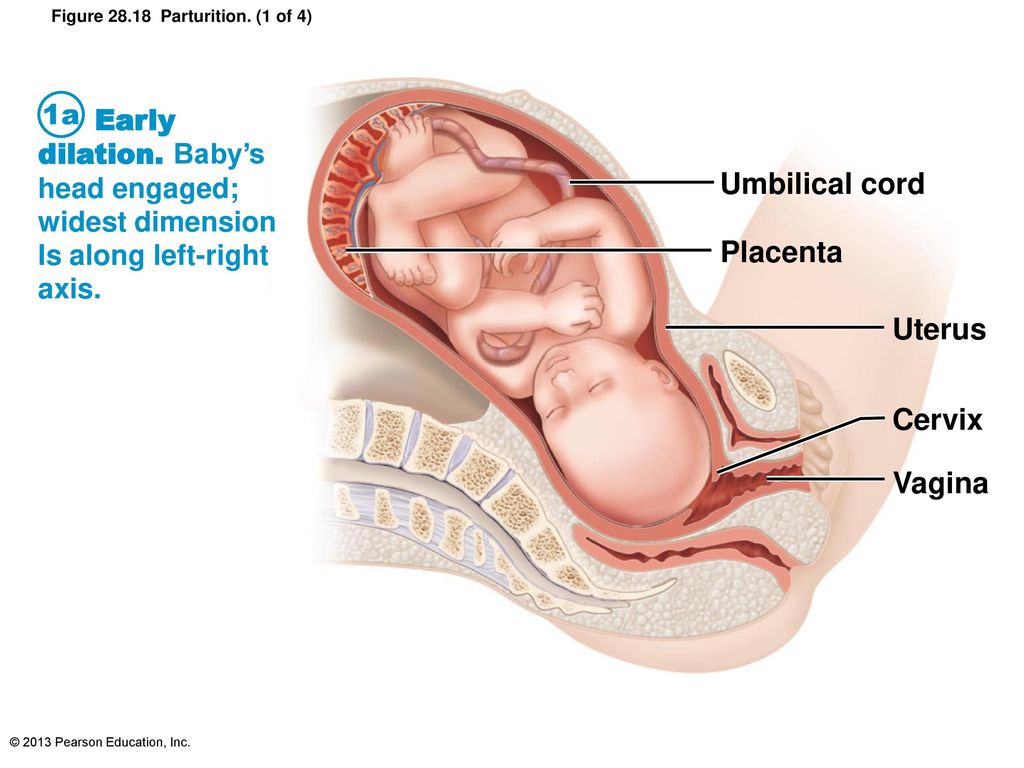 nine0003
nine0003
Knots in the umbilical cord
There are two types of knots - true and false. A false cord knot occurs when the blood vessels in the cord are slightly longer than the cord and "throw a loop" that looks like an extension of the cord. These nodes are normal and do not interfere with the development of the baby. Sometimes the umbilical cord binds into real knots, and then there is reason to be afraid, because with a tight contraction, oxygen delivery to the child is disrupted. With a true node, 0.5% of newborns are born, so these cases are not very common. nine0003
Umbilical cord knots usually form during the first trimester of pregnancy, but no later than the 16th week. Why is this happening? Usually the cause is a very mobile child, as Iveta Berzina, a natural birth midwife, noticed in her practice. Excessive stirring and somersaulting of the fetus in the abdomen can also contribute to mom's stress or too fast-paced lifestyle, so sometimes it's worth living calmer and thinking about the emotions that a pregnant woman experiences while expecting a baby, says the midwife. As long as the nodes are not tightly pulled together, they do no harm, because nutrients and oxygen can freely reach the child through them. nine0003
As long as the nodes are not tightly pulled together, they do no harm, because nutrients and oxygen can freely reach the child through them. nine0003
In turn, gynecologist Laura Ratzene notes that there are also studies that it is movements that contribute to the fact that the umbilical cord is long. “It is not uncommon for women to misunderstand the influence of emotions on pregnancy. Under prolonged conditions of high stress, the mother releases more cortisol than usual, crosses the placenta, and activates the baby's pituitary-adrenal axis. It can affect the development of the baby's brain, low birth weight, reduces pregnancy time. Of course, the baby feels the emotions of the mother through hormonal changes, but this process should not be simplified. nine0003
“While actively working in the delivery room, we do often see mothers who are worried about knots and entanglements. It is important to understand that knots and entanglements are dynamic processes. Whether this will interfere with childbirth can be seen during them. If necessary, they will perform a caesarean section or help the baby to be born faster vaginally so that he does not suffer.
If necessary, they will perform a caesarean section or help the baby to be born faster vaginally so that he does not suffer.
Birth situations are very different. I have attended a vaginal delivery in which the push-out period was slightly longer, the tones were altered accordingly, and the baby was born with five wraps around the neck. And there was a planned caesarean section with four true nodes. Once there was a funny case when the baby had changes in tones during childbirth, the birth did not move forward, a caesarean section was performed, during which it was found that the child grabbed and squeezed the umbilical cord with his hand, ”says the childbirth specialist about his experience. nine0003
Sometimes the umbilical cord is tied into real knots, and then there is reason to be afraid, because when tightly tightened, oxygen delivery to the child is disrupted. With a true knot, 0.5% of newborns are born.
Until the knots are tightened, they are not dangerous, if the opposite happens, then the child dies, because he can no longer receive oxygen or nutrients. As already mentioned, the entire length of the umbilical cord is virtually impossible to examine during ultrasonography because it loops between and behind parts of the fetal body. True umbilical cord knots are rare and can only be seen on ultrasonography if the cord loop containing the knot is located in a part of the uterus that can be visualized on ultrasonography and the knot is floating freely in the amniotic fluid. Much more important than this fact is to find out what is the blood circulation in the umbilical cord, which can be ascertained by doing a Doppler study. nine0003
Should the umbilical cord be cut or pulsated after childbirth?
After the baby was born, the umbilical cord fulfilled its function. With her cutting, the life of mother and child takes on a new dimension - they are still very connected, but not in a literal sense anymore.
At birth, approximately one third of the circulating blood is still in the placenta. When it pulses, blood is pumped from the placenta to the baby. It is recommended to cut the umbilical cord no earlier than 1.5–3 minutes after the birth of the child, since at this time the child receives an additional 80–100 milliliters of blood and thus reduces the risk of developing iron deficiency anemia in the newborn in the first six months after birth. nine0003
If you wait for the umbilical cord pulsation to end completely, then it usually stops after three to five minutes on average, but it can be longer - after 10-15 minutes. In addition, it does not matter whether it was a caesarean section or natural childbirth.
Only in two situations is early (less than one minute) clamping of the umbilical cord recommended - the newborn has severe asphyxia and immediate resuscitation is necessary.
For comparison, it can be mentioned that the loss of 30 milliliters of blood in a newborn equates to the loss of 600 milliliters of blood in an adult. [2]
In turn, allowing the umbilical cord to remain connected to the placenta until it falls off on its own, according to gynecologists and birth specialists at King's College London, there is a serious risk of increased infection for the baby.