Tightness in legs during pregnancy
Aching, Painful, Or Heavy Legs During Pregnancy
Having aching legs during pregnancy is the icing on the cake of all of your physical ailments. But contrary to cake, heavy or aching legs are not something to be desired. While things like morning sickness and fatigue can be expected, when leg pain hits, it might catch you off guard.
To help make your leg troubles a little more bearable, we’ll give you some basic information and help you identify the signs, causes, and treatments for your aching and heavy legs.
Blood Circulation And Heavy Or Aching Legs During Pregnancy
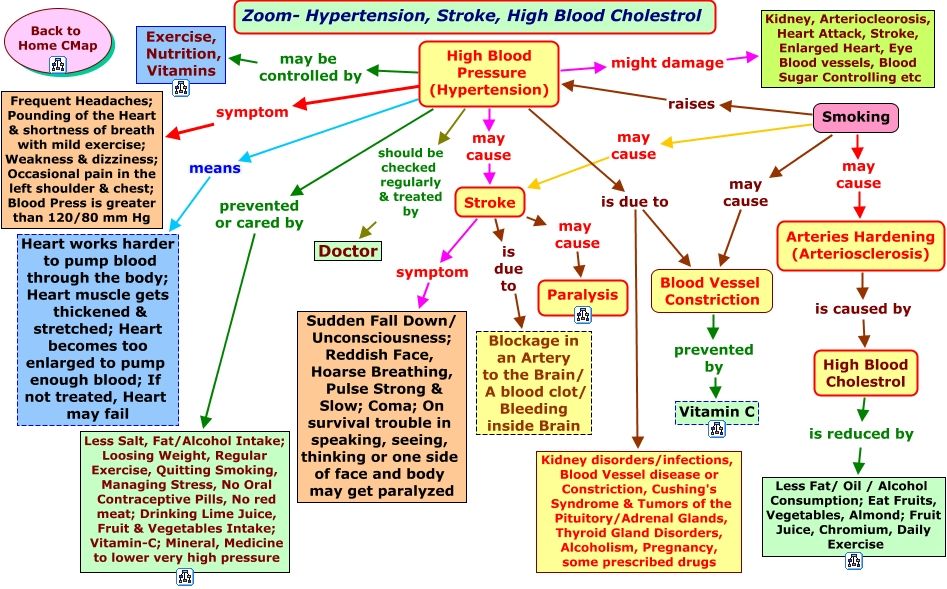
Pregnancy is a period during which the risk of circulatory disruptions becomes particularly high. These disruptions are the consequence of the related increase in body weight and hormonal changes, as seen below:
- As early as the first trimester, the increase in hormones creates circumstances in which the blood in the veins can easily stagnate, weakening vein walls and the firmness of blood vessels.
Estrogen levels can lead to inflammation (edema), and progesterone modifies the vein walls and vessel dilation.
- Throughout pregnancy, the increased volume of the uterus leads to increased pressure on the main vein responsible for returning blood to the heart.
- Finally, an increase in blood weight and volume (of 20% to 30%) contributes to increased pressure on the leg veins, which is doubled or tripled. The valves are separated further from each other by distension of the veins and no longer play their role of impeding blood return.
Blood circulation in the leg veins can be considerably disrupted. The symptoms vary significantly from woman to woman and pregnancy to pregnancy, ranging from simple discomfort to disabling pain.
After delivery, these impairments most often go away on their own within a few weeks.
The Role Of Veins And Vascular Insufficiency
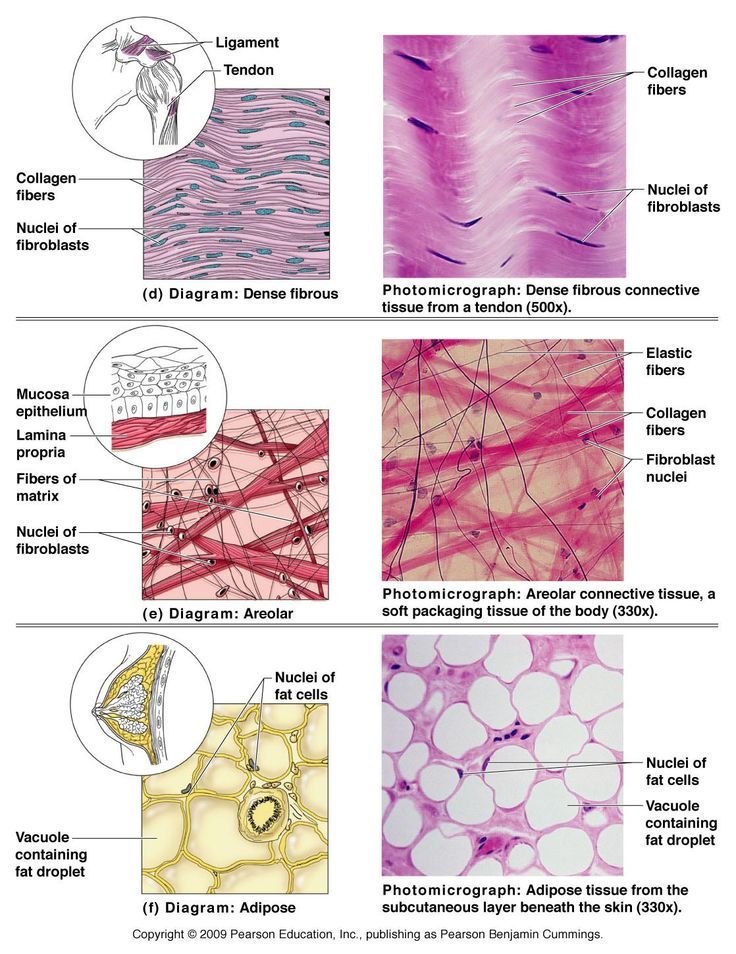
In their normal state, arteries supply the body’s tissues and organs with essential substances for their healthy functioning, such as oxygen. Veins, on the other hand, return blood to the heart.
Veins, on the other hand, return blood to the heart.
Blood pressure and the firmness of vein walls allow blood to flow from the lower to the upper portion of the legs. This blood flow through the veins and back up to the heart is called venous return.
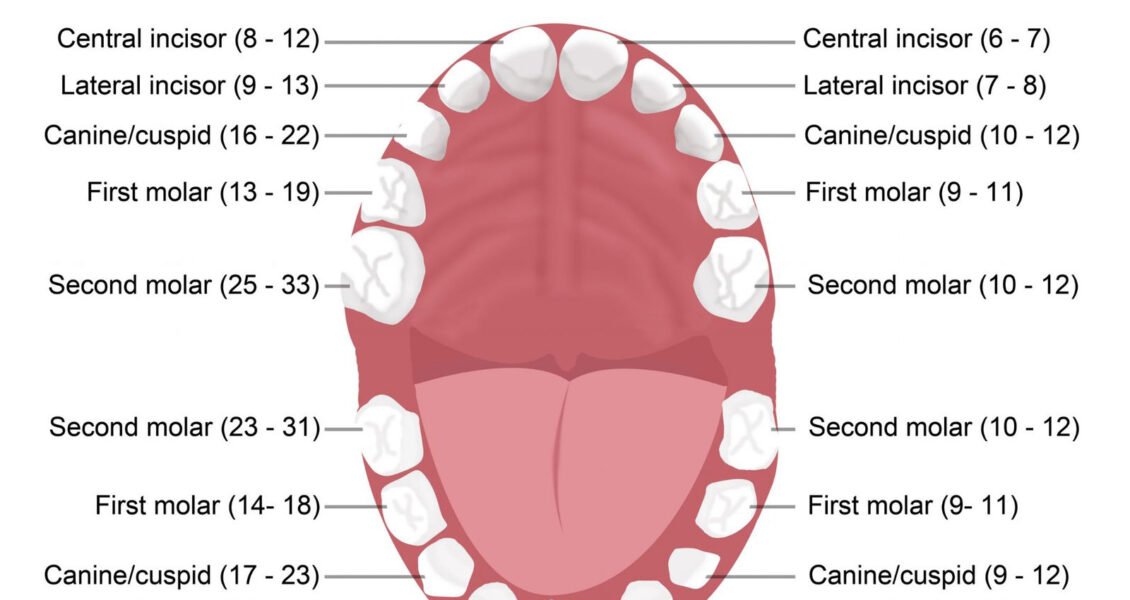
Valves, acting as small flaps, are positioned every 2 to 5 centimeters (0.8 to 2 inches) in the veins. These valves ensure that blood always flows in the same direction without ever “falling” back down the other way.
The calf muscles and compression of the instep also play a role in blood flow, particularly when walking.
Contributing Factors
Several factors can increase the risk of vascular insufficiency during pregnancy:
- Heredity: If your mom has had circulatory issues, you run a higher risk of experiencing them yourself.
- Working in a standing position and shuffling. Prolonged sitting can also disrupt venous return.
- A sedentary lifestyle and lack of physical exercise.
- Excess body weight prior to pregnancy, or significant weight gain during pregnancy.

- Previous pregnancies: The risk of venous insufficiency increases with the number of previous pregnancies carried to term — 23 percent for the first pregnancy and 31 percent for the fourth.
Healthy Habits
To avoid circulatory impairments during pregnancy, prevention is essential. If you need to, try to lose weight before getting pregnant and then limit your weight gain during pregnancy.
Here are some other healthy habits to help you avoid vascular insufficiency:
- Take walks or do light exercise, which boosts blood flow
- Wear shoes with a small heel that is neither too high nor too flat (3 to 4 cm or 1 to 1.5 inches)
- Avoid tight-fitting clothes and constricting socks
- If you suffer from any plantar arch problems, wear corrective insoles
- In certain cases, wearing compression stockings and taking venotonics may be recommended during pregnancy, starting in the second month
If you experience the sensation of heavy legs despite these measures, try some of these tips to help ease the discomfort:
- Raise your feet from the foot of your bed
- At the end of each shower, spray cold water over your legs in an upward motion from the ankles to the thighs
- Avoid sources of heat (prolonged exposure to the sun, high-temperature baths, underfloor heating, etc.
 )
) - Massage your legs every day, from the ankles to the knees, using a specific treatment cream to increase blood return and stimulate blood flow
Signs Of Heavy Or Aching Legs
Aching or heavy legs first appear as a sensation of discomfort, fatigue, and heaviness in the legs. These sensations can be the first sign of an actual circulation impairment alongside other characteristics, such as having pain:
- In the interior and posterior area of the calf that radiates up the leg toward the inside of the knee
- Most often felt towards the end of the day
- If you remain standing for a long time or if you are in contact with heat (summer temperatures, hot baths, hot-wax treatments, etc.)
- Increase as the pregnancy progresses
- Relieved by cold temperatures, winter climates, rest, elevation of the legs, and walking
- Accompanied by cramps at night, restlessness of the legs (painful discomfort that requires that one move one’s legs for relief), inflammation (edema of the ankles), varicosities, and even varicose veins
If you are experiencing any of these symptoms, talk about it with your doctor at your next visit. Your doctor may be able to prescribe a suitable treatment for you.
Your doctor may be able to prescribe a suitable treatment for you.
Causes Of Aching Or Heavy Legs
Like most expecting moms, you’re probably wondering what’s causing your aching or heavy legs. The sensation of heavy or aching legs is related to a loss of firmness and elasticity of the vein walls, which causes a slowing of blood circulation in the veins. Because of this, the veins dilate and blood pressure increases.
Valves — the small flaps that normally keep blood from flowing back down the leg veins — have difficulty maintaining this pressure and progressively become deficient.
Resistance to leaks weakens and blood stagnates in the lower portion of the veins, which further impairs vein walls. A vicious cycle takes hold.
On top of this, other factors could be causing your aching legs, such as:
- Nerve pressure: When your uterus expands, it puts pressure on certain nerves, which can trigger spasms and cause pain in your legs.
- Dehydration: If your body doesn’t get the right amount of hydration during your pregnancy — and it needs a lot! — it can really suffer.
 Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route!
Whether you’re dealing with morning sickness, stress, or cramps, drinking water can be the easy answer to all your pregnancy woes. When in doubt, take the water route! - Increase in your weight: Your legs are carrying around more weight than they’re used to. They’re having to work a little harder each day, so at the end of the day, they’re tired just like you.
- Swelling: Swelling is no stranger to pregnancy, especially in the heat. When your ankles and feet start to swell in the heat, as we’ve mentioned above, circulation gets restricted. This is when your legs start to ache and get heavy. (Note: If you notice consistent swelling in your legs and feet, or your leg starts to feel warm, reach out to your obstetrician right away.)
- Changes in your posture as your baby grows: Throughout stages of your pregnancy, your baby has taken different positions inside your uterus. This can take a toll on your body, especially your back.
 Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them.
Your posture starts to change throughout your pregnancy without you even noticing at times, but your legs are sure to take notice of the change. Your legs have to support you throughout these different stages, and it can impact them. - Fluid retention: Your growing uterus puts pressure on the veins that carry blood back from your lower body, which partially blocks blood flow. As a result, fluid remains in your legs and feet.
- Joint laxity: As we’ve discussed, when you’re carrying the extra weight from your precious baby, it’s a lot for your legs — but it’s also a lot for your joints. Your joints can easily become stressed from the added pressure. Your joints may seem a little loose and you might even waddle when you walk!
At-Home Treatment
Most often, your leg aches can be relieved at home. That’s something to shout about because we know leg aches can really be a Debby Downer as you wrap up your day!
Here are a few ideas to relieve your leg aches and heavy legs at the end of the day:
- Stretch your calf muscles by flexing and releasing each foot a few times
- Take short walks throughout the day to boost blood flow
- Avoid standing or sitting with your legs crossed for long periods
- Take a warm bath before bed (After getting out of a relaxing bath, don’t forget to apply Stretch Marks Oil to help limit the appearance of stretch marks! It leaves your skin restored, refreshed, and noticeably smoother.
 )
) - Massage your legs throughout the day and especially before bed (Try using our Body Firming Gel to give your legs a little massage. It hydrates your skin, giving it a firmer look and overall feel.)
- Take a calcium supplement (with the go-ahead from your doctor)
- Drink a glass of milk before bed
- Prop your legs up on a pillow (make sure your legs are elevated above your heart)
- Wear compression leggings or socks
- Increase your potassium intake
Medical Treatment
If your legs are painful and you see no improvement after trying the recommended measures outlined in the previous section, do not hesitate to see a doctor. They can prescribe suitable treatment for your condition.
Various methods — from medicinal to physical to surgical — may be considered, depending on the severity of your circulatory impairments:
- Compression via pantyhose, stockings, or socks is the basic treatment for anyone experiencing venous insufficiency.
 Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement.
Different models are available depending on the strength of compression necessary. Significant progress has been made in improving the esthetics of these garments. The cost of some of these compression methods may be eligible for Social Security reimbursement. - Venotonics have anti-inflammatory properties, stimulating muscle tone and protecting the elasticity of the vein walls. They must be taken for an extended period of time in order to be effective.
- Kinesitherapy and exercises to build up the leg muscle also have a role to play. Walking, swimming and biking are the best types of activity. Spa treatments, massages, and manual lymphatic drainage can also provide valuable relief.
- If varicose veins developed during your pregnancy and are still present after delivery, vein sclerotherapy or surgery may be considered. These techniques can be performed under local anesthesia, requiring neither an epidural nor general anesthesia, and the patient can go home the same day as treatment, or the following day.

A Comfortable Pregnancy
Aching and heavy legs can be caused by a variety of factors, as we listed above. Although these unpleasant sensations usually disappear on their own after delivery, they should not be taken lightly.
Heavy legs can turn into vascular pathologies that can sometimes be disabling. Monitor your heavy legs closely and give them the appropriate care from the very first signs to limit the risk of complications.
But keep in mind that most often, it’s not a cause for concern or harmful to your baby. Use at-home treatments to ease your leg aches and heavy legs. You may have to try a few before you find what works for you.
And while you’re at it, continue taking care of yourself during your pregnancy by treating your skin. Using the right products that have been clinically proven to effectively help expecting mothers, like our Stretch Marks Cream, will make for one comfortable pregnancy!
Leg Pain During Pregnancy: Exercises to Try
Leg Pain During Pregnancy: Exercises to TryMedically reviewed by Janine Kelbach, RNC-OB — By Natasha Freutel on February 24, 2016
While you await the arrival of your precious baby, you may be feeling new kinds of aches and pains. Leg and joint pain during the second or third trimester may be the result of added weight, changing body shape, and biomechanics. It can also be caused by fluid retention and joint laxity.
Leg and joint pain during the second or third trimester may be the result of added weight, changing body shape, and biomechanics. It can also be caused by fluid retention and joint laxity.
Pregnancy pain can have an impact on daily life and cause changes in sleep quantity and quality. Some common pregnancy aches include swollen and painful feet and legs, and calf cramps. Some women also report radiating pain down the back of the legs and hip pain.
Another common pregnancy symptom is swelling. Many pregnant women report swelling of the:
- face
- legs
- ankles
- feet
Mild swelling is a normal part of pregnancy. It happens because of the 50 percent increase in blood and bodily fluids needed to support the growing baby. But excessive swelling can be a sign of a more severe pregnancy complication. If you experience severe swelling, it’s important to be evaluated by a doctor.
Pregnancy back pain is widely studied, but there’s less research on hip, knee, and foot pain during pregnancy and postpartum. A study published in the Journal of Family Practice reports a high occurrence of low body pain among pregnant and postpartum women. It’s most likely related to changes in the way a pregnant woman moves due to a growing baby belly.
A study published in the Journal of Family Practice reports a high occurrence of low body pain among pregnant and postpartum women. It’s most likely related to changes in the way a pregnant woman moves due to a growing baby belly.
Try these exercises to help decrease swelling, pain, and discomfort during pregnancy.
Swollen feet and ankles are common during pregnancy. This simple exercise helps increase circulation and blood flow to the feet to decrease swelling and pain.
Equipment needed: none
Muscles worked: ankle dorsiflexors, plantarflexors
- Lie on a bed with your feet slightly elevated on a pillow.
- Begin by pulling your toes toward your face to flex your feet, then point your toes away from you.
- Repeat 10 times continuously.
- Perform 3 sets.
Some women suffer from sore calf muscles during pregnancy. This might be caused by weight gain, poor body mechanics, or improper footwear. Stretching can help promote relaxation of the muscles, leading to decreased pain.
Stretching can help promote relaxation of the muscles, leading to decreased pain.
Equipment needed: a wall
Muscles worked: gastrocnemius, soleus
- Stand to face a wall. Place both hands on the wall for support.
- Put one foot up against the wall with your toes pointing toward the ceiling.
- Lean toward the wall, keeping your leg straight until you feel a stretch in the back of your lower leg.
- Hold for 20-30 seconds. Repeat on other leg.
Tight hamstrings can cause low back pain and discomfort during pregnancy. This exercise helps stretch the hamstrings. It also activates and strengthens the muscles of the buttocks.
Equipment needed: none
Muscles worked: hamstrings, glutes
- Stand with your feet parallel, hip-width apart.
- Put your hands behind your head and stand up tall, keeping your chest wide.
- Keep your legs relatively straight with a slight bend in your knees.
 Bend at the hips, moving them back as you lower yourself toward parallel. Bend until you feel a stretch in the back of your legs. Try to keep your back in a straight line.
Bend at the hips, moving them back as you lower yourself toward parallel. Bend until you feel a stretch in the back of your legs. Try to keep your back in a straight line. - Move slowly through this movement 10 times.
- Perform 3 sets.
This exercise can increase strength and stability in the muscles of the lower back and core. It also works the quadriceps, the important muscles that support the ligaments of the knee.
Equipment needed: exercise ball
Muscles worked: gluteus maximus, hamstrings, deep core muscles
- Stand against a wall with an exercise ball positioned between your midback and the wall.
- Place your feet far enough away from the wall so that when you lower down into a squat, your knees can bend to 90 degrees. Having your feet too close to the wall will put stress on the knee joint. Feet should be parallel and a little wider than hip-width apart.
- Lower your body down into a sitting position while rolling the ball up your back.

- Hold for 1 second, return to starting position. Repeat 10 times.
Sciatic pain is common during pregnancy. It can cause shooting or aching pain down the buttocks, back of the leg, and foot. Foam rolling is a great way to soothe and relax tight muscles that may be contributing to increased pain.
Equipment needed: foam roller
Muscles worked: hamstrings, calf muscles, glutes, piriformis
- Place a foam roller on the ground.
- Sit on the foam roller, supporting yourself with your hands behind you.
- Cross one foot over the other knee in a figure 4 position.
- Slowly move your buttocks back and forth over the foam roller until you find a tender spot.
- Continue this movement over the tender area for 30-60 seconds.
- Try rolling the foam roller down the back of your upper leg until you find another tender area.
- Repeat on other side.
Exercises and stretching can have a positive effect on mobility during pregnancy. They can also help decrease pain and dysfunction. The 2002 guidelines for physical activity during pregnancy recommend regular exercise for its overall health benefits to both mom and baby.
They can also help decrease pain and dysfunction. The 2002 guidelines for physical activity during pregnancy recommend regular exercise for its overall health benefits to both mom and baby.
Always see your doctor before starting an exercise program to make sure it’s safe. Discontinue exercise and seek medical help if you have any of the following symptoms:
- vaginal bleeding
- dyspnoea before exertion
- dizziness
- headache
- chest pain
- muscle weakness
- calf pain or swelling
- preterm labor
- decreased fetal movement
- amniotic fluid leakage
Calf or leg pain can be a symptom of a more serious condition like a blood clot or thrombosis. Seek immediate medical attention if you have pain accompanied by redness, warmth, or swelling in the calf.
Share on Pinterest
Last medically reviewed on February 24, 2016
- Parenthood
- Pregnancy
- Pregnancy Health
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Artal, R., O’Toole, M., & White, S. (2003). Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. British Journal of Sports Medicine, 37(1), 6-12
doi.org/10.1136/bjsm.37.1.6 - Dumas, G. A., & Reid, J. G. (1997). Laxity of knee cruciate ligaments during pregnancy. The Journal of Orthopaedic and Sports Physical Therapy, 26(1), 2-6
doi.org/10.2519/jospt.1997.26.1.2 - Swelling During Pregnancy. (2015)
americanpregnancy.org/pregnancy-health/swelling-during-pregnancy/ - Vullo, V. J., Richardson, J. K., & Hurvitz, E. A. (1996). Hip, knee, and foot pain during pregnancy and the postpartum period. The Journal of Family Practice, 43(1), 63–68
ncbi. nlm.nih.gov/pubmed/8691182
nlm.nih.gov/pubmed/8691182
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Share this article
Medically reviewed by Janine Kelbach, RNC-OB — By Natasha Freutel on February 24, 2016
related stories
5 Stretches for Tailbone Pain During Pregnancy
Sciatica During Pregnancy: Symptoms, Causes, Treatments
Pregnancy Yoga Stretches for Back, Hips, and Legs
5 Ways to Perform Squats Safely During Pregnancy
Pregnancy Sciatica: 5 Natural Ways to Find Pain Relief Without Drugs
Read this next
5 Stretches for Tailbone Pain During Pregnancy
Medically reviewed by Janine Kelbach, RNC-OB
Many pregnant women experience uncomfortable tailbone pain. This gentle stretching routine will help ease some of the discomfort.
READ MORE
Sciatica During Pregnancy: Symptoms, Causes, Treatments
Medically reviewed by Beth Holloway, RN, MEd
Many pregnant women experience sciatic pain.
 Here's a look at the causes, symptoms, and ways to find relief.
Here's a look at the causes, symptoms, and ways to find relief. READ MORE
Pregnancy Yoga Stretches for Back, Hips, and Legs
Medically reviewed by Peggy Pletcher, M.S., R.D., L.D., CDE
Practicing yoga during pregnancy can help ease some of your aches and pains. Follow this gentle routine to stretch and relax your muscles.
READ MORE
5 Ways to Perform Squats Safely During Pregnancy
Medically reviewed by Peggy Pletcher, M.S., R.D., L.D., CDE
Performing squat exercises during pregnancy can be beneficial to both mom and baby. Here are five safe variations to try.
READ MORE
Pregnancy Sciatica: 5 Natural Ways to Find Pain Relief Without Drugs
Medically reviewed by Michael Weber, MD
A baby pushing on your bladder is uncomfortable enough without the added pain of sciatica.
 Here are some ways to find relief.
Here are some ways to find relief.READ MORE
Your Guide to a Pregnancy-Safe Skin Care Routine
When you're expecting, pregnancy-safe skin care can help ensure the health of you and your baby. We'll tell you what to avoid — and some good…
READ MORE
Can Ectopic Pregnancy Be Diagnosed With Ultrasound?
Medically reviewed by Valinda Riggins Nwadike, MD, MPH
Ectopic pregnancy is a serious condition that requires accurate and swift diagnosis. Ultrasound for ectopic pregnancy diagnosis is just one tool your…
READ MORE
Is It Safe to Consume Flaxseeds During Pregnancy?
Given the inconclusive and conflicting stances about eating flaxseeds during pregnancy, it might be better to err on the side of caution.
READ MORE
Pregnancy After Miscarriage: Answers to Your Questions
Medically reviewed by Amanda Kallen, MD
Getting pregnant after a miscarriage can be an emotional experience, filled with joy but also anxiety and guilt.
 Learn more about pregnancy after…
Learn more about pregnancy after…READ MORE
What Is a Nurse Midwife and How to Tell If They Are Right for You
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
A nurse midwife is a nurse with education, training, and certification to provide prenatal, delivery, and women's care.
READ MORE
Leg pain during pregnancy: causes and how to get rid of it
Feet in pregnant women hurt for various reasons. Since there is a considerable load on the legs during pregnancy, this is not surprising. Just don't ignore the pain. Sometimes, if a woman feels pain in her legs, we can talk about pathology.
We tell you what pain in the legs during pregnancy can be associated with and what to do to alleviate the symptoms. nine0003
Why my feet hurt during pregnancy
During pregnancy, the center of gravity usually shifts, which creates an excessive load on the legs. Therefore, many women who are carrying a child experience pain in their feet. In general, during pregnancy, a woman's body is rebuilt, so pain can also occur for other reasons that are also not associated with the development of diseases.
Therefore, many women who are carrying a child experience pain in their feet. In general, during pregnancy, a woman's body is rebuilt, so pain can also occur for other reasons that are also not associated with the development of diseases.
Causes of leg pain in pregnant women
The most common causes of foot pain in pregnant women include: nine0003
-
Natural increase in body weight;
-
The shift in the center of gravity, which increases the load on the feet;
-
Excessive accumulation of fluid in the body can cause swelling and, as a result, throbbing pain;
-
Aching pain, swelling after walking or standing for a long time - these symptoms appear in women prone to varicose veins; nine0003
-
Cramping that cramps the legs or only the feet can occur due to an increased concentration of progesterone in the blood, as well as due to iron and calcium deficiency.
Consider the cases when the feet hurt during pregnancy due to existing diseases.
Flat feet
If flat feet have already been, then during pregnancy, if the disease is not treated, it only gets worse. There are cases when a woman had the first stage of flat feet, and in the last trimester - already the third. Usually, transverse flat feet are more acutely tolerated. Its symptoms: nine0003
-
Burning in the feet;
-
By the end of the day, the legs are very tired, they may swell;
-
In the evening there are cramps in the area of calves and shins, which are accompanied by pain in the feet;
-
Pain in the area of the kneecaps, pelvis and back - these symptoms appear when flat feet are neglected; nine0003
-
Calluses and growth that affects the base of the thumb;
-
Hammer toe deformity.
It is important to diagnose the transverse flatfoot of the foot in time. Usually orthopedic traumatologists deal with this issue.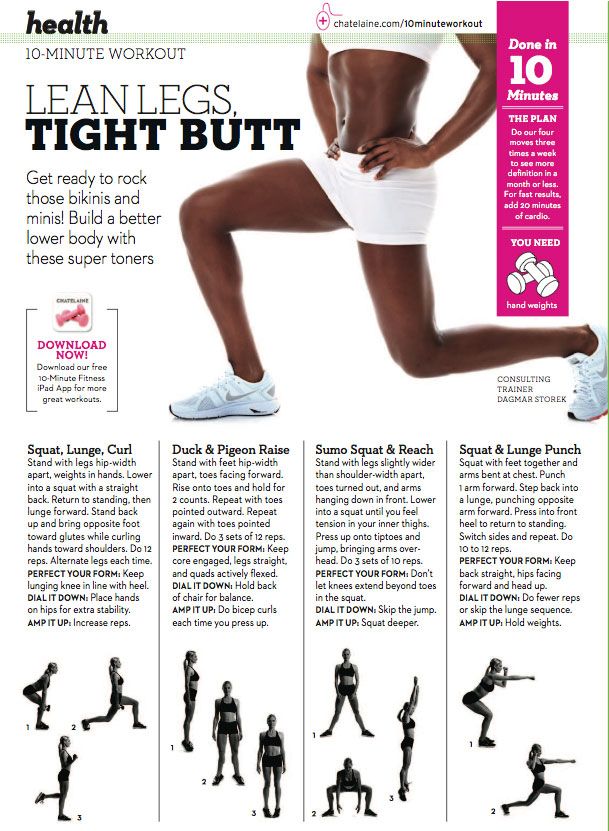 To diagnose the disease, the doctor sends an x-ray. Pregnancy is not an absolute contraindication for x-rays. Radiation should be avoided only in the first three months of pregnancy. Before the procedure, be sure to warn the doctor about your situation. nine0003
To diagnose the disease, the doctor sends an x-ray. Pregnancy is not an absolute contraindication for x-rays. Radiation should be avoided only in the first three months of pregnancy. Before the procedure, be sure to warn the doctor about your situation. nine0003
Only after studying the radiographs, the doctor can confirm the diagnosis. Further steps will depend entirely on the stage of the disease. At the initial stages, the disease is cured by conservative methods, in advanced cases, surgical intervention is required.
Conservative treatments include:
-
treatment with medications if there is inflammation;
- nine0002 wearing orthopedic insoles and other devices;
-
physiotherapy;
-
massage;
-
exercise therapy.
In the fight against flat feet, orthopedic insoles, which are designed for pregnant women, have proven themselves well. They help to evenly distribute the load on the legs of women. nine0003
They help to evenly distribute the load on the legs of women. nine0003
Varicose veins
Even if a woman has never suffered from this disease, there is a risk that pregnancy will worsen the condition of the vessels.
Since mother and baby have a common circulatory system, varicose veins can provoke oxygen starvation in the fetus. The fact is that it is with the mother's blood that the child receives all the necessary substances to maintain his life.
It is not difficult to recognize varicose veins on your own. The most obvious signs that can be seen with the naked eye are pronounced vascular networks. It is worth making an appointment with a doctor if you have symptoms such as: nine0003
-
Aching pain in the legs, especially after exercise;
-
Fatigue and heaviness in the legs at the end of the day;
-
tingling, itching and burning;
-
Numbness of limbs or cramps.
The treatment of the disease is carried out by a phlebologist (vascular surgeon). nine0003
Is it possible to do foot massage during pregnancy?
If the attending specialist does not see any contraindications for massage, then the procedure will only benefit. Foot massage during pregnancy will help not only alleviate the condition of the legs, but also improve the mood of the expectant mother. Massage has a positive effect on the emotional state of the mother, and therefore on the unborn child.
How to get rid of foot pain
Often, with pain in the legs, a woman can help herself. These recommendations will help get rid of leg pain or at least reduce it: nine0003
-
During pregnancy, aching and tired feet come to the rescue in the evening foot baths. Water should be at room temperature. It is also useful to rinse the feet with cold water;
-
It is advisable to sleep on the left side - on the right is the inferior vena cava, which carries the bulk of the blood, so it is better to remove the load from it;
-
A contrast shower helps to get rid of pain in the legs - this procedure will also strengthen the walls of blood vessels; nine0003
To avoid unpleasant pain in the legs, it is also important to follow preventive measures:
-
Drink enough water.
 Edema appears when the body is dehydrated, and not vice versa;
Edema appears when the body is dehydrated, and not vice versa; -
Motion. To improve blood flow, it is useful to move and do light exercise. Walking is the best activity for pregnant women. When driving, it is important to take regular breaks to stretch your legs; nine0003
-
Leg lift. If you have to sit for a long time, it is advisable to raise your legs more often. To do this, you can put a stand or a small bench near you;
-
Balanced diet. This applies mainly to the consumption of salt, since it is it that retains water in the body. In general, the diet should be varied, with sufficient protein;
nine0016 -
Avoidance of heavy workloads. Long stay on your feet, lifting weights and any physical labor - all this negatively affects the health of blood vessels during pregnancy.
 You should also pay attention to the position of the body. For example, a pose in which the legs are crossed harms the vessels; nine0003
You should also pay attention to the position of the body. For example, a pose in which the legs are crossed harms the vessels; nine0003 -
Correct posture. With proper posture, the load on the legs is distributed evenly. It is important to ensure that the lower back does not bend too much or the body does not lean back too much;
-
Comfortable shoes and clothes. Clothing or shoes that are tight on the body can block blood flow. Therefore, it is not recommended to wear socks with tight elastic bands that leave marks on the body, and shoes that are too narrow and short; nine0003
-
Be careful with sunburn. If there is a tendency to varicose veins, you should not stay under the sun for a long time - ultraviolet rays weaken blood vessels.
Weight control. Almost all women gain weight during pregnancy. It is only important to ensure that the “increase” fits into the norm, since excess weight provokes swelling;
If you follow these simple recommendations, you can minimize the pain in the legs during pregnancy. If you suspect flat feet, you can always contact our orthopedic center. A specialist doctor will diagnose and, in case of illness, prescribe an effective treatment regimen. nine0003
A specialist doctor will diagnose and, in case of illness, prescribe an effective treatment regimen. nine0003
Preeclampsia and pregnancy | Ida-Tallinna Keskaigla
Preeclampsia and pregnancy
The purpose of this information leaflet is to provide the patient with information about the nature, occurrence, risk factors, symptoms and treatment of preeclampsia.
What is preeclampsia?
Pre-eclampsia is a disease that occurs during pregnancy and is characterized by high blood pressure and protein in the urine. Preeclampsia is one of the most common complications of pregnancy. Epilepsy-like seizures occur in severe preeclampsia and are life-threatening. nine0003
What symptoms may indicate the development of preeclampsia?
High blood pressure - blood pressure values are 140/90 mmHg. Art. or higher. If systolic (upper) or diastolic (lower) blood pressure rises by 30 mm Hg.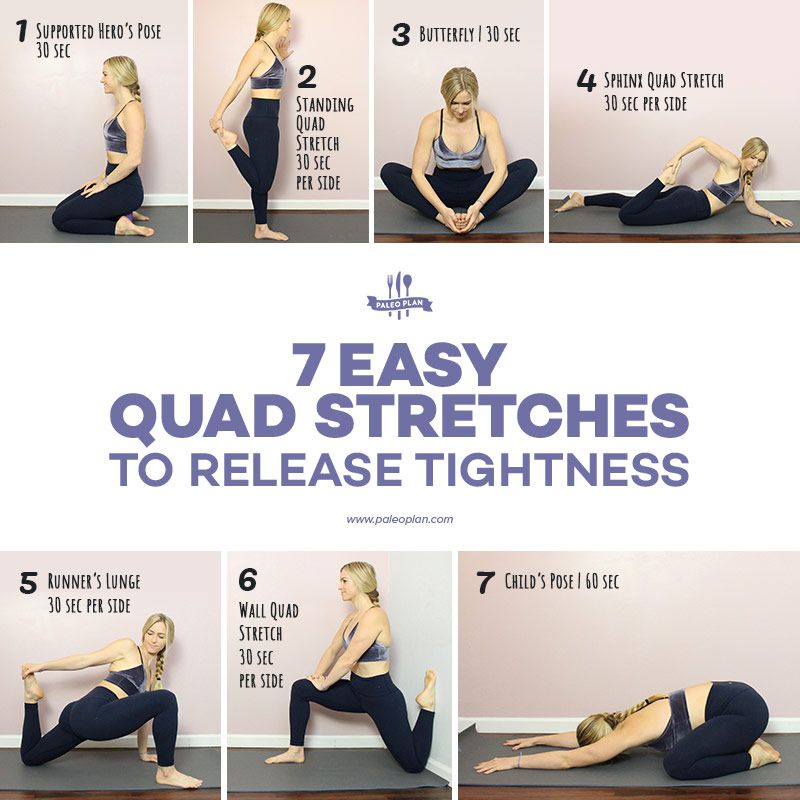 Art. or more, then such an increase cannot be ignored.
Art. or more, then such an increase cannot be ignored.
Protein in urine - 300 mg in urine collected over 24 hours, or +1 value on a rapid test.
Swelling of the arms, legs or face , especially under the eyes or if the skin is pitted when pressed. Edema can occur in all pregnant women and is generally harmless, but rapidly developing edema should be taken into account.
Headache that does not improve after taking pain medication.
Visual disturbances - double vision or blurred vision, dots or flashes before the eyes, auras.
Nausea or pain in the upper abdomen - These symptoms are often mistaken for indigestion or gallbladder pain. Nausea in the second half of pregnancy is not normal.
Rapid weight gain - 2 kg or more per week.
As a rule, there is a mild course of the disease that occurs at the end of pregnancy and has a good prognosis.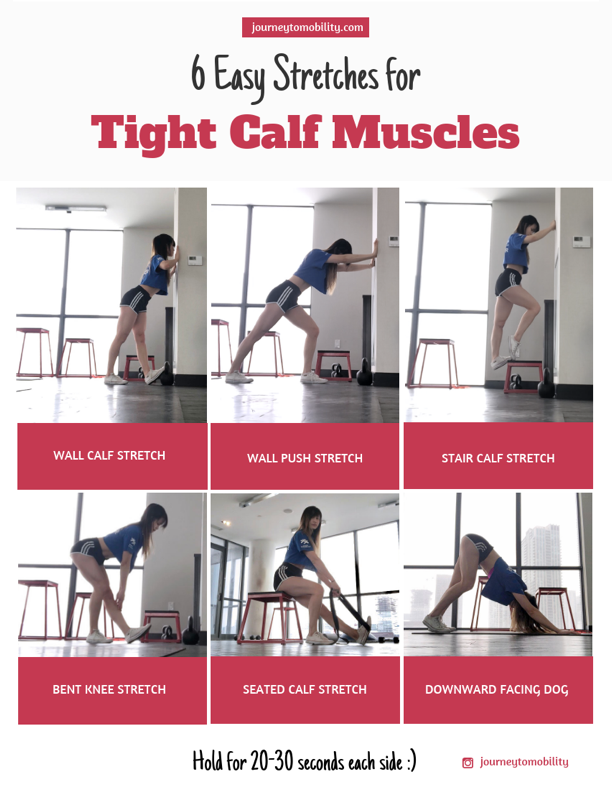 Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance. nine0003
Sometimes, preeclampsia can worsen quickly and be dangerous to both mother and fetus. In such cases, rapid diagnosis and careful monitoring of the mother and child are of paramount importance. nine0003
Unfortunately, most women show symptoms in the final stages of the disease. If you experience any of the above symptoms, you should contact your midwife, gynecologist, or the Women's Clinic emergency department.
Is preeclampsia called toxemia of pregnancy?
Previously, pre-eclampsia was indeed called toxicosis, or toxemia, since it was believed that the cause of the disease was toxins, that is, poisons in the blood of a pregnant woman.
What is the difference between preeclampsia and gestational hypertension?
Pregnancy hypertension is an increase in blood pressure above normal after the 20th week of pregnancy. With hypertension of pregnant women, protein in the urine is not observed.
What is HELLP syndrome?
HELLP syndrome is one of the most severe forms of preeclampsia. HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold. nine0003
HELLP syndrome is rare and sometimes develops before symptoms of preeclampsia appear. Sometimes the syndrome is difficult to diagnose, as the symptoms resemble gallbladder colic or a cold. nine0003
When does preeclampsia occur?
Preeclampsia usually occurs after the 20th week of pregnancy. As a rule, preeclampsia goes away after delivery, but complications can occur up to six weeks after delivery, during which careful monitoring of the condition is necessary. If by the sixth week after birth, blood pressure does not return to normal, then you need to contact a cardiologist, who will begin treatment against hypertension.
What is the cause of preeclampsia? nine0200
The causes of the disease are still not clear, there are only unproven hypotheses.
How does the disease affect pregnant women and pregnancy?
Most preeclamptic pregnancies have a favorable outcome and a healthy baby is born. However, the disease is very serious and is one of the most common causes of death of the child and mother. Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death. nine0003
Preeclampsia affects a woman's kidneys, liver, and other vital organs, and if left untreated, it can cause seizures (eclampsia), cerebral hemorrhage, multiple organ failure, and death. nine0003
How does the disease affect the fetus?
In preeclampsia, the fetus does not receive enough oxygen and nutrients to grow, and intrauterine growth retardation may occur. In addition, the placenta may separate from the uterine wall before the baby is born. Since the only treatment for preeclampsia is childbirth, sometimes a pregnancy has to be terminated prematurely. Until the 34th week of pregnancy, the lungs of the fetus have not yet matured, and steroid hormones are injected intramuscularly into the pregnant woman to prepare his lungs. In addition to the immaturity of the lungs, the health of a premature baby is threatened by many other diseases. nine0003
Who is at risk of developing preeclampsia?
Preeclampsia occurs in approximately 8% of pregnant women, many of whom have no known risk factors.
What are the risk factors for preeclampsia?
Patient-related risk factors
- First pregnancy
- Pre-eclampsia during a previous pregnancy
- Age over 40 or under 18
- Pre-pregnancy high blood pressure
- Diabetes before or during pregnancy
- Multiple pregnancy
- Overweight (BMI> 30)
- Systemic lupus erythematosus or other autoimmune disease
- Polycystic ovary syndrome
- Long interval between two pregnancies
Risk factors associated with the patient's family
- Pre-eclampsia in the mother's or father's family
- Parental high blood pressure or heart disease
- Diabetes mellitus
What is the prevention and treatment of preeclampsia
The first trimester screening, or Oscar test, in addition to the most common chromosomal disorders, also calculates the risk of preeclampsia. In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0003
In case of high risk, pregnant women are advised to take aspirin (acetylsalicylic acid) at a dose of 150 mg in the evenings until the 36th week of pregnancy. This helps reduce the chance of preeclampsia by the 34th week of pregnancy by up to 80%. nine0003
Childbirth is the only treatment for preeclampsia. Sometimes a child can be born naturally, but sometimes, if the disease is very acute, an emergency caesarean section is necessary. The best time to have a baby is after the 37th week of pregnancy. Bed rest, medications, and, if necessary, hospitalization can sometimes help bring the condition under control and prolong the pregnancy. Often, a doctor will refer a woman with preeclampsia to the hospital for observation, as the condition of the fetus and pregnant woman may suddenly worsen. nine0003
Does bed rest help?
Bed rest is sometimes sufficient to control mild preeclampsia. In this case, the patient often visits a doctor who measures blood pressure, does blood and urine tests, and monitors the course of the disease. The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
The condition of the fetus is also often examined using a cardiotocogram (CTG) and ultrasound.
Are medications used to treat preeclampsia?
High blood pressure sometimes requires medication. The medications used have few side effects, the drugs prescribed do not have much effect on the fetus, but are very important in the treatment of maternal high blood pressure. nine0003
Seizures are a rare but very serious complication of preeclampsia. Magnesium sulfate is sometimes given intravenously to prevent seizures in a pregnant woman with preeclampsia both during and after childbirth. It is safe for the fetus, but the mother may experience side effects such as hot flashes, sweating, thirst, visual disturbances, mild confusion, muscle weakness, and shortness of breath. All these side effects disappear when the drug is discontinued.
Can preeclampsia recur? nine0200
Preeclampsia does not necessarily recur in the next pregnancy, but the main risk factor for preeclampsia is the presence of preeclampsia in a previous pregnancy(s).