Care plan for preeclampsia
6 Preeclampsia & Gestational Hypertensive Disorders Nursing Care Plans
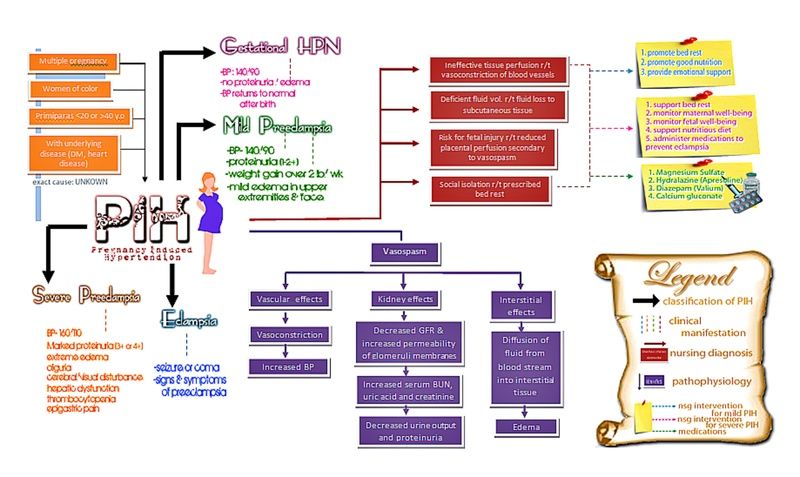
Hypertensive disorders of pregnancy (also known as pregnancy-associated hypertensive disorders, pregnancy induced hypertension) are the most common complications that occur during pregnancy and are a major cause of maternal and fetal morbidity and mortality. These disorders include gestational hypertension, preeclampsia, eclampsia, chronic hypertension, and chronic hypertension with superimposed preeclampsia. If left untreated, preeclampsia can lead to a life-threatening complication called HELLP (hemolysis, elevated liver enzymes, low platelet count) syndrome. It is estimated that preeclampsia alone complicates 2-8% of pregnancies globally.
Hypertensive disorders in pregnancy include five categories of hypertension and are defined as such by the American College of Obstetricians and Gynecologists (ACOG):
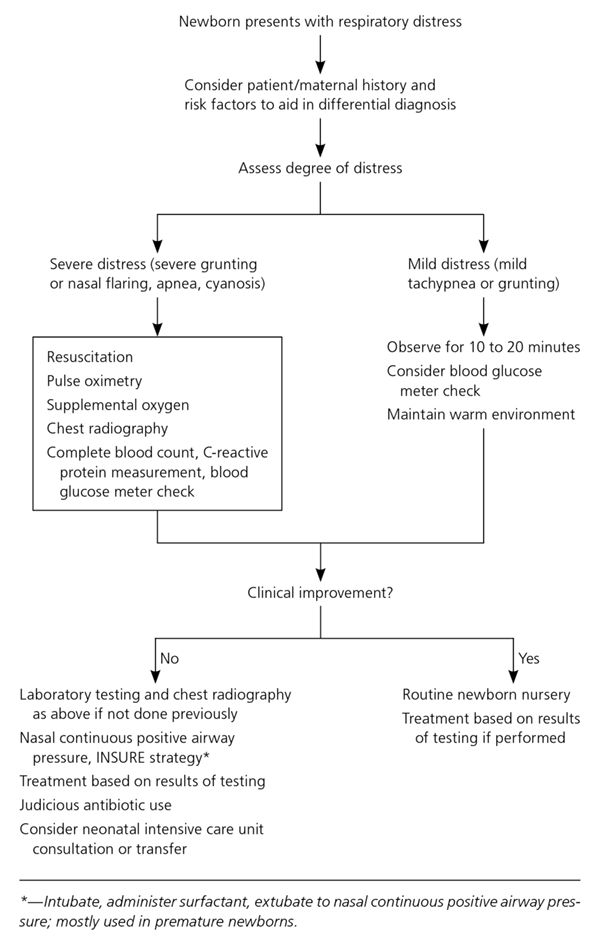
Nursing care planning and management for pregnant clients with hypertensive disorders or preeclampsia involve early detection, thorough assessment, and prompt treatment of preeclampsia. Another priority is to ensure the mother’s safety and deliver a healthy newborn as close to a full term as possible.
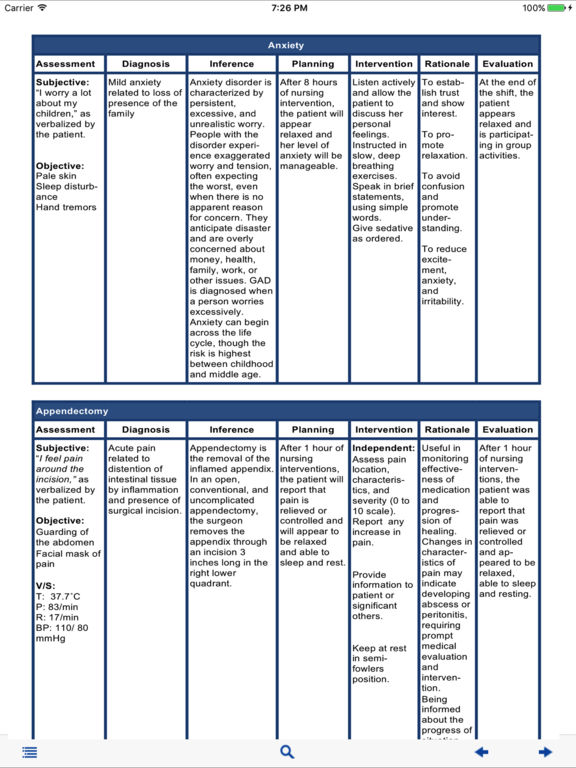
Here are six nursing diagnoses for your nursing care plans for pregnant patients with hypertensive disorders, focusing on managing clients with preeclampsia.
Decreased Cardiac OutputA decrease in circulating blood volume due to the shifting of fluid from the intravascular to the interstitial spaces occurs in a pregnant client with a hypertensive disorder due to the decrease of the circulating blood volume and the total vascular volume and an increase in the systemic vascular resistance, the heart rate decreases as well as the stroke volume. These mechanisms lead to a decrease in cardiac output seen among clients with hypertensive disorders in pregnancy.
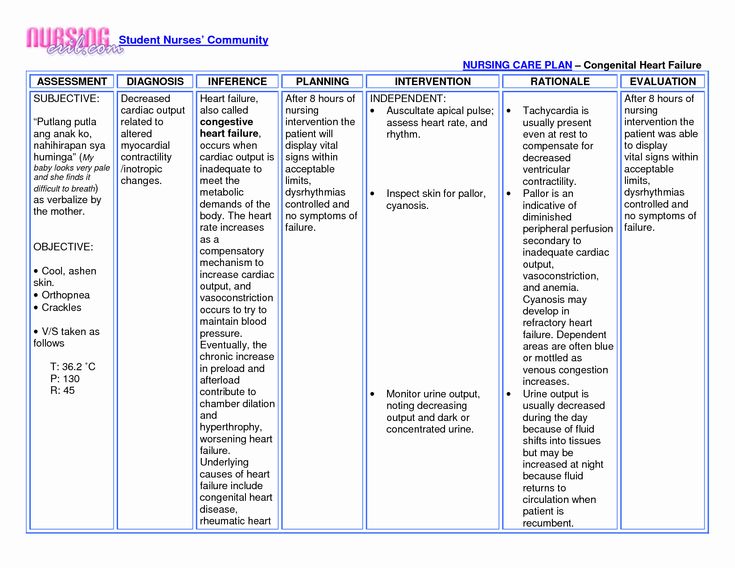
Nursing Diagnosis- Decreased Cardiac Output
- Decreased venous return
- Increased systemic vascular resistance
- Change in blood pressure/hemodynamic readings
- Diminished peripheral pulses
- Tachycardia
- Edema
- Shortness of breath/dyspnea
- Alteration in mental status
- Decreased urine output
- The client remains normotensive throughout the remainder of the pregnancy.
- The client reports absence and/or decreased episodes of dyspnea.
- The client alters activity level as the condition warrants.
1. Assess blood pressure and pulse every one (1) hour or as indicated.
Accurate measurement of blood pressure is essential for the early detection of hypertensive disorders. Hypertension is defined as a systolic blood pressure greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg. Blood pressure may be elevated because of the increase in systemic vascular resistance whereas decreased cardiac output may also be reflected by diminished peripheral pulses. Rising blood pressure indicates the progression of preeclampsia. Use a consistent and standardized method when taking blood pressure measurements to maintain accuracy.
2. Assess the mean arterial pressure (MAP) at 11-13 and 20-24 weeks gestation. A pressure of 90 mm Hg is considered predictive of preeclampsia.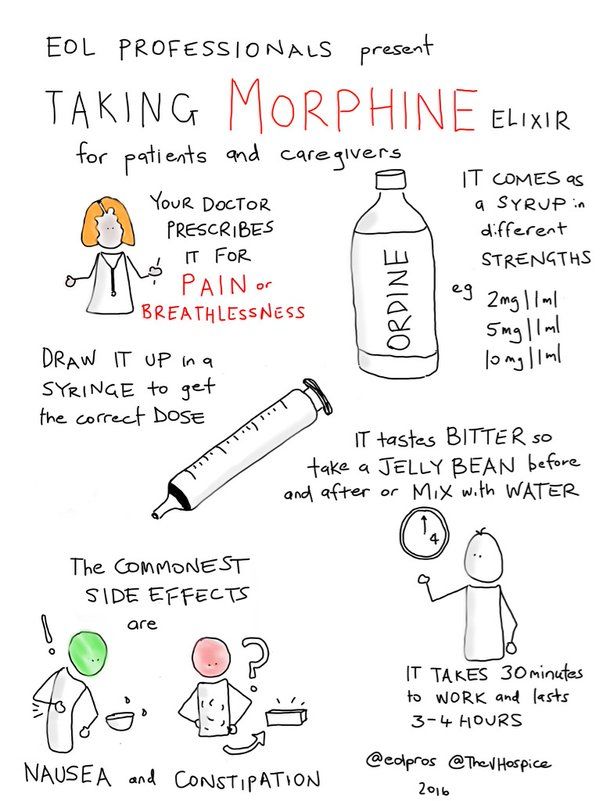
Mean arterial pressure (MAP) is the average arterial pressure throughout one cardiac cycle and is influenced by cardiac output and systemic vascular resistance. MAP prediction is best when measured during 11-13 weeks and at 20-24 weeks than at only one of these gestational ranges. MAP is increased from the first trimester in pregnancies developing preeclampsia (Gallo et al., 2014). Women with early-onset preeclampsia have higher mean arterial blood pressure levels at 20 weeks of gestation (Mayrink et al., 2019).
3. Assess for crackles, wheezes, and dyspnea; note respiratory rate/effort. Note client snoring.
Pulmonary edema may transpire with modification in peripheral vascular resistance and a drop in plasma colloid osmotic pressure. Fluid from the intravascular spaces shifts to the interstitial spaces, depleting the circulating blood volume but overwhelming the important organs of the body, especially the lungs. Pregnancy-onset snoring may also be a risk factor for developing gestational hypertension and preeclampsia (O’Brien et al.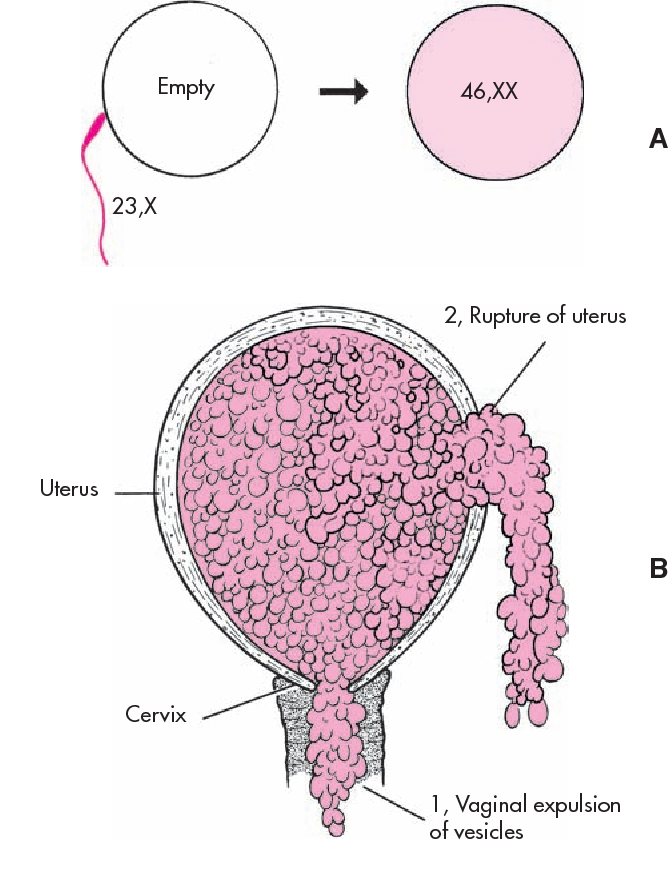 , 2012).
, 2012).
4. Auscultate for the apical pulse and assess the client’s heart rate and rhythm.
Tachycardia may be present when the body compensates for the decrease in circulating volume that can hardly reach the peripheries and distant tissues.
5. Assess the client’s neurological status.
Decreased cardiac output can precipitate alternations in the sensorium due to inadequate cerebral perfusion. Neurologic complications associated with preeclampsia may also manifest. These symptoms include cerebral edema, hemorrhage, irritability, headaches, hyperreflexia, seizures.
6. Assess the client for visual disturbances.
Alteration in the sensorium may indicate inadequate cerebral perfusion secondary to decreased cardiac output. Vision changes are due to arteriolar vasospasms and decreased blood circulation to the retina. These symptoms may include dimming of vision, blind or dark spots in the visual speed, blurring of vision, double vision.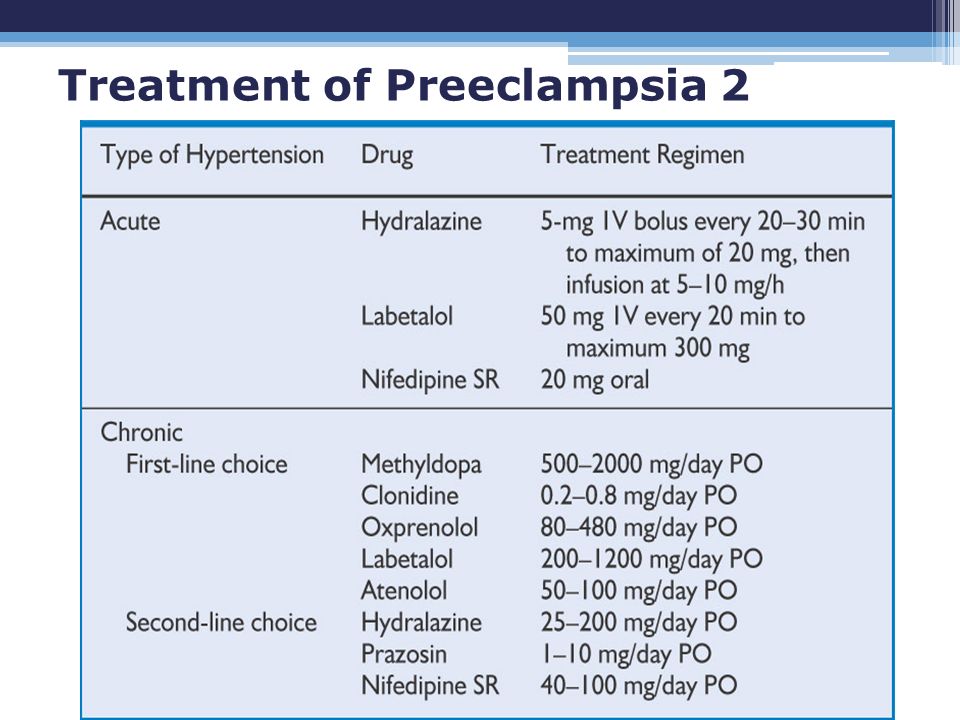
7. Assess the client for indications for an earlier delivery.
Worsening preeclampsia that may progress to eclampsia warrants the need for an emergency early delivery. The fetal blood supply can be cut off, resulting in fetal distress and ultimately fetal death if delivery is not hastened (Sinkey et al., 2020; Espinoza 2012). These symptoms include uncontrolled severe-range blood pressure, refractory headaches, upper abdominal pain, visual disturbances, stroke.
8. Monitor and measure the client’s urine output as per protocol. Maintain strict intake and output.
In preeclampsia, the kidneys respond to reduced cardiac output by retaining water and sodium. Intrarenal vasospasms cause oliguria in severe preeclampsia due to a reduction in glomerular filtration rate. Contraction of the intravascular space secondary to vasospasms worsens renal sodium and water retention (ACOG, 2020).
9. Monitor and measure the client’s 24-hour urine for proteinuria.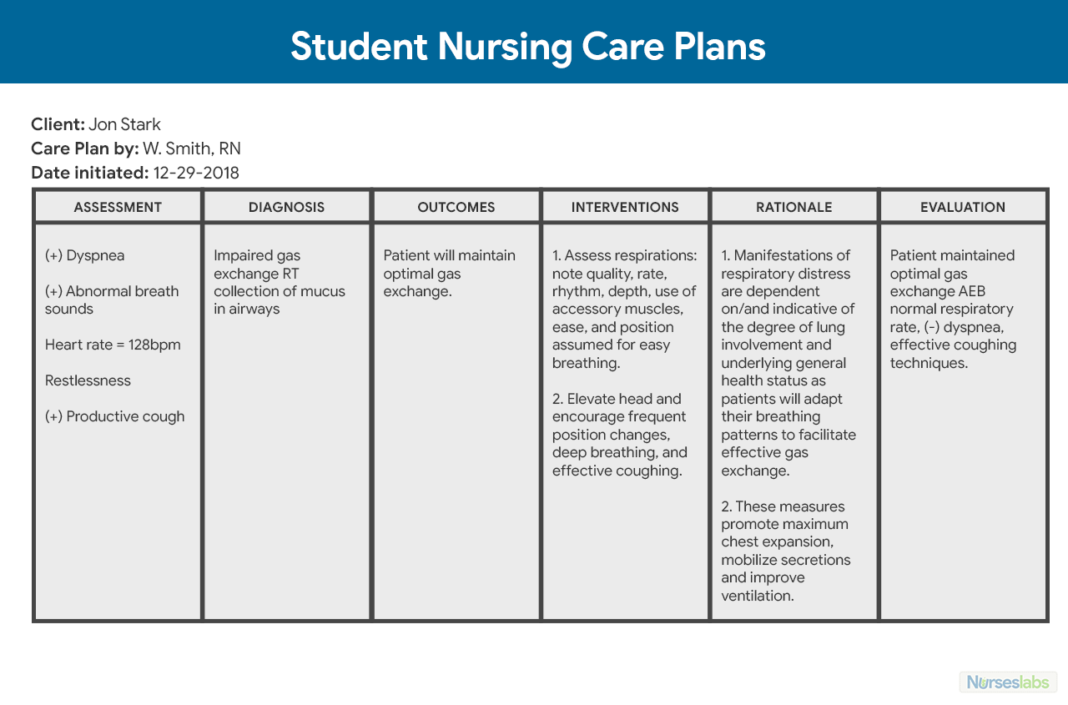
Proteinuria is ideally determined by the evaluation of a 24-hour urine collection. However, current guidelines state that massive proteinuria is not considered a severe feature of preeclampsia. Reduced kidney perfusion causes renal deterioration and damages glomerular endothelial cells allowing protein molecules to pass into the urine, causing proteinuria. In some instances where it may be difficult to collect a 24-hour urine sample, preeclampsia may be diagnosed as hypertension with either thrombocytopenia, renal insufficiency, impaired liver function, pulmonary edema.
1. Provide frequent rest periods with bed rest. Restrict activity rather than instituting complete bed rest.
Improves venous return, cardiac output, and renal-placental perfusion. Help the client understand the importance of reduced activity and frequent rest periods and plan ways to manage them. Activity diverts blood from the placenta, reducing the infant’s oxygen supply.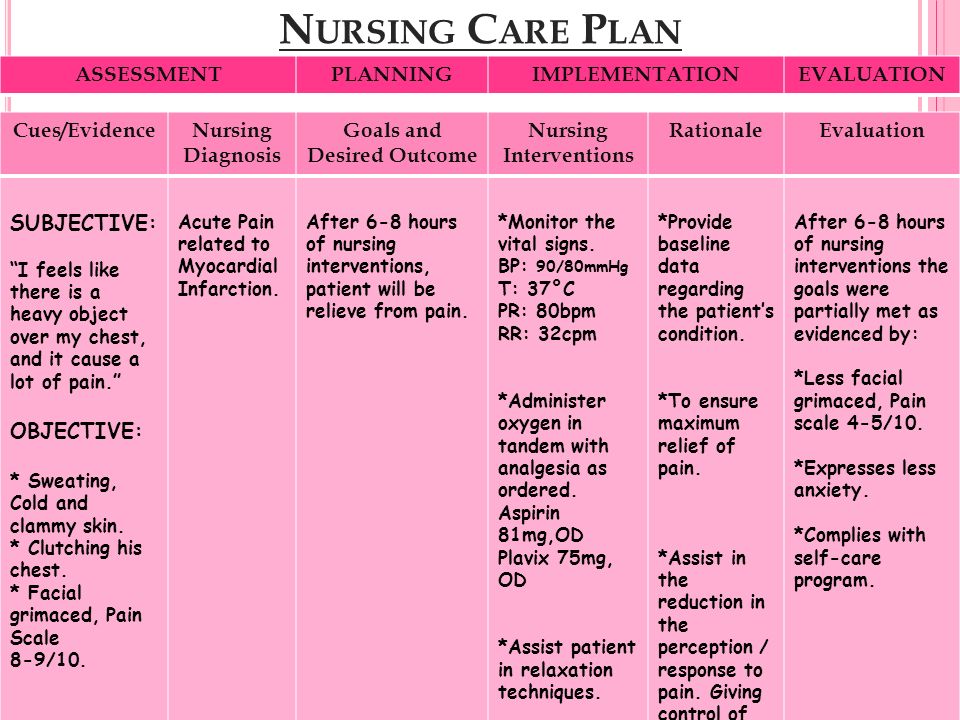 Although frequently recommended by healthcare providers, no evidence has been found that complete bed rest improves pregnancy outcomes. Rather, prolonged bed rest can increase the risk of complications due to immobility (e.g., muscle atrophy, weight loss, cardiovascular deconditioning, psychologic stress, etc.). Therefore, restricted activity rather than complete bed rest is recommended (Ghulmiyyah et al., 2012).
Although frequently recommended by healthcare providers, no evidence has been found that complete bed rest improves pregnancy outcomes. Rather, prolonged bed rest can increase the risk of complications due to immobility (e.g., muscle atrophy, weight loss, cardiovascular deconditioning, psychologic stress, etc.). Therefore, restricted activity rather than complete bed rest is recommended (Ghulmiyyah et al., 2012).
2. Instruct the client to elevate legs when sitting or lying down.
Elevating the legs decreases venous stasis and may also reduce the incidence of thrombus and embolus formation in the client on bed rest.
3. Monitor the client’s BP and instruct monitoring of BP at home.
Monitor BP every 15 minutes during the critical phase and every 1 to 4 hours as the client’s condition improves. If the client is an outpatient, instruct both the client and a family member to monitor the BP two to four times per day in the same arm and the same position.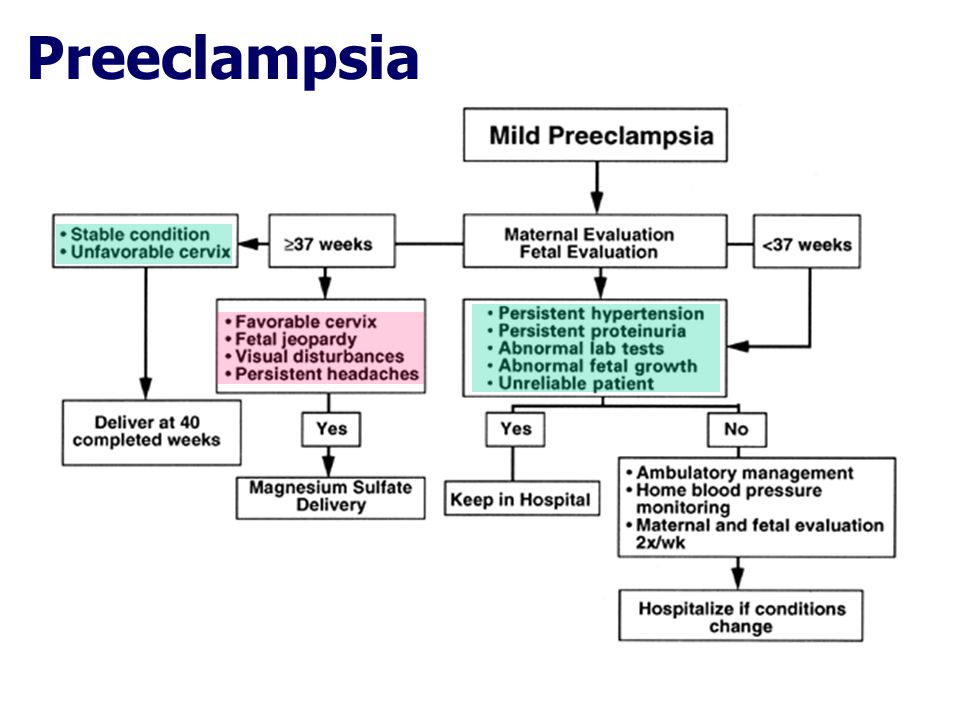 A family member must be taught the technique to ensure accurate measurements. Rising blood pressure levels may indicate worsening preeclampsia.
A family member must be taught the technique to ensure accurate measurements. Rising blood pressure levels may indicate worsening preeclampsia.
4. Record and graph vital signs, especially BP and pulse.
The client with preeclampsia does not display the normal cardiovascular response to pregnancy (left ventricular hypertrophy, increased plasma volume, vascular relaxation with decreased peripheral resistance). Hypertension (the second manifestation of preeclampsia after edema) occurs due to increased sensitization to angiotensin II, which increases BP and promotes aldosterone release to increase sodium/water reabsorption from the renal tubules constricts blood vessels.
5. Monitor for invasive hemodynamic parameters such as cardiac output, as indicated.
Provides a precise picture of vascular changes and fluid volume. Prolonged vascular constriction, increased hemoconcentration, and fluid shifts decrease cardiac output.
6. Administer low-dose aspirin as indicated.
Administer low-dose aspirin as indicated.
When initiated before 16 weeks gestation, low-dose aspirin effectively prevents preeclampsia, severe preeclampsia, preterm birth, and intrauterine growth restriction in patients with high-risk pregnancies (Fantasia, 2018; Xu et al., 2015). It is recommended that daily dose aspirin therapy be initiated late in the first trimester for women who have a history of early-onset preeclampsia and subsequent preterm birth at less than 34 weeks of gestation or a history of preeclampsia in more than one previous pregnancy.
7. Administer antihypertensive medications as ordered. Observe for side effects of antihypertensive drugs.
If blood pressure does not respond to conservative measures, short-term medication may be needed with other therapies (e.g., fluid replacement, magnesium sulfate). Antihypertensive treatment should be initiated as soon as reasonably possible for acute-onset severe hypertension that persists (ACOG, 2020). Antihypertensive drugs work directly on arterioles to promote relaxation of cardiovascular smooth muscles and help increase blood supply to the cerebrum, kidneys, uterus, and placenta (Lightstone, 2013). Intravenous hydralazine, or labetalol, and oral nifedipine are three agents commonly used to control hypertension in pregnancy.
Antihypertensive drugs work directly on arterioles to promote relaxation of cardiovascular smooth muscles and help increase blood supply to the cerebrum, kidneys, uterus, and placenta (Lightstone, 2013). Intravenous hydralazine, or labetalol, and oral nifedipine are three agents commonly used to control hypertension in pregnancy.
- 7.1. Hydralazine (Apresoline, Neopresol).
Administered intravenously, hydralazine reduces blood pressure by relaxing the smooth muscles. The vasodilating effect reduces peripheral vascular resistance. Check BP every minute for 5 mins then every 5 mins for 30 mins. - 7.2. Labetalol Hydrochloride (Normodyne, Trandate).
Given intravenously, labetalol is an alpha- and beta-blocker that decreases peripheral vascular resistance without significant change in cardiac output or causing tachycardia. Contraindicated with asthma and congestive heart failure. Closely monitor blood pressure after administration.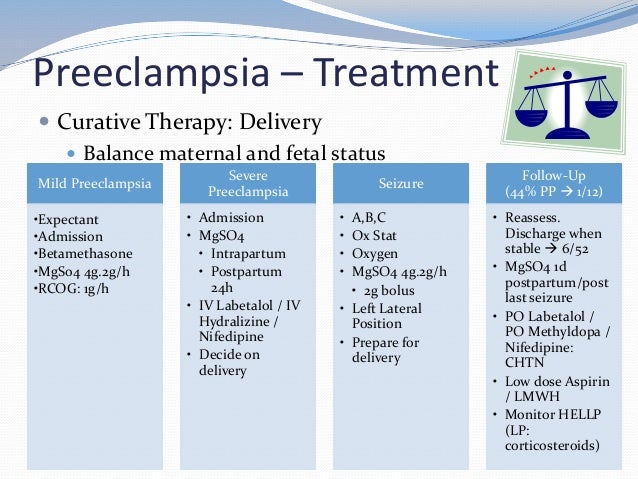
- 7.3. Methyldopa (Aldomet).
Interferes with chemical neurotransmission to reduce peripheral vascular resistance. Can cause CNS sedation, sleepiness, postural hypotension. - 7.4. Nifedipine (Adalat).
Calcium channel blocker that dilates arterioles and decreases systemic vascular resistance by relaxing arterial smooth muscle. Nifedipine can potentiate the CNS effects of magnesium sulfate. Closely monitor blood pressure after administration. - 7.5. Sodium Nitroprusside (Nitropress).
Used in rare scenarios where other antihypertensive agents have failed to control blood pressure.
8. Prepare for the birth of fetus by cesarean delivery, labor when severe preeclamptic or eclamptic condition is stabilized, but vaginal delivery is not feasible.
If conservative treatment is ineffective and labor induction is ruled out, then surgical procedure is the only means of halting the hypertensive problems.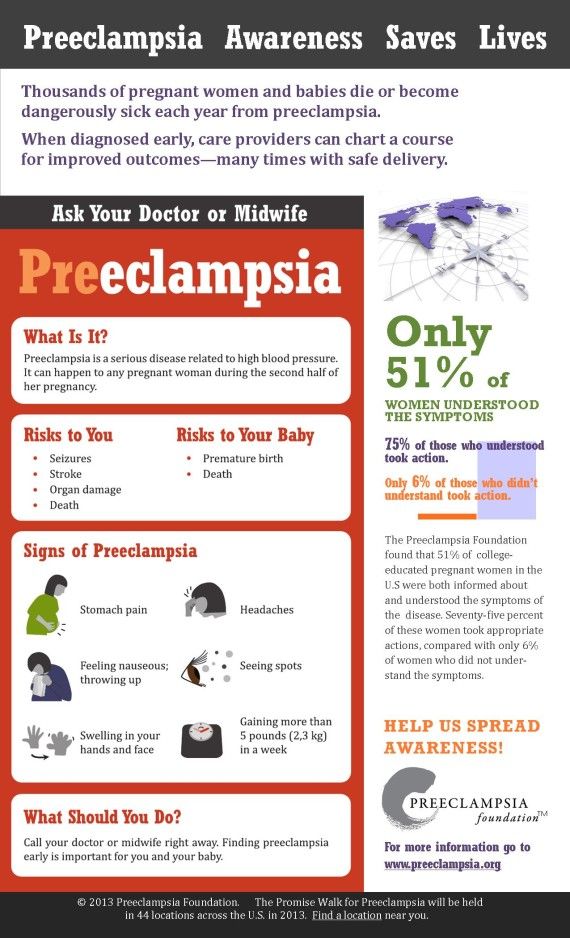 Delivery of the fetus is the cure for preeclampsia. If preeclampsia is severe, the fetus is often in greater danger from being in the uterus because its oxygen and nutritional supply may be cut off or its growth can be restricted. Fetal death sometimes can occur.
Delivery of the fetus is the cure for preeclampsia. If preeclampsia is severe, the fetus is often in greater danger from being in the uterus because its oxygen and nutritional supply may be cut off or its growth can be restricted. Fetal death sometimes can occur.
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy.
References and sources for this nursing care plan for hypertensive disorders in pregnancy.
Preeclampsia Nursing Diagnosis & Care Plan
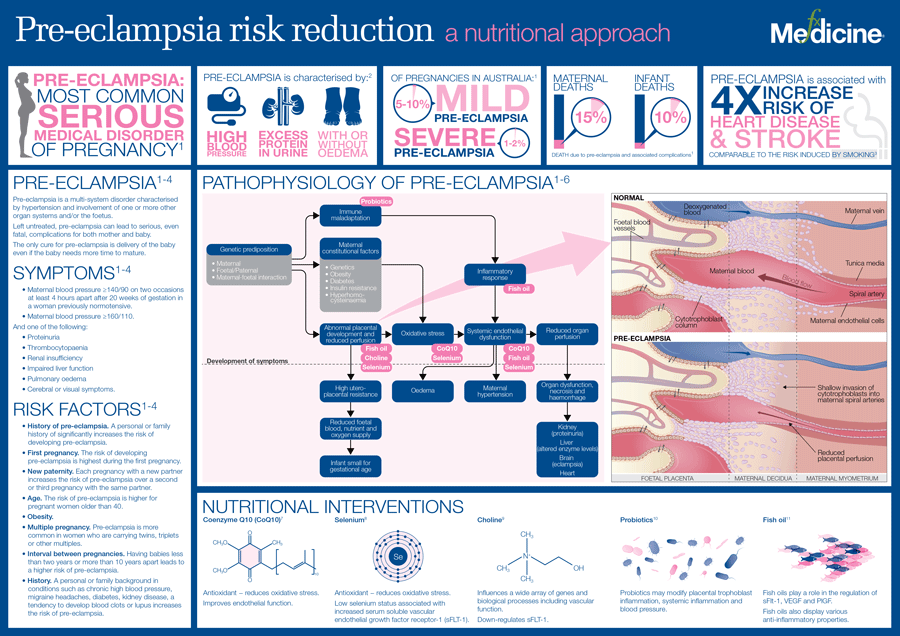
Preeclampsia is a serious complication that occurs during pregnancy and affects 5-7% of pregnancies worldwide. It is characterized by high blood pressure and protein in the urine (proteinuria). The exact cause is unknown though research shows genetics or blood vessel abnormalities with the placenta could be a potential cause.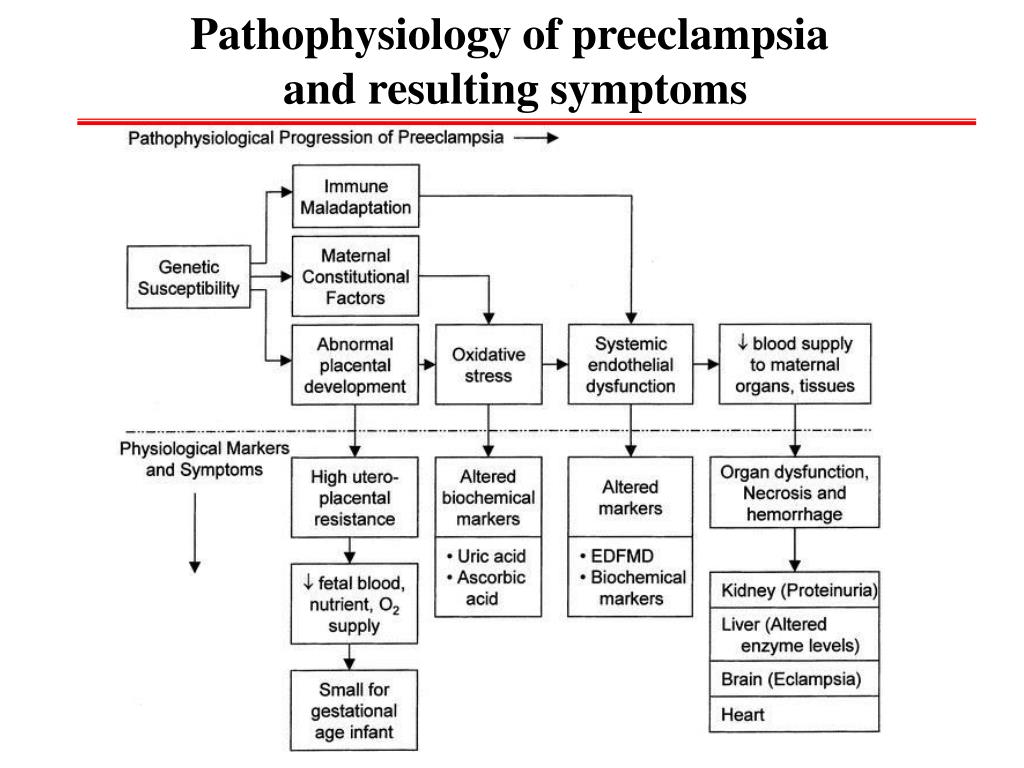
The following risk factors increase the chance of a woman developing preeclampsia:
- Multiple-gestation pregnancy
- Obesity
- Family history of preeclampsia
- Women giving birth for the first time
- Women younger than 20 years of age or older than 40 years of age
- Overproduction of amniotic fluid (polyhydramnios)
- Underlying diseases like hypertension, diabetes, renal disease, and autoimmune disorders
Hypertension, proteinuria, and edema are the classic triad symptoms of preeclampsia. Other symptoms include:
- Constant headaches
- Vision abnormalities
- Shortness of breath
- Epigastric pain
- Fluctuations in fetal heart rate
- Vaginal bleeding
Preeclampsia, if untreated, can hinder the baby’s growth and may develop into eclampsia. Eclampsia is a severe complication of preeclampsia that can lead to seizures.
The only way to treat preeclampsia is to deliver the baby.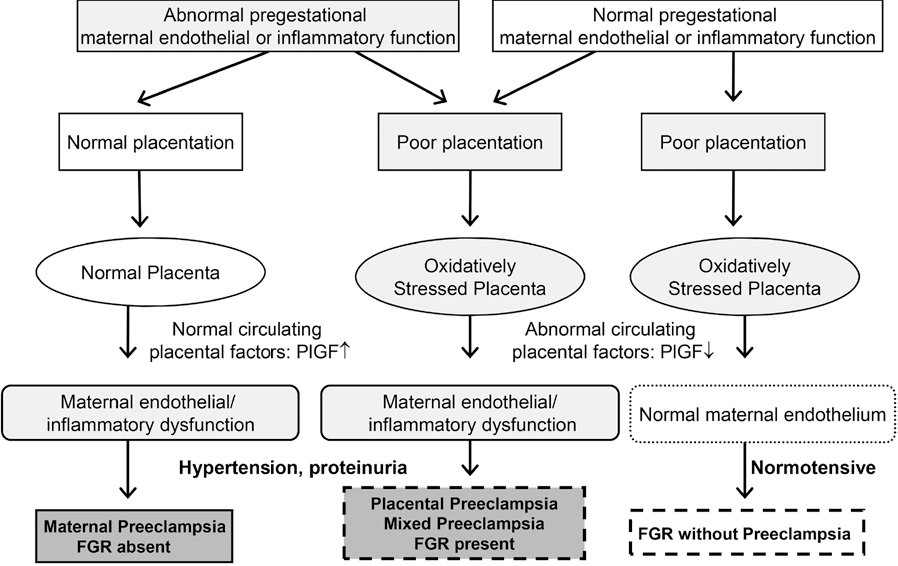 After delivery, preeclampsia usually resolves within days to weeks.
After delivery, preeclampsia usually resolves within days to weeks.
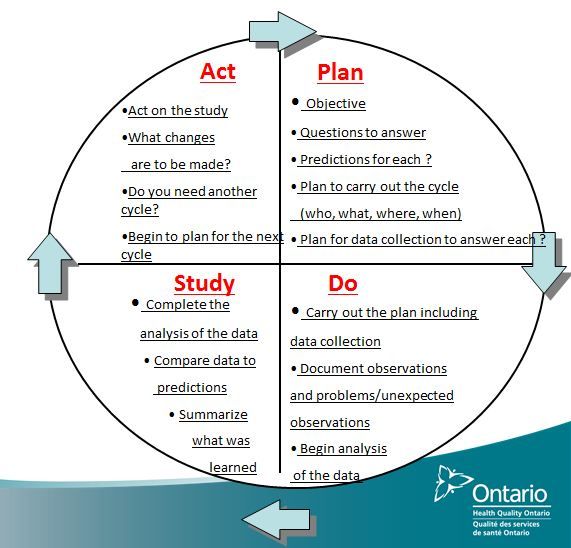
The Nursing Process
Nurses can first identify high-risk pregnancies to prevent preeclampsia. Focus on a thorough nursing assessment, education, and antenatal care.
The majority of cases are avoidable. Interventions include:
- Monitoring the patient’s blood pressure and symptoms
- Stress management
- Weight management
- Proper nutrition
- Monitoring fetal heart rate (FHR)
- Regular OB/GYN follow-ups and prenatal care
Nursing Care Plans Related to Preeclampsia
Risk for Imbalanced Fluid Volume Care Plan
Risk for imbalanced fluid volume associated with preeclampsia is caused by fluid shifts which can lead to overloading organs and tissues.
Nursing Diagnosis: Risk for Imbalanced Fluid Volume
Related to:
- Plasma protein loss
- Decreased osmotic pressure
- Fluid shifting out of the vascular space
- Narrowing of the blood vessels
- Highly concentrated blood (Hemoconcentration)
- Elevated blood flow resistance
- Body cell degeneration (for pregnant mothers of older age)
- Decreased kidney filtration
- Sodium retention
As evidenced by:
A risk diagnosis is not evidenced by signs and symptoms as the problem has not yet occurred.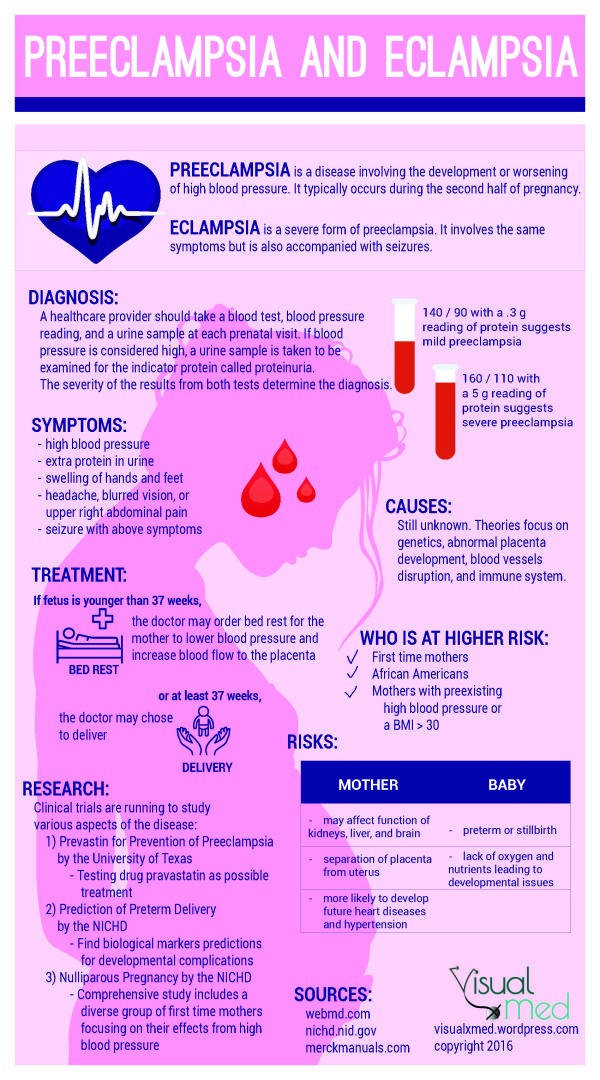 Interventions are aimed at prevention.
Interventions are aimed at prevention.
Expected outcomes:
- Patient will be able to maintain adequate fluid volume as evidenced by blood pressure within normal limits
- Patient will be able to demonstrate efficient fluid intake and output
- Patient will remain free from generalized or pulmonary edema
Imbalanced Fluid Volume Assessment
1. Monitor blood pressure.
High blood pressure during pregnancy causes a concern for preeclampsia. Increased blood pressure may cause the heart to have to work harder due to the additional fluid in the body.
2. Assess for edema, proteinuria, and weight gain.
Proteinuria, edema, and weight gain are symptoms of preeclampsia. Protein in the urine (proteinuria) occurs from impaired renal filtration. Weight gain is likely related to fluid retention.
Note the following symptoms:
- Proteinuria of 1+ to 2+ on a random sample
- Minor facial or upper extremity edema
- Weight gain of more than 2 pounds per week in the second trimester and less than 1 pound per week in the third trimester
3. Monitor fetal well-being and status.
Monitor fetal well-being and status.
Preeclampsia is a significant factor in fetal death. If fluid is not balanced, the fetus is at higher risk of hypoxia and growth retardation.
Imbalanced Fluid Volume Interventions
1. Manage preeclampsia.
Collaborate with the healthcare team in treating preeclampsia to manage symptoms of fluid volume imbalance and prevent further complications.
2. Administer fluids.
IV fluids are administered to expand the intravascular volume. Care must be taken to not worsen or cause pulmonary edema.
3. Instruct on diet recommendations.
Limiting sodium and taking calcium, magnesium, and potassium supplements prevent the progression of edema and hypertension in preeclampsia.
4. Monitor intake and output.
Oliguria or reduced urine output can signal decreased kidney function from poor circulatory blood volume.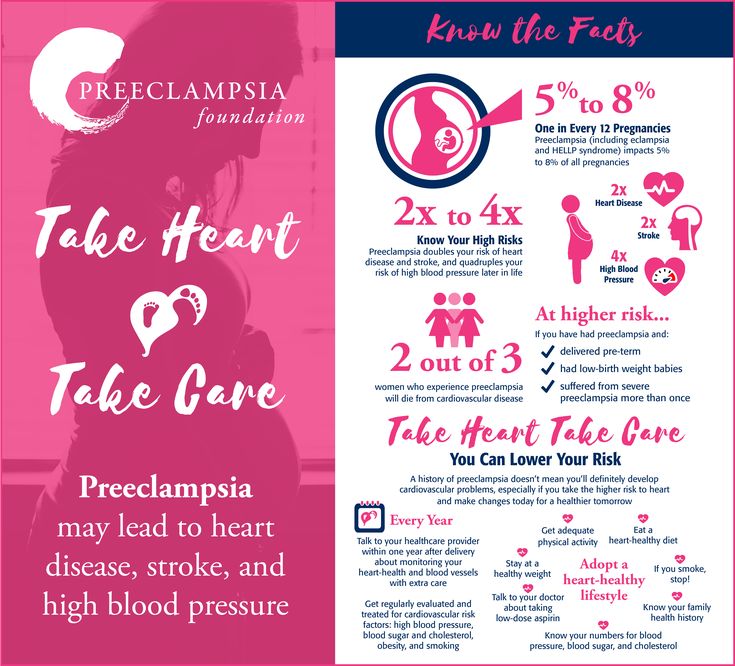
Decreased Cardiac Output Care Plan
Decreased cardiac output associated with preeclampsia can be caused by increased cardiac demands and decreased blood supply.
Nursing Diagnosis: Decreased Cardiac Output
Related to:
- Hypovolemia
- Decreased venous return
- Increased systemic vascular resistance
As evidenced by:
- Alterations in blood pressure
- Alterations in hemodynamic readings
- Edema
- Dyspnea
- Alterations in mental status
Expected outcomes:
- Patient will be able to maintain adequate blood pressure within acceptable limits
Decreased Cardiac Output Assessment
1. Assess the patient’s blood pressure.
During pregnancy, hypertension is defined as blood pressure >140/90 mm Hg. Preeclampsia is diagnosed with new onset hypertension with proteinuria after 20 weeks of pregnancy.
2. Assess for indications of poor cardiac function and impending heart failure.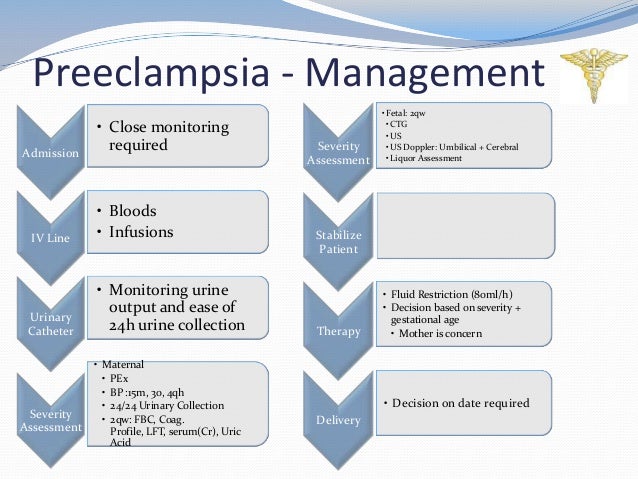
The nurse can assess for the following symptoms:
- Excessive fatigue
- Intolerance to exertion
- Sudden or rapid weight gain
- Edema in the extremities
- Progressive or worsening shortness of breath
4. Assess the patient’s platelet count.
In preeclamptic women, a low platelet count is linked to a higher risk of abnormal coagulation and decreased cardiac output.
5. Assess for fetal growth.
Preeclampsia reduces cardiac output and can affect the arteries that provide blood to the placenta. The fetus may not get enough oxygen or nutrients which may result in fetal growth restriction.
Decreased Cardiac Output Interventions
1. Position the patient comfortably on the left side-lying position.
Left side-lying promotes adequate circulation. This position makes it easier for nutrient-rich blood to flow from the heart to the placenta to support the fetus.
2. Administer oxygen as prescribed.
Increase the amount of oxygen available for heart function which will increase the blood supply to the placenta and fetus.
3. Administer antihypertensives.
Cardiac medications should be administered to reduce hypertension with precautions that are safe for the mother and the fetus.
4. Restrict fluids as ordered.
If there is the presence of edema and cardiopulmonary congestion, restrict fluid intake as ordered.
6. Encourage reduced activity.
Rest periods and reduced activity is recommended. Physical activity diverts blood away from the placenta. Complete bed rest is not necessary.
7. Prepare for cesarean section.
If complications of preeclampsia due to decreased cardiac output are present, an emergency cesarean section is performed. This is to prevent maternal and fetal death.
Deficient Knowledge Care Plan
Deficient knowledge associated with preeclampsia can result in delayed recognition and treatment and poorer outcomes.
Nursing Diagnosis: Deficient Knowledge
Related to:
- Pathophysiology of preeclampsia
- Management of preeclampsia
- Risk factors for preeclampsia
- Self-care and nutritional needs of preeclampsia
- Complications of preeclampsia
- Lack of exposure to preeclampsia
- Inaccurate information about preeclampsia
- Misconceptions about preeclampsia
As evidenced by:
- Rapid progress of preeclampsia
- Development of preventable complications
- Unawareness of symptoms
- Inquiries about preeclampsia
- Misconceptions about preeclampsia
- Inaccurate or insufficient instructions in the prevention or management of preeclampsia
Expected outcomes:
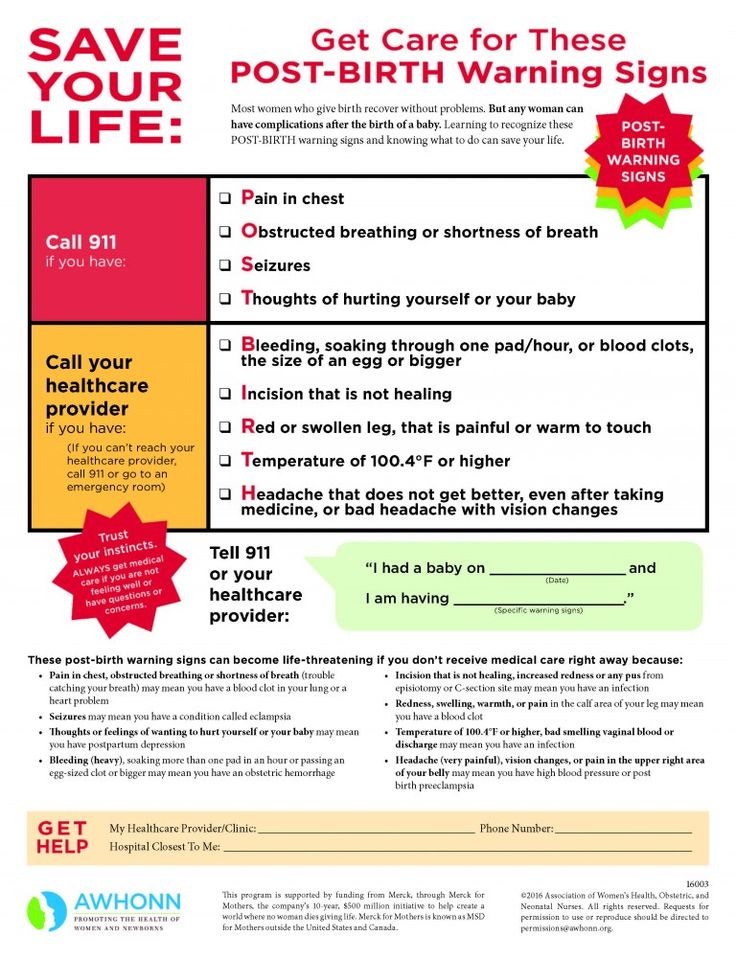
- Patient will be able to verbalize understanding of preeclampsia and its management
- Patient will be able to verbalize possible complications and when to contact a healthcare provider
- Patient will be able to demonstrate behavior and lifestyle modifications in the prevention of preeclampsia
Deficient knowledge Assessment
1. Determine the patient’s knowledge level of preeclampsia.
Determine the patient’s knowledge level of preeclampsia.
Assessing the patient’s current knowledge and understanding of preeclampsia will help the nurse determine appropriate resources to guide learning.
2. Determine misconceptions about preeclampsia.
Preeclampsia can be misinterpreted by the patient due to past information or influences by family, friends, and cultures. Ask the patient directly about their understanding and clarify any questions as needed.
4. Assess readiness to learn.
Pregnancy can be an exciting and frightening journey, especially for first-time moms. Establish an uninterrupted time to provide information on preeclampsia that is not overwhelmed by other instructions.
Deficient knowledge Interventions
1. Instruct on symptoms to report.
Provide verbal and written instructions on symptoms to report to the healthcare provider such as blurred vision, headaches, epigastric pain, or difficulty breathing.
2. Involve the support system.
A mother requires support from her partner and family members. Information can be provided to support persons to monitor the patient and encourage healthy habits.
3. Encourage using positive reinforcement.
Positive reinforcement can be used to encourage behavior modification and teach new skills. It promotes motivation for further attempts at learning.
4. Instruct on appointments and tests.
Completing follow-up appointments, glucose monitoring, and blood pressure assessments will ensure a healthy pregnancy and delivery.
References and Sources
- Doenges, M. E., Moorhouse, M. F., & Murr, A. C. (2019). Nurse’s pocket guide: Diagnoses, interventions, and rationales (15th ed.). F A Davis Company.
- Moura, S. B., Lopes, L. M., Murthi, P., & Costa, F. D. (2012, December 17). Prevention of Preeclampsia. PubMed Central (PMC).
 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3534321/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3534321/ - Pillitteri, A., & Silbert-Flagg, J. (2015). Nursing Care of a Family Experiencing a Sudden Pregnancy Complication. In Maternal & child health nursing: Care of the childbearing & Childrearing family (8th ed., pp. 1210-1224). LWW.
- Silvestri, L. A., & CNE, A. E. (2019). Risk Conditions Related to Pregnancy. In Saunders comprehensive review for the NCLEX-RN examination (8th ed., pp. 687-688). Saunders.
Preeclampsia. What is Preeclampsia?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Preeclampsia is a severe variant of preeclampsia that occurs after the 20th week of gestational age, is characterized by multiple organ disorders with a primary lesion of the central nervous system, and precedes eclampsia. Manifested by headaches, nausea, vomiting, visual disturbances, hyperreflexia, lethargy, drowsiness or insomnia. It is diagnosed on the basis of data from daily monitoring of blood pressure, urinalysis, coagulogram, transcranial dopplerography. For treatment, infusion therapy, anticonvulsant, antihypertensive, anticoagulant, membrane stabilizing agents are used. With the ineffectiveness of appointments, an emergency caesarean section is indicated. nine0006
Manifested by headaches, nausea, vomiting, visual disturbances, hyperreflexia, lethargy, drowsiness or insomnia. It is diagnosed on the basis of data from daily monitoring of blood pressure, urinalysis, coagulogram, transcranial dopplerography. For treatment, infusion therapy, anticonvulsant, antihypertensive, anticoagulant, membrane stabilizing agents are used. With the ineffectiveness of appointments, an emergency caesarean section is indicated. nine0006
ICD-10
O14 Pregnancy-induced hypertension with significant proteinuria
- Causes of pre-eclampsia
- Pathogenesis
- Symptoms of pre-eclampsia
- Complications
- Diagnostics
- Treatment of preeclampsia
- Prognosis and prevention
- Prices for treatment
General
Often, preeclampsia develops after the 28th week of gestation against the background of milder forms of preeclampsia.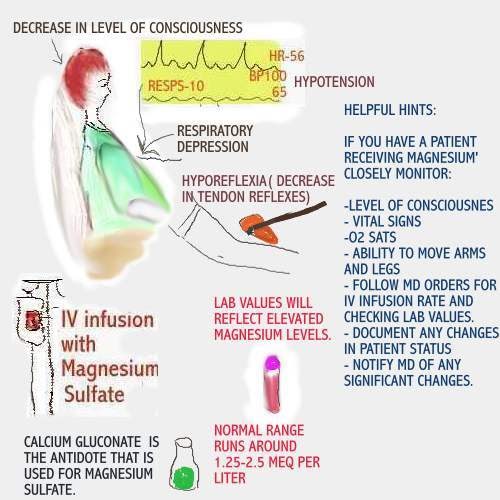 The preeclamptic state is observed in 5% of pregnant women, women in labor and puerperas. In 38-75% of patients, it occurs in the prenatal period, in 13-36% - in childbirth, in 11-44% - after childbirth. In 62% of cases, preeclampsia precedes eclampsia, although, according to some authors, in other patients, the disorder remains unrecognized due to the rapid development of convulsive syndrome. More often, the disease occurs in predisposed women during the first teenage, late, multiple pregnancy, repeated gestation with a history of preeclampsia, the presence of obesity, extragenital pathology (chronic arterial hypertension, diseases of the liver, kidneys, collagenoses, diabetes mellitus, antiphospholipid syndrome). nine0006
The preeclamptic state is observed in 5% of pregnant women, women in labor and puerperas. In 38-75% of patients, it occurs in the prenatal period, in 13-36% - in childbirth, in 11-44% - after childbirth. In 62% of cases, preeclampsia precedes eclampsia, although, according to some authors, in other patients, the disorder remains unrecognized due to the rapid development of convulsive syndrome. More often, the disease occurs in predisposed women during the first teenage, late, multiple pregnancy, repeated gestation with a history of preeclampsia, the presence of obesity, extragenital pathology (chronic arterial hypertension, diseases of the liver, kidneys, collagenoses, diabetes mellitus, antiphospholipid syndrome). nine0006
Preeclampsia
Causes of preeclampsia
The etiology of the disorder, as well as other forms of gestosis, has not been finally established to date. A likely factor contributing to the development of preeclampsia is the pathological reaction of the body of a predisposed woman to physiological changes during pregnancy.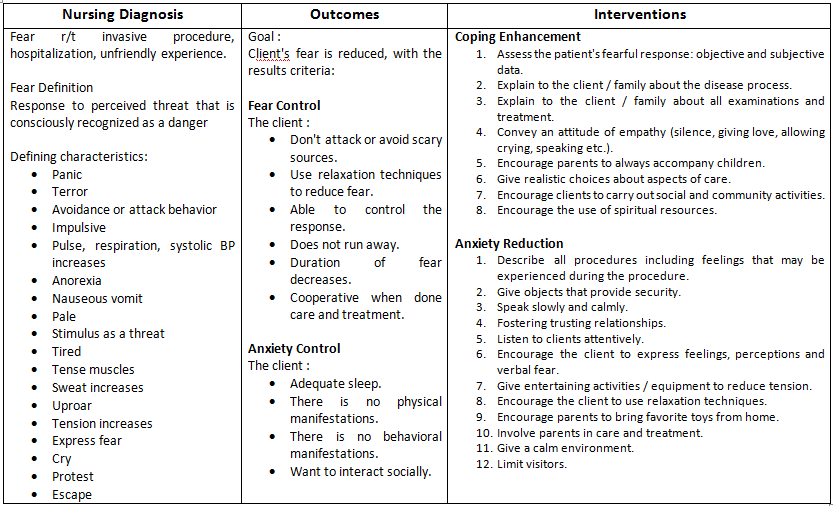 More than 30 reasoned etiopathogenetic theories of the onset of the disease have been proposed by specialists in the field of obstetrics, the main of which are: nine0006
More than 30 reasoned etiopathogenetic theories of the onset of the disease have been proposed by specialists in the field of obstetrics, the main of which are: nine0006
- Hereditary. The role of genetic factors in the development of preeclampsia is confirmed by its more frequent diagnosis in patients whose mothers suffered from preeclampsia. Patients have defects in the genes 7q36-eNOS, 7q23-ACE, AT2P1, C677T. The mode of inheritance is presumably autosomal recessive.
- Immune. Penetration into the maternal circulation of foreign antigens of the fetus is accompanied by the response production of antibodies. The deposition of the formed immune complexes in various tissues triggers complex protective mechanisms, which are manifested by the activation of endothelial cells and acute endotheliosis. nine0016
- Placental. Some authors associate preeclampsia with impaired cytotrophoblast invasion. As a result, there is no transformation of the smooth muscle layer of the uterine arteries, which subsequently leads to their spasm, deterioration of intervillous blood flow, hypoxia and, as a result, damage to the endothelium.
- Cortico-visceral. Proponents of the theory consider preeclampsia as a neurotic hemodynamic disorder caused by a violation of the relationship between the cortex and subcortical regions. This approach explains the provoking role of severe stress and is confirmed by functional changes in the EEG. nine0016
Since individual theories cannot fully explain all the clinical manifestations of the disease, it is justified to consider preeclampsia as a polyetiological condition with common mechanisms of pathogenesis. The immediate causes of the development of preeclampsia are improperly selected therapy for dropsy of pregnancy and nephropathy, non-compliance by the patient with medical recommendations, and high therapeutic resistance of milder variants of gestosis.
Pathogenesis
The key link in the mechanism of development of preeclampsia is the generalization of acute endotheliosis and vasoconstriction, initially localized in the placenta, with the involvement of brain tissues in the pathological process.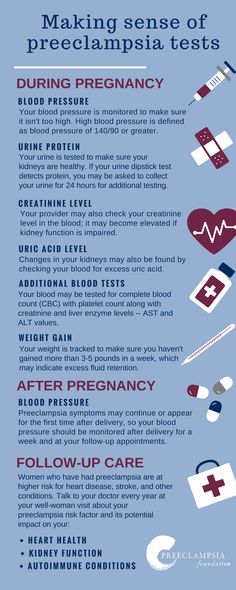 Vascular dysfunction leads to damage to cell membranes, impaired metabolism of neurons with the occurrence of hypersensitivity and increased excitability of nerve cells. The defeat of the suprasegmental subcortical structures is accompanied by polysystemic autonomic disorders, detected in more than 90% of patients with severe forms of preeclampsia.
Vascular dysfunction leads to damage to cell membranes, impaired metabolism of neurons with the occurrence of hypersensitivity and increased excitability of nerve cells. The defeat of the suprasegmental subcortical structures is accompanied by polysystemic autonomic disorders, detected in more than 90% of patients with severe forms of preeclampsia.
In parallel, pregnant women and women in labor with preeclampsia develop pyramidal insufficiency, which indicates a disorder at the level of the cortical sections and is manifested by tendon-periosteal hyperreflexia, anisoreflexia, the occurrence of pathological reflexes, and an increase in convulsive readiness. The last to be affected are the brain stem regions. Destructive processes caused by microcirculation disorders also occur in other organs - the liver, kidneys, lung tissue. The situation is aggravated by coagulopathic disorders characteristic of gestosis. nine0006
Symptoms of preeclampsia
Usually, the disorder occurs against the background of previous nephropathy.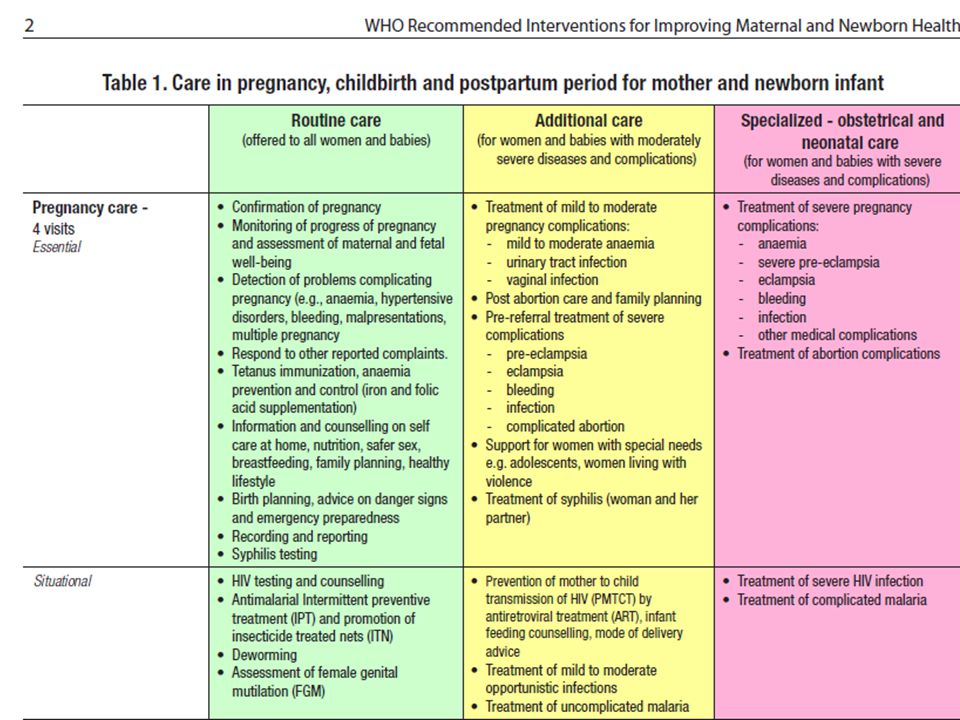 Existing edema, arterial hypertension, moderate astheno-vegetative symptoms (dizziness, weakness, insufficient sleep, meteotropism, emotional lability) are accompanied by signs of CNS damage and increased intracranial pressure. The patient complains of intense headache, heaviness in the back of the head, fatigue, looks lethargic, lethargic, indifferent, sometimes responds inappropriately. There is increased drowsiness or insomnia, trembling of outstretched fingers, sweating of the palms and feet. nine0006
Existing edema, arterial hypertension, moderate astheno-vegetative symptoms (dizziness, weakness, insufficient sleep, meteotropism, emotional lability) are accompanied by signs of CNS damage and increased intracranial pressure. The patient complains of intense headache, heaviness in the back of the head, fatigue, looks lethargic, lethargic, indifferent, sometimes responds inappropriately. There is increased drowsiness or insomnia, trembling of outstretched fingers, sweating of the palms and feet. nine0006
In 25% of women with a clinic of preeclampsia, visual disorders are detected - a feeling of blurred vision, flickering of sparks or flies, fear of light, double vision, loss of individual fields of vision. Perhaps the appearance of nausea, vomiting, pain in the epigastrium and right hypochondrium. In severe cases, there are muscle twitches, delirium, hallucinations, petechial rash, indicating a violation of blood clotting. The pre-eclamptic state is relatively short, lasting no more than 3-4 days, after which it is stopped by the correct therapy or passes into eclampsia.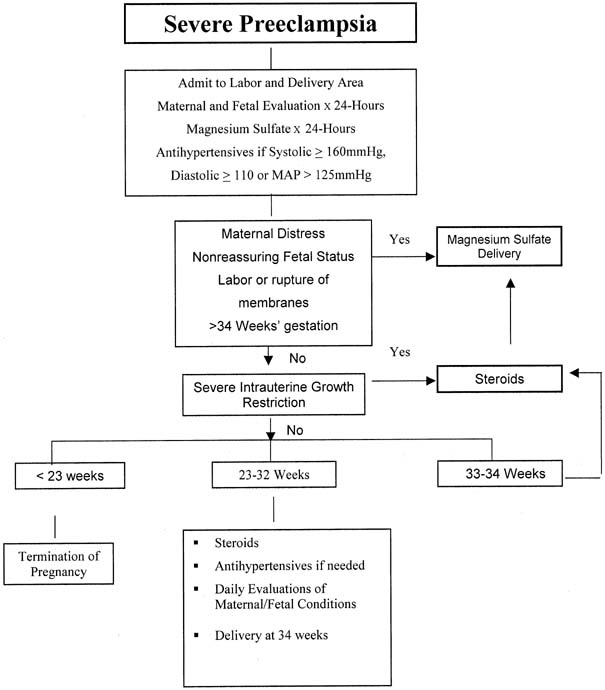 nine0006
nine0006
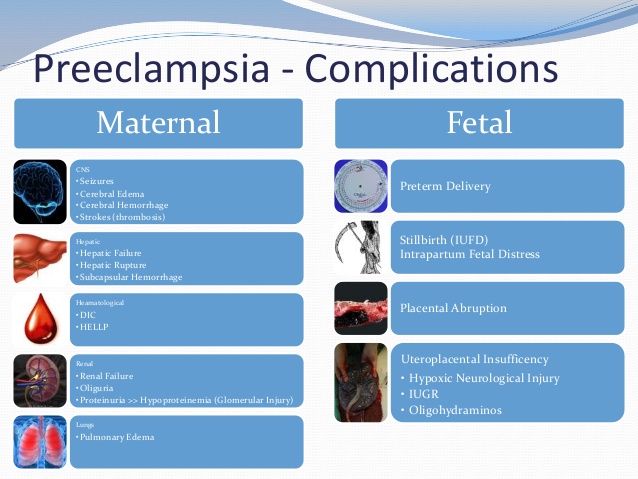
Complications
The most formidable complication of preeclampsia is eclampsia, the most severe type of preeclampsia with high rates of maternal and perinatal mortality. In 1-3% of patients, there is a loss of vision (amaurosis) caused by edema, vascular changes, retinal detachment or ischemia of the occipital lobe of the cortex due to circulatory disorders in the posterior cerebral artery basin. Perhaps the development of a hypertensive crisis, cerebral edema, stroke, HELLP-syndrome, detachment of a normally located placenta, the occurrence of postpartum coagulopathic bleeding and DIC. Fetoplacental insufficiency is usually aggravated, signs of intrauterine fetal hypoxia are growing. nine0006
Women who have had preeclampsia are 4 times more likely to develop cardiovascular diseases (hypertension, angina pectoris, heart attacks, strokes, congestive heart failure) in the future, and the risk of developing type 2 diabetes mellitus doubles.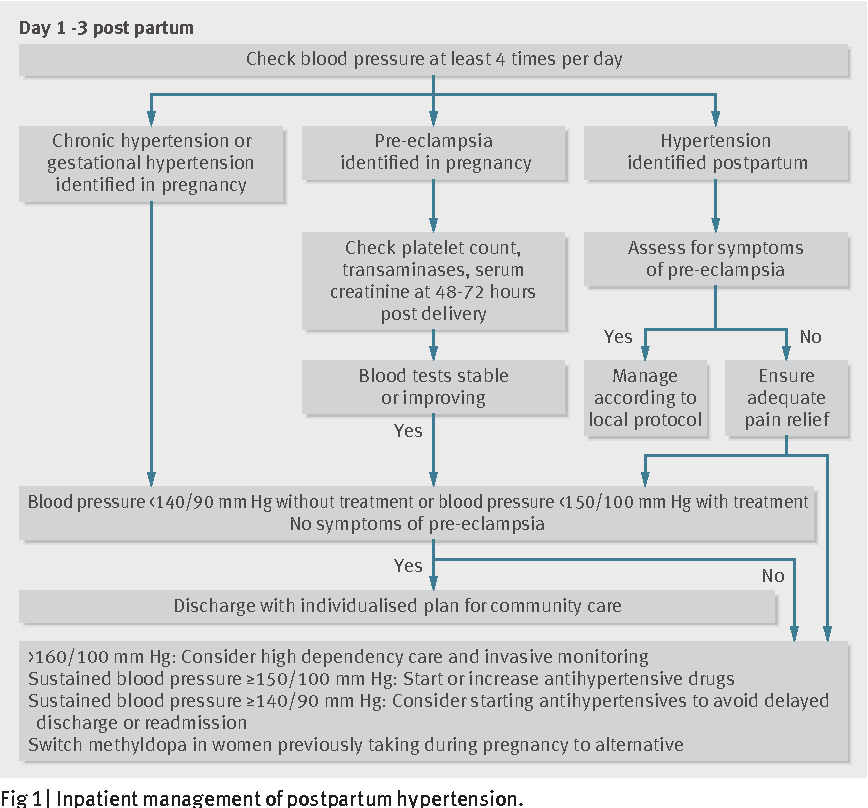 In a third of patients, gestosis is diagnosed in subsequent pregnancies.
In a third of patients, gestosis is diagnosed in subsequent pregnancies.
Diagnostics
Timely diagnosis of preeclampsia is usually not particularly difficult if the pregnant woman has been under the supervision of an obstetrician-gynecologist for a long time about previous nephropathy. During the initial treatment of a patient with characteristic complaints, an examination plan is recommended with the identification of specific markers of preeclampsia: nine0006
- Blood pressure control. Daily monitoring with automatic measurement of blood pressure using a special device is shown. In patients with preeclampsia, blood pressure usually exceeds 180/110 mm Hg. Art. with a pulse amplitude of more than 40 mm Hg. Art. The arterial hypertension index is 50% or more.
- Evaluation of the hemostasis system. Preeclampsia is characterized by coagulopathy of consumption and activation of the fibrinolytic system. It is recommended to study the content of fibrinogen, its degradation products (RFMK), antithrombin III, endogenous heparin, to evaluate APTT, prothrombin (MHO), thrombin time.
 nine0016
nine0016 - Urinalysis. Proteinuria is an important symptom of preeclampsia. The protein content in the urine exceeds 5 g / l, granular casts, leukocyturia can be detected. Hourly urine output is often reduced to 40 ml or less. To assess the severity of kidney damage, the daily amount of protein in the urine is determined.
- TKDG of cerebral vessels. It is used for an objective assessment of cerebral blood flow. In the course of transcranial Doppler sonography, the presence of signs of an increase in cerebral perfusion pressure and a decrease in vascular resistance, characteristic of preeclampsia, is confirmed. nine0016
Taking into account possible obstetric complications, the patient is shown ultrasound of the uterus and placenta, dopplerography of the uteroplacental blood flow, CTG, fetometry, and fetal phonocardiography. Differential diagnosis is carried out with diseases of the brain (thrombosis of the sinuses of the hard shell, meningitis, tumors, stroke), non-convulsive forms of epilepsy, retinal detachment.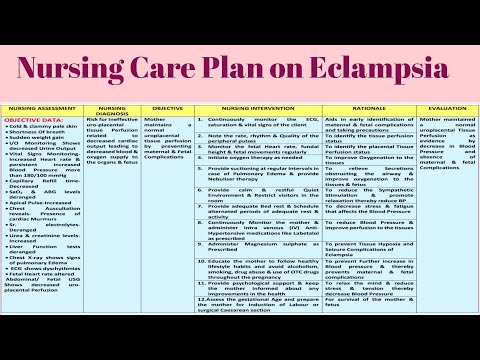 A pregnant woman is consulted by an anesthesiologist-resuscitator, therapist, neuropathologist, ophthalmologist, cardiologist, nephrologist.
A pregnant woman is consulted by an anesthesiologist-resuscitator, therapist, neuropathologist, ophthalmologist, cardiologist, nephrologist.
Treatment of preeclampsia
The patient is urgently admitted to the intensive care unit of the nearest hospital with a delivery room. The main therapeutic task is to reduce reflex and central hyperreactivity, prevent convulsive syndrome, stabilize vital functions, and correct multiple organ disorders. A pregnant woman with preeclampsia is shown a strict medical and protective regimen. The treatment regimen includes the appointment of the following groups of drugs:
- Anticonvulsants. The “gold standard” is the introduction of magnesium sulfate through an infusomat. The drug has a sedative, anticonvulsant, antispasmodic, hypotensive effect, effectively reduces intracranial pressure. Simultaneously with the improvement of cerebral hemodynamics, it relaxes the myometrium and increases the intensity of blood flow in the uterus.
 If necessary, tranquilizers are additionally used.
If necessary, tranquilizers are additionally used. - Antihypertensives. Imidazoline derivatives are preferred, which have a central α2-adrenomimetic effect, stimulate I1-imadazoline receptors in the nucleus of the solitary tract and thereby increase the parasympathetic effect on the myocardium. Perhaps parenteral administration of peripheral vasodilators, hybrid β- and α1-blockers with a rapid antihypertensive effect. nine0016
- Infusion formulations. To normalize oncotic and osmotic pressure, colloidal, protein, balanced crystalloid solutions are injected intravenously. Infusion therapy improves the rheological properties of blood, central and peripheral hemodynamics, tissue perfusion, reduces the severity of multiple organ disorders, and restores water and electrolyte balance.
According to indications, sedatives, direct-acting anticoagulants, antioxidants, membrane stabilizers, drugs to improve blood flow in tissues, and prevent fetal respiratory distress syndrome are used.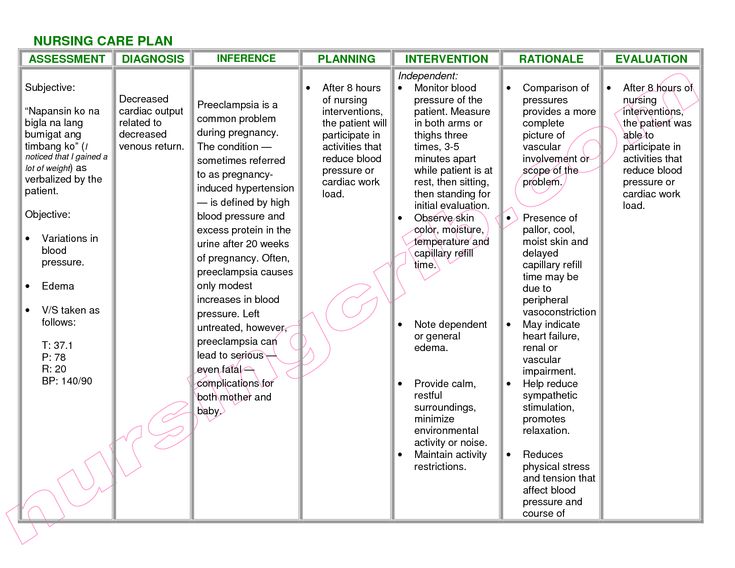 With the ineffectiveness of intensive therapy within a day from the moment of hospitalization, emergency delivery by caesarean section is recommended. Patients with rapidly increasing symptoms of preeclampsia undergo surgery within 2-4 hours. Natural childbirth with high-quality anesthesia (long-term epidural anesthesia), perineotomy or episiotomy is possible only with a significant improvement in the patient's well-being, persistent stabilization of blood pressure, and laboratory parameters. nine0006
With the ineffectiveness of intensive therapy within a day from the moment of hospitalization, emergency delivery by caesarean section is recommended. Patients with rapidly increasing symptoms of preeclampsia undergo surgery within 2-4 hours. Natural childbirth with high-quality anesthesia (long-term epidural anesthesia), perineotomy or episiotomy is possible only with a significant improvement in the patient's well-being, persistent stabilization of blood pressure, and laboratory parameters. nine0006
Prognosis and prevention
The outcome of gestation in pregnant women with symptoms of preeclampsia depends on the availability of medical care and the correct choice of management tactics. In any case, the prognosis for the mother and fetus is considered serious. The level of maternal mortality in recent years has been reduced to 0.07 per 1000 births, perinatal mortality ranges from 21 to 146 per 1000 observations. Prevention of preeclampsia involves regular examinations at the antenatal clinic, monitoring of pressure and laboratory parameters in patients with dropsy of pregnancy, nephropathies, careful implementation of all medical prescriptions, normalization of sleep and rest, psycho-emotional peace, control of weight gain, protein-enriched diet with low salt content.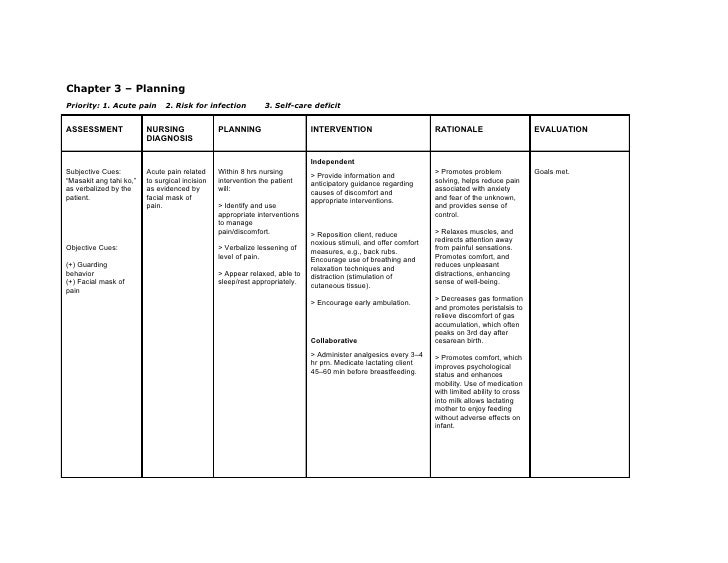 nine0006
nine0006
Sources
- Emergency care for preeclampsia and its complications (eclampsia, HELLP syndrome). Clinical guidelines (treatment protocols). – 2014.
- Uncomplicated preeclampsia / Vetrov V.V., Voinov V.A., Ivanov D.O. — 2012.
- Preeclampsia. Opportunities for prevention / Olompieva T.M., Olina A.A. / / Proceedings of the conference "Two hearts as one". – 2015.
- Management of pregnant women with preeclampsia in the antenatal clinic / Kiseleva N.I., Zanko S.N., Arestova I.M., Sidorenko V.N.// Protection of motherhood and childhood. – 2016 - No1 (27). nine0016
- This article was prepared based on the site materials: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.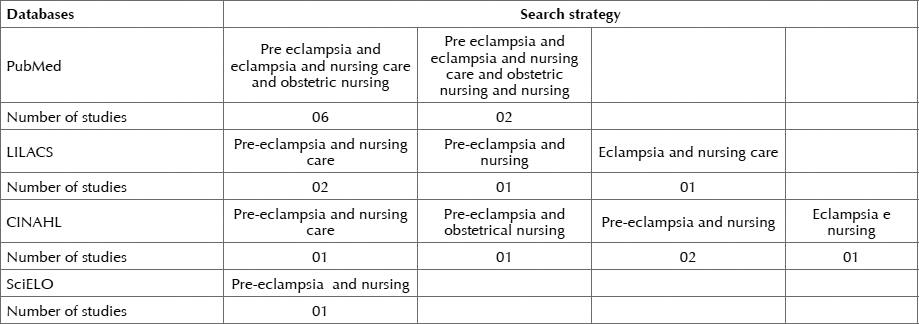
Clinical guidelines “Preeclampsia. Eclampsia. Edema, proteinuria and hypertensive disorders during pregnancy, childbirth and the postpartum period”
Skip to main content- Home
-
- News
- Articles
- Official comments of the department
-
- Newspaper "Be healthy!"
- magazine "Medicine Transbaikalia"
- Collection "Best Doctor of the Trans-Baikal Territory"
- Photo gallery
- Press center
-
- Position
- vacancies of the Ministry of Health
- Information on the conduct of competitions
- The results of competitions
- Commission on compliance with the requirements for official behavior
- Procedure for receipt for the Public Service
- Information for the admission to the Public Service
- Certification of specialists
- Zemsky doctor
- Professional standards
- Target training
- for training at the expense of the NSZ
- Portal of continuous medical and pharmaceutical training (NMO)
- Information on the income of the heads of healthcare institutions
- Information about the SZP of the leading link MO
- need to know about corruption
- List of corrupt positions
- Schedule of Direct Lines
- Regulatory legal acts
- Methodological materials
- form, forms
- reports, reports, reviews, statistical information
- Procedure for appealing decisions of the Ministry of Health
- Plansuivables Plansa
- Audit results
- specialists
- Audit plan
- Audit results
- Plans for conducting inspections
- Results of inspections
-
- State Programs of the Russian Federation
- Healthcare Development of the Trans -Baikal Territory
- Complex measures to improve the narcological situation in the Trans -Baikal Territory
- BMP
- BMP
- BMP
- citizens
- Vital and essential drugs price register
-
- IVF questionnaire
- Documents
- Waiting sheets