Stages of cervix during pregnancy
Anatomy of pregnancy and birth - cervix
Anatomy of pregnancy and birth - cervix | Pregnancy Birth and Baby beginning of content5-minute read
Listen
Where is the cervix?
The cervix plays a critical role throughout a woman’s life, but never more so than during conception, pregnancy and childbirth. The cervix changes during these events, so it’s important to understand the role of this organ and what these changes mean for you and your baby.
The cervix is the muscular channel or opening that runs between the uterus (also known as the womb) and the vagina. The cervix is located in the pelvis and lies behind the bladder and near the front of the rectum. It is held in its position by tough, flexible ligaments.
Illustration showing the female reproductive system.What does the cervix do in women who are not pregnant?
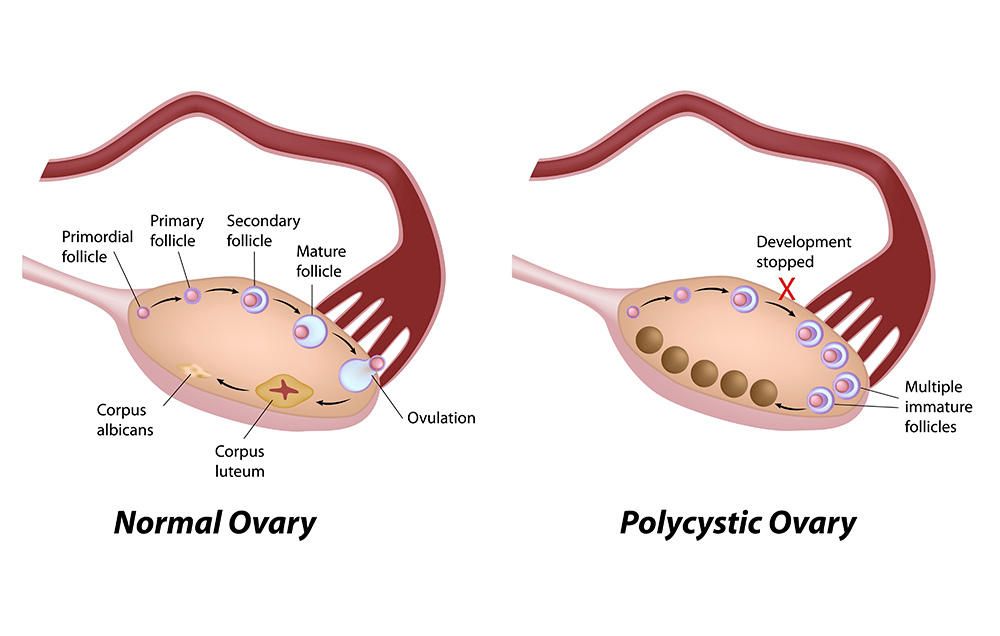
In women who are not pregnant, the cervix is narrow and firm. Its size, shape and lining undergo subtle changes throughout a woman’s menstrual cycle.
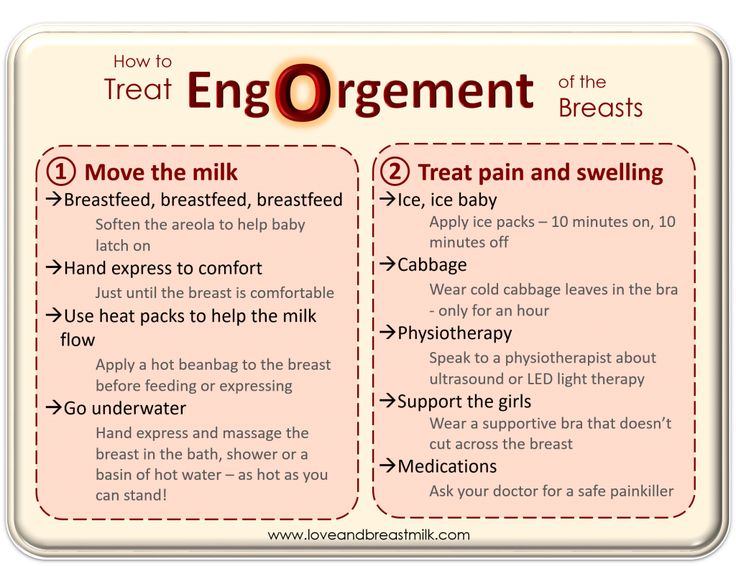
For instance, the cervix has a smooth covering of mucus. When a woman is ovulating, the mucus becomes stretchy and elastic, which helps sperm move and survive following intercourse, and is known as ‘fertile mucus’. When a woman is not ovulating, the mucus takes on a more creamy texture and can be milky or yellow in colour. This change in consistency indicates that sperm are less likely to reach the uterus after intercourse at this time in the menstrual cycle.
The cervix contains a channel, referred to as the 'cervical canal', which also has an important role in women who are not pregnant. Sperm enters the uterus after intercourse and menstrual blood leaves the uterus during menstruation through this channel.
What is the function of the cervix during conception and pregnancy?
The cervix has several important functions during conception.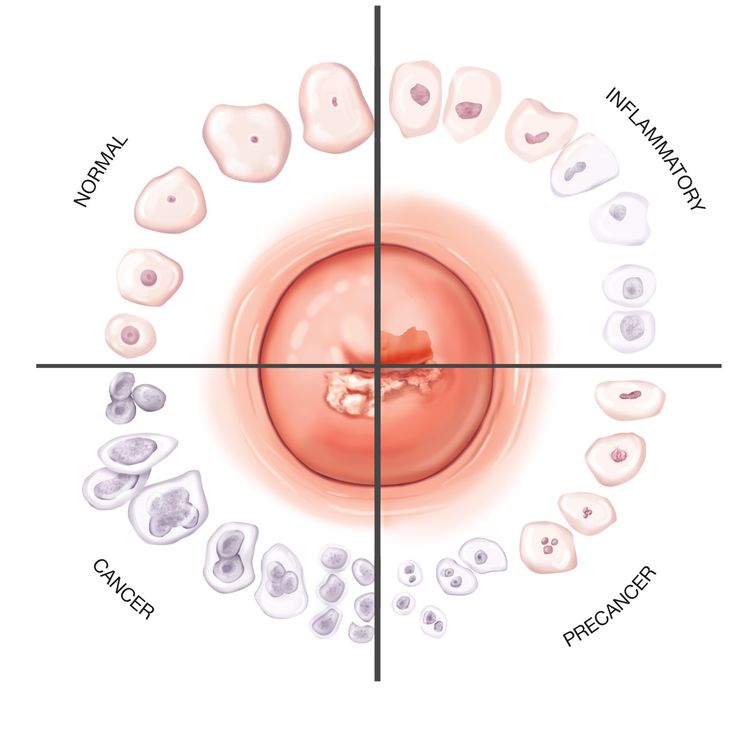 After a woman conceives, the mucus on the surface of the cervix becomes sticky and thick. This stops new sperm and microorganisms, such as bacteria and viruses, from entering the uterus and potentially harming the fetus.
After a woman conceives, the mucus on the surface of the cervix becomes sticky and thick. This stops new sperm and microorganisms, such as bacteria and viruses, from entering the uterus and potentially harming the fetus.
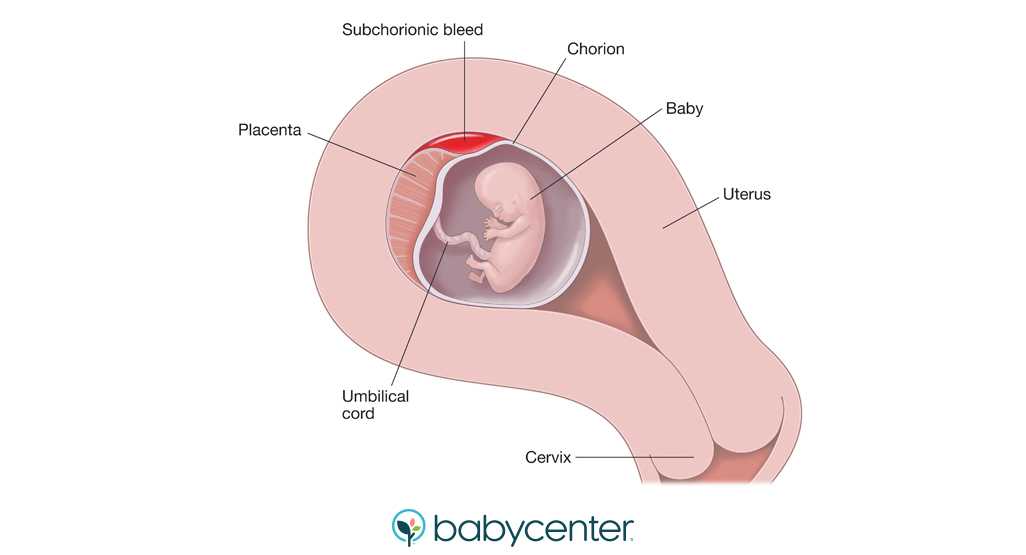
The cervix also plays a crucial role during pregnancy. From conception until just before birth, the cervix protects the growing baby by increasing in size and strength, helping to keep the baby safe and secure in the uterus.
How does the cervix change during labour?
The cervix undergoes dramatic changes during labour in a process known as ‘effacement’ or ‘ripening’. It starts out long and firm, and as labour progresses, it softens, widens and becomes more elastic.
Changes to the cervix are partly triggered by contractions of the muscles of the uterus, which help open the cervix. As the cervix begins to open, you may see a clear, pink, or slightly bloody discharge (sometimes referred to as the 'show'). This is the release of the mucus plug, that sits over the cervical canal during pregnancy.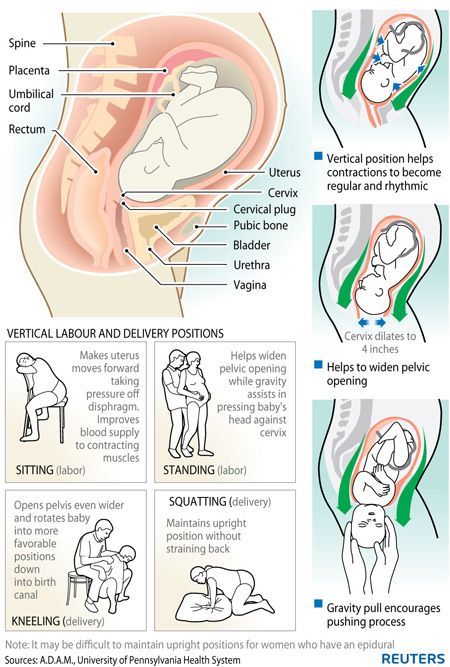
The first stage of labour begins when you feel contractions — your cervix will start to soften and to open. The time it takes for the cervix to open (or dilate) will vary from woman to woman and can range from several hours to days or even weeks. Once the cervix is dilated more than 3cm, and contractions are strong and regular, labour is said to be ‘established’.
Established labour is also known as the 'active phase'. This phase continues until the cervix dilates to approximately 7cm, with the contractions being strong, painful and around every 3 or 4 minutes.
This is followed by the ‘transition phase’, when the cervix continues to fully open. There is now less time to rest in between contractions.
First stage of labour is complete when the cervix is fully open (referred to as 'fully dilated'), the baby moves through the pelvis and the mother can begin pushing the baby out. Being fully dilated might not actually be a 10cm opening of the cervix. Rather it is when the doctor or midwife cannot feel any cervix when they perform a vaginal examination.
The second stage of labour is when your baby is being born and the third stage is when the placenta is delivered.
What problems can occur with the cervix during pregnancy, labour, or birth?
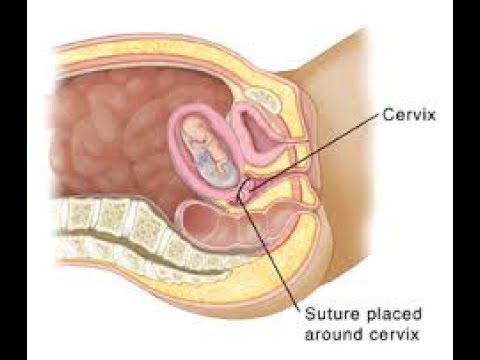
The cervix is monitored throughout pregnancy, labour and birth to identify any problems. For instance, if the cervix is weak, it might be difficult to keep the baby in the uterus for the whole pregnancy. This can lead to premature labour and birth.
During labour, contractions might not be regular or strong enough to fully open the cervix, which slows labour down. In these situations, the doctor or midwife might intervene by breaking the mother's waters or using a hormone to increase contractions and speed up the dilation of the cervix.
It is important that the mother does not begin pushing the baby out until the cervix is fully dilated. This is because pushing too soon might swell the cervix, which can slow down the birth.
Read more here about complications in labour, and how they are managed.
Sources:
MSD Manual (Female internal genital organs), Translational Research in Anatomy (March 2016) (The structure and function of the cervix during pregnancy), Women's Health (Understanding your menstrual cycle fact sheet), Mater Mother's Hospital (Labour and birth information), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth), Royal Women's (Stages of labour), King Edward Memorial Hospital (Second stage of labour and birth), SA Health (Induction of labour techniques), Queensland Health (Vaginal examinations in labour)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2020
Back To Top
Related pages
- Anatomy of pregnancy and birth - uterus
- Anatomy of pregnancy and birth - perineum and pelvic floor
- Anatomy of pregnancy and birth - pelvis
- Anatomy of pregnancy and birth - abdominal muscles
- Anatomy of pregnancy and birth
Need more information?
Uterus, cervix & ovaries - fact sheet | Jean Hailes
This fact sheet discusses some of the health conditions that may affect a woman's uterus, cervix and ovaries.
Read more on Jean Hailes for Women's Health website
Placenta previa - Better Health Channel
Placenta previa means the placenta has implanted at the bottom of the uterus, over the cervix or close by.
Read more on Better Health Channel website
Diaphragm - how effective is the diaphragm - Sexual Health Victoria
A diaphragm is a shallow, cup-shape made of silicone inserted inside the cervix. In Australia there is one size diaphragm available sold as Caya®.
Read more on Sexual Health Victoria website
Pap smear tests - MyDr.com.au
Pap smear tests are currently used in Australia as a screening test for cervical cancer.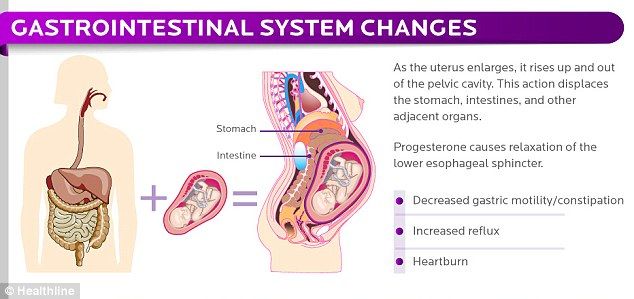 A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
A Pap smear test can detect changes in the cells of the cervix that may develop into cancer.
Read more on myDr website
Labour & birth: what to expect | Raising Children Network
Early labour signs include a show, waters breaking and pain. During labour, your contractions increase and your cervix dilates, so you can birth your baby.
Read more on raisingchildren.net.au website
Induction of labour
Inducing labour allows women to deliver their baby normally by stimulating labour contractions. There are several medical and surgical techniques which can be used.
Read more on Parenthub website
What happens to your body in childbirth
During childbirth, your body's hormones, ligaments and muscles, as well as the shape of your pelvis, all work together to bring your baby safely into the world.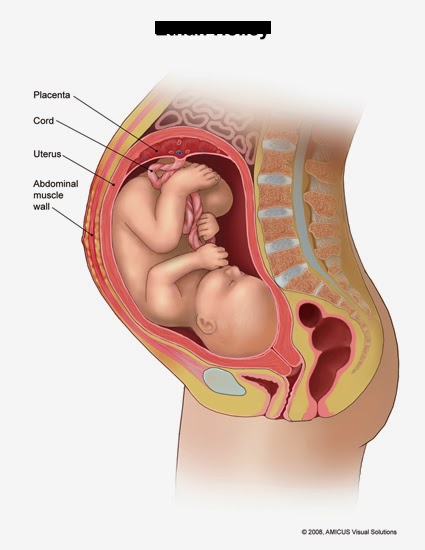
Read more on Pregnancy, Birth & Baby website
Dilatation and curettage (D&C) - Better Health Channel
A dilatation and curettage (D&C) is an operation performed on women to lightly scrape away the womb lining.
Read more on Better Health Channel website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Cervical Screening | Pap Smear | Jean Hailes
All you need to know about cervical screening tests and how they differ from pap smears. Learn why and when you should have one and how they work.
Read more on Jean Hailes for Women's Health website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.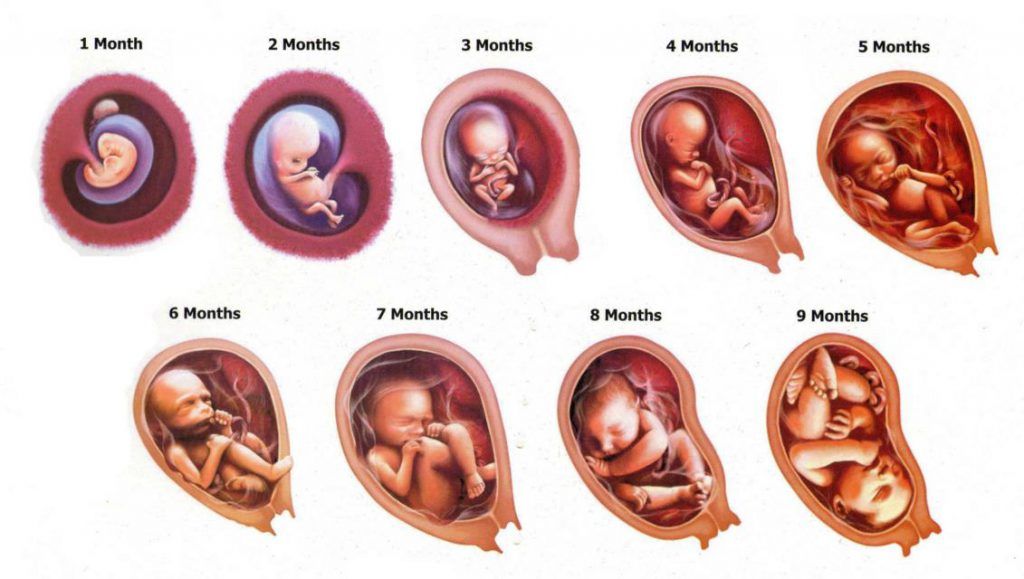
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.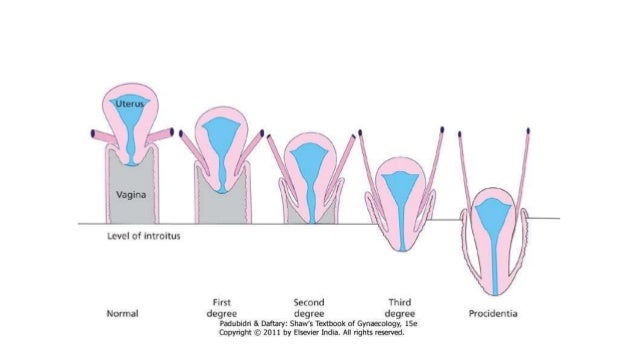 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Cervix Dilation Chart: Stages of Labor
The cervix, which is the lowest portion of the uterus, opens when a woman has a baby, through a process called cervical dilation. The process of the cervix opening (dilating) is one way that healthcare staff track how a woman’s labor is progressing.
During labor, the cervix opens to accommodate the passage of baby’s head into the vagina, which is around 10 centimeters (cm) dilated for most term babies.
If your cervix is dilated with regular, painful contractions, you’re in active labor and getting closer to delivering your baby.
The first stage of labor is divided into two parts: the latent and active phases.
The latent phase of labor is the first stage of labor. It can be thought of more as the “waiting game” stage of labor. For first-time moms, it can take a while to move through the latent phase of labor.
In this stage, contractions aren’t yet strong or regular. The cervix is essentially “warming up,” softening, and shortening as it prepares for the main event.
You might consider picturing the uterus as a balloon. Think of the cervix as the neck and opening of the balloon. As you fill that balloon up, the neck of the balloon draws up with the pressure of the air behind it, similar to the cervix.
The cervix is simply the bottom opening of the uterus drawing up and opening wider to make room for the baby.
Active stage of laborA woman is considered to be in the active stage of labor once the cervix dilates to around 5 to 6 cm and contractions begin to get longer, stronger, and closer together.
The active stage of labor is characterized more by the rate of regular cervical dilation per hour. Your doctor will expect to see your cervix opening at a more regular rate during this stage.
How long does stage 1 of labor last?There’s no scientific hard and fast rule for how long the latent and active phases last in women. The active stage of labor can range from a woman dilating anywhere from 0.5 cm per hour up to 0.7 cm per hour.
How fast your cervix dilates will also depend on if it’s your first baby or not. Mothers who have delivered a baby before tend to move more quickly through labor.
Some women will simply progress more quickly than others. Some women may “stall” at a certain stage, and then dilate very quickly.
In general, once the active stage of labor kicks in, it’s a safe bet to expect a steady cervical dilation every hour. Many women don’t start really dilating more regularly until closer to around 6 cm.
The first stage of labor ends when a woman’s cervix is fully dilated to 10 cm and fully effaced (thinned out).
The second stage of labor begins when a woman’s cervix is fully dilated to 10 centimeters. Even though a woman is fully dilated, it doesn’t mean that the baby is necessarily going to be delivered immediately.
A woman may reach full cervical dilation, but the baby may still need time to move down the birth canal fully to be ready for birth. Once the baby is in prime position, it’s time to push. The second stage ends after the baby is delivered.
How long does stage 2 of labor last?In this stage, there’s again a wide range for how long it can take for the baby to come out. It can last anywhere from minutes to hours. Women may deliver with only a few hard pushes, or push for an hour or more.
Pushing occurs only with contractions, and the mother is encouraged to rest between them. At this point, the ideal frequency of contractions will be about 2 to 3 minutes apart, lasting 60 to 90 seconds.
In general, pushing takes longer for first-time pregnant people and for women who have had epidurals.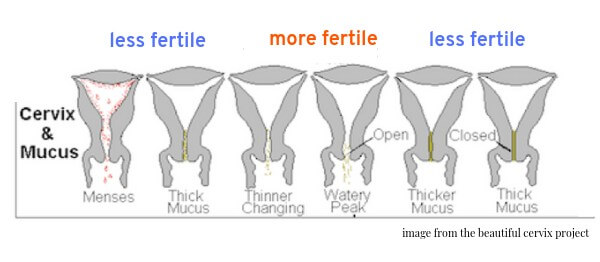 Epidurals can reduce the woman’s urge to push and interfere with her ability to push. How long a woman is allowed to push depends on:
Epidurals can reduce the woman’s urge to push and interfere with her ability to push. How long a woman is allowed to push depends on:
- the hospital’s policy
- the doctor’s discretion
- the health of the mom
- the health of the baby
The mother should be encouraged to change positions, squat with support, and rest between contractions. Forceps, vacuum, or cesarean delivery is considered if the baby isn’t progressing or the mother is becoming exhausted.
Again, every woman and baby is different. There’s no universally accepted “cut-off time” for pushing.
The second stage ends with the birth of the baby.
The third stage of labor is perhaps the most forgotten phase. Even though the “main event” of birth has occurred with the birth of the baby, a woman’s body still has important work to do. In this stage, she’s delivering the placenta.
A woman’s body actually grows an entirely new and separate organ with the placenta. Once the baby is born, the placenta no longer has a function, so her body must expel it.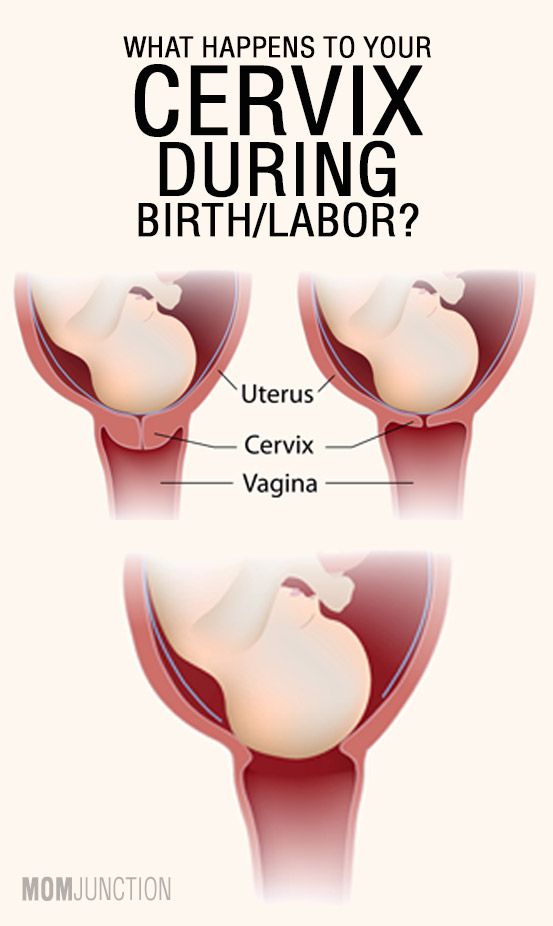
The placenta is delivered the same way as the baby, through contractions. They may not feel as strong as the contractions that are needed to expel the baby. The doctor directs the mother to push and the delivery of the placenta is typically over with one push.
How long does stage 3 of labor last?The third stage of labor can last anywhere from 5 to 30 minutes. Putting the baby on the breast for breastfeeding will hasten this process.
Postpartum recovery
Once the baby is born and the placenta has been delivered, the uterus contracts and the body recovers. This is often referred to as the fourth stage of labor.
After the hard work of moving through the stages of labor is finished, a woman’s body will need time to return to its nonpregnant state. On average, it takes about 6 weeks for the uterus to return to its nonpregnant size and for the cervix to return to its prepregnancy state.
Changes in the cervix during pregnancy
Pregnancy is always pleasant, but sometimes not planned.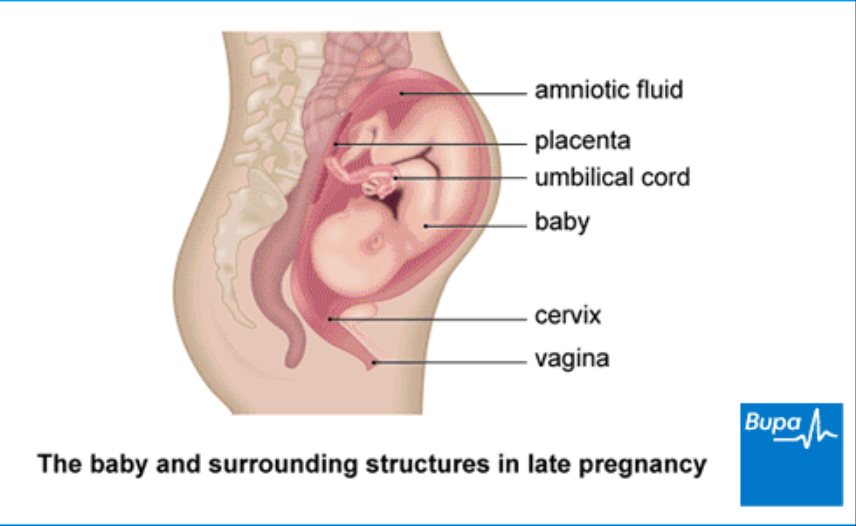 And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
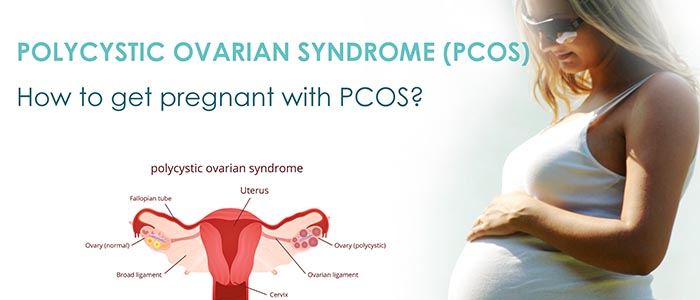
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is called the supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix, the cervical canal passes, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina.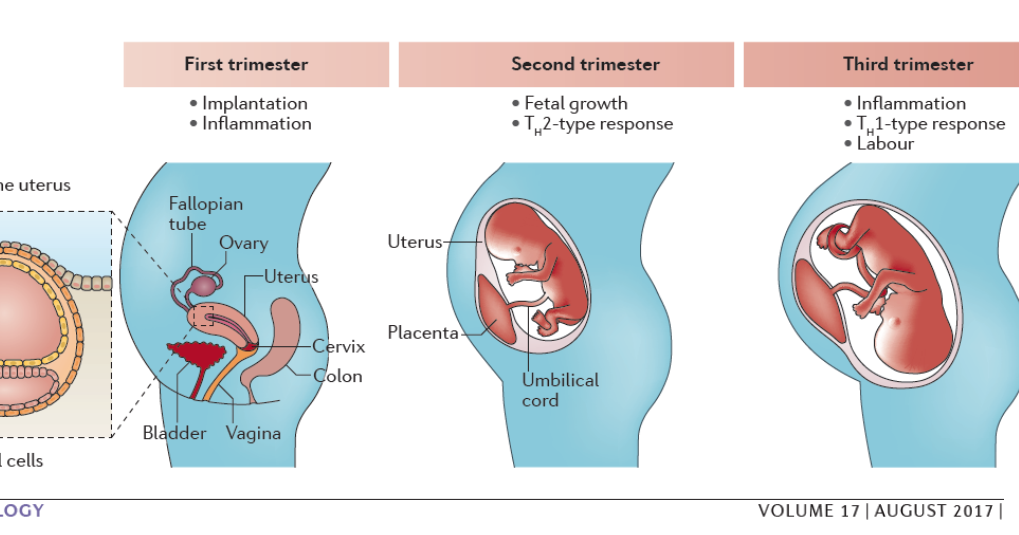 Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm. nine0003
Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm. nine0003
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary. nine0003
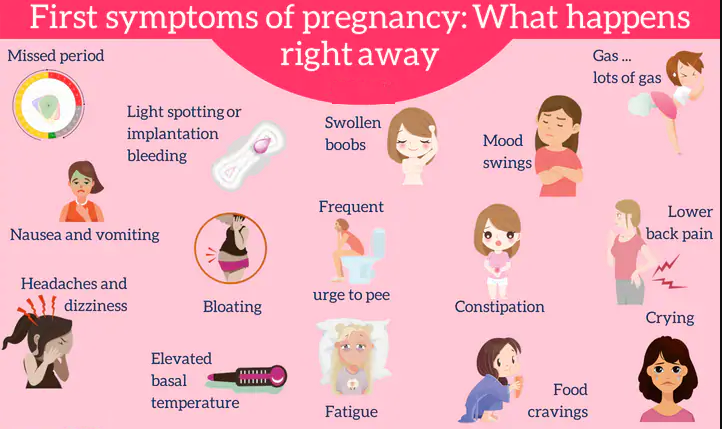
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft.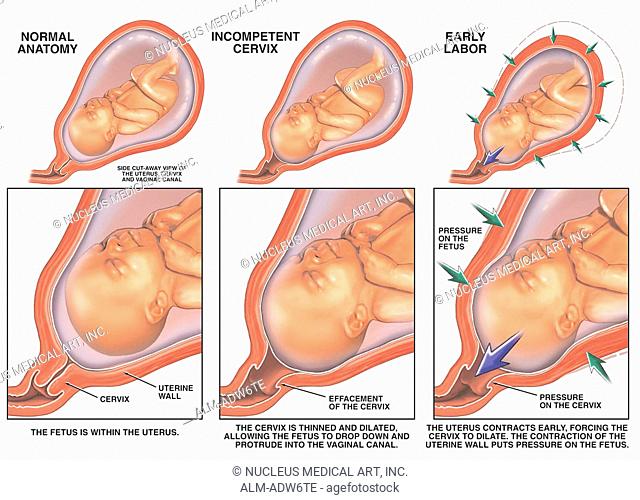 During pregnancy, the cervical glands expand and become more branched.
During pregnancy, the cervical glands expand and become more branched.
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones. nine0003
Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones. nine0003
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection.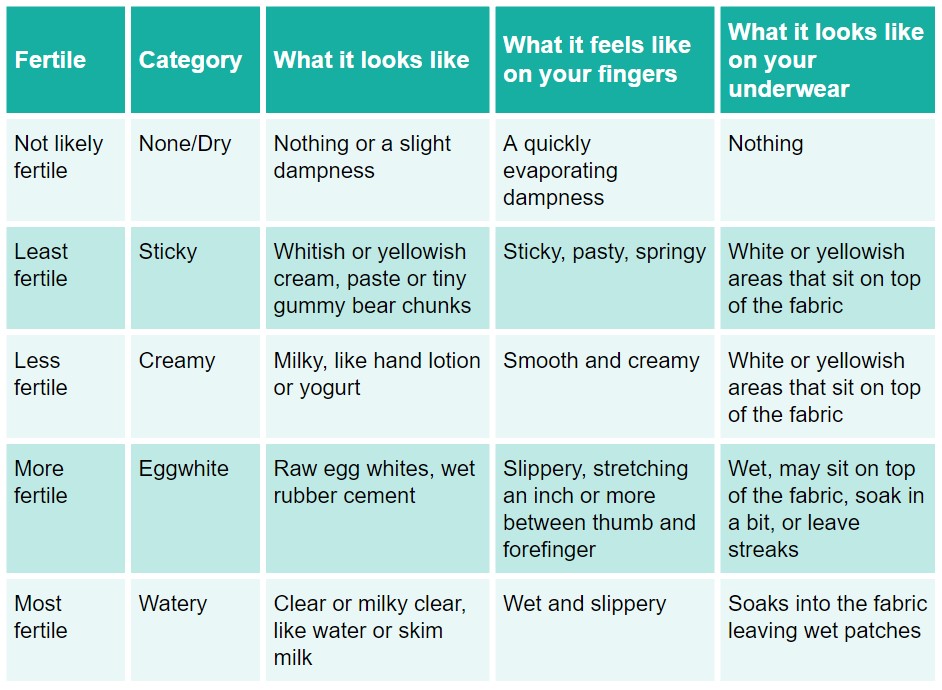 Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth. nine0003
Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth. nine0003
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be: nine0003
The reasons may be: nine0003
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20–23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders; nine0032
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.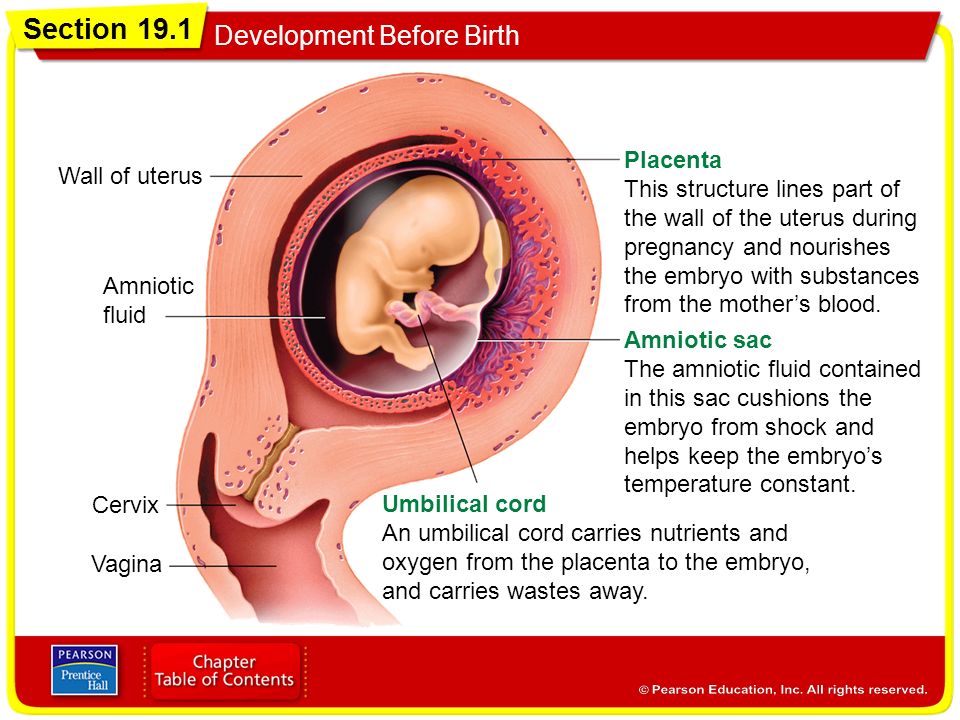 nine0003
nine0003
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select a clinic
Clinical Hospital of IDKClinic "Mother and Child" Entuziastov Samara
nine0002 All directionsSpecialist consultations (adults)Specialist consultations (children's)Laboratory of molecular geneticsGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsUltrasound examinations for adults01.
Specialist consultations (adults)
02.
Specialist consultations (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
other gynecological operations
07.
Telemedicine for adults
08. examinations
09.
Adult ultrasound examinations
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Management of pregnant women with invasive cervical cancer | Payanidi Yu.G., Borovkova E.I., Dobrokhotova Yu.E., Arutyunyan A.M.
Introduction
Cervical cancer (CC) is one of the most common malignancies in pregnant women, with an incidence of 0.8 to 1.5 cases per 10,000 births. During pregnancy and during the first year after childbirth, up to 3% of cases of the disease are verified [1, 2].
There have been no large randomized trials on which recommendations for the management of pregnant women with cervical cancer can be based.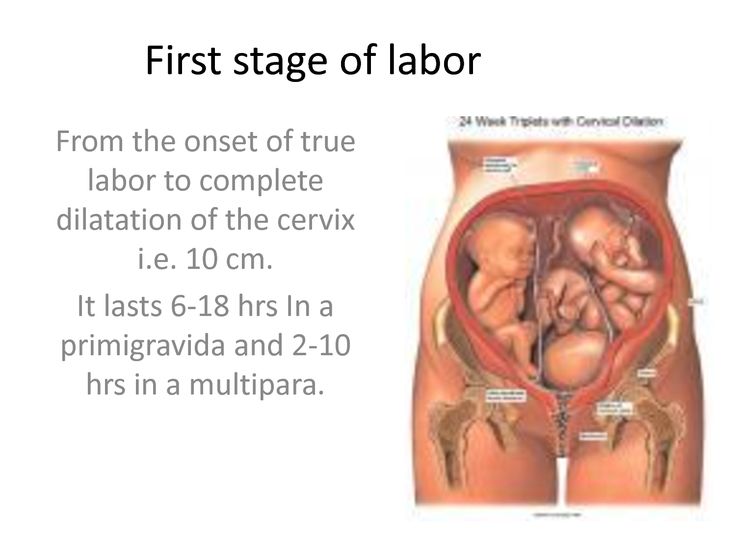 And in the treatment of this category of patients, recommendations based on materials from studies involving non-pregnant patients are applied. At the same time, the tactics of managing pregnant women with cervical cancer is additionally determined by the gestational age, the stage of the tumor process, and the patient's desire to maintain the pregnancy. Treatment should be individual, timely, with minimal risk to the woman and fetus [2]. nine0096 During pregnancy, cervical cancer in most cases is diagnosed in the early stages, and the average gestational age is 19.5 weeks. [3, 4]. Clinical manifestations of cervical cancer during pregnancy are often absent or may be mistaken for obstetric complications (vaginal bleeding, pelvic pain, pain along the sciatic nerve, anemia).
And in the treatment of this category of patients, recommendations based on materials from studies involving non-pregnant patients are applied. At the same time, the tactics of managing pregnant women with cervical cancer is additionally determined by the gestational age, the stage of the tumor process, and the patient's desire to maintain the pregnancy. Treatment should be individual, timely, with minimal risk to the woman and fetus [2]. nine0096 During pregnancy, cervical cancer in most cases is diagnosed in the early stages, and the average gestational age is 19.5 weeks. [3, 4]. Clinical manifestations of cervical cancer during pregnancy are often absent or may be mistaken for obstetric complications (vaginal bleeding, pelvic pain, pain along the sciatic nerve, anemia).
Tactics of treatment of patients with cervical cancer
The tactics of treating patients with cervical cancer is determined by the stage of the disease, gestational age, as well as the involvement of regional lymph nodes in the process.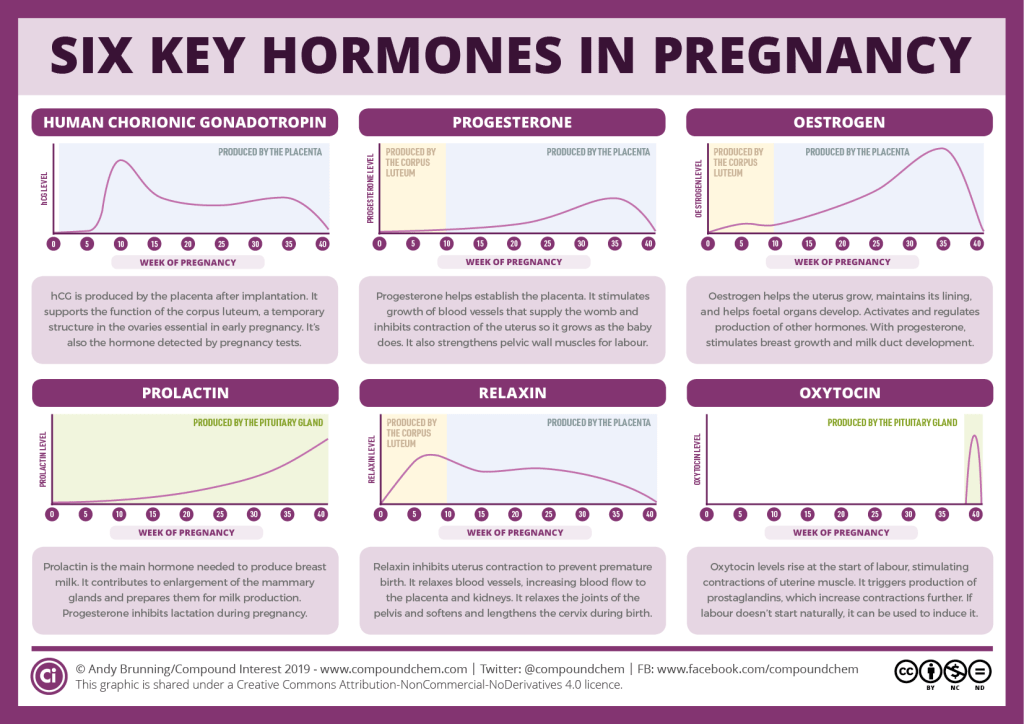 The main methods of treatment are surgical and medical (chemotherapy) [5–7] (Table 1). nine0096
The main methods of treatment are surgical and medical (chemotherapy) [5–7] (Table 1). nine0096
According to the order of the Ministry of Health of Russia No. 572n dated November 1, 2012, all pregnant women are subject to mandatory cytological screening, which allows for a timely diagnosis. If signs suspicious of a microinvasive process are identified, an atypical conization of the cervix is performed with a cone height of not more than 1.5 cm. During pregnancy, curettage of the cervical canal is not performed due to the high risk of abortion after this manipulation. Cervical conization can be performed at any gestational age, but not less than 4 weeks before. before the expected birth. In stage IA1 (invasion up to 3 mm and horizontal extension up to 7 mm without vascular invasion), conization is the optimal and safe method of treatment. The risk of metastasis is 0.8% for squamous cell carcinoma and 1.5% for adenocarcinoma. If pelvic lymph node involvement is suspected, pelvic lymphadenectomy (PLAE) or sentinel lymph node biopsy is indicated [8].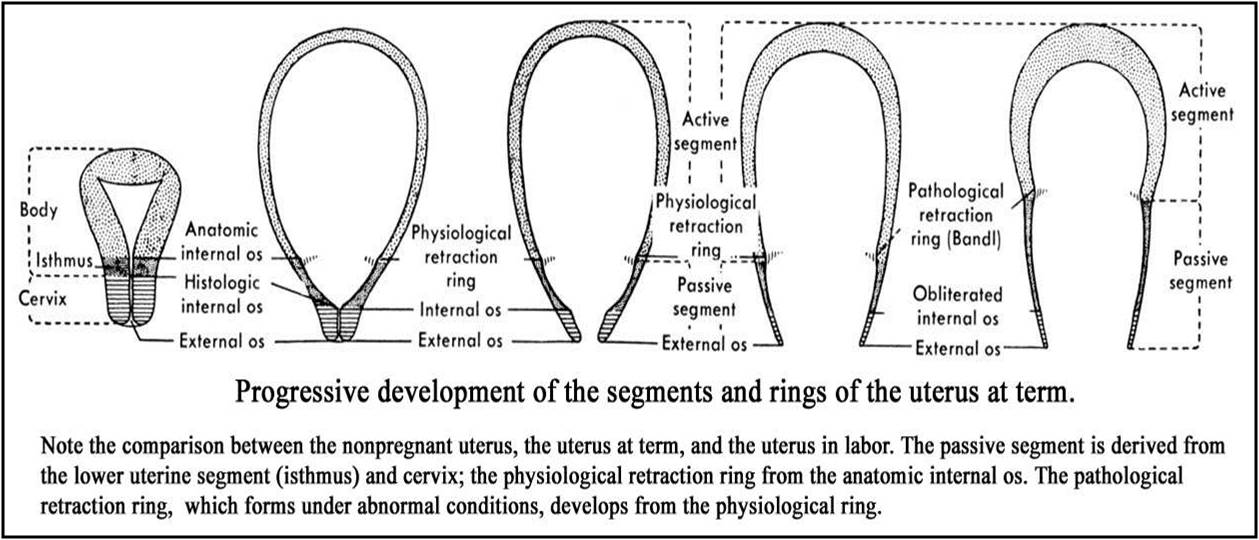 nine0096 Case management up to 22 weeks . gestation with IA2 and IB1 stage and tumor up to 2 cm.
nine0096 Case management up to 22 weeks . gestation with IA2 and IB1 stage and tumor up to 2 cm.
At the first stage, an atypical conization of the cervix with lymphadenectomy is performed. If lymph node metastasis is confirmed, termination of the pregnancy should be considered. In the absence of lymph node involvement, it is possible to prolong pregnancy with standard therapy after delivery (in stage IA2) or neoadjuvant chemotherapy (NAHT) (in stage IB1) with delayed standard treatment after delivery [9] (Fig. 1).
Management of patients over 22 weeks. with IA2 and IB1 stage with a tumor up to 2 cm. At this gestational age, atypical cervical conization is performed to stage the process. Pelvic lymphadenectomy is not performed due to technical limitations related to the size of the uterus. When stage IA2 is confirmed, standard treatment is carried out after delivery; at stage IB1, neoadjuvant polychemotherapy is started [9].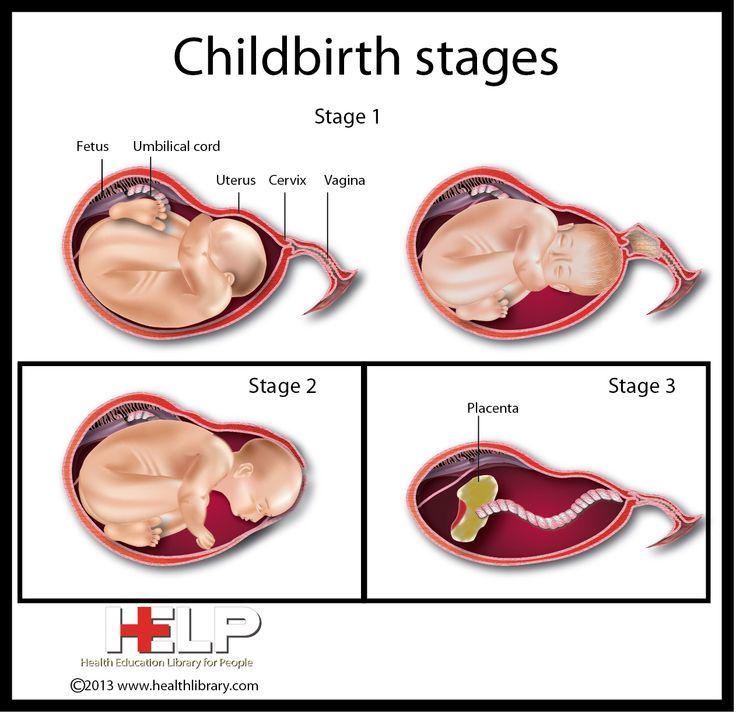
Management of pregnant women up to 22 weeks. with IB1 stage and tumor up to 2–4 cm. TLAE is carried out to clarify the prevalence of the process. If lymph node involvement is confirmed, termination of pregnancy is recommended followed by standard treatment. In case of intact lymph nodes after 12 weeks. start NAC [9].
Pregnant women up to 22 weeks' gestation. with confirmed cervical cancer IB2 and stage IIA , termination of pregnancy is recommended regardless of the involvement of the lymph nodes [9]. After 22 weeks conduct several NACT courses. The last course must be completed no later than 3 weeks. before childbirth [9].
Surgical treatment
Diagnosis of cervical cancer is based on histological examination, but the prognosis of the disease is determined by the size of the tumor and the involvement of the lymph nodes in the pathological process. In the first half of pregnancy (up to 22 weeks), laparoscopic PLAE is a safe and highly informative operation [10].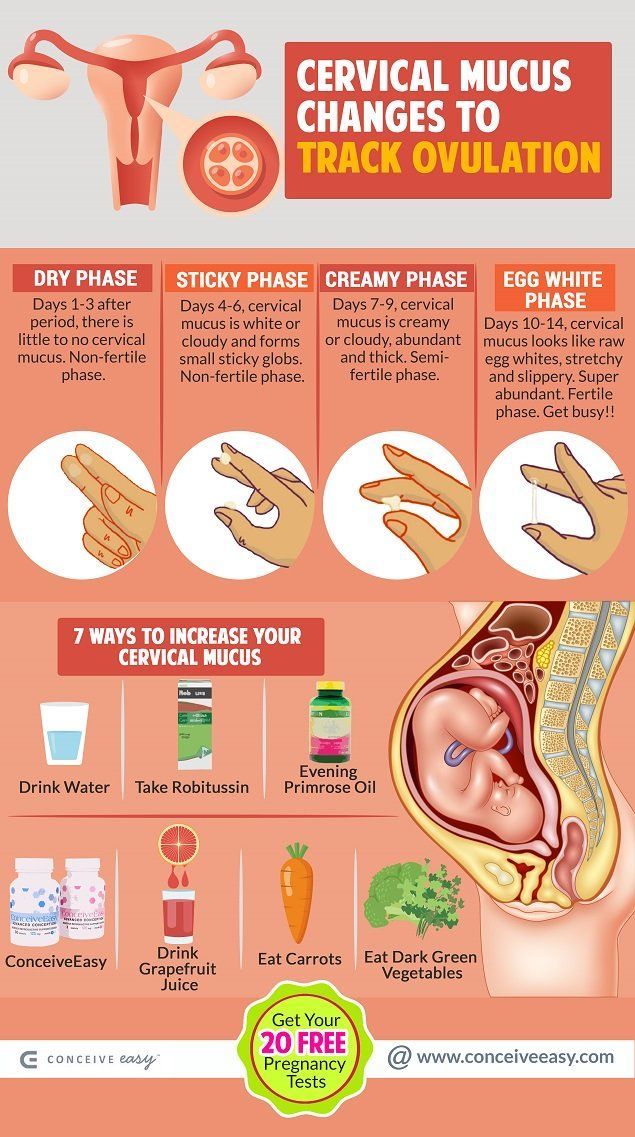 When metastases are detected, termination of pregnancy and chemoradiotherapy are indicated [11]. Prolongation of pregnancy is acceptable with intact lymph nodes and the onset of NAC [11]. Trachelectomy during pregnancy is not recommended due to low efficiency and high risk of miscarriage (up to 34%) [12]. nine0003
When metastases are detected, termination of pregnancy and chemoradiotherapy are indicated [11]. Prolongation of pregnancy is acceptable with intact lymph nodes and the onset of NAC [11]. Trachelectomy during pregnancy is not recommended due to low efficiency and high risk of miscarriage (up to 34%) [12]. nine0003
Neoadjuvant chemotherapy
In the case of prolongation of pregnancy in patients with locally advanced cervical cancer, NAC allows to stabilize the tumor process [6]. The calculation of the therapeutic dose and the choice of the drug is identical to those outside of pregnancy. However, it must be taken into account that the physiological changes associated with pregnancy (hemodilution, hypoproteinemia, acceleration of the glomerular filtration rate, the appearance of a third space - the amniotic cavity) affect the pharmacokinetic properties of chemotherapy drugs. nine0096 According to international protocols, chemotherapy is not performed in the first trimester of pregnancy due to the high risk of embryotoxic and teratogenic effects.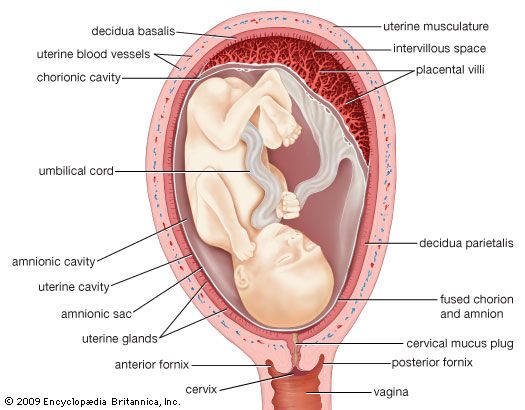 During pregnancy in patients with cervical cancer, chemotherapy can be performed starting from the second trimester: with stage IB1, no metastases in the lymph nodes and tumor size <2 cm; at stage IB1 and tumor size of 2–4 cm, in the absence of metastases to the lymph nodes or when lymphadenectomy is impossible, as well as at stages IB2–IIB - until the period of fetal maturity [4, 12]. nine0096 In the vast majority of cases, NAC allows to stabilize the tumor process and prolong pregnancy until the fetus reaches viability and maturity. The most common regimen includes cisplatin (50–100 mg/m 2 ) alone or in combination with paclitaxel (175 mg/m 2 ). Courses are held at intervals of every 3 weeks. [13]. Less common is the combination of cisplatin (75 mg/m 2 ) with ifosfamide 2 g/m 2 cycles every 2 weeks. [12, 14]. nine0003
During pregnancy in patients with cervical cancer, chemotherapy can be performed starting from the second trimester: with stage IB1, no metastases in the lymph nodes and tumor size <2 cm; at stage IB1 and tumor size of 2–4 cm, in the absence of metastases to the lymph nodes or when lymphadenectomy is impossible, as well as at stages IB2–IIB - until the period of fetal maturity [4, 12]. nine0096 In the vast majority of cases, NAC allows to stabilize the tumor process and prolong pregnancy until the fetus reaches viability and maturity. The most common regimen includes cisplatin (50–100 mg/m 2 ) alone or in combination with paclitaxel (175 mg/m 2 ). Courses are held at intervals of every 3 weeks. [13]. Less common is the combination of cisplatin (75 mg/m 2 ) with ifosfamide 2 g/m 2 cycles every 2 weeks. [12, 14]. nine0003
Tactics of delivery of pregnant women with cervical cancer
The last course of polychemotherapy should be completed within 3 weeks. before the expected date of birth. This is associated with the risk of giving birth to a child with suppressed bone marrow and a high probability of developing infectious complications in him [14, 15]. Currently, it is recommended to prolong pregnancy at least until full term (37 weeks), in the absence of such an opportunity, at least up to 34 weeks. [14–17].
before the expected date of birth. This is associated with the risk of giving birth to a child with suppressed bone marrow and a high probability of developing infectious complications in him [14, 15]. Currently, it is recommended to prolong pregnancy at least until full term (37 weeks), in the absence of such an opportunity, at least up to 34 weeks. [14–17].
After conization of the cervix, performed at stages IA1–IA2, vaginal delivery is theoretically possible [9]. In the case of advanced cervical cancer, the method of delivery is a corporal caesarean section followed by a Wertheim operation. The choice of delivery method depends on the stage of the disease, taking into account the desire of the patient to maintain fertility [1, 2, 12, 18–20].
Conclusion
The "gold standard" for the treatment of cervical cancer in pregnant women has not yet been developed. It should be recognized that the above ESGO clinical guidelines, unfortunately, cannot answer all questions. For example, from our point of view, an important prognostic factor is the biological characteristics of the neoplasm, which are not taken into account in the recommendations. It is also not clear what the tactics of treatment are at the advanced stages of the process and whether the recommended vaginal delivery is not risky at the IA2 stage of the disease, etc. based on world experience. It is necessary to emphasize the special role of a multidisciplinary approach with the participation of an oncogynecologist, an obstetrician-gynecologist, a neonatologist, chemo- and radiation therapists, a psychologist, and a lawyer in solving a number of important issues. nine0003
For example, from our point of view, an important prognostic factor is the biological characteristics of the neoplasm, which are not taken into account in the recommendations. It is also not clear what the tactics of treatment are at the advanced stages of the process and whether the recommended vaginal delivery is not risky at the IA2 stage of the disease, etc. based on world experience. It is necessary to emphasize the special role of a multidisciplinary approach with the participation of an oncogynecologist, an obstetrician-gynecologist, a neonatologist, chemo- and radiation therapists, a psychologist, and a lawyer in solving a number of important issues. nine0003
Information about the authors:
1 Payanidi Yuliya Gennadievna — Doctor of Medical Sciences, Senior Researcher of the Gynecological Department, ORCID iD 0000-0001-5950-4543;
2Borovkova Ekaterina Igorevna – Doctor of Medical Sciences, Professor of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0001-7140-262Х;
2 Dobrokhotova Yulia Eduardovna — Doctor of Medical Sciences, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0001-6571-3448; nine0096 2 Harutyunyan Anna Meruzhanovna — postgraduate student of the Department of Obstetrics and Gynecology, Faculty of Medicine, ORCID iD 0000-0002-6392-5444.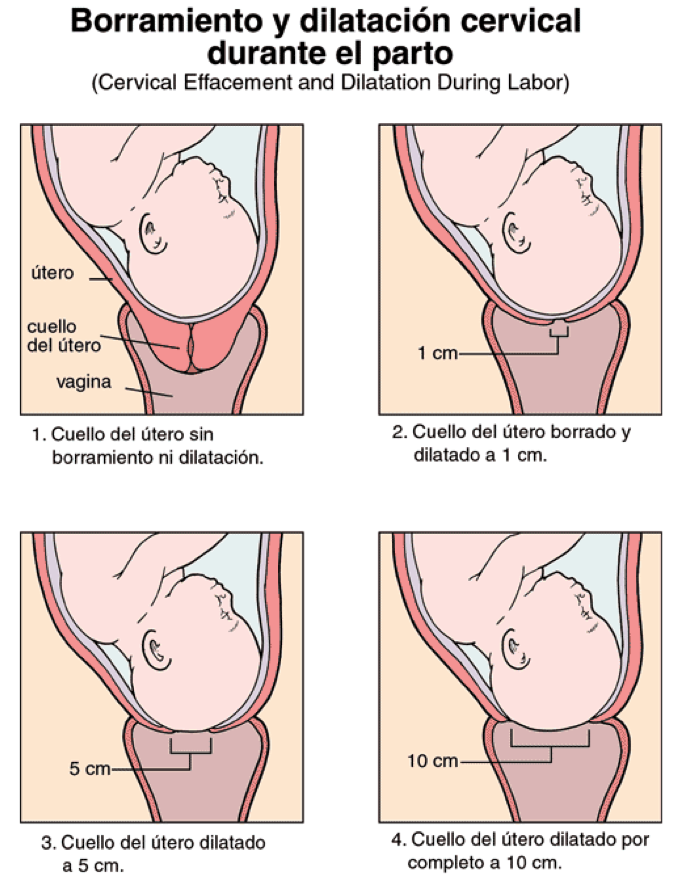
1 Federal State Budgetary Institution “N.N. N.N. Blokhin" of the Ministry of Health of Russia. 115478, Russia, Moscow, Kashirskoe shosse, 24.
2 N.I. Pirogov of the Ministry of Health of Russia. 117997, Russia, Moscow, st. Ostrovityanova, 1.
Contact information: Borovkova Ekaterina Igorevna, e-mail: [email protected]. nine0017 Financial transparency: none of the authors has a financial interest in the presented materials or methods. No conflict of interest . Article received 12/13/2018.
About the authors:
1 Yulia G. Payanidi — MD, PhD, Senior Researcher of the Department of Gynecology, ORCID iD 0000-0001-5950-4543;
2 Ekaterina I. Borovkova — MD, PhD, Professor of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0001-7140-262Х; nine0096 2 Yulia E. Dobrokhotova – MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology, Medical Faculty, ORCID iD 0000-0001-6571-3448;
2 Anna M.