Polycystic ovarian syndrome pregnancy complications
Pregnancy complications in women with polycystic ovary syndrome
Review
. 2015 Sep-Oct;21(5):575-92.
doi: 10.1093/humupd/dmv029. Epub 2015 Jun 27.
Stefano Palomba 1 , Marlieke A de Wilde 2 , Angela Falbo 3 , Maria P H Koster 2 , Giovanni Battista La Sala 4 , Bart C J M Fauser 2
Affiliations
Affiliations
- 1 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy stefanopalomba@tin.
it.
- 2 Department of Reproductive Medicine & Gynecology, University Medical Center Utrecht, Heidelberglaan 100, Utrecht 3584 CX, The Netherlands.
- 3 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy.
- 4 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy University of Modena and Reggio Emilia, Via Università 4, Modena 41100, Italy.
- PMID: 26117684
- DOI: 10.1093/humupd/dmv029
Review
Stefano Palomba et al. Hum Reprod Update. 2015 Sep-Oct.
Hum Reprod Update. 2015 Sep-Oct.
. 2015 Sep-Oct;21(5):575-92.
doi: 10.1093/humupd/dmv029. Epub 2015 Jun 27.
Authors
Stefano Palomba 1 , Marlieke A de Wilde 2 , Angela Falbo 3 , Maria P H Koster 2 , Giovanni Battista La Sala 4 , Bart C J M Fauser 2
Affiliations
- 1 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy stefanopalomba@tin.
 it.
it. - 2 Department of Reproductive Medicine & Gynecology, University Medical Center Utrecht, Heidelberglaan 100, Utrecht 3584 CX, The Netherlands.
- 3 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy.
- 4 Unit of Gynecology & Obstetrics, IRCCS - Arcispedale Santa Maria Nuova, Viale Risorgimento 80, Reggio Emilia 42123, Italy University of Modena and Reggio Emilia, Via Università 4, Modena 41100, Italy.
- PMID: 26117684
- DOI: 10.1093/humupd/dmv029
Abstract
Background: The great majority of studies performed so far concerning women diagnosed with polycystic ovary syndrome (PCOS) have focused on diagnosis, menstrual cycle abnormalities, hirsutism and infertility.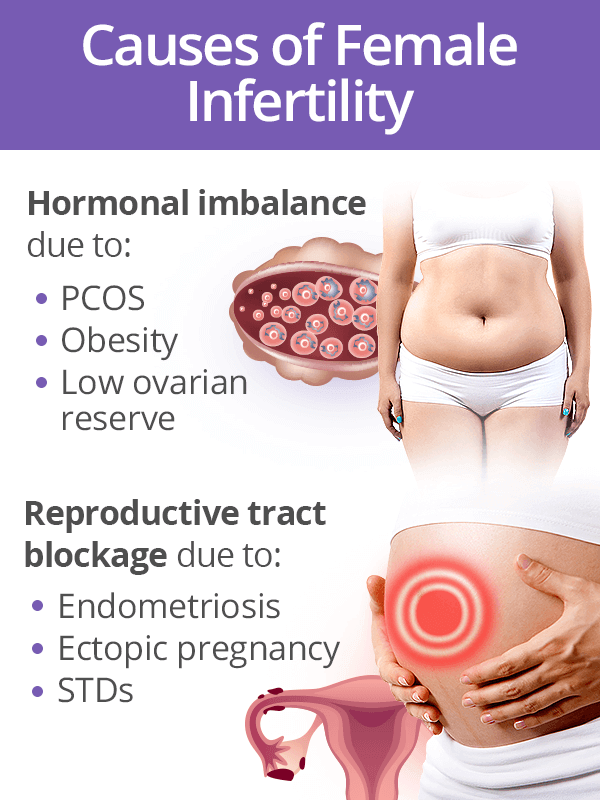 Although progress has been made in developing methods for achieving a pregnancy and reducing multiple gestations in women with PCOS, little attention has been paid to pregnancy complications and subsequent child outcomes. This review aims to summarize current knowledge regarding the clinical and pathophysiological features of pregnancy and children in women with PCOS.
Although progress has been made in developing methods for achieving a pregnancy and reducing multiple gestations in women with PCOS, little attention has been paid to pregnancy complications and subsequent child outcomes. This review aims to summarize current knowledge regarding the clinical and pathophysiological features of pregnancy and children in women with PCOS.
Methods: A literature search up to April 2015 was performed in PubMed, Medline, the Cochrane Library and Web of Science without language restriction. All articles were initially screened for title and abstract and full texts of eligible articles were subsequently selected. Systematic reviews with meta-analysis were initially included for each specific subject. Recent randomised controlled trials (RCTs), which were not included in the systematic reviews, were also included. In addition to evidence from meta-analyses or RCTs, we used non-randomized prospective, uncontrolled prospective, retrospective and experimental studies. When specific data for patients with PCOS were lacking, results from general population studies were reported.
When specific data for patients with PCOS were lacking, results from general population studies were reported.
Results: Women with PCOS exhibit a clinically significant increased risk of pregnancy complications compared with controls. Data which were not adjusted for BMI or other confounders demonstrated in PCOS a 3-4-fold increased risk of pregnancy-induced hypertension and pre-eclampsia, a 3-fold increased risk of gestational diabetes and 2-fold higher chance for premature delivery. Features characteristic of PCOS, such as hyperandrogenism, obesity, insulin resistance and metabolic abnormalities, may contribute to the increased risk of obstetric and neonatal complications. Limited available data suggest that offspring of women with PCOS have an increased risk for future metabolic and reproductive dysfunction. Underlying pathophysiological mechanisms of pregnancy complications along with its association with health of offspring remain uncertain. To date, the strategies for prevention and management of pregnancy complications in women with PCOS, and whether long-term health of these women is influenced, and to what extent, by pregnancy and/or pregnancy complications, remain to be elucidated.
To date, the strategies for prevention and management of pregnancy complications in women with PCOS, and whether long-term health of these women is influenced, and to what extent, by pregnancy and/or pregnancy complications, remain to be elucidated.
Conclusions: Women with PCOS show an increased risk of pregnancy complications. Heterogeneous aetiological factors involved in PCOS and associated co-morbidities may all be involved in compromised pregnancy and child outcomes. In women with PCOS, a possible relationship with genetic, environmental, clinical and biochemical factors involved in this complex condition, as well as with pregnancy complications and long-term health for both mother and child, remains to be established.
Keywords: PCOS; complications; obstetrics; polycystic ovary syndrome; pregnancy.
© The Author 2015.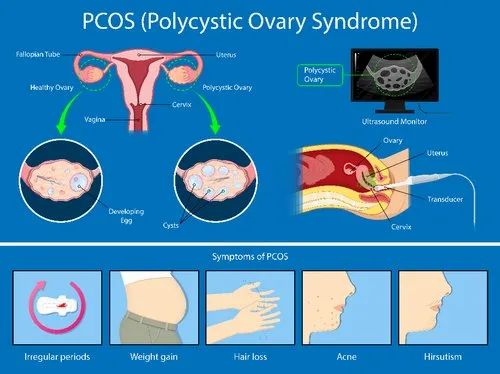 Published by Oxford University Press on behalf of the European Society of Human Reproduction and Embryology. All rights reserved. For Permissions, please email: [email protected].
Published by Oxford University Press on behalf of the European Society of Human Reproduction and Embryology. All rights reserved. For Permissions, please email: [email protected].
Similar articles
-
A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome.
Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS. Boomsma CM, et al. Hum Reprod Update. 2006 Nov-Dec;12(6):673-83. doi: 10.1093/humupd/dml036. Epub 2006 Aug 4. Hum Reprod Update. 2006. PMID: 16891296 Review.
-
Pregnancy outcomes and the effect of metformin treatment in women with polycystic ovary syndrome: an overview.
Ghazeeri GS, Nassar AH, Younes Z, Awwad JT. Ghazeeri GS, et al.
 Acta Obstet Gynecol Scand. 2012 Jun;91(6):658-78. doi: 10.1111/j.1600-0412.2012.01385.x. Epub 2012 May 1. Acta Obstet Gynecol Scand. 2012. PMID: 22375613 Review.
Acta Obstet Gynecol Scand. 2012 Jun;91(6):658-78. doi: 10.1111/j.1600-0412.2012.01385.x. Epub 2012 May 1. Acta Obstet Gynecol Scand. 2012. PMID: 22375613 Review. -
Irregular menstruation and hyperandrogenaemia in adolescence are associated with polycystic ovary syndrome and infertility in later life: Northern Finland Birth Cohort 1986 study.
West S, Lashen H, Bloigu A, Franks S, Puukka K, Ruokonen A, Järvelin MR, Tapanainen JS, Morin-Papunen L. West S, et al. Hum Reprod. 2014 Oct 10;29(10):2339-51. doi: 10.1093/humrep/deu200. Epub 2014 Aug 1. Hum Reprod. 2014. PMID: 25085801 Free PMC article.
-
Pregnancy complications in infertile patients with polycystic ovary syndrome: updated evidence.
Palomba S, Falbo A, Daolio J, Battaglia FA, La Sala GB.
 Palomba S, et al. Minerva Ginecol. 2018 Dec;70(6):754-760. doi: 10.23736/S0026-4784.18.04230-2. Epub 2018 Apr 11. Minerva Ginecol. 2018. PMID: 29644330 Review.
Palomba S, et al. Minerva Ginecol. 2018 Dec;70(6):754-760. doi: 10.23736/S0026-4784.18.04230-2. Epub 2018 Apr 11. Minerva Ginecol. 2018. PMID: 29644330 Review. -
[Effect of hyperandrogenism on obstetric complications of singleton pregnancy from in vitro fertilization in women with polycystic ovary syndrome].
Wei DM, Zhang ZZ, Wang Z, Li P, Wang JF, Liu YJ, Zhang JT, Shi YH. Wei DM, et al. Zhonghua Fu Chan Ke Za Zhi. 2018 Jan 25;53(1):18-22. doi: 10.3760/cma.j.issn.0529-567X.2018.01.005. Zhonghua Fu Chan Ke Za Zhi. 2018. PMID: 29374881 Clinical Trial. Chinese.
See all similar articles
Cited by
-
Association of ADAMTS proteoglycanases downregulation with IVF-ET outcomes in patients with polycystic ovary syndrome: a systematic review and meta-analysis.

Shi Y, Shi Y, He G, Wang G, Liu H, Shao X. Shi Y, et al. Reprod Biol Endocrinol. 2022 Dec 13;20(1):169. doi: 10.1186/s12958-022-01035-9. Reprod Biol Endocrinol. 2022. PMID: 36510316 Free PMC article.
-
Effect of different timing of letrozole initiation on pregnancy outcome in polycystic ovary syndrome.
Shi L, Ye S, Gao M, Chen Y, Jin X, Zhang Z. Shi L, et al. Front Endocrinol (Lausanne). 2022 Nov 24;13:1059609. doi: 10.3389/fendo.2022.1059609. eCollection 2022. Front Endocrinol (Lausanne). 2022. PMID: 36506073 Free PMC article.
-
Decoding the molecular cascade of embryonic-uterine modulators in pregnancy loss of PCOS mother- an "in vivo" study.
Dhadhal S, Nampoothiri L. Dhadhal S, et al.
 Reprod Biol Endocrinol. 2022 Dec 7;20(1):165. doi: 10.1186/s12958-022-01041-x. Reprod Biol Endocrinol. 2022. PMID: 36476384 Free PMC article.
Reprod Biol Endocrinol. 2022 Dec 7;20(1):165. doi: 10.1186/s12958-022-01041-x. Reprod Biol Endocrinol. 2022. PMID: 36476384 Free PMC article. -
Role of EGFR expressed on the granulosa cells in the pathogenesis of polycystic ovarian syndrome.
Zhang JH, Zhan L, Zhao MY, Wang JJ, Xie FF, Xu ZY, Xu Q, Cao YX, Liu QW. Zhang JH, et al. Front Endocrinol (Lausanne). 2022 Nov 11;13:971564. doi: 10.3389/fendo.2022.971564. eCollection 2022. Front Endocrinol (Lausanne). 2022. PMID: 36440230 Free PMC article.
-
Polycystic Ovarian Syndrome (PCOS): Does the Challenge End at Conception?
Mirza FG, Tahlak MA, Rjeili RB, Hazari K, Ennab F, Hodgman C, Khamis AH, Atiomo W. Mirza FG, et al. Int J Environ Res Public Health.
 2022 Nov 12;19(22):14914. doi: 10.3390/ijerph292214914. Int J Environ Res Public Health. 2022. PMID: 36429632 Free PMC article. Review.
2022 Nov 12;19(22):14914. doi: 10.3390/ijerph292214914. Int J Environ Res Public Health. 2022. PMID: 36429632 Free PMC article. Review.
See all "Cited by" articles
Publication types
MeSH terms
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments
Polycystic ovarian syndrome (PCOS) and pregnancy – symptoms and treatments | Pregnancy Birth and Baby beginning of content7-minute read
Listen
What is PCOS?
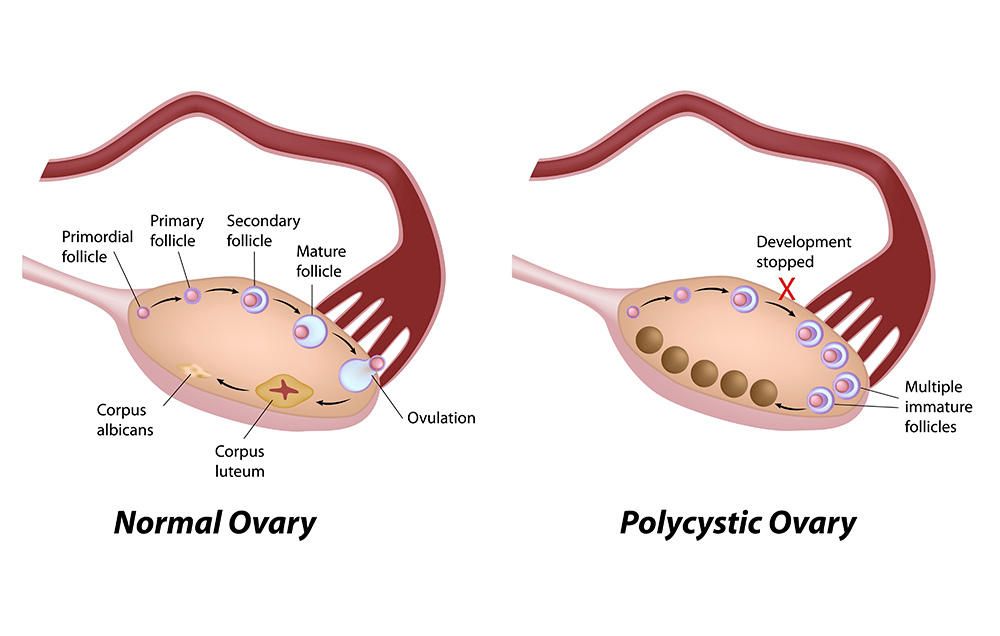
Polycystic ovarian syndrome, or PCOS, is a common condition.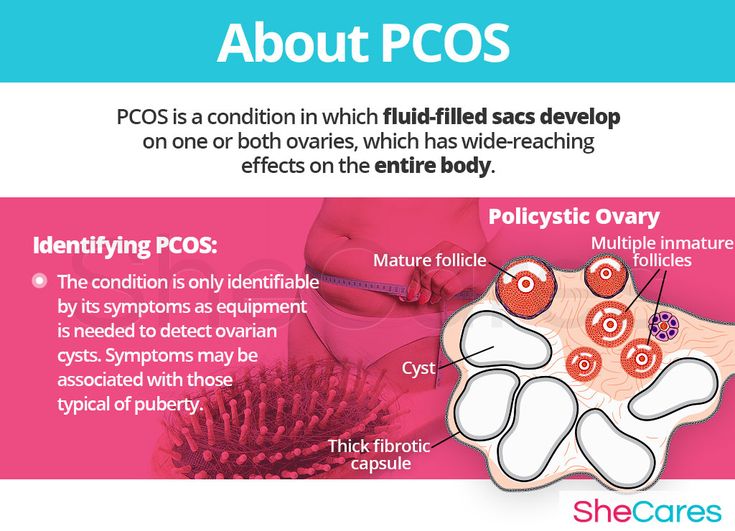
People with PCOS can have:
- higher than normal levels of androgens (male-type hormones)
- problems with ovulation (the release of eggs from the ovaries)
- multiple cysts on the ovaries
This can affect your menstrual cycle, fertility and appearance.
If you have PCOS you may struggle to become pregnant and may be at higher risk of developing some pregnancy complications.
Illustration showing a normal ovary and a polycystic ovary.What are the symptoms of PCOS?
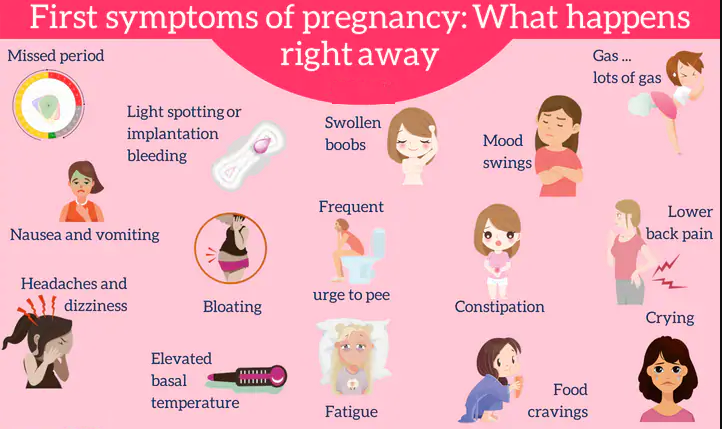
There are many signs and symptoms that are associated with PCOS. These can include:
- irregular menstrual periods
- cysts on the ovaries
- infertility
- weight gain
- acne
- depression
- excessive face and body hair
- thinning or balding head hair
- insulin resistance (where your cells don't respond to insulin and your blood sugar levels rise)
Some of these symptoms (such as acne, excess face and body hair, and scalp hair loss) are due to increased levels of the hormones called androgens.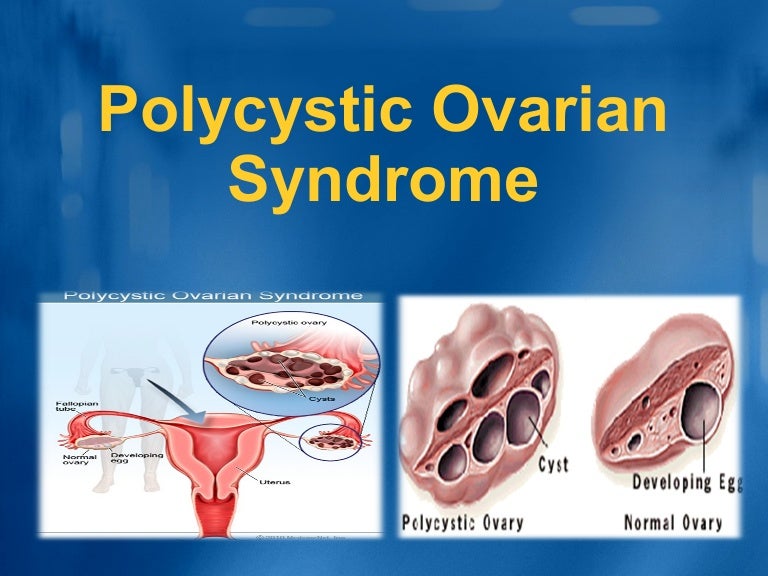 These hormones are found in all females, but those with PCOS have slightly higher amounts.
These hormones are found in all females, but those with PCOS have slightly higher amounts.
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
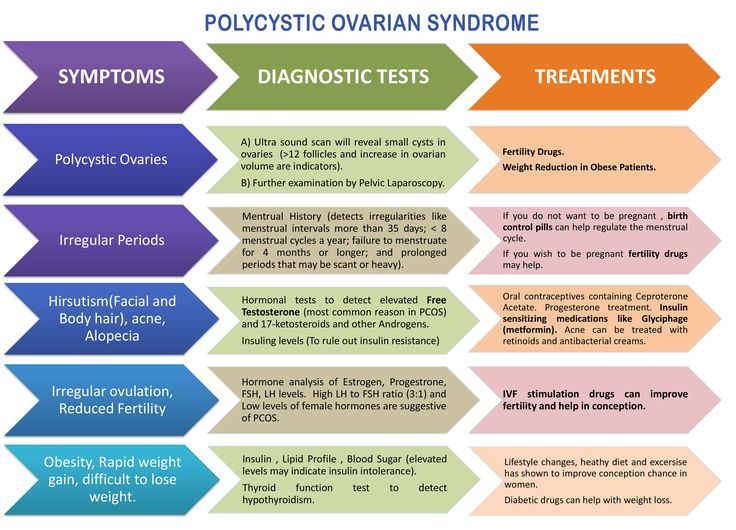
How is PCOS diagnosed?
It often takes a while to get a PCOS diagnosis. This is because the condition can mimic other problems. Sometimes, people only find out that they have PCOS when they have tests to find out why they are having trouble getting pregnant.
If you think you might have PCOS, see your doctor. Early diagnosis means that your symptoms can be treated early.
At your appointment, your doctor will:
- ask about your symptoms
- ask for your medical history
- examine you
Your doctor may also recommend blood tests and an ultrasound scan to look for any cysts in the ovaries.
In general, to be diagnosed with PCOS, you need to have 2 out of 3 of the following;
- irregular periods, or no periods
- symptoms due to increased levels of androgen hormones, or a blood test showing you have increased levels of androgen hormones
- an ultrasound scan showing multiple cysts on your ovary or ovaries
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.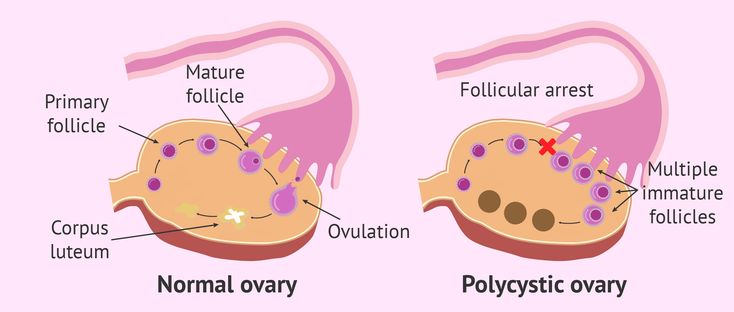
Will PCOS affect my fertility?
If you have PCOS, you might struggle to get pregnant.
Fortunately, with lifestyle changes or infertility treatment, most people with PCOS can become pregnant. Talk to your doctor or fertility specialist for individual advice for your situation.
Can PCOS increase my risk of complications during pregnancy?
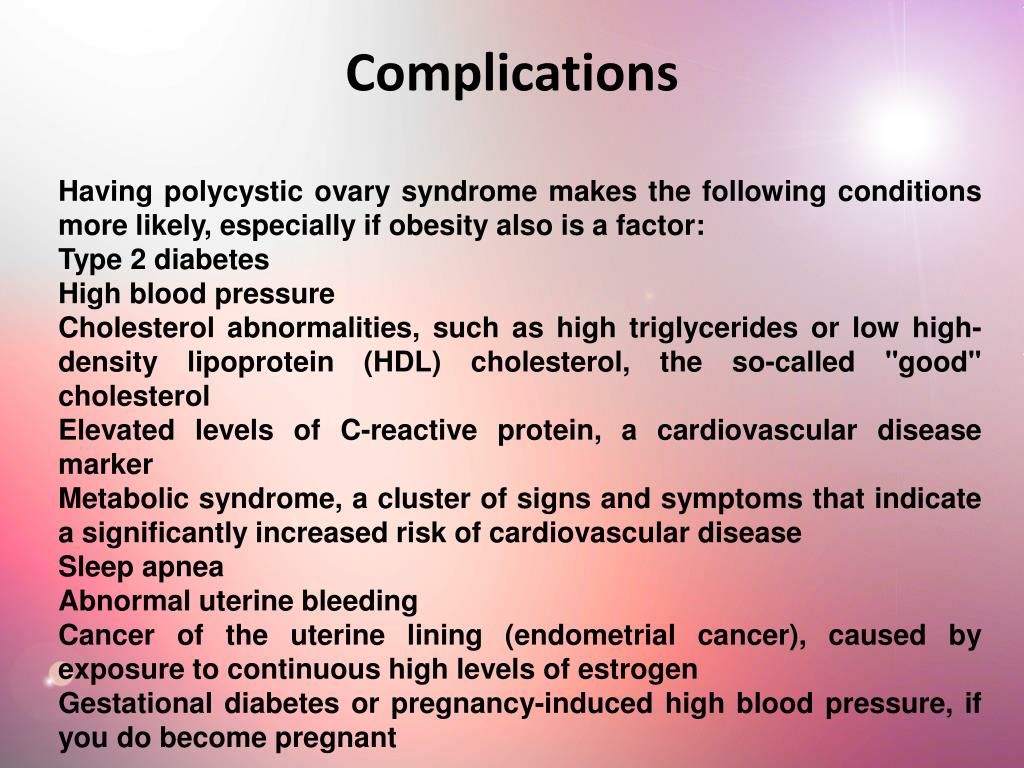
Having PCOS can increase your risk of some complications during pregnancy, such as:
- high blood pressure
- gestational diabetes
- premature birth
If you have PCOS, you are also at increased risk of having a baby larger than expected for their gestational age. This comes with a higher risk of needing a caesarean delivery.
Babies born to people with PCOS have a higher chance of being admitted to a newborn intensive care unit.
Pregnant women with PCOS may have a higher risk of miscarriage and stillbirth. However, more research is needed in this area.
If you have PCOS and are pregnant, it is important you talk with your doctor.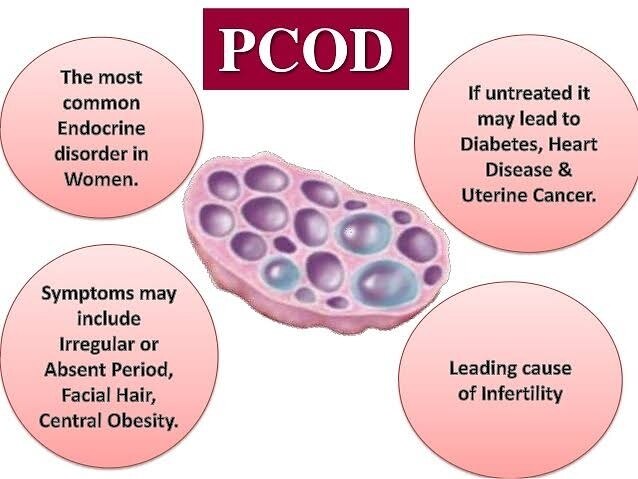 The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
The risk of these complications can be reduced by monitoring your PCOS symptoms and taking extra care during your pregnancy.
What steps can I take to look after my health?
You can make lifestyle changes to manage your PCOS and look after your health. These include:
- maintaining a healthy weight
- eating healthily
- exercising
- managing stress
- getting enough sleep
These lifestyle changes can reduce the symptoms of PCOS and improve your chance of falling pregnant.
If you are overweight, a 5% to 10% loss in weight can increase your fertility.
Speak to your doctor for guidance on how to make effective lifestyle changes.
How is PCOS treated?
Treatment for PCOS depends on each person. Speak to your doctor about the best treatment for you.
If you are trying to fall pregnant, your PCOS treatment will focus on:
- restoring regular ovulation
- weight loss
- improving your general health and wellbeing
If you have made lifestyle changes and are still struggling to fall pregnant, your doctor may order fertility tests.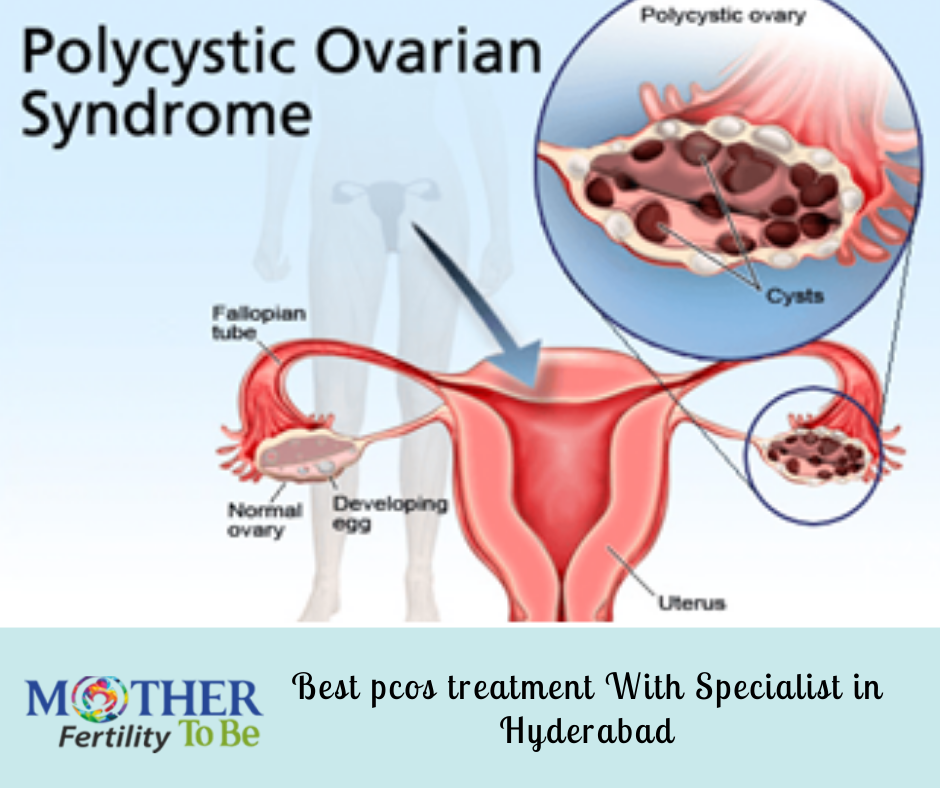 They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
They may also prescribe fertility medicines to help you ovulate. In some cases, they may recommend surgery.
Another possibility is in vitro fertilisation (IVF), which offers the best chance of conception. However, this can be expensive and is usually only considered when all other options have been unsuccessful.
If you are not trying to fall pregnant, your PCOS treatment will focus on:
- reducing your symptoms
- reducing your risk of long-term health issues, including heart disease and type 2 diabetes
Speak to your doctor. They can help you manage your PCOS symptoms by providing:
- weight loss management strategies
- treatment for sleeping problems
- acne treatment
- medicines, including hormonal contraception (birth control) to manage irregular menstruation
Dealing with infertility and PCOS symptoms can be difficult. You may experience feelings of depression and anxiety. Your doctor can refer you to a counsellor or psychologist for your mental health.
Resources and support
Visit the Jean Hailes website for more information on PCOS and its complications.
Hormones Australia also supplies information on PCOS, including questions to ask your doctor.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Australian Family Physician (Polycystic ovary system), Jean Hailes (PCOS), Royal Australian College of General Practitioners (Polycystic ovary system - clinical guidelines), The Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Long-term consequences of PCOS - statement)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Need more information?
Polycystic Ovary Syndrome (PCOS) | Your Fertility
PCOS can be associated with a range of symptoms including irregular periods and difficulties getting pregnant
Read more on Your Fertility website
Fact sheets | Your Fertility
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years
Read more on Your Fertility website
What is PCOS?
Polycystic ovary syndrome (PCOS) is the most common hormonal condition affecting women in their reproductive years.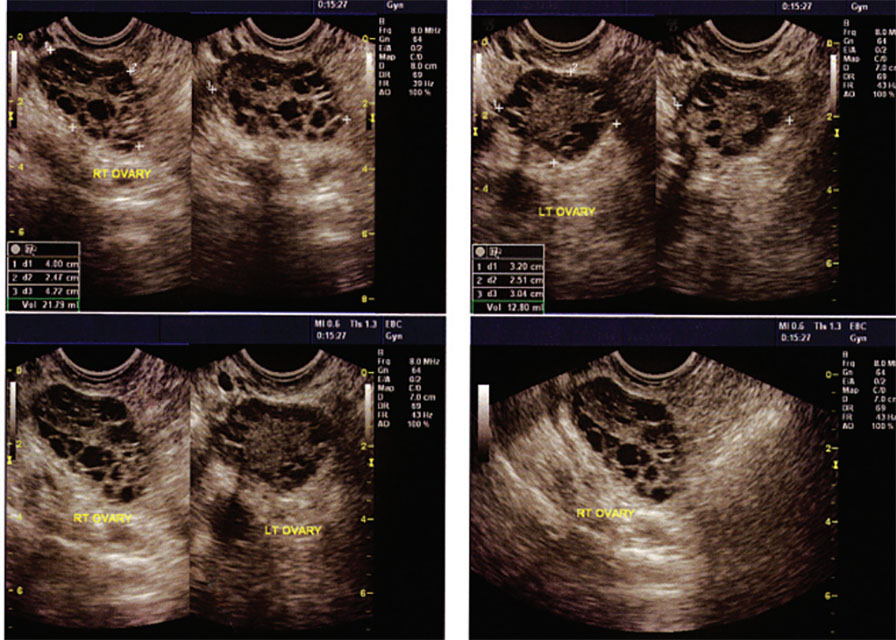
Read more on Your Fertility website
Polycystic ovarian syndrome (PCOS) - Better Health Channel
Polycystic ovarian syndrome is a hormonal condition associated with irregular menstrual cycles, excess hair growth, acne, reduced fertility, and increased risk of diabetes and mood changes.
Read more on Better Health Channel website
Polycystic ovary syndrome (PCOS) | Dietitians Australia
PCOS is a common hormonal condition of the ovaries that can cause problems such as an irregular menstrual cycle, weight gain, impaired fertility and poor mental health. Diet and lifestyle changes are the first steps to manage PCOS, and an Accredited Practising Dietitian specialising in PCOS is the most qualified professional to help.
Read more on Dietitians Australia website
Fertility explained | VARTA
Fertility is the ability to conceive a child. Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins.
Most of us take our fertility for granted but the process of reproduction is complex, so some people may experience difficulties when trying for a baby. There are a range of factors that can affect fertility. Taking care of your preconception health by modifying your lifestyle can improve your chance of a pregnancy and the health of your future child. Medical conditions such as polycystic ovary syndrome (PCOS) and endometriosis can reduce fertility, however it may just take longer to get pregnant. In some cases, medical procedures can be used to preserve fertility. Fertility preservation (freezing of gametes for later use) is used by people who are not ready to have a baby during their most fertile years or for those facing medical treatment that might impair their fertility. Understanding reproduction It is useful to understand how eggs and sperm are normally formed, and how conception occurs to understand the causes of infertility and how they are targeted in fertility treatment. The hormones which control the production of sperm and eggs are called gonadotrophins.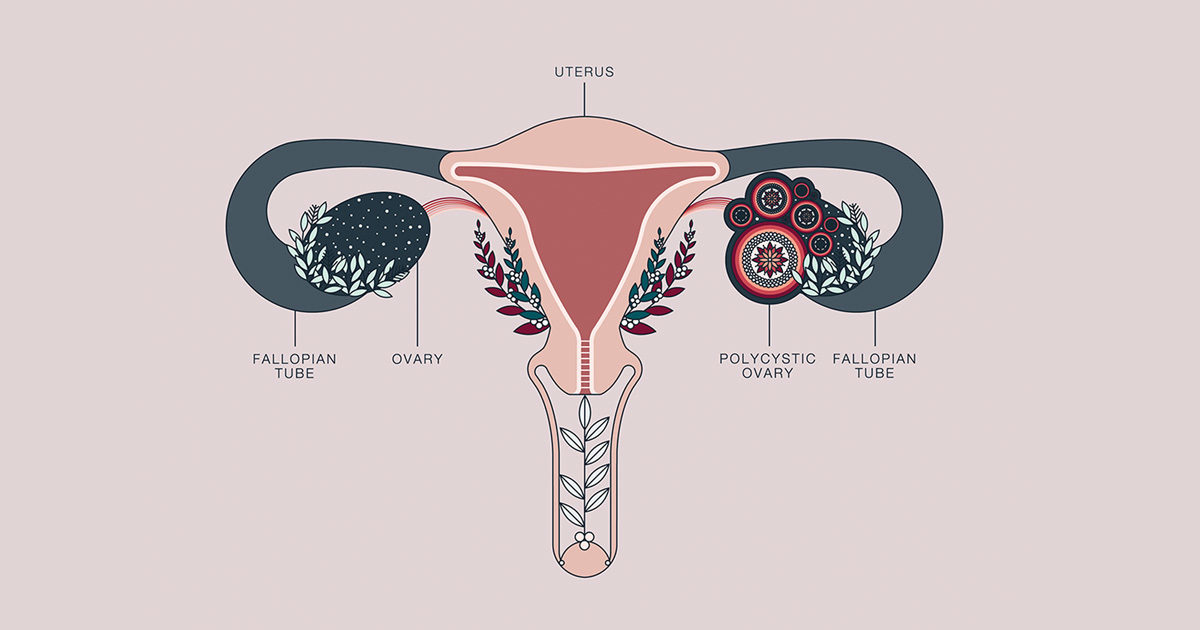 There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised.
There are two types of gonadotrophins: follicle-stimulating hormone (FSH) and luteinising hormone (LH). In men, they stimulate the testicles to produce sperm and testosterone. In women, they act on the ovaries where the eggs develop. The female sex hormones, oestrogen and progesterone, are produced by the ovaries when eggs mature and are released (ovulation). For women, the production of sex hormones and the release of an egg is known as the menstrual cycle. It is counted from the first day of the period until the day before the start of the next period. In an average cycle of 28 days, ovulation happens on day 14. However, cycle length varies between women, and it is important to note that ovulation occurs earlier in women with shorter cycles and later in women with longer cycles. Sperm are produced at the rate of about 300 million per day. They take some 80 days to mature. Each sperm has a head, which contains the genetic material, and a tail, which propels it up through the vagina, uterus, and fallopian tubes where the egg is fertilised. Conception occurs when an egg and a sperm come together. At ovulation, an egg is released from the ovary into the fallopian tube. If sperm is present at that time, the egg can be fertilised. The fertilised egg then starts to divide and becomes an embryo. After ovulation, the ovary produces progesterone which prepares the lining of the uterus - the endometrium - for the growing embryo. A few days after implantation, the embryo starts to produce human chorionic gonadotrophins (HCG) - the hormone that gives a positive pregnancy test reading. If an embryo does not form or attach to the endometrium (implantation), the level of progesterone drops and the next period starts.
Conception occurs when an egg and a sperm come together. At ovulation, an egg is released from the ovary into the fallopian tube. If sperm is present at that time, the egg can be fertilised. The fertilised egg then starts to divide and becomes an embryo. After ovulation, the ovary produces progesterone which prepares the lining of the uterus - the endometrium - for the growing embryo. A few days after implantation, the embryo starts to produce human chorionic gonadotrophins (HCG) - the hormone that gives a positive pregnancy test reading. If an embryo does not form or attach to the endometrium (implantation), the level of progesterone drops and the next period starts.
Read more on Victorian Assisted Reproductive Treatment Authority website
Good fertility health
Your age and your health can affect your chances of falling pregnant. Maintaining a healthy lifestyle may help you improve your fertility.
Read more on Pregnancy, Birth & Baby website
All about Polycystic Ovary Syndrome (PCOS) | Jean Hailes
Read about causes, signs and symptoms of PCOS, as well as diagnosis and treatments available to help. Jean Hailes is Australia's leader in women's health.
Read more on Jean Hailes for Women's Health website
Ovulation and fertility - Better Health Channel
The female body shows several signs of ovulation and you may experience some or all of these signs.
Read more on Better Health Channel website
The Pink Elephants Support Network - Female Fertility Issues - Pink Elephants
The Pink Elephants Support Network are a not for profit charity, formed to support women through miscarriage, pregnancy loss and beyond.
Read more on Pink Elephants Support Network website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.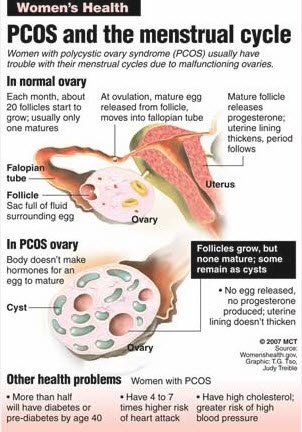
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.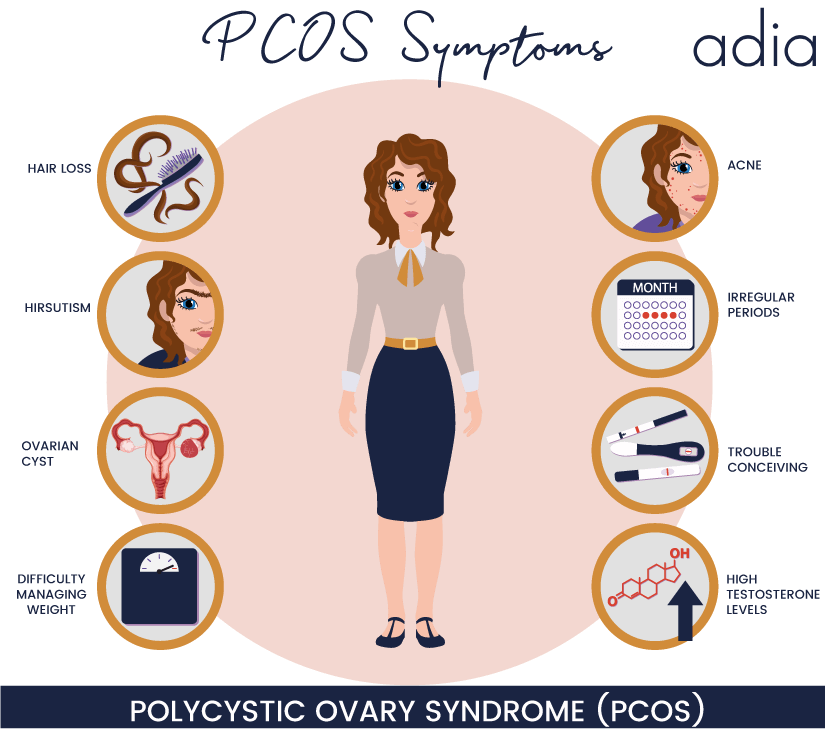
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
How to get pregnant with polycystic ovaries?
Polycystic disease is a common hormonal disease that affects the functioning of a woman's ovaries. The dangers of PCOS include irregular menstrual periods, excessive hair growth, acne, weight gain, and other problems. Left untreated, PCOS can even lead to infertility. In this article, we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".
In this article, we will tell you more about causes of polycystic , polycystic ovaries and pregnancy , and also give an answer to the question: “ Is it possible to give birth with polycystic ovaries? ".
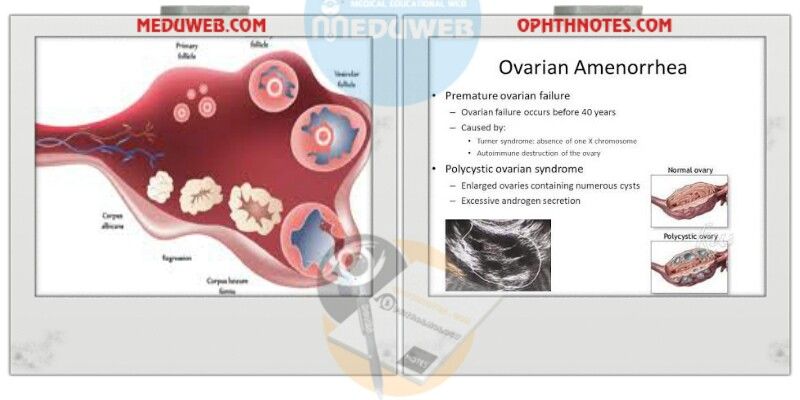
What is polycystic ovary syndrome?
Polycystic ovary syndrome (PCOS) is a hormonal disorder common among women of reproductive age. Women with PCOS may have menstrual irregularities and elevated levels of male hormones (androgens). Numerous small collections of fluid (follicles) may form in the ovaries, and an egg may not be released regularly. This condition should not be confused with multifollicular ovaries, because with multifollicular ovaries, ovulation and a normal menstrual cycle can persist, unlike polycystic disease. nine0019
50-75% of cases of endocrine infertility. 20-22% of marital infertility. It is detected in 5-16% of women of reproductive age. These are the figures for the diagnosis of "Polycystic Ovary".
Symptoms of polycystic ovary syndrome
Polycystic ovary syndrome is accompanied by characteristic symptoms, upon noticing which it is necessary to seek advice from an endocrinologist or gynecologist. For some women, symptoms begin around the time of their first menstrual period. Others discover symptoms of PCOS only after they have gained a lot of weight or have problems getting pregnant. In some cases, PCOS may be asymptomatic. nine0019
The most common symptoms of PCOS:
- Irregular periods. Lack of ovulation prevents the lining of the uterus from falling off every month. Some women with PCOS have fewer than eight periods a year, or none at all.
- Severe bleeding. The lining of the uterus builds up over a longer period of time, so menstruation may be heavier than usual.
- Hair growth . More than 70 percent of women with this condition grow hair on their face and body, including on their back, abdomen, and chest.
 Excess hair growth is called hirsutism.
Excess hair growth is called hirsutism. - Acne . Male hormones can make the skin more oily than normal and cause breakouts on areas such as the face, chest, and upper back.
- Weight gain. Up to 80 percent of women with PCOS are overweight or obese.
- Male pattern baldness. nine0039 The hair on the scalp becomes thinner and may fall out.
- Darkening of the skin. Dark patches of skin may develop in body folds, such as the neck, groin area, and under the breasts.
- Headaches. Hormonal changes may cause headaches in some women.
Irregular periods
Infrequent, irregular periods, long or no periods are the most common symptom of PCOS. For example, with PCOS, you may have fewer than nine periods a year, more than 35 days between periods, and abnormally heavy periods. nine0019
Hyperandrogenism
Hyperandrogenism is a disease characterized by high levels of androgens. It is more common in women than in men. Symptoms of hyperandrogenism may include acne, seborrhea (inflammation of the skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent periods.
It is more common in women than in men. Symptoms of hyperandrogenism may include acne, seborrhea (inflammation of the skin), hair loss on the scalp, increased body or facial hair, and infrequent or absent periods.
Hyperandrogenism is a defining feature of women and young girls with PCOS. Polycystic disease causes a malfunction of the ovaries or adrenal glands, which leads to the production of excess androgens (male sex hormones). nine0019
Anovulation
Anovulation occurs when an egg is not released from the ovary during the menstrual cycle. The egg is essential for pregnancy. Since several hormones are involved in ovulation, there are many causes of anovulation, one of which is PCOS. Chronic anovulation is a common cause of infertility.
Diagnosis
There is no test to definitively diagnose polycystic ovary syndrome (PCOS). The doctor will likely begin by discussing your medical history, including menstrual periods and weight changes. A physical exam will include checking for signs of excessive hair growth, acne, and weight gain. nine0019
nine0019
Your doctor may recommend:
- Gynecological examination. A physician visually and manually examines the reproductive organs for growths or other abnormalities.
- Blood tests. A blood test is given to determine the level of hormones. This will help rule out possible causes of menstrual irregularities or excess androgens that mimic PCOS. An additional blood test may also be needed to measure insulin resistance as well as fasting cholesterol and triglyceride levels. nine0041
- Ultrasound examination (ultrasound). The doctor will check the appearance of the ovaries and the thickness of the lining of the uterus. A rod-shaped device (sensor) (transvaginal ultrasound) is inserted into the vagina, which emits sound waves and converts them into images on a computer screen.
Is it possible to get pregnant with PCOS
How to get pregnant with PCOS? Getting pregnant with PCOS can be difficult, but that doesn't mean it's impossible.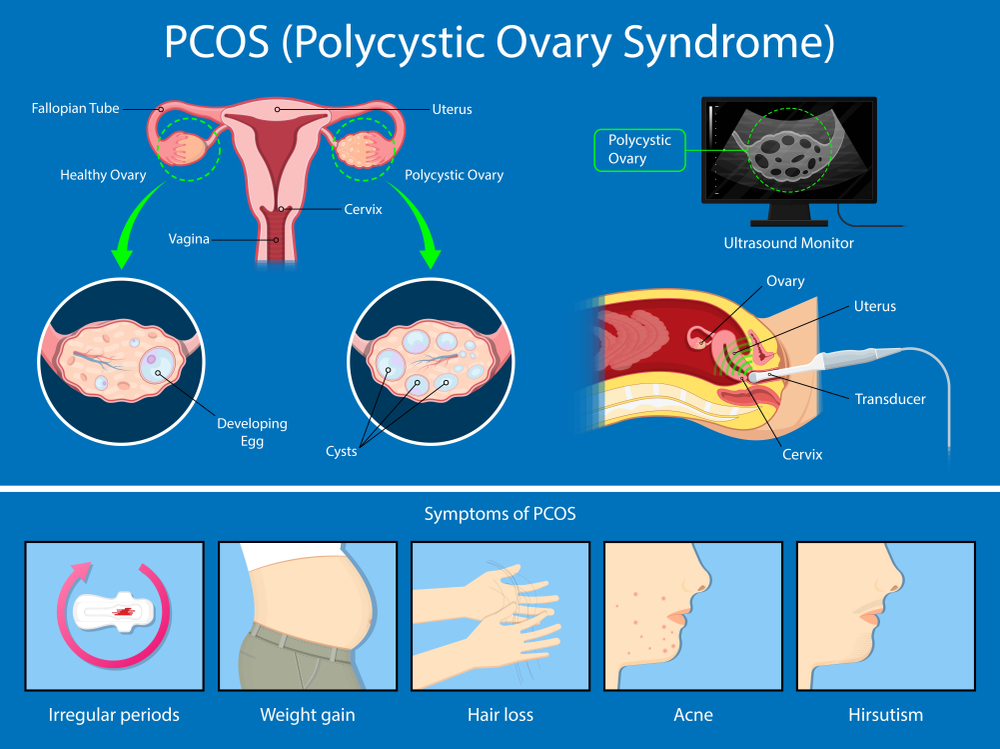 While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy. nine0019
While PCOS can affect your hormones and therefore your fertility, there are medical treatments and lifestyle changes you can make to improve your chances of pregnancy. nine0019
Is it possible to get pregnant with polycystic ovaries? To get pregnant, you must ovulate, which PCOS most often prevents. Women who do not ovulate regularly with PCOS do not release enough eggs for fertilization. Pregnancy with PCOS is further complicated by the fact that PCOS causes a hormonal imbalance that changes the quality of cervical fluid, making it difficult for sperm to survive.
It is impossible to say categorically that PCOS is infertility, but PCOS is one of the main causes of infertility in women. nine0019
Is it possible to get pregnant with PCOS? And although there are no exact statistics on the chances of pregnancy, 70 to 80 percent of women with PCOS have fertility problems. PCOS disrupts the normal menstrual cycle and makes it difficult to conceive.
Is it possible to get pregnant with PCOS? Polycystic ovary syndrome is not a sentence and it is possible to get pregnant, albeit problematic. However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
However, if PCOS is left untreated, the chances of getting pregnant decrease with age.
It is possible to get pregnant with polycystic disease, but most often pregnancy with polycystic disease is difficult. This condition can increase the risk of pregnancy complications. Women with PCOS are twice as likely to have a preterm birth than women without. They are also at greater risk of miscarriage, high blood pressure, and gestational diabetes. However, by managing the symptoms, many women with PCOS can become pregnant and have a healthy baby.
How to get pregnant with PCOS? Women with PCOS can become pregnant using fertility treatments that improve ovulation. Losing weight and lowering your blood sugar can increase your chances of a healthy pregnancy. nine0019
Pregnancy planning for PCOS
How to get pregnant with PCOS? While your chances of getting pregnant with PCOS may be lower, there are a few things you can do to increase those chances.
- Call your doctor.
 How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle. nine0039
How to get pregnant with polycystic ovaries? Normalization of hormones and menstruation is the first step. Your doctor may prescribe medications to help your body deal with insulin better and regulate your menstrual cycle. nine0039 - Maintain a healthy weight. Is it possible to get pregnant with PCOS? Weight loss can lower insulin levels, androgen levels, and restore ovulation. Ask your doctor about a weight management program and meet with a nutritionist regularly for help with your weight loss goals.
- Eat right. Polycystic Ovarian Diet includes sugary foods, simple carbohydrates and unhealthy fats. Add to your menu: fresh and cooked fruits and vegetables, whole grains such as brown rice, oats and barley, beans and lentils, chicken, fish. nine0041
- Be active. Exercise helps lower blood sugar levels. How to get pregnant with insulin resistance? If you have PCOS, increasing daily activity such as walking, exercising, walking can help treat or even prevent insulin resistance, control your weight, and avoid developing diabetes.

- Lead a healthy lifestyle. Follow a healthy lifestyle with PCOS, give up bad habits, unhealthy diet, lack of sports and irregular sleep. nine0041
Treatment for PCOS
Treatment for PCOS focuses on your individual problems such as infertility, acne or obesity. Also, the direction of PCOS treatment largely depends on whether a woman is planning a pregnancy or not. Specific treatment may include lifestyle changes or medications.
How to treat PCOS?
Lifestyle changes
Your doctor may recommend weight loss through a low-calorie diet combined with moderate exercise. Even small weight loss - like losing 5 percent of your body weight - can improve your condition. Can you get pregnant with PCOS? Losing weight can also increase the effectiveness of medications your doctor recommends to treat PCOS and help with infertility. nine0019
Treatment with drugs for polycystic ovaries
To regulate the menstrual cycle, the doctor may recommend:
Combination birth control pills.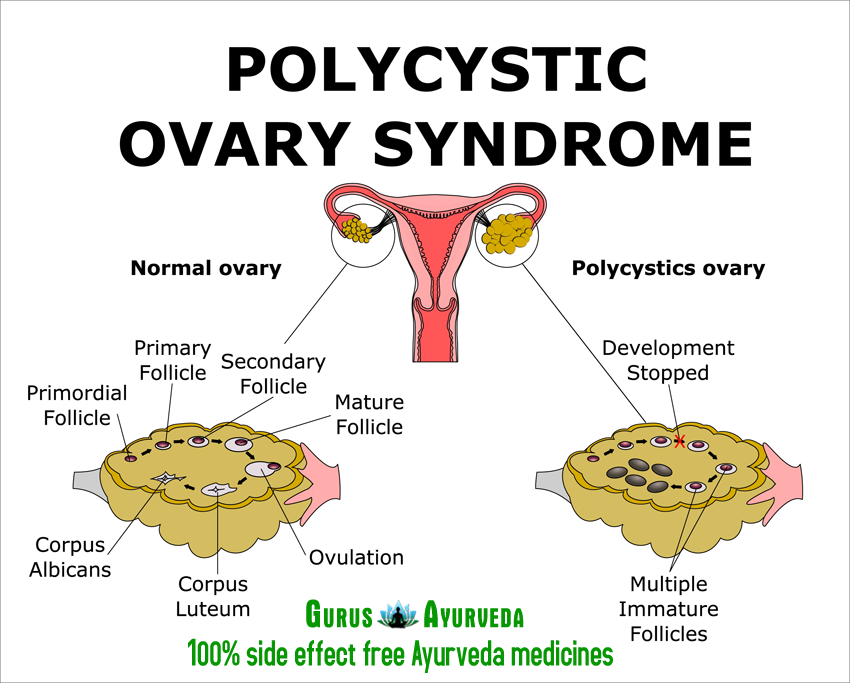 Estrogen and progestin tablets reduce androgen production and regulate estrogen. Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin. nine0019
Estrogen and progestin tablets reduce androgen production and regulate estrogen. Hormone regulation can reduce the risk of endometrial cancer and correct abnormal bleeding, excess hair growth, and acne. Instead of pills, you can use a skin patch or vaginal ring containing a combination of estrogen and progestin. nine0019
Progestin therapy. Daily progestin may: restore normal hormonal balance, regulate ovulation, stop excessive hair growth, protect against endometrial cancer, and help get pregnant with sleep deprivation.
How to induce ovulation in PCOS? To help induce ovulation in PCOS, your doctor may recommend:
Clomiphene is a fertility medication that can help women with PCOS get pregnant.
Metformin is a drug used to treat type 2 diabetes. It also treats PCOS by increasing insulin levels.
Operation
How to get pregnant with PCOS? Surgery may be an option to improve fertility if other treatments don't work. Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS. nine0019
Ovarian drilling is a procedure in which tiny holes are made in the ovary using a laser or a thin, heated needle to restore normal ovulation and the possibility of pregnancy with PCOS. nine0019
Important! To determine the right treatment and choose the right drug, you need to consult a doctor!
Help Doc.ua: you can make an appointment with a gynecologist-endocrinologist on the website.
Polycystic ovary syndrome and pregnancy academician V.I. Kulakova
Ministry of Health of Russia, Moscow
Purpose of the study. To conduct a systematic analysis of the data presented in the current literature on obstetric complications in women with polycystic ovary syndrome (PCOS). nine0200 Material and methods. The review includes data from foreign and domestic studies published in the electronic databases Medline, PubMed, Cochrane Library over the past 10 years.
Results. The present review considers data on such complications of pregnancy in PCOS as miscarriage, multiple pregnancy, gestational hypertension and preeclampsia, gestational diabetes mellitus, the birth of small-to-term babies with macrosomia, as well as some pathophysiological processes that may underlie complications. nine0200 Conclusion. The hyperandrogyny, insulin resistance, obesity, and dyslipidemia characteristic of PCOS are likely to be critical factors in the processes of trophoblast invasion and placentation, and may also affect the health of the mother and child. Preconception counseling for women with PCOS and careful monitoring during pregnancy is recommended to prevent adverse pregnancy outcomes.
nine0200 Conclusion. The hyperandrogyny, insulin resistance, obesity, and dyslipidemia characteristic of PCOS are likely to be critical factors in the processes of trophoblast invasion and placentation, and may also affect the health of the mother and child. Preconception counseling for women with PCOS and careful monitoring during pregnancy is recommended to prevent adverse pregnancy outcomes.
Polycystic ovary syndrome (PCOS) is considered one of the most common endocrine disorders in women. Its frequency of occurrence depends both on diagnostic criteria and on the racial and ethnic characteristics of the population, varying from 6 to 21% [1]. Diagnostic criteria for PCOS are hyperandrogenism, ovarian dysfunction and their polycystic morphological structure. Despite the fact that 50% of patients with PCOS are overweight or obese and 30–70% have insulin resistance, these signs of the metabolic syndrome are not considered diagnostic criteria for PCOS [2]. The association of PCOS with impaired reproductive function is well known, but PCOS is also associated with other metabolic disorders that can have a negative impact on women's reproductive health and quality of life [3].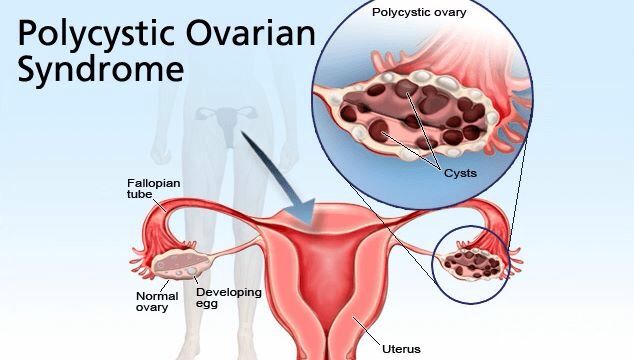 Hyperandrogenism, hyperinsulinemia and obesity have a pronounced effect on the course of pregnancy in patients with PCOS. nine0019
Hyperandrogenism, hyperinsulinemia and obesity have a pronounced effect on the course of pregnancy in patients with PCOS. nine0019
PCOS-associated obstetric complications include miscarriage, gestational diabetes, gestational hypertension, weight gain or loss in newborns, and increased perinatal mortality and operative delivery rates [4, 5]. The presence of these associations was mainly confirmed by the results of three large meta-analyses [6–8]. They can be considered the basis of modern ideas about the impact of PCOS on pregnancy. However, the results of these meta-analyses were obtained by synthesizing data from retrospective and prospective studies, often characterized by small sample sizes, lack of consideration for likely confounders, such as body mass index (BMI). nine0019
Significantly, the heterogeneity of PCOS itself and the small number of large randomized controlled trials (RCTs) studying the course of pregnancy in this pathology limit the understanding of causal relationships between PCOS and pregnancy complications.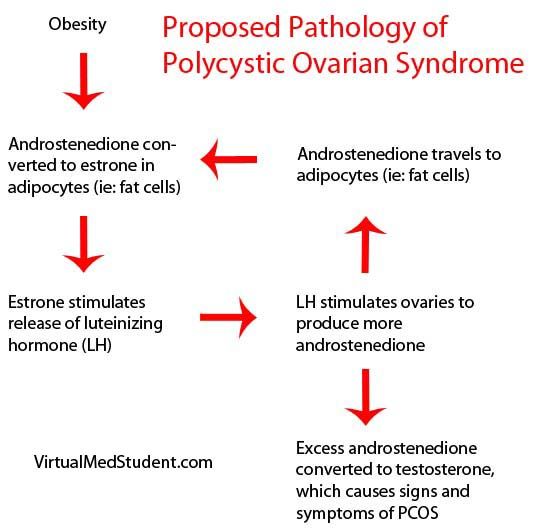 Currently, the only consensus document has been adopted indicating an increased risk of complications in pregnant women with PCOS. It mentions obesity and/or insulin resistance as possible factors for worsening prognosis [9].
Currently, the only consensus document has been adopted indicating an increased risk of complications in pregnant women with PCOS. It mentions obesity and/or insulin resistance as possible factors for worsening prognosis [9].
The present review considers the data of modern scientific literature concerning pregnancy complications in PCOS, as well as some pathophysiological processes that may underlie this association.
Miscarriage
Whether pregnant women with PCOS are at increased risk of spontaneous miscarriage remains a matter of debate. According to the 2012 Amsterdam Consensus, the incidence of early pregnancy loss in patients with PCOS is comparable to that in healthy women [9]. A meta-analysis of the course of pregnancies following in vitro fertilization (IVF) programs in patients with and without PCOS did not reveal differences in the incidence of miscarriages (OR 0.9, 95% CI 0.5-1.8) [10] . None of the 9 studies included in this meta-analysis showed differences between these groups. A recent study including 1084 patients (including 71 with PCOS) who underwent an IVF program showed that, after adjusting for hypertensive complications in pregnant women, the risk of delivery before 37 weeks of gestation did not reach statistical significance [11]. nine0019
A recent study including 1084 patients (including 71 with PCOS) who underwent an IVF program showed that, after adjusting for hypertensive complications in pregnant women, the risk of delivery before 37 weeks of gestation did not reach statistical significance [11]. nine0019
However, the results of the large Australian Longitudinal Study of Women's Health showed that the incidence of miscarriage was significantly higher in the group of pregnant women with PCOS compared with the control group (20% versus 15%, respectively, P=0.003) [12]. Although unlike BMI, PCOS is not considered an independent risk factor for miscarriage in overweight and obese women (OR 1.2, 95% CI 1.04–1.4, P=0.02 and OR 1.4, 95% CI 1.1–1.6, P=0.001, respectively). A recent retrospective observational study by A.E. Joham et al. (2014), in which case-control comparisons were made for age and BMI 9068 pregnant women with PCOS showed an increased incidence of miscarriage and preterm birth (corrected OR 1.70, 95% CI 1.