Pregnancy and viral infection
Colds and the Flu | Respiratory Infections During Pregnancy
If you are pregnant, it’s important to take precautions against viral infections. A viral infection is a contagious illness. Most viruses will not hurt your baby. However, some viruses can cause miscarriage or birth defects in your baby. A virus can affect your respiratory tract (breathing) and can cause other symptoms. The flu and the common cold are examples of viral infections. Other examples are:
- chickenpox (varicella)
- fifth disease
- Cytomegalovirus
- rubella (also called German measles)
- Zika virus
Pregnant women can be exposed to people with viral infections. They spread directly through touching, kissing, or sexual activity. You can get them indirectly, through coughing or sneezing. They also spread through contact with infected surfaces, food, and water. This doesn’t mean you will become sick.
Path to improved health
Contact your doctor right away if you are pregnant and exposed to someone who has a viral infection. The doctor will want to know which virus and what type of contact you had. They also may ask about your symptoms.
Here are some questions your doctor may ask you:
- Did you touch or kiss the infected person?
- How long were you in contact with the infected person?
- When did the infected person get sick?
- Did a doctor diagnose the infected person’s illness? Were any tests done?
What if I’m exposed to influenza?
Influenza can be more serious for pregnant women. You may get very sick. However, it hardly ever causes birth defects in the baby. If you are pregnant during flu season (October through March), you should get a flu shot.
What should I do if I’m exposed to chickenpox?
Chickenpox is caused by the varicella virus and is highly contagious. It can be serious during pregnancy. Sometimes, chickenpox can cause birth defects. If you have had chickenpox in the past, it is unlikely you will catch it again. If you have not had chickenpox or if you are not sure, see your doctor.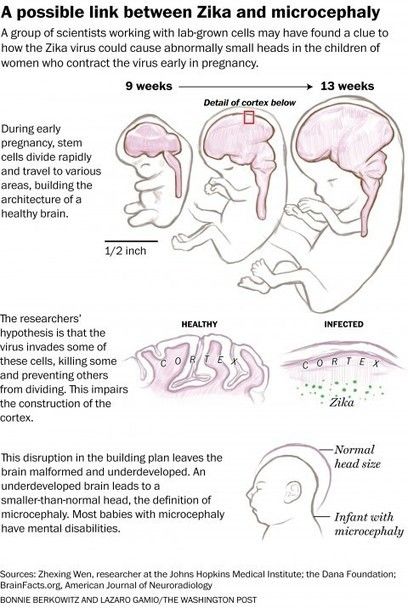 Your doctor will test your blood to see if you are immune.
Your doctor will test your blood to see if you are immune.
Many people who don’t remember having chickenpox are immune. If your blood test shows that you are not immune, you can take medicines to make your illness less severe and help protect your baby from chickenpox.
What should I do if I’m exposed to fifth disease?
Fifth disease is a common virus in children. About half of all adults are sensitive to fifth disease and can catch it from children.
Children who have fifth disease often get a rash on their body and have cold-like symptoms. Their cheeks may be red and look like they’ve been slapped or pinched. Adults who get fifth disease do not usually have the “slapped cheek” rash. Adults who contract fifth disease often have very sore joints.
If you get fifth disease early in your pregnancy, you could have a miscarriage. Fifth disease also can cause birth defects in your baby, such as severe anemia. Call your doctor if you are exposed to fifth disease. Your doctor may have you take a blood test to see if you’re immune. You also may need an ultrasound exam to see if the baby has been infected.
You also may need an ultrasound exam to see if the baby has been infected.
What if I’m exposed to cytomegalovirus?
Cytomegalovirus usually doesn’t cause any symptoms. This makes it hard to know if you have it. It is the most common infection that can be passed from mother to baby. Cytomegalovirus affects 1 of every 100 pregnant women. It can cause birth defects, such as hearing loss, development disabilities, or even death of the fetus.
It’s important to prevent cytomegalovirus because there is no way to treat it. Women who work in day care centers or a health care setting have the highest risk of getting infected. Pregnant women with these jobs should wash their hands after handling diapers and avoid snuggling or kissing the babies. If you think you’ve been exposed to a person who has cytomegalovirus, see your doctor right away.
What if I’m exposed to rubella?
Since 1969, almost all children have had the rubella vaccine, so it is a rare disease today. At the first prenatal visit, all pregnant women should be tested to see if they are immune to rubella. Women who are not immune should get the vaccine after the baby is born. Talk to your doctor if you are trying to become pregnant. Then you can get the vaccine in advance if you are not immune.
At the first prenatal visit, all pregnant women should be tested to see if they are immune to rubella. Women who are not immune should get the vaccine after the baby is born. Talk to your doctor if you are trying to become pregnant. Then you can get the vaccine in advance if you are not immune.
Symptoms of rubella in adults are joint pain and a possible ear infection. The virus can cause severe birth defects or death of the fetus. Talk to your doctor if you have these symptoms or have been exposed.
What if I’m exposed to Zika virus?
The Zika virus is a travel-related virus that can cause birth defects if a woman is exposed during pregnancy. Zika outbreaks have been reported in South America, Central America, and North America. The virus can cause microcephaly (the baby’s head and brain are smaller than normal. This causes an intellectual disability). The infection is transmitted through an infected mosquito bite or is passed to a woman through sexual contact. Women who are pregnant or hope to become pregnant should avoid travel to these regions and use a condom during sex if your partner has traveled to the area. Your doctor will tell you how long you must wait before trying to become pregnant if your partner has been exposed to the virus.
Your doctor will tell you how long you must wait before trying to become pregnant if your partner has been exposed to the virus.
Things to consider
Most other viruses do not seem to increase the natural risk for birth defects. This includes viruses such as regular measles, mumps, roseola, mononucleosis (“mono”), and bronchiolitis. In normal pregnancies, the risk of serious birth defects is 2% to 3%.
To protect yourself from all infectious viruses:
- Wash your hands frequently, especially after using the restroom or before a meal.
- Avoid contact with people who are knowingly infected.
- Get a flu shot and other vaccines either before or during pregnancy, as needed.
When to see your doctor
Contact your doctor right away if you have been exposed to an infected person or have symptoms of a virus. They can provide treatment, if possible, and monitor your baby for signs of infection.
Questions to ask your doctor
- How do I know if I’ve been exposed to someone infected with a virus?
- What can I do to prevent exposure?
- How do I know if I’m immune to certain viruses?
- At what point should I get a flu shot?
- Are there any other vaccines I should get before or during pregnancy?
- What should I do once I become exposed to a harmful virus?
Infections in pregnancy that may affect your baby
Throughout life, we all encounter many viruses and bacteria.
This page is about infections that can cause problems in pregnancy, their symptoms and what to do if you're worried.
Chickenpox in pregnancy
Chickenpox infection in pregnancy can be dangerous for both you and your baby, so it's important to seek advice early if you think you may have chickenpox.
There's a 90% chance you are immune to chickenpox infection. But if you've never had chickenpox (or you're unsure if you've had it) and you come into contact with a child or adult who does, speak to your GP, obstetrician or midwife immediately. A blood test will find out if you're immune.
CMV in pregnancy
CMV (cytomegalovirus) is a common virus that's part of the herpes group, which can also cause cold sores and chickenpox. CMV infections are common in young children.
Infection can be dangerous during pregnancy as it can cause problems for unborn babies, such as hearing loss, visual impairment or blindness, learning difficulties and epilepsy.
CMV is particularly dangerous to the baby if the pregnant mother has not had the infection before.
It's not always possible to prevent a CMV infection, but you can reduce the risk by:
- washing your hands regularly with soap and hot water, particularly if you have been changing nappies, or work in a nursery or daycare centre
- not kissing young children on the face – it's better to kiss them on the head or give them a hug
- not sharing food or cutlery with young children, and not drinking from the same glass as them
This is particularly important if you have a job that brings you into close contact with young children. In this case, you can have a blood test to find out whether you have previously been infected with CMV.
Find out more about cytomegalovirus
Group B streptococcus in pregnancy
Group B streptococcus (GBS, or group B strep) rarely causes harm or symptoms.
It causes no problem in most pregnancies but, in a small number, group B strep infects the baby, usually just before or during labour, leading to serious illness.
If you've already had a baby who had a GBS infection, you should be offered antibiotics during labour to reduce the chances of your new baby getting the infection. You should also be offered them during labour if you've had a group B strep urinary tract infection during the pregnancy.
GBS infection of the baby is more likely if:
- you go into premature labour (before 37 weeks of pregnancy)
- your waters break early
- you have a fever during labour
- you currently carry GBS
Your midwife or doctor will assess whether you should be offered antibiotics during labour to protect your baby from being infected.
It's possible to be tested for GBS late in pregnancy. Talk to your doctor or midwife if you have concerns.
Infections transmitted by animals
Cats
Cat faeces may contain toxoplasma – an organism that causes toxoplasmosis. Toxoplasmosis can harm your baby.
To reduce the risk of infection:
- avoid emptying cat litter trays while you're pregnant
- if nobody else can empty the litter tray, use disposable rubber gloves – trays should be cleaned daily
- avoid close contact with sick cats
- even if you do not have a cat, wear gloves if gardening in case the soil is contaminated with faeces
- wash your hands and gloves after gardening
- if you do come into contact with cat faeces, wash your hands thoroughly
- follow general food hygiene rules – see how to prepare food safely and how to store food safely
Sheep
Lambs and sheep can carry an organism that is known to cause miscarriage in ewes.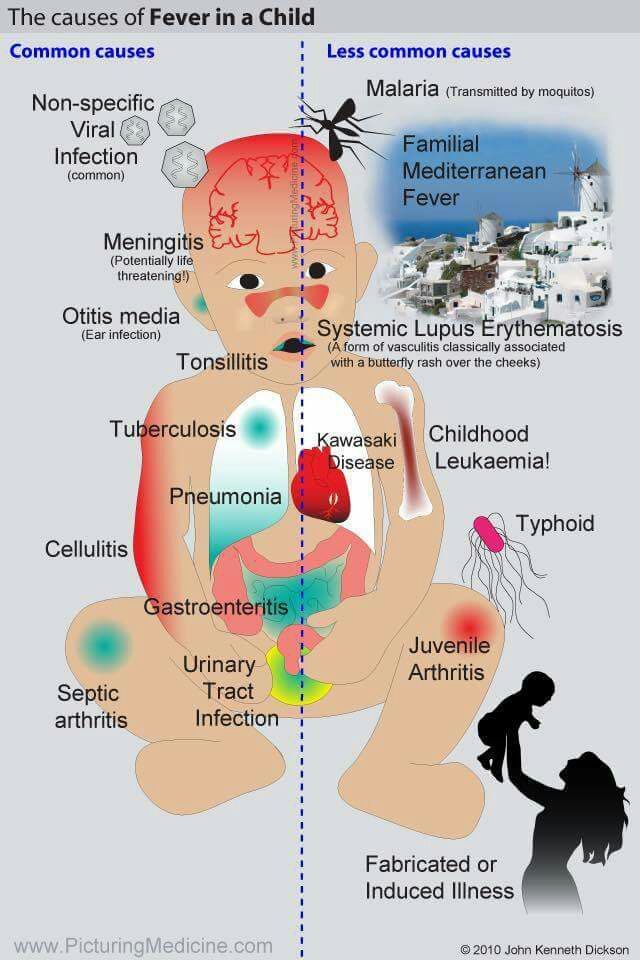 They also carry toxoplasma.
They also carry toxoplasma.
Avoid lambing or milking ewes, as well all contact with newborn lambs. Tell your doctor if you experience flu-like symptoms after coming into contact with sheep.
Pigs
Research is ongoing to see if pigs can be a source of hepatitis E infection. This infection is dangerous if you're pregnant.
Prevent infections by:
- cooking meat and meat products thoroughly
- avoid eating raw or undercooked meat and shellfish
- washing your hands thoroughly before preparing, serving and eating food
Find more information on hepatitis E on GOV.UK
Hepatitis B
Hepatitis B is a virus that infects the liver. Many people with hepatitis B will show no sign of illness, but they can be carriers and may infect others.
The virus is spread by having sex with an infected person without using a condom, and by direct contact with infected blood. If you have hepatitis B or are infected during pregnancy, you can pass the infection on to your baby at birth.
You'll be offered a blood test for hepatitis B as part of your antenatal care. Babies who are at risk should be given the hepatitis B vaccine at birth to prevent infection and serious liver disease later on in life.
Hepatitis C
The hepatitis C virus infects the liver. Many people with hepatitis C have no symptoms and are unaware they are infected. The virus is transmitted by direct contact with infected blood.
In people who take illegal drugs, this can be a result of sharing blood-contaminated needles.
People who received a blood transfusion in the UK prior to September 1991, or blood products prior to 1986, may also be at risk.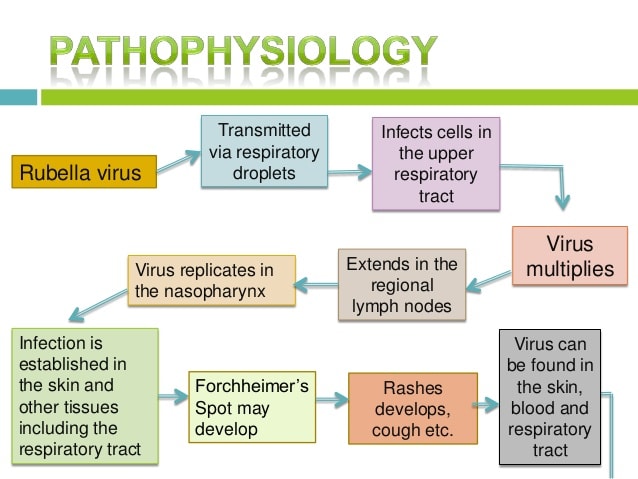
Hepatitis C can also be transmitted by receiving medical or dental treatment in countries where hepatitis C is common and infection control may be poor, or by having sex with an infected partner.
If you have hepatitis C, you may pass the infection on to your baby, although the risk is much lower than with hepatitis B or HIV. This cannot currently be prevented.
Your baby can be tested for hepatitis C and, if they're infected, they can be referred for specialist assessment.
Herpes in pregnancy
Genital herpes infection can be dangerous for a newborn baby.
You can get herpes through genital contact with an infected person or from oral sex with someone who has cold sores (oral herpes).
Initial infection causes painful blisters or ulcers on the genitals. Less severe outbreaks usually occur for some years afterwards.
Treatment is available if your first infection occurs in pregnancy. If your first infection occurs near the end of pregnancy or during labour, a caesarean section may be recommended to reduce the risk of passing herpes on to your baby.
If you or your partner have herpes, use condoms or avoid sex during an outbreak. Avoid unprotected oral sex as herpes is very easy to pass on.
Tell your midwife or doctor if either you or your partner have recurring herpes or develop sores.
HIV in pregnancy
You'll be offered a confidential HIV (human immunodeficiency virus) test as part of your routine antenatal care. Your midwife or doctor will discuss the test with you, and counselling will be available if the result is positive.
Read more about screening for HIV in pregnancy
Current evidence suggests that if you're HIV positive, in good health and without symptoms of the infection you're unlikely to be adversely affected by pregnancy.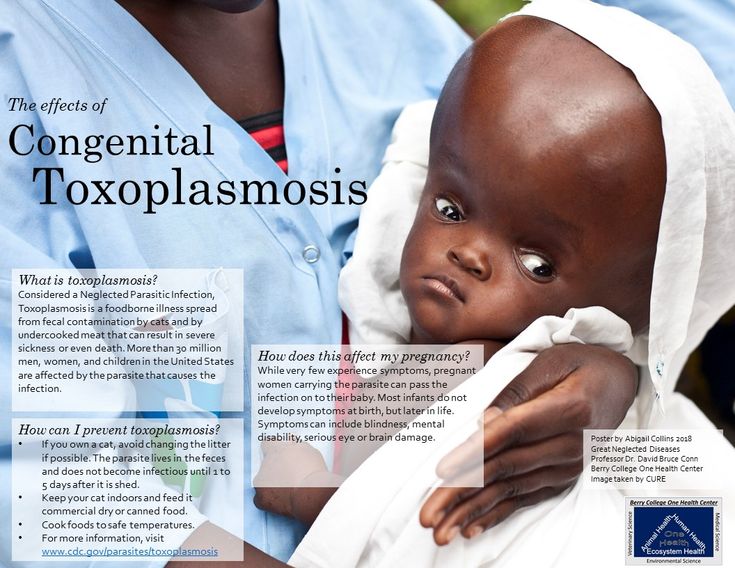
However, HIV can be passed to your baby during pregnancy, birth, breastfeeding or chestfeeding.
If you're diagnosed with HIV, you and your doctor will need to discuss the management of your pregnancy and birth to reduce the risk of infection for your baby.
Treatment in pregnancy greatly reduces the risk of passing on HIV to the baby – from 1 in 4 to fewer than 1 in 100. Your baby will be tested for HIV at birth and at regular intervals for 18 months.
You'll be advised not to breastfeed or chestfeed, as HIV can be transmitted to your baby in this way.
If you're HIV positive, talk to your doctor or midwife about your own health and the options open to you. You can also contact organisations such as Positively UK or the Terrence Higgins Trust for information and support.
The British HIV Association has more information on HIV and pregnancy
Video: HIV and pregnancy
This video explores Sarah's story of HIV and pregnancy.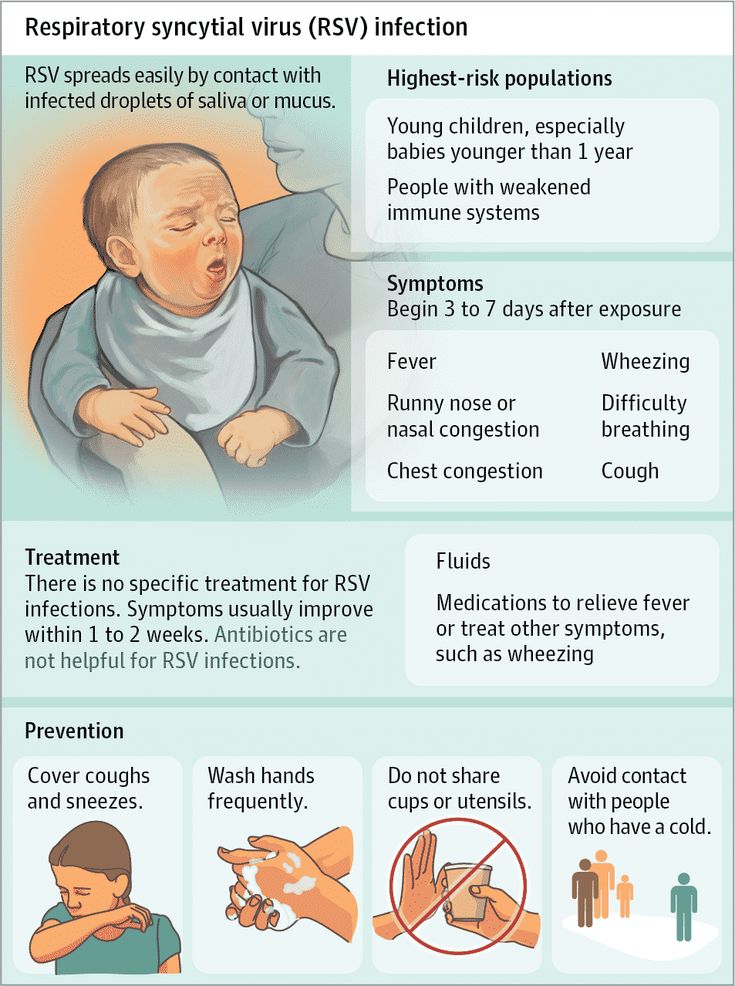
Media last reviewed: 16 November 2020
Media review due: 16 November 2023
Slapped cheek syndrome in pregnancy
Slapped cheek syndrome is common in children. It typically causes a rash on the face.
Slapped cheek syndrome is highly infectious and can be harmful to the baby.
If you come into contact with anyone who is infected, you should talk to your doctor, who can carry out a blood test to check whether you're immune. In most cases, the baby is not affected if you have slapped cheek syndrome.
Rubella (german measles) in pregnancy
Rubella is rare in the UK thanks to the high uptake of MMR (measles, mumps and rubella) vaccination.
But if you develop rubella in the first 4 months of pregnancy, it can lead to serious problems, including birth defects and miscarriage.
If you're pregnant, you should contact your GP or midwife as soon as possible if:
- you come into contact with someone who has rubella
- you have a rash or come into contact with anyone who does
- you have symptoms of rubella
It's unlikely you have rubella in these circumstances, but you may need a blood test to check.
If you're pregnant and are not sure whether you've had 2 doses of the MMR vaccine, ask your GP practice to check your vaccination history.
If you have not had both doses or there's no record, you should ask for the vaccine when you go for your 6-week postnatal check after the birth. This will protect you in any future pregnancies.
MMR vaccine cannot be given during pregnancy.
STIs in pregnancy
STIs often have no symptoms, so you may not know if you have one.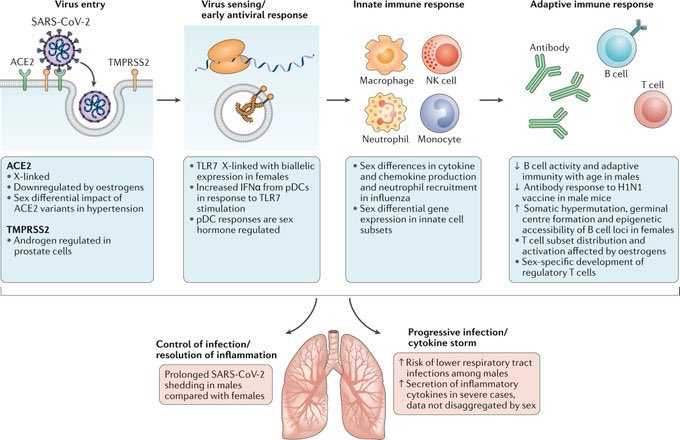 However, many STIs can affect your baby's health both during pregnancy and after the birth.
However, many STIs can affect your baby's health both during pregnancy and after the birth.
If you have any reason to believe you or your partner may have an STI, go for a check-up as soon as possible. You can ask your GP or midwife. If you prefer, you can go to a sexual health clinic. Confidentiality is guaranteed.
Find a sexual health service near you
If you're under 25, you can also visit a Brook centre for free confidential advice. You may also be able to order a free chlamydia test online.
Zika virus
The Zika virus can cause birth defects if you catch it while pregnant. In particular, it can cause the baby to have an abnormally small head (microcephaly).
Zika does not naturally occur in the UK. Seek travel health advice before your trip if you plan to go to an affected area, such as:
- South or Central America
- the Caribbean
- southeast Asia
- the Pacific region – for example, Fiji
While pregnant, it's recommended that you postpone non-essential travel to high-risk areas.
Get information on the country-specific risk on GOV.UK
It is also recommended that you avoid getting pregnant while travelling and for 3 months after returning to the UK.
Zika is spread by mosquitoes. You can reduce your risk of mosquito bites by using insect repellent and wearing loose clothing that covers your arms and legs.
Influenza and SARS in pregnant women
HomeFor patientsInformation Influenza and SARS in pregnant women
Viral infections are now regarded as one of the main causes of reproductive losses. On the one hand, the infectious agent has a direct damaging effect on the fetus, and on the other hand, causing significant changes in the immune responses of the mother's body, leads to a complicated course of pregnancy. A special place among infectious diseases of pregnant women is occupied by influenza and other acute respiratory viral infections transmitted by airborne droplets.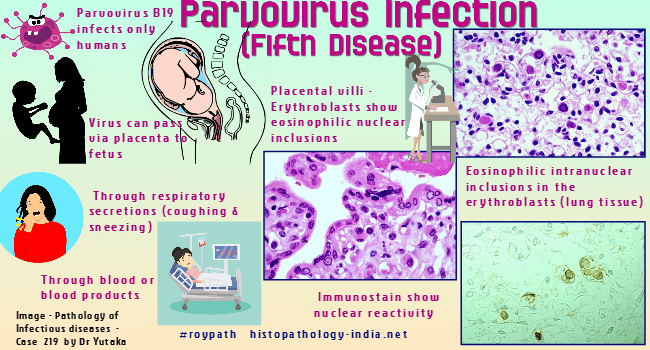 nine0003
nine0003
The urgency of the problem of acute respiratory diseases of a viral nature is determined by their prevalence, uncontrollability, high contagiousness, allergization and the development of secondary immunodeficiency states after an illness.
The ecological features of modern urbanization provide a real basis for the frequent encounter of women with various respiratory viruses during the entire period of pregnancy. In extragenital pathology of pregnant women, acute respiratory infections occupy the first place in terms of prevalence - more than 2/3 of the total incidence of acute infections. This is due to the high susceptibility of pregnant women to viral infections, the tendency to chronicity of pathological processes, which is due to the peculiarities of the immunity of pregnant women. nine0003
The impact of viral infection on the course of pregnancy and the condition of the fetus is characterized by two main mechanisms. Firstly, the possible infection of the placenta, amniotic membranes, as well as the fetus itself, teratogenic (causing malformations) effect on the embryo and fetus, the development of local lesions of the fetus, as well as infection of the fetus with clinical manifestations in the postnatal period (after birth). Secondly, a possible indirect effect as a result of the development of a pregnant fever, a violation of homeostasis (balance, constancy) in the body, etc. , and the fetus. nine0003
Secondly, a possible indirect effect as a result of the development of a pregnant fever, a violation of homeostasis (balance, constancy) in the body, etc. , and the fetus. nine0003
The main links in the pathogenesis of a viral infection in a pregnant woman, which determine the high risk of perinatal pathology, are:
Activation of the blood coagulation system by the toxic effect of the virus on the vascular wall;
Pathological changes in the immune system resulting from a viral infection; nine0003
Activation of chronic intrauterine infection.
The possibility of transmission of respiratory group viruses, which include viruses that cause ARVI, through the placenta from a sick mother to a fetus has been proven, which leads to the involvement of all three components of the mother-placenta-fetus system in the infectious process.
Modern researchers consider gestosis (toxicosis of the second half of pregnancy), including its severe forms, as a causal factor of placental insufficiency (PI), a direct relationship between the severity of late gestosis and the severity of PI has been proven. Recent studies have confirmed the assumption that the placenta serves as a kind of "reservoir" in the process of intrauterine infection, as it has been proven that under the influence of viruses, some structures of the placenta change, and viruses reproduce in them. nine0003
Recent studies have confirmed the assumption that the placenta serves as a kind of "reservoir" in the process of intrauterine infection, as it has been proven that under the influence of viruses, some structures of the placenta change, and viruses reproduce in them. nine0003
Specific prophylaxis of influenza does not eliminate the problem of respiratory viral infections, since the share of ARVI of non-influenza etiology is up to 75% even during influenza epidemic periods. In addition, the physiological changes in the immune system that occur in the body of pregnant women do not allow them to use vaccine preparations to prevent infectious diseases.
The risk group for ARVI infection includes women who had the incidence of these infections more than three times in the previous year of pregnancy. This sign is a classic confirmation of immunological deficiency in the patient. They are characterized by: a protracted, recurrent course of diseases (rhinitis, pharyngitis, laryngotracheitis, bronchitis), the presence of foci of chronic infection (chronic tonsillitis, sinusitis). In the pathological process in such patients, to one degree or another, other body systems are also involved, which ensure its protection when it encounters the external environment. The most common pathology of the digestive tract: from dysfunctions and dysbiosis to chronic colitis, enteritis, enterocolitis, pancreatitis and cholecystitis. nine0003
In the pathological process in such patients, to one degree or another, other body systems are also involved, which ensure its protection when it encounters the external environment. The most common pathology of the digestive tract: from dysfunctions and dysbiosis to chronic colitis, enteritis, enterocolitis, pancreatitis and cholecystitis. nine0003
Features of the course of SARS in pregnant women
Pregnant women are characterized by a protracted course of SARS in the absence of severe clinical manifestations. This is due to the ability of respiratory group viruses to reproduce in the placenta, as well as the peculiarity of the immune system of the pregnant woman (a state of physiological immunodeficiency).
The main clinical symptoms of acute respiratory infections: symptoms of general intoxication (malaise, weakness, increased fatigue, etc.) against the background of subfebrile or normal temperature, symptoms of rhinitis or nasopharyngitis. nine0003
The most typical ARVI clinic for pregnant women is often the reason for insufficient attention to the very fact of the disease, both on the part of doctors and the woman herself, however, ARVI leads to a breakdown in physiological immune mechanisms and does not exclude the possibility of complications during pregnancy.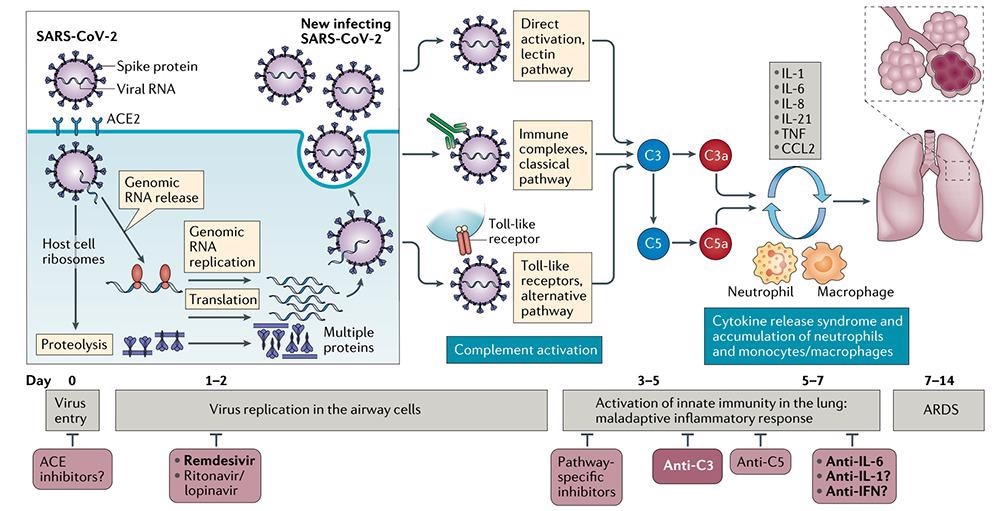
Features of pregnancy after SARS. Influence of acute respiratory viral infections in pregnant women on the health of their newborns
The most typical complications of pregnancy after acute respiratory viral infections are:
- more than double the incidence of placental insufficiency;
- increase in cases of early onset of preeclampsia;
- oligohydramnios - as a concomitant sign of placental insufficiency, as well as a manifestation of viral damage to the fetoplacental complex;
- the threat of premature termination of pregnancy is more common in the 2nd trimester, namely at 17-26 weeks, for pregnant women after ARVI, a constant course of the threat of termination of pregnancy is characteristic, insensitive to ongoing standard therapy; nine0048
- intrauterine growth retardation and intrauterine fetal hypoxia;
- increase in neonatal morbidity:
- hypoxic lesion of the central nervous system is most characteristic of acute respiratory viral infections in the 2nd trimester;
- chronic placental insufficiency (inflammatory and degenerative changes in the placenta, impaired differentiation of placental tissue, suppression of compensatory-adaptive vascular reactions of chorionic villi).

Characteristics of the state of the immune system of pregnant women after SARS
When studying the state of systemic immunity in pregnant women who had ARVI, depending on the duration of pregnancy, in comparison with similar indicators in healthy pregnant women, the following patterns were revealed.
Past ARVI causes changes in the immune status, is characterized, as a rule, by changes in the content of leukocytes and lymphocytes and their populations. A characteristic sign of the immunogram of pregnant women who have had ARVI is lymphocytopenia (destruction of lymphocytes), while during the physiological development of pregnancy, an increase in the total number of leukocytes occurs. Lymphocytopenia can be explained by the direct damaging effect of respiratory viruses on lymphoid cells, its degree depends both on the virulent properties of the viral pathogen and on the adaptive capabilities of the organism. nine0003
The effect of viruses on immunological reactivity lies in the fact that in the course of infection, not one, but a series of indicators characterizing the immune response of the organism affected by the virus to foreign antigens changes.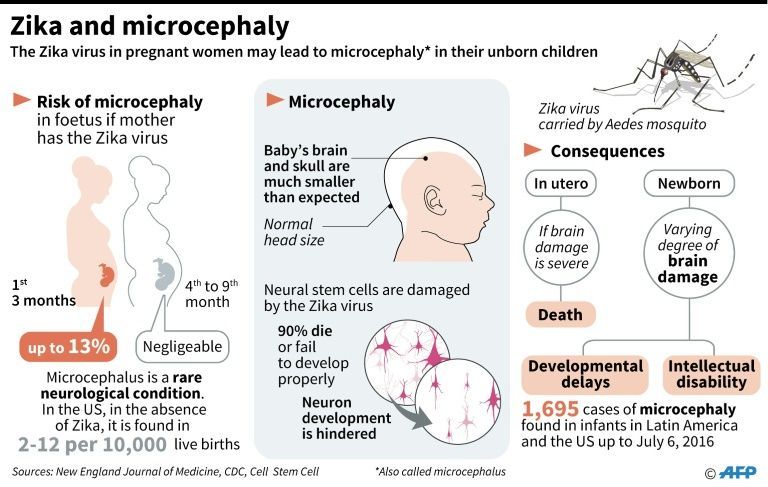 There is a disorder of immunological reactivity, caused by a violation of all the functions of immunocompetent cells as a result of the reproduction of the virus.
There is a disorder of immunological reactivity, caused by a violation of all the functions of immunocompetent cells as a result of the reproduction of the virus.
The occurrence of defects in immunological reactivity should be considered as an essential element of the pathogenesis of ARVI. The presence of these defects does not prevent the formation of specific immunity against the homologous virus. nine0003
Methods of prevention and treatment of acute respiratory viral infections in pregnant women
It is known that specific prevention of influenza and acute respiratory viral infections by vaccine preparations is contraindicated during pregnancy. Researchers both here and abroad pay attention to the search and implementation in practice of methods of non-specific protection of the population from respiratory viral infections. It should be noted that one of the most promising methods of viral infection tactics is immunocorrection. From this point of view, the use of modern immunobiological preparations, adaptogens and eubiotics, is promising. nine0003
nine0003
Therapeutic measures with the use of immunotropic drugs are carried out after ARVI in the 2-3 trimesters of pregnancy, as well as 10-14 days before the expected date of delivery in the following groups of patients:
- diseases more than 3 times in the previous year of pregnancy;
- pregnant women who had ARVI with a complicated course of pregnancy;
- in the presence of a positive prognosis for the development of perinatal pathology. nine0048
Preventive measures
All pregnant women should refrain as much as possible from visiting public places with a large crowd of people in case of a threat and an epidemic of influenza and SARS.
Pregnant women with acute respiratory infections three or more times a year prior to pregnancy should be classified as a high risk group for the development of complications.
This group of patients, as well as all pregnant women with the threat and occurrence of an epidemic of influenza and SARS, need to undergo a course of non-specific prophylaxis. nine0003
nine0003
The use of vitamin-mineral complexes helps to form an antiviral immune response, they protect the cell membrane from the damaging effect of an infectious agent (vitamins A, C, E; trace elements selenium, magnesium, iron), phytotherapy can also be used.
Preventive measures are necessary for women at high risk of ARVI at the stage of preconception preparation and from the first trimester of pregnancy, as well as for all pregnant women with the threat of an influenza epidemic and ARVI at any stage of pregnancy. nine0003
Orvi during pregnancy - is it dangerous?
Pregnancy of most women falls during the SARS season. People around are coughing, sneezing, and it is almost impossible to protect yourself from the ubiquitous infection. Out of habit, expectant mothers endure a mild cold, at best at home with plenty of warm drinks, and at worst, on their feet. Unfortunately, what goes easily outside of pregnancy can create additional risks for the baby and expectant mother.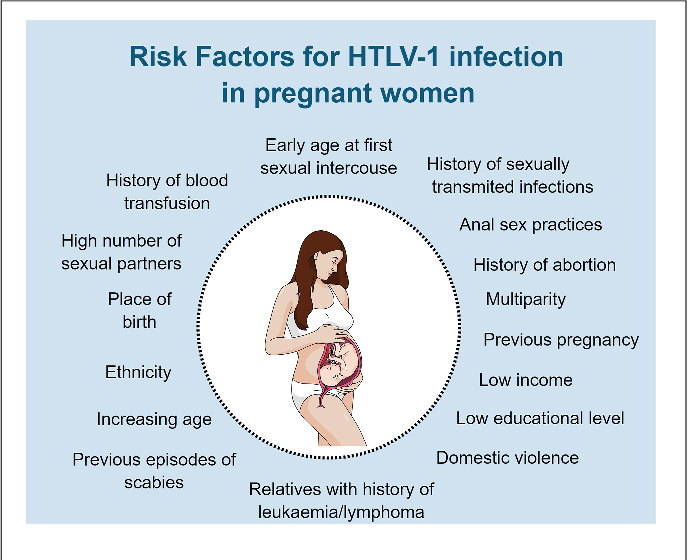
VIRUSES AND IMMUNITY IN PREGNANCY
Only influenza and COVID-19 are considered dangerous SARS. But for pregnant women, even typical seasonal diseases can create increased risks, which usually go away on their own in 7-10 days. These are adenoviruses, rhinoviruses, respiratory syncytial virus, parainfluenza - more than 200 species in total.
The reason is a decrease in the overall immune defense of the body under the influence of hormones. Pregnancy hormones suppress the mother's immune defenses so that her body does not reject the baby. The flip side of this is vulnerability to previously harmless infections. nine0003
The main target of infections in pregnant women is the placenta. This delicate organ is a convenient place for viruses to multiply. He has a good blood supply, the cells have the receptors necessary for the attachment of many viruses. The result is inflammation, and, as a result, problems for both the mother and the fetus.
The second not quite common target for viruses that usually affect the upper respiratory tract - the kidneys.
WHAT IS THE COMMON COLD?
It happens that a cold during pregnancy passes without negative consequences, but unfortunately, problems also arise quite often. nine0003
Since viruses primarily affect the placenta, this can lead to placental insufficiency (impaired circulation between the placenta and the fetus). The blood of mother and child does not come into direct contact. Oxygen for the baby is transferred through the placenta. In the same place, maternal red blood cells take up carbon dioxide. If part of the placenta is inflamed, this affects gas exchange.
Fetoplacental insufficiency develops in 62.9% of women who had ARVI during pregnancy. Most often, the damage is small, and the mother's body can compensate for it. Therefore, the fetus clearly suffers from oxygen starvation only in 45.2% of those who have had a cold. Intrauterine growth retardation occurs even less often - in 26.7%. nine0003
The most dangerous complication - intrauterine infection - develops in 27.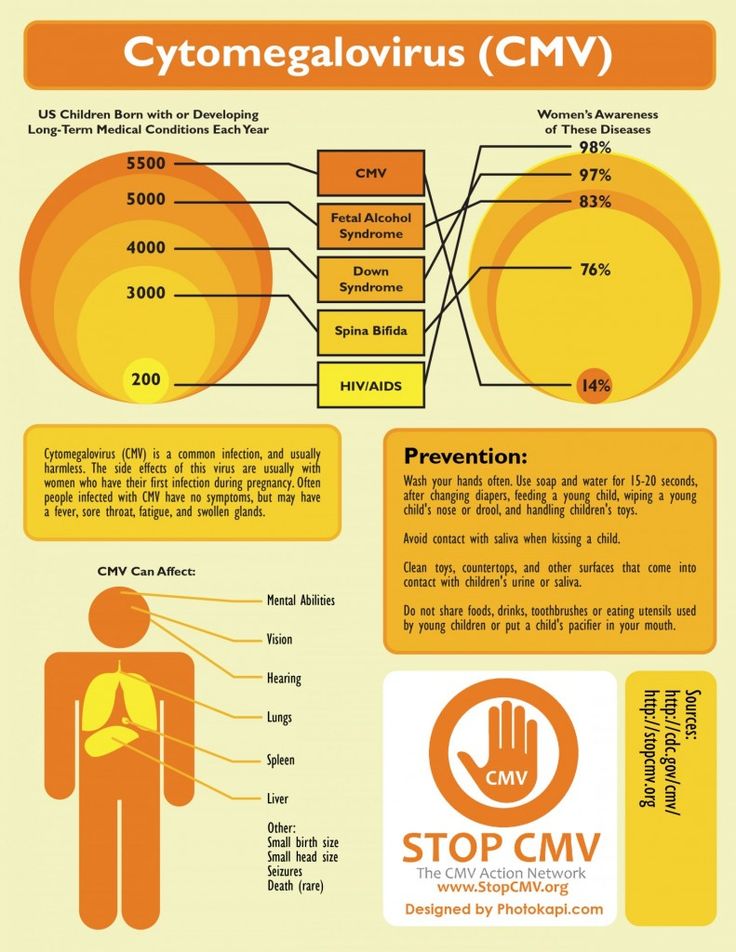 4% of pregnant women after a cold. The body of the unborn child can be affected by both viruses and bacteria that came after them.
4% of pregnant women after a cold. The body of the unborn child can be affected by both viruses and bacteria that came after them.
For women, a seemingly mild infection in 87.3% of cases turns into preeclampsia (fortunately, usually in a mild degree) and 10.4% - pyelonephritis (inflammation of the renal pelvis). In 75% of cases, the level of platelets in women decreases and almost always (with a probability of 90%) anemia develops: there are fewer red blood cells. This reduces the ability to compensate for placental insufficiency and complicates the situation for the baby. nine0003
HOW TO KNOW YOU NEED HELP?
Most of the conditions caused by a cold go unnoticed by a pregnant woman. Only pyelonephritis has clear signs: it is impossible to miss its characteristic fever and severe pain. It is impossible not to notice the pronounced gestosis. Anemia imperceptibly harms the baby. Thrombocytopenia creates a risk of bleeding.
Pregnant women should be treated by an obstetrician-gynecologist or a qualified therapist who knows the specifics of managing patients who are expecting a baby.