Umbilical cord connected to mother
Anatomy, Abdomen and Pelvis, Umbilical Cord - StatPearls
Introduction
The umbilical cord is considered both the physical and emotional attachment between mother and fetus. This structure allows for the transfer of oxygen and nutrients from the maternal circulation into fetal circulation while simultaneously removing waste products from fetal circulation to be eliminated maternally. On the other hand, mothers associate an emotional connection to the fetus through the cord. It may merit consideration as the route of love and care during pregnancy. Thus, some poets call it the string of life.
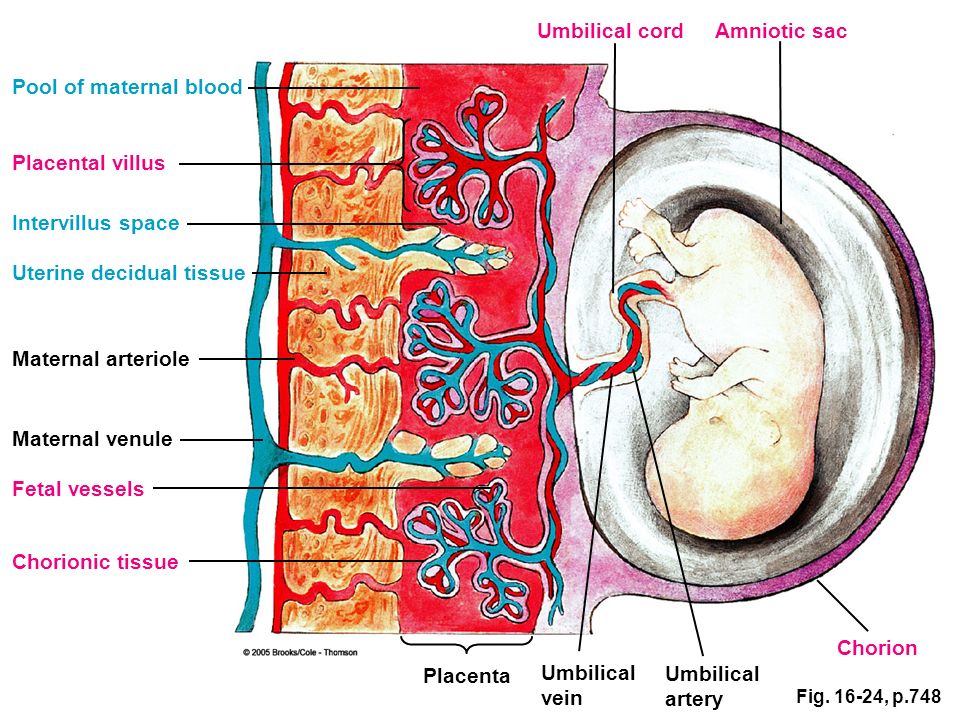
The umbilical cord is a bundle of blood vessels that develops during the early stages of embryological development. It is enclosed inside a tubular sheath of amnion and consists of two paired umbilical arteries and one umbilical vein. During development, the umbilical arteries have a vital function of carrying deoxygenated blood away from the fetus to the placenta.[1] However, after birth, a significant distal portion of the umbilical artery degenerates. These remnants later obliterate, forming the medial umbilical ligament.[2] At the same time, the proximal portion of each umbilical artery serves as a branching point for the development of the anterior internal iliac arteries. The internal iliac arteries later give rise to the superior vesical arteries that supply the urinary bladder and ureters as well as the ductus deferens and seminal vesicles in males.[3][4] The umbilical cord is a vital structure for the entire period of development since it functions to tether the fetus to the placenta and the uterine wall while also acting as the primary route to enable blood to circulate between the fetus and placenta.[5]
Structure and Function
Anatomical Features of an Umbilical Cord
The umbilical cord is a soft, tortuous cord with a smooth outer covering of amnion. It extends from the umbilicus of the fetus to the center of the placenta. Its length ranges from 50 cm to 60 cm, with a diameter of about 1 cm.[6] The umbilical cord is composed of a gelatinous ground substance called Wharton's jelly or substantia gelatinea funiculi umbilicalis.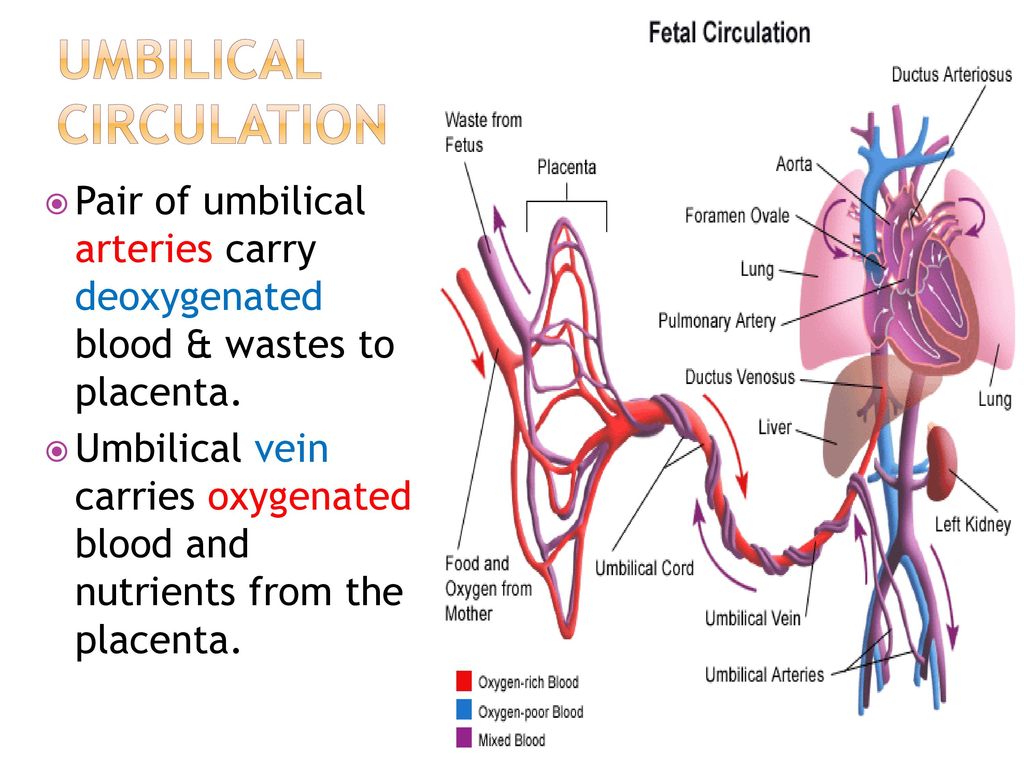 It is composed of mucopolysaccharides from the conjugation of hyaluronic acid and chondroitin sulfate. As previously mentioned, three vessels comprise the umbilical cord: two umbilical arteries and one umbilical vein. It also encloses the urachus (a remnant of allantois).[7] The urachus is a fibrous remnant of the allantois that extends through the umbilical cord and is located in the space of Retzius between the peritoneum posteriorly and the transverse fascia anteriorly. The urachus serves as a drainage canal for the urinary bladder of the fetus.[8]
It is composed of mucopolysaccharides from the conjugation of hyaluronic acid and chondroitin sulfate. As previously mentioned, three vessels comprise the umbilical cord: two umbilical arteries and one umbilical vein. It also encloses the urachus (a remnant of allantois).[7] The urachus is a fibrous remnant of the allantois that extends through the umbilical cord and is located in the space of Retzius between the peritoneum posteriorly and the transverse fascia anteriorly. The urachus serves as a drainage canal for the urinary bladder of the fetus.[8]
Function
The umbilical arteries carry deoxygenated blood from fetal circulation to the placenta. The two umbilical arteries converge together about at 5 mm from the insertion of the cord, forming a type of vascular connection called the Hyrtl's anastomosis.[9] The primary function of Hartl's anastomosis is to equalize blood flow and pressure between the umbilical and placental arteries.[10] As the arteries enter the placenta, each bifurcates into smaller branches called the chorionic vessels.
Embryology
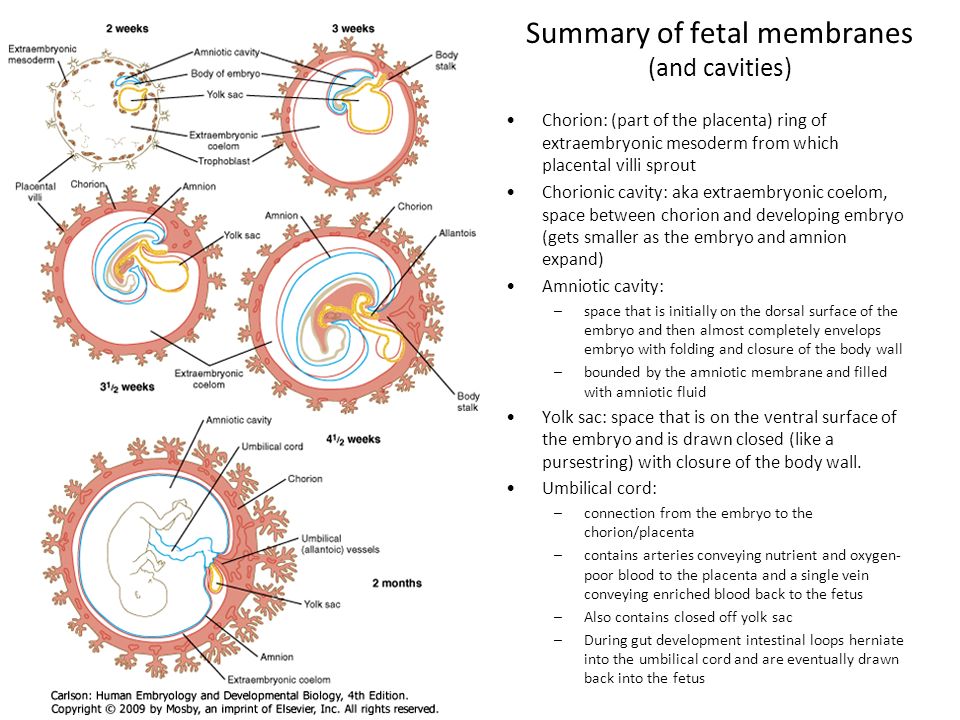
During the early stages of embryonic development, gastrulation occurs and differentiates germinal tissues into three distinct layers: outer ectoderm, intra-embryonic mesoderm, and inner endoderm.[11] The formation of the umbilical cord occurs over three stages and coincides with the gastrulation process.
I. Formation of the Primitive Umbilical Ring
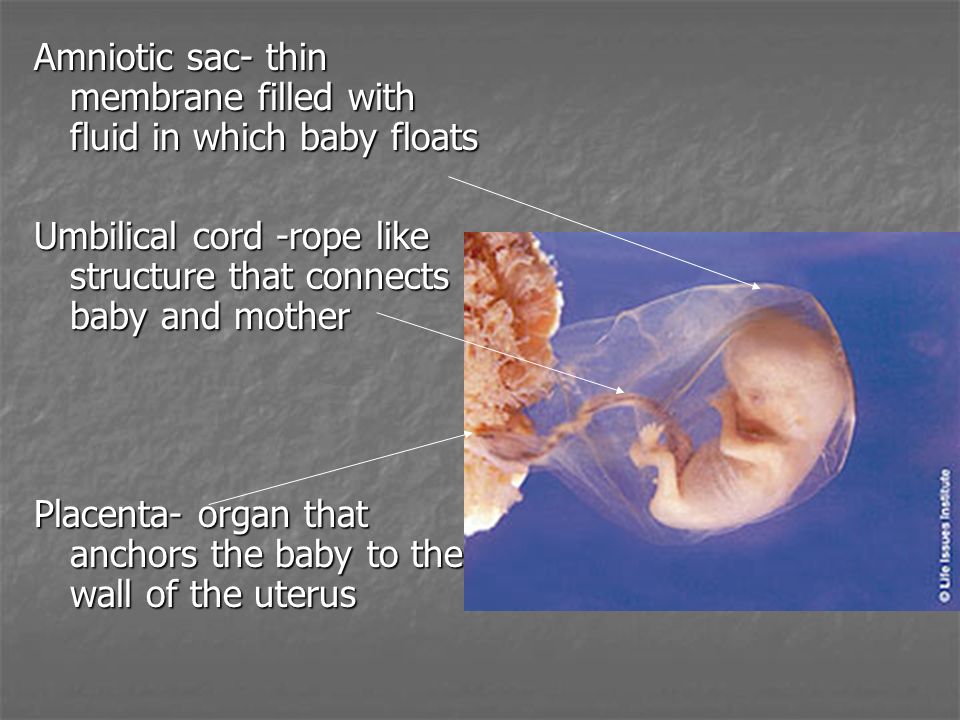
This developmental stage happens together with the folding of the embryonic disc. During this stage, the embryonic disc bulges into the amniotic cavity as a result of folding. At the same time, the amnio-ectodermal junction, which is the tight connection between the embryonic amnion and the ectodermal layer, becomes the ventral aspect of the embryo. Then, the line of reflection between the amnion and the ectoderm acquires an oval outline called the primitive umbilical ring.
II. Formation of the Primitive Umbilical Cord
This stage of development starts in the fifth week of pregnancy, during which the primitive umbilical ring constricts to form a tubular sheath.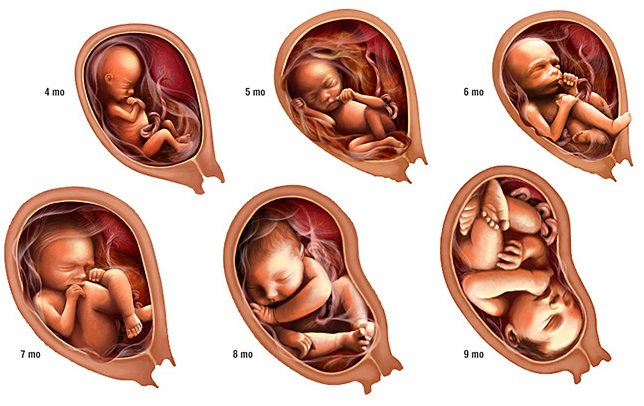 The tubular sheath is called the primitive umbilical cord. It encloses the body stalk, the yolk sac, and its vessels, as well as a part of the allantois.
The tubular sheath is called the primitive umbilical cord. It encloses the body stalk, the yolk sac, and its vessels, as well as a part of the allantois.
III. Formation of the Definitive Umbilical Cord
During this stage, the umbilical cord elongates, and its fundamental structures undergo primary changes. For instance, The extraembryonic mesoderm of the body stalk starts to differentiate into a mucoid substance called Wharton's jelly. Wharton's jelly develops gradually and forms the main bulk of the umbilical cord. The remnants of the extraembryonic coelom inside the umbilical cord progressively degenerate. The yolk sac becomes obliterated together with the vitellointestinal duct that connects the yolk sac with the midgut. Similarly, the distal part of the allantois becomes obliterated. However, the allantoic vessels persist and elongate to form the umbilical vessels. Finally, during the sixth week, a part of the midgut loop enters the umbilical cord developing a physiological hernia.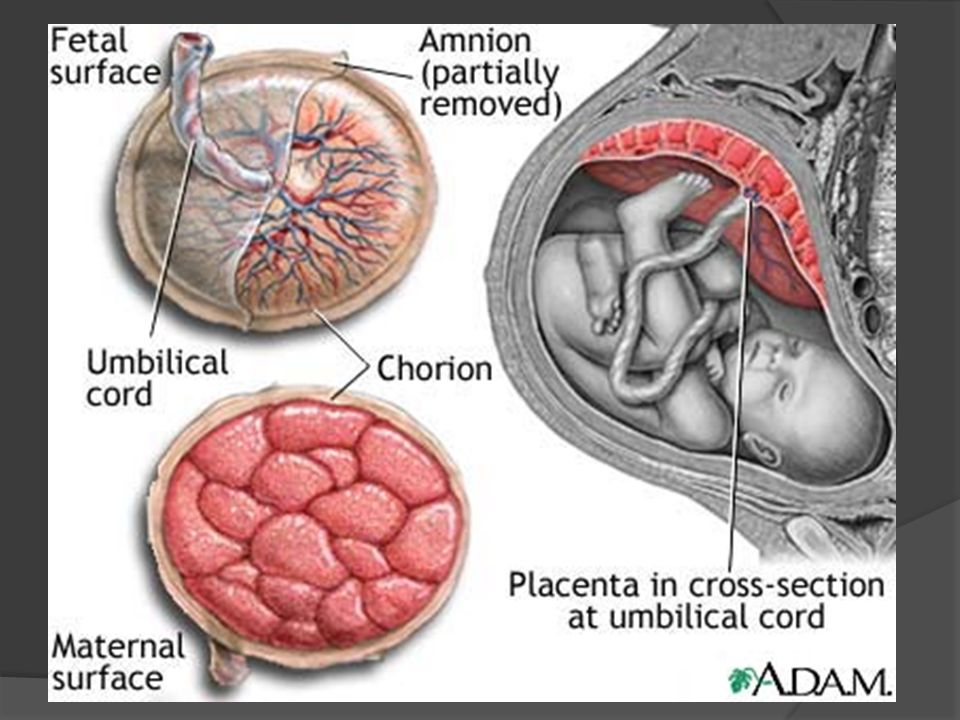 That physiological hernia is usually corrected when that part of the midgut returns to the abdominal cavity after the tenth week of pregnancy.[12]
That physiological hernia is usually corrected when that part of the midgut returns to the abdominal cavity after the tenth week of pregnancy.[12]
Blood Supply and Lymphatics
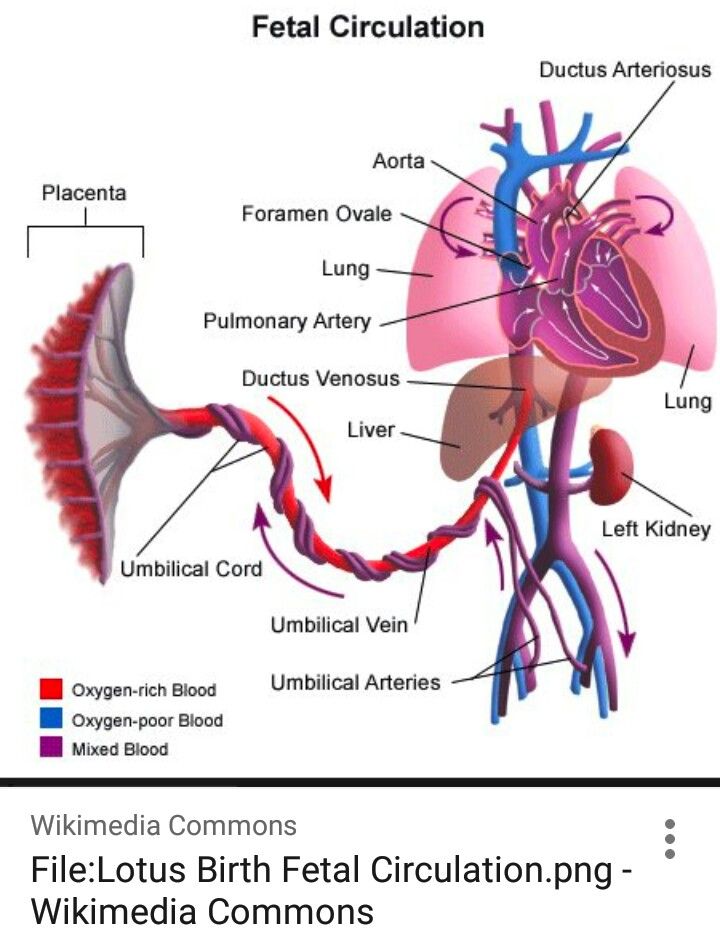
The umbilical cord, together with the placenta, contributes to the flow and regulation of fetal circulation. The two umbilical arteries arise from the internal iliac arteries of the fetus and enter the umbilical cord before further branching at the level of the placenta. At the placental level, each umbilical artery bifurcates into smaller arterioles that continue to branch further to distribute blood to the chorionic villi. The capillaries of the villi fuse to form venules that converge to form the umbilical vein. The umbilical vein carries oxygenated blood and nutrients from the mother to the fetus.[13]
As fetal growth ensues, both placental intervillous circulation and umbilical circulation develop gradually, until maturation is complete at the end of the first trimester. At midgestation, the percentage of umbilical blood in fetal circulation is about 30% of the fetal cardiac output.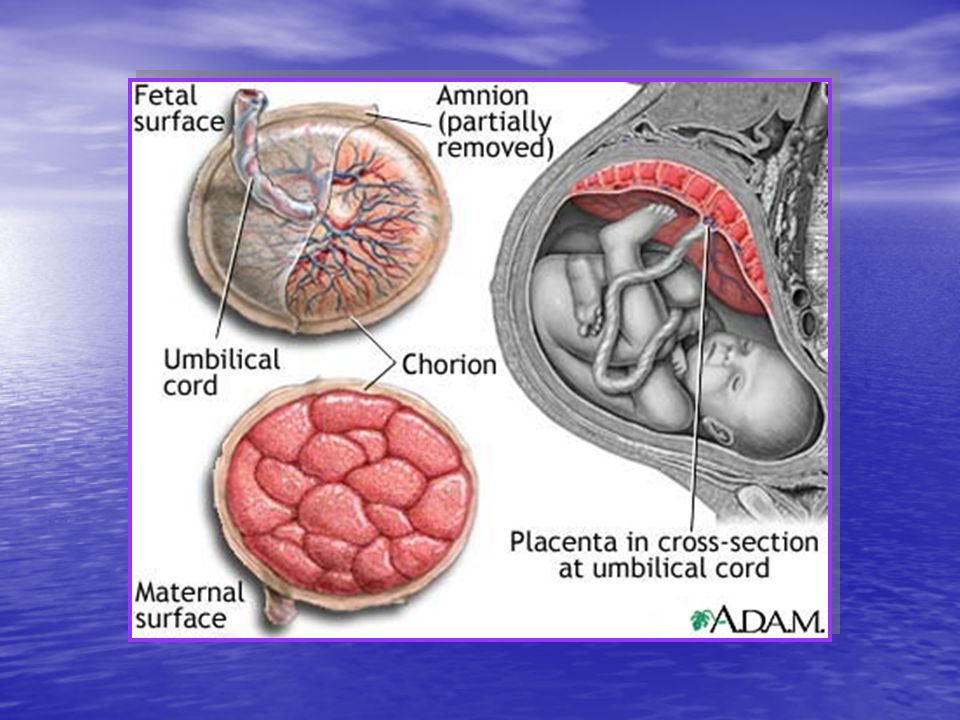 During the last trimester of pregnancy, umbilical blood flow declines significantly as it becomes inversely proportional to the fetal weight measured in kilograms. That percentage decreases considerably during the last trimester till it reaches less than 20%. The umbilical vein enters the abdominal region of the fetus. It carries the oxygenated blood with nutrients to the fetal liver parenchyma and ductus venosus. Then, blood flows to the inferior vena cava and foramen ovale of the fetal heart.[14]
During the last trimester of pregnancy, umbilical blood flow declines significantly as it becomes inversely proportional to the fetal weight measured in kilograms. That percentage decreases considerably during the last trimester till it reaches less than 20%. The umbilical vein enters the abdominal region of the fetus. It carries the oxygenated blood with nutrients to the fetal liver parenchyma and ductus venosus. Then, blood flows to the inferior vena cava and foramen ovale of the fetal heart.[14]
On the other hand, the role and distribution of lymphatic drainage for the placenta, as well as the umbilical cord, has been scarcely discussed in scientific resources. However, recent research has shown D2-40 expression at the level of placental stromal has a vital role in the fetal lymphatic drainage. This expression links to podoplanin-expressing cells whose function is related to forming a lymphatic-like reticular network. The thinking is that those cells are responsible for providing lymphatic drainage for the umbilical cord and the placenta. [15]
[15]
Nerves
The umbilical cord lacks intrinsic and extrinsic innervations during all stages of embryonic development. Vasoactive substances secreted locally within the umbilical vessels wall or carried through the fetal circulation are responsible for regulating the smooth muscle tension within the umbilical vasculature. For instance, nitrous oxide and prostacyclin play an essential role in maintaining the low vascular resistance within the umbilical and placental circulation. Furthermore, catecholamines are primary contributors for vasoconstriction of the umbilical vessels immediately after parturition.[16]
Muscles
The bulk of the umbilical cord consists of Wharton's jelly since it does not have any voluntary skeletal muscles. However, the umbilical vasculature has several smooth muscle layers of various compositions and thicknesses. The walls of umbilical vessels consist mainly of three layers: tunica externa, tunica media, and tunica interna.
Tunica externa
Also referred to as the tunica adventitia, it is the outermost layer of the umbilical vessels that consists of fibrous and elastic connective tissue with varying amounts of collagen and elastic fibers.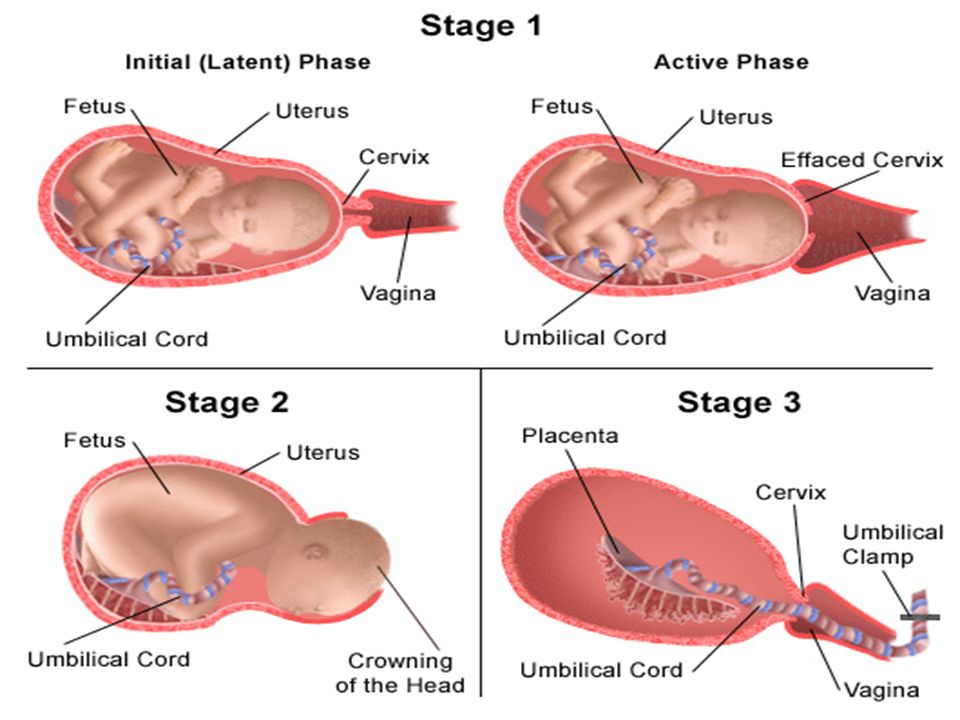 The connective tissue of this layer is quite dense near the tunica media. It transitions to loose connective tissue as it extends toward the periphery of the umbilical vessels. The umbilical arteries have denser connective tissue in their tunica externa compared to that of the umbilical vein.[17]
The connective tissue of this layer is quite dense near the tunica media. It transitions to loose connective tissue as it extends toward the periphery of the umbilical vessels. The umbilical arteries have denser connective tissue in their tunica externa compared to that of the umbilical vein.[17]
Tunica media
This section is the intermediate layer within the wall of the umbilical vessels. It represents the muscular bulk of the vessels and consists mainly of smooth muscle. It provides structural support for the vessels. It is also responsible for changing the diameter of the umbilical vessels. Thus, it contributes primarily to regulate blood flow and blood pressure. It is commonly the thickest layer within the vascular wall. It is much thicker in the umbilical arteries compared to the umbilical vein. Moreover, tunica media of the umbilical arteries contain well-defined internal and external elastic membranes that may be less defined or absent in the umbilical vein wall. [18]
[18]
Tunica interna
Also called the tunica intima, it is the innermost layer of the umbilical vasculature. It is composed of simple squamous epithelium resting on a basement membrane consists of connective tissue rich in elastic fibers. Those layers together form the endothelium of the umbilical vessels. The tunica interna of the umbilical vein contains valves that direct the blood flow in one direction and prevent its regurgitation in the opposite direction. Those valves are absent in the wall of the umbilical arteries.[19]
Physiologic Variants
Umbilical Cord Coiling Patterns
One of the most common morphological variations of the umbilical cord is its different helical coiling patterns. The degree of coiling is measured by the umbilical cord index (UCI). Commonly, the umbilical cord coiling pattern has a UCI of 0.2 coil/cm. The rope model is considered the most common pattern of umbilical cord coiling. On the other hand, hyper-coiling of the umbilical cord is defined as having a UCI greater than 0.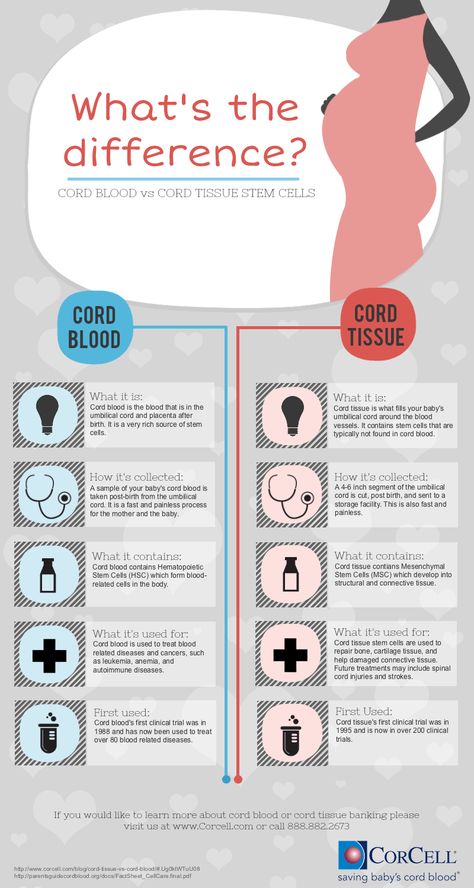 3 coil/cm and a relatively high incidence of about 6% to 21% of all pregnancies.[20] Also, the umbilical cord can coil in an undulating pattern that has a relatively high incidence compared to other coiling patterns, such as segmented or linked coiling of the umbilical cord. It was found clinically that abnormal coiling of the umbilical cord is closely associated with the fetal vascular obstruction, which in its role can eventually lead to fetal thrombi, avascular villi or villous stromal vascular karyorrhexis that commonly occur with segmented coiling pattern of the umbilical cord [21].
3 coil/cm and a relatively high incidence of about 6% to 21% of all pregnancies.[20] Also, the umbilical cord can coil in an undulating pattern that has a relatively high incidence compared to other coiling patterns, such as segmented or linked coiling of the umbilical cord. It was found clinically that abnormal coiling of the umbilical cord is closely associated with the fetal vascular obstruction, which in its role can eventually lead to fetal thrombi, avascular villi or villous stromal vascular karyorrhexis that commonly occur with segmented coiling pattern of the umbilical cord [21].
False Knots of the Umbilical Cord
False knots are bulging masses located on the surface of the umbilical cord. Sometimes, excessive torsion of the umbilical cord inside the uterus can cause these bulging masses to appear as knots on uterine ultrasonography grossly. The knot appearance of this condition forms via the excessive accumulation of Wharton's Jelly bulks alternating with areas with relatively less amount of jelly composing constrictions after each bulging.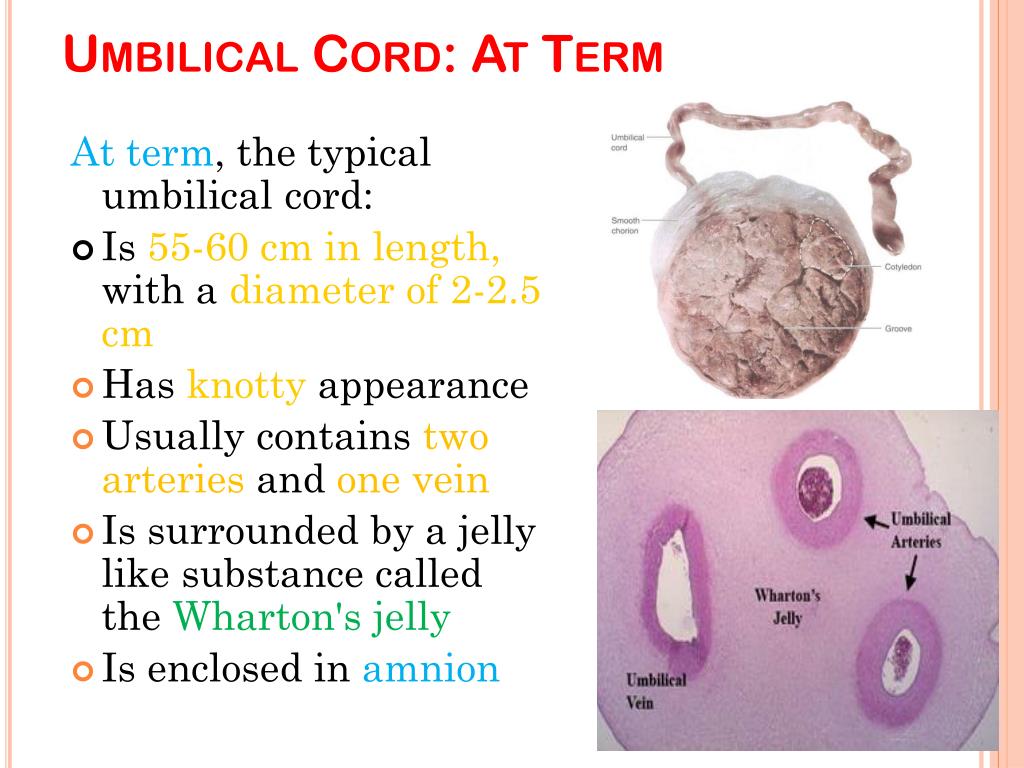 Hence, they were identified as false knots of the umbilical cord. This physiologic variation does not affect the stability of the fetal position, nor does it affect umbilical blood flow and pressure. Thus, false knots do not represent a considerable risk to the fetus.[22]
Hence, they were identified as false knots of the umbilical cord. This physiologic variation does not affect the stability of the fetal position, nor does it affect umbilical blood flow and pressure. Thus, false knots do not represent a considerable risk to the fetus.[22]
Single Umbilical Artery
The incidence of having a single umbilical artery is very low overall. However, It is known to be more common in multiparous females compared to nulliparous ones. Many studies have reported that the left umbilical artery is more often absent than the right.[23] The side of umbilical artery absence has very minimal significance with the exception that one study concluded that infants with a single umbilical artery identified by ultrasound in utero had reported the presence of congenital abnormalities, including cardiac, renal, intestinal, and skeletal anomalies when the left umbilical artery was absent.[23][24][25][26][27] Also, it is noted that the incidence of urinary tract infection is higher in infants with a single umbilical artery.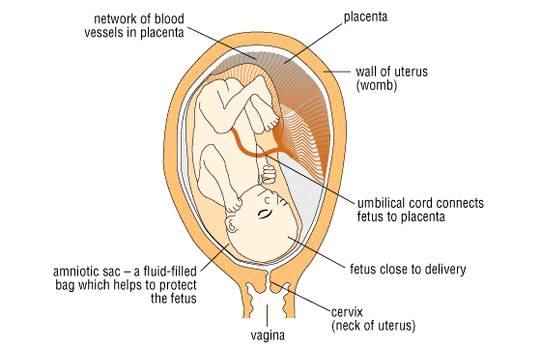 [28]
[28]
Surgical Considerations
Anesthetic Considerations
Placental and umbilical blood flow impact fetal oxygen delivery. Myometrial tone and maternal blood pressure have a direct correlation with uterine artery blood flow. Volatile anesthetics usually decrease myometrial tone and tend to reduce maternal blood pressure. Subsequently, there is a decrease in fetal oxygenation due to a reduction in placental blood flow. Maintenance of patent umbilical arteries and baseline maternal arterial blood pressure is essential for maintaining sound cardiac output for the fetus. For example, maternal hypercapnia leads to fetal hypoxia and metabolic acidosis as a result of umbilical venous flow reduction. Similarly, maternal hypocapnia should be avoided during all maternal or fetal procedures since it has a direct correlation with fetal hypoxia. Consequently, inhalation anesthesia is the best option for fetal and intrauterine procedures. Moreover, epidural anesthesia plays a critical role in the prevention of premature labor during the postoperative period of maternal surgeries.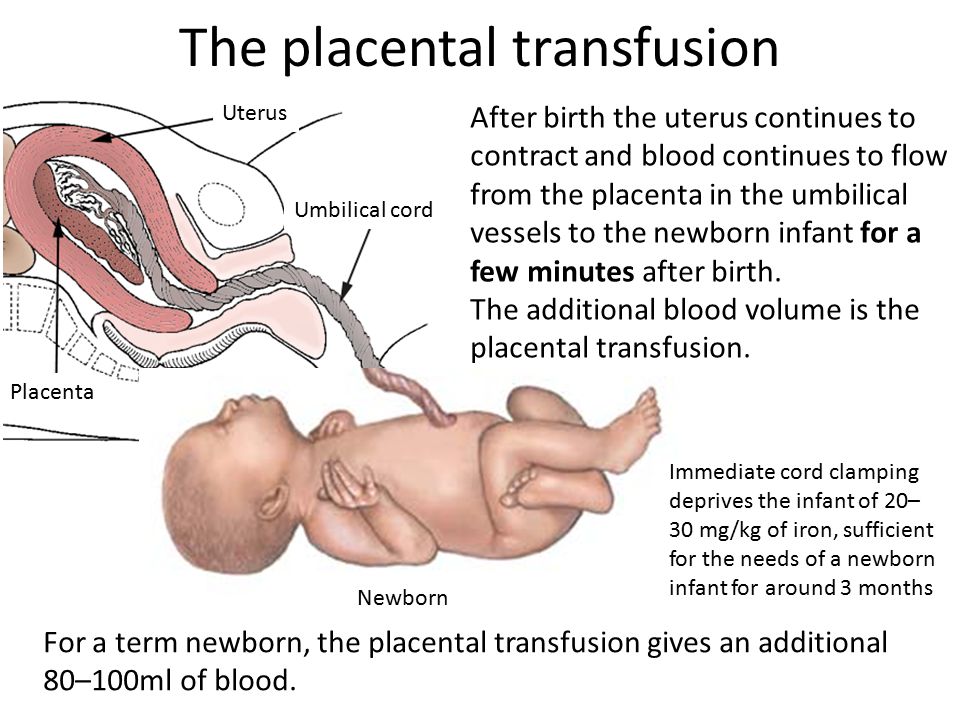 [29]
[29]
Intravenous Administration/Catheterization
The umbilical vein is considered the primary site for cannulation. The umbilical vein remains open for approximately one week after labor, and it can be useful for administering intravenous fluids and medications for newborns requiring more aggressive resuscitation efforts. The umbilical vein has a larger lumen than the umbilical arteries due to its thinner tunica media—catheterization through the umbilical vein to the ductus venosus. Finally, the catheter arrives at the inferior vena cava below the right atrium.[30] Furthermore, umbilical artery lines may also be used for resuscitative efforts during the first week after delivery. Umbilical artery catheterization is routinely used for direct access to monitor arterial blood gas, arterial blood pressure, and angiography. In the neonatal intensive care, umbilical artery catheterization is typically used to provide blood samples for laboratory testings.[31]
Clinical Significance
Different types of umbilical cord abnormalities may be potentially fatal or pose a severe threat to fetal health.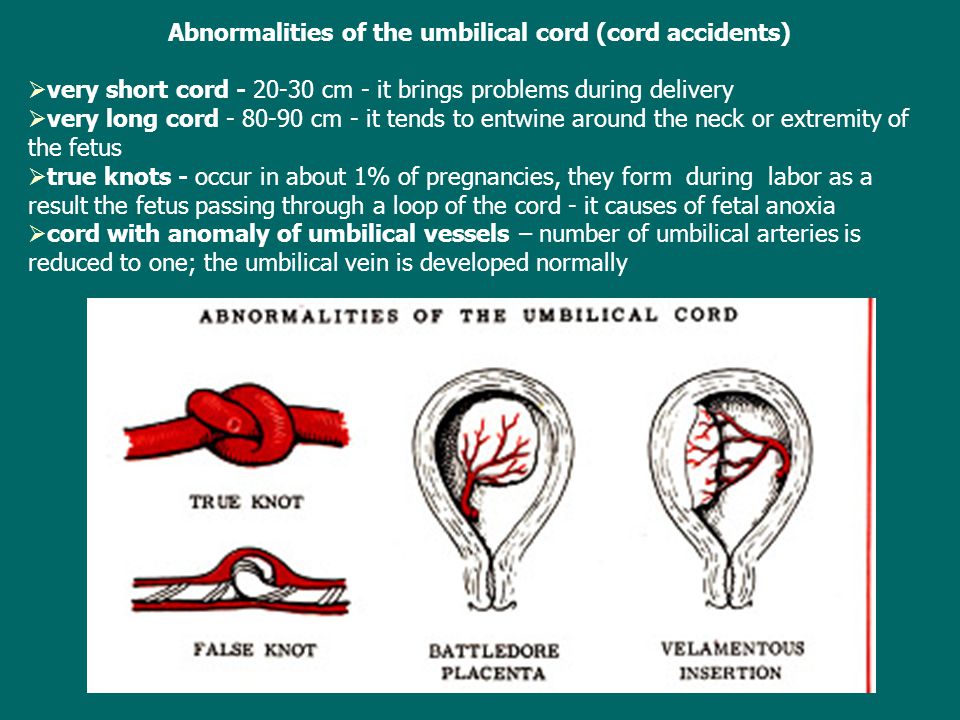 Thus, it is of great clinical significance to have early detection of these malformations to be able to provide a proper diagnosis and plan of care.
Thus, it is of great clinical significance to have early detection of these malformations to be able to provide a proper diagnosis and plan of care.
Velamentous Insertion
The incidence of velamentous insertion of the umbilical cord is significantly high for in vitro fertilization(IVF)-induced pregnancies compared to naturally-conceived pregnancies. It happens in about 10% of pregnancies and 20% of IVF pregnancies.[32] Velamentous insertion of the umbilical cord occurs when the placental end of the umbilical cord consists of umbilical arteries and vein surrounded by fetal membranes without Wharton's jelly. The exact reason for this condition is still unclear. However, the most current hypothesis suggests that during IVF pregnancy, half of the placenta undergoes excessive proliferation making the site of the insertion of the umbilical cord move peripherally away from its center. Conversely, the other pole of the placenta involutes and the umbilical cord becomes unable to follow the migration of the placenta.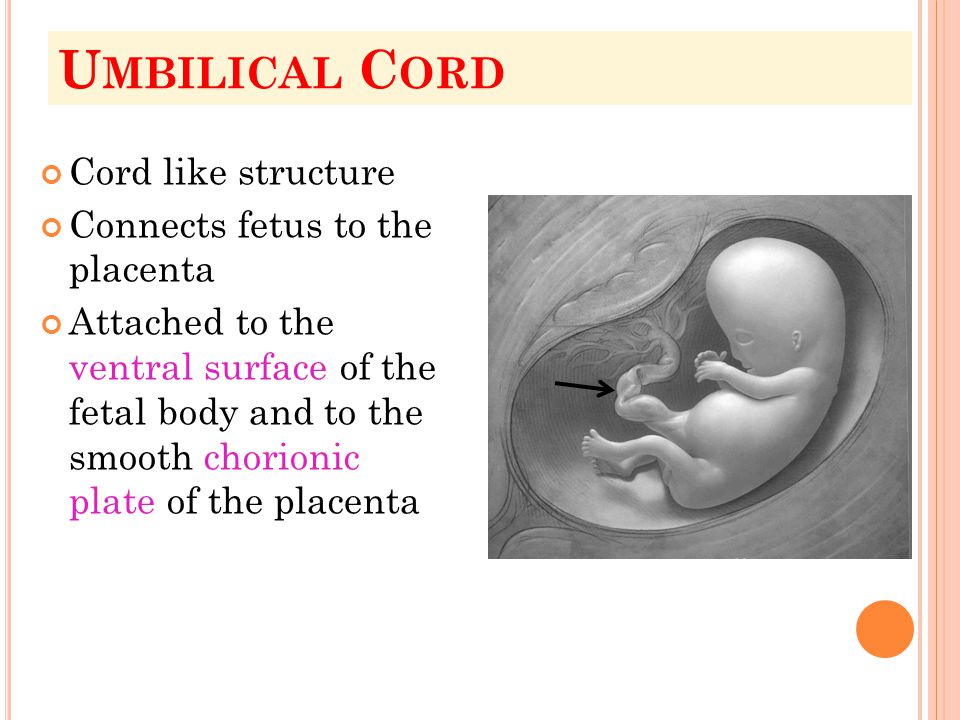 This condition casts risk for the fetus during delivery.[33]
This condition casts risk for the fetus during delivery.[33]
Four-Vessel Umbilical Cord
Normal umbilical cord anatomy consists of three vessels represented by two umbilical arteries and one umbilical vein. By the seventh week of gestation, the right umbilical vein usually obliterates, leaving a single (left) umbilical vein patent. However, there have been documented cases of umbilical cords containing four-vessels. The persistence of two umbilical veins and two umbilical arteries within the umbilical cord is associated with multiple cardiovascular and gastrointestinal anomalies.[34] When both the right and left umbilical veins remain open, a condition called persistent right umbilical vein (PRUV). This condition usually happens due to a deficiency in folic acid during the first trimester of pregnancy. This condition may cause teratogenic effects for the fetus and act as a risk factor for its overall physical health.[35]
True Knots of the Umbilical Cord
These are real tangling nodules of the umbilical vessels along the length of the umbilical cord.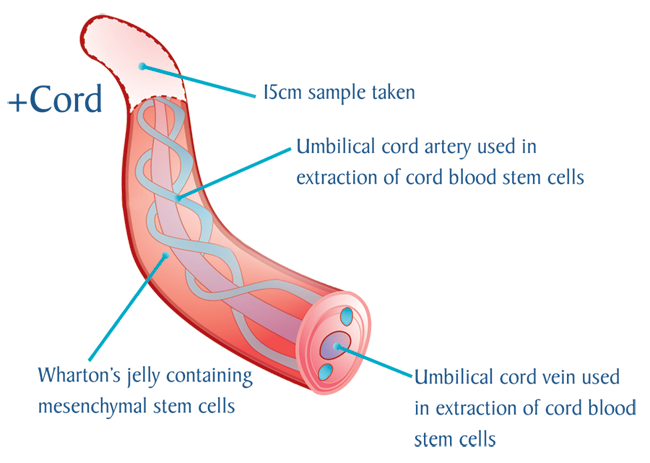 They usually occur early in pregnancy as a result of various predisposing factors. Most commonly, the development of true knots is associated with the presence of excessive amniotic fluid, causing high pressure on the umbilical cord vessels, increasing their torsional force, causing deep knots of those vessels. Also, an increase in the movement of the fetus in utero plays a vital role in creating that teratogenic deformity as supercoils of the umbilical cord can cause it to knot over itself. True knot deformities of the umbilical cord are very dangerous because they may obstruct the blood flow in the umbilical vessels, which may eventually lead to fetal demise.[36]
They usually occur early in pregnancy as a result of various predisposing factors. Most commonly, the development of true knots is associated with the presence of excessive amniotic fluid, causing high pressure on the umbilical cord vessels, increasing their torsional force, causing deep knots of those vessels. Also, an increase in the movement of the fetus in utero plays a vital role in creating that teratogenic deformity as supercoils of the umbilical cord can cause it to knot over itself. True knot deformities of the umbilical cord are very dangerous because they may obstruct the blood flow in the umbilical vessels, which may eventually lead to fetal demise.[36]
Very Short Umbilical Cord
An umbilical cord is considered significantly short when its length is less than approximately 40 cm. A short umbilical cord can lead to premature separation from the placenta resulting in an interruption in fetal circulation and, as a result, intrauterine bleeding followed by fetal death.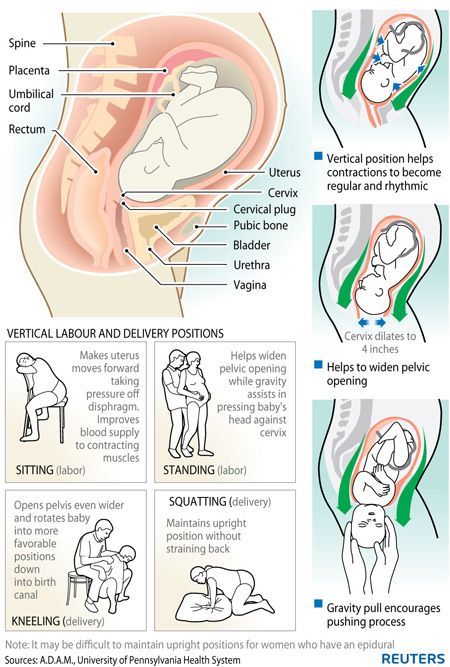 [37]
[37]
Very Long Umbilical Cord
If an umbilical cord is longer than 65 to 70 cm, it is clinically considered long. An abnormally long umbilical cord has the greater potential wind around the neck of the fetus multiple times contribute to fetal death, or it may also protrude from the mother's cervix.[37]
Omphalocele
Also referred to as exomphalos, an omphalocele is an abdominal wall defect that causes the herniation of bowel and sometimes other organs into the umbilical cord. The pathophysiology behind this condition is due to the failure of the reduction of the physiological umbilical hernia.[38] Surgical correction is considered for such conditions to prevent intestinal obstruction of the neonate.
Abnormal attachment of the umbilical cord to the placenta
Sometimes, the umbilical cord may have an abnormal attachment site on the placenta. For example, the umbilical cord may attach to the placenta significantly off-center, giving rise to eccentric attachment deformity.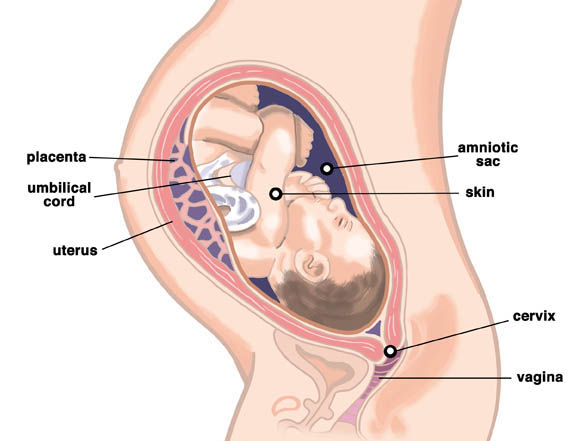 The placenta may take a deformed shape called battledore placenta. This deformity results from the marginal attachment of the umbilical cord to the placenta.[39] It closely correlates with abnormal hyper-coiling of the umbilical cord in most cases.
The placenta may take a deformed shape called battledore placenta. This deformity results from the marginal attachment of the umbilical cord to the placenta.[39] It closely correlates with abnormal hyper-coiling of the umbilical cord in most cases.
Delayed Umbilical Cord Separation
Normal separation of the umbilical cord can occur anytime after delivery with no reliable, constant timeline. However, generally speaking, separation of the umbilical cord is considered delayed if it happens later than the first three weeks after delivery. There are many factors and pathological conditions associated with the incidence of delayed cord separation. For instance, the topical application of antibiotics, alcohol, and triple dye after delivery has a significant contribution to delayed cord separation. Moreover, pathological conditions such as; infections, immune disorders, and the presence of urachal remnants can also delay umbilical cord separation. Interestingly, researchers found a correlation between each low birth weight, cesarian delivery, and prematurity and the increased risk of delayed umbilical cord separation. It is clinically significant to consider further workup in newborns with delayed umbilical cord separation and skin infections or those with persistent urachal remnants. These infants most likely have an underlying immunologic disorder.[40]
It is clinically significant to consider further workup in newborns with delayed umbilical cord separation and skin infections or those with persistent urachal remnants. These infants most likely have an underlying immunologic disorder.[40]
Umbilical Cysts
Cysts classify into two main categories: true cysts and pseudocysts. They usually occur near or around the insertion of the cord into the fetal umbilicus. Umbilical cord cysts generally develop during the first trimester with a standard resolution by the end of the twelfth week of gestation. Umbilical cysts have an incidence of 3.4% of all pregnancies. The exact etiology of umbilical cysts is not defined clinically. However, they appear to be closely related to chromosomal abnormalities, including trisomies of chromosomes 13 and 18, imperforate anus, and angiomyxoma of the cord.[41] The most frequently encountered type of cyst is a pseudocyst. Pseudocysts are also known as Wharton's jelly cysts. They lack epithelial tissue and occur commonly as a result of focal edema of Wharton's jelly.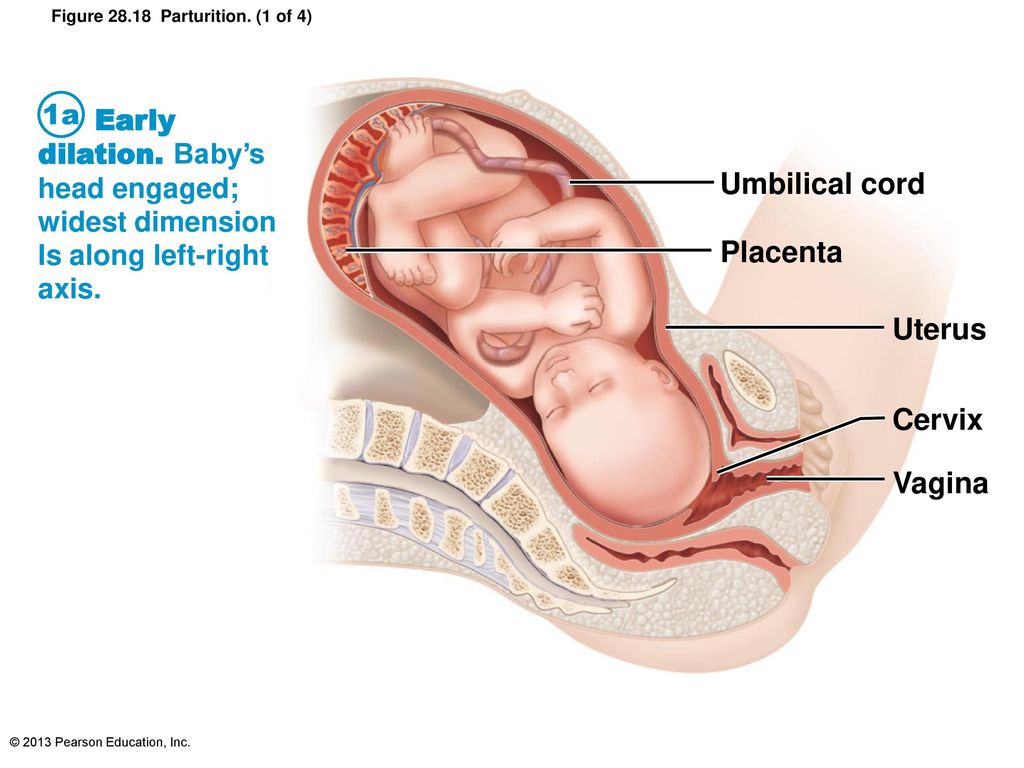 Also, they can develop as a result of mucoid degeneration inside the cord. It is not uncommon to see single cysts or multiple focal lesions. The diameter of these lesions is less than 2 cm approximately.
Also, they can develop as a result of mucoid degeneration inside the cord. It is not uncommon to see single cysts or multiple focal lesions. The diameter of these lesions is less than 2 cm approximately.
On the contrary, true cysts of the umbilical cord develop commonly from the omphalomesenteric duct or other primitive embryonic structures, including the allantois. True cysts have a distinct epithelial lining; hence they are known as true cysts.[42] In general, umbilical cysts are considered clinically significant. They serve as an early indicator of chromosomal abnormalities, especially if cysts persist during the second and third trimester of pregnancy. Thus, fetal karyotyping and amniocentesis are useful diagnostic procedures to determine any underlying conditions associated with them.
Umbilical Granuloma
An umbilical granuloma is a red nodule that may develop after the umbilical cord has separated from the naval of a newborn. On average, the diameter of a granuloma is about five mm.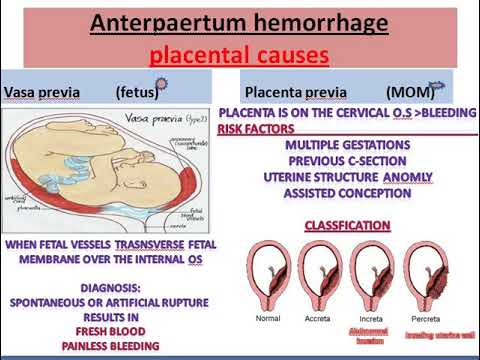 [40] The development of this lesion involves an abnormal proliferation of fibroblasts at the umbilicus forming thick layers of granulation tissue and endothelium. The vessels enclosed within the lesion have a dotted or strawberry-like appearance.[43] The mainstay of treatment is chemical cauterization with silver nitrate. Extra caution is needed to avoid injury or chemical burns of the surrounding skin. However, it is of great clinical significance to provide further evaluation of persistent umbilical granulomas as they can be mistaken for polyps that may require surgical removal.
[40] The development of this lesion involves an abnormal proliferation of fibroblasts at the umbilicus forming thick layers of granulation tissue and endothelium. The vessels enclosed within the lesion have a dotted or strawberry-like appearance.[43] The mainstay of treatment is chemical cauterization with silver nitrate. Extra caution is needed to avoid injury or chemical burns of the surrounding skin. However, it is of great clinical significance to provide further evaluation of persistent umbilical granulomas as they can be mistaken for polyps that may require surgical removal.
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
Figure
Development of the Fetal membrane and the Placenta, Diagram illustrating a later stage in the development of the umbilical cord, Placental villi, Umbilical cord, Allantois, Heart, Embryo. Contributed by Gray's Anatomy Plates
Figure
Development of Fetal Membranes and Placenta, Fetus in utero; between fifth and sixth months, Umbilical cord, Cervix uteri.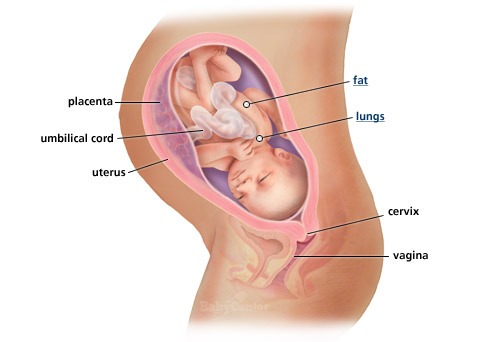 Contributed by Gray's Anatomy Plates
Contributed by Gray's Anatomy Plates
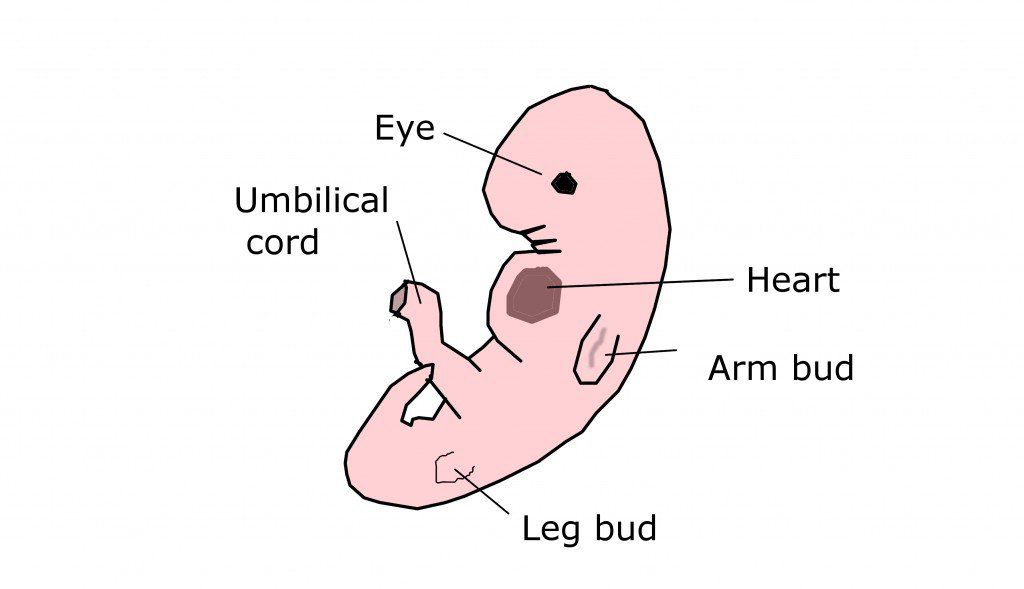
Figure
The Branchial Region, Embryo of about six weeks, Umbilical cord, Embryology. Contributed by Gray's Anatomy Plates
Figure
Umbilical cord. Image courtesy S Bhimji MD
References
- 1.
Barrios-Arpi LM, Rodríguez Gutiérrez JL, Lopez-Torres B. Histological characterization of umbilical cord in alpaca (Vicugna pacos). Anat Histol Embryol. 2017 Dec;46(6):533-538. [PubMed: 28884482]
- 2.
Tokar B, Yucel F. Anatomical variations of medial umbilical ligament: clinical significance in laparoscopic exploration of children. Pediatr Surg Int. 2009 Dec;25(12):1077-80. [PubMed: 19727772]
- 3.
Mamatha H, Hemalatha B, Vinodini P, Souza AS, Suhani S. Anatomical Study on the Variations in the Branching Pattern of Internal Iliac Artery. Indian J Surg. 2015 Dec;77(Suppl 2):248-52. [PMC free article: PMC4692843] [PubMed: 26730003]
- 4.
Hooper SB, Polglase GR, te Pas AB.
 A physiological approach to the timing of umbilical cord clamping at birth. Arch Dis Child Fetal Neonatal Ed. 2015 Jul;100(4):F355-60. [PubMed: 25540147]
A physiological approach to the timing of umbilical cord clamping at birth. Arch Dis Child Fetal Neonatal Ed. 2015 Jul;100(4):F355-60. [PubMed: 25540147]- 5.
Di Naro E, Ghezzi F, Raio L, Franchi M, D'Addario V. Umbilical cord morphology and pregnancy outcome. Eur J Obstet Gynecol Reprod Biol. 2001 Jun;96(2):150-7. [PubMed: 11384798]
- 6.
Fathi AH, Soltanian H, Saber AA. Surgical anatomy and morphologic variations of umbilical structures. Am Surg. 2012 May;78(5):540-4. [PubMed: 22546125]
- 7.
Parada Villavicencio C, Adam SZ, Nikolaidis P, Yaghmai V, Miller FH. Imaging of the Urachus: Anomalies, Complications, and Mimics. Radiographics. 2016 Nov-Dec;36(7):2049-2063. [PubMed: 27831842]
- 8.
Umeda S, Usui N, Kanagawa T, Yamamichi T, Nara K, Ueno T, Owari M, Uehara S, Oue T, Kimura T, Okuyama H. Prenatal and Postnatal Clinical Course of an Urachus Identified as an Allantoic Cyst in the Umbilical Cord. Eur J Pediatr Surg.
 2016 Apr;26(2):200-2. [PubMed: 26981767]
2016 Apr;26(2):200-2. [PubMed: 26981767]- 9.
Ullberg U, Sandstedt B, Lingman G. Hyrtl's anastomosis, the only connection between the two umbilical arteries. A study in full term placentas from AGA infants with normal umbilical artery blood flow. Acta Obstet Gynecol Scand. 2001 Jan;80(1):1-6. [PubMed: 11167180]
- 10.
Ullberg U, Lingman G, Ekman-Ordeberg G, Sandstedt B. Hyrtl's anastomosis is normally developed in placentas from small for gestational age infants. Acta Obstet Gynecol Scand. 2003 Aug;82(8):716-21. [PubMed: 12848642]
- 11.
Coetzee AJ, Castro E, Peres LC. Umbilical Cord Coiling and Zygosity: Is there a Link? Fetal Pediatr Pathol. 2015;34(5):336-9. [PubMed: 26291249]
- 12.
Hubbard LJ, Stanford DA. The Umbilical Cord Lifeline. J Emerg Nurs. 2017 Nov;43(6):593-595. [PubMed: 29100578]
- 13.
Kiserud T, Acharya G. The fetal circulation. Prenat Diagn. 2004 Dec 30;24(13):1049-59.
 [PubMed: 15614842]
[PubMed: 15614842]- 14.
Strong A, Gračner T, Chen P, Kapinos K. On the Value of the Umbilical Cord Blood Supply. Value Health. 2018 Sep;21(9):1077-1082. [PubMed: 30224112]
- 15.
Jin ZW, Nakamura T, Yu HC, Kimura W, Murakami G, Cho BH. Fetal anatomy of peripheral lymphatic vessels: a D2-40 immunohistochemical study using an 18-week human fetus (CRL 155 mm). J Anat. 2010 Jun;216(6):671-82. [PMC free article: PMC2952380] [PubMed: 20408907]
- 16.
Marx GF, Joshi CW, Orkin LR. Placental transmission of nitrous oxide. Anesthesiology. 1970 May;32(5):429-32. [PubMed: 5445031]
- 17.
DeFreitas MJ, Mathur D, Seeherunvong W, Cano T, Katsoufis CP, Duara S, Yasin S, Zilleruelo G, Rodriguez MM, Abitbol CL. Umbilical artery histomorphometry: a link between the intrauterine environment and kidney development. J Dev Orig Health Dis. 2017 Jun;8(3):349-356. [PubMed: 28260559]
- 18.
Hardy KJ, Nye DH. The anatomy of the umbilical vein.
 Aust N Z J Surg. 1969 Nov;39(2):127-32. [PubMed: 5264514]
Aust N Z J Surg. 1969 Nov;39(2):127-32. [PubMed: 5264514]- 19.
Baudin B, Bruneel A, Bosselut N, Vaubourdolle M. A protocol for isolation and culture of human umbilical vein endothelial cells. Nat Protoc. 2007;2(3):481-5. [PubMed: 17406610]
- 20.
Kashanian M, Akbarian A, Kouhpayehzadeh J. The umbilical coiling index and adverse perinatal outcome. Int J Gynaecol Obstet. 2006 Oct;95(1):8-13. [PubMed: 16860802]
- 21.
Ernst LM, Minturn L, Huang MH, Curry E, Su EJ. Gross patterns of umbilical cord coiling: correlations with placental histology and stillbirth. Placenta. 2013 Jul;34(7):583-8. [PubMed: 23642640]
- 22.
Feliks M, Howorka E. [Functional value of false knots of the umbilical cord]. Ginekol Pol. 1968 Jun;39(6):617-24. [PubMed: 5675023]
- 23.
Lubusky M, Dhaifalah I, Prochazka M, Hyjanek J, Mickova I, Vomackova K, Santavy J. Single umbilical artery and its siding in the second trimester of pregnancy: relation to chromosomal defects.
 Prenat Diagn. 2007 Apr;27(4):327-31. [PubMed: 17286313]
Prenat Diagn. 2007 Apr;27(4):327-31. [PubMed: 17286313]- 24.
Geipel A, Germer U, Welp T, Schwinger E, Gembruch U. Prenatal diagnosis of single umbilical artery: determination of the absent side, associated anomalies, Doppler findings and perinatal outcome. Ultrasound Obstet Gynecol. 2000 Feb;15(2):114-7. [PubMed: 10775992]
- 25.
Blazer S, Sujov P, Escholi Z, Itai BH, Bronshtein M. Single umbilical artery--right or left? does it matter? Prenat Diagn. 1997 Jan;17(1):5-8. [PubMed: 9021822]
- 26.
Budorick NE, Kelly TF, Dunn JA, Scioscia AL. The single umbilical artery in a high-risk patient population: what should be offered? J Ultrasound Med. 2001 Jun;20(6):619-27; quiz 628. [PubMed: 11400936]
- 27.
Abuhamad AZ, Shaffer W, Mari G, Copel JA, Hobbins JC, Evans AT. Single umbilical artery: does it matter which artery is missing? Am J Obstet Gynecol. 1995 Sep;173(3 Pt 1):728-32. [PubMed: 7573234]
- 28.

Sepulveda W, Peek MJ, Hassan J, Hollingsworth J. Umbilical vein to artery ratio in fetuses with single umbilical artery. Ultrasound Obstet Gynecol. 1996 Jul;8(1):23-6. [PubMed: 8843614]
- 29.
Hoagland MA, Chatterjee D. Anesthesia for fetal surgery. Paediatr Anaesth. 2017 Apr;27(4):346-357. [PubMed: 28211140]
- 30.
Tomek S, Asch S. Umbilical vein catheterization in the critical newborn: a review of anatomy and technique. EMS World. 2013 Feb;42(2):50-2. [PubMed: 23469464]
- 31.
Umbilical-artery catheters. N Engl J Med. 1979 Feb 08;300(6):316-7. [PubMed: 759887]
- 32.
Shevell T, Malone FD, Vidaver J, Porter TF, Luthy DA, Comstock CH, Hankins GD, Eddleman K, Dolan S, Dugoff L, Craigo S, Timor IE, Carr SR, Wolfe HM, Bianchi DW, D'Alton ME. Assisted reproductive technology and pregnancy outcome. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1039-45. [PubMed: 16260523]
- 33.
Yanaihara A, Hatakeyama S, Ohgi S, Motomura K, Taniguchi R, Hirano A, Takenaka S, Yanaihara T.
 Difference in the size of the placenta and umbilical cord between women with natural pregnancy and those with IVF pregnancy. J Assist Reprod Genet. 2018 Mar;35(3):431-434. [PMC free article: PMC5904058] [PubMed: 29134477]
Difference in the size of the placenta and umbilical cord between women with natural pregnancy and those with IVF pregnancy. J Assist Reprod Genet. 2018 Mar;35(3):431-434. [PMC free article: PMC5904058] [PubMed: 29134477]- 34.
Painter D, Russell P. Four-vessel umbilical cord associated with multiple congenital anomalies. Obstet Gynecol. 1977 Oct;50(4):505-7. [PubMed: 904818]
- 35.
Kim JH, Jin ZW, Murakami G, Chai OH, Rodríguez-Vázquez JF. Persistent right umbilical vein: a study using serial sections of human embryos and fetuses. Anat Cell Biol. 2018 Sep;51(3):218-222. [PMC free article: PMC6172587] [PubMed: 30310717]
- 36.
Sepulveda W, Shennan AH, Bower S, Nicolaidis P, Fisk NM. True knot of the umbilical cord: a difficult prenatal ultrasonographic diagnosis. Ultrasound Obstet Gynecol. 1995 Feb;5(2):106-8. [PubMed: 7719859]
- 37.
Olaya-C M, Bernal JE. Clinical associations to abnormal umbilical cord length in Latin American newborns.
 J Neonatal Perinatal Med. 2015;8(3):251-6. [PubMed: 26485559]
J Neonatal Perinatal Med. 2015;8(3):251-6. [PubMed: 26485559]- 38.
Wakhlu A, Wakhlu AK. The management of exomphalos. J Pediatr Surg. 2000 Jan;35(1):73-6. [PubMed: 10646778]
- 39.
Hoopmann M, Kagan KO. Abnormal Placentation and Umbilical Cord Insertion. Ultraschall Med. 2020 Apr;41(2):120-137. [PubMed: 32259863]
- 40.
Muniraman H, Sardesai T, Sardesai S. Disorders of the Umbilical Cord. Pediatr Rev. 2018 Jul;39(7):332-341. [PubMed: 29967078]
- 41.
Hannaford K, Reeves S, Wegner E. Umbilical cord cysts in the first trimester: are they associated with pregnancy complications? J Ultrasound Med. 2013 May;32(5):801-6. [PubMed: 23620322]
- 42.
Whipple NS, Bennett EE, Kaza E, O'Connor M. Umbilical Cord Pseudocyst in a Newborn. J Pediatr. 2016 Oct;177:333. [PubMed: 27473880]
- 43.
Ancer-Arellano J, Argenziano G, Villarreal-Martinez A, Cardenas-de la Garza JA, Villarreal-Villarreal CD, Ocampo-Candiani J.
 Dermoscopic findings of umbilical granuloma. Pediatr Dermatol. 2019 May;36(3):393-394. [PubMed: 30811653]
Dermoscopic findings of umbilical granuloma. Pediatr Dermatol. 2019 May;36(3):393-394. [PubMed: 30811653]
All about the placenta and umbilical cord
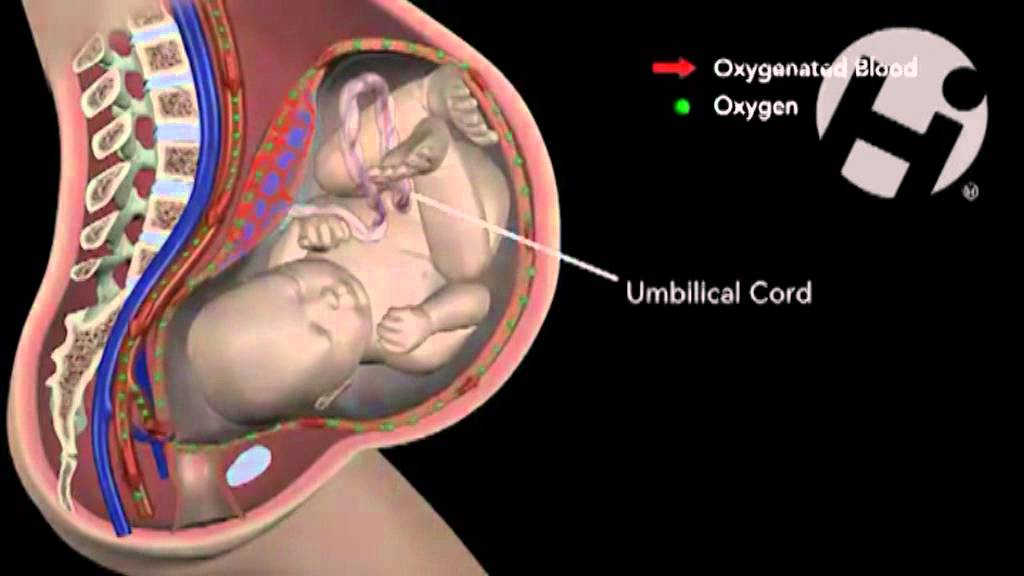
Soon after a baby is conceived, a support system, comprised of the placenta and umbilical cord, begins to develop. These two structures are essential for sustaining a healthy pregnancy, explains Donald Davis, an obstetrician in Medicine Hat, Alta., and past president of the Society of Obstetricians and Gynaecologists of Canada.
What are the placenta and umbilical cord?
The placenta provides all the oxygen, water and nutrients the baby needs to grow in the uterus, and transmits fetal waste and carbon dioxide from the baby to the mother’s system for excretion. It also produces hCG (human chorionic gonadotropin), the hormone considered necessary to establish a healthy pregnancy.
The placenta is attached to the fetus through the umbilical cord, the lifeline between mother and baby. It contains one vein, carrying oxygenated blood from the placenta to the baby, and two arteries, bringing deoxygenated blood from the baby to the placenta.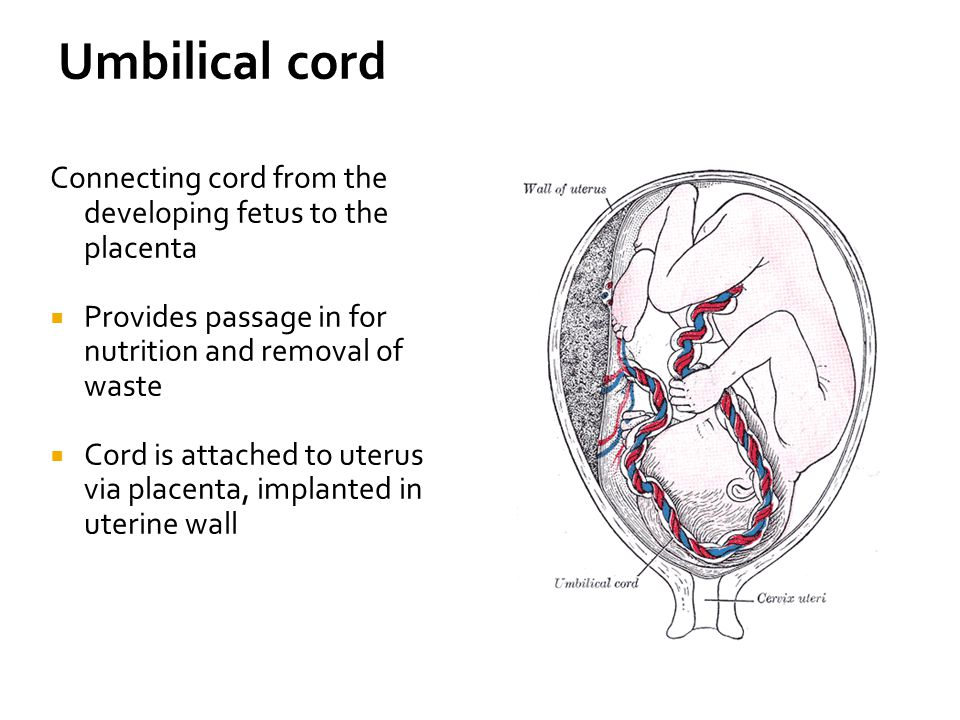
How do they grow?
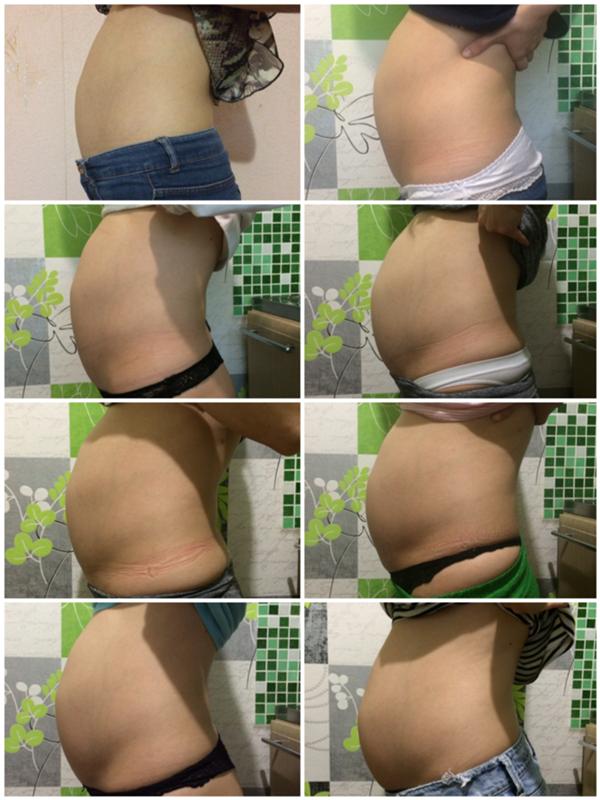
When an egg is fertilized, it divides into two components — one becomes the embryo, which develops into the fetus, and the other becomes the placenta, which grows along the lining of the uterus. The umbilical cord develops from embryonic tissue and will grow about 60 centimetres long.
What can a mother do to keep the placenta healthy?
Healthy habits, such as eating nutritious foods and not smoking, are important during pregnancy. If you have health problems, such as high blood pressure, which can adversely affect the health of the vessels of the placenta, talk to your doctor before becoming pregnant.
What are some complications of the baby’s support system?
Placenta previa is a rare condition where the placenta develops in an abnormal position next to or covering the cervix. Sometimes women with this condition develop bleeding and require special care during pregnancy. In some cases, a low-lying placenta moves to a better place late in pregnancy, but if it is over the cervix at term, a Caesarean section is needed to safely deliver the baby.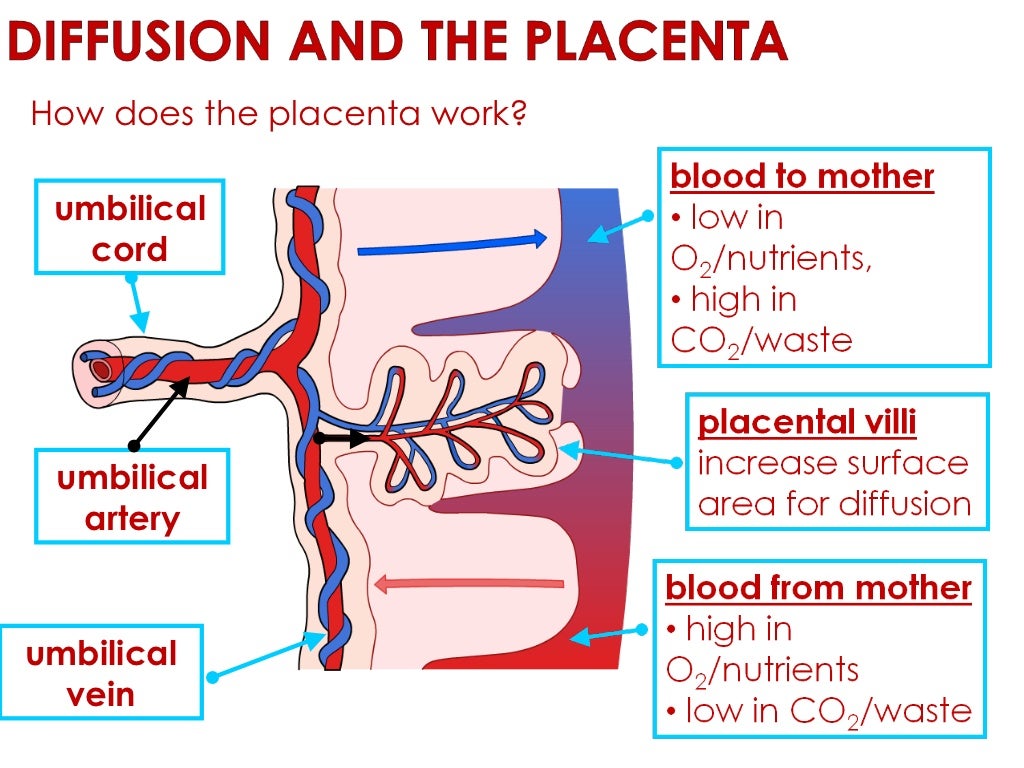
Placental abruption is premature separation of the placenta from the wall of the uterus, which usually causes bleeding. If it’s severe enough, this condition requires a Caesarean section.
While it’s possible for the umbilical cord to get wrapped around the baby’s neck or a limb, this isn’t usually a cause for concern. In rare cases, the wrapped cord can become compressed, decreasing blood flow to the baby. If a problem with the cord is suspected, your physician may be able to identify it by listening to the baby’s heart or monitoring the blood through the cord with ultrasound.
What happens after the birth?
When the baby is born, the cord is clamped and cut. Recent Canadian research has shown that there are health benefits to delaying the cutting of the cord for about two minutes. If you have opted for cord-blood banking, blood will be painlessly withdrawn from the cord after it’s cut, but usually before the placenta is delivered.
The uterus contracts a few times following the birth of the baby to expel the placenta (sometimes called the afterbirth). Your caregiver will then inspect the placenta to make sure it’s intact.
Your caregiver will then inspect the placenta to make sure it’s intact.
Umbilical cord: everything you need to know.
06/29/2022
Future parents often know about the umbilical cord (umbilical cord) only that it is clamped after the birth of a child. Meanwhile, the umbilical cord plays an important role in the course of a healthy pregnancy, and the blood and tissues of the umbilical cord are a kind of bio-insurance for the health of your family for many years and even decades in the future.
So, what are the functions of the umbilical cord?
The umbilical cord is a wonderful thread that connects mother and child for 9months of pregnancy. A narrow, tube-like structure, the umbilical cord runs from the belly of the developing embryo to the placenta, delivering oxygen and nutrient-rich blood and removing the baby's waste products. It begins to develop about 5 weeks after conception. As the baby grows, the umbilical cord gets longer and longer, forming a neat coil in the womb, until it reaches its full length (50-60 cm) at about 28 weeks.
There are blood vessels inside the umbilical cord: two arteries and one vein. The vessels are located in the thickness of a powerful connective tissue that protects them from possible compression. The vein delivers fresh oxygen and nutrients to the baby through the placenta, which in turn is connected to the mother's bloodstream. The arteries transport the waste products of the child. The path is the same: through the placenta, they enter the mother's bloodstream and are filtered through her kidneys. nine0003
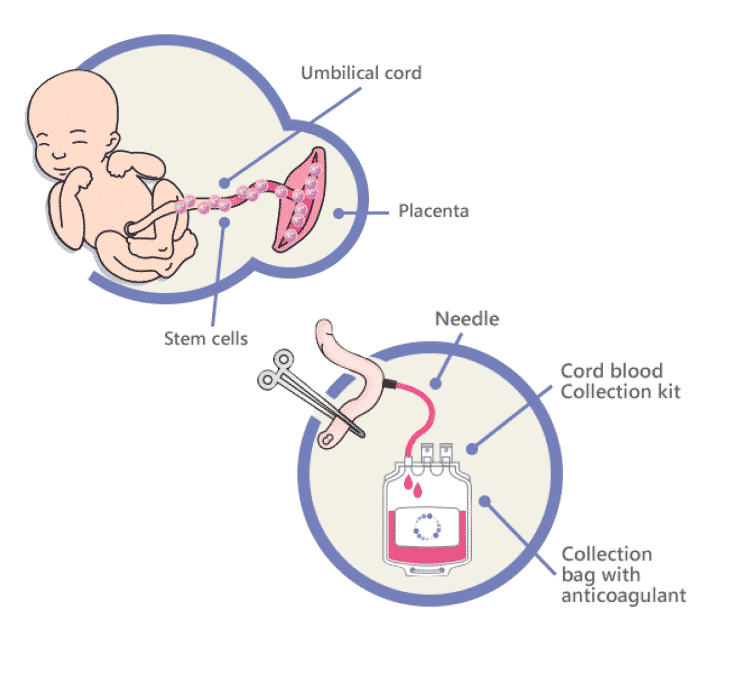
The blood that flows through the umbilical cord is called cord blood. It is a rich source of hematopoietic stem cells. These cells can be harvested and stored for use in more than 80 treatments for diseases including leukemia, lymphomas, metabolic disorders, various anemias, and more.
The connective tissue that protects the vessels in the umbilical cord is called Wharton's jelly. It is a gelatinous substance composed mainly of collagen. It is Wharton's jelly that allows the umbilical cord to do its job throughout pregnancy, preventing it from contracting or bending.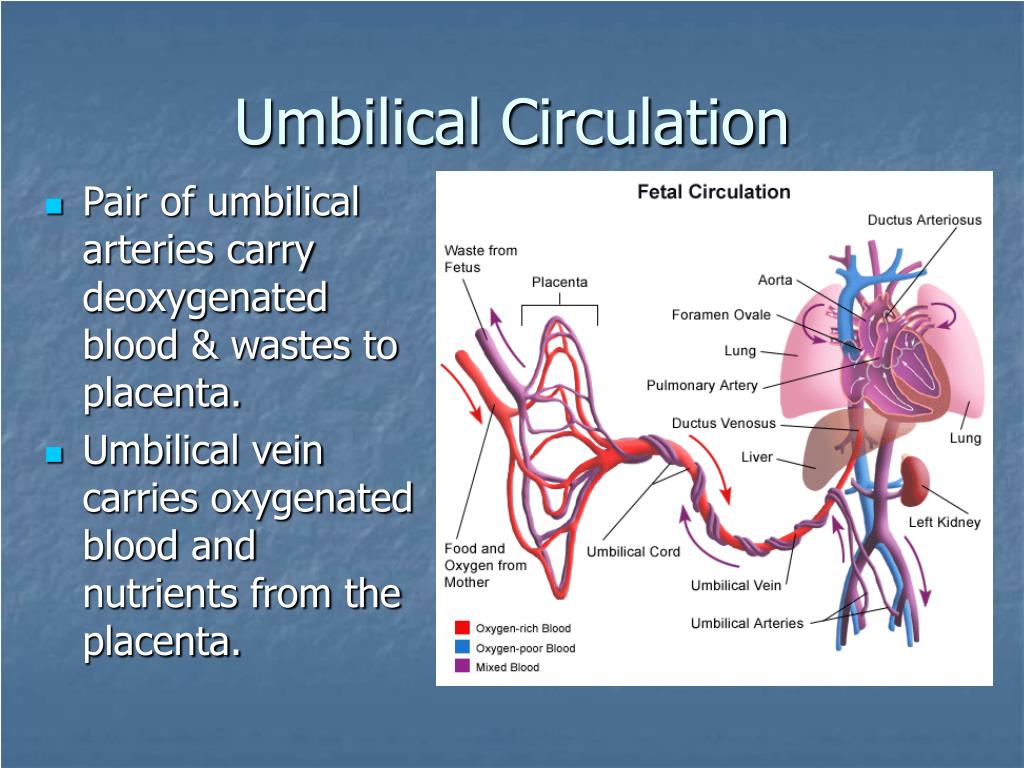 In addition, it is in the connective tissue of the umbilical cord that mesenchymal stem cells (MSCs) are located, which are currently being actively explored as a potential treatment for a wide range of serious diseases. Like cord blood, cord tissue and MSCs can be banked. nine0003
In addition, it is in the connective tissue of the umbilical cord that mesenchymal stem cells (MSCs) are located, which are currently being actively explored as a potential treatment for a wide range of serious diseases. Like cord blood, cord tissue and MSCs can be banked. nine0003
What happens to the umbilical cord after the baby is born?
When a baby is born, the umbilical cord is no longer needed, so it is cut. This process is quick and painless; since the umbilical cord contains no nerves, the baby will not feel anything.
Cords are usually discarded unless the family decides to collect and store cord blood and/or cord tissue from their child. The collection of these biomaterials is quick, easy and low risk, however, the collection needs to be planned in advance for the family: biobanks must be notified of the intention to save blood and tissue, and parents will need to have a cord blood and / or tissue collection kit (most banks recommend purchasing set at least six weeks before the due date). nine0003
nine0003
CryoCentre LLC works on an all-inclusive basis: when concluding a Contract for stem cell collection, we form and send a set to the maternity hospital specified by the clients. If the place of future birth is not determined, the set is kept at the parents' home in the appropriate conditions determined by the bank.
About the pulsation of the umbilical cord.
Delayed cord clamping is 30-60 seconds after the baby is born. This practice is recommended by major medical organizations, including the World Health Organization (WHO). Delayed cord clamping allows more fetal red blood cells from the placenta to pass through the cord into the baby's body, as recommended. This maintains iron stores during the first months of life, reducing the risk of developing iron deficiency anemia. This practice is also believed to promote healthy brain development in the first few years of life. Delayed cord clamping can be performed for both vaginal delivery and caesarean delivery, and is suitable for term and premature babies. It is also fully compatible with newborn cord blood banking. nine0003
It is also fully compatible with newborn cord blood banking. nine0003
There is an Indonesian form of childbirth, the so-called "lotus birth". In this case, the umbilical cord is not cut and the baby remains attached to the placenta until two weeks after birth. This practice is not generally accepted and has not been shown to provide any health benefits to infants. The vast majority of medical practitioners advise against doing this, arguing that lotus childbirth is deadly for newborns, as it seriously increases the risk of bacterial infections. nine0029
If you have questions about cord blood and/or cord storage, talk to your doctor, call CryoCentre LLC to make an informed decision for your family's bioinsurance health.
Placenta and umbilical cord: what is important to know?
9 monthsHealth
By the 12-14th week of pregnancy, the placenta and umbilical cord are finally formed - structures that exist only during pregnancy and perform the functions of exchange between mother and baby. What are these temporary organs and how do they affect the development and condition of the baby? nine0003
What are these temporary organs and how do they affect the development and condition of the baby? nine0003
Placenta
Placenta (from Latin placenta – “pie, cake, pancake”) plays an invaluable role in the development of the fetus, ensuring its growth, development, nutrition, respiration and excretion of waste metabolic products, as well as protecting the fetus from all kinds of harmful impacts.
The placenta is a spongy oval or semicircular organ with a lobed structure. Each lobule of the placenta contains many small vessels. With a normal full-term pregnancy and a fetal weight of 3300-3400 g, the diameter of the placenta is from 15 to 25 cm, thickness 2-4 cm, weight 500 g.
Two systems of blood vessels converge in this organ: one of them (maternal) connects the placenta with the vessels of the uterus, the other (fetal) with the umbilical cord of the fetus. The baby's blood vessels come very close to the mother's, but the maternal and fetal blood streams never mix.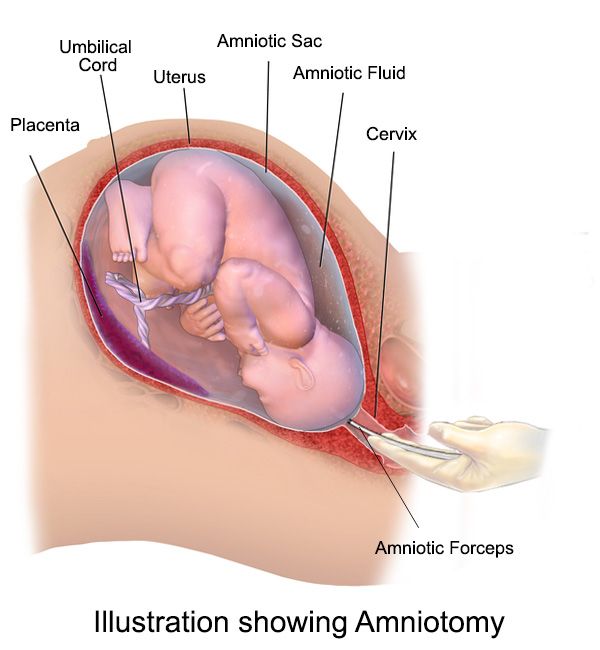 Between the two vascular systems there is a barrier membrane (one layer of cells) - the "customs and border service" of the placenta. Through it, the exchange of substances between mother and baby takes place: the maternal circulatory system brings oxygen and nutrients to the placenta and removes waste products and carbon dioxide from the placenta. The placental barrier allows the protective proteins (antibodies) of the mother to the child, ensuring its protection, and at the same time delays the cells of the woman's immune system that can cause a rejection reaction of the fetus, recognizing a foreign object in it. It is impenetrable to many harmful substances, viruses, bacteria. In addition, the placenta produces hormones that are important for successful pregnancy, and enzymes that destroy harmful substances. nine0003
Between the two vascular systems there is a barrier membrane (one layer of cells) - the "customs and border service" of the placenta. Through it, the exchange of substances between mother and baby takes place: the maternal circulatory system brings oxygen and nutrients to the placenta and removes waste products and carbon dioxide from the placenta. The placental barrier allows the protective proteins (antibodies) of the mother to the child, ensuring its protection, and at the same time delays the cells of the woman's immune system that can cause a rejection reaction of the fetus, recognizing a foreign object in it. It is impenetrable to many harmful substances, viruses, bacteria. In addition, the placenta produces hormones that are important for successful pregnancy, and enzymes that destroy harmful substances. nine0003
Umbilical cord
From the fetal part of the placenta come vessels that unite into larger ones, which eventually form the umbilical cord. The umbilical cord is a long cord (normally from 40 to 60 cm), up to 2 cm thick, consisting of connective tissue, inside of which there are two arteries and one vein.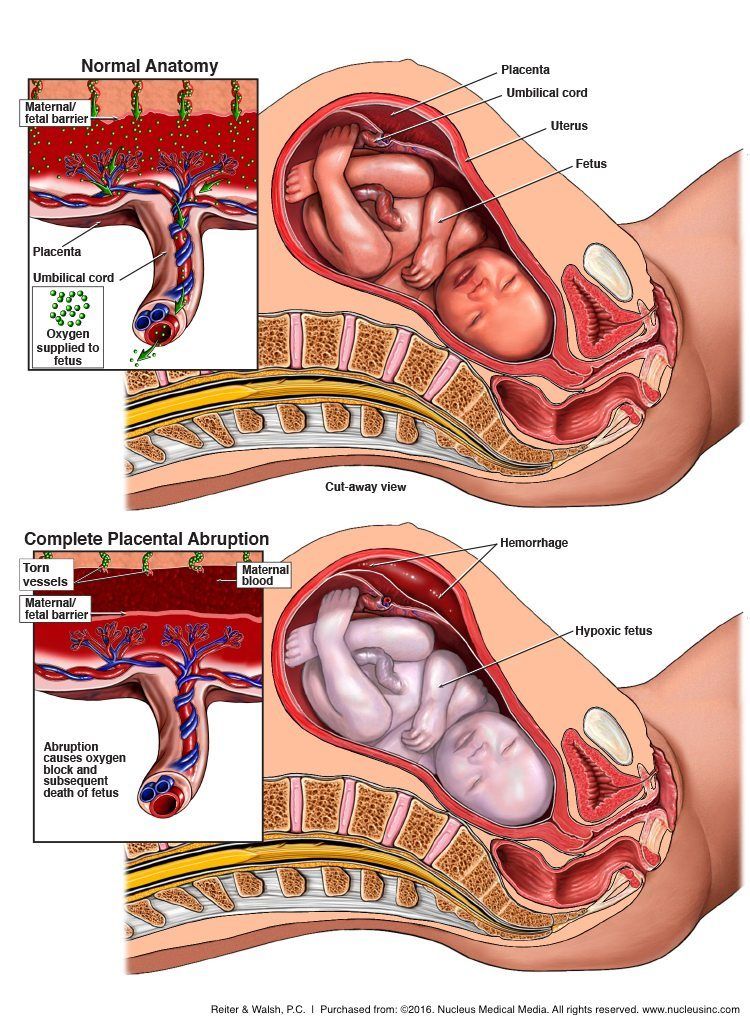 Despite the apparent discrepancy, the vessel called the venous carries arterial blood, while the two arterial vessels carry venous blood. These large vessels are surrounded by a special protective jelly-like substance - Wharton's jelly, which, due to its consistency, plays an important protective role - it protects the vessels from squeezing. The umbilical cord connects the placenta and the baby through the umbilical ring. The single umbilical vein that leaves the placenta enters the fetal abdomen through the umbilical ring and carries oxygenated blood, nutrients, and drugs that have passed the placental barrier. Through the arteries of the umbilical cord, the baby's blood flows back to the placenta, it carries waste products of decay and carbon dioxide. This is how fetal-placental blood flow occurs. After the birth of the baby, when the umbilical cord is cut, the connection between the blood circulation of the fetus and the blood flow of the mother stops, and only the navel reminds of their "blood" connection.
Despite the apparent discrepancy, the vessel called the venous carries arterial blood, while the two arterial vessels carry venous blood. These large vessels are surrounded by a special protective jelly-like substance - Wharton's jelly, which, due to its consistency, plays an important protective role - it protects the vessels from squeezing. The umbilical cord connects the placenta and the baby through the umbilical ring. The single umbilical vein that leaves the placenta enters the fetal abdomen through the umbilical ring and carries oxygenated blood, nutrients, and drugs that have passed the placental barrier. Through the arteries of the umbilical cord, the baby's blood flows back to the placenta, it carries waste products of decay and carbon dioxide. This is how fetal-placental blood flow occurs. After the birth of the baby, when the umbilical cord is cut, the connection between the blood circulation of the fetus and the blood flow of the mother stops, and only the navel reminds of their "blood" connection. nine0003
nine0003
Placental disorders
A change in the size (diameter and thickness) of the placenta, detected by ultrasound, does not always indicate that the pregnancy is unfavorable. Most often, such "deviations" are only an individual feature and do not affect the development of the fetus. Only significant deviations deserve attention.
Small placenta, or placental hypoplasia. Such a diagnosis is valid only with a significant decrease in the size of the placenta. The cause of this condition is most often genetic abnormalities, while the fetus often lags behind in development and has other malformations. nine0003
A thin placenta is considered to be a placenta with insufficient weight, but at the same time of normal size. Sometimes a thin placenta accompanies placental insufficiency and is therefore a risk factor for intrauterine growth retardation and serious problems in the neonatal period.
An increase in the thickness and size of the placenta can also be the result of an abnormal pregnancy.