Stress incontinence in pregnancy
Incontinence During Pregnancy and After Childbirth
Written by WebMD Editorial Contributors
In this Article
- What Types of Incontinence Are Experienced During and After Pregnancy?
- How Is Urinary Incontinence During Pregnancy Treated?
- What Are Kegel Exercises?
- When Should You See a Health Care Professional About Incontinence?
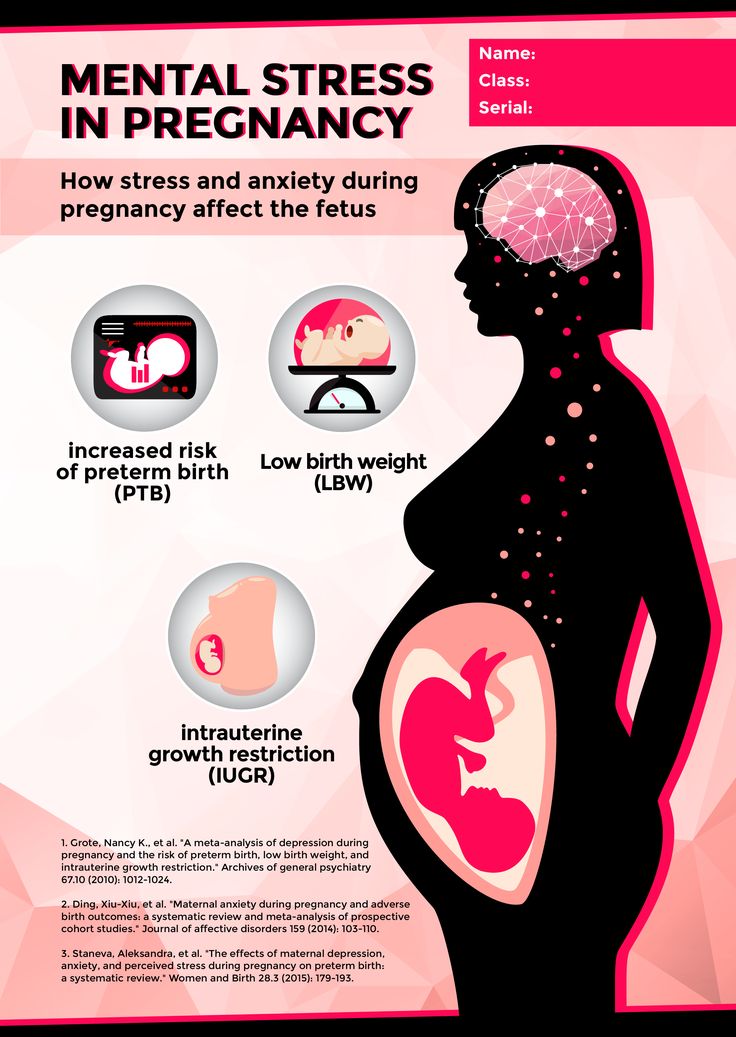
During pregnancy, many women experience at least some degree of urinary incontinence, which is the involuntary loss of urine. The incontinence may be mild and infrequent for some pregnant women. But it can be more severe for others. Age and body mass index are risk factors for pregnancy incontinence, according to one study.
Incontinence can continue after pregnancy and may not be present right after childbirth. Some women do not have bladder problems until they reach their 40s.
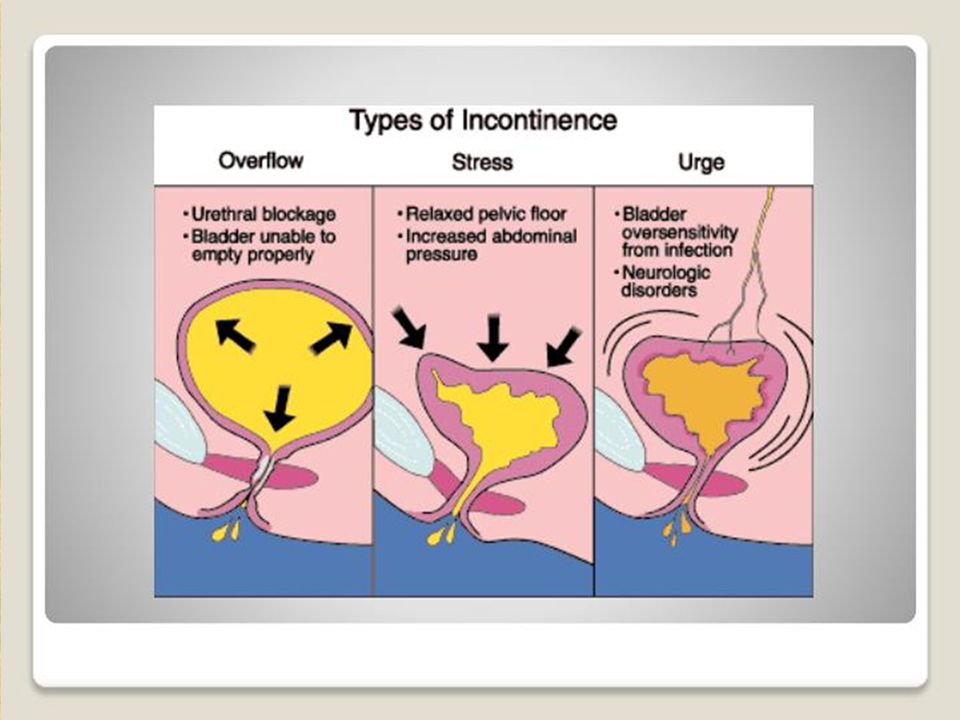
What Types of Incontinence Are Experienced During and After Pregnancy?
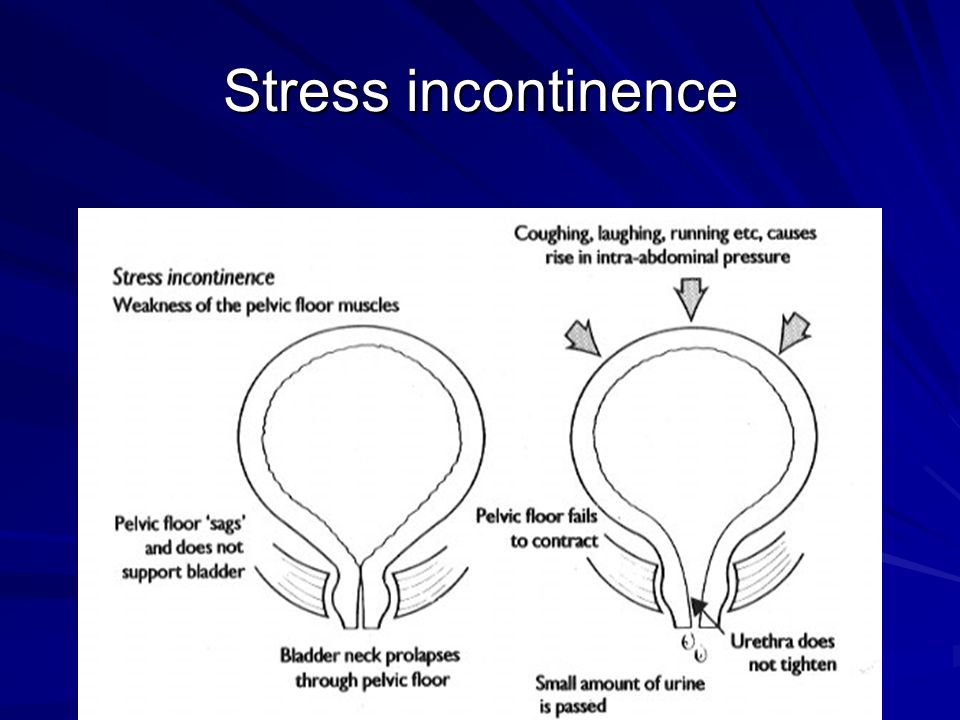
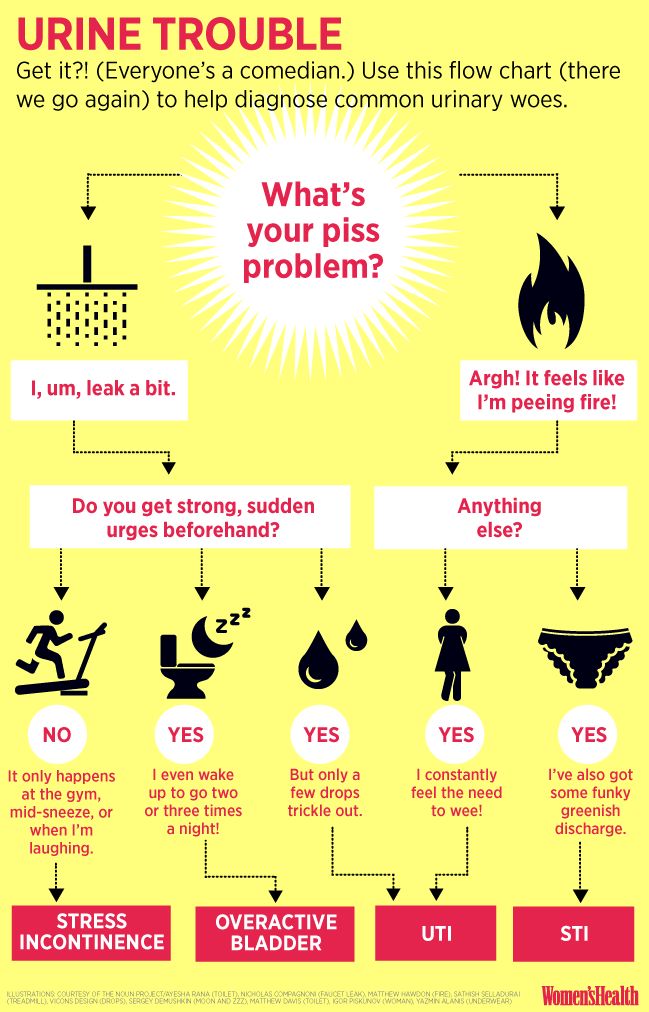
The kind of incontinence experienced during pregnancy is usually stress incontinence (SI). Stress incontinence is the loss of urine caused by increased pressure on the bladder. In stress incontinence, the bladder sphincter does not function well enough to hold in urine.
Urinary incontinence during pregnancy can also be the result of an overactive bladder. Women who have an overactive bladder (OAB) need to urinate more than usual because their bladders have uncontrollable spasms. In addition, the muscles surrounding the urethra -- the tube through which urine passes from the bladder -- can be affected. These muscles are meant to prevent urine from leaving the body, but they may be "overridden" if the bladder has a strong contraction.
The bladder sphincter is a muscular valve that lies at the bottom of the bladder. It works to control the flow of urine. In pregnancy, the expanding uterus puts pressure on the bladder. The muscles in the bladder sphincter and in the pelvic floor can be overwhelmed by the extra stress or pressure on the bladder. Urine may leak out of the bladder when there is additional pressure exerted -- for example, when a pregnant woman coughs or sneezes.
After pregnancy, incontinence problems may continue, because childbirth weakens the pelvic floor muscles, which can cause an overactive bladder. Pregnancy and childbirth also may contribute to bladder control problems because of the following conditions:
- Damage to the nerves that control the bladder
- The fact that the urethra and bladder have moved during pregnancy
- An episiotomy, a cut made in the pelvic floor muscle during delivery of a baby to allow the fetus to come out more easily
How Is Urinary Incontinence During Pregnancy Treated?
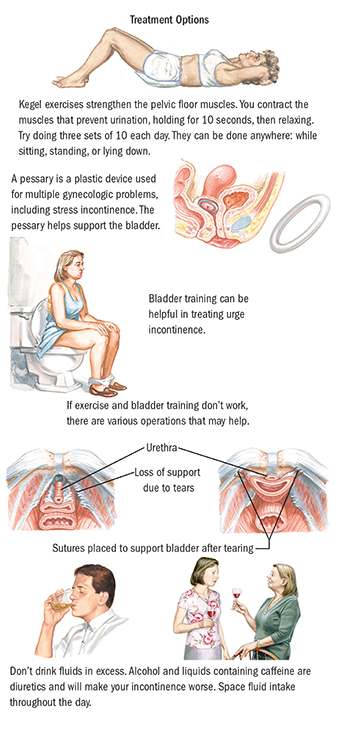
Behavioral methods such as timed voiding and bladder training can be helpful in treating urinary incontinence during and after pregnancy. These techniques are often used first and can be done at home. The changes in habits that behavioral methods involve do not have serious side effects.
To practice timed voiding, you use a chart or diary to record the times that you urinate and when you leak urine.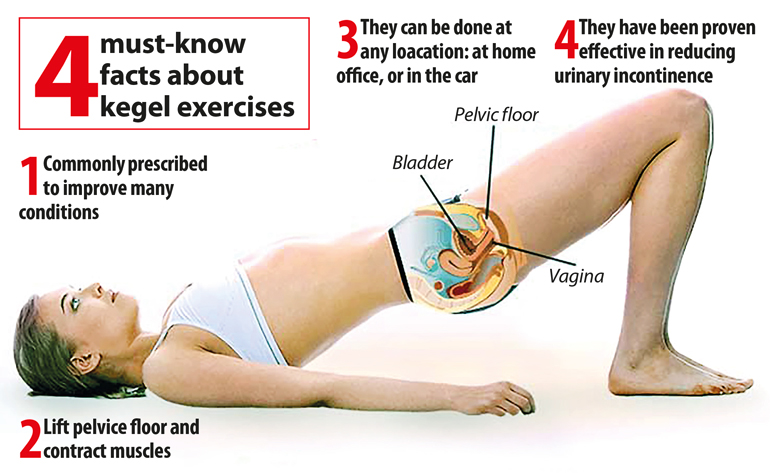 This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
In bladder training, you "stretch out" the intervals at which you go to the bathroom by waiting a little longer before you go. For instance, to start, you can plan to go to the bathroom once an hour. You follow this pattern for a period of time. Then you change the schedule to going to the bathroom every 90 minutes. Eventually you change it to every two hours and continue to lengthen the time until you are up to three or four hours between bathroom visits.
Another method is to try to postpone a visit to the bathroom for 15 minutes with the first urge. Do this for two weeks and then increase the amount of time to 30 minutes and so on.
In certain cases, a woman may use a pessary, a device to block the urethra or to strengthen the pelvic muscles. In addition, medications also can be helpful in controlling muscle spasms in the bladder or strengthening the muscles in the urethra.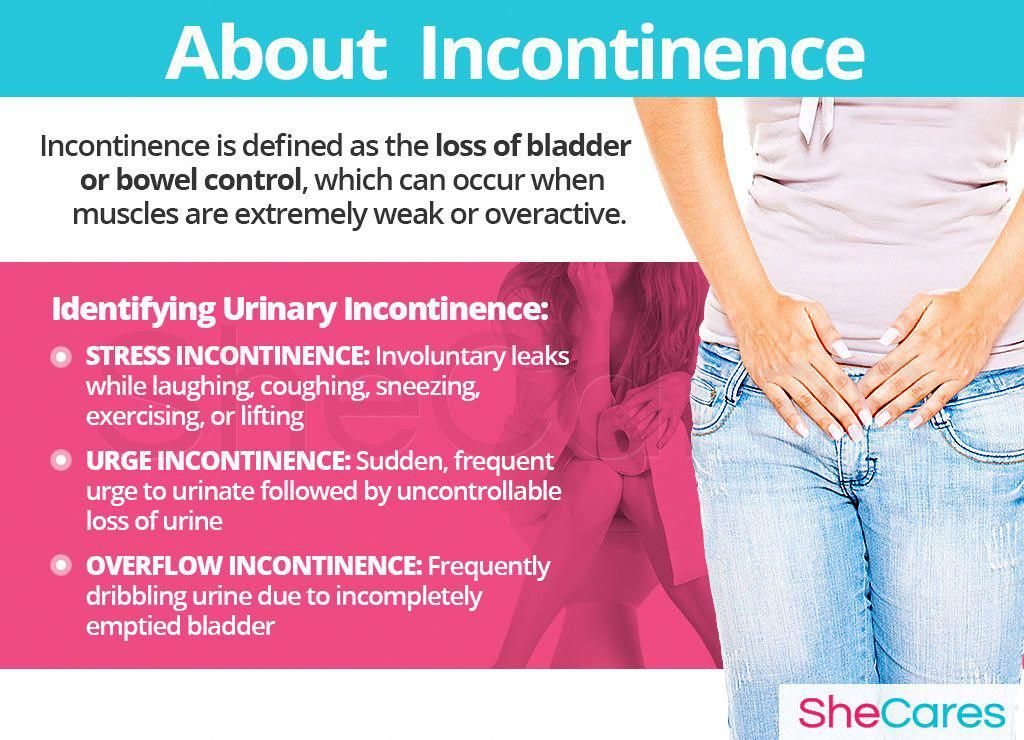 Some drugs can help to relax an overactive bladder.
Some drugs can help to relax an overactive bladder.
What Are Kegel Exercises?
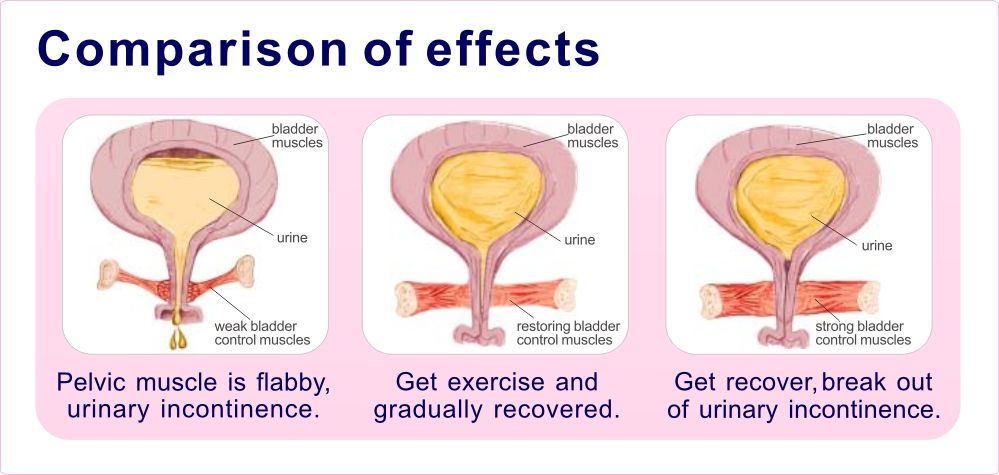
Kegel exercises are another method that can be used to help control urinary incontinence. These exercises help tighten and strengthen the muscles in the pelvic floor. Strengthening the pelvic floor muscles can improve the function of the urethra and rectal sphincter.
One way to find the Kegel muscles is to sit on the toilet and begin urinating. Then stop urinating mid-stream. The muscles that you use to stop the flow of urine are the Kegel muscles. Another way to help locate the Kegel muscles is to insert a finger into the vagina and try to make the muscles around your finger tighter.
To perform Kegel exercises, you should:
- Keep your abdominal, thigh, and buttocks muscles relaxed.
- Tighten the pelvic floor muscles.
- Hold the muscles until you count to 10.
- Relax the pelvic floor muscles until you count to 10.
Do 10 Kegel exercises in the morning, afternoon, and at night. They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
When Should You See a Health Care Professional About Incontinence?
Talk to your doctor if you still have bladder problems six weeks after delivery. Accidental leaking of urine may mean that you have another medical condition. The loss of bladder control should be treated or it can become a long-term problem.
Stress urinary incontinence in pregnant women: a review of prevalence, pathophysiology, and treatment
1. Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. [PubMed] [Google Scholar]
2. Dolan LM, Walsh D, Hamilton S, Marshall K, Thompson K, Ashe RG. A study of quality of life in primigravidae with urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:160–164. [PubMed] [Google Scholar]
2004;15:160–164. [PubMed] [Google Scholar]
3. Mascarenhas T, Coelho R, Oliveira M, Patricio B (2003) Impact of urinary incontinence on quality of life during pregnancy and after childbirth. Paper presented at the 33th annual meeting of the International Continence Society, Florence, Italy, October 9, 2003
4. van de Pol GG, Van Brummen HJ, Bruinse HW, Heintz AP, van der Vaart CH. Is there an association between depressive and urinary symptoms during and after pregnancy? Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1409–1415. [PMC free article] [PubMed] [Google Scholar]
5. van Brummen HJ, Bruinse HW, Van de Pol G, Heintz AP, Van der Vaart CH. What is the effect of overactive bladder symptoms on woman’s quality of life during and after first pregnancy? BJU Int. 2006;97(2):296–300. [PubMed] [Google Scholar]
6. van Brummen HJ, Bruinse HW, van de Pol G, Heintz AP, van der Vaart CH. Bothersome lower urinary tract symptoms 1 year after first delivery: prevalence and the effect of childbirth.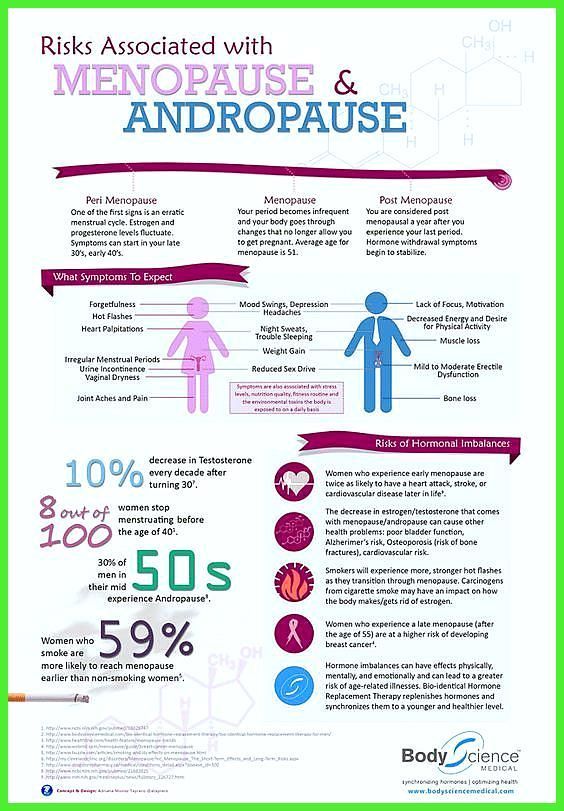 BJU Int. 2006;98(1):89–95. [PubMed] [Google Scholar]
BJU Int. 2006;98(1):89–95. [PubMed] [Google Scholar]
7. Milsom I, Altman D, Lapitan MC, Nelson R, Sillén U, Thom D. Epidemiology of urinary (UI) and faecal (FI) incontinence and pelvic organ prolapse (POP) In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence: 4th International Consultation on Incontinence. Paris: Health Publication Ltd; 2009. pp. 35–112. [Google Scholar]
8. Kocaöz S, Talas MS, Atabekoğlu CS. Urinary incontinence in pregnant women and their quality of life. J Clin Nurs. 2010;19(23–24):3314–3323. [PubMed] [Google Scholar]
9. Adaji SE, Shittu OS, Bature SB, Nasir S, Olatunji O. Suffering in silence: pregnant women’s experience of urinary incontinence in Zaria, Nigeria. Eur J Obstet Gynecol Reprod Biol. 2010;150(1):19–23. [PubMed] [Google Scholar]
10. Marecki M, Seo JY. Perinatal urinary and fecal incontinence: suffering in silence. J Perinat Neonatal Nurs. 2010;24(4):330–340. [PubMed] [Google Scholar]
11. King JK, Freeman RM. Is antenatal bladder neck mobility a risk factor for postpartum stress urinary incontinence? Br J Obstet Gynaecol.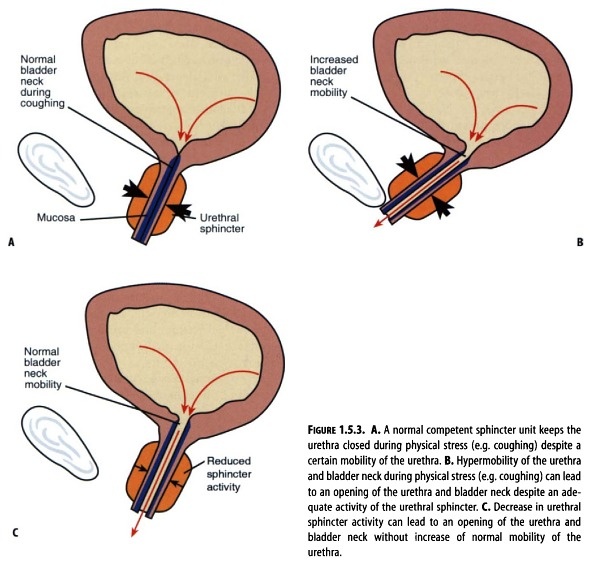 1998;105:1300–1307. [PubMed] [Google Scholar]
1998;105:1300–1307. [PubMed] [Google Scholar]
12. Schytt E, Lindmark G, Waldenstrom U. Symptoms of stress incontinence 1 year after childbirth: prevalence and predictors in a national Swedish sample. Acta Obstet Gynecol Scand. 2004;83:928–936. [PubMed] [Google Scholar]
13. Burgio KL, Zyczynski H, Locher JL, Richter HE, Redden DT, Wright KC. Urinary incontinence in the 12-month postpartum period. Obstet Gynecol. 2003;102:1291–1298. [PubMed] [Google Scholar]
14. Hvidman L, Foldspang A, Mommsen S, Nielsen JB. Postpartum urinary incontinence. Acta Obstet Gynecol Scand. 2003;82:556–563. [PubMed] [Google Scholar]
15. Liang CC, Wu MP, Lin SJ, Lin YJ, Chang SD, Wang HH. Clinical impact of and contributing factors to urinary incontinence in women 5 years after first delivery. Int Urogynecol J. 2013;24(1):99–104. [PubMed] [Google Scholar]
16. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement.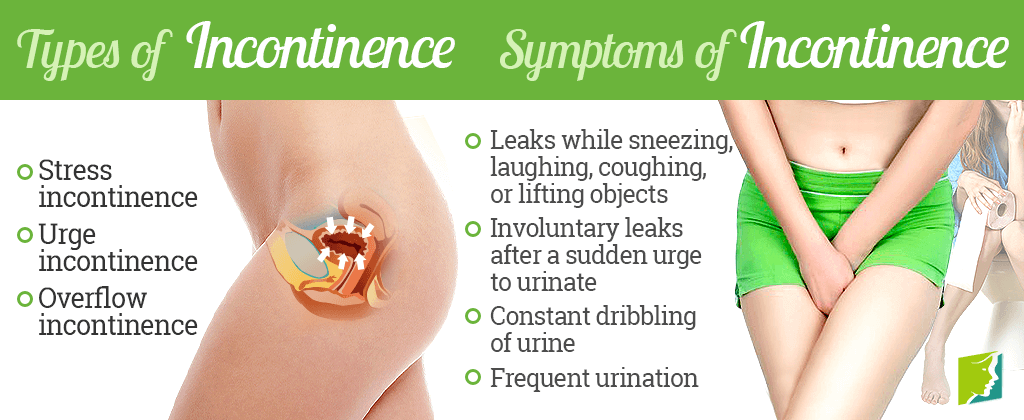 BMJ 21;339:b2535 [PMC free article] [PubMed]
BMJ 21;339:b2535 [PMC free article] [PubMed]
17. Wesnes SL, Rortveit G, Bø K, Hunskaar S. Urinary incontinence during pregnancy. Obstet Gynecol. 2007;109(4):922–928. [PubMed] [Google Scholar]
18. Mørkved S, Bø K. Prevalence of urinary incontinence during pregnancy and postpartum. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:394–398. [PubMed] [Google Scholar]
19. Mason L, Glenn S, Walton I, Appletion C. The prevalence of stress incontinence during pregnancy and following delivery. Midwifery. 1999;15(2):120–128. [PubMed] [Google Scholar]
20. Diez-Itza I, Ibañez L, Arrue M, Paredes J, Murgiondo A, Sarasqueta C. Influence of maternal weight on the new onset of stress urinary incontinence in pregnant women. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(10):1259–1263. [PubMed] [Google Scholar]
21. Whitford HM, Alder B, Jones M. A cross-sectional study of knowledge and practice of pelvic floor exercises during pregnancy and associated symptoms of stress urinary incontinence in North-East Scotland. Midwifery. 2007;23(2):204–217. [PubMed] [Google Scholar]
Midwifery. 2007;23(2):204–217. [PubMed] [Google Scholar]
22. Huebner M, Antolic A, Tunn R. The impact of pregnancy and vaginal delivery on urinary incontinence. Int J Gynecol Obstet. 2010;110(3):249–251. [PubMed] [Google Scholar]
23. Viktrup L, Lose G, Rolff M, Barford K. The symptom of stress incontinence caused by pregnancy or delivery in primiparas. Obstet Gynecol. 1992;79:945–949. [PubMed] [Google Scholar]
24. Zhu L, Li L, Lang JH, Xu T. Prevalence and risk factors for peri- and postpartum urinary incontinence in primiparous women in China: a prospective longitudinal study. Int Urogynecol J. 2012;23(5):563–572. [PubMed] [Google Scholar]
25. Liang CC, Chang SD, Lin SJ, Lin YJ. Lower urinary tract symptoms in primiparous women before and during pregnancy. Arch Gynecol Obstet. 2012;285(5):1205–1210. [PubMed] [Google Scholar]
26. Sun MJ, Chen GD, Chang SY, Lin KC, Chen SY. Prevalence of lower urinary tract symptoms during pregnancy in Taiwan. J Formos Med Assoc. 2005;104(3):185–189. [PubMed] [Google Scholar]
2005;104(3):185–189. [PubMed] [Google Scholar]
27. Al-Mehaisen LM, Al-Kuran O, Lataifeh IM, et al. Prevalence and frequency of severity of urinary incontinence symptoms in late pregnancy: a prospective study in the north of Jordan. Arch Gynecol Obstet. 2009;279(4):499–503. [PubMed] [Google Scholar]
28. Sharma JB, Aggarwal S, Singhal S, Kumar S, Roy KK. Prevalence of urinary incontinence and other urological problems during pregnancy: a questionnaire based study. Arch Gynecol Obstet. 2008;279(6):845–851. [PubMed] [Google Scholar]
29. Thomason AD, Miller JM, Delancey JO. Urinary incontinence symptoms during and after pregnancy in continent and incontinent primiparas. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(2):147–151. [PubMed] [Google Scholar]
30. Raza-Khan F, Graziano S, Kenton K, Shott S, Brubaker L. Peripartum urinary incontinence in a racially diverse obstetrical population. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(5):525–530. [PubMed] [Google Scholar]
31. Martins G, Soler ZA, Cordeiro JA, Amaro JL, Moore KN. Prevalence and risk factors for urinary incontinence in healthy pregnant Brazilian women. Int Urogynecol J. 2010;21(10):1271–1277. [PubMed] [Google Scholar]
Martins G, Soler ZA, Cordeiro JA, Amaro JL, Moore KN. Prevalence and risk factors for urinary incontinence in healthy pregnant Brazilian women. Int Urogynecol J. 2010;21(10):1271–1277. [PubMed] [Google Scholar]
32. Chiarelli P, Campbell E. Incontinence during pregnancy. Prevalence and opportunities for continence promotion. Aust N Z J Obstet Gynaecol. 1997;37(1):66–73. [PubMed] [Google Scholar]
33. Brown SJ, Donath S, MacArthur C, McDonald EA, Krastev AH. Urinary incontinence in nulliparous women before and during pregnancy: prevalence, incidence, and associated risk factors. Int Urogynecol J. 2010;21(2):193–202. [PubMed] [Google Scholar]
34. Bø K, Pauck Øglund G, Sletner L, Mørkrid K, Jenum A. The prevalence of urinary incontinence in pregnancy among a multi-ethnic population resident in Norway. Br J Obstet Gynaecol. 2012;119(11):1354–1360. [PubMed] [Google Scholar]
35. Fritel X, Fauconnier A, Bader G, et al. Diagnosis and management of adult female stress urinary incontinence: guidelines for clinical practice from the French College of Gynaecologists and Obstetricians. Eur J Obstet Gynecol Reprod Biol. 2010;151(1):14–19. [PubMed] [Google Scholar]
Eur J Obstet Gynecol Reprod Biol. 2010;151(1):14–19. [PubMed] [Google Scholar]
36. Wijma J, Weis Potters AE, Tinga DJ, Aarnoudse JG. The diagnostic strength of the 24-h pad test for self-reported symptoms of urinary incontinence in pregnancy and after childbirth. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):525–530. [PMC free article] [PubMed] [Google Scholar]
37. Thorp JM, Norton PA, Wall LL, Kuller JA, Eucker B, Wells E. Urinary incontinence in pregnancy and the puerperium: a prospective study. Am J Obstet Gynecol. 1999;181:266–273. [PubMed] [Google Scholar]
38. van Kerrebroeck P, Abrams P, Chaikin D, et al. The standardisation of terminology in nocturia: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21(2):179–183. [PubMed] [Google Scholar]
39. Francis WJ. Disturbances of bladder function in relation to pregnancy. J Obstet Gynaecol Br Emp. 1960;67:353–366. [PubMed] [Google Scholar]
40. Davis K, Kumar D. Pelvic floor dysfunction: a conceptual framework for collaborative patient-centred care. J Adv Nurs. 2003;43(6):555–568. [PubMed] [Google Scholar]
Davis K, Kumar D. Pelvic floor dysfunction: a conceptual framework for collaborative patient-centred care. J Adv Nurs. 2003;43(6):555–568. [PubMed] [Google Scholar]
41. Morkved S, Bo K, Schei B, Salvesen KA. Pelvic floor muscle training during pregnancy to prevent urinary incontinence: a single-blind randomized controlled trial. Obstet Gynecol. 2003;101(2):313–319. [PubMed] [Google Scholar]
42. FitzGerald MP, Graziano S. Anatomic and functional changes of the lower urinary tract during pregnancy. Urol Clin N Am. 2007;34(1):7–12. [PubMed] [Google Scholar]
43. McKinnie V, Swift SE, Wang W, et al. The effect of pregnancy and mode of delivery on the prevalence of urinary and fecal incontinence. Am J Obstet Gynecol. 2005;193(2):512–518. [PubMed] [Google Scholar]
44. Joanna Briggs Institute The Joanna Briggs Institute best practice information sheet: the effectiveness of pelvic floor muscle exercises on urinary incontinence in women following childbirth. Nurs Health Sci.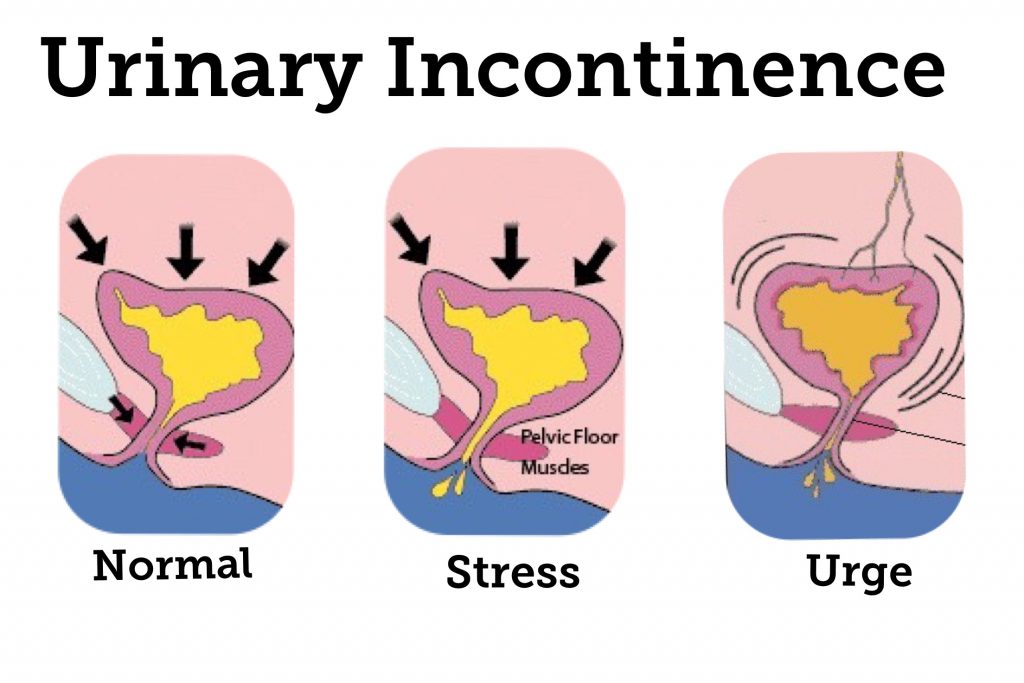 2011;13(3):378–381. [PubMed] [Google Scholar]
2011;13(3):378–381. [PubMed] [Google Scholar]
45. Morkved S, Salvesen KA, Bo K, Eik-Nes S. Pelvic floor muscle strength and thickness in continent and incontinent nulliparous pregnant women. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:384–390. [PubMed] [Google Scholar]
46. Hojberg KE, Salvig JD, Winslow NA, Lose G, Secher NJ. Urinary incontinence: prevalence and risk factors at 16 weeks of gestation. Br J Obstet Gynecol. 1999;106:842–850. [PubMed] [Google Scholar]
47. MacLennan AH, Taylor AW, Wilson DH, Wilson D. The prevalence of pelvic floor disorder and their relationship to gender, age, parity and mode of delivery. Br J Obstet Gynecol. 2000;107:1460–1470. [PubMed] [Google Scholar]
48. Peyrat L, Haillot O, Bruyere F, Boutin JM, Bertrand P, Lanson Y. Prevalence and risk factors of urinary incontinence in young and middle-aged women. Br J Urol. 2002;89:61–66. [PubMed] [Google Scholar]
49. Viktrup L. The risk of urinary tract symptom five years after the first delivery. Neurourol Urodyn. 2002;21(1):2–29. [PubMed] [Google Scholar]
Neurourol Urodyn. 2002;21(1):2–29. [PubMed] [Google Scholar]
50. Pregazzi R, Sartore A, Troiano L, et al. Postpartum Urinary symptoms: prevalence and risk factors. Obstet Gynecol. 2002;103(2):179–182. [PubMed] [Google Scholar]
51. Greer WJ, Richter HE, Bartolucci AA, Burgio KL. Obesity and pelvic floor disorders: a systematic review. Obstet Gynecol. 2008;112(2 Pt 1):341–349. [PMC free article] [PubMed] [Google Scholar]
52. Bump RC, Sugerman H, Fantl JA, McClish DM. Obesity and lower urinary tract function in women: effect of surgically induced weight loss. Am J Obstet Gynecol. 1992;166:392–399. [PubMed] [Google Scholar]
53. Glazener CM, Herbison GP, MacArthur C, et al. New postnatal urinary incontinence: obstetric and other risk factors in primiparae. Br J Obstet Gynaecol. 2006;113(2):208–217. [PubMed] [Google Scholar]
54. Van Kessel K, Reed S, Newton K, Meier A, Lentz G. The second stage of labor and stress urinary incontinence. Am J Obstet Gynecol. 2011;184(7):1571–1575.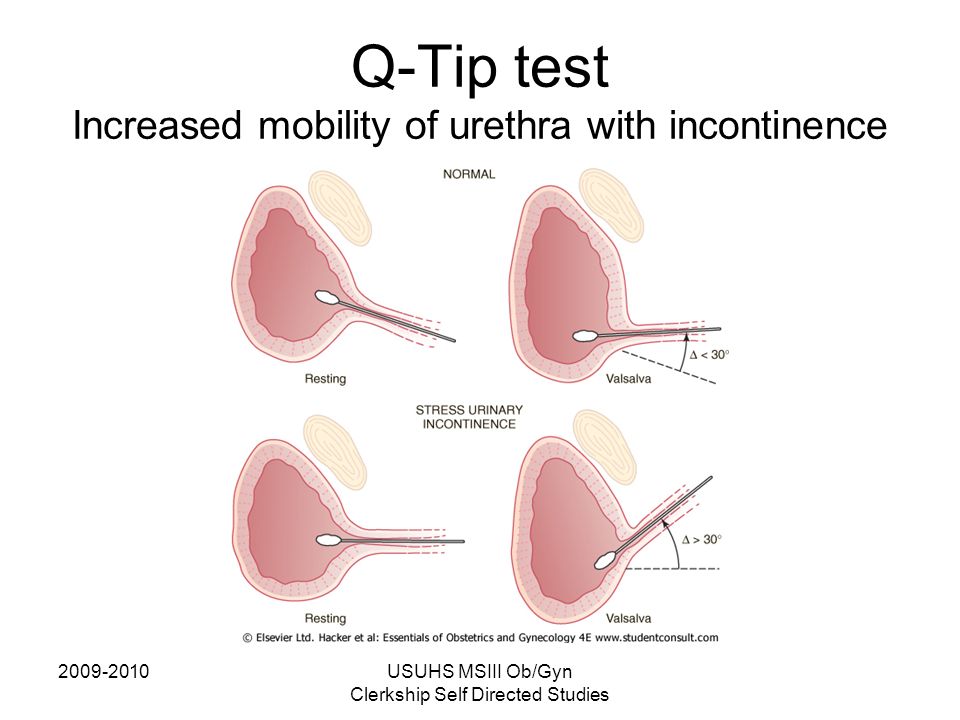 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
55. Wesnes SL, Hunskaar S, Bo K, Rortveit G. The effect of urinary incontinence status during pregnancy and delivery mode on incontinence postpartum. A cohort study. Br J Obstet Gynaecol. 2009;116(5):700–707. [PMC free article] [PubMed] [Google Scholar]
56. Gyhagen M, Bullarbo M, Nielsen T, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. Br J Obstet Gynaecol. 2013;120(2):152–160. [PubMed] [Google Scholar]
57. Singh K, Jakab M, Reid WM, Berger LA, Hoyte L. Three-dimensional magnetic resonance imaging assessment of levator ani morphologic features in different grades of prolapse. Am J Obstet Gynecol. 2003;188:910–915. [PubMed] [Google Scholar]
58. Stothers L, Friedman B. Risk factors for the development of stress urinary incontinence in women. Curr Urol Rep. 2011;12(5):363–369. [PubMed] [Google Scholar]
59. Wijma J, Weis Potters AE, van der Mark TW, Tinga DJ, Aarnoudse JG. Displacement and recovery of the vesical neck position during pregnancy and after childbirth. Neurourol Urodyn. 2007;26(3):372–376. [PubMed] [Google Scholar]
Wijma J, Weis Potters AE, van der Mark TW, Tinga DJ, Aarnoudse JG. Displacement and recovery of the vesical neck position during pregnancy and after childbirth. Neurourol Urodyn. 2007;26(3):372–376. [PubMed] [Google Scholar]
60. Hilde G, Stær-Jensen J, Ellström Engh M, Brækken IH, Bø K. Continence and pelvic floor status in nulliparous women at midterm pregnancy. Int Urogynecol J. 2012;23(9):1257–1263. [PubMed] [Google Scholar]
61. Dietz HP, Wilson PD. Childbirth and pelvic floor trauma. Best Pract Res Clin Obstet Gynaecol. 2005;19(6):913–924. [PubMed] [Google Scholar]
62. Dietz HP, Schierlitz L. Pelvic floor trauma in childbirth—myth or reality? Aust N Z J Obstet Gynaecol. 2005;45(1):3–11. [PubMed] [Google Scholar]
63. Keane DP, Sims TJ, Abrams P, Bailey AJ. Analysis of collagen status in premenopausal nulliparous women with genuine stress incontinence. Br J Obstet Gynaecol. 1997;104(9):994–998. [PubMed] [Google Scholar]
64. Dietz HP, Eldridge A, Grace M, Clarke B. Does pregnancy affect pelvic organ mobility? Aust N Z J Obstet Gynaecol. 2004;44:517–520. [PubMed] [Google Scholar]
Does pregnancy affect pelvic organ mobility? Aust N Z J Obstet Gynaecol. 2004;44:517–520. [PubMed] [Google Scholar]
65. Wijma J, Weis Potters AE, de Wolf BTHM, Tinga DJ, Aarnoudse JG. Anatomical and functional changes in the lower urinary tract during pregnancy. Br J Obstet Gynaecol. 2001;108:726–732. [PubMed] [Google Scholar]
66. Jundt K, Scheer I, Schiessl B, Karl K, Friese K, Peschers UM. Incontinence, bladder neck mobility, and sphincter ruptures in primiparous women. Eur J Med Res. 2010;15(6):246–252. [PMC free article] [PubMed] [Google Scholar]
67. Chaliha C, Kalia V, Stanton SL, Monga A, Sultan AH. Antenatal prediction of postpartum urinary and fecal incontinence. Obstet Gynecol. 1999;94:689–694. [PubMed] [Google Scholar]
68. Falconer C, Ekman G, Malmstrom A, Ulmsten U. Decreased collagen synthesis in stress-incontinence women. Obstet Gynecol. 1994;84:583–586. [PubMed] [Google Scholar]
69. Chen B, Wen Y, Yu X, Polan ML. The role of neutrophil elastase in elastin metabolism of pelvic tissues from women with stress urinary incontinence.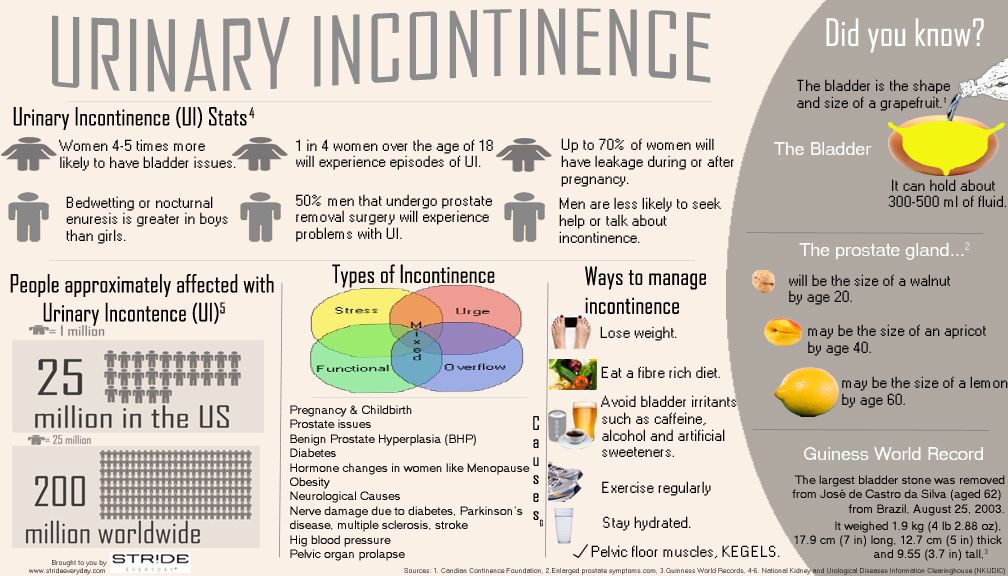 Neurourol Urodyn. 2007;26(2):274–279. [PubMed] [Google Scholar]
Neurourol Urodyn. 2007;26(2):274–279. [PubMed] [Google Scholar]
70. Lin G, Shindel AW, Banie L, et al. Molecular mechanisms related to parturition-induced stress urinary incontinence. Eur Urol. 2009;55(5):1213–1222. [PMC free article] [PubMed] [Google Scholar]
71. Skorupski P, Jankiewicz K, Miotła P et al (2012) The polymorphisms of the MMP-1 and the MMP-3 genes and the risk of pelvic organ prolapse. Int Urogynecol J. doi:10.1007/s00192-012-1970-1 [PMC free article] [PubMed]
72. Altman D, Forsman M, Falconer C, Lichtenstein P. Genetic influence on stress urinary incontinence and pelvic organ prolapse. Eur Urol. 2008;54(4):918–922. [PubMed] [Google Scholar]
73. Dietz HP, Hansell NK, Grace ME, Eldridge AM, Clarke B, Martin NG. Bladder neck mobility is a heritable trait. Br J Obstet Gynaecol. 2005;112(3):334–339. [PubMed] [Google Scholar]
74. Lince SL, van Kempen LC, Vierhout ME, Kluivers KB. A systematic review of clinical studies on hereditary factors in pelvic organ prolapse. Int Urogynecol J. 2012;23(10):1327–1336. [PMC free article] [PubMed] [Google Scholar]
Int Urogynecol J. 2012;23(10):1327–1336. [PMC free article] [PubMed] [Google Scholar]
75. Hilton P, Dolan LM. Pathophysiology of urinary incontinence and pelvic organ prolapse. Br J Obstet Gynaecol. 2004;111(sup.1):5–9. [PubMed] [Google Scholar]
76. Kristiansson P, Samuelsson E, Schoultz B, Svardsudd K. Reproductive hormones and stress urinary incontinence in pregnancy. Acta Obstet Gynecol Scand. 2001;80:1125–1130. [PubMed] [Google Scholar]
77. Kristiansson P, Svardsudd K, Schoultz B. Serum relaxin, symphyseal pain, and back pain during pregnancy. Am J Obstet Gynecol. 1996;175:1342–1347. [PubMed] [Google Scholar]
78. Harvey MA, Johnston SL, Davies GA. Mid-trimester serum relaxin concentrations and post-partum pelvic floor dysfunction. Acta Obstet Gynecol Scand. 2008;87(12):1315–1321. [PubMed] [Google Scholar]
79. Chaliha C, Stanton SL. Urological problems in pregnancy. Br J Urol. 2002;89:469–476. [PubMed] [Google Scholar]
80. van Geelen JM, Lemmens WA, Eskes TK, Martin CB. , Jr The urethral pressure profile in pregnancy and after delivery in healthy nulliparous women. Am J Obstet Gynecol. 1982;144(6):636–649. [PubMed] [Google Scholar]
, Jr The urethral pressure profile in pregnancy and after delivery in healthy nulliparous women. Am J Obstet Gynecol. 1982;144(6):636–649. [PubMed] [Google Scholar]
81. Swift SE, Ostergard DR. Effects of progesterone on the urinary tract. Int Urogynecol J. 1993;4(4):232–236. [Google Scholar]
82. Tincello DG, Teare J, Fraser WD. Second trimester concentration of relaxin and pregnancy related incontinence. Eur J Obstet Gynecol Reprod Biol. 2003;106:237–238. [PubMed] [Google Scholar]
83. Chaliha C, Bland JM, Monga A, Stanton SL, Sultan AH. Pregnancy and derivery: a urodynamic viewpoint. Br J Obstet Gynaecol. 2000;107:1354–1359. [PubMed] [Google Scholar]
84. Viktrup L, Rortveit G, Lose G. Risk of stress urinary incontinence twelve years after the first pregnancy and delivery. Obstet Gynecol. 2006;108(2):248–254. [PubMed] [Google Scholar]
85. Thom DH, Rortveit G. Prevalence of postpartum urinary incontinence: a systematic review. Acta Obstet Gynecol Scand. 2010;89(12):1511–1522.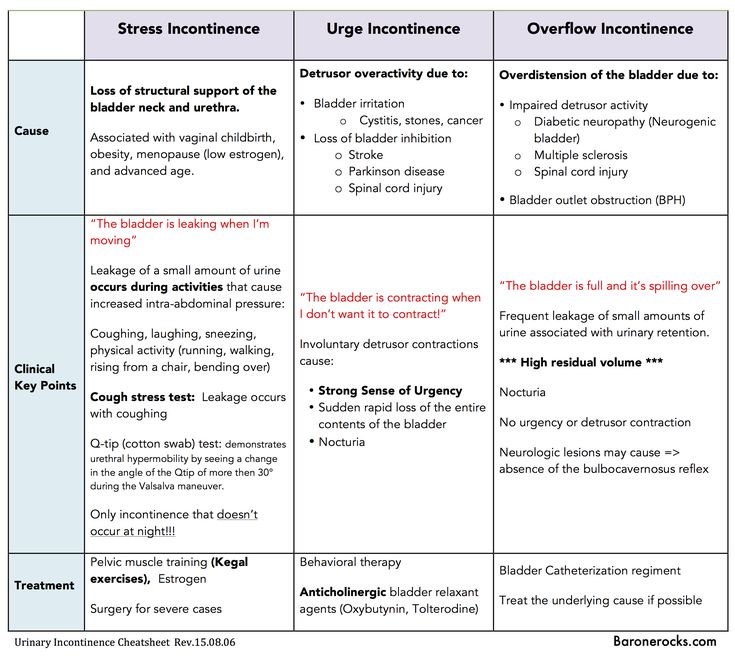 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
86. Viktrup L, Lose G, Rolf M, Barfoed K. The frequency of urinary symptoms during pregnancy and puerperium in the primipara. Int Urogynecol J. 1993;4(1):27–30. [Google Scholar]
87. Dinc A, Kizilkaya Beji N, Yalcin O. Effect of pelvic floor muscle exercises in the treatment of urinary incontinence during pregnancy and the postpartum period. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(10):1223–1231. [PubMed] [Google Scholar]
88. Serati M, Salvatore S, Khullar V, et al. Prospective study to assess risk factors for pelvic floor dysfunction after delivery. Acta Obstet Gynecol Scand. 2008;87(3):313–318. [PubMed] [Google Scholar]
89. Groutz A, Rimon E, Peled S, et al. Cesarean section: does it really prevent the development of postpartum stress urinary incontinence? A prospective study of 363 women one year after their first delivery. Neurourol Urodyn. 2004;23(1):2–6. [PubMed] [Google Scholar]
90. Arrue M, Ibañez L, Paredes J, et al. Stress urinary incontinence six months after first vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):210–214. [PubMed] [Google Scholar]
Stress urinary incontinence six months after first vaginal delivery. Eur J Obstet Gynecol Reprod Biol. 2010;150(2):210–214. [PubMed] [Google Scholar]
91. Hvidman L, Foldspang A, Mommsen S, Bugge Nielsen J. Correlates of urinary incontinence in pregnancy. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(5):278–283. [PubMed] [Google Scholar]
92. Fritel X, Ringa V, Quiboeuf E, Fauconnier A. Female urinary incontinence, from pregnancy to menopause: a review of epidemiological and pathophysiological findings. Acta Obstet Gynecol Scand. 2012;91(8):901–910. [PubMed] [Google Scholar]
93. Brostrøm S, Lose G. Pelvic floor muscle training in the prevention and treatment of urinary incontinence in women—what is the evidence? Acta Obstet Gynecol Scand. 2008;87(4):384–402. [PubMed] [Google Scholar]
94. Kegel N. Progressive resistance exercise in the functional retroration of the perineal muscle. Am J Obstet Gynaecol. 1948;56:238–248. [PubMed] [Google Scholar]
95. Hay-Smith J, Herbison P, Mørkved S (2002) Physical therapies for prevention of urinary and faecal incontinence in adults. Cochrane Database Syst Rev (2):CD003191 [PubMed]
Cochrane Database Syst Rev (2):CD003191 [PubMed]
96. Sangsawang B, Serisathien Y. Effect of pelvic floor muscle exercise programme on stress urinary incontinence among pregnant women. J Adv Nurs. 2012;68(9):1997–2007. [PubMed] [Google Scholar]
97. Price N, Dawood R, Jackson SR. Pelvic floor exercise for urinary incontinence: a systematic literature review. Maturitas. 2010;67(4):309–315. [PubMed] [Google Scholar]
98. Sampselle CM, Miller JM, Mims BL, Delancey JOL, Ashton-Miller JA, Antonakos CL. Effect of pelvic muscle exercise on transient incontinence during pregnancy and after birth. Obstet Gynecol. 1998;91(3):406–412. [PubMed] [Google Scholar]
99. Morkved S, Bo K, Schei B, Salvesen KA. Pelvic floor muscle training during pregnancy to prevent urinary incontinence: a single-blind randomized controlled trial. Obstet Gynecol. 2003;101(2):313–319. [PubMed] [Google Scholar]
100. Ko PC, Liang CC, Chang SD, Lee JT, Chao AS, Cheng PJ. A randomized controlled trial of antenatal pelvic floor exercises to prevent and treat urinary incontinence. Int Urogynecol J. 2011;22(1):17–22. [PubMed] [Google Scholar]
Int Urogynecol J. 2011;22(1):17–22. [PubMed] [Google Scholar]
101. Stafne S, Salvesen K, Romundstad P, Torjusen I, Mørkved S. Does regular exercise including pelvic floor muscle training prevent urinary and anal incontinence during pregnancy? A randomised controlled trial. Br J Obstet Gynaecol. 2012;119(10):1270–1280. [PubMed] [Google Scholar]
102. Glazener CM, Herbison GP, Wilson PD, et al. Conservative management of persistent postnatal urinary and faecal incontinence: randomised controlled trial. BMJ. 2001;323(7313):593–596. [PMC free article] [PubMed] [Google Scholar]
103. Reilly ET, Freeman RM, Waterfield MR, Waterfield AE, Steggles P, Pedlar F. Prevention of postpartum stress incontinence in primigravidae with increased bladder neck mobility: a randomised controlled trial of antenatal pelvic floor exercises. Br J Obstet Gynaecol. 2002;109(1):68–76. [PubMed] [Google Scholar]
104. Newman DK. Conservative management of urinary incontinence in women. Prim Care Updat Obstet Gynecol. 2001;8(4):153–162. [PubMed] [Google Scholar]
2001;8(4):153–162. [PubMed] [Google Scholar]
105. Alewijnse D, Mesters I, Metsemakers J, van den Borne B. Predictors of long-term adherence to pelvic floor muscle exercise therapy among women with urinary incontinence. Heal Educ Res. 2003;18(5):511–524. [PubMed] [Google Scholar]
106. Burns PA, Pranikoff K, Nochajski TH, Hadley EC, Levy KJ, Ory MG. A comparison of effectiveness of biofeedback and pelvic muscle exercise treatment of stress incontinence in older community-dwelling women. J Gerontol. 1993;48:167–174. [PubMed] [Google Scholar]
107. Goode PS, Burgio KL, Locher JL, et al. Effect of behavioral training with or without pelvic floor electrical stimulation on stress incontinence in women: a randomized controlled trial. JAMA. 2003;290(3):345–352. [PubMed] [Google Scholar]
108. Bø K, Kvarstein B, Nygaard I. Lower urinary tract symptoms and pelvic floor muscle exercise adherence after 15 years. Obstet Gynecol. 2005;105(5 Pt 1):999–1005. [PubMed] [Google Scholar]
109. Allahdin S, Kambhampati L. Stress urinary incontinence in continent primigravidas. J Obstet Gynaecol. 2012;32(1):2–5. [PubMed] [Google Scholar]
Allahdin S, Kambhampati L. Stress urinary incontinence in continent primigravidas. J Obstet Gynaecol. 2012;32(1):2–5. [PubMed] [Google Scholar]
What causes urinary incontinence in pregnant women
One of the signs of pregnancy is frequent urination. In process of increase in term the phenomenon is expressed more often, especially at night. Unfortunately, this is often not the only change in the work of the expectant mother's urination organs. Against the background of metamorphoses occurring in the body of a woman, various disorders in the functioning of the kidneys and bladder appear. One of these troubles can be urinary incontinence in pregnant women. The condition causes discomfort but is not a serious health threat. The main symptoms are involuntary excretion of urine in small portions. This usually manifests itself at the moment of tension in the abdominal muscles. If a woman laughs, sneezes or coughs, the laundry suddenly becomes wet. There is no need to be afraid of this, in most cases the condition intensifies in the 2nd or 3rd trimester, but after childbirth the body returns to normal.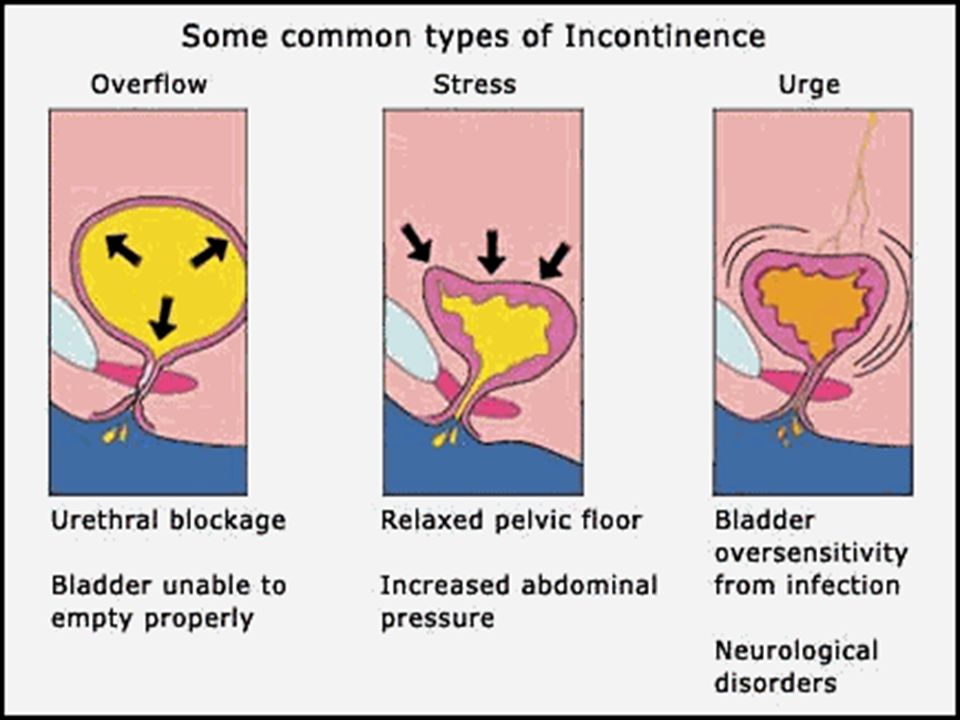 However, to rule out the presence of serious problems, it is worth consulting with your doctor. nine0003
However, to rule out the presence of serious problems, it is worth consulting with your doctor. nine0003
Types of urinary incontinence during pregnancy
Most often, 3 types of urinary incontinence in a pregnant woman appear, and in each case there are characteristic signs.
- Stress. It manifests itself with the tension of the abdominal muscles and fluctuations of the diaphragm. That is, it is enough to sneeze, cough or laugh so that a couple of drops of urine appear on the linen. The condition is typical for the first trimester.
- Urgent. Symptoms are sudden urge to urinate. They arise so unexpectedly that the expectant mother simply does not have enough time to run to the bathroom. One of the causes of the condition lies in the irritation of the urinary canal. You can also blame the failure of the nervous system and overstretching of the muscles in the pelvis. The condition is typical for the last trimester, but also occurs after childbirth. nine0010
- Full bladder syndrome.
 The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.
The symptom is the inability to completely empty the bladder. A woman often feels an acute urge to urinate, and after leaving the toilet it seems that urine remains in the ureter. The reason may be hidden in the stretched and therefore sluggish walls of the bladder.
Regardless of the cause of urinary incontinence in a pregnant woman, the condition causes discomfort and stress. This is not a reason to panic, in fact, the situation is not so critical - most often, not the entire volume of urine from the bladder is released, but only a small amount. To calm down in such a difficult period, it is enough to consult a doctor and get an appointment if necessary. nine0003
Main causes of urinary incontinence in pregnant women
Given that it is not difficult to find an explanation for urinary incontinence in a pregnant woman, it should not cause much concern. It is only necessary to identify the causes and make sure that this is due to physiology, and not diseases of the genitourinary system.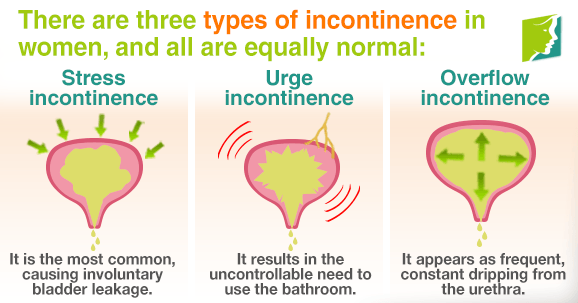 The doctor who leads the pregnancy will help dispel fears.
The doctor who leads the pregnancy will help dispel fears.
The main cause is weakened muscles in the pelvic area. Excessive stretching of muscle tissue leads to loss of tone. As a result, the sphincter that holds urine, the walls of the bladder, and other muscles are weakened. This is due to hormonal changes, as well as changes in the size of internal organs. For example, the growing uterus during pregnancy compresses the bladder. As a result, its volume decreases, and urination occurs more often. nine0003
Another cause of urinary incontinence in a woman during pregnancy is the impact of a baby's foot on the bladder. This phenomenon does not happen to everyone. Doctors explain its severity by the position and size of the fetus, as well as the physical form of the expectant mother.
The number of previous pregnancies and births is also thought to increase the risk of urinary incontinence. Especially if the pregnancies go one after another, and the woman's muscles simply do not have time to recover. nine0003
nine0003
Other factors associated with urinary incontinence during pregnancy are overweight and a sedentary lifestyle. A protracted birth process provokes a problem already in the postpartum period.
Healthy urinary retention occurs when the following conditions are met:
- when the bladder is in a normal position;
- immobility of the urethra;
- good work of the muscles surrounding the bladder and pelvic floor muscles; nine0010
- with the functional and anatomical integrity of the urethra and bladder closure apparatus.
What to do to deal with the problem
As mentioned above, urinary incontinence in women during pregnancy is most often associated with physiological changes, so no treatment is required. However, given the responsibility for the health of the baby during this period, you need to consult a doctor and, according to his appointment, take a urine test. This is necessary to exclude or identify urinary infections and diseases associated with them.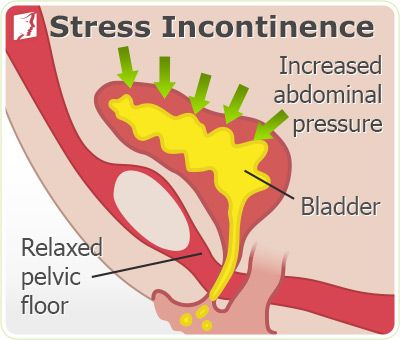 nine0003
nine0003
If the tests do not show deviations, it remains only to calm down and practice hygiene more often. The doctor will give recommendations on hygiene products - their choice and the frequency of changing underwear. But even without a specialist, we can say that the replacement of pads and panties is carried out as needed. Lingerie should fit the size, and it is better to choose a special cut for expectant mothers so that it does not press anywhere. Decorative details on underwear are not welcome, you should give preference to simple panties made of natural fabric. nine0003
If there is a problem, you will often have to wash yourself, go to the toilet on time. Doctors advise you to lean forward slightly when urinating. This will allow the urethra to open completely. At the end, you need to push slightly (without fanaticism) to completely empty the bubble.
Reducing the pressure on the diaphragm can help reduce the risk of urine leakage when sneezing and coughing.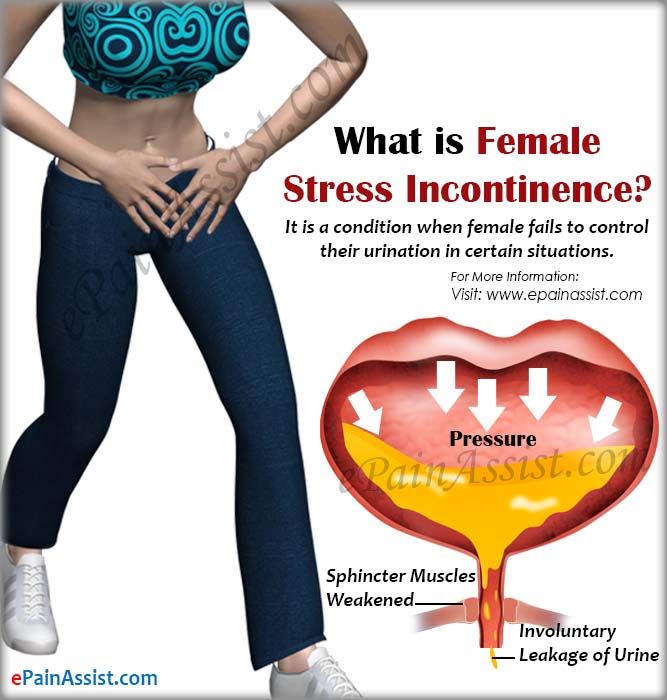 To do this, you need to open your mouth, normalizing the pressure.
To do this, you need to open your mouth, normalizing the pressure.
Examination and treatment
Before dealing with incontinence, it is imperative to establish its cause by contacting a doctor. The doctor, in turn, will prescribe the necessary examination. It usually consists of several stages:
- Urodynamic examination. With the help of it, the work of the upper and lower urinary tract is evaluated.
- Clinical examination. It includes a routine urine test and urine culture for flora, as well as a study in a gynecological chair - during an external examination, the doctor can assess the mobility of the bladder neck during a cough test or straining, assess the condition of the vaginal mucosa and skin, and also identify a possible genital prolapse. nine0010
- Ultrasound examination. It is carried out to study the functioning of the renal system, the urethrovesical segment, the condition of the urethra in a pregnant woman with stress urinary incontinence, as well as to confirm the presence or absence of pathologies of the genitals.
In addition to tests and examinations, you will most likely be asked to keep a special diary in which for several days you will record several parameters of urination, such as the amount of urine released per urination, the number of urination per day, all cases of urinary incontinence, the number of used during the day pads and physical activity. nine0003
Only after the examination, conclusions are drawn about the methods of treatment, which are often necessary only in extreme cases. If no pathology or inflammatory processes are detected, then most likely no special treatment will be carried out, since after childbirth, incontinence most often goes away on its own or occurs less and less.
If incontinence is due to weakening of the pelvic floor muscles, then the situation can be significantly improved with the help of special exercises. Currently, there are a large number of complexes for intimate gymnastics. One of the most popular was developed by the American gynecologist and MD Arnold Kegel.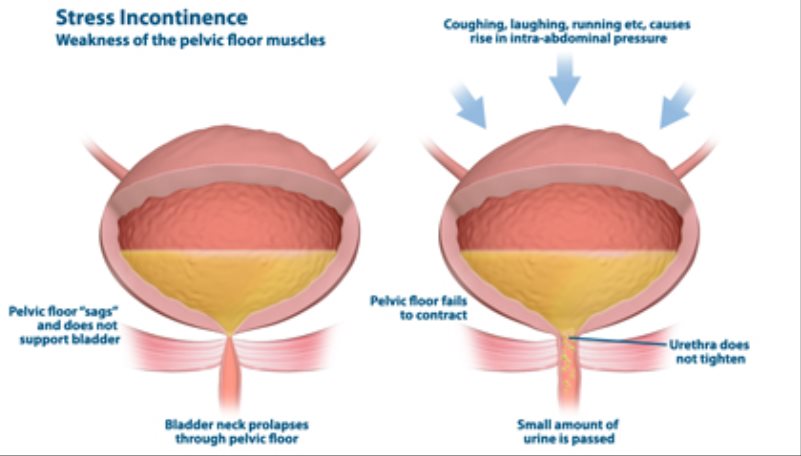 The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay). nine0003
The simplest and, perhaps, the most effective exercise that can be done several times a day is the repeated tension and relaxation of the "intimate muscles" (slow or intense, without delay). nine0003
It is important to know that if you have never strengthened intimate muscles before pregnancy, you need to do this with caution, in no case overdo it.
It is possible that the doctor will prescribe you some herbal preparation that supports the functioning of the bladder and has an antispasmodic, anti-inflammatory and antimicrobial effect.
Treatment with decoctions of herbs (rose hips, sage, dill, lingonberries) may also be recommended. They have not only preventive, but also curative properties. nine0003
Pelvic (intimate) muscle training
To reduce the risk of urinary incontinence in a pregnant woman at night and during the day, doctors recommend doing special exercises. These are Kegel exercises that are useful not only for expectant mothers, but for all women, without exception, regardless of age. The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article. nine0003
The bottom line is to alternate tension and relaxation of intimate muscles. It is not difficult to determine the zone for training - during urination, you need to interrupt the process for a couple of minutes. At this moment, those muscles that are involved in gymnastics will just tighten. You need to do exercises before childbirth, during pregnancy and after the baby is born. A simple and understandable set of exercises will reduce the risk of any problems with the urinary system. You can read more about gymnastics in another article. nine0003
How to ensure your comfort and peace of mind
So that urinary incontinence in pregnant women in the early, and especially in the later stages (38-39 weeks), does not cause increased discomfort, manufacturers of hygiene products produce special pads. One of the options is German MoliMed urological pads. They are specifically designed to provide comfort during involuntary urination. Features of these pads:
- anatomically shaped to prevent urine from leaking out; nine0010
- absorbent layer that instantly absorbs liquids and odors;
- secure fit on underwear;
- small thickness so that the pad is not visible under clothing;
- safe even for sensitive skin;
- the ability to choose a product based on the amount of discharge.
If you need help choosing the right hygiene products, the PAUL HARTMANN Sp. z o.o. hotline will advise you. nine0003
How else can you help yourself
Go to the toilet as often as possible during the day. At the same time, you should not reduce your fluid intake. The expectant mother should drink as much as she wants. But you need to try not to drink large amounts of liquid an hour before bedtime.
Many women use disposable pads to avoid trouble. This should be done only when absolutely necessary, since the frequent use of sanitary pads can provoke colpitis, which, in turn, can lead to infection of the membranes, and as a result, a miscarriage or premature birth due to rupture of the membranes. nine0003
You can somewhat alleviate the condition with the help of a prenatal bandage. Its regular correct wearing allows you to somewhat ease the load on the bladder, respectively, reduce the number of urges to urinate.
Home - Seni
Home - Seni- Seni Club
- Where to buy
- Request a free sample
- Contacts
- nine0010
- Change country
- menu
Urological pads for women with mild to moderate urinary incontinence
More details
Urological pads for women with mild to moderate urinary incontinence
nine0002 Urological inserts for men with mild to moderate urinary incontinenceMore details
Urological inserts for men with mild to moderate urinary incontinence
A wide range of absorbent products for people in need of reliable protection.
More
A wide range of absorbent products for people who need reliable protection.
Absorbent briefs
Absorbent briefs for active people who need comfortable protection. nine0003
Read more
Absorbent briefs for active people who need comfortable protection.
skin care
Daily skin care products
More details
Cosmetics for daily skin care
A well-chosen product not only ensures the comfort of the person who uses it, but also avoids unnecessary costs. nine0003
Find product
It is important to choose the correct size of the product. An incorrectly selected size can lead not only to leakage, but even harm to health. Use the special "form" to select the correct size.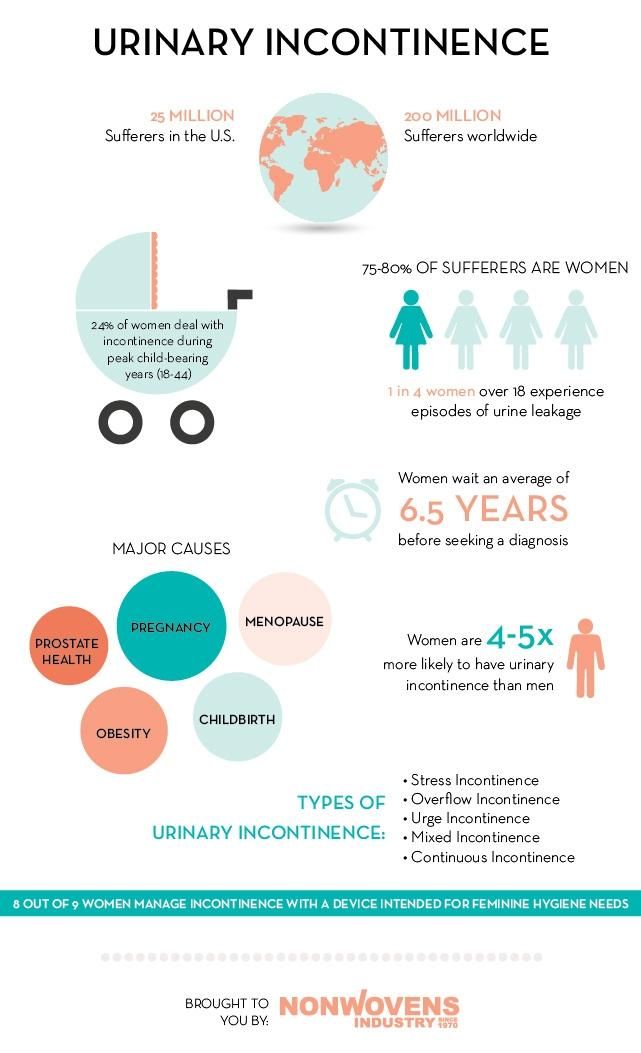
Find size
Seni care products have been helping to properly care for skin that needs especially delicate care for many years. Depending on the purpose, conditions of use and individual characteristics of the skin, seni care cosmetics are conventionally divided into 2 areas: for specialized care and for the care of dry and sensitive skin. Informative packaging design, convenient color identification with special symbols make it easy to choose the right cosmetic product. nine0003
Read more
How to control urinary incontinence
The most effective method of dealing with urinary incontinence is the "small steps" method.
Read more
Hygiene of a seriously ill person
Remember that in many respects it depends on you in what condition the patient's skin will be.