Threatened miscarriage with heartbeat and closed cervix
Threatened Abortion - StatPearls - NCBI Bookshelf
Continuing Education Activity
A threatened abortion is vaginal bleeding during pregnancy that does not meet diagnostic criteria for spontaneous abortion. In a threatened abortion, the cervical os remains closed. The World Health Organization (WHO) defines a threatened abortion as pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation. A threatened abortion can present during early pregnancy with lower abdominal pain, and/or vaginal bleeding. Nearly 25 percent of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50 percent of these progress to an actual abortion. The bleeding in a threatened abortion is mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
Outline threatened abortion.
Summarize the differences between threatened abortion and other abortion types including elective, inevitable, incomplete, complete, or missed.
Explain how to manage a patient presenting with a threatened abortion.
Describe how the facilitation of interprofessional team education and discussion can optimize the effective detection of a threatened abortion and inform the need for subsequent evaluations.
Access free multiple choice questions on this topic.
Introduction
Abortion is the medical term for a pregnancy loss before 20 weeks of gestational age. The types of spontaneous abortion include threatened, inevitable, incomplete, complete, septic, and missed abortion[1].
A threatened abortion is defined as vaginal bleeding before 20 weeks gestational age in the setting of a positive urine and/or blood pregnancy test with a closed cervical os, without passage of products of conception and without evidence of a fetal or embryonic demise. The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
Other types of abortion should be considered if the cervical os is open, if there is determined to be an extrauterine pregnancy, if there is determined to be an intrauterine pregnancy without a fetal heartbeat, or if there is evidence of the passage of products of conception[3].
Nearly 25% of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50% of these progress to loss of the pregnancy. The bleeding during a threatened abortion is typically mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. [4][5][6][7]
Etiology
The exact etiology of a threatened or spontaneous abortion is not always known. It is widely accepted that the vast majority of spontaneous abortions cannot be prevented or modified likely because they are due to chromosomal abnormalities in at least half of all cases[8]. For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10]. When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence.
For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10]. When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence. It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
Epidemiology
Threatened abortion can occur in any pregnancy regardless of maternal age, race, comorbidities, lifestyle, or socioeconomic status[10]. If a woman has previously had bleeding in the first trimester of pregnancy, her risk of bleeding in the first trimester of subsequent pregnancies does appear to be increased. Risk factors for any type of miscarriage include advanced maternal age, advanced paternal age, prior history of pregnancy loss, TORCH infections, uncontrolled hyperglycemia, obesity, uncontrolled thyroid disease, significant stressors, use of teratogenic medications, and presence of a subchorionic hemorrhage[12].
Pathophysiology
A threatened abortion occurs when a pregnant patient at less than 20 weeks gestation presents with vaginal bleeding. The cervical os is closed on a physical exam. The patient may also experience abdominal cramping, pelvic pain, pelvic pressure, and/or back pain.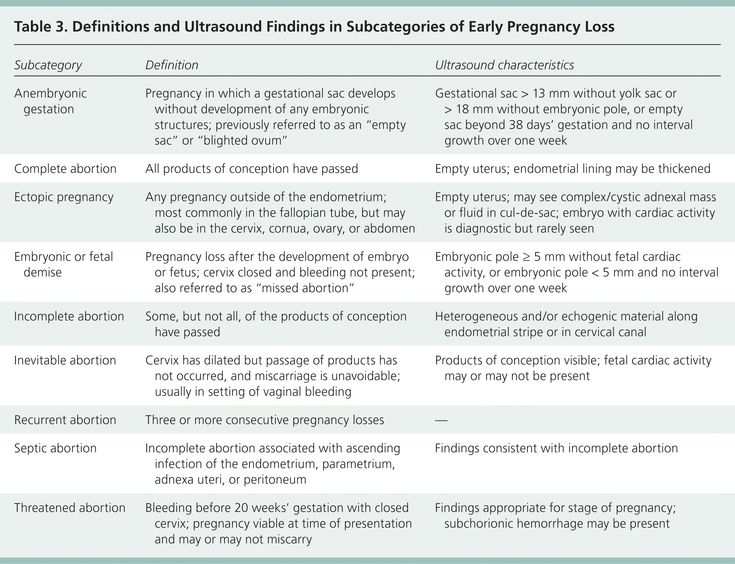 Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Histopathology
It is strongly recommended that all products of conception from any type of abortion are considered for histopathological examination. For patients with repeat pregnancy loss, karyotyping should be given as an option for products of conception to rule in or rule out chromosomal abnormalities as likely cause of spontaneous abortion. This information can help patients determine the best options for moving forward if they desire future pregnancies[16].
History and Physical
A pelvic exam is mandatory to determine the type of abortion. Determining factors include the amount and site of bleeding, whether the cervix is dilated, and whether fetal tissue has passed. In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis. The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis. The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
Evaluation
The diagnosis is made by history, physical exam, measurement of beta-human chorionic gonadotropin (beta-hCG), and an ultrasound[10].
A thorough history should be obtained including pregnancy history, medical history, and history of present illness. History of present illness should include when and how symptoms/bleeding began, modifying factors, any treatments trialed up to the point of evaluation, and helping the patient to describe and quantify the bleeding[20][5].
Transvaginal ultrasound may be used to locate the pregnancy and determine if the fetus is viable. The ultrasound can also help rule out ectopic pregnancy and to evaluate for retained products of conception. A yolk sac is typically seen at 36 days, and a heartbeat is seen on ultrasound at approximately 45 days after the last menstruation[21].
A beta-hCG level of 1500 lU/mL to 2000 lU/mL is associated with a gestational sac on ultrasound. Beta-hCG doubles in 48 hours in 85% of intrauterine pregnancies. Beta-hCG is usually detectable the first nine to 11 days following ovulation and reaches 200 IU/mL at the expected time of menses[22].
Rh factor will also determine if Rhogam should be administered to prevent hemolytic disease of the newborn in this pregnancy and subsequent pregnancies[23].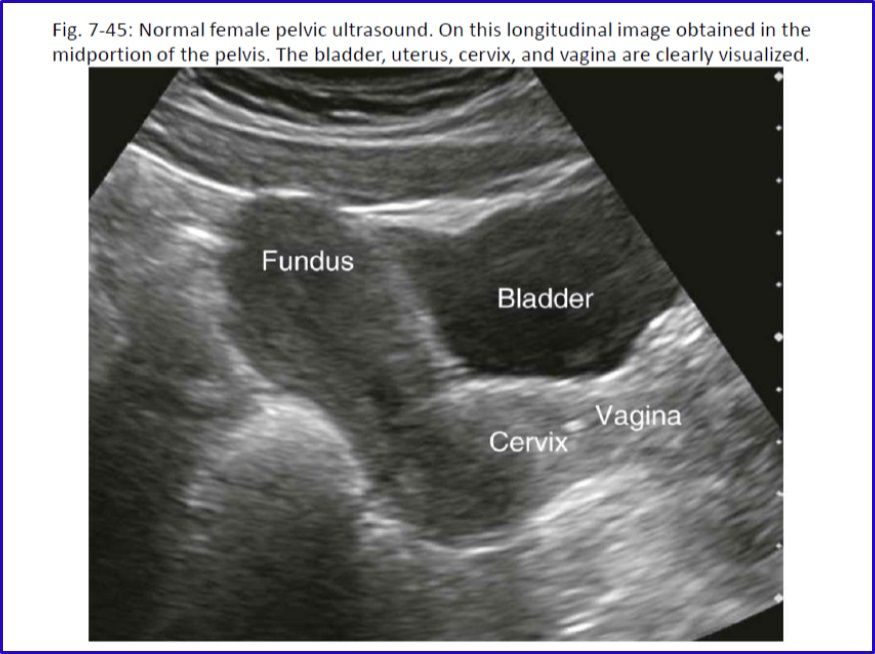
Hemoglobin and hematocrit levels help monitor the degree of blood loss.
A urinalysis can also be obtained. Urinary tract infection (UTI) has been associated with signs and symptoms of threatened abortion[24].
During the pelvic exam, suction or cotton swabs may be needed to remove blood and products of conception to allow for better visualization of the cervix. Ringed forceps can also be used to remove tissue that may be protruding from the cervical os. All tissue must be examined to determine if it is a clot or products of conception. Evidence of products of conception protruding from the cervix or within the vagina changes the diagnosis from a threatened abortion to a complete or incomplete abortion. Evaluation of the amount of bleeding/blood loss should be performed through a thorough history, as well as during the pelvic examination[25].
Treatment / Management
Alloimmunization prevention by the administration of Rh(D) immunoglobulin should be considered for patients who have vaginal bleeding in the setting of pregnancy in a patient who is Rh-[26]. It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
Patients with a threatened abortion should be managed expectantly without any medical or surgical interventions. However, patients should be given strict return precautions concerning excessive vaginal bleeding, abdominal pain, or fever and patients should be educated on the importance of follow-up. Analgesia can be provided to help relieve discomfort from cramping. NSAIDs should be avoided in the setting of a threatened abortion, as the pregnancy may continue to progress to viability[27]. Follow-up is recommended with serial transvaginal ultrasounds until a viable intrauterine pregnancy is confirmed or until progression to an inevitable, incomplete, or complete abortion occurs. Clinicians can consider serial quantitative beta hCG testing as recommended for a pregnancy of unknown origin to continue to monitor for the viability of the pregnancy, especially in the setting where an intrauterine pregnancy with cardiac activity has not been confirmed by ultrasound[28]. In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22]. The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding.
Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation. [31][32][33][34]
Differential Diagnosis
Clinicians should consider several differential diagnoses when encountering vaginal bleeding in the setting of pregnancy. Vulvar, vaginal, cervical trauma should be ruled out during a pelvic examination. Cervical friability can lead to vaginal bleeding which can be caused by cervicitis from an infection or due to premalignant or malignant changes on the cervix. Clinical judgment should determine whether or not the patient should undergo a Pap smear and/or cultures for infection at the time of examination. Other types of abortion should be considered including elective, inevitable, incomplete, complete, septic, and missed abortion[25].
Prognosis
Studies have shown that about 20% of women experience vaginal bleeding before 20 weeks of pregnancy. Furthermore, about 50% of those patients who experience a threatened abortion progress to a pregnancy loss. Studies have shown that there may be an increased risk of adverse outcomes later in pregnancy if there was vaginal bleeding during the first trimester of that pregnancy. For example, there may be a greater risk of placenta previa, placental abruption, necessitation for manual removal of the placenta after delivery, cesarean delivery, preterm premature ruptured membranes, preterm birth, low-birthweight infant, fetal-growth restriction, and fetal or neonatal death. [2]
Complications
Pregnancy loss (progression to inevitable, incomplete, complete, missed abortion)
Heavy bleeding
Retained products of conception
Endometritis
Septic abortion
Complications later in pregnancy as discussed in "Prognosis" [20]
Consultations
Patients with recurrent pregnancy loss or recurrent bleeding during pregnancy should be offered evaluation by a reproductive endocrinology and infertility specialist and/or by a maternal-fetal medicine specialist. If a patient is determined to have a coagulopathy, a hematology consult should be considered[10].
Deterrence and Patient Education
Patient education should be provided as both verbal and written explanations and instructions. It should be explained to the patient that it is possible her pregnancy will continue and it is also possible that she will undergo a miscarriage. The patient needs to understand that the vast majority of miscarriages are not preventable and that she is not at fault for the loss of the pregnancy if a loss does occur[35]. Providers should explain to the patient that mild to moderate bleeding and cramping can be expected, but uncontrolled pain or heavy bleeding should be evaluated by an obstetric care provider or in the emergency department. Many providers explain that saturating more than 1-2 pads per hour for 2 hours is considered to be heavy bleeding and should be promptly evaluated[36]. Patients can be instructed to take acetaminophen as directed for pain relief. Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety. Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Pearls and Other Issues
Most patients with a threatened abortion can be observed from home with close follow-up. Repeat ultrasounds and beta-hCG levels will help to determine progression to a viable pregnancy or to an inevitable, complete, incomplete, or missed abortion. Patients with increased vaginal bleeding require evaluation for hemorrhagic anemia and may be candidates for a blood transfusion or pregnancy evacuation[38].
Enhancing Healthcare Team Outcomes
The diagnosis and management of a threatened abortion involve an interprofessional team that can include an emergency department physician, obstetrician, radiologist, midlevel providers, and nursing staff. For patients to be safely monitored expectantly, good communication between clinicians and the patient is key. All members of the care team need to be on the same page regarding the possibility of pregnancy loss and the importance of return precautions[39].
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Alves C, Rapp A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 18, 2022. Spontaneous Abortion. [PubMed: 32809356]
- 2.
Redinger A, Nguyen H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 27, 2022. Incomplete Abortions. [PubMed: 32644497]
- 3.
de Codt M, Balza C, Jadoul P, Forget P, Squifflet JL, Bernard P, Luyckx M. Hysteroscopic Resection for Missed Abortion: Feasibility, Operative Technique and Potential Benefit Compared to Curettage. Front Surg. 2020;7:64.
[PMC free article: PMC7505996] [PubMed: 33102514]
- 4.
Karataşlı V, Kanmaz AG, İnan AH, Budak A, Beyan E. Maternal and neonatal outcomes of adolescent pregnancy. J Gynecol Obstet Hum Reprod. 2019 May;48(5):347-350. [PubMed: 30794955]
- 5.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019 Feb 01;99(3):166-174. [PubMed: 30702252]
- 6.
Goodarzi P, Falahzadeh K, Aghayan H, Payab M, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Adibi H, Gilany K, Arjmand B. Therapeutic abortion and ectopic pregnancy: alternative sources for fetal stem cell research and therapy in Iran as an Islamic country. Cell Tissue Bank. 2019 Mar;20(1):11-24. [PubMed: 30535614]
- 7.
Boiko VI, Nikitina IM, Babar TV, Boiko AV. The problem of miscarriage in multiple pregnancy. Wiad Lek. 2018;71(7):1195-1199. [PubMed: 30448784]
- 8.
Yang J, Chen M, Ye X, Chen F, Li Y, Li N, Wu W, Sun J.
A cross-sectional survey of pregnant women's knowledge of chromosomal aneuploidy and microdeletion and microduplication syndromes. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:82-90. [PubMed: 33176246]
- 9.
Weghofer A, Barad DH, Darmon SK, Kushnir VA, Albertini DF, Gleicher N. Euploid miscarriage is associated with elevated serum C-reactive protein levels in infertile women: a pilot study. Arch Gynecol Obstet. 2020 Mar;301(3):831-836. [PMC free article: PMC7060953] [PubMed: 32107607]
- 10.
Devall AJ, Coomarasamy A. Sporadic pregnancy loss and recurrent miscarriage. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:30-39. [PubMed: 32978069]
- 11.
Wierzejska R, Wojda B. Folic acid supplementation in pregnancy and prevention of fetal neural tube defects. Przegl Epidemiol. 2020;74(2):362-369. [PubMed: 33115226]
- 12.
du Fossé NA, van der Hoorn MP, van Lith JMM, le Cessie S, Lashley EELO. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis.
Hum Reprod Update. 2020 Sep 01;26(5):650-669. [PMC free article: PMC7456349] [PubMed: 32358607]
- 13.
Carp HJA. Progestogens and pregnancy loss. Climacteric. 2018 Aug;21(4):380-384. [PubMed: 29565684]
- 14.
Wahabi HA, Fayed AA, Esmaeil SA, Bahkali KH. Progestogen for treating threatened miscarriage. Cochrane Database Syst Rev. 2018 Aug 06;8(8):CD005943. [PMC free article: PMC6513446] [PubMed: 30081430]
- 15.
Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018 Jan;220:122-131. [PubMed: 29207325]
- 16.
Xu J, Chen M, Liu QY, Hu SQ, Li LR, Li J, Ma RM. Detecting trisomy in products of conception from first-trimester spontaneous miscarriages by next-generation sequencing (NGS). Medicine (Baltimore). 2020 Jan;99(5):e18731. [PMC free article: PMC7004681] [PubMed: 32000376]
- 17.
Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019 Sep 15;100(6):357-364. [PubMed: 31524362]
- 18.
Stewart KT, Lee JS, Pan K, Albert AY, Fisher S. Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: a retrospective cohort study. Eur J Contracept Reprod Health Care. 2020 Dec;25(6):474-479. [PubMed: 32869658]
- 19.
Long Y, Zhu H, Hu Y, Shen L, Fu J, Huang W. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020 Jul 01;7(7):CD011174. [PMC free article: PMC7389314] [PubMed: 32609376]
- 20.
Storey A, White K, Treder K, Woodhams E, Bell S, Cannon R. First-Trimester Abortion Complications: Simulation Cases for OB/GYN Residents in Sepsis and Hemorrhage. MedEdPORTAL. 2020 Oct 16;16:10995. [PMC free article: PMC7566226] [PubMed: 33094159]
- 21.
Mj G, K B, R M, G D.
Abdominal ectopic pregnancy with implantation on the rectum. Ulster Med J. 2020 Sep;89(2):101-102. [PMC free article: PMC7576386] [PubMed: 33093695]
- 22.
Pereira PP, Cabar FR, Gomez ÚT, Francisco RPV. Pregnancy of unknown location. Clinics (Sao Paulo). 2019;74:e1111. [PMC free article: PMC6784610] [PubMed: 31618321]
- 23.
Yoham AL, Casadesus D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 23, 2022. Rho(D) Immune Globulin. [PubMed: 32491807]
- 24.
Gágyor I, Strube-Plaschke S, Rentzsch K, Himmel W. Management of urinary tract infections: what do doctors recommend and patients do? An observational study in German primary care. BMC Infect Dis. 2020 Nov 09;20(1):813. [PMC free article: PMC7650164] [PubMed: 33167875]
- 25.
Milman T, Walker M, Thomas J. Pregnancy of unknown location. CMAJ. 2020 Sep 28;192(39):E1132. [PMC free article: PMC7532014] [PubMed: 32989026]
- 26.
Mayekar RV, Paradkar GV, Bhosale AA, Sachan R, Beeram S, Anand AR, Mundle SR, Trivedi Y, Md R, Patole KP, Sambarey PW, Daftary GV, John J, Divekar GH.
Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial. Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]
- 27.
Zafeiri A, Mitchell RT, Hay DC, Fowler PA. Over-the-counter analgesics during pregnancy: a comprehensive review of global prevalence and offspring safety. Hum Reprod Update. 2021 Jan 04;27(1):67-95. [PubMed: 33118024]
- 28.
Grenache DG. Current Practices When Reporting Quantitative Human Chorionic Gonadotropin Test Results. J Appl Lab Med. 2020 Sep 01;5(5):850-857. [PubMed: 32761058]
- 29.
Ali S, Majid S, Niamat Ali M, Taing S, El-Serehy HA, Al-Misned FA. Evaluation of etiology and pregnancy outcome in recurrent miscarriage patients. Saudi J Biol Sci. 2020 Oct;27(10):2809-2817. [PMC free article: PMC7499272] [PubMed: 32994741]
- 30.
Walsh CA. Maternal activity restriction to reduce preterm birth: Time to put this fallacy to bed.
Aust N Z J Obstet Gynaecol. 2020 Oct;60(5):813-815. [PubMed: 32691407]
- 31.
Morin L, Cargill YM, Glanc P. Ultrasound Evaluation of First Trimester Complications of Pregnancy. J Obstet Gynaecol Can. 2016 Oct;38(10):982-988. [PubMed: 27720100]
- 32.
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, Delabaere A, Gallot V, Iraola E, Lavoue V, Legendre G, Lejeune-Saada V, Leveque J, Nedellec S, Nizard J, Quibel T, Subtil D, Vialard F, Lemery D., Collège National des Gynécologues Obstétriciens Français. Pregnancy loss: French clinical practice guidelines. Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26. [PubMed: 27039249]
- 33.
Mellerup N, Sørensen BL, Kuriigamba GK, Rudnicki M. Management of abortion complications at a rural hospital in Uganda: a quality assessment by a partially completed criterion-based audit. BMC Womens Health. 2015 Sep 20;15:76. [PMC free article: PMC4576397] [PubMed: 26388296]
- 34.
Schindler AE, Carp H, Druckmann R, Genazzani AR, Huber J, Pasqualini J, Schweppe KW, Szekeres-Bartho J. European Progestin Club Guidelines for prevention and treatment of threatened or recurrent (habitual) miscarriage with progestogens. Gynecol Endocrinol. 2015 Jun;31(6):447-9. [PubMed: 25976550]
- 35.
Diamanti A, Papadakis S, Schoretsaniti S, Rovina N, Vivilaki V, Gratziou C, Katsaounou PA. Smoking cessation in pregnancy: An update for maternity care practitioners. Tob Induc Dis. 2019;17:57. [PMC free article: PMC6770622] [PubMed: 31582946]
- 36.
Shamsi S, Mirza TT, Shejuti TR, Nigar K, Nahar S, Begum S, Sharmin T, Panna LK, Islam N, Jahan T. An Overview of Unsafe Abortion: Patterns and Outcomes in a Tertiary Level Hospital. Mymensingh Med J. 2020 Jul;29(3):523-529. [PubMed: 32844789]
- 37.
Smith C, Hashmi SS, Czerwinski J, Wagner VF, Promecene P, Milentijevic I, Ramdaney A. The impact of genetic counseling on women's grief and coping following termination of pregnancy for fetal anomaly.
J Genet Couns. 2021 Apr;30(2):522-532. [PubMed: 33103308]
- 38.
Bondick CP, M Das J, Fertel H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 3, 2022. Subchorionic Hemorrhage. [PubMed: 32644443]
- 39.
Ogunyemi D, Haltigin C, Vallie S, Ferrari TM. Evolution of an obstetrics and gynecology interprofessional simulation-based education session for medical and nursing students. Medicine (Baltimore). 2020 Oct 23;99(43):e22562. [PMC free article: PMC7581067] [PubMed: 33120744]
Threatened Abortion - StatPearls - NCBI Bookshelf
Continuing Education Activity
A threatened abortion is vaginal bleeding during pregnancy that does not meet diagnostic criteria for spontaneous abortion. In a threatened abortion, the cervical os remains closed. The World Health Organization (WHO) defines a threatened abortion as pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation. A threatened abortion can present during early pregnancy with lower abdominal pain, and/or vaginal bleeding. Nearly 25 percent of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50 percent of these progress to an actual abortion. The bleeding in a threatened abortion is mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. This activity examines when this condition should be considered on differential diagnosis and how to properly evaluate it. This activity highlights the role of the interprofessional team in caring for patients with this condition.
Objectives:
Outline threatened abortion.
Summarize the differences between threatened abortion and other abortion types including elective, inevitable, incomplete, complete, or missed.
Explain how to manage a patient presenting with a threatened abortion.
Describe how the facilitation of interprofessional team education and discussion can optimize the effective detection of a threatened abortion and inform the need for subsequent evaluations.
Access free multiple choice questions on this topic.
Introduction
Abortion is the medical term for a pregnancy loss before 20 weeks of gestational age. The types of spontaneous abortion include threatened, inevitable, incomplete, complete, septic, and missed abortion[1].
A threatened abortion is defined as vaginal bleeding before 20 weeks gestational age in the setting of a positive urine and/or blood pregnancy test with a closed cervical os, without passage of products of conception and without evidence of a fetal or embryonic demise. The definition of a threatened abortion by the World Health Organization (WHO) is pregnancy-related bloody vaginal discharge or frank bleeding during the first half of pregnancy without cervical dilatation[2].
Other types of abortion should be considered if the cervical os is open, if there is determined to be an extrauterine pregnancy, if there is determined to be an intrauterine pregnancy without a fetal heartbeat, or if there is evidence of the passage of products of conception[3].
Nearly 25% of pregnant women have some degree of vaginal bleeding during the first two trimesters and about 50% of these progress to loss of the pregnancy. The bleeding during a threatened abortion is typically mild to moderate. The abdominal pain may present as intermittent cramps, suprapubic pain, pelvic pressure, or lower back pain. [4][5][6][7]
Etiology
The exact etiology of a threatened or spontaneous abortion is not always known. It is widely accepted that the vast majority of spontaneous abortions cannot be prevented or modified likely because they are due to chromosomal abnormalities in at least half of all cases[8]. For pregnancy losses that are determined to have a normal chromosomal makeup, termed euploid abortions, maternal and paternal factors play a more significant role[9]. Optimization of maternal health before pregnancy, correcting structural abnormalities of the uterus, and minimizing exposure to teratogens or infections during early pregnancy can reduce the risks for spontaneous abortion[10]. When optimizing maternal health, special consideration should be given to chronic illnesses such as diabetes and thyroid disease, as well as extremes of weight and use of tobacco products, alcohol, or illicit drugs. Some studies have shown that folic acid supplementation immediately before and during early pregnancy may reduce the risk of spontaneous abortionf[11]. It has also been shown in several studies that increasing paternal age is associated with increased risk for pregnancy loss, likely due to increased chromosomal abnormalities[12]. Women should also be educated about reducing the risk of traumatic events and should be screened for risk for intimate partner violence. It is reasonable to recommend preconception counseling to modify these risk factors. [6][13][14][15]
Epidemiology
Threatened abortion can occur in any pregnancy regardless of maternal age, race, comorbidities, lifestyle, or socioeconomic status[10]. If a woman has previously had bleeding in the first trimester of pregnancy, her risk of bleeding in the first trimester of subsequent pregnancies does appear to be increased. Risk factors for any type of miscarriage include advanced maternal age, advanced paternal age, prior history of pregnancy loss, TORCH infections, uncontrolled hyperglycemia, obesity, uncontrolled thyroid disease, significant stressors, use of teratogenic medications, and presence of a subchorionic hemorrhage[12].
Pathophysiology
A threatened abortion occurs when a pregnant patient at less than 20 weeks gestation presents with vaginal bleeding. The cervical os is closed on a physical exam. The patient may also experience abdominal cramping, pelvic pain, pelvic pressure, and/or back pain. Vaginal bleeding usually begins first followed by cramping abdominal pain hours to days later. Bleeding is the most predictive risk factor for pregnancy loss. More than half of threatened abortions will abort. The risk of spontaneous abortion, in a patient with threatened abortion, is less if fetal cardiac activity is present[1].
Histopathology
It is strongly recommended that all products of conception from any type of abortion are considered for histopathological examination. For patients with repeat pregnancy loss, karyotyping should be given as an option for products of conception to rule in or rule out chromosomal abnormalities as likely cause of spontaneous abortion. This information can help patients determine the best options for moving forward if they desire future pregnancies[16].
History and Physical
A pelvic exam is mandatory to determine the type of abortion. Determining factors include the amount and site of bleeding, whether the cervix is dilated, and whether fetal tissue has passed. In a threatened abortion, the vaginal exam may reveal a closed cervical os with no tissue. There is usually no cervical motion tenderness[17]. In rare cases, the pelvic exam will reveal uterine and bilateral adnexal tenderness. It is important to note that in a threatened abortion there is no passage of tissue and the cervical os is, by definition, closed[2]. These observations differentiate the condition from an inevitable or incomplete abortion. Women with a threatened abortion usually have stable vital signs, but if hypovolemia is present, one should suspect bleeding or sepsis. The abdomen in most cases is non-tender and soft. If it is confirmed that there is no viable fetus, a discussion concerning expectant management or induction of abortion should occur with the patient. The method of inducing abortion is either surgical with a suction dilation and curettage or medical with a medication like misoprostol[18][19].
Evaluation
The diagnosis is made by history, physical exam, measurement of beta-human chorionic gonadotropin (beta-hCG), and an ultrasound[10].
A thorough history should be obtained including pregnancy history, medical history, and history of present illness. History of present illness should include when and how symptoms/bleeding began, modifying factors, any treatments trialed up to the point of evaluation, and helping the patient to describe and quantify the bleeding[20][5].
Transvaginal ultrasound may be used to locate the pregnancy and determine if the fetus is viable. The ultrasound can also help rule out ectopic pregnancy and to evaluate for retained products of conception. A yolk sac is typically seen at 36 days, and a heartbeat is seen on ultrasound at approximately 45 days after the last menstruation[21].
A beta-hCG level of 1500 lU/mL to 2000 lU/mL is associated with a gestational sac on ultrasound. Beta-hCG doubles in 48 hours in 85% of intrauterine pregnancies. Beta-hCG is usually detectable the first nine to 11 days following ovulation and reaches 200 IU/mL at the expected time of menses[22].
Rh factor will also determine if Rhogam should be administered to prevent hemolytic disease of the newborn in this pregnancy and subsequent pregnancies[23].
Hemoglobin and hematocrit levels help monitor the degree of blood loss.
A urinalysis can also be obtained. Urinary tract infection (UTI) has been associated with signs and symptoms of threatened abortion[24].
During the pelvic exam, suction or cotton swabs may be needed to remove blood and products of conception to allow for better visualization of the cervix. Ringed forceps can also be used to remove tissue that may be protruding from the cervical os. All tissue must be examined to determine if it is a clot or products of conception. Evidence of products of conception protruding from the cervix or within the vagina changes the diagnosis from a threatened abortion to a complete or incomplete abortion. Evaluation of the amount of bleeding/blood loss should be performed through a thorough history, as well as during the pelvic examination[25].
Treatment / Management
Alloimmunization prevention by the administration of Rh(D) immunoglobulin should be considered for patients who have vaginal bleeding in the setting of pregnancy in a patient who is Rh-[26]. It has been determined that a 50 mcg dose of immunoglobulin is effective at alloimmunization prevention up to and through the 12th week of gestation, however, it is considered acceptable to give the standard 300 mcg dose due to availability or provider preference[23].
Patients with a threatened abortion should be managed expectantly without any medical or surgical interventions. However, patients should be given strict return precautions concerning excessive vaginal bleeding, abdominal pain, or fever and patients should be educated on the importance of follow-up. Analgesia can be provided to help relieve discomfort from cramping. NSAIDs should be avoided in the setting of a threatened abortion, as the pregnancy may continue to progress to viability[27]. Follow-up is recommended with serial transvaginal ultrasounds until a viable intrauterine pregnancy is confirmed or until progression to an inevitable, incomplete, or complete abortion occurs. Clinicians can consider serial quantitative beta hCG testing as recommended for a pregnancy of unknown origin to continue to monitor for the viability of the pregnancy, especially in the setting where an intrauterine pregnancy with cardiac activity has not been confirmed by ultrasound[28]. In these cases, it is possible that the pregnancy has not reached the gestational age by which cardiac activity would be expected on ultrasound or it is possible that the pregnancy will not be viable[22].
The patient should be counseled about the possibility of spontaneous abortion of the pregnancy, as well as the possibility that the pregnancy may continue to progress towards viability. Several trials have shown that progesterone supplementation does not improve outcomes for patients with threatened abortion and progesterone is not currently recommended as treatment or prevention for patients with threatened abortion.[29] Bedrest and other activity restrictions have not been found to be efficacious in the prevention of a threatened abortion progressing to spontaneous abortion and have been shown to increase the risk of other complications including deep vein thrombosis and/or pulmonary embolism and therefore should not be recommended[30]. Some providers do prefer to advise patients to avoid strenuous activities and to maintain pelvic rest at least until the cessation of vaginal bleeding. Clinicians should recommend that patients start or continue to take prenatal vitamins with folic acid supplementation.
[31][32][33][34]
Differential Diagnosis
Clinicians should consider several differential diagnoses when encountering vaginal bleeding in the setting of pregnancy. Vulvar, vaginal, cervical trauma should be ruled out during a pelvic examination. Cervical friability can lead to vaginal bleeding which can be caused by cervicitis from an infection or due to premalignant or malignant changes on the cervix. Clinical judgment should determine whether or not the patient should undergo a Pap smear and/or cultures for infection at the time of examination. Other types of abortion should be considered including elective, inevitable, incomplete, complete, septic, and missed abortion[25].
Prognosis
Studies have shown that about 20% of women experience vaginal bleeding before 20 weeks of pregnancy. Furthermore, about 50% of those patients who experience a threatened abortion progress to a pregnancy loss. Studies have shown that there may be an increased risk of adverse outcomes later in pregnancy if there was vaginal bleeding during the first trimester of that pregnancy. For example, there may be a greater risk of placenta previa, placental abruption, necessitation for manual removal of the placenta after delivery, cesarean delivery, preterm premature ruptured membranes, preterm birth, low-birthweight infant, fetal-growth restriction, and fetal or neonatal death. [2]
Complications
Pregnancy loss (progression to inevitable, incomplete, complete, missed abortion)
Heavy bleeding
Retained products of conception
Endometritis
Septic abortion
Complications later in pregnancy as discussed in "Prognosis" [20]
Consultations
Patients with recurrent pregnancy loss or recurrent bleeding during pregnancy should be offered evaluation by a reproductive endocrinology and infertility specialist and/or by a maternal-fetal medicine specialist. If a patient is determined to have a coagulopathy, a hematology consult should be considered[10].
Deterrence and Patient Education
Patient education should be provided as both verbal and written explanations and instructions. It should be explained to the patient that it is possible her pregnancy will continue and it is also possible that she will undergo a miscarriage. The patient needs to understand that the vast majority of miscarriages are not preventable and that she is not at fault for the loss of the pregnancy if a loss does occur[35]. Providers should explain to the patient that mild to moderate bleeding and cramping can be expected, but uncontrolled pain or heavy bleeding should be evaluated by an obstetric care provider or in the emergency department. Many providers explain that saturating more than 1-2 pads per hour for 2 hours is considered to be heavy bleeding and should be promptly evaluated[36]. Patients can be instructed to take acetaminophen as directed for pain relief. Patients should avoid ibuprofen for pain control during a threatened abortion as it is contraindicated in pregnancy and the patient's pregnancy may progress to viability. Patients who undergo threatened abortion should be evaluated for mood disorders including depression and anxiety.
Especially if a threatened abortion proceeds to pregnancy loss, the patient should be allowed to grieve as appropriate for each individual and should be offered grief counseling[37].
Pearls and Other Issues
Most patients with a threatened abortion can be observed from home with close follow-up. Repeat ultrasounds and beta-hCG levels will help to determine progression to a viable pregnancy or to an inevitable, complete, incomplete, or missed abortion. Patients with increased vaginal bleeding require evaluation for hemorrhagic anemia and may be candidates for a blood transfusion or pregnancy evacuation[38].
Enhancing Healthcare Team Outcomes
The diagnosis and management of a threatened abortion involve an interprofessional team that can include an emergency department physician, obstetrician, radiologist, midlevel providers, and nursing staff. For patients to be safely monitored expectantly, good communication between clinicians and the patient is key. All members of the care team need to be on the same page regarding the possibility of pregnancy loss and the importance of return precautions[39].
Review Questions
Access free multiple choice questions on this topic.
Comment on this article.
References
- 1.
Alves C, Rapp A. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jul 18, 2022. Spontaneous Abortion. [PubMed: 32809356]
- 2.
Redinger A, Nguyen H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Jun 27, 2022. Incomplete Abortions. [PubMed: 32644497]
- 3.
de Codt M, Balza C, Jadoul P, Forget P, Squifflet JL, Bernard P, Luyckx M. Hysteroscopic Resection for Missed Abortion: Feasibility, Operative Technique and Potential Benefit Compared to Curettage. Front Surg. 2020;7:64. [PMC free article: PMC7505996] [PubMed: 33102514]
- 4.
Karataşlı V, Kanmaz AG, İnan AH, Budak A, Beyan E. Maternal and neonatal outcomes of adolescent pregnancy. J Gynecol Obstet Hum Reprod. 2019 May;48(5):347-350. [PubMed: 30794955]
- 5.
Hendriks E, MacNaughton H, MacKenzie MC. First Trimester Bleeding: Evaluation and Management. Am Fam Physician. 2019 Feb 01;99(3):166-174. [PubMed: 30702252]
- 6.
Goodarzi P, Falahzadeh K, Aghayan H, Payab M, Larijani B, Alavi-Moghadam S, Tayanloo-Beik A, Adibi H, Gilany K, Arjmand B. Therapeutic abortion and ectopic pregnancy: alternative sources for fetal stem cell research and therapy in Iran as an Islamic country. Cell Tissue Bank. 2019 Mar;20(1):11-24. [PubMed: 30535614]
- 7.
Boiko VI, Nikitina IM, Babar TV, Boiko AV. The problem of miscarriage in multiple pregnancy. Wiad Lek. 2018;71(7):1195-1199. [PubMed: 30448784]
- 8.
Yang J, Chen M, Ye X, Chen F, Li Y, Li N, Wu W, Sun J. A cross-sectional survey of pregnant women's knowledge of chromosomal aneuploidy and microdeletion and microduplication syndromes. Eur J Obstet Gynecol Reprod Biol. 2021 Jan;256:82-90. [PubMed: 33176246]
- 9.
Weghofer A, Barad DH, Darmon SK, Kushnir VA, Albertini DF, Gleicher N.
Euploid miscarriage is associated with elevated serum C-reactive protein levels in infertile women: a pilot study. Arch Gynecol Obstet. 2020 Mar;301(3):831-836. [PMC free article: PMC7060953] [PubMed: 32107607]
- 10.
Devall AJ, Coomarasamy A. Sporadic pregnancy loss and recurrent miscarriage. Best Pract Res Clin Obstet Gynaecol. 2020 Nov;69:30-39. [PubMed: 32978069]
- 11.
Wierzejska R, Wojda B. Folic acid supplementation in pregnancy and prevention of fetal neural tube defects. Przegl Epidemiol. 2020;74(2):362-369. [PubMed: 33115226]
- 12.
du Fossé NA, van der Hoorn MP, van Lith JMM, le Cessie S, Lashley EELO. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: a systematic review and meta-analysis. Hum Reprod Update. 2020 Sep 01;26(5):650-669. [PMC free article: PMC7456349] [PubMed: 32358607]
- 13.
Carp HJA. Progestogens and pregnancy loss. Climacteric. 2018 Aug;21(4):380-384.
[PubMed: 29565684]
- 14.
Wahabi HA, Fayed AA, Esmaeil SA, Bahkali KH. Progestogen for treating threatened miscarriage. Cochrane Database Syst Rev. 2018 Aug 06;8(8):CD005943. [PMC free article: PMC6513446] [PubMed: 30081430]
- 15.
Pillai RN, Konje JC, Richardson M, Tincello DG, Potdar N. Prediction of miscarriage in women with viable intrauterine pregnancy-A systematic review and diagnostic accuracy meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2018 Jan;220:122-131. [PubMed: 29207325]
- 16.
Xu J, Chen M, Liu QY, Hu SQ, Li LR, Li J, Ma RM. Detecting trisomy in products of conception from first-trimester spontaneous miscarriages by next-generation sequencing (NGS). Medicine (Baltimore). 2020 Jan;99(5):e18731. [PMC free article: PMC7004681] [PubMed: 32000376]
- 17.
Curry A, Williams T, Penny ML. Pelvic Inflammatory Disease: Diagnosis, Management, and Prevention. Am Fam Physician. 2019 Sep 15;100(6):357-364.
[PubMed: 31524362]
- 18.
Stewart KT, Lee JS, Pan K, Albert AY, Fisher S. Outcome of using vaginal misoprostol for treatment of retained products of conception after first trimester miscarriage: a retrospective cohort study. Eur J Contracept Reprod Health Care. 2020 Dec;25(6):474-479. [PubMed: 32869658]
- 19.
Long Y, Zhu H, Hu Y, Shen L, Fu J, Huang W. Interventions for non-tubal ectopic pregnancy. Cochrane Database Syst Rev. 2020 Jul 01;7(7):CD011174. [PMC free article: PMC7389314] [PubMed: 32609376]
- 20.
Storey A, White K, Treder K, Woodhams E, Bell S, Cannon R. First-Trimester Abortion Complications: Simulation Cases for OB/GYN Residents in Sepsis and Hemorrhage. MedEdPORTAL. 2020 Oct 16;16:10995. [PMC free article: PMC7566226] [PubMed: 33094159]
- 21.
Mj G, K B, R M, G D. Abdominal ectopic pregnancy with implantation on the rectum. Ulster Med J. 2020 Sep;89(2):101-102. [PMC free article: PMC7576386] [PubMed: 33093695]
- 22.
Pereira PP, Cabar FR, Gomez ÚT, Francisco RPV. Pregnancy of unknown location. Clinics (Sao Paulo). 2019;74:e1111. [PMC free article: PMC6784610] [PubMed: 31618321]
- 23.
Yoham AL, Casadesus D. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): May 23, 2022. Rho(D) Immune Globulin. [PubMed: 32491807]
- 24.
Gágyor I, Strube-Plaschke S, Rentzsch K, Himmel W. Management of urinary tract infections: what do doctors recommend and patients do? An observational study in German primary care. BMC Infect Dis. 2020 Nov 09;20(1):813. [PMC free article: PMC7650164] [PubMed: 33167875]
- 25.
Milman T, Walker M, Thomas J. Pregnancy of unknown location. CMAJ. 2020 Sep 28;192(39):E1132. [PMC free article: PMC7532014] [PubMed: 32989026]
- 26.
Mayekar RV, Paradkar GV, Bhosale AA, Sachan R, Beeram S, Anand AR, Mundle SR, Trivedi Y, Md R, Patole KP, Sambarey PW, Daftary GV, John J, Divekar GH. Recombinant anti-D for prevention of maternal-foetal Rh(D) alloimmunization: a randomized multi-centre clinical trial.
Obstet Gynecol Sci. 2020 May;63(3):315-322. [PMC free article: PMC7231934] [PubMed: 32489976]
- 27.
Zafeiri A, Mitchell RT, Hay DC, Fowler PA. Over-the-counter analgesics during pregnancy: a comprehensive review of global prevalence and offspring safety. Hum Reprod Update. 2021 Jan 04;27(1):67-95. [PubMed: 33118024]
- 28.
Grenache DG. Current Practices When Reporting Quantitative Human Chorionic Gonadotropin Test Results. J Appl Lab Med. 2020 Sep 01;5(5):850-857. [PubMed: 32761058]
- 29.
Ali S, Majid S, Niamat Ali M, Taing S, El-Serehy HA, Al-Misned FA. Evaluation of etiology and pregnancy outcome in recurrent miscarriage patients. Saudi J Biol Sci. 2020 Oct;27(10):2809-2817. [PMC free article: PMC7499272] [PubMed: 32994741]
- 30.
Walsh CA. Maternal activity restriction to reduce preterm birth: Time to put this fallacy to bed. Aust N Z J Obstet Gynaecol. 2020 Oct;60(5):813-815. [PubMed: 32691407]
- 31.
Morin L, Cargill YM, Glanc P. Ultrasound Evaluation of First Trimester Complications of Pregnancy. J Obstet Gynaecol Can. 2016 Oct;38(10):982-988. [PubMed: 27720100]
- 32.
Huchon C, Deffieux X, Beucher G, Capmas P, Carcopino X, Costedoat-Chalumeau N, Delabaere A, Gallot V, Iraola E, Lavoue V, Legendre G, Lejeune-Saada V, Leveque J, Nedellec S, Nizard J, Quibel T, Subtil D, Vialard F, Lemery D., Collège National des Gynécologues Obstétriciens Français. Pregnancy loss: French clinical practice guidelines. Eur J Obstet Gynecol Reprod Biol. 2016 Jun;201:18-26. [PubMed: 27039249]
- 33.
Mellerup N, Sørensen BL, Kuriigamba GK, Rudnicki M. Management of abortion complications at a rural hospital in Uganda: a quality assessment by a partially completed criterion-based audit. BMC Womens Health. 2015 Sep 20;15:76. [PMC free article: PMC4576397] [PubMed: 26388296]
- 34.
Schindler AE, Carp H, Druckmann R, Genazzani AR, Huber J, Pasqualini J, Schweppe KW, Szekeres-Bartho J.
European Progestin Club Guidelines for prevention and treatment of threatened or recurrent (habitual) miscarriage with progestogens. Gynecol Endocrinol. 2015 Jun;31(6):447-9. [PubMed: 25976550]
- 35.
Diamanti A, Papadakis S, Schoretsaniti S, Rovina N, Vivilaki V, Gratziou C, Katsaounou PA. Smoking cessation in pregnancy: An update for maternity care practitioners. Tob Induc Dis. 2019;17:57. [PMC free article: PMC6770622] [PubMed: 31582946]
- 36.
Shamsi S, Mirza TT, Shejuti TR, Nigar K, Nahar S, Begum S, Sharmin T, Panna LK, Islam N, Jahan T. An Overview of Unsafe Abortion: Patterns and Outcomes in a Tertiary Level Hospital. Mymensingh Med J. 2020 Jul;29(3):523-529. [PubMed: 32844789]
- 37.
Smith C, Hashmi SS, Czerwinski J, Wagner VF, Promecene P, Milentijevic I, Ramdaney A. The impact of genetic counseling on women's grief and coping following termination of pregnancy for fetal anomaly. J Genet Couns. 2021 Apr;30(2):522-532.
[PubMed: 33103308]
- 38.
Bondick CP, M Das J, Fertel H. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Aug 3, 2022. Subchorionic Hemorrhage. [PubMed: 32644443]
- 39.
Ogunyemi D, Haltigin C, Vallie S, Ferrari TM. Evolution of an obstetrics and gynecology interprofessional simulation-based education session for medical and nursing students. Medicine (Baltimore). 2020 Oct 23;99(43):e22562. [PMC free article: PMC7581067] [PubMed: 33120744]
Threatened abortion. What is Threatened Abortion?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Threatened abortion is the risk of termination of pregnancy no later than 22 weeks of gestation. The condition is accompanied by aching or pulling pain in the lower abdomen, the release of a small amount of blood, but the cervix retains its structure. Diagnosis is based on the complaints of the pregnant woman, clinical symptoms, examination, ultrasound data. The goal of treatment is to preserve the fetus and prolong childbearing as much as possible. Hormonal drugs, antispasmodics are used to relieve the tone of the myometrium, symptomatic treatment aimed at stopping bleeding. nine0006
ICD-10
O20.0 Threatened abortion
- Causes
- Pathogenesis
- Symptoms of threatened abortion
- Complications
- Diagnostics
- Treatment of threatened miscarriage
- Prognosis and prevention
- Prices for treatment
General
Clinical protocols recommend against using the term "threatened abortion" in order to reduce the psychological burden on a woman who is at risk of losing a desired pregnancy. Instead, it is proposed to call this condition a threatened miscarriage. The definition includes cases when detachment of the fetal egg occurs at an early stage - up to 12 weeks. The appearance of uterine tone and bleeding from 12 to 22 weeks is considered a late threat of abortion. Later this period, similar symptoms are called the threat of premature birth. It is erroneously believed that a miscarriage is provoked by sexual activity, blunt abdominal trauma, and physical activity. The main causes are chromosomal abnormalities, infections, endocrine disorders. nine0006
Threatened abortion
Causes
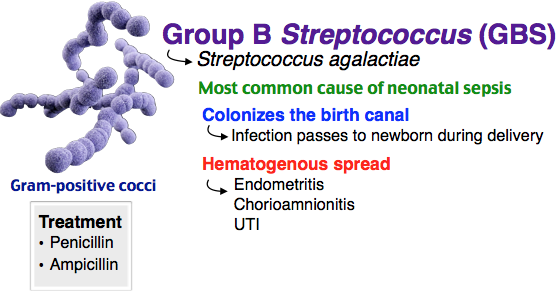
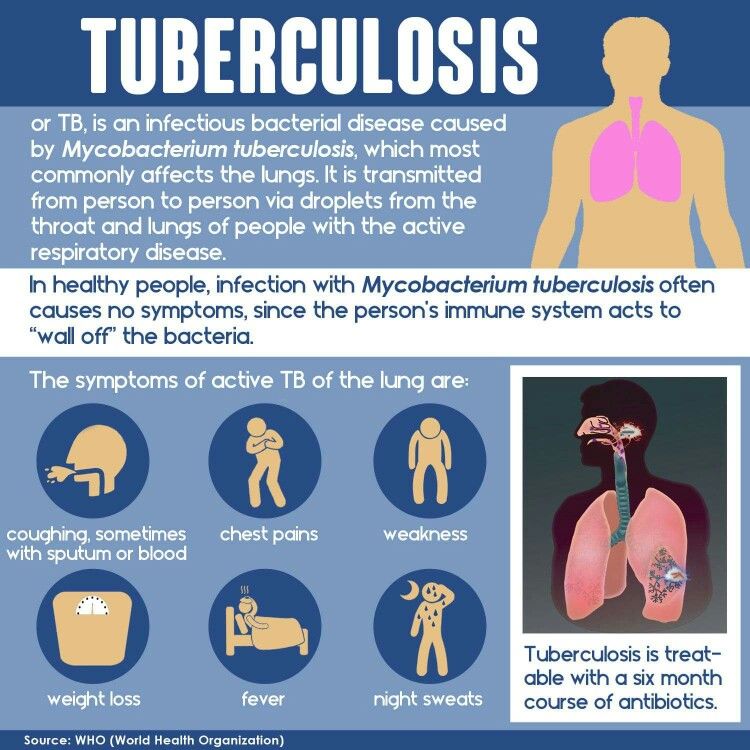
Spontaneous threat of termination of short-term pregnancy in 50% of patients is associated with chromosomal abnormalities of the embryo. After 16 weeks, threatened miscarriage is the result of genetic defects in 10% of cases. The shorter the gestational age, the higher the likelihood that a threatened abortion will turn into a spontaneous miscarriage. The infection can cause a violation of the development of the fetal egg and a threatening abortion in chronic endometritis, viral infection during childbearing. The danger is higher at an early stage, until the placenta is formed, which acts as a protective filter. nine0006
Allocate factors that significantly increase the risk of threatened abortion. They are associated with endogenous conditions, features of the lifestyle of the expectant mother. Of great importance are the transferred acute and chronic diseases, as well as the action of external stimuli and pathogens. These factors are taken into account when registering a woman with an obstetrician-gynecologist and managing pregnancy:
- Mother's age. In women aged 20-30, threatening abortion occurs in 9-15%, after 30 years this figure increases to 20%, and in 45-year-olds - up to 80%. Young girls under 18 years of age also often face the development of a threat of interruption of gestation due to the immature hypothalamic-pituitary system, physiological dysfunction of the ovaries.
nine0016
- Endocrine diseases of the mother. Pathology of the thyroid gland, uncompensated diabetes mellitus, polycystic ovary syndrome cause endocrine changes that worsen the condition of the endometrium, the production of hormones of the corpus luteum of the ovaries. Obesity leads to a change in the synthesis of steroid hormones, which leads to their imbalance.
- History of pregnancy loss. In women with recurrent miscarriage, the risk is 30%. If there was a history of normal childbirth and there are no spontaneous miscarriages, then the risk of interruption of gestation in a pregnant woman is only 5%. nine0016
- Taking medicines. The use of drugs with a teratogenic effect (retinoids, anticoagulants), large doses of non-steroidal anti-inflammatory drugs inhibit the synthesis of prostaglandins and impair embryo implantation, which can later cause a threat of miscarriage.
- Action of toxic substances. The threat of interruption of gestation may occur in women working in hazardous conditions, in hazardous industries.
Alcohol has a toxic effect on the endometrium and the fetus with systematic use, smoking 10 cigarettes a day, and cocaine use. Dose-dependent effect has coffee, soft drinks with caffeine. The danger is the use of 4-5 cups of strong drink or 100 mg of caffeine per day. nine0016
- Autoimmune diseases. Antiphospholipid syndrome, systemic lupus erythematosus are associated with the formation of antibodies to phospholipids and other cell structures. A woman is more prone to microthrombosis. Thrombi form in the vessels of the endometrium, which disrupts the nutrition of the embryo, leading to a threatening abortion or death of the fetal egg.
Pathogenesis
The mechanism of development of a threatened miscarriage is associated with an increase in the contractility of the uterus. In the event of an infection, the blood flow in the vessels that feed the embryo is disturbed, their spasm occurs. The embryo does not receive the right amount of nutrients and oxygen. At this stage, his death may occur. Spasm of microvessels leads to their rupture, there is a slight bleeding into the wall of the uterus, a retrochorial hematoma is formed. It exfoliates the fetal egg from the endometrium. If the bleeding is not stopped in time, a threatened abortion turns into a miscarriage in the course. Pregnancy loss in the 1st and early 2nd trimester occurs without rupture of the membranes. nine0006
Symptoms of threatened abortion
Unpleasant symptoms appear against the background of complete well-being. The pregnant woman begins to feel a feeling of discomfort in the lower abdomen, which gradually turns into a pulling, aching pain. The pain is localized indistinctly above the pubis, may radiate to the sacrum, lower back, perineum. With a threatened abortion, sensations do not turn into contractions, otherwise this indicates the progression of the pathology and a developing miscarriage.
Discharge from the genital tract at the initial stage may be absent. This is typical for the formation of a small hematoma behind the fetal egg, which is not emptied into the uterine cavity. If its detachment occurs along the edge, then the pregnant woman notices bloody spotting or bloody-bloody discharge on the linen, which looks like streaks of dark blood mixed with mucus. With the threat of a miscarriage, they do not transform into massive bleeding with scarlet or dark blood. Allocations appear several times a day, gradually their number decreases under the influence of therapy. If this does not happen, the progression of the pathology is assumed. nine0006
Violation of general well-being is not typical. Pain in the lower abdomen does not reduce the working capacity of the pregnant woman, but there is a desire to lie down and relax. Often this helps to reduce the intensity of discomfort. Increased pain is provoked by nervous experiences, physical activity or lack of proper rest. Sexual relations can also become a factor in the progression of threatened abortion.
Complications
If you do not contact a gynecologist in time, a threatening miscarriage can develop into an abortion in a move that cannot be stopped. In this case, severe cramping pains appear, which can lead to the opening of the cervix. At week 22, the fetus is not viable, so the birth leads to its death. Termination of pregnancy is accompanied by bleeding. A woman needs medical care to reduce the risk of massive blood loss, the addition of infectious complications. Temperature or signs of intoxication indicate a septic abortion. nine0006
An incomplete miscarriage is an incomplete process in which the fetus separates, but the fetal membranes remain in the uterus. This disrupts uterine contractions, the vessels of the uterus gape, so there is a high probability of bleeding. Complications of this condition can be hemorrhagic shock, DIC, endometritis. Inflammation of the mucous membrane in the future becomes the cause of infertility, resistant to treatment.
Diagnostics
If characteristic complaints appear, it is necessary to contact an obstetrician-gynecologist for examination and diagnosis. After confirming the diagnosis, hospitalization may be required for treatment and follow-up. Examination of a pregnant woman includes: nine0006
- Examination on a chair. Physical examination shows that the cervix is tightly closed, but there may be a small amount of brown discharge in the vagina. Bimanual examination does not cause pain, the vaginal vaults are free. On palpation, the uterus remains unexcitable, soft, but there is a slight soreness. The ovaries are not palpable.
- Laboratory diagnostics. Needed to evaluate ovarian function and monitor pregnancy. Blood is taken for hCG, to confirm a progressing pregnancy, the analysis is carried out in dynamics with an interval of several days. Determine the level of progesterone. According to the indications, an estrogen test may be prescribed. nine0016
- Ultrasound of the small pelvis.
The "gold standard" for diagnosing a threatened miscarriage is an ultrasound transvaginal probe, the accuracy of the technique is higher than in transabdominal examination. According to ultrasound, signs of fetal viability are determined. A fetal egg is visualized in the uterine cavity, a heartbeat is determined in the embryo or fetus. With doubtful results, the study is repeated twice by different specialists with an interval of 7-10 days.
Treatment of threatened miscarriage
A pregnant woman with bleeding and the threat of miscarriage in the short term should be urgently hospitalized in the gynecology department. She is assigned a medical-protective regime, it is not recommended to get out of bed. In some institutions, as an additional method of therapy, raising the foot end of the bed by 5 cm is practiced. Medication-preserving therapy is prescribed:
- Progesterone preparations. Use dydrogesterone or micronized progesterone. They are prescribed to maintain the function of the placenta according to an individual scheme.
For women who have had interruptions for a short period in the past, drugs are prescribed preventively until signs of danger appear. nine0016
- Estrogens. They are included in the treatment regimen from the 6th week of gestation, if, according to the results of the tests, their deficiency is revealed. Needed to improve the action of progesterone. The dosage is selected individually.
- Removal of uterine tone. For the relief of pain and muscle spasm in pregnant women, it is allowed to use drotaverine, papaverine. They are prescribed intramuscularly, later they switch to tablet forms. A solution of magnesium sulfate has a pronounced tocolytic effect. It is used to reduce uterine tone, lower blood pressure and improve fetal nutrition. nine0016
- Hemostatic therapy. To stop bleeding, sodium etamsylate is used in the form of a solution intramuscularly or intravenously. Aminocaproic and tranexamic acid are approved for use.
Prognosis and prevention
With timely access to an obstetrician-gynecologist and proper treatment, the prognosis is favorable. The fetus can be saved if the area of detachment of the fetal egg is small, the bleeding has stopped, and the hematoma gradually resolves. The remaining period of gestation, the woman is under the close supervision of a doctor in order to notice the deterioration in time and take measures to prevent complications. Prevention of threatening spontaneous abortion consists in preconception preparation, sanitation of foci of infection in the body. Women need to start taking folic acid and vitamin E 2 months before conception. nine0006
You can share your medical history, what helped you in the treatment of threatened abortion.
Sources
- Miscarriage in early pregnancy: diagnosis and management. Clinical guidelines / ed. Serova V.N. – 2016.
- Clinical guidelines. Obstetrics and gynecology / ed. Serova V.N., Sukhnya G.T. - 2014.
- Procedure for the provision of medical care in the profile "Obstetrics and Gynecology" / Order of the Ministry of Health of the Russian Federation dated November 1, 2012 No.
572n. nine0016
- This article was prepared based on the site materials: https://www.krasotaimedicina.ru/
IMPORTANT
Information from this section cannot be used for self-diagnosis and self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
Obstetrician-gynecologist of the Reproductive Health Center "SM-Clinic" told about whether it is possible not to notice a miscarriage
Unfortunately, the loss of a child at an early stage of pregnancy is quite common. After the first miscarriage, a woman lives in constant fear and is afraid that the second attempt to become a mother will turn into a tragedy.
“A miscarriage is the spontaneous termination of a pregnancy before the fetus reaches a viable term. A fetus weighing up to 500 g is considered viable, which corresponds to a period of less than 22 weeks of pregnancy. Many women face this diagnosis. About 80 percent of miscarriages occur before 12 weeks of pregnancy.” nine0005
Causes of miscarriage
Approximately half of early miscarriages occur due to genetic pathologies in the development of the fetus, that is, from defects in the number and composition of chromosomes. It is in the first weeks that the formation of the baby's organs begins, which requires 23 normal chromosomes from each of the future parents. When at least one abnormal changes occur, there is a risk of losing a child.
At 8-11 weeks the rate of such miscarriages is 41-50%, at 16-19 weeksweeks of pregnancy, the frequency of miscarriages caused by chromosomal defects drops to 10 to 20 percent.
There are other causes of miscarriage. Among them:
- Congenital and acquired disorders of the anatomy of the genital organs If there are fibroids, polyps in the uterus, this can cause abnormal development of the embryo.
- Infectious causes Numerous studies have shown that the risk of miscarriage increases in the presence of sexually transmitted infections. Dangerous for a pregnant woman are measles, rubella, cytomegalovirus, as well as diseases that occur with an increase in body temperature. Intoxication of the body often leads to the loss of a child.
- Endocrine causes Problems with gestation occur with diabetes, thyroid diseases, disorders of the adrenal glands.
- Unfavorable ecology, exposure
- Blood clotting disorder (thrombosis, antiphospholipid syndrome) APS (antiphospholipid syndrome) is a disease in which the human body produces a lot of antibodies to phospholipids, the chemical structures that make up parts of cells. The body mistakenly perceives its own phospholipids as foreign and begins to defend itself against them: it produces antibodies to them that damage blood components.
Is it possible not to notice a miscarriage
Sometimes women mistake a miscarriage for normal menstruation. This occurs during the so-called biochemical pregnancy, when there is a violation of the implantation of the embryo at a very early stage and menstruation begins. But before the appearance of spotting, the test will show two strips.
The classic variant is when a miscarriage is manifested by bleeding against the background of a long delay in menstruation, which rarely stops on its own. Therefore, even if a woman does not follow the menstrual cycle, the signs of an interrupted pregnancy will be immediately noticed by the doctor during examination and ultrasound. nine0005
Alarm
The symptoms of a miscarriage can be completely different, and depending on them, as a rule, it is possible to predict the likelihood of maintaining and successfully continuing this pregnancy.
For the threat of miscarriage is characterized by pulling pains in the lower abdomen and lumbar region, scanty bloody discharge from the genital tract. Ultrasound signs: the tone of the uterus is increased, the cervix is not shortened and closed, the body of the uterus corresponds to the gestational age, the fetal heartbeat is recorded. nine0006
Started miscarriage - pain and discharge from the genital tract are more pronounced, the cervix is ajar.
Miscarriage in progress - cramping pains in the lower abdomen, copious bloody discharge from the genital tract. On examination, as a rule, the uterus does not correspond to the gestational age, the cervix is open, the elements of the fetal egg are in the cervix or in the vagina.
Incomplete miscarriage - the pregnancy was interrupted, but there are delayed elements of the fetal egg in the uterine cavity. This is manifested by ongoing bleeding due to the lack of a full contraction of the uterus. nine0006
Non-progressive pregnancy - death of an embryo (before 9 weeks) or a fetus up to 22 weeks of gestation in the absence of any signs of termination of pregnancy.
Important!
Severe abdominal pain and spotting at any stage of pregnancy is a reason for an urgent appeal to an obstetrician-gynecologist with a solution to the issue of hospitalization in a gynecological hospital.
Is it possible to avoid miscarriage
“Today, there are no methods for preventing miscarriages,” the doctor says. “Therefore, it is very important to comprehensively prepare for pregnancy before it occurs by visiting an obstetrician-gynecologist and following all the necessary recommendations for examination and taking the necessary drugs. ”
But if, nevertheless, the pregnancy could not be maintained, then the birth of a child can be planned again no earlier than 3-6 months after the miscarriage. This time is needed to figure out, together with the attending physician, what are the causes of miscarriage and whether it is possible to avoid them in the future. nine0006
By the way, a common misconception for both women and men is that only the woman is to blame for the loss of pregnancy, but this is far from being the case.
“A man is also responsible, which is why future dads are required to perform a study - a spermogram and be screened for genital infections, since with a pathology of spermatozoa, the likelihood of miscarriage due to genetic abnormalities increases many times,” emphasizes our expert.
There is always a chance
Most women whose first pregnancy ends in a miscarriage, when examined before pregnancy and the causes are eliminated, have a high chance of a successful next pregnancy (about 85 percent).