Sunburn that turns into a rash
Poisoning, Allergy, Treatment, Causes, Pictures, and More
A sun rash can occur due to a genetic condition or the use of a certain medication. The rash may appear as small blisters and cause an itching or burning feeling, among other symptoms.
Sun rash is a type of photodermatosis, where exposure to sunlight causes a reaction on your skin. One common sun rash is called polymorphous light eruption (PMLE), sometimes also called a sun poisoning rash.
PMLE is a red, itchy rash that appears because of exposure to sunlight.
Many people incorrectly refer to PMLE as a sun allergy. In fact, as mentioned, PMLE is a type of photodermatosis. This refers to a sun-related skin disorder. It is one of the most common forms, occurring in around 10 to 20 percent of people.
Other kinds of sun rash can:
- have hereditary causes
- relate to the use of certain medications
- have links to exposure to compounds in certain plants
We explain how to spot sun rash, what causes it, and how to manage symptoms once they develop.
Sun rash typically appears several hours or days after sun exposure. It can develop anywhere on the body that’s exposed to sunlight. Some kinds of sun rash occur on skin that’s usually covered in the fall and winter, such as your chest or arms.
Characteristics of the rash can vary between people depending on skin type, but they can include:
- groups of small bumps or blisters
- itchy red patches
- areas of the skin that feel like they’re burning
- raised or rough patches of skin
If a person also has a severe sunburn, they might also feel a fever or headache.
Some people who get sun rash live with a rare photodermatosis called solar urticaria (sun allergy hives). Folks with solar urticaria may feel the following symptoms alongside sun rash:
- faintness
- breathlessness
- headache
- other allergy symptoms
These symptoms will usually happen within a few minutes of sun exposure for people with solar urticaria.
Doctors have yet to work out exactly what causes sun rash.
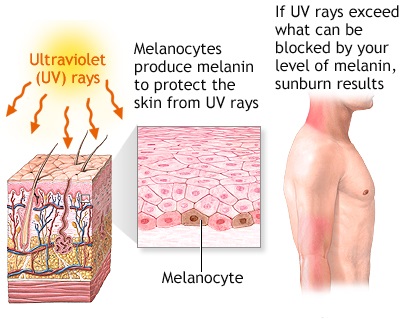
UV radiation from the sun or artificial sources like sunlamps might cause reactions in some people with a sensitivity to this type of light. The resulting immune reaction triggers the rash.
Some risk factors for certain kinds of sun rash can include:
- being assigned female at birth
- having light skin
- living in Northern regions, such as Scandinavia, Central Europe, and the United States
- having a family history of sun rash
- living in high altitude areas
If you experience a rash after being out in the sun, it’s important to speak with a doctor, such as a dermatologist (if you have access to one). They can rule out other conditions like contact dermatitis or lupus.
Your doctor can also examine the area to see what kind of sun-induced rash it might be. If you’ve never had a sun rash before and suddenly get one, call your doctor.
You should get immediate medical attention if your rash becomes widespread and painful or if you also have a fever. Sometimes, sun rashes can mimic other, more serious ailments, so it’s best to have a medical professional examine you.
Sometimes, sun rashes can mimic other, more serious ailments, so it’s best to have a medical professional examine you.
Healthcare professionals do not always recommend treatment for sun rash. Most of the time, it can resolve without treatment in a few days. However, this depends on the specific rash and if there’s severe sun poisoning.
The following remedies can help you manage your comfort while the rash is visible:
- Apply anti-itching creams. If your rash itches, an over-the-counter (OTC) anti-itch corticosteroid cream like hydrocortisone can be helpful. OTC oral antihistamines can also help.
- Try cold compresses or a cool bath. These can also provide itch relief.
- Avoid scratching at any blisters. If you have any blisters or if the rash is painful, don’t scratch or pop the blisters. This can lead to infection. You can cover the blisters with gauze to help protect them and take an OTC pain-relieving medication like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol)
- Use gentle moisturizers.
 As your skin starts to heal, you can use gentle moisturizers to relieve itching from dry or irritated skin.
As your skin starts to heal, you can use gentle moisturizers to relieve itching from dry or irritated skin.
These remedies aren’t effective for everyone. If the treatments don’t have the desired effect, you might need to reach out to a doctor. They can prescribe you a stronger anti-itch cream or oral medication to relieve symptoms.
For people who regularly take medication for another condition, a doctor can let you know if your sun rash is a side effect of the medication.
If your sun rash is due to an allergy, your doctor might prescribe allergy medication or corticosteroids to help address any symptoms you might be having. Sometimes, a physician will prescribe the antimalarial medication hydroxychloroquine, since it’s been shown to address symptoms of certain types of photodermatoses.
There are precautions you can take to minimize your risk of sun rash happening again:
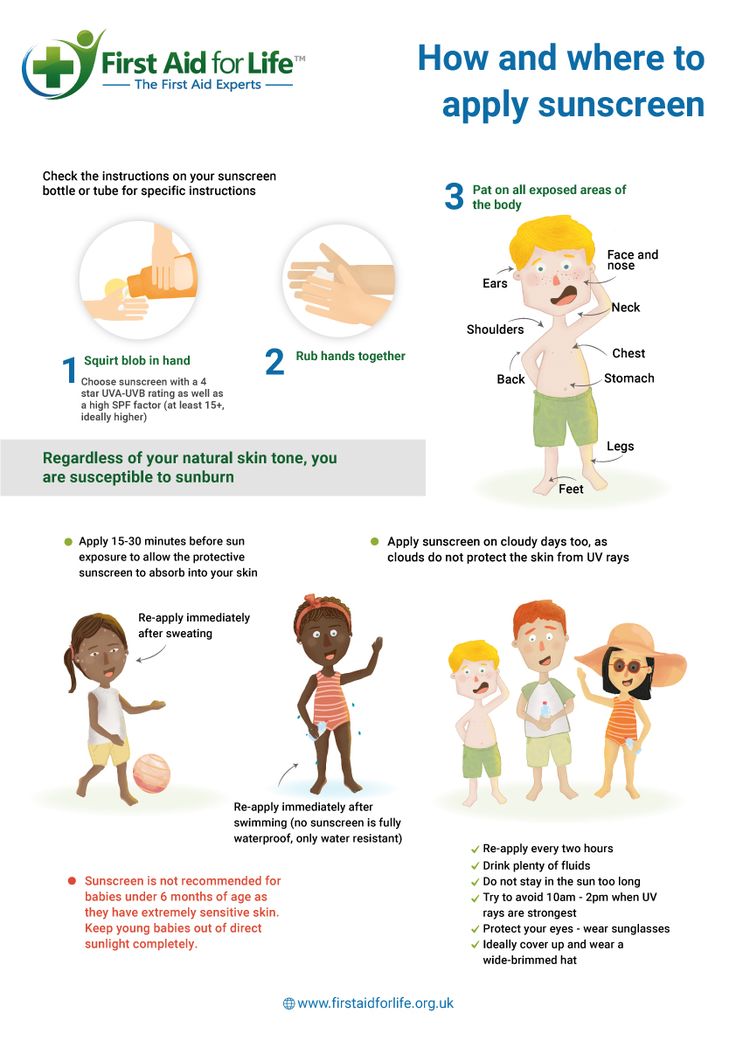
- Wear sunscreen. Apply sunscreen with an SPF of at least 30 about a half hour before going out into the sun, and reapply every 2 hours (sooner if you go swimming or are sweating a lot).
- Protect your skin with long-sleeve shirts and a wide-brim hat. You might also want to think about wearing specially made clothes that contain sun protective factors.
- Avoid the sun between 10 a.m. and 2 p.m., when the sun’s rays are most intense. For extra protection, stay out of the sun until after 4 p.m.
- Depending on the type of sun rash, it may be beneficial to gradually expose yourself to more light in the spring. This might help reduce the likelihood of developing a rash. Work with your doctor to be on the safe side.
Sun rash often goes away on its own, but it can recur with exposure to sunlight.
Sun rash typically goes away within a few days, depending on the underlying cause. If your rash recurs despite taking precautions or doesn’t seem to be improving with treatment, call your doctor.
Poisoning, Allergy, Treatment, Causes, Pictures, and More
A sun rash can occur due to a genetic condition or the use of a certain medication. The rash may appear as small blisters and cause an itching or burning feeling, among other symptoms.
The rash may appear as small blisters and cause an itching or burning feeling, among other symptoms.
Sun rash is a type of photodermatosis, where exposure to sunlight causes a reaction on your skin. One common sun rash is called polymorphous light eruption (PMLE), sometimes also called a sun poisoning rash.
PMLE is a red, itchy rash that appears because of exposure to sunlight.
Many people incorrectly refer to PMLE as a sun allergy. In fact, as mentioned, PMLE is a type of photodermatosis. This refers to a sun-related skin disorder. It is one of the most common forms, occurring in around 10 to 20 percent of people.
Other kinds of sun rash can:
- have hereditary causes
- relate to the use of certain medications
- have links to exposure to compounds in certain plants
We explain how to spot sun rash, what causes it, and how to manage symptoms once they develop.
Sun rash typically appears several hours or days after sun exposure. It can develop anywhere on the body that’s exposed to sunlight. Some kinds of sun rash occur on skin that’s usually covered in the fall and winter, such as your chest or arms.
It can develop anywhere on the body that’s exposed to sunlight. Some kinds of sun rash occur on skin that’s usually covered in the fall and winter, such as your chest or arms.
Characteristics of the rash can vary between people depending on skin type, but they can include:
- groups of small bumps or blisters
- itchy red patches
- areas of the skin that feel like they’re burning
- raised or rough patches of skin
If a person also has a severe sunburn, they might also feel a fever or headache.
Some people who get sun rash live with a rare photodermatosis called solar urticaria (sun allergy hives). Folks with solar urticaria may feel the following symptoms alongside sun rash:
- faintness
- breathlessness
- headache
- other allergy symptoms
These symptoms will usually happen within a few minutes of sun exposure for people with solar urticaria.
Doctors have yet to work out exactly what causes sun rash.
UV radiation from the sun or artificial sources like sunlamps might cause reactions in some people with a sensitivity to this type of light. The resulting immune reaction triggers the rash.
Some risk factors for certain kinds of sun rash can include:
- being assigned female at birth
- having light skin
- living in Northern regions, such as Scandinavia, Central Europe, and the United States
- having a family history of sun rash
- living in high altitude areas
If you experience a rash after being out in the sun, it’s important to speak with a doctor, such as a dermatologist (if you have access to one). They can rule out other conditions like contact dermatitis or lupus.
Your doctor can also examine the area to see what kind of sun-induced rash it might be. If you’ve never had a sun rash before and suddenly get one, call your doctor.
You should get immediate medical attention if your rash becomes widespread and painful or if you also have a fever. Sometimes, sun rashes can mimic other, more serious ailments, so it’s best to have a medical professional examine you.
Sometimes, sun rashes can mimic other, more serious ailments, so it’s best to have a medical professional examine you.
Healthcare professionals do not always recommend treatment for sun rash. Most of the time, it can resolve without treatment in a few days. However, this depends on the specific rash and if there’s severe sun poisoning.
The following remedies can help you manage your comfort while the rash is visible:
- Apply anti-itching creams. If your rash itches, an over-the-counter (OTC) anti-itch corticosteroid cream like hydrocortisone can be helpful. OTC oral antihistamines can also help.
- Try cold compresses or a cool bath. These can also provide itch relief.
- Avoid scratching at any blisters. If you have any blisters or if the rash is painful, don’t scratch or pop the blisters. This can lead to infection. You can cover the blisters with gauze to help protect them and take an OTC pain-relieving medication like ibuprofen (Advil, Motrin) or acetaminophen (Tylenol)
- Use gentle moisturizers.
 As your skin starts to heal, you can use gentle moisturizers to relieve itching from dry or irritated skin.
As your skin starts to heal, you can use gentle moisturizers to relieve itching from dry or irritated skin.
These remedies aren’t effective for everyone. If the treatments don’t have the desired effect, you might need to reach out to a doctor. They can prescribe you a stronger anti-itch cream or oral medication to relieve symptoms.
For people who regularly take medication for another condition, a doctor can let you know if your sun rash is a side effect of the medication.
If your sun rash is due to an allergy, your doctor might prescribe allergy medication or corticosteroids to help address any symptoms you might be having. Sometimes, a physician will prescribe the antimalarial medication hydroxychloroquine, since it’s been shown to address symptoms of certain types of photodermatoses.
There are precautions you can take to minimize your risk of sun rash happening again:
- Wear sunscreen. Apply sunscreen with an SPF of at least 30 about a half hour before going out into the sun, and reapply every 2 hours (sooner if you go swimming or are sweating a lot).

- Protect your skin with long-sleeve shirts and a wide-brim hat. You might also want to think about wearing specially made clothes that contain sun protective factors.
- Avoid the sun between 10 a.m. and 2 p.m., when the sun’s rays are most intense. For extra protection, stay out of the sun until after 4 p.m.
- Depending on the type of sun rash, it may be beneficial to gradually expose yourself to more light in the spring. This might help reduce the likelihood of developing a rash. Work with your doctor to be on the safe side.
Sun rash often goes away on its own, but it can recur with exposure to sunlight.
Sun rash typically goes away within a few days, depending on the underlying cause. If your rash recurs despite taking precautions or doesn’t seem to be improving with treatment, call your doctor.
Photodermatosis: a common sun allergy
Summer sun dermatitis, often referred to as sun allergy, is the most common form of photodermatosis. This disease is caused by increased sensitivity of the skin to ultraviolet radiation and is caused by exposure to sunlight. This phenomenon is not rare today - about 20% of the population worldwide faces photodermatosis. Allergies show up as small red itchy dots. This usually happens after 12 hours. Relapses are often inevitable. Sun allergies can be more severe: more dots, more itching, and more affected areas. nine0003
This disease is caused by increased sensitivity of the skin to ultraviolet radiation and is caused by exposure to sunlight. This phenomenon is not rare today - about 20% of the population worldwide faces photodermatosis. Allergies show up as small red itchy dots. This usually happens after 12 hours. Relapses are often inevitable. Sun allergies can be more severe: more dots, more itching, and more affected areas. nine0003
Sun allergies are very common in women between the ages of 15 and 35. It causes discomfort and negatively affects the appearance, is expressed in the appearance of small red spots that cause intense itching and burning. On the face, these spots usually do not appear, but they are on the neck, shoulders, arms and legs. Other symptoms of photodermatosis: peeling of the skin, rashes in the form of papules or folliculitis (pustules), prolonged pigmentation in the affected areas.
Often the symptoms do not appear immediately. Unlike sunburn, photodermatosis can develop only a few hours after returning home (phototoxic reaction), and sometimes even after a few days (photoallergic reaction). nine0003
nine0003
Photodermatosis is caused by ultraviolet rays, especially UVA rays. Their negative impact is increased by deodorants, perfumes, ointments and creams that were applied to sensitive skin before sun exposure. Some substances in perfumes and cosmetics can react with ultraviolet light and cause allergies. This property has, for example, eosin contained in lipstick, and para-aminobenzoic acid, which is part of some sunscreens. Other substances have a similar effect: phenol, retinoids, salicylic, boric and polyunsaturated fatty acids, parsley juice, rose oil, bergamot, musk, St. John's wort and sandalwood. nine0003
It is not uncommon for medications to cause symptoms of sun allergy. In particular: barbiturates, antihistamines, cytostatics, oral contraceptives, hormone replacement therapy drugs, sulfonamides, chlorpromazine, certain cardiovascular drugs, certain antibiotics and certain anti-inflammatory drugs. An increased reaction to ultraviolet light is also manifested in the case of a decrease in the protective function of the skin due to additional exposure to it (for example, peeling, cosmetic manipulations). Often the cause of photodermatosis is a violation of the hepatobiliary and gastrointestinal tract. nine0003
Often the cause of photodermatosis is a violation of the hepatobiliary and gastrointestinal tract. nine0003
And there is only one way to solve this problem - to prevent its occurrence. The ideal solution is to avoid the sun or wear protective clothing. If the sun cannot be avoided:
- do not sunbathe between 11.00 – 16.00
- before going to the beach, do not use perfumes and creams containing alcohol
- sunbathe gradually (20-30 minutes a day)
- Use a broad spectrum sunscreen with a strong protection factor (against UVA and UVB rays). The first days only on limited areas of the skin. And only after making sure that there is no photodermatosis, when applying these products to certain areas of the skin, use them on all surfaces of the skin. nine0016
- reapply the cream every two hours
- if it was still not possible to avoid negative effects on the skin, and there is no way to consult a doctor, you can remove the acute manifestations of photodermatosis using cold lotions and special after-sun products containing panthenol.