Viability at 24 weeks of pregnancy
the long-term impacts of being born extremely early
Scientists are watching out for the health of adults born extremely premature, such as these people who took part in a photography project.Credit: Red Méthot
They told Marcelle Girard her baby was dead.
Back in 1992, Girard, a dentist in Gatineau, Canada, was 26 weeks pregnant and on her honeymoon in the Dominican Republic.
When she started bleeding, physicians at the local clinic assumed the baby had died. But Girard and her husband felt a kick. Only then did the doctors check for a fetal heartbeat and realize the baby was alive.
The couple was medically evacuated by air to Montreal, Canada, then taken to the Sainte-Justine University Hospital Center. Five hours later, Camille Girard-Bock was born, weighing just 920 grams (2 pounds).
Babies born so early are fragile and underdeveloped. Their lungs are particularly delicate: the organs lack the slippery substance, called surfactant, that prevents the airways from collapsing upon exhalation. Fortunately for Girard and her family, Sainte-Justine had recently started giving surfactant, a new treatment at the time, to premature babies.
After three months of intensive care, Girard took her baby home.
Today, Camille Girard-Bock is 27 years old and studying for a PhD in biomedical sciences at the University of Montreal. Working with researchers at Sainte-Justine, she’s addressing the long-term consequences of being born extremely premature — defined, variously, as less than 25–28 weeks in gestational age.
Families often assume they will have grasped the major issues arising from a premature birth once the child reaches school age, by which time any neurodevelopmental problems will have appeared, Girard-Bock says. But that’s not necessarily the case. Her PhD advisers have found that young adults of this population exhibit risk factors for cardiovascular disease — and it may be that more chronic health conditions will show up with time.
Camille Girard-Bock, born at 26 weeks of gestation, is now studying the effects of prematurity for a PhD. Credit: Red Méthot
Credit: Red Méthot
Girard-Bock doesn’t let these risks preoccupy her. “As a survivor of preterm birth, you beat so many odds,” she says. “I guess I have some kind of sense that I’m going to beat those odds also.”
She and other against-the-odds babies are part of a population which is larger now than at any time in history: young adults who are survivors of extreme prematurity. For the first time, researchers can start to understand the long-term consequences of being born so early. Results are pouring out of cohort studies that have been tracking kids since birth, providing data on possible long-term outcomes; other studies are trialling ways to minimize the consequences for health.
These data can help parents make difficult decisions about whether to keep fighting for a baby’s survival. Although many extremely premature infants grow up to lead healthy lives, disability is still a major concern, particularly cognitive deficits and cerebral palsy.
Researchers are working on novel interventions to boost survival and reduce disability in extremely premature newborns. Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Several compounds aimed at improving lung, brain and eye function are in clinical trials, and researchers are exploring parent-support programmes, too.
Researchers are also investigating ways to help adults who were born extremely prematurely to cope with some of the long-term health impacts they might face: trialling exercise regimes to minimize the newly identified risk of cardiovascular disease, for example.
“We are really at the stage of seeing this cohort becoming older,” says neonatologist Jeanie Cheong at the Royal Women’s Hospital in Melbourne, Australia. Cheong is the director of the Victorian Infant Collaborative Study (VICS), which has been following survivors for four decades. “This is an exciting time for us to really make a difference to their health.”
The late twentieth century brought huge changes to neonatal medicine. Lex Doyle, a paediatrician and previous director of VICS, recalls that when he started caring for preterm infants in 1975, very few survived if they were born at under 1,000 grams — a birthweight that corresponds to about 28 weeks’ gestation. The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
The introduction of ventilators, in the 1970s in Australia, helped, but also caused lung injuries, says Doyle, now associate director of research at the Royal Women’s Hospital. In the following decades, doctors began to give corticosteroids to mothers due to deliver early, to help mature the baby’s lungs just before birth. But the biggest difference to survival came in the early 1990s, with surfactant treatment.
“I remember when it arrived,” says Anne Monique Nuyt, a neonatologist at Sainte-Justine and one of Girard-Bock’s advisers. “It was a miracle.” Risk of death for premature infants dropped to 60–73% of what it was before1,2.
Marcelle Girard looks in at baby Camille, born weighing just 920 grams (2 pounds).Credit: Camille Girard-Bock
Today, many hospitals regularly treat, and often save, babies born as early as 22–24 weeks. Survival rates vary depending on location and the kinds of interventions a hospital is able to provide. In the United Kingdom, for example, among babies who are alive at birth and receiving care, 35% born at 22 weeks survive, 38% at 23 weeks, and 60% at 24 weeks3.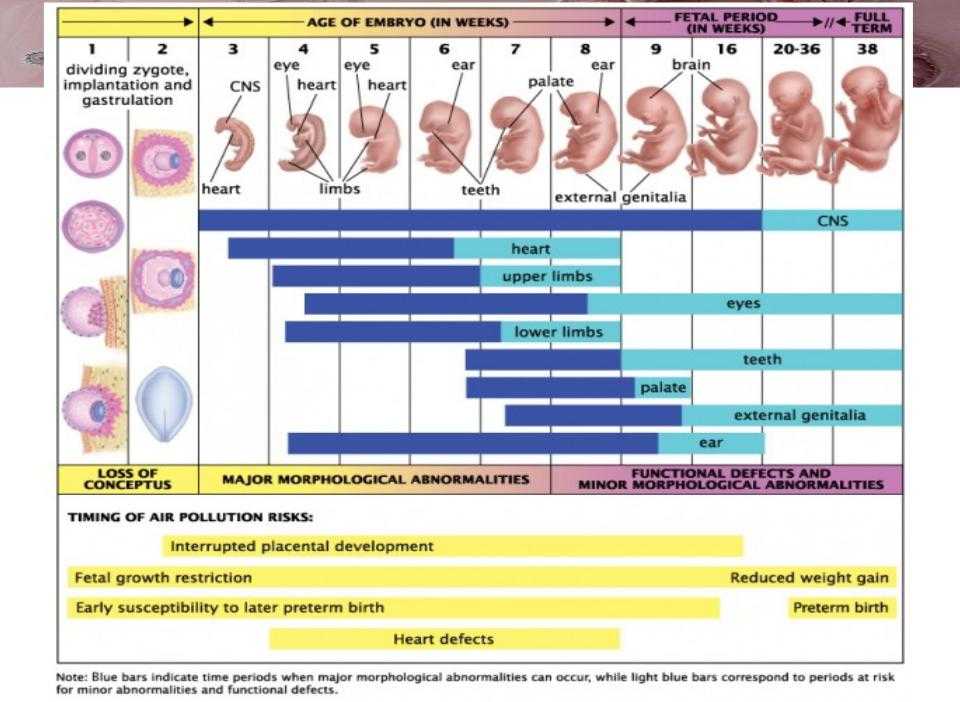
For babies who survive, the earlier they are born, the higher the risk of complications or ongoing disability (see ‘The effects of being early’). There is a long list of potential problems — including asthma, anxiety, autism spectrum disorder, cerebral palsy, epilepsy and cognitive impairment — and about one-third of children born extremely prematurely have one condition on the list, says Mike O’Shea, a neonatologist at the University of North Carolina School of Medicine in Chapel Hill, who co-runs a study tracking children born between 2002 and 2004. In this cohort, another one-third have multiple disabilities, he says, and the rest have none.
“Preterm birth should be thought of as a chronic condition that requires long-term follow-up,” says Casey Crump, a family physician and epidemiologist at the Icahn School of Medicine at Mount Sinai in New York, who notes that when these babies become older children or adults, they don’t usually get special medical attention. “Doctors are not used to seeing them, but they increasingly will. ”
”
What should doctors expect? For a report in the Journal of the American Medical Association last year4, Crump and his colleagues scraped data from the Swedish birth registry. They looked at more than 2.5 million people born from 1973 to 1997, and checked their records for health issues up until the end of 2015.
Source: Ref. 4
Of the 5,391 people born extremely preterm, 78% had at least one condition that manifested in adolescence or early adulthood, such as a psychiatric disorder, compared with 37% of those born full-term. When the researchers looked at predictors of early mortality, such as heart disease, 68% of people born extremely prematurely had at least one such predictor, compared with 18% for full-term births — although these data include people born before surfactant and corticosteroid use were widespread, so it’s unclear if these data reflect outcomes for babies born today. Researchers have found similar trends in a UK cohort study of extremely premature births. In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
In results published earlier this year5, the EPICure study team, led by neonatologist Neil Marlow at University College London, found that 60% of 19-year-olds who were extremely premature were impaired in at least one neuropsychological area, often cognition.
Such disabilities can impact education as well as quality of life. Craig Garfield, a paediatrician at the Northwestern University Feinberg School of Medicine and the Lurie Children’s Hospital of Chicago, Illinois, addressed a basic question about the first formal year of schooling in the United States: “Is your kid ready for kindergarten, or not?”
To answer it, Garfield and his colleagues analysed standardized test scores and teacher assessments on children born in Florida between 1992 and 2002. Of those born at 23 or 24 weeks, 65% were considered ready to start kindergarten at the standard age, 5–6 years old, with the age adjusted to take into account their earlier birth. In comparison, 85.3% of children born full term were kindergarten-ready6.
Despite their tricky start, by the time they reach adolescence, many people born prematurely have a positive outlook. In a 2006 paper7, researchers studying individuals born weighing 1,000 grams or less compared these young adults’ perceptions of their own quality of life with those of peers of normal birthweight — and, to their surprise, found that the scores were comparable. Conversely, a 2018 study8 found that children born at less than 28 weeks did report having a significantly lower quality of life. The children, who did not have major disabilities, scored themselves 6 points lower, out of 100, than a reference population.
As Marlow spent time with his participants and their families, his worries about severe neurological issues diminished. Even when such issues are present, they don’t greatly limit most children and young adults. “They want to know that they are going to live a long life, a happy life,” he says. Most are on track to do so. “The truth is, if you survive at 22 weeks, the majority of survivors do not have a severe, life-limiting disability. ”
”
A nurse uses electroencephalography (EEG) to carry out a check of brain development on a baby born at 25 weeks.Credit: BSIP/Universal Images Group via Getty
BreathlessBut scientists have only just begun to follow people born extremely prematurely into adulthood and then middle age and beyond, where health issues may yet lurk. “I’d like scientists to focus on improving the long-term outcomes as much as the short-term outcomes,” says Tala Alsadik, a 16-year-old high-school student in Jeddah, Saudi Arabia.
When Alsadik’s mother was 25 weeks pregnant and her waters broke, doctors went so far as to hand funeral paperwork to the family before consenting to perform a caesarean section. As a newborn, Alsadik spent three months in the neonatal-intensive-care unit (NICU) with kidney failure, sepsis and respiratory distress.
The complications didn’t end when she went home. The consequences of her prematurity are on display every time she speaks, her voice high and breathy because the ventilator she was put on damaged her vocal cords. When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
When she was 15, her navel unexpectedly began leaking yellow discharge, and she required surgery. It turned out to be caused by materials leftover from when she received nutrients through a navel tube.
The brain, interrupted
That certainly wasn’t something her physicians knew to check for. In fact, doctors don’t often ask if an adolescent or adult patient was born prematurely — but doing so can be revealing.
Charlotte Bolton is a respiratory physician at the University of Nottingham, UK, where she specializes in patients with chronic obstructive pulmonary disease (COPD). People coming into her practice tend to be in their 40s or older, often current or former smokers. But in around 2008, she began to notice a new type of patient being referred to her owing to breathlessness and COPD-like symptoms: 20-something non-smokers.
Quizzing them, Bolton discovered that many had been born before 32 weeks. For more insight, she got in touch with Marlow, who had also become concerned about lung function as the EPICure participants aged. Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Alterations in lung function are a key predictor of cardiovascular disease, the leading cause of death around the world. Clinicians already knew that after extremely premature birth, the lungs often don’t grow to full size. Ventilators, high oxygen levels, inflammation and infection can further damage the immature lungs, leading to low lung function and long-term breathing problems, as Bolton, Marlow and their colleagues showed in a study of 11-year-olds9.
Treatments for premature babies have improved in recent decades, but survival rates vary by age and country.Credit: Mohammed Hamoud/Getty
VICS research backs up the cardiovascular concerns: researchers have observed diminished airflow in 8-year-olds, worsening as they aged10, as well as high blood pressure in young adults11. “We really haven’t found the reason yet,” says Cheong. “That opens up a whole new research area.”
At Sainte-Justine, researchers have also noticed that young adults who were born at 28 weeks or less are at nearly three times the usual risk of having high blood pressure12.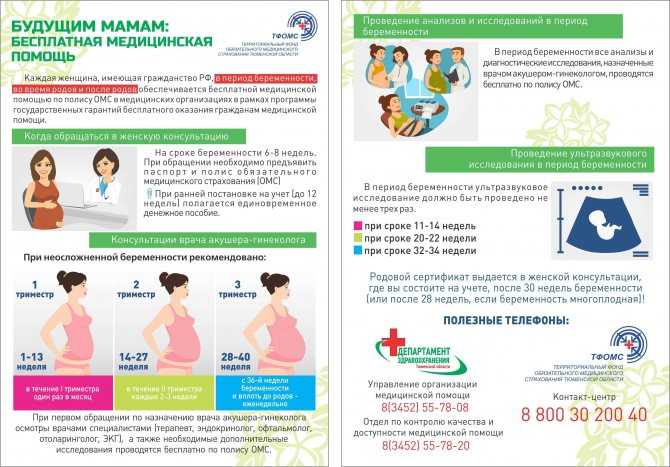 The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The researchers figured they would try medications to control it. But their patient advisory board members had other ideas — they wanted to try lifestyle interventions first.
The scientists were pessimistic as they began a pilot study of a 14-week exercise programme. They thought that the cardiovascular risk factors would be unchangeable. Preliminary results indicate that they were wrong; the young adults are improving with exercise.
Girard-Bock says the data motivate her to eat healthily and stay active. “I’ve been given the chance to stay alive,” she says. “I need to be careful.”
From the startFor babies born prematurely, the first weeks and months of life are still the most treacherous. Dozens of clinical trials are in progress for prematurity and associated complications, some testing different nutritional formulas or improving parental support, and others targeting specific issues that lead to disability later on: underdeveloped lungs, brain bleeds and altered eye development.
For instance, researchers hoping to protect babies’ lungs gave a growth factor called IGF-1 — which the fetus usually gets from its mother during the first two trimesters of pregnancy — to premature babies in a phase II clinical trial reported13 in 2016. Rates of a chronic lung condition that often affects premature babies halved, and babies were somewhat less likely to have a severe brain haemorrhage in their earliest months.
Could baby’s first bacteria take root before birth?
Another concern is visual impairment. Retina development halts prematurely when babies born early begin breathing oxygen. Later it restarts, but preterm babies might then make too much of a growth factor called VEGF, causing over-proliferation of blood vessels in the eye, a disorder known as retinopathy. In a phase III trial announced in 2018, researchers successfully treated 80% of these retinopathy cases with a VEGF-blocking drug called ranibizumab14, and in 2019 the drug was approved in the European Union for use in premature babies.
Some common drugs might also be of use: paracetamol (acetaminophen), for example, lowers levels of biomolecules called prostaglandins, and this seems to encourage a key fetal vein in the lungs to close, preventing fluid from entering the lungs15.
But among the most promising treatment programmes, some neonatologists say, are social interventions to help families after they leave the hospital. For parents, it can be nerve-racking to go it alone after depending on a team of specialists for months, and lack of parental confidence has been linked to parental depression and difficulties with behaviour and social development in their growing children.
At Women & Infants Hospital of Rhode Island in Providence, Betty Vohr is director of the Neonatal Follow-Up Program. There, families are placed in private rooms, instead of sharing a large bay as happens in many NICUs. Once they are ready to leave, a programme called Transition Home Plus helps them to prepare and provides assistance such as regular check-ins by phone and in person in the first few days at home, and a 24/7 helpline.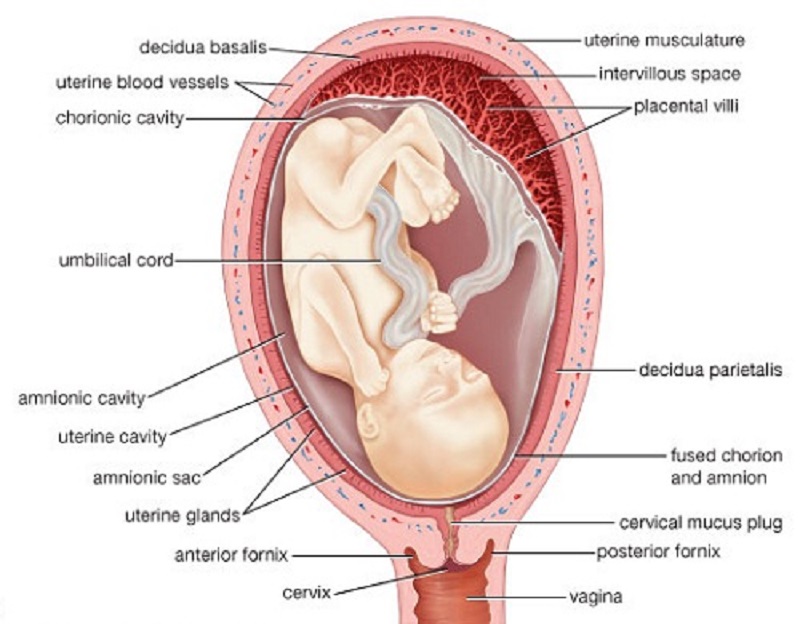 For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
For mothers with postnatal depression, the hospital offers care from psychologists and specialist nurses.
The results have been significant, says Vohr. The single-family rooms resulted in higher milk production by mothers: 30% more at four weeks than for families in more open spaces. At 2 years old, children from the single-family rooms scored higher on cognitive and language tests16. After Transition Home Plus began, babies discharged from the NICU had lower health-care costs and fewer hospital visits — issues that are of great concern for premature infants17. Other NICUs are developing similar programmes, Vohr says.
With these types of novel intervention, and the long-term data that continue to pour out of studies, doctors can make better predictions than ever before about how extremely premature infants will fare. Although these individuals face complications, many will thrive.
Alsadik, for one, intends to be a success story. Despite her difficult start in life, she does well academically, and plans to become a neonatologist. “I, also, want to improve the long-term outcomes of premature birth for other people.”
“I, also, want to improve the long-term outcomes of premature birth for other people.”
Fetal viability by week: What age is the age of viability?
If you've been told you may have to give birth very early, you probably have questions and concerns about your baby being born so young. Most babies can survive outside the womb when they're around 22 to 23 weeks, but it's difficult to pinpoint an exact age.
After that, the chances of survival increase steadily, and babies around 28 weeks generally have a high rate of surviving with little or no long-term health problems. Several things – like your health and the sex of your baby – can also impact when they'll be able to survive outside the womb.
What is fetal viability?
Fetal viability is typically defined as the point when your baby can survive outside the womb. Depending on when your baby is born though, they may need around-the-clock medical care and intervention in order to survive. Viability is a broad-spectrum term that includes the periviable, or premature stages.
When will my baby reach the point of fetal viability?
Unfortunately, fetal viability is not always so clear cut. While fetal viability is generally considered to occur at 24 weeks, some doctors now consider 22 or 23 weeks a potential point of viability, thanks to amazing advances in medical technology that allow some babies to survive at younger gestational ages (gestational age simply means the time your baby was in the womb).
It may be more helpful to look at how the American College of Obstetricians and Gynecologists (ACOG) breaks down survival rates based on premature birth ages, since the rates change dramatically during the late-second trimester and early-third trimester weeks.
- Before 23 weeks, a baby's rate of survival remains low, even with interventions: only 5 to 6 percent.
- At 23 weeks, the rate increases to 23 to 27 percent.
- At 24 weeks, a baby's survival rate reaches 42 to 59 percent.
- By 25 weeks, the survival rate is as high as 67 to 76 percent.

Essentially, the absolute earliest a baby could survive outside the womb is between 22 and 23 weeks, though a baby born this early would require major life-saving interventions. This is still considered the point of fetal viability, however, since a small number of babies can and do survive birth at this stage.
What is a periviable birth?
A periviable birth is one that occurs between 20 and 25 weeks of pregnancy or gestation, or at the limit of viability. Because the 20 to 25-week gestational age includes the earliest point of fetal viability, there will be more complications associated with these births, more potential short- and long-term health risks, and more interventions needed to help a periviable baby survive.
Advertisement | page continues below
There is some overlap here with premature birth, which is usually defined as a birth that occurs before 37 weeks of pregnancy. While many premature babies have a high chance of survival – one that increases with every week they spend in the womb, growing closer to full term – the outcomes for periviable babies are less certain.
For example, the survival rate for babies before 24 weeks is 50 percent, but babies born about one month later, at 28 weeks, have an 80 to 90 percent survival rate. Likewise, the chances of long-term health effects decrease as your baby gets older, gestationally-speaking; about 40 percent of babies born before 24 weeks have long-term health effects, compared to 10 percent of babies born at 28 weeks.
Is there anything I can do to predict if my baby can survive outside the womb?
The closer your baby gets to their due date, the better their chances of surviving and being healthy in the long term. Once your baby reaches 26 weeks, their chances of surviving without serious consequences improve dramatically.
Before 26 weeks, there are many factors that affect your baby's chances of survival and having long-term health problems if they're born very early. These include:
- Maternal age and health
- Having a genetic abnormality, like Down syndrome
- Having complications, such as preeclampsia or placental abruption
- Your baby's sex (girl babies have a higher survival rate than boys)
- Whether your baby is a singleton or multiple (solo babies have a better survival rate)
- Your baby's birth weight
Learn more about the outlook for preemies born at various gestational ages.
Was this article helpful?
Yes
No
24 weeks of pregnancy - what is happening, the development of the fetus, sensations, how the stomach looks like
1 2 3 four five 6 7 8 nine10 eleven 12 13
1st trimester
fourteen 15 sixteen 17 eighteen nineteen20 21 22 23 24 25 26 27 28
2 trimester
29 thirty 31 32 33 34 35 36 37 38 3940 41 42
3rd trimester
WHAT'S HAPPENING
By the end of the 23rd - 24th week of pregnancy, the baby's body is rapidly approaching perfection. His face has acquired characteristic features and looks the way you will see him after childbirth. All organs and systems of the child are actively functioning. The bronchi are fully formed, and the lungs are covered with a film of surfactant (a mixture of surfactants) that will prevent them from drying out. By the 24th week of pregnancy, the sweat and sebaceous glands begin to work in the fetus. nine0003
His face has acquired characteristic features and looks the way you will see him after childbirth. All organs and systems of the child are actively functioning. The bronchi are fully formed, and the lungs are covered with a film of surfactant (a mixture of surfactants) that will prevent them from drying out. By the 24th week of pregnancy, the sweat and sebaceous glands begin to work in the fetus. nine0003
YOUR WELL FEELING
You've put on even more weight and it's getting harder to breathe. At the 24th week of pregnancy, constipation, heartburn, night cramps in the lower extremities, and swelling may still bother you. Because of the large belly, it is difficult for you to move around, it is inconvenient to sleep and lace up your shoes yourself. You may also notice that you get tired quickly. Try to rest during the day, because further this feeling will only intensify.
At 23 to 24 weeks pregnant, many women experience Braxton Hicks training contractions. This is not dangerous at all: with the help of minor muscle contractions, the uterus prepares for the upcoming birth. When you feel contractions, lie down for half an hour and rest. If, after this, muscle contractions continue, moreover, with a certain frequency and the addition of other symptoms, this may be a premature birth. 24 weeks of pregnancy is the period when the baby is not yet ready to be born, so if you experience pain in the back and abdomen, spotting, strong pressure in the pelvis, you should call an ambulance! nine0003
When you feel contractions, lie down for half an hour and rest. If, after this, muscle contractions continue, moreover, with a certain frequency and the addition of other symptoms, this may be a premature birth. 24 weeks of pregnancy is the period when the baby is not yet ready to be born, so if you experience pain in the back and abdomen, spotting, strong pressure in the pelvis, you should call an ambulance! nine0003
Changes in your body can cause various pains. So, for example, at 24 weeks of pregnancy, pain in the back and lower back appears due to a shift in the center of gravity. One of the stages of preparation for childbirth is the “divergence” of the pelvic bones, so you may also feel discomfort in the sacrum.
Many expectant mothers by the 23rd - 24th week of pregnancy face all the troubles associated with hemorrhoids. At the first signs of illness, review your daily diet and include high-fiber foods and foods that have a laxative effect on the menu. Also try not to overcool and rest more often.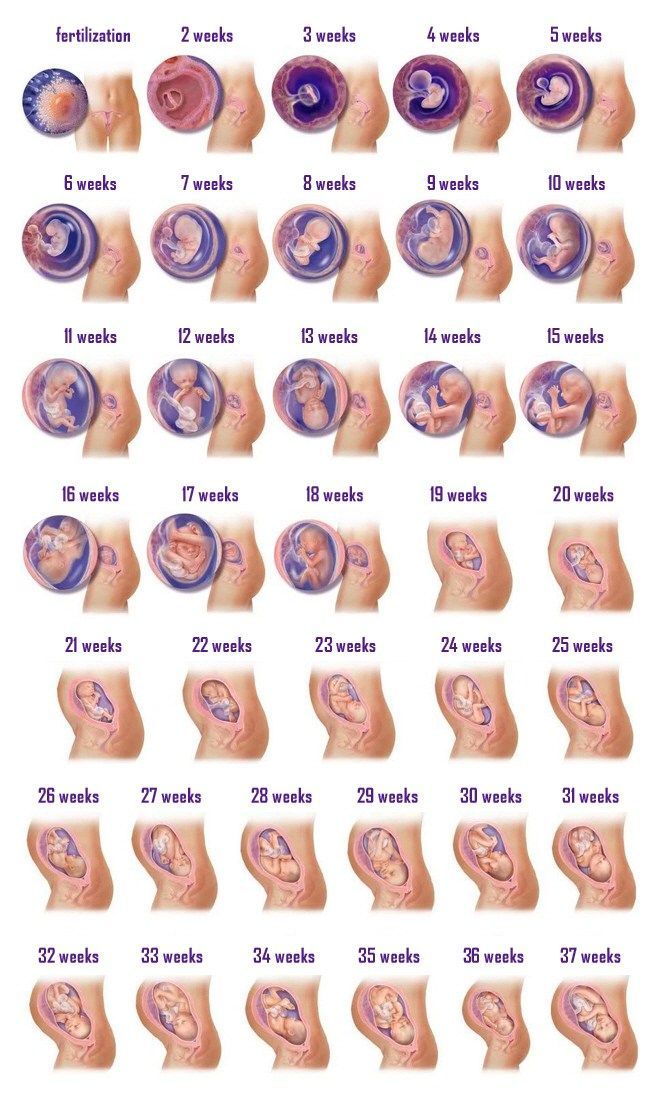 In addition, rectal suppositories can be purchased at the pharmacy, but only after consulting a doctor. nine0003
In addition, rectal suppositories can be purchased at the pharmacy, but only after consulting a doctor. nine0003
RISK FACTORS
One of the dangers of the 24th week of pregnancy is diabetes, so it is very important for the expectant mother to know her blood sugar level. If it has increased slightly, this is considered normal, but its strong increase is a sign of gestational diabetes, which increases the risk of difficult childbirth, provokes overweight in the fetus and can cause a decrease in blood pressure in the newborn.
Premature birth is possible at 24 weeks of gestation. Their onset is accompanied by paroxysmal pains in the abdomen and pelvis, as well as tension and "petrification" of the uterus. At the same time, amniotic fluid may be discharged, sometimes brown mucous discharge or mixed with blood appears. nine0003
Another risk at the 23rd - 24th week of pregnancy is swelling, which can be one of the symptoms of preeclampsia. Outwardly, they are not immediately visible, so you need to carefully monitor your weight, try not to overeat, take vitamins recommended by your doctor, keep drinking and exercise.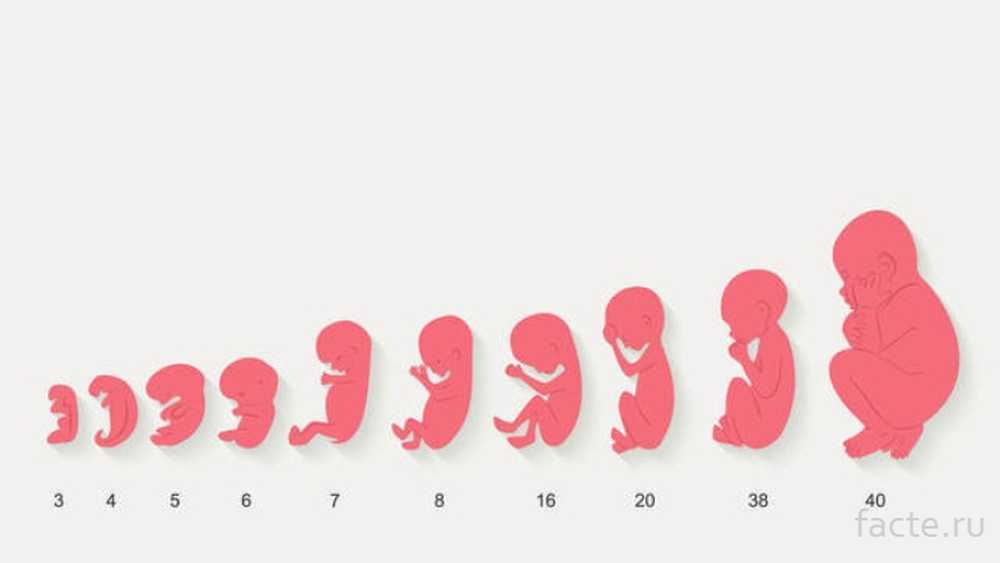
MEDICAL SUPERVISION
Ultrasound examination at the 24th week of pregnancy is rarely done. It is prescribed only according to indications or if a screening ultrasound was missed. During the examination, the doctor determines the position of the fetus in the uterus, evaluates the correct development of the child's organs, the baby's motor activity and heartbeat, the condition and location of the placenta, the amount of amniotic fluid. nine0003
In addition, at 24 weeks of pregnancy, general tests may be prescribed. Typically, such studies are carried out with violations of the health of the expectant mother in order to check the number of red blood cells and white blood cells, sugar levels and the presence of protein in the urine.
RECOMMENDATIONS FOR THE 24TH WEEKS OF PREGNANCY
At the 23rd - 24th week of pregnancy, you need to carefully monitor your health, not only from a medical, but also from a psychological point of view. Try not to get nervous over trifles, because adrenaline attacks can harm the baby. nine0003
nine0003
Now it is very important to keep active: if your health allows, walk more often, go in for swimming, yoga for pregnant women. At 24 weeks of pregnancy, sports for expectant mothers are allowed and even recommended! Systematic fitness classes normalize all the systems of your body, prepare it for the upcoming stresses in childbirth and ensure the successful development of the child. An excellent option is exercises with a fitball (aerobics with a large gymnastic ball): they will help unload the joints and spine, improve blood circulation in the placenta and normalize intestinal motility. nine0003
After 23-24 weeks of pregnancy, women often have trouble sleeping. To have a good rest, be sure to ventilate the bedroom at night. A special pillow for pregnant women will help you get comfortable in bed. A good remedy for night cramps in the legs is a massage with grape seed oil or wheat germ, and chamomile or mint tea with lemon will relieve heartburn.
Pregnancy and childbirth nine0050 Sixth month of pregnancy: changes in the female body and fetal development by week Pregnancy and childbirthEating Right During Pregnancy
How to create a healthy diet for a pregnant woman, what vitamins should be present in the diet, how much liquid should be drunk, what drinks to prefer and what to avoid, what foods are considered harmful for pregnant women and how to keep weight under control while staying in a good mood.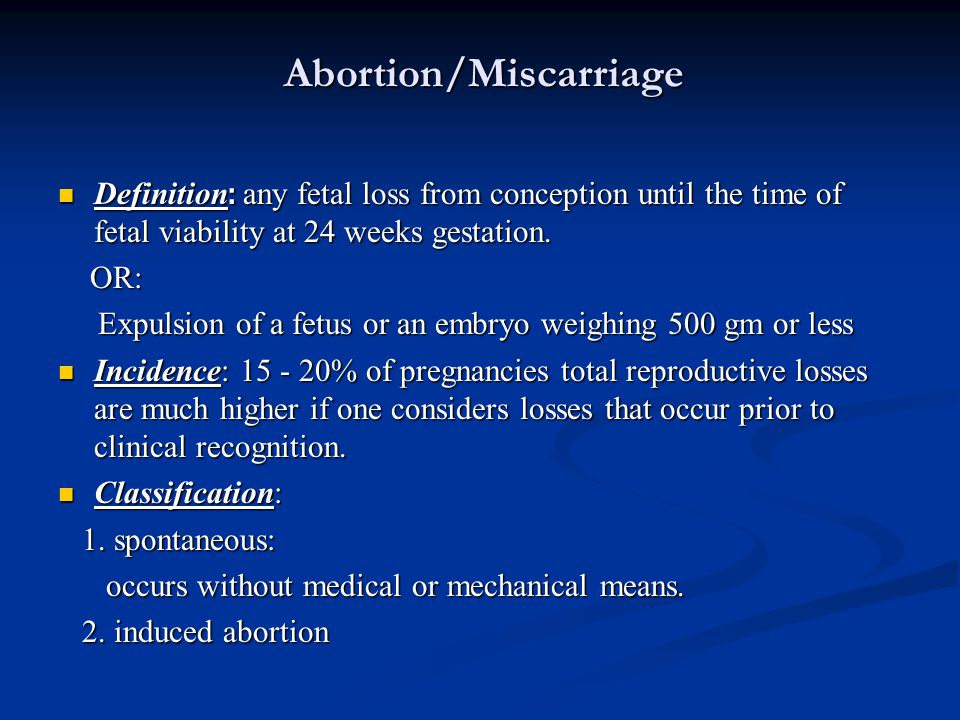 nine0003 Pregnancy and childbirth
nine0003 Pregnancy and childbirth
Tests and examinations during pregnancy
Pregnancy and childbirthHealth and immunity during pregnancy
How does the immunity of a pregnant woman work, how to strengthen it, how to protect the baby from viruses. nine0003 Child nutrition
Vitamins and minerals during pregnancy and breastfeeding
Putting order in our knowledge about what vitamins and minerals and in what quantity are necessary for the health of the child, and what foods contain them.
Pregnancy and childbirth nine0050 Sports during pregnancyWhat is the use of sports during the period of expectation of a baby and which sport to choose?
23 weeks pregnant 25th week of pregnancy
Pregnancy calendar
You are pregnant! Your baby will be born in 40 weeks. What changes will occur in your body, how your baby will grow will tell "Calendar of pregnancy". nine0003
What changes will occur in your body, how your baby will grow will tell "Calendar of pregnancy". nine0003
1-2 weeks
Pregnancy begins at the moment of fertilization or conception.
Fertilization is a complex biological process of the fusion of female and male germ cells (egg and sperm). The resulting cell (zygote) is a new daughter organism.
A mature egg leaves the ovary approximately on the 12-14th day of the menstrual cycle (ovulation) and enters the fallopian tube, where it remains viable for 24 hours. During an orgasm, a man ejects from 200 to 400 million spermatozoa into the woman's vagina. Some of them penetrate through the cervix into the uterine cavity, and from there into the fallopian tubes. Here, spermatozoa retain the ability to fertilize for 48 hours. Thus, within 6-7 days of a woman's menstrual cycle, conception is possible. nine0003
Fertilization of the female egg is performed by a single sperm in the upper part of the fallopian tube.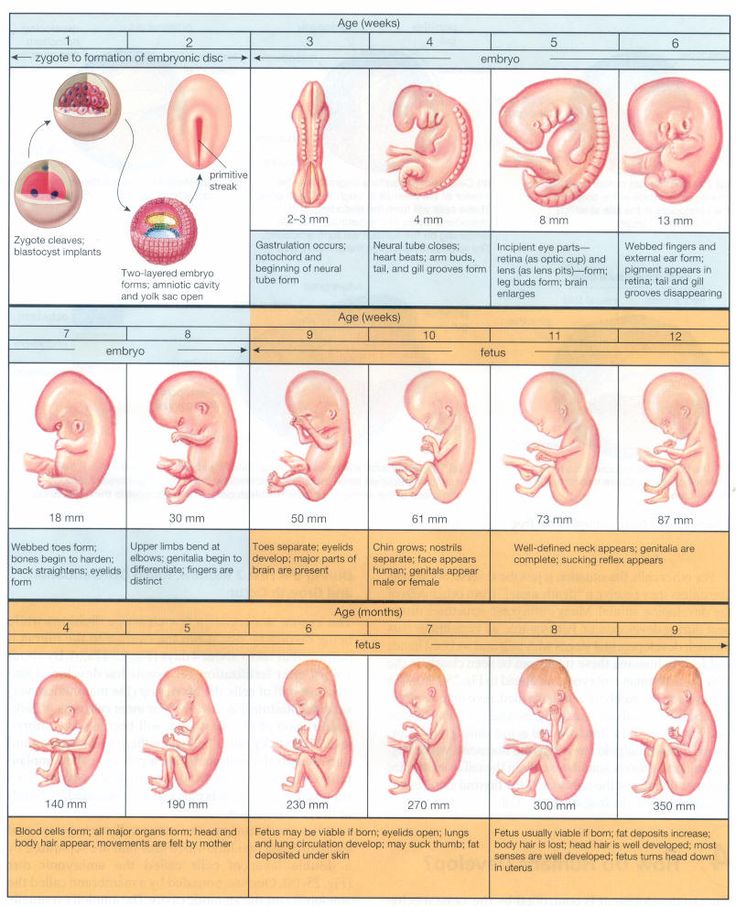 There are two types of sperm: those containing the Y chromosome (“male”) and the X chromosome (“female”). When an egg cell (containing the X chromosome) fuses with a sperm cell, their genetic material is combined and the sex of the child is determined. If there are two X chromosomes in the child's genetic makeup, it's a girl; if an X chromosome and a Y chromosome, it's a boy. It is impossible to change the sex of the child, so you should not follow the "folk beliefs" that guarantee the birth of a child of a given gender. nine0003
There are two types of sperm: those containing the Y chromosome (“male”) and the X chromosome (“female”). When an egg cell (containing the X chromosome) fuses with a sperm cell, their genetic material is combined and the sex of the child is determined. If there are two X chromosomes in the child's genetic makeup, it's a girl; if an X chromosome and a Y chromosome, it's a boy. It is impossible to change the sex of the child, so you should not follow the "folk beliefs" that guarantee the birth of a child of a given gender. nine0003
The fertilized egg begins to divide with the formation of a multicellular organism and move through the fallopian tube into the uterine cavity. During this period, the nutrition of the embryo is carried out at the expense of those substances that have been accumulated in the egg. If the peristalsis of the tube is slowed down (due to inflammatory diseases), the embryo penetrates the wall of the fallopian tube with the occurrence of an ectopic pregnancy.
Implantation (introduction) of the embryo into the uterine wall occurs 7-8 days after fertilization. nine0003
nine0003
On the seventh day of pregnancy, the outer layer of the embryo (trophoblast) begins to produce a hormone - chorionic gonadotropin. This hormone gives the mother's body information that pregnancy has occurred, and begins its functional restructuring. Diagnostic test strips detect the chorionic gonadotropin in the urine of a pregnant woman, which makes it possible to diagnose pregnancy at an early stage.
3-4 weeks
You do not have the expected menstruation, nausea in the morning, and frequent urination during the day. You become emotionally labile, irritable, whiny. Basal body temperature is above 37°C. nine0070 In appearance, your unborn child resembles a small auricle measuring 4 mm, surrounded by a small amount of amniotic fluid. On the 21st day after conception, the brain and spinal cord are formed. By the end of the first month, the circulation of embryonic blood is established, the umbilical cord has formed - the connection of the embryo with the future placenta. The eye sockets, the rudiments of arms and legs appeared, the laying and development of other internal organs of the fetus is underway: the liver, kidneys, urinary tract, and digestive organs. nine0003
The eye sockets, the rudiments of arms and legs appeared, the laying and development of other internal organs of the fetus is underway: the liver, kidneys, urinary tract, and digestive organs. nine0003
5-6 weeks
You no longer doubt that you are pregnant. Regardless of how you feel, all pregnant women need to visit a antenatal clinic and undergo an examination that will allow you to identify and correct existing health problems in time.
Starting from the 5th week, there may be a threat of termination of pregnancy. This will be evidenced by: periodic pain in the lower abdomen and in the lumbar region, a feeling of pressure on the rectum, an increased amount of mucus. If you experience these symptoms, you should consult a doctor. nine0003
By week 6, the face is formed in the embryo: eyes, nose, jaws and limbs.
7-8 weeks
From the 7th week of pregnancy, the yellow body of pregnancy undergoes reverse development, the production of hormones begins to be carried out by the forming placenta.
The baby develops large blood vessels, the heart becomes four-chambered. Bile ducts appear in the liver. There is a development of the endocrine glands, the brain. The auricles are already formed, fingers have appeared on the limbs. The embryo begins to move. At week 8, under the influence of the Y chromosome, the formation of male gonads (testicles) occurs. They begin to produce testosterone - the male sex hormone, which will lead to the formation of the sexual characteristics of the boy. nine0003
9-10 weeks
Your metabolism is changing significantly to provide the growing body with all the necessary "building materials" - amino acids, energy. Disadaptation to such a restructuring can result in toxicosis of the 1st half of pregnancy. It is characterized by nausea, vomiting, salivation, weight loss. When the first symptoms appear, consult a doctor.
At the tenth week, the development of the oral cavity, intestines, rectum, and bile ducts ends in the embryo. The formation of the face and hemispheres of the brain was completed. The development of the cerebellum, the main coordinator of movements, begins. nine0003
The formation of the face and hemispheres of the brain was completed. The development of the cerebellum, the main coordinator of movements, begins. nine0003
11-12 weeks
The body has adapted to the new conditions. By this time, nausea, vomiting, salivation practically disappear. You become balanced, calm.
After 12 weeks, uterine growth becomes noticeable
13-14 weeks
By this time, the formation of the main organs of the unborn child is completed. In appearance, the fetus resembles a small person.
15-16 weeks
A change in skin pigmentation is possible - the midline of the abdomen, nipples and the skin around them have darkened. These phenomena should pass soon after childbirth. nine0070 The formation of the placenta ends. The fetus and placenta represent a single functional system. During this period of pregnancy, the fetus floats freely in the amniotic fluid. The composition of the amniotic fluid can determine the condition of the fetus.
17-18 weeks
These days, your unborn child begins to move. His limbs, ligamentous apparatus, cerebellum have already developed enough. By this time, the formation of the immune system is completed.
19-20 weeks
There have been big changes in your body. The pulse quickened, cardiac output increased significantly (40% higher than the initial level) and the volume of circulating blood (almost 500 ml). nine0003
Due to the increased volume of plasma compared to the mass of red blood cells, hemoglobin decreases in blood tests.
Some women during this period experience frequent and painful urination, pain in the lumbar region on the right or left, weakness. A large uterus presses down on the bladder, the mouth of the ureters, disrupting the outflow of urine. Stagnation of urine and incomplete emptying of the renal pelvis create conditions for the development of infection. Bacteriuria develops and pyelonephritis of pregnant women may occur. If there is any suspicion of pyelonephritis, you should immediately consult a doctor, because this disease is not only dangerous for your health, but also for the further growth and development of the fetus. nine0003
If there is any suspicion of pyelonephritis, you should immediately consult a doctor, because this disease is not only dangerous for your health, but also for the further growth and development of the fetus. nine0003
The weight of the baby is 300-350 grams, he often and quite actively moves, swallows amniotic fluid, begins to open his eyes.
21-22 weeks
In these weeks, the fetus already has a mass of 400-500 grams, and it develops very intensively bones and muscles, which require calcium from your body. Therefore, if you do not want to lose your white-toothed smile, then, on the advice of your obstetrician-gynecologist, start taking calcium supplements regularly. This will help save your teeth and get rid of leg cramps. They appear for the same reason of calcium deficiency. nine0003
23-24 weeks
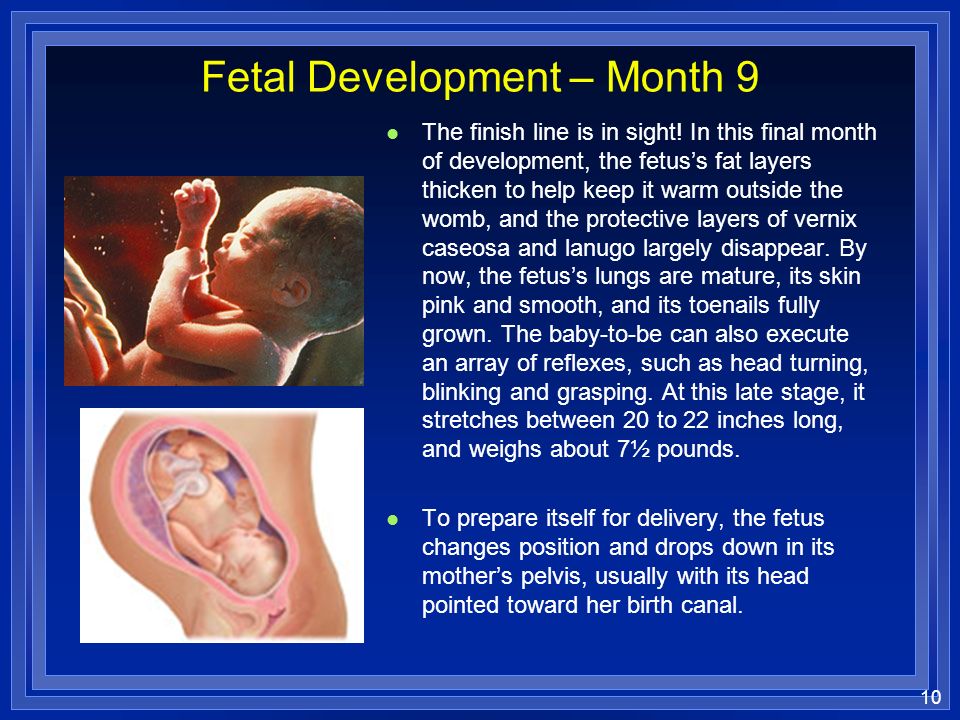
At this time, the weight of the fetus is 500-600 g. It already has all the organs and systems fully formed. Until that time, only his lungs remained immature. And now, by 24 weeks, they begin to ripen. And the cells lining the lung alveoli produce surfactant, a substance that, by lubricating the alveoli, prevents them from sticking together during breathing. However, the amount of surfactant is so small that a child born at this time will not be able to breathe on its own. To survive outside the uterus, he needs sophisticated breathing equipment, incubators, a control system, infusors for nutrition, infusion media, artificial surfactant. nine0003
And now, by 24 weeks, they begin to ripen. And the cells lining the lung alveoli produce surfactant, a substance that, by lubricating the alveoli, prevents them from sticking together during breathing. However, the amount of surfactant is so small that a child born at this time will not be able to breathe on its own. To survive outside the uterus, he needs sophisticated breathing equipment, incubators, a control system, infusors for nutrition, infusion media, artificial surfactant. nine0003
There are perinatal centers where children born during these terms of pregnancy are nursed. It is very difficult. And therefore, the longer the pregnancy is prolonged, the more likely the birth of a healthy and viable child. Therefore, try to do everything so that the child is born on time, full-term and healthy.
By this gestational age, the uterus is at a height of about 24 cm above the pubic bone, and now it not only builds up muscles, but is also stretched by the fetus that completely filled its cavity. nine0003
nine0003
25-26 weeks
The fetus already has a mass of 700-750 g. Due to the improvement of the brain structures in his body, a connection is established with the adrenal cortex and they begin to produce corticoids - hormones necessary for adaptation. The pituitary gland of the fetus reaches such a degree of maturity that the production of adrenocorticotropic hormone begins, which also stimulates hormonal production by the adrenal glands. In short, all forces are thrown to the upcoming "publication". But the most obvious changes in these weeks occur in the lungs - there is an increased maturation of cells that produce surfactant. However, a fetus born during this period can only survive in incubators with artificial lung ventilation, artificial feeding with special infusion media. Therefore, try to keep both him and yourself from rash steps. nine0003
At this time, it's time to start preparing for the future feeding of the child. Under the influence of placental lactogen, your breasts, that is, the mammary glands, are growing rapidly.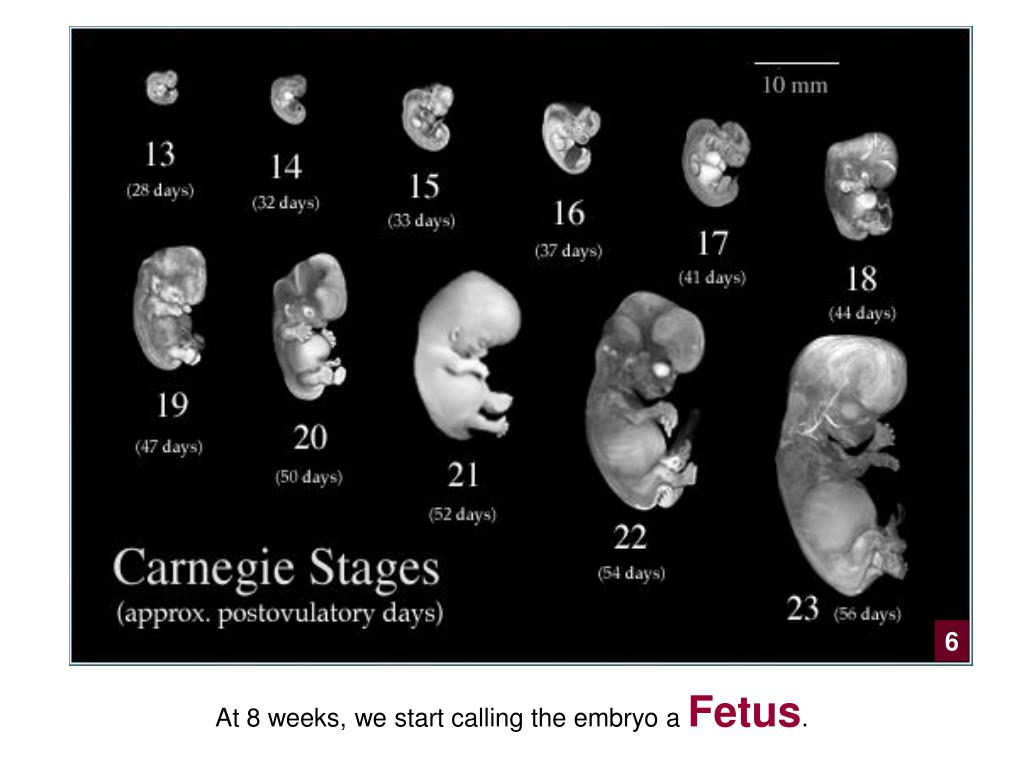 From time to time, droplets of colostrum may appear on the nipples. Daily air baths, washing with cool water, rubbing the nipples with a rough towel will help prepare the nipples for feeding. If the nipples are flat, start to stretch them little by little.
From time to time, droplets of colostrum may appear on the nipples. Daily air baths, washing with cool water, rubbing the nipples with a rough towel will help prepare the nipples for feeding. If the nipples are flat, start to stretch them little by little.
27-28 weeks
This period completes the second trimester of pregnancy. By this time, the fetus weighs up to 1000 g and has a height of up to 35 cm. However, he still cannot live on his own, because. his lungs are not mature enough and special equipment is still needed to nurse him. During these periods of pregnancy, there is an intensive growth of the fetus, the formation of muscles. His movements become more active. Periods of movement alternate with its relatively calm state when the fetus is sleeping. With an ultrasound, you can see that he already knows how to suck his thumb and even smile! nine0003
The fundus of the uterus stands on average at a height of 27-28 cm above the womb.
29-30 weeks
The third trimester of pregnancy begins. The uterus stands at a height of 29-30 cm, it becomes more difficult for you to breathe. Now one of the most serious complications can develop - toxicosis of the second half of pregnancy, which is characterized by the appearance of edema, increased blood pressure and the appearance of protein in the urine. For early diagnosis of this complication, it is necessary to carefully observe an obstetrician-gynecologist and follow all his recommendations, incl. strict weight control. In the III trimester of pregnancy, the daily weight gain should be no more than 50 g, i.e. no more than 300 g per week. You should also monitor the ratio of drunk and secreted fluid. nine0003
The uterus stands at a height of 29-30 cm, it becomes more difficult for you to breathe. Now one of the most serious complications can develop - toxicosis of the second half of pregnancy, which is characterized by the appearance of edema, increased blood pressure and the appearance of protein in the urine. For early diagnosis of this complication, it is necessary to carefully observe an obstetrician-gynecologist and follow all his recommendations, incl. strict weight control. In the III trimester of pregnancy, the daily weight gain should be no more than 50 g, i.e. no more than 300 g per week. You should also monitor the ratio of drunk and secreted fluid. nine0003
31-32 weeks
Have you asked your doctor how the fetus is? Find out now it's very important. Its position can be longitudinal, transverse, oblique. Correct, normal is the longitudinal position of the fetus. Childbirth is safer with cephalic presentation. From this period of pregnancy, it is necessary to wear a prenatal bandage that will support the anterior abdominal wall and help maintain the correct position and presentation of the fetus. If the presentation of the fetus is breech, i.e. above the entrance to the pelvis is the pelvic end of the fetus, then the bandage should not be worn yet. There is gymnastics to correct the presentation of the fetus. nine0003
If the presentation of the fetus is breech, i.e. above the entrance to the pelvis is the pelvic end of the fetus, then the bandage should not be worn yet. There is gymnastics to correct the presentation of the fetus. nine0003
In the morning and evening for 1 hour, do the following: lie down on the bed on your left side and lie quietly for 15 minutes, then turn over to your right side and lie for the next 15 minutes, and then repeat these turns 2 more times.
Pregnant women with Rh-negative blood and with O (I) blood type need blood tests for Rh - or group immune antibodies. Immunization of pregnant women with Rh-negative blood is carried out from 28 weeks and within 72 hours after childbirth according to the indications, which will be discussed by the doctor observing you in the antenatal clinic. nine0003
33-34 weeks
The fetus already has a mass of 1800-2100 g, a height of 40-41 cm. By the end of this period, its lungs will begin to produce surfactant in full and will be able to breathe without special equipment. The fetus is fully developed, its chances of surviving in case of preterm birth are greatly increased. However, there is still extremely little subcutaneous fat, so his skin is thin and has a red color. Such a newborn retains heat very poorly and at birth needs an incubator or a heating pad. His body is still covered with fluff and cheese-like grease, the auricles are still very small, but they are already beginning to straighten out, the boy's testicles descend into the scrotum. nine0003
The fetus is fully developed, its chances of surviving in case of preterm birth are greatly increased. However, there is still extremely little subcutaneous fat, so his skin is thin and has a red color. Such a newborn retains heat very poorly and at birth needs an incubator or a heating pad. His body is still covered with fluff and cheese-like grease, the auricles are still very small, but they are already beginning to straighten out, the boy's testicles descend into the scrotum. nine0003
Caring for a premature baby is the hardest work for the whole family, associated with high material costs, physical overload of parents, and this work is not always rewarded, since a child can be born and remain sick. Therefore, up to 37 weeks of pregnancy, a woman should be especially attentive to her condition and, at the slightest suspicion of an increase in the tone of the uterus, starting frequent and regular contractions, immediately consult a doctor.
Doctors know that women, in anticipation of the arrival of a new person in the house, begin to glue walls and paint ceilings during this period. Don't take unnecessary risks. For this, prenatal leave is provided from 30 weeks, so that you can avoid overwork, do not push in transport, and have the opportunity to sleep. So repairs, stuffy shops, queues are no longer for you. nine0003
Don't take unnecessary risks. For this, prenatal leave is provided from 30 weeks, so that you can avoid overwork, do not push in transport, and have the opportunity to sleep. So repairs, stuffy shops, queues are no longer for you. nine0003
35-36 weeks
The fetus already has a mass of 2100-2700 g and a height of 44-45 cm. It is advisable to see a doctor during this period of pregnancy at least once every 10 days.
37-38 weeks
From this point on, your pregnancy is considered full-term. And if you have a baby in these weeks, he will live. Its development is complete. Now he has a mass of approximately 2700-3000 g. Height is 49-50 cm. The remaining two weeks he will add a little in weight and height.
It becomes easier for you to breathe, as the fetal head is pressed tightly against the entrance to the pelvis, the uterus pulls the anterior abdominal wall more, and therefore its bottom sank lower. Tension of the uterus; small sharp pulling pains in the lumbar region.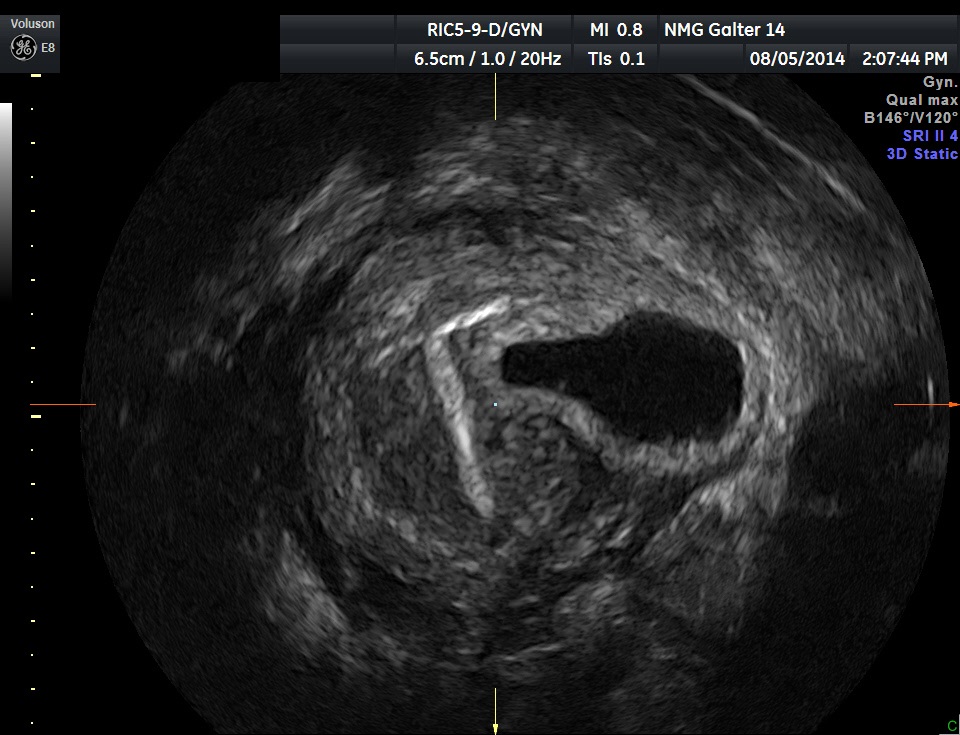 nine0003
nine0003
With an exacerbation of extragenital diseases, the appearance of signs of toxicosis in the second half of pregnancy, with an incorrect position of the fetus, with some gynecological diseases, against which pregnancy develops, a scar on the uterus, etc., early prenatal hospitalization is required. Do not forget to take an exchange card, passport, medical insurance policy and birth certificate to the hospital.
39-40 weeks
You can find out the approximate day of delivery by the date of the last normal menstruation - count back three months and add 7 days. The resulting number will be the estimated date of birth. More precisely, according to many parameters, ultrasound data, additional studies, the date of the first fetal movement, the date of the first visit to the obstetrician-gynecologist, especially if the visit was before 11-12 weeks of pregnancy. nine0003
The child already has all the signs of maturity. His weight is more than 3000 g, and his height is more than 50 cm, he has fair skin, a sufficient amount of subcutaneous fat, he retains heat and does not need special heating.