Sores on forehead
Rashes on Forehead: Symptoms, Causes, and Treatment
Many conditions can cause a forehead rash, so you may find yourself with one or more of the following symptoms on your skin:
- redness
- bumps
- lesions
- blisters
- itching
- flaking
- scaling
- swelling
- oozing
- bleeding
Additionally, you may experience other symptoms unrelated to your forehead rash. These may include flu-like symptoms.
Infections and viruses
An infection or virus may be the source of your forehead rash. These cases will likely require a doctor’s visit to diagnose and treat the rash.
Bacterial staphylococcal
This type of infection may be more commonly known as a staph infection. It’s caused by bacteria that lives on your skin. It’s the most common type of skin infection in the United States.
You’ll likely contract a staph infection through a break in your skin. Some staph infections appear as just a pimple or lesion that looks inflamed and irritated.
A serious type of staph infection is known as MRSA. A staph infection requires the attention of a doctor.
Chickenpox
Visible signs of chickenpox are an itchy rash, blisters, and blotchy skin. The blisters are liquid-filled. They break open and scab over.
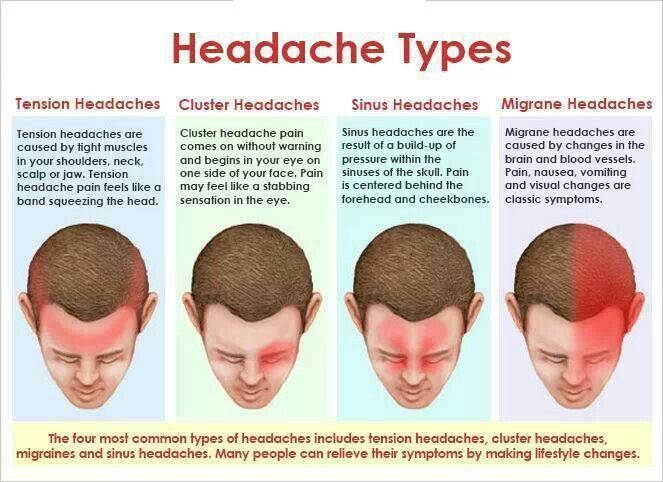
You’ll likely have other symptoms because of this virus, such as fever, fatigue, and headache. The condition is contagious for up to a week after the skin rash first appears.
Measles
A rash caused by measles will occur several days after you begin to notice other symptoms such as:
- a high fever
- red and watery eyes
- a runny nose
You may also have a cough and spots inside your mouth.
The red bumpy rash that follows these symptoms a few days later will begin at your hairline and forehead. The rash will spread down your body and fade after a few days.
Impetigo
Impetigo is a form of Group A Streptococcus infection. You may also refer to this as strep. You may think of strep throat, but you can also get strep on your skin.
You may think of strep throat, but you can also get strep on your skin.
Impetigo appears as itchy, small red spots that may group on the face. The spots will eventually break open and ooze. This stage is contagious if someone else touches the area. Eventually the spots will crust over and appear yellowish in color.
This infection is common in warm-weather months.
Folliculitis
Folliculitis occurs when a hair follicle becomes infected or irritated. The resulting rash can be red, bumpy, and itchy.
You can contract folliculitis from:
- a staph infection
- bacteria in hot water (such as a hot tub)
- an overgrowth of yeast bacteria on your skin
- an irritation after shaving
- having a suppressed immune system
Ringworm
This fungal infection appears as a circular, or ringed, rash. The red, scaly, and itchy rash may start small and expand in rings as it spreads on your forehead. This condition can be spread to others.
You may get ringworm on your forehead by sharing a pillow or a hat with someone who has the condition.
Shingles
Shingles begins as a painful, burning sensation and develops with areas of small blisters after a few days. The blisters will burst and crust over with time.
You may have this rash in the end stage for up to a month. This condition is caused by the same virus that causes chickenpox, which lives on your body as an inactive virus for years.
Allergies
Your forehead rash may be the result of an allergic reaction. There are several types of allergic reactions that can affect the skin.
Contact dermatitis
This rash is the result of your skin coming into contact with a substance to which it’s allergic. Contact dermatitis can appear as a rash on the forehead that’s
- red
- dry
- cracked
- stiff
- blistered
- weeping
- burning
- itchy
- painful.
It can also look like hives.
You may be more susceptible to contact dermatitis on your forehead because it comes into contact with many cleansers, soaps, makeup, shampoos, and other products for your hair and face that contain irritating chemicals and other substances.
Atopic dermatitis (eczema)
Another type of allergic rash is atopic dermatitis, or eczema. This rash can appear as red, dry, and itchy. It generally occurs in patches on the skin.
You cannot cure eczema. It’s a chronic condition. You’ll notice that it comes and goes and may get worse when exposed to a trigger, such as cold and dry weather.
Autoimmune
Autoimmune conditions occur because of an overreaction of the immune system. They result in a variety of symptoms. Some autoimmune systems manifest as rashes, such as psoriasis.
This chronic autoimmune condition appears in many forms, but often looks red, scaly, and patchy on the skin. The rashes caused by psoriasis come and go on the body and may be triggered by certain environmental factors like stress.
Other skin conditions
Acne
Acne is a very common skin condition, affecting 40 to 50 million people in the United States at any given time.
Acne is caused by clogged pores and can become infected if bacteria enters the pores. This condition can appear red and inflamed if the infection is under the skin, or may look like nodules or lesions on the skin.
Dandruff
You may experience itching and flaking skin on the forehead because of dandruff. This occurs when there’s an abundance of yeast on your skin or when your scalp is irritated by a chemical or excess oil in the skin.
Rosacea
This is a chronic condition that can cause redness on the face, as well as bumps. It occurs when your body sends more blood to the skin’s surface.
You may experience a rash from rosacea because of triggers like alcohol, certain foods, sun, and stress. Women, those with fair skin, and those who are middle-aged are most susceptible to this condition.
Other causes
Heat rash, sweat rash, and sunburn
Your forehead rash may be the result of exposure to heat, sweat, or the sun. You may have bumps and blisters that are red or pink, or your skin may appear red or pink in color.
Heat rash can occur because of humidity or overdressing. You may get a heat rash or sweat rash if you were exercising or in hot and humid weather while wearing a hat or headband.
You’re susceptible to sunburn if you expose your bare skin to the sun without sunscreen and protective clothing.
Stress
It’s possible that your forehead rash is due to stress. Stress can trigger other conditions that may cause the rash, or the rash may be your body’s response to the stress.
Medications and drug allergies
You may experience a forehead rash because of medications you’re taking or because of drug use. You may notice a rash a few days after starting a new medication or if you’ve been exposed to the sun while taking a photosensitive medication.
This rash may look like a few blotchy spots to begin with and spread over time.
Meningitis
A spotted rash on your forehead or other parts of your body that is purple, pink, or light red accompanied by flu-like symptoms, a stiff neck, and a headache may be the sign of a very serious infection called meningitis.
Meningitis should be treated immediately by a doctor.
Stevens-Johnson syndrome
A rare cause of a skin rash that can occur on your forehead and other parts of your body is Stevens-Johnson syndrome. This will appear as a red or purple rash and be accompanied by other flu-like symptoms. You need immediate medical care with this condition.
Rashes on forehead in babies
Forehead rashes in babies are likely related to one of the causes listed above. You should contact your child’s doctor if your baby develops a forehead rash for prompt diagnosis and treatment.
The doctor will examine your child and ask about other symptoms.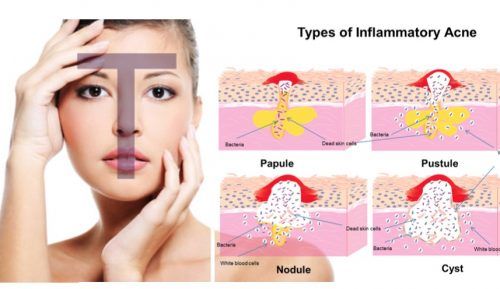 Some concerning symptoms that may accompany the rash may include diarrhea, fever, and blistered skin.
Some concerning symptoms that may accompany the rash may include diarrhea, fever, and blistered skin.
Rashes on forehead alongside HIV
You may experience a forehead rash if you have HIV. You may experience an HIV rash early in the course of infection or at any other time.
Rash is one of the most prevalent side effects of HIV medication. You may also be more susceptible to a forehead rash from one of the causes listed above because your immune system is compromised. See a doctor about your forehead rash if you have HIV.
Rashes on forehead during pregnancy
You may experience a range of changes to your skin during pregnancy that may result in a rash on your forehead. Hormone changes can result in a darkening of the skin (called melisma), as well as acne. After pregnancy, your skin should return to normal.
One concerning skin-related condition of pregnancy is cholestasis of pregnancy. This is when your increased hormones interfere with the bile in your gallbladder.
Cholestasis can result in very itchy skin and can pop up on any part of your body, especially your hands and feet. You need to see a doctor immediately if this occurs.
You may decide to seek the diagnosis of a doctor if your forehead rash is severe, persists, or is accompanied by other symptoms. The doctor will look at your physical symptoms, discuss any other symptoms with you, and may order tests to determine the cause of the rash.
Some treatments for certain forehead rashes include:
- Infections or fungi. May need prescription antibiotics or antifungal medications.
- Chronic conditions like atopic dermatitis, rosacea, and psoriasis. Avoid triggers.
- Contact dermatitis. Avoid products or substances that cause irritation.
- Heat rash, sunburn, and photosensitive medications. Protect your skin from sun exposure.
- Acne and other skin conditions. Use topical creams or medications recommended for the specific condition.

Consult a doctor before treating any forehead rash to make sure you’re using the right methods to alleviate the symptoms.
See a doctor if you suspect your rash is a symptom of a more serious condition. Other reasons to see a doctor include if the rash:
- spreads
- is painful
- is accompanied by a fever or flu-like symptoms
- blisters
- appears infected
Also see a doctor if the rash persists for a prolonged period of time.
Many skin conditions and other health conditions may cause a forehead rash. To reduce the symptoms of your rash, see a doctor for a proper diagnosis and treatment plan.
Common Causes & Treatment Options
Written by WebMD Editorial Contributors
Whether your shoes are too tight or you touched a hot stove, the result is all too familiar: a painful pocket of skin that's filled with fluid. A single blister like that is usually easy to treat at home, but if you see signs of infection, it's time to call your doctor.
What Causes Blisters?
Friction. You can get blisters when something rubs against your skin, like a tool handle or a new pair of shoes. Unlike corns and calluses, which show up after rubbing that's gone on for a long time, friction blisters come from brief, intense contact on a small area.
Burns. You can get a blister from getting too close to a flame or steam, or if you touch a hot surface. A severe sunburn can also cause blisters.
Cold. An extremely low temperature on your skin can cause blisters. For example, you might get one if your doctor freezes off a wart.
Irritants or allergy triggers. Your skin may blister if you come in contact with certain chemicals, cosmetics, and many plant allergens. You may hear your doctor call this problem irritant or allergic contact dermatitis.
Drug reactions. Sometimes your blisters may be a reaction to a drug you take. When your doctor prescribes a new medicine, always let them know about any drug reactions you've had in the past. And call your doctor if you get a blister after taking a medication.
And call your doctor if you get a blister after taking a medication.
Autoimmune diseases. Three diseases that curb your immune system -- your body's defense against germs -- can cause blisters:
- Pemphigus vulgaris, a possibly life-threatening skin disease, causes painful blisters in the mouth or skin. They become raw and crusted over after they burst.
- Bullous pemphigoid causes less severe blisters that heal faster and are not life-threatening. It mostly happens in elderly people.
- Dermatitis herpetiformis causes small, itchy blisters. It's a long-term condition that usually starts when you're a young adult. It's linked to gluten sensitivity.
Infection. Blisters are a common symptom of conditions like chickenpox, cold sores, shingles, and a skin infection called impetigo.
Genes.There are rare genetic diseases that cause the skin to be fragile and to blister.
How to Treat Your Blisters
If you leave your blister alone, it often gets better in 1 or 2 weeks. While it's healing, stay away from the activity that brought on the blister.
While it's healing, stay away from the activity that brought on the blister.
Some steps you can take to help the healing process:
Put on a loose bandage. It protects your blister while it heals.
Keep it padded. If your blister rubs up against your shoe, you can stop it from getting worse by using padding underneath the bandage.
Usually, there's no need to drain your blister, but you may want to if it's large and hurts a lot. If you decide to do it, use a small needle that you've sterilized with rubbing alcohol. Then pierce the edge of the blister. Afterward, wash the spot with soap and water and cover with petroleum jelly.
When to Call Your Doctor
Be on the lookout for signs that your blister is infected. Call your doctor if it gets more painful or you notice:
- Pus leaking out
- Swelling
- Redness
Trophic ulcer on the skin - symptoms, causes, signs, diagnosis and treatment in "SM-Clinic"
Phlebologist deals with the treatment of this disease
Book online Request a call
- What is it?
- Types of trophic ulcer
- Trophic ulcer symptoms
- Causes of trophic ulcers
- Trophic ulcer diagnostics
- Expert opinion
- Conservative treatment of trophic ulcer
- Surgical treatment of trophic ulcer
- Questions and answers
- Doctors
Types of trophic ulcers
Depending on the etiological factor, trophic ulcers can be of the following types:
- venous - caused by varicose veins or chronic venous insufficiency;
- arterial - provoked by the pathology of the arteries, more often by atherosclerosis; nine0008
- diabetic - often occurs against the background of type 2 diabetes;
- hypertensive - develops in severe hypertension;
- infectious - observed with syphilis, tuberculosis;
- neurotrophic - due to disorders in the functioning of the nervous system, more often a spinal injury.
If only the skin is affected, they speak of a superficial trophic ulcer. If subcutaneous fat is involved in the process, the ulcer is considered deep. When muscles and bones are affected, the defect is classified as very deep. Small ulcers are called defects with an area of up to 5 cm², medium - up to 20 cm², large - up to 50 cm², giant - more than 50 cm². nine0003
Symptoms of a trophic ulcer
The imminent appearance of a trophic ulcer on an extremity may be indicated by increased pain in the legs, pronounced edema, impaired skin sensitivity, and the formation of a local cyanotic spot. The location of the defect is often the lower leg, foot, interdigital spaces.
Due to the accumulation of toxic substances, the quality of the skin changes significantly. It becomes thick, tightly attached to the fiber, it is impossible to move it with your fingers or take it into a fold. Over time, hyperpigmentation and severe dryness appear, the skin acquires an unnatural shine. Later, cracks form in the zone of changes, through which lymph is released drop by drop. The formation of a whitish spot indicates the aggravation of atrophic changes. nine0003
Later, cracks form in the zone of changes, through which lymph is released drop by drop. The formation of a whitish spot indicates the aggravation of atrophic changes. nine0003
Further, imperceptibly for the patient himself, the skin is injured. To form a defect, a small scratch or damage in the shoe is enough. Some patients develop multiple small wounds in the area of skin cracks. First, a small, red weeping wound appears. Gradually, its edges expand. It is possible to merge several ulcers into one, larger one. Over time, the depth of the defect increases, active wetting is observed, and an unpleasant odor appears. nine0003
Causes of trophic ulcers
The following diseases can provoke the formation of trophic ulcers:
- Venous insufficiency, vasculitis, varicose veins. Trophic changes are caused by a violation of the outflow of venous blood.
- Arterial hypertension, atherosclerosis. Chronic ischemia of tissues is observed, as a result of changes in pressure in the arteries or a violation of their patency.
- Diabetes mellitus. Accompanied by microcirculatory disturbances in peripheral areas, changes in the acid-base state of tissues, and nerve damage. nine0008
- Injuries. An ulcer can occur as a result of damage to the spinal structures or peripheral nerve fibers, as well as after frostbite, deep burns.
A certain role in the development of the disease is played by infectious factors, intoxication, prolonged forced position of the body. However, in more than 70% of cases, ulcers are formed due to chronic pathologies of the veins.
Get advice
If you experience these symptoms, we recommend that you make an appointment with your doctor. Timely consultation will prevent negative consequences for your health. nine0003
You can find out more about the disease, prices for treatment and sign up for a consultation with a specialist by phone:
+7 (495) 292-39-72
Request a call back Book online
Why SM-Clinic?
1
Treatment is carried out in accordance with clinical guidelines
2
Comprehensive assessment of the nature of the disease and treatment prognosis
3
Modern diagnostic equipment and own laboratory
4
High level of service and balanced pricing policy
Diagnosis of a trophic ulcer
With a trophic ulcer, it is advisable to contact a phlebologist. Diagnosis of pathology is not difficult, the diagnosis is established at the stage of an objective examination of the patient. However, there are no specific treatments for the disease. Fighting only a skin defect with medications is ineffective if the underlying disease that causes skin damage is not treated. nine0003
Diagnosis of pathology is not difficult, the diagnosis is established at the stage of an objective examination of the patient. However, there are no specific treatments for the disease. Fighting only a skin defect with medications is ineffective if the underlying disease that causes skin damage is not treated. nine0003
In order to identify the etiological factor, the phlebologist conducts a thorough survey of the patient, collects an anamnesis. Based on the information received, the doctor prescribes an instrumental examination. If venous pathology is suspected, ultrasound duplex scanning and dopplerography are indicated. If there is a suspicion of diabetes, a blood sugar test is prescribed and an endocrinologist is consulted. If there is a history of spinal injury, the patient is examined by a neurosurgeon.
To select the optimal treatment tactics, an examination of the arteries of the extremities is carried out, and a bacteriological analysis of the discharge from the wound is prescribed (determines the type of pathogens and their sensitivity to antibacterial agents).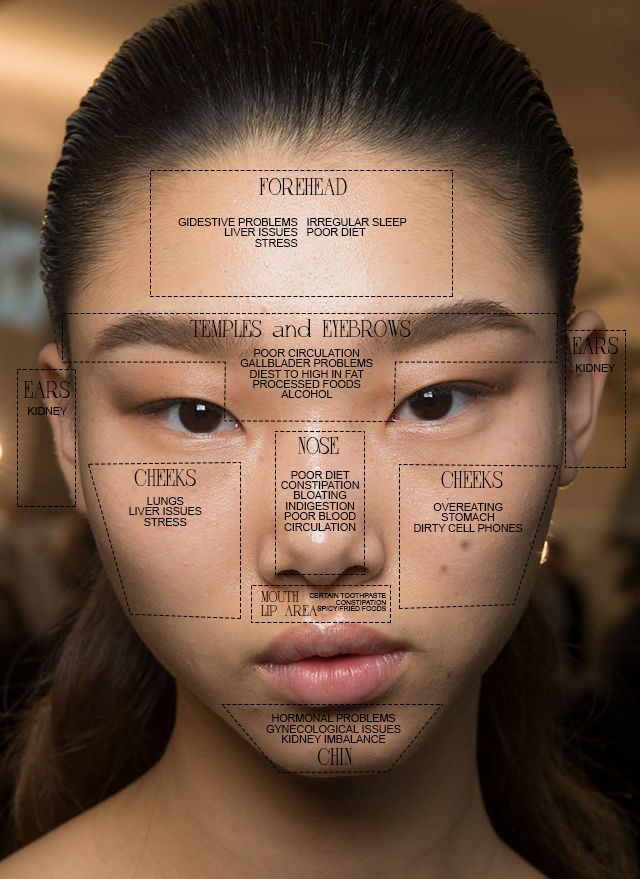 nine0003
nine0003
Expert opinion
Trophic ulcers are always a secondary process that develops against the background of the underlying disease (diabetes mellitus, arterial hypertension, varicose veins, etc.). This means that if you take control of the causative pathology, then you can avoid trophic disorders in the skin. However, even if you consult a doctor at the first signs of ulcer formation, you will be able to avoid severe disabling consequences that can progress quite quickly. nine0003
Gon Igor Alexandrovich,
surgeon, phlebologist, doctor of the highest category, Ph.D.
Methods of treatment
Treatment of trophic ulcers is aimed at relieving symptoms and suppressing the pathogenetic mechanisms of the underlying disease, preventing infection of the skin defect and stimulating its healing. It requires an integrated approach and active participation, both on the part of the doctor and the patient. In complex therapy, conservative and surgical techniques are used.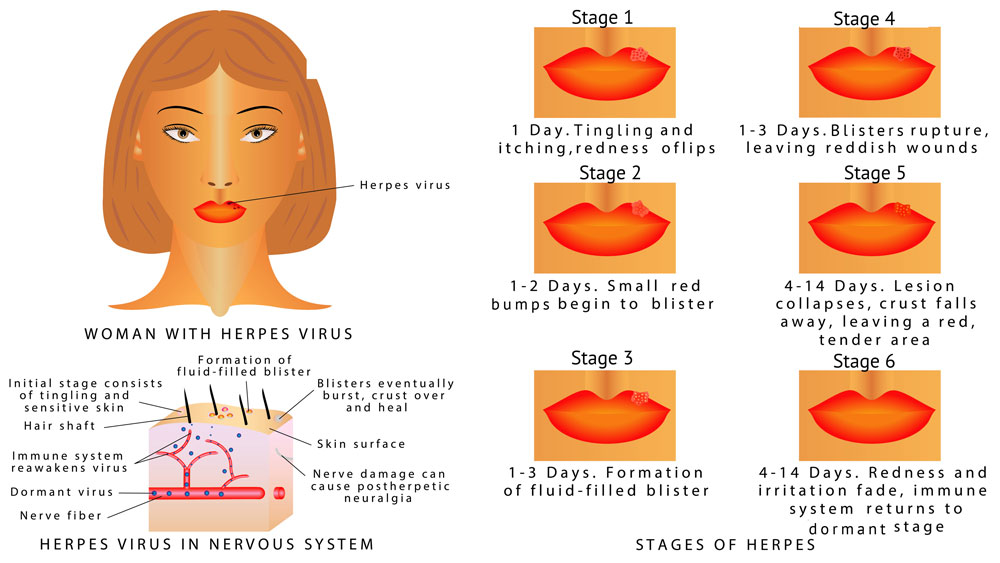 After the ulcer has healed, the patient must be constantly monitored by a doctor and undergo courses of treatment for the underlying pathology in order to maintain the remission stage. Therapy of superficial defects is possible on an outpatient basis, with deep ulcers and a severe course of the underlying disease, treatment is carried out in a hospital. nine0003
After the ulcer has healed, the patient must be constantly monitored by a doctor and undergo courses of treatment for the underlying pathology in order to maintain the remission stage. Therapy of superficial defects is possible on an outpatient basis, with deep ulcers and a severe course of the underlying disease, treatment is carried out in a hospital. nine0003
Conservative treatment
The first step is to control the disease that caused the ulcer. With venous insufficiency, venotonics and antiplatelet agents are prescribed. With atherosclerosis, a diet and drugs from the statin group are indicated. In diabetes mellitus, lipid-lowering agents, antiplatelet agents, and drugs to improve microcirculation are selected.
Almost all patients with trophic ulcers require lifestyle changes. It is important to exclude any load on the affected area. In some cases, strict bed rest may be prescribed. nine0003
Direct treatment of an ulcer involves daily cleansing of the surrounding tissues with water and soap and debridement of the skin defect with antiseptic agents. To prevent infection and septic complications, systemic antibiotics are prescribed, taking into account the results of a sensitivity test. For resorption of the scab and thrombotic masses, compresses with enzymes, heparin are applied; to stop inflammation, agents with a hormonal component, preparations based on dexpanthenol are used. nine0003
To prevent infection and septic complications, systemic antibiotics are prescribed, taking into account the results of a sensitivity test. For resorption of the scab and thrombotic masses, compresses with enzymes, heparin are applied; to stop inflammation, agents with a hormonal component, preparations based on dexpanthenol are used. nine0003
It is important to dress regularly and use sterile dry dressings to protect the wound. In stationary conditions, physiotherapy procedures are often prescribed that accelerate healing. Patients with venous insufficiency are shown to use compression underwear during the treatment period and after the defect has healed.
Surgical treatment
In case of varicose ulcers, after the defect has healed, surgical removal of the affected veins or treatment using non-surgical methods (laser coagulation, adhesive obliteration, radiofrequency ablation) can be performed. In case of damage to the arteries, revascularizing operations are performed aimed at restoring the trophism of peripheral tissues. For large defects that do not heal for a long time, a surgical operation involves skin plasty of the wound. nine0003
For large defects that do not heal for a long time, a surgical operation involves skin plasty of the wound. nine0003
Questions and answers
If you have a problem, you can contact a dermatologist, therapist, endocrinologist. Most patients are treated by a phlebologist.
Treatment includes washing the wound, treatment with antibacterial and healing agents, regular dressings. However, even strict adherence to these recommendations does not guarantee the healing of a trophic ulcer, since the underlying disease remains untreated. Procrastination and attempts to self-treat are the main mistakes of patients with trophic skin defects. Some of them get to the doctor after the wound becomes deep and reaches the bone tissue. Some patients delay the visit to a specialist until the color of the limb changes, which may be a sign of gangrene. nine0003
Doctors prescribe drugs based on heparin and dexpanthenol. Means with a combined composition of several antibiotics are used. It is possible to use hormonal creams and ointments. A good effect is given by drugs with an antibacterial, hormonal, antifungal and healing component. When choosing a local remedy, it is important to take into account the features of the development of the disease. Often, doctors recommend that patients alternate several drugs at once.
It is possible to use hormonal creams and ointments. A good effect is given by drugs with an antibacterial, hormonal, antifungal and healing component. When choosing a local remedy, it is important to take into account the features of the development of the disease. Often, doctors recommend that patients alternate several drugs at once.
No. A predisposing factor to the development of the disease are microcirculatory disorders, which are “own” for each patient. Trophic ulcers are a consequence of circulatory disorders and activation of their own opportunistic flora. The danger is infections that can enter an open wound and be released along with the exudate. Naturally, when caring for a person, you must carefully follow the rules of hygiene so as not to transfer the pathogenic flora to your skin and not to infect the ulcer through unwashed hands or dressings. nine0003
Babadzhanov B.R., Sultanov I.Yu. "Complex therapy of long-term non-healing trophic ulcers". Angiology and Vascular Surgery 2002.![]()
Vasyutkov V.Ya., Protsenko N.V. Trophic ulcers of the foot and lower leg. M. 1993.
>
Diseases referred to Phlebologist
Varicose veins (varicose veins) Lymphedema Postthrombophlebitic disease Vascular asterisks Vascular reticulum vein thrombosis Thrombophilia Thrombophlebitis Phlebitis Chronic venous insufficiency (XBH)
All doctors
VDNKh metro station
Belorusskaya metro station
Lesnaya, 57, pp. 57, 1
Raskova lane, 14/22
m. Youth
m. Textiles
m. Dynamo
m. Sevastopolskaya
m. Chertanovskaya
m. Krylatski
Voikovskaya metro station
Baltiyskaya metro station
Novye Cheryomushki metro station
Vodny stadium metro station
All doctors
Loading
nine0002 LicensesGo to the license section Go to the legal information section
possible causes and treatment methods
Ulcers on the face are an unpleasant problem that causes a lot of trouble and inconvenience.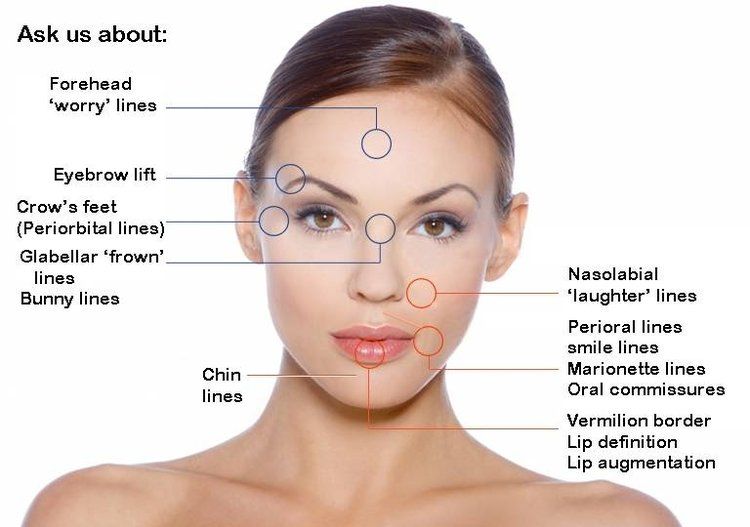 This formation often causes itching and a burning sensation. The disease must be treated in a timely manner, otherwise large wounds may occur, which will begin to bleed over time.
This formation often causes itching and a burning sensation. The disease must be treated in a timely manner, otherwise large wounds may occur, which will begin to bleed over time.
Ulcers: Causes
Our skin is one of the most delicate. The upper layer of the skin is constantly exposed to negative factors: frequent changes in temperature, various mechanical damage and other influences that can damage the epidermis. The appearance of ulcers is evidence that some disturbances in work have appeared in the human body. Through these changes, the rate of regeneration of the upper layer of the skin slows down. nine0003
The appearance of ulcers on the face can lead to quite a lot of problems for a person.
What are ulcers and what are they?
Human skin tends to recover after a certain time. Unfortunately, there are some factors that can interfere with the normal course of skin regeneration. During this period, various diseases can appear with their visible course. During such diseases, in the event of any wounds, the epidermis recovers either slowly or does not regenerate at all. nine0003
During such diseases, in the event of any wounds, the epidermis recovers either slowly or does not regenerate at all. nine0003
Unfortunately, in places where the skin is prone to necrosis, new tissue has not yet appeared - sores appear. Their surface may not heal for a very long time. The visual appearance of the patient worsens, and the skin, covered with ulcerative manifestations, becomes a kind of "gateway" for a large number of infections and bacteria. During the formation of ulcerative wounds, metabolism is disturbed, which helps rapid tissue regeneration.
Cold on the face: features, possible causes and...
If there is a cold on the face, then many things become inaccessible. It hurts to smile, you can't kiss, and...
According to the existing classification, the following types of pathological conditions of the skin are distinguished:
- Ulcers on the face that appear after certain injuries. These include mechanical damage - thermal, radiation, chemical, mechanical and electrical.
- The appearance of various tumors (benign or malignant). Such diseases include sarcoma or lymphogranulomatosis. nine0008
- In case of disturbance of normal arterial circulation. This can happen with the following diseases: anemia, diabetes, scurvy, as well as a variety of blood diseases.
- Ulcers on the face can also appear after infections have entered the body.
- If the patient already has tumors or progressive paralysis (so-called neurotrophic disorders).
- In the case of Raynaud's disease, as well as other diseases that entail disorders and changes in the tissues of the vessel walls (syphilitic aortitis, endarteritis obliterans, atherosclerosis). nine0008
- Ulceration may occur in case of penetration. They appear near the organs or can form in the cavity.
Thanks to the existing classification, modern medicine can quickly determine the cause of even weeping ulcers on the face, as well as quickly diagnose and prescribe the right therapy.
Varieties of ulcers, what they look like, symptoms, causes, methods...
In the article, we will consider what an ulcer of the skin and mucous membranes looks like, developing in different...
Signs of ulcers
Such skin disorders may begin along with other disorders of the normal functioning of the body. The most common symptoms and signs:
- The appearance of hypersensitivity in a certain area of the body after mechanical impact.
- Change in appearance - skin density, bruising, skin peeling, etc.
- After the skin has peeled off, new skin appears at a very slow rate. Instead, a non-healing and hypersensitive surface may appear. nine0008
With properly selected therapy, the skin will recover much faster: the ulcer is cleared of pus, the recovery rate will be faster than the rate of death of the epidermis.
What diseases cause ulcers on the patient's skin? If the skin condition changes, the patient may develop the following diseases:
- The appearance of tumors.
- Varicose veins, thrombophlebitis, thrombosis, vasospasm, arteriovenous fistulas, embolism.
- Lymph drainage may occur with anemia and diabetes.
- Progressive paralysis.
- Changes in the vascular walls.
All diseases can lead to the appearance of additional infections, as well as bleeding with poor quality and untimely diagnosis and treatment.
Therapy for ulcers
Since the appearance of ulcers is a sign of a certain disease, it is necessary to treat them, taking into account this disease. Many are interested in how to treat ulcers on the face? Complex therapy should be aimed not only at removing the external manifestation of the disease, but also at treating the underlying disease. The medicine is prescribed strictly by a doctor. Self-medication can be harmful.
All external manifestations can be easily and quickly removed using elementary hygiene. The doctor can add bed rest, physiotherapy. If necessary, fixation of the limbs is prescribed. The skin must be cleansed of pus. Often people develop lupus erythematosus. Clinical recommendations regarding the treatment of this disease directly depend on the form of the disease and the individual characteristics of the organism. Often, in the presence of such skin problems, dressings with a hypertonic solution are applied to the wounds, which help to draw out purulent secretions and relieve inflammation. nine0003
The skin must be cleansed of pus. Often people develop lupus erythematosus. Clinical recommendations regarding the treatment of this disease directly depend on the form of the disease and the individual characteristics of the organism. Often, in the presence of such skin problems, dressings with a hypertonic solution are applied to the wounds, which help to draw out purulent secretions and relieve inflammation. nine0003
Expert advice
Vitamin intake should not be ignored. Well helps hardening of the body. In especially advanced cases, surgical intervention is prescribed, during which the doctor will remove all dead tissue. Self-medication is dangerous to do, because it does more harm than good. It is important not to mask unpleasant symptoms, but to eliminate them forever. If a non-healing ulcer appears on the face, you should seek help from a dermatologist.
Traditional treatments
Folk methods of treating ulcers and basalioma of the skin of the nose include the following: using fresh cabbage and potato juice for washing wounds, applying compresses from strawberry decoction and juice from lilac tree leaves. These methods can help improve visually the skin. Unfortunately, ulcers are a manifestation of an internal disturbance in the functioning of the body, so complex therapy should be aimed at treating the whole organism as a whole.
These methods can help improve visually the skin. Unfortunately, ulcers are a manifestation of an internal disturbance in the functioning of the body, so complex therapy should be aimed at treating the whole organism as a whole.
Terminal
When contacting a specialist, drugs will be prescribed that will help increase the level of immunity, and will also help protect the body from the penetration of additional infections and bacteria into it. If you lead an unhealthy lifestyle, then a basalioma of the skin of the nose, which is a malignant neoplasm, may appear. Proper nutrition plays a particularly important role. In no case can you independently eliminate problems by squeezing out acne and other formations. A dangerous infection can enter the body, which can greatly harm a person, even death. During the treatment, it is forbidden to use cosmetics and perform thermal procedures. You can not visit the sauna and bath. It is important to avoid alcohol and not smoking tobacco products, as this will only inflame the skin more.