Sore bottom baby
Nappy rash - NHS
Nappy rash is common in babies and can usually be treated at home.
Check if your baby has nappy rash
Symptoms of nappy rash can include:
- red or raw patches on your baby’s bottom or the whole nappy area
- skin that looks sore and feels hot to touch
- scaly and dry skin
- an itchy or painful bottom
- your baby seeming uncomfortable or distressed
- spots, pimples, or blisters on bottom (spots can appear red or brown, but may be less noticeable on brown and black skin)
Credit:
HOUIN / BSIP / SCIENCE PHOTO LIBRARY: https://www.sciencephoto.com/media/615341/view
Things you can do to help with nappy rash
Nappy rash can be treated and prevented by following some simple advice.
Do
-
change wet or dirty nappies as soon as possible
-
keep the skin clean and dry – pat or rub the skin gently to dry it
-
leave nappies off when possible
-
use extra absorbent nappies
-
make sure your baby's nappies fit properly
-
clean your baby’s skin with water or fragrance-free and alcohol-free baby wipes
-
bath your baby daily (but not more than twice a day, as washing too much can make the skin dry out)
-
use olive oil to remove nappy rash ointment rather than water
Don’t
-
do not use soaps, baby lotion or bubble bath as they can irritate the skin
-
do not use talcum powder or antiseptics on nappy rash
-
do not put nappies on too tightly as it can irritate the skin
A pharmacist can help with nappy rash
If the rash is causing your baby discomfort, a pharmacist can recommend a nappy rash cream or medicine to treat it at home.
They may suggest using a thin layer of a barrier cream to protect the skin or giving your baby child's paracetamol for pain relief (only suitable for babies over 2 months old).
Non-urgent advice: See a health visitor or GP if:
- your baby's nappy rash does not go away, gets worse or spreads to other areas
- your baby has a high temperature
- your baby seems very uncomfortable
Treatment for nappy rash
A GP may prescribe treatment if your baby is in a lot of discomfort or they think your baby might have an infection.
They may prescribe:
- a steroid cream or ointment to help with redness and soreness
- an antifungal cream, if they think your baby has a thrush infection
- antibiotics, if they think your baby has a bacterial infection
Causes of nappy rash
It's normal for babies to sometimes get nappy rash.
It can be caused by:
- your baby's skin being in contact with pee or poo for a long time
- not cleaning the nappy area or changing the nappy often enough
- the nappy rubbing against your baby's skin
- an allergic reaction to soap, detergent or bubble bath
- irritation from fragranced baby wipes or wipes containing alcohol
- some types of medicines, such as antibiotics or laxatives (used to make a baby poo more often)
- thrush (a fungal infection)
Page last reviewed: 1 January 2023
Next review due: 1 January 2026
Nappy rash treatment and prevention
About nappy rash
Nappy rash is a very common skin condition. It happens when the skin on your child’s bottom is damaged and irritated.
The main cause of nappy rash is wearing a wet or dirty nappy for too long.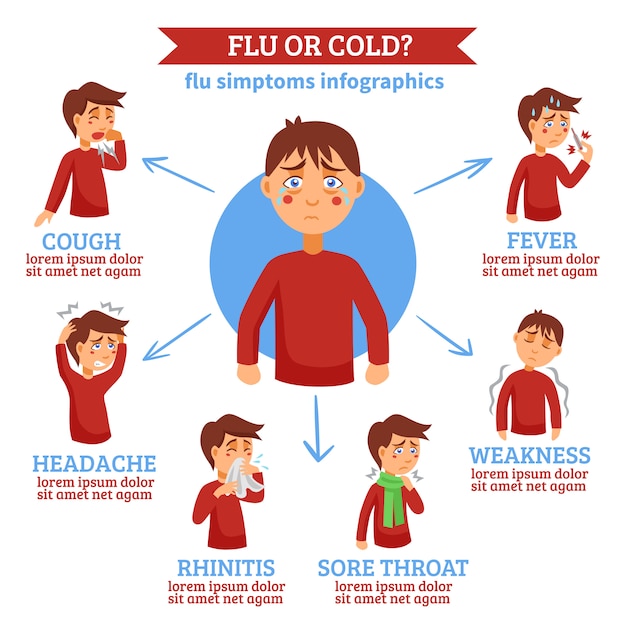 This is because your child’s skin can be irritated by a chemical called ammonia, which is in wee and poo. The dampness of wee and poo can be irritating too.
This is because your child’s skin can be irritated by a chemical called ammonia, which is in wee and poo. The dampness of wee and poo can be irritating too.
Other things that can cause nappy rash or make it worse include:
- friction between the nappy and the skin
- plastic pants – they stop air circulating normally and keep the nappy area damp
- soaps, detergents, fragrance and plant or food products left on the skin from bathing or left on cloth nappies from washing
- a chemical called methylisothiazolinone, which is in some disposable baby wipes
- conditions like eczema, psoriasis, thrush or impetigo.
Nappy rash is less common in babies who are breastfed, because their poo is less irritating. And it’s more common in babies who wear cloth nappies, because cloth nappies are less breathable and absorb less moisture than disposable nappies.
Symptoms of nappy rash
The skin on your child’s bottom and genitals will look inflamed and sore. On children with darker skin, the inflammation might look brown, purple or grey. On children with lighter skin, the inflammation might look red. Some areas of skin might be raised or swollen, and there might be breaks in the skin. These breaks are called ulcers.
On children with darker skin, the inflammation might look brown, purple or grey. On children with lighter skin, the inflammation might look red. Some areas of skin might be raised or swollen, and there might be breaks in the skin. These breaks are called ulcers.
Skin folds aren’t usually affected because wee doesn’t get into them. But nappy rash might sometimes go up onto your child’s tummy or spread up towards your baby’s back.
The rash can be uncomfortable and even painful, which can make your child irritable.
Does your child need to see a doctor about nappy rash?
Maybe. You should take your child to the GP if your child:
- has nappy rash that hasn’t improved after a week, even when you use the treatment below
- has blisters, crusts or pimples
- is upset and isn’t sleeping
- has an unexplained fever
- has nappy rash that’s spreading
- has inflammation, swelling or a scab at the end of their penis.
Diagnosing nappy rash
Your GP will talk to you about your child and look at their skin to diagnose nappy rash. Sometimes the GP might take a swab to identify any thrush or bacteria on the skin.
Sometimes the GP might take a swab to identify any thrush or bacteria on the skin.
Treatment for nappy rash
The aim of nappy rash treatment is to repair the damaged and irritated skin and protect it from any dampness and friction that might cause more damage.
Change your baby’s nappies frequently
Frequent nappy changes keep the nappy area dry and give your child’s skin a chance to heal. Check your child every hour or so to see whether their nappy is wet or soiled. Change wet or soiled nappies straight away.
Clean your baby’s skin
Use lukewarm water and cotton wool or a light cotton cloth to gently clean your baby’s skin after each nappy change.
When you bath your baby, use a gentle, soap-free wash. Pat your baby’s skin dry and gently apply a simple moisturiser.
Use a protective cream after each nappy change
Apply a simple, cheap barrier cream at every nappy change. You could use a zinc cream or a petroleum jelly like Vaseline. You can get these creams from a supermarket or your pharmacy without a prescription.
You can get these creams from a supermarket or your pharmacy without a prescription.
You should apply the cream thickly enough to create a barrier that stops wee and poo from getting onto the skin. You’ll know you’re putting the cream on thickly enough if you can still see some of the cream at the next nappy change.
Nappy-free time
Give your baby’s bottom some air for as long as possible every day. Let your baby play or sleep without their nappy – just put a towel underneath them.
To allow air to circulate freely and reduce friction, you could also fasten your baby’s nappy loosely or use a larger nappy.
Use disposable nappies
Disposable nappies absorb more moisture. If you regularly use cloth nappies, consider switching to disposable nappies for a short time until the rash has healed. Avoid plastic overpants if you’re using cloth nappies.
Wash and rinse cloth nappies thoroughly
Get rid of soap residue on cloth nappies by rinsing well in fresh water, particularly after using bleach-based detergents. Make sure that nappies are dry before using them again.
Make sure that nappies are dry before using them again.
Diet
Try to give your child fluids earlier in the evening to minimise night-time nappy wetting.
Highly acidic foods like citrus fruits, strawberries, pineapple, tomatoes and tomato-based products can make nappy rash worse. During episodes of nappy rash, you could consider reducing the amount of these foods and drinks in your child’s diet.
Medications
For severe nappy rash or nappy rash that won’t go away with simple measures, your GP might recommend using weak corticosteroid creams or ointments like hydrocortisone 1%. These are very safe to use for a little while under the supervision of your doctor. Always follow the instructions on the packet when putting these creams on your baby.
Your GP might also prescribe particular creams or ointments if your baby has a secondary infection with bacteria or fungus (thrush).
Complications of nappy rash: thrush and other infections
It will take weeks for your child’s skin to repair itself. While this is happening, your child’s skin might be more easily irritated.
While this is happening, your child’s skin might be more easily irritated.
Your child might also be more likely to get other infections like thrush. Thrush looks like bright, inflamed patches with clearly defined borders in the nappy area. You might also see a lot of dots or pus-filled bumps (pustules) beyond the outer edge of the rash. Thrush can affect the skin folds too.
Treat thrush with an antifungal cream prescribed by your GP. Thrush can take longer to clear than regular nappy rash and often comes back. Treatment can take a long time.
Nappy rash also increases the risk of urinary tract infection and vaginal infections in girls. This is why it’s important to treat nappy rash and prevent it if you can.
Prevention of nappy rash
Prevention is always better than treatment.
You can reduce the chance of your child getting nappy rash by keeping their nappy area clean and dry. Change your child’s nappy frequently and give their bottom air as often as you can.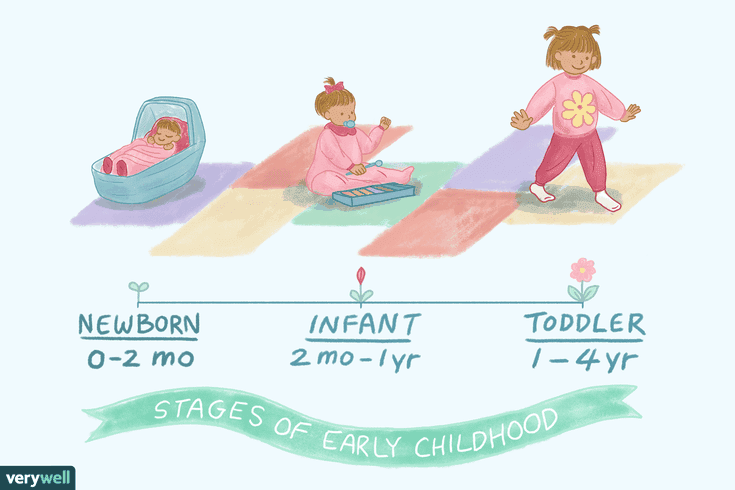
Protective barrier creams like petroleum jelly or zinc and castor oil can help keep your child’s skin in good condition.
Eye examination in children - MEDSI
It is very important that the child's visual system develops correctly. To do this, you must regularly undergo examinations by a qualified ophthalmologist. Over the years, the load on the eyes increases, and some diseases can only be cured in childhood.
Getting ready for the first eye examination
Eye examinations for children of different ages have their own characteristics. But usually the procedure consists of the following elements:
- Collection of complaints and anamnesis
- Refraction and visual acuity test to determine if the child needs glasses (or lenses)
- Eye movement friendliness examination
- Biomicroscopy for examination of the anterior part of the eye (eyelid, lens, cornea, etc.)
- Ophthalmoscopy for examining the fundus to detect possible changes
Parents should tell the doctor if there are any cases of eye disease in the family, and if the child has problems such as:
- Prematurity
- Complications during childbirth
- Delayed motor development
Parents should also inform the ophthalmologist if they notice how the child constantly rubs his eyes, cannot fix his gaze, blinks too often, etc. First visit - at the age (up to 6 months) 1 month, to exclude congenital pathologies
First visit - at the age (up to 6 months) 1 month, to exclude congenital pathologies
- Once every 6 or 12 months, if pathologies, illnesses or other problems with vision were recorded
- Every 2 years if no problems were noted
Early childhood screening
When examining the eyesight of the youngest children, the doctor determines whether the visual system is developing correctly. To do this, such manipulations are used as:
- Eye fixation and tracking assessment using a moving object (this can be a bright ball on a thread or a light spot)
- Evaluation of refraction (optics of the eye) with an automatic refractometer or manually
- Examination of the condition of the fundus and its environments using an ophthalmoscope
Such research methods allow to determine the presence of the following pathologies:
- Atrophy of the nerve (optic)
- Glaucoma
- Retinopathy
- Cataract
- Refractive errors (nearsightedness, farsightedness, astigmatism)
With the normal development of the visual system, a child is able to distinguish colors at the age of 2-3 months, and determine the shapes of objects and the distance to them - at the age of about a year.
Examination of children of preschool age
At this age, a visual examination in children helps to detect the presence of such disorders as:
- Amblyopia
- Strabismus
- Violation of volumetric vision, color perception
- Astigmatism
- Myopia
- Hyperopia
The following examinations are used for this:
- For strabismus: the child is shown an object and at the same time one by one close his eyes to determine the presence of an adjusting movement; if it is registered, then its direction is monitored - inward or outward, which means divergent or convergent strabismus. Also, the presence of strabismus is detected with the help of special tests, computer or printed, and on the device "Synoptofor" (from the age of four)
- Evaluation of refraction through retinoscopy (skiascopy): a doctor using a special mirror - a skiascope (retinoscope) - illuminates the pupil, in the lumen of which a non-static shadow will be visible; a special ruler with negative or positive lenses helps to determine which lens is needed to neutralize the shadow, i.
 e. to accurately determine the refraction
e. to accurately determine the refraction - Visual acuity analysis (using illustrated charts designed for children)
- Evaluation of eye mobility: the ophthalmologist moves the object in 8 directions and thus evaluates the degree of mobility
- Fundus examination
- Assessment of binocular vision using green and red filters placed in front of the left and right eyes, respectively. Then the child is asked to look at multi-colored circles; normally the child sees circles of both colors
- Examination under magnification of the anterior segment of the eye - conjunctiva, iris, eyelid, lens and cornea
Examination of school-age children
Schoolchildren experience severe visual stress, therefore, during a preventive examination, a doctor can diagnose such diseases and disorders during this period:
- Astigmatism
- Hyperopia (farsightedness)
- Incorrect functioning of the eye muscles or nerve
- Myopia (myopia)
- Dystrophic pathologies
Various methods are used to detect such violations:
- Determination of binocularity or monocularity
- Convergence assessment - alignment of the visual axes of the eyes when examining nearby objects
- Examination of visual acuity (by means of tables with letters)
- Fundus structure analysis
- Inspection of the structures of the anterior part of the eye
Parents should pay attention to such signs as:
- Unwillingness to do homework
- Constant eye rubbing
- Regular complaints of headache.

- Squinting when looking into the distance, the child looks from under his brows
These signs may be indicative of visual problems that prevent the child from studying normally because they have difficulty understanding text on the board or in the textbook.
Advantages of the procedure at MEDSI
- MEDSI specialists apply an integrated approach to the diagnosis of eye diseases, which includes both standard ophthalmic procedures and additional types of examinations (according to indications):
- Echobiometry
- Tonometry
- Analysis of eye secretions for bacterial and viral infections
- Clinics use only modern equipment from leading world manufacturers (Germany, Japan, USA, etc.)
- Appointments are conducted by highly qualified doctors with experience in working with children
- If necessary, it is possible to visit a pediatric ophthalmologist at home
- Specialists will help you choose both glasses and contact lenses
To make an appointment for a consultation, call 8 (495) 7-800-500.
Do not delay treatment, see a doctor now:
- Pediatric ophthalmologist appointment
- Ophthalmologist appointment
- Ophthalmoscopy under mydriasis
Pathology of the fundus . What are we treating. MNTK "Eye Microsurgery"
Pathology of the fundus:
1. Peripheral retinal dystrophies
2. Diabetic retinopathy
3. Retinal vein thrombosis
1. Peripheral retinal dystrophies
On the periphery of the retina, degenerative processes often develop, which are dangerous because they can lead to thinning and ruptures and, as a result, retinal detachment. Retinal detachment is dangerous with a significant decrease in vision. Peripheral vitreo-chorioretinal dystrophies (PVCRD) can develop in patients of all age groups, including children.
Causes of occurrence. Peripheral dystrophies occur with any type of refraction - both in nearsighted and farsighted, and in people with normal vision. There are many possible predisposing factors: hereditary, myopia of any degree, inflammatory eye diseases, craniocerebral and injuries of the organ of vision.
It is known that in people with myopia, peripheral degenerative changes in the retina are much more common due to an increase in the anterior-posterior axis of the eye, resulting in stretching of its membranes and thinning of the retina at the periphery.
Signs of peripheral retinal dystrophy. As a rule, changes in the retina in the periphery are asymptomatic and are detected during an accidental examination of the fundus by an ophthalmologist. In the presence of risk factors, the detection of dystrophy may be the result of a thorough targeted examination. This is the “cunning” of this pathology, which at any moment can cause a formidable complication - retinal detachment. Some patients complain of the appearance of lightning, flashes, a large number of floaters before the eyes, especially in the evening.
Some patients complain of the appearance of lightning, flashes, a large number of floaters before the eyes, especially in the evening.
Types of peripheral retinal dystrophies. It is necessary to distinguish between peripheral chorioretinal dystrophies (PCRD), when the pathological process affects only the retina and choroid, and peripheral vitreochororetinal dystrophies (PVCRD), with the involvement of the vitreous body. With PCRD, the so-called thinning and perforated retinal breaks are formed. Through these defects, fluid from the vitreous cavity can penetrate into the subretinal space, thereby leading to the development of retinal detachment. In PVRD, the mechanism of formation of a retinal tear is associated with the presence of traction from the vitreous body - against the background of adhesion of the vitrium with the retina at the site of dystrophy, in the presence of concomitant local detachment of the posterior hyaloid membrane, tension of the retina by the vitreous body occurs.
"Dangerous" types of dystrophies:
1. Lattice dystrophy
2. "Trace of the snail"
3. Any retinal breaks with or without localized retinal detachment
4. Vitreoretinal traction
Diagnosis of peripheral retinal dystrophies.
A complete diagnosis of peripheral dystrophies is possible when examining the fundus under conditions of maximum medical expansion of the pupil with the help of a special three-mirror Goldman lens, which allows you to see the most extreme parts of the retina.
Treatment. The goal of treatment is to prevent retinal detachment. Perform preventive laser coagulation of the retina in the area of dystrophic changes or delimiting laser coagulation around an existing gap.
Prevention. Timely diagnosis of peripheral dystrophies in patients at risk, followed by regular monitoring and, if necessary, preventive laser coagulation is the main way to prevent dangerous PCRD and retinal detachment. Patients with existing retinal pathology and patients at risk (myopic, patients with a hereditary predisposition, children born as a result of a difficult pregnancy and childbirth, patients with arterial hypertension) should be examined 1-2 times a year.
Patients with existing retinal pathology and patients at risk (myopic, patients with a hereditary predisposition, children born as a result of a difficult pregnancy and childbirth, patients with arterial hypertension) should be examined 1-2 times a year.
Fig. 1 Retinal dystrophy according to the type of “lattice”
Fig. 2 Retinal dystrophy “cochlea mark”
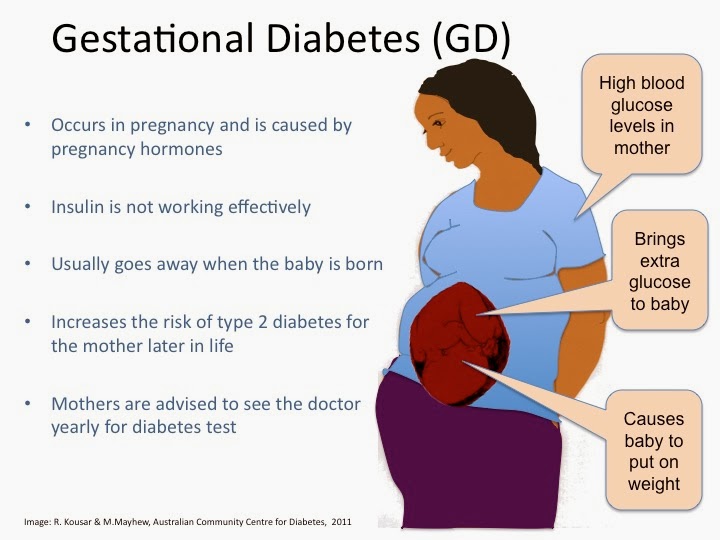
2. Diabetic retinopathy
Diabetic retinopathy is the most serious and frequent complication of diabetes mellitus. The disease is expressed in damage to the vessels of the retina and, in the absence of proper medical supervision and timely treatment, leads to blindness.
In diabetes mellitus, all blood vessels in the body are affected, but first of all, very small ones - capillaries. It is with damage to the capillaries that changes in the retina of the eye begin. The integrity of the vascular wall is violated, and then its permeability, hemorrhages, retinal edema occur, with prolonged existence of which the nerve cells are compressed and die.
The saddest thing is that diabetic changes in the retina may not manifest themselves for a very long time.
Over time, in the absence of control over the course of the disease, the blood supply to the retina worsens even more, so-called newly formed vessels prone to hemorrhages and scar tissue begin to grow in the oxygen starvation zones of the retina. This tissue grows over the surface of the retina and deep into the vitreous body, stretching and wrinkling the retina, causing it to detach. Vision progressively decreases.
Fig. 3 Preproliferative diabetic retinopathy
Fig.4 Proliferative diabetic retinopathy
Symptoms of diabetic retinopathy
Retinal damage is painless, in the early stages of diabetic retinopathy, the patient may not notice a decrease in vision. The occurrence of intraocular hemorrhages is accompanied by the appearance of a veil and floating dark spots in front of the eye, which usually disappear without a trace after a while (Fig.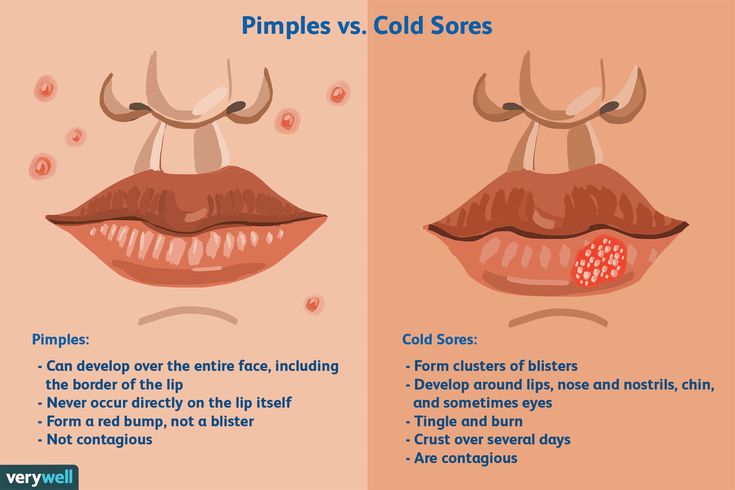 6). Massive vitreous hemorrhages lead to rapid and complete loss of vision. The development of edema of the central parts of the retina responsible for reading and the ability to see small objects can also cause a sensation of a veil before the eye (Fig. 7). Characterized by the appearance of difficulties when performing work at close range or reading.
6). Massive vitreous hemorrhages lead to rapid and complete loss of vision. The development of edema of the central parts of the retina responsible for reading and the ability to see small objects can also cause a sensation of a veil before the eye (Fig. 7). Characterized by the appearance of difficulties when performing work at close range or reading.
Fig.5 Normal vision
Fig.6 Vitreous hemorrhage
Fig.7 Macular edema
Prevention of blindness in diabetes
Most diabetic patients with a disease duration of more than 10 years have certain signs of retinal damage. Careful control of blood glucose levels, proper diet, and a healthy lifestyle can reduce, but do not eliminate, the risk of blindness from the eye complications of diabetes. Therefore, the surest way to prevent blindness is strict adherence to the frequency of fundus examinations by an ophthalmologist.
Necessary frequency of examinations of patients with diabetes mellitus by an ophthalmologist.
| Time of onset of diabetes | Time of first inspection |
| Age up to 30 years | After 5 years |
| Age over 30 | When making a diagnosis |
| Pregnancy | First trimester* |
| Inspection results | Frequency of re-examinations |
| No DR | Annually |
| Nonproliferative DR | 4-6 months |
| Proliferative, preproliferative DR, or diabetic macular edema | Laser treatment is prescribed, the frequency between the stages of which ranges from 2-3 weeks to 4-6 months. |
* during pregnancy, repeated examinations are carried out every trimester, even if there are no changes in the fundus.
Treatment of diabetic retinopathy
Since retinal damage in diabetes is secondary, systemic management of the underlying disease is extremely important - careful monitoring of blood glucose levels, blood pressure, and kidney function.
As a conservative treatment, various drugs are used that help strengthen the walls of blood vessels, resolve hemorrhages, improve metabolism and blood supply to the eye. However, numerous medications cannot stop the progression of the disease and should be used as supportive measures.
One of the main treatments for diabetic retinopathy is retinal laser photocoagulation.
The essence of laser exposure is reduced to:
- destruction of avascular areas of the retina, which are the source of the release of growth factors of newly formed (inferior) vessels, which are the source of hemorrhages in the eye cavity and retinal edema;
- to increase the direct supply of oxygen to the retina from the choroid;
- thermal coagulation of newly formed vessels.

In preproliferative or proliferative DR, laser burns are applied throughout the retina, excluding its central sections (panretinal laser coagulation).
Newly formed vessels are subjected to focal laser irradiation. This surgical method is especially highly effective when treated early, preventing blindness in 90% or more cases for a long time. In advanced situations, the effectiveness of laser coagulation is greatly reduced.
In the case of diabetic macular edema, the central parts of the retina are exposed to laser exposure. The long-term effect of treatment is largely determined by the systemic status of the patient. With a large height and area of macular edema, in addition to laser coagulation of the retina, it is necessary to introduce special drugs into the vitreous body - angiogenesis inhibitors.
Thus, laser coagulation of the retina is currently the method of choice for treating ocular complications of diabetes.
In advanced cases, surgical treatment is indicated.
3.Retinal vein thrombosis
Cardiovascular diseases rank first in terms of morbidity and mortality in almost all countries of the world.
As a rule, this pathology develops in patients after 40 years of age, but in recent decades there has been a persistent trend towards a decrease in the age of patients with this disease. It is known that diseases of the cardiovascular system negatively affect all organs and systems of the body. Often there are ophthalmic complications of cardiovascular pathology, such as retinal vein thrombosis - a violation of blood circulation in the central retinal vein or its branches.
Symptoms of retinal vein thrombosis
Thrombosis of the central retinal vein is accompanied by a sharp decrease in vision.
It usually occurs suddenly. Often the cause of its occurrence is an increase in blood pressure, physical overstrain and emotional stress. Thrombosis usually occurs in one eye, but occasionally this condition occurs on both sides. With thrombosis of one of the branches of the central retinal vein, the changes are limited to the area of the affected vessel. Visual disturbance occurs to a lesser extent. Vision after thrombosis of the central retinal vein is significantly restored, usually fails. In the fundus, edema of the macular region and the optic nerve head is found - the main reason for the decrease in central vision; the veins are sharply dilated and tortuous, there are multiple hemorrhages around the vessels. It is believed that the picture of thrombosis of the central retinal vein is similar to a “crushed tomato”.
With thrombosis of one of the branches of the central retinal vein, the changes are limited to the area of the affected vessel. Visual disturbance occurs to a lesser extent. Vision after thrombosis of the central retinal vein is significantly restored, usually fails. In the fundus, edema of the macular region and the optic nerve head is found - the main reason for the decrease in central vision; the veins are sharply dilated and tortuous, there are multiple hemorrhages around the vessels. It is believed that the picture of thrombosis of the central retinal vein is similar to a “crushed tomato”.
Fig. 8 Thrombosis of the inferior temporal branch of the central retinal vein
In order to correctly diagnose and select an individual approach to the treatment of each individual patient, it is necessary to perform OCT angiography to identify the area and height of the retinal edema, and to determine the zones of the non-perfused retina.