Soft spot on baby's head name
5 Warning Signs From Your Baby’s Soft Spot – Cleveland Clinic
When you’re a new parent, you learn that you need to protect that soft spot, or fontanelle, on your baby’s head. It rarely requires much attention, but it reminds you just how fragile your infant is.
That’s why, if something changes — is the soft spot sunken in a little? — you may worry there’s something wrong.
A change in the fontanelle isn’t always a major problem, but it can sometimes reveal internal issues, says Violette Recinos, MD, Section Head of Pediatric Neurosurgery at Cleveland Clinic.
“It is a good indicator of the baby’s potential hydration status and brain status,” she says. “It’s like an automatic pressure sensor.”
What is the fontanelle?
The fontanelle is the space between different plates of a baby’s skull that will eventually come together. This aspect of an infant’s skull structure typically allows for easy delivery through the birth canal and for rapid head growth during the first year of life, Dr. Recinos says.
There are actually two soft spots — one at the back of the head and another on top. The posterior one closes within a few months of birth, while the top fontanelle typically remains until just past a child’s first birthday.
Dr. Recinos explains what changes in the fontanelle can tell you about your infant’s health.
Sunken in soft spot
This is often a sign of dehydration, she says. It may occur if your child is sick and not getting enough fluids.
What you should do: See your pediatrician if the sunken appearance persists and you can’t get your baby to take in more fluids.
Advertising Policy
Swollen soft spot
After a fall, a swollen soft spot (particularly if it’s accompanied by vomiting) is sometimes a sign of head trauma.
What you should do: Seek medical treatment right away.
Bulging soft spot
Fluid buildup (hydrocephalus) can cause rapid head growth and can make the soft spot look “full,” Dr.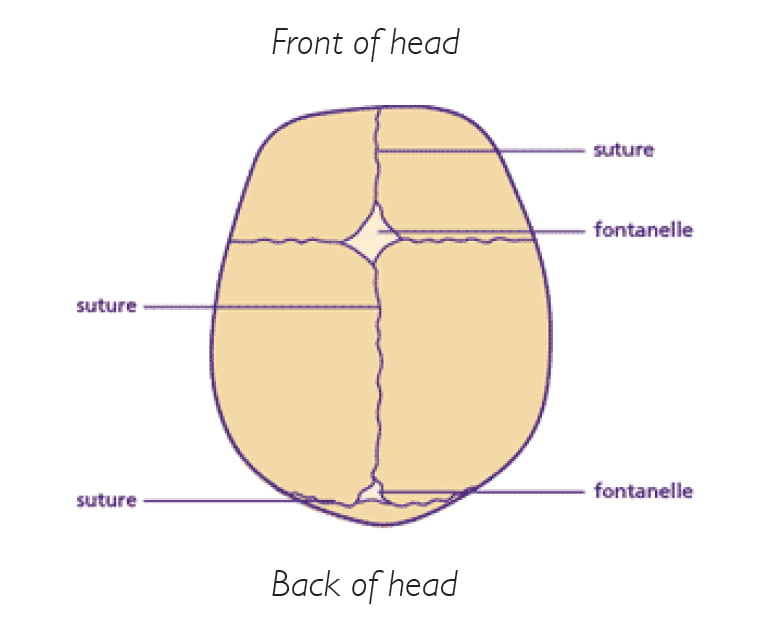 Recinos says.
Recinos says.
A bulging fontanelle also might signal internal bleeding or a tumor or mass causing pressure in the head.
What you should do: If their soft spot is bulging, that’s a reason to seek care from your pediatrician, she says.
Seek emergency care if your infant exhibits fatigue, vomiting or unusual mental status along with the fontanelle’s fullness. Treatment for these conditions may include surgery to insert a shunt that relieves fluid buildup or to remove any underlying mass, Dr. Recinos says.
Disappearing soft spot
Most of the time the soft spot is obvious, particularly on a newborn. But at times it can seem to disappear quickly.
This may scare parents, but it typically means it’s just a “quiet fontanelle,” not that it has fused together prematurely, Dr. Recinos says.
Advertising Policy
As long as your child’s head is growing normally, all is probably well, she says. But your pediatrician may suggest an imaging test to make sure the fontanelle is still open.
Occasionally, though, the skull bones do close earlier than normal on one side, causing craniosynostosis. Depending on which bones fused, the baby may develop an abnormal head shape. For example, sagittal craniosynostosis, the most common form, results in a longer head that is shaped somewhat like a football.
What you should do: Children with craniosynostosis may need surgery to open the fused bones and reshape the skull. In some cases, the child will wear a helmet afterward until the site heals and the head shape normalizes.
Soft spot that doesn’t close
If the soft spot stays big or doesn’t close after about a year, it is sometimes a sign of a genetic condition such as congenital hypothyroidism.
What you should do: Talk to your doctor about treatment options.
The bottom line? If you have any questions or concerns about your baby’s soft spot, it’s a good idea to check in with your pediatrician to make sure all is well.
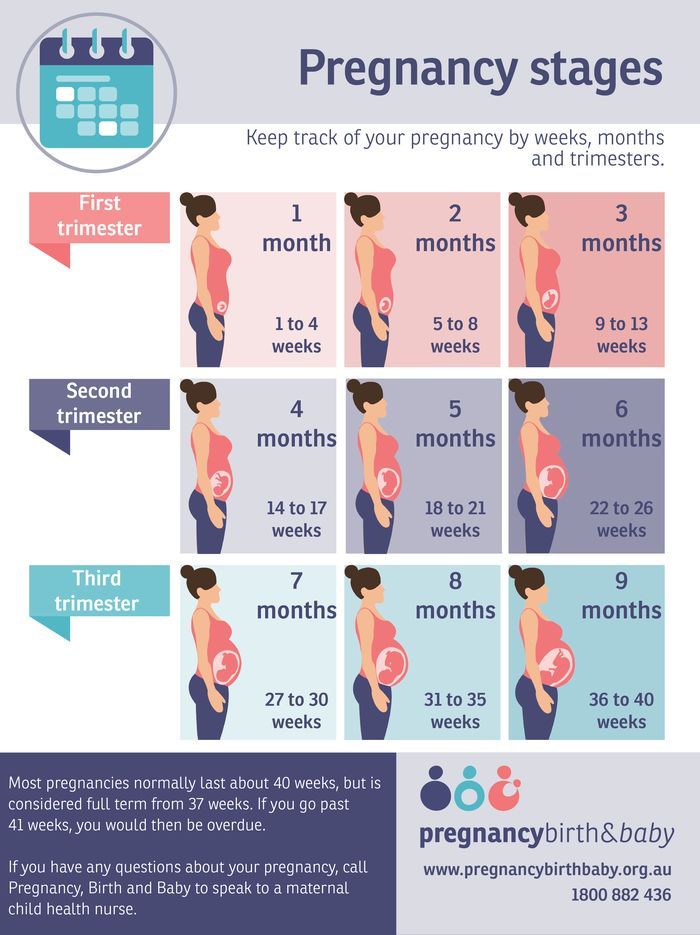
About the fontanelle | Pregnancy Birth and Baby
About the fontanelle | Pregnancy Birth and Baby beginning of content5-minute read
Listen
What is a fontanelle?
A fontanelle is a ‘soft spot’ of a newborn baby’s skull. It is a unique feature that is important for the normal growth and development of your baby’s brain and skull. Your health team will check your baby’s fontanelles during routine visits.
If you touch the top of your baby’s head you can feel a soft spot in between the bones — this is a fontanelle.
A newborn baby’s skull is made up of sections of bone known as plates that are joined together by fibrous joints called sutures. The sutures provide some flexibility and allow your baby’s head to narrow slightly as it travels through the birth canal. The sutures also enable your baby’s head to grow in the first years of life.
The sutures also enable your baby’s head to grow in the first years of life.
There are 2 fontanelles on your baby’s skull. These are the skin-covered gaps where the skull plates meet. The anterior fontanelle is at the top of your baby’s head, and the posterior fontanelle is located at the back of your baby’s head.
Illustration showing the anterior and posterior (front and back) fontanelles of a baby's skull.When will my baby’s fontanelles close?
The posterior fontanelle usually closes by the time your baby is 2 months old. The anterior fontanelle can close any time between 4 and 26 months of age. Around 1 in every 2 babies will have a closed fontanelle by the time they are 14 months old.
Can I touch my baby’s fontanelles?
Yes, you can gently touch your baby’s fontanelles. If you run your fingers softly along your baby’s head you are can probably feel them. Your doctor will touch your baby’s fontanelles as part of their routine medical examination. There is no need to be concerned or worried about touching your baby’s fontanelles as long as you are gentle.
What does a normal fontanelle look like?
Your baby’s fontanelle should feel soft and flat. If you softly touch a fontanelle, you may at times feel a slight pulsation — this is normal. If a fontanelle changes, or feels different to how it usually does, show your doctor or midwife as it may be a sign that your baby’s health may need to be checked.
Sunken fontanelle
If you notice that your baby’s fontanelles are low or sunken, your baby may be dehydrated.
However, you may notice other signs of dehydration in your baby before their fontanelles becomes sunken.
Other signs of dehydration include:
- having fewer wet nappies
- not feeding well
- loosing fluids from vomiting or diarrhoea
- perspiration (or sweating) in very hot weather
- being less alert or floppy
Bulging fontanelle
A bulging or swollen fontanelle may be a sign of a number of serious but rare conditions including meningitis or encephalitis (infections in the brain), cerebral haemorrhage (bleeding in the brain), hydrocephalus, an abscess or another cause of increased pressure in the brain.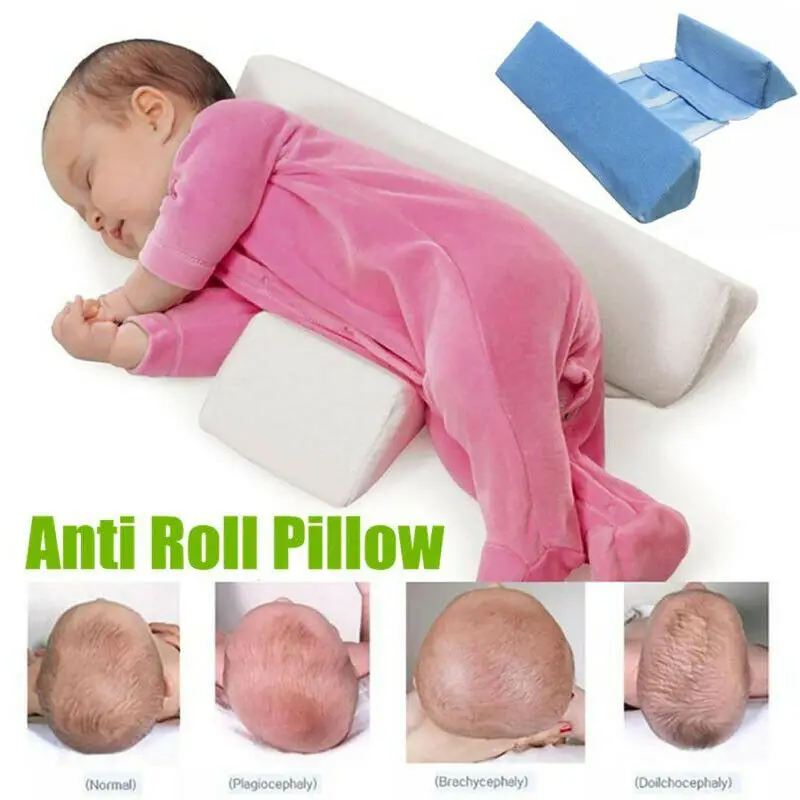
If you think that your baby’s fontanelles are bulging or sunken, seek medical advice immediately.
What if a fontanelle closes too soon?
Your baby’s fontanelles may close early. This can happen for several reasons. Your baby may have hyperthyroidism (high levels of the thyroid hormone) or hyperparathyroidism (high levels of parathyroid hormone). Another cause of early fontanelle closure is a condition known as craniosynostosis. Craniosynostosis occurs when one or more of the fibrous joints (sutures) between the bone plates in a baby’s skull fuse too early, before the brain has finished growing. As the brain continues to grow, it pushes on the skull from the inside but cannot expand into the closed over area. This causes the skull to have an unusual shape.
If you notice that your baby’s fontanelles seem to have closed early, if you can feel a ridge along your baby’s skull, or if you think that your baby’s head has an unusual shape, take your baby to see their GP or paediatrician.
What if a fontanelle doesn’t close?
Your baby’s fontanelles may not close on time for several reasons. Common reasons for delayed fontanelle closure include congenital hypothyroidism (low thyroid hormones from birth), Down syndrome, increased pressure inside the brain, rickets and familial macrocephaly (a genetic tendency to have a large head).
If one or both of your baby’s fontanelles haves not closed by the time they are 2 years old, speak to your GP or paediatrician.
If you have any concerns about your baby’s fontanelles you should make an appointment to see your child health nurse, GP or paediatrician.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Children’s Health Queensland Hospital and Health Service (Craniosynostosis), American Family Physician (The Abnormal Fontanel), Australian Family Physician (The 6 week check - An opportunity for continuity of care), WA Health (Bulging Anterior Fontanelle), The Royal Children's Hospital Melbourne (Clinical Practice Guidelines: Dehydration)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: February 2022
Back To Top
Related pages
- Regular health checks for babies
- Knowing your baby is well - podcast
- How to know when your baby is well - video
- How your baby’s brain develops
Need more information?
Newborn baby essentials
Find out some of the essentials for looking after your newborn. Find out when your baby will need to have health checkups and immunisations. There is also lots of information on nappies, giving your baby a bath and teeth development.
Read more on Pregnancy, Birth & Baby website
Colic in infants - MyDr.com.au
Colic is a pattern of unexplained, excessive crying in an otherwise healthy and well-fed baby and happens to 1 in 5 Australian babies.
Read more on myDr website
Knowing your baby is well - podcast
Listen to Dianne Zalitis, midwife and Clinical Lead at Pregnancy, Birth and Baby, talk to Feed Play Love with Shevonne Hunt about signs your baby is well.
Read more on Pregnancy, Birth & Baby website
Common worries and fears for parents
New parents often worry that they don't know what to do. However, there are practical ways to deal with the challenges so you can enjoy your baby more.
Read more on Pregnancy, Birth & Baby website
Flattened head
Plagiocephaly (flattened or misshapen head) means an uneven or asymmetrical head shape. Plagiocephaly won't affect your baby's brain development but it should be treated.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pediatric orthopedic traumatologist
New parents always have many questions about the development of their child. We asked the most frequently asked questions to the traumatologist-orthopedist of the Evromed clinic, Dmitry Olegovich Sagdeev.
- A small child is recommended to be shown to an orthopedist quite often: a month, three months, six months, a year . .. What is the reason for this, what exactly does the orthopedist evaluate?
.. What is the reason for this, what exactly does the orthopedist evaluate?
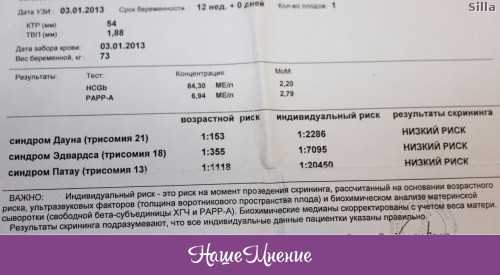
- The orthopedist watches how the child's musculoskeletal system develops during periods of its active development in order to notice possible deviations in its development in time and correct them. At an early stage - a month - we do an ultrasound of the hip joints, so as not to miss any congenital pathology. At three to four months, ultrasound is repeated for control in order to see the dynamics of joint development.
According to the results of an ultrasound examination, the doctor may suspect violations of the formation and dynamics of the development of the hip joint.
The doctor of ultrasound diagnostics evaluates the formation of the joint according to a special scale (Graf's scale), and then the orthopedist determines whether correction is required with therapeutic exercises, whether any physiotherapy is needed, etc.
The earlier deviations in the development of the child are detected, the more effective the treatment will be.
At about six months, the child begins to sit down, then he will get up, walk, and it is important to know how his hip joint is formed and, if there are violations, to have time to correct them before that moment.
Hip dysplasia is a defect in the formation of the hip joint, which in severe forms leads to the formation of subluxation or dislocation of the femoral head.
- When hip dysplasia is detected, orthopedic structures are usually prescribed: Freik pillows, Vilensky splints, etc. They look pretty scary, and parents are afraid that the child will be uncomfortable in them.
- The child will not experience discomfort. He still does not have a stable understanding of what position his lower limbs should be in, so the design will not interfere with him.
At the same time, due to the impact of these structures, the child's legs are located at a certain angle, and in this position the femoral head is centered in the cavity, it is in the correct position, any deforming load is removed from it, which allows the joint to develop properly.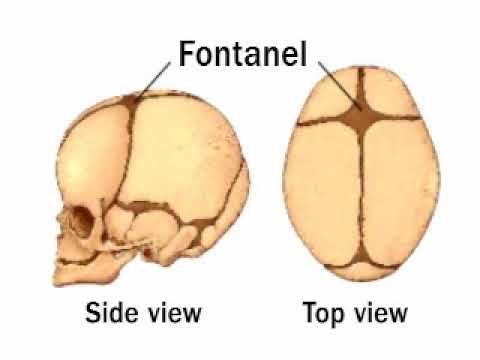 If this is not done, then a constant deforming load will be placed on the head of the femur, which will ultimately lead to subluxation and dislocation of the hip. This will be a severe degree of hip dysplasia.
If this is not done, then a constant deforming load will be placed on the head of the femur, which will ultimately lead to subluxation and dislocation of the hip. This will be a severe degree of hip dysplasia.
- In addition to dysplasia, ultrasound always looks at the formation of ossification nuclei in the hip joint. Why is their proper development so important to us?
The head of the femur is made up of cartilage. The ossification nucleus is located inside the femoral head and, gradually increasing, it seems to reinforce it from the inside and give the structure stability under axial load. In the absence of the ossification nucleus, any axial load on the thigh leads to its deformation, as a result of which subluxation and further dislocation of the hip may develop. Accordingly, if the core of ossification does not develop or develops with a delay, any axial loads are strictly prohibited: you can’t stand, and even more so, you can’t walk.
- Can I sit down?
- With a slow rate of ossification (ossification, bone formation), sitting is not prohibited, provided that the roof of the acetabulum is normally formed, the femoral head is centered. This is determined by ultrasound.
This is determined by ultrasound.
— What influences the formation of ossification nuclei, how can their development be stimulated?
- First of all - activity. Therefore, we recommend that you engage in therapeutic exercises with your child immediately from birth. Mom needs to do gymnastics with the child every day. Moreover, it is important that this should be a normal load, the so-called static load - when the child lies, and the mother spreads his arms and legs. I categorically do not recommend the “dynamic gymnastics” that is gaining popularity now - a set of exercises in which the child is twisted, twirled, swayed, rotated by the arms and legs, etc. to dislocation with rupture of the ligaments of the joint.
From 2.5 months, the child can and even needs to visit the pool. Individual lessons with a trainer in the water are very useful for the development of the musculoskeletal system, cardiovascular and respiratory systems, muscle training, and strengthening of the immune system.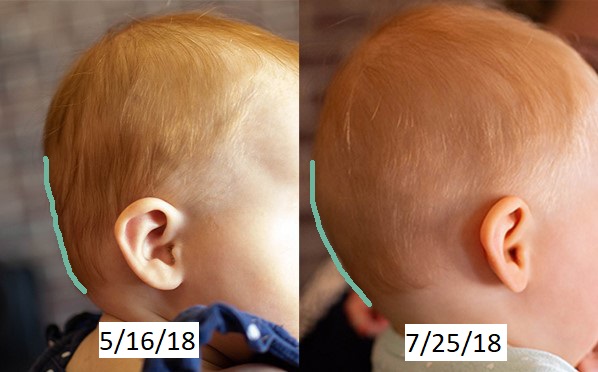
As an auxiliary procedure, massage is useful.
Vitamin D is also needed, it stimulates the development of bone tissue. Vitamin D is recommended to be given to almost all children under two years of age, and to some even later. This issue is resolved jointly by a pediatrician and an orthopedist, doctors select the dosage of the drug and the duration of its administration. There is little sunlight in our region, which provokes vitamin D deficiency in almost all children, which leads to rickets. In Siberia, most children who do not take vitamin D have some degree of rickets.
If there are indications, the doctor may prescribe physiotherapy: magnetotherapy, electrophoresis, applications with polymineral mud wipes. These are effective, time-tested methods.
- Doctors say that the child should not be planted before he sits down on his own, put, stimulated for early standing, walking. What is it connected with?
- This is due to the fact that in a small child the musculoskeletal system is still immature, and both it and the central nervous system are not ready for active axial loads. If we begin to actively verticalize the child, stimulate him to sit, stand, this can lead to spinal deformity, disruption of the formation of joints. At the start, they should develop without axial loads, as laid down by nature. The systems, and, first of all, the central nervous system, must mature so that the signal from the brain from the so-called “central computer” to the periphery reaches the periphery undistorted and the response from the periphery to the center is also adequate. No need to rush. When these structures are ready, the child himself will sit down, and crawl, and stand up.
If we begin to actively verticalize the child, stimulate him to sit, stand, this can lead to spinal deformity, disruption of the formation of joints. At the start, they should develop without axial loads, as laid down by nature. The systems, and, first of all, the central nervous system, must mature so that the signal from the brain from the so-called “central computer” to the periphery reaches the periphery undistorted and the response from the periphery to the center is also adequate. No need to rush. When these structures are ready, the child himself will sit down, and crawl, and stand up.
- What are the age norms when a child sits down, gets up?
— There are indeed certain norms, but we should not focus too much on them. Each child develops according to his own individual program, there is no need to adjust everyone to one standard. To assess its development, it is necessary to take into account many different circumstances, ranging from the characteristics of the course of pregnancy and the birth of a child. I think doctors need more time and norms to adequately assess whether the child is developing correctly or not, and if there is a delay, see it in time and help the baby.
I think doctors need more time and norms to adequately assess whether the child is developing correctly or not, and if there is a delay, see it in time and help the baby.
Children begin to sit down at about six months, crawl - at 7-8 months. Classical development: the child first sat down, then crawled, then begins to get up, move around with support. Then, when he felt that he was ready, he broke away from the support and took the first independent steps. This happens when the musculoskeletal system has matured, the central nervous system, the vestibular apparatus have adapted. And all these systems have learned to work together correctly.
Some babies start crawling before they sit down, others will get up before they can crawl. It happens that a child does not crawl at all, but immediately got up and went. All these are features of individual development.
- Why are such devices as a walker bad, allowing the child to "go" much earlier, entertaining him?
- Walkers knock down the "program" of the correct interaction between the central nervous system, the vestibular apparatus and the musculoskeletal system. In walkers, the child occupies an unnatural position, he does not take a full step in them, but simply hangs, pushes off with his toes and moves in space. His brain and muscles remember this incorrect program of vertical position and movement, and later, when the child tries to start walking without a walker, these incorrect settings work for him, the wrong muscle groups that should keep him in an upright position turn on, and the child falls. After a walker, it is very difficult for a child to maintain balance on his own, and subsequently it is quite difficult to correct this.
In walkers, the child occupies an unnatural position, he does not take a full step in them, but simply hangs, pushes off with his toes and moves in space. His brain and muscles remember this incorrect program of vertical position and movement, and later, when the child tries to start walking without a walker, these incorrect settings work for him, the wrong muscle groups that should keep him in an upright position turn on, and the child falls. After a walker, it is very difficult for a child to maintain balance on his own, and subsequently it is quite difficult to correct this.
- Another problem associated with the fact that the child was placed before he was ready is flat feet. Right?
- Flat feet can be congenital and functional (acquired).
If the child is placed too early, he may develop an incorrect foot placement. And often as a result, doctors diagnose flat-valgus deformity of the feet. This flat-valgus planting of the feet is usually not pathological. On examination, the doctor determines whether the foot is movable or rigid (inactive), and if the foot is movable, it is easily brought into the correction position, then we are not talking about deformity, this is just an incorrect setting, which is corrected by therapeutic exercises, the correct distribution of loads.
On examination, the doctor determines whether the foot is movable or rigid (inactive), and if the foot is movable, it is easily brought into the correction position, then we are not talking about deformity, this is just an incorrect setting, which is corrected by therapeutic exercises, the correct distribution of loads.
All these attitudes that mothers complain about: raking with toes, an apparent curvature of the limbs - this is a consequence of the transition of the child from a horizontal position to a vertical one and his adaptation to upright posture. During the prenatal period of development, the fetus is tightly “packed” inside the uterus: the arms are pressed to the body, and the legs are folded in a rather unnatural way for a person - the feet are turned inward, the bones of the lower leg and thigh are also twisted inward, and the hips in the hip joints, on the contrary, turn outward as much as possible . When the baby is just learning to stand, the incorrect position of the feet is imperceptible, because the turn of his legs in the hip joints and the twisting of the bones of the thighs and lower legs occurred in opposite directions - that is, they compensated for each other, and the feet seem to stand straight. Then the ratio in the hip joint begins to change - the head of the femur is centered, and this happens a little faster than the change in the rotation of the bones of the legs. And during this period, parents notice "clubfoot" and begin to worry. But in fact, in most cases, this is an absolutely normal stage of development, and there is no need to panic that the child somehow walks unevenly, puts his foot in the wrong way. Nature is smart, it has provided the whole mechanism for the development of the lower extremities, and you should not interfere in this process. Of course, if this worries you, then it makes sense to consult a doctor to determine whether these changes are physiological or pathological. If pathology - we treat, if physiology - no need to treat.
For the prevention of incorrect installation of the foot, passive therapeutic exercises, the choice of the correct orthopedic regimen, are necessary.
A small child cannot yet actively fulfill the direct wishes of his parents and do gymnastics himself, therefore, at this stage, a passive effect is recommended: walking barefoot on uneven surfaces, on grass, on sand, on pebbles (of course, we make sure that the child is not injured, that the surfaces are safe). As the child grows up (after about three years), we move on to active exercise therapy in a playful way. For example, we run on our heels to wash our faces, to have breakfast on our toes, we go to the bedroom like a penguin, watch cartoons like a bear. Try to make it interesting for the child to do this, and then he will get used to it and will be happy to do the exercises himself.
It is important for the correct installation of the foot and the selection of shoes. Shoes should be light, with an elastic sole, arch support - lined arch. If the arch on the sole is laid out, no additional insoles are needed (unless the doctor has prescribed). The height of the shoe is up to the ankle (you don’t need to buy high berets), so that the ankle can work freely and the short muscles of the lower leg can develop correctly - the very ones that hold the transverse and longitudinal arch of the foot.
For a child starting to walk, it is optimal that the shoes have a closed heel and toe - this is how the toes are protected from possible injuries if the child stumbles.
Is real flat feet treated differently?
- Yes, “real” flat feet cannot be cured by gymnastics. If this is congenital flat feet, then it is treated quite difficult and multi-stage. There are many surgical techniques that the doctor selects depending on the severity of the case and its features. Treatment begins with staged plaster casts. There are minimally invasive surgical aids on the tendon-ligamentous apparatus with the subsequent use of special devices - brace. There are also various surgical benefits associated with intervention on the joints of the foot, aimed at correcting the ratio of the bones of the foot and eliminating plano-valgus deformity.
Why treat flat feet and clubfoot?
- Because these violations lead to the deformation of the entire skeleton. From the bottom up, like a snowball, there are violations. Incorrect support leads to incorrect installation of the hip, the position of the pelvis changes, the knee joints suffer, receiving a modified load. To even out the load on the knee joint, the hip begins to rotate, trying to bring some kind of support position. The hip turned around, began to dislocate from the hip joint. To prevent him from dislocating, the pelvis tilted. The pelvis tilted - the angle of inclination of the spine changed. Accordingly, the spine bent to leave the head straight. As a result: gross violations of gait and the entire musculoskeletal system, scoliotic deformities of the spine. These conditions do not pose a threat to life, but the quality of life in a person with orthopedic problems suffers greatly.
To even out the load on the knee joint, the hip begins to rotate, trying to bring some kind of support position. The hip turned around, began to dislocate from the hip joint. To prevent him from dislocating, the pelvis tilted. The pelvis tilted - the angle of inclination of the spine changed. Accordingly, the spine bent to leave the head straight. As a result: gross violations of gait and the entire musculoskeletal system, scoliotic deformities of the spine. These conditions do not pose a threat to life, but the quality of life in a person with orthopedic problems suffers greatly.
- Another very common diagnosis that is made to newborn children is torticollis. How serious is this pathology?
- Many children are diagnosed with neurogenic functional torticollis, often they are diagnosed with subluxation of the first cervical vertebra (C1). Most often, this is a functional disorder that resolves on its own with minimal intervention from us, and it does not pose any threat to the health of the child.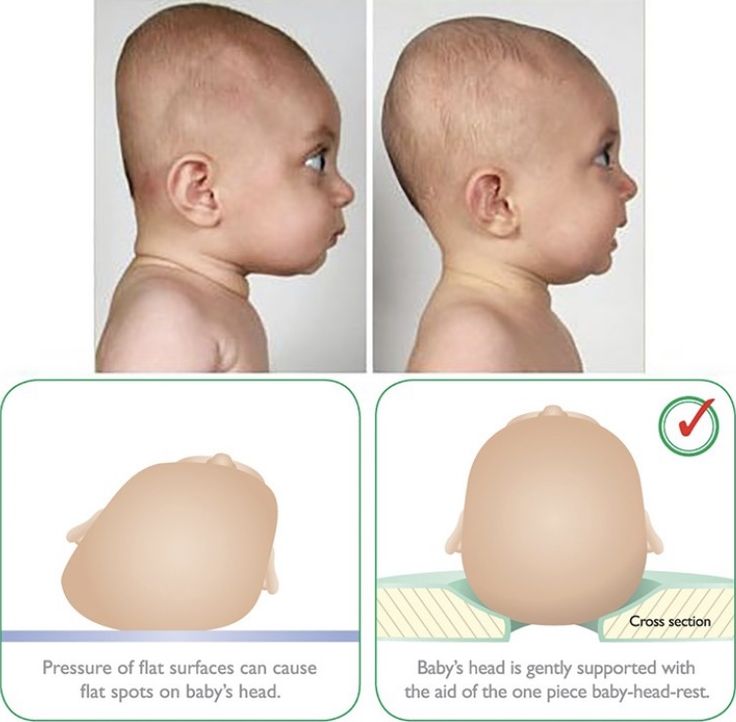
Children with functional torticollis are observed jointly by a neurologist and an orthopedist, usually corrective styling, an orthopedic pillow and a soft fixing collar are enough to resolve this situation without any complications.
Functional torticollis is important to separate from congenital muscular torticollis. If the latter is suspected, an ultrasound of the sternocleidomastoid muscles of the neck is performed in two months, which allows us to make the correct diagnosis with a high dose of probability. If an ultrasound examination reveals any changes in the sternocleidomastoid muscle, then we begin to conduct a comprehensive treatment aimed at eliminating torticollis and restoring the functional ability of the sternocleidomastoid muscle. The treatment includes fixing the head with an orthopedic collar, physiotherapy courses are prescribed, aimed at improving muscle nutrition and restoring their structure. With unsuccessful conservative treatment, if the deformity increases, then after a year, surgical treatment of congenital muscular torticollis is performed.
If you have any doubts, questions, worries, do not be afraid to consult a doctor. A pediatric orthopedist, neurologist, pediatrician are specialists who are always ready to answer your questions and help your baby grow up healthy.
Elbow subluxation
A very common injury in children is subluxation of the head of the radius in the elbow joint. Three bones join at the elbow joint: the humerus, ulna, and radius. To hold these bones, there are ligaments. In young children, the ligaments are very elastic, loose and can easily slide over the bone. With age, the ligaments become stronger, and subluxation no longer occurs so easily.
This injury happens when the child is pulled sharply by the arm: dad twisted, just abruptly lifted the child by the wrists (the child must be lifted, supporting the armpits) or it even happens that the parent of the child is leading the hand, the baby slipped, hung on the arm - and subluxation occurs .
At the moment of injury, you can hear how the joint clicked. Usually, with an injury, the child experiences short-term sharp pain, which disappears almost immediately. The main sign of injury is that the child stops bending the arm at the elbow - children keep the injured arm fully extended.
Usually, with an injury, the child experiences short-term sharp pain, which disappears almost immediately. The main sign of injury is that the child stops bending the arm at the elbow - children keep the injured arm fully extended.
As soon as possible after the injury, the child should be shown to a traumatologist who will set the subluxation and return the ligament to its place.
When should I contact a traumatologist?
Children often fall, hit, get injured in one way or another. How to determine when you can get by with a band-aid and iodine, and when you need to go to the emergency room?
- Any cut, stab wound should be shown to the doctor. Do not fill the wound with brilliant green or iodine! This will add a chemical burn to the cut. It is not necessary to apply cotton wool to an open wound - its fibers are then extremely difficult to remove from the wound. If the injury site is heavily soiled, rinse with clean water.
 Then cover the wound with a clean cloth (sterile bandage, handkerchief, etc.), apply a pressure bandage, and go to the emergency room as soon as possible. The doctor will carry out the primary surgical treatment of the wound, thoroughly clean it (you are unlikely to be able to do this on your own), restore the integrity of all structures and apply a bandage.
Then cover the wound with a clean cloth (sterile bandage, handkerchief, etc.), apply a pressure bandage, and go to the emergency room as soon as possible. The doctor will carry out the primary surgical treatment of the wound, thoroughly clean it (you are unlikely to be able to do this on your own), restore the integrity of all structures and apply a bandage. - If there is noticeable swelling at the site of injury. This may indicate that this is not just a bruise, but also a fracture, dislocation or rupture of the ligaments.
- If the child has lost consciousness, even briefly. This may indicate a traumatic brain injury, which can have serious consequences.
- If the child vomited after the injury. Vomiting, nausea, pallor also indicate the possibility of a traumatic brain injury.
- If a child hits his head. The consequences of a blow to the head may not be immediately noticeable, and at the same time have very serious consequences.
- If the child hits the stomach.
 A blow to the stomach may damage internal organs and cause internal bleeding.
A blow to the stomach may damage internal organs and cause internal bleeding. - If a child falls from a height (from a chair, table, etc.), falls off a bicycle, etc. It happens that outwardly it does not manifest itself in any way, but internal organs are damaged.
- If the child is anxious, behaves unusually.
In general - in case of any doubt, it is better to play it safe and see a doctor. Injuries in children is such a question when it is better, as they say, to overdo it than underdo it. There is no need to be shy, to be afraid that you are distracting ambulance doctors or emergency room doctors for nothing. Your child's health is the most important!
Beware of the trampoline!
Trampoline is a very popular entertainment among modern children. Unfortunately, this fun can lead to serious problems. The most common injury that children and teenagers get on trampolines is a compression fracture of the spine. Recently, there have been a lot of cases of compression fractures of the spine, including those who are professionally involved in trampoline sports.
There is no safe way to be on trampolines. A child, even without falling, can break the spine, because during jumps the spine receives very large axial loads. Especially, of course, it is dangerous for children with a weak muscular corset.
Childhood injuries
The process of cognition of the surrounding space by a child is rarely without injury. And if it was not possible to protect the baby from a fracture, cut, bite or burn, then it is important to use the “golden hour” as efficiently as possible - the first 60 minutes after the incident, when the health and sometimes the life of the child depend only on the actions of adults.
Parents need to be ready for literally anything. Steps, sharp corners, sockets, a stove with a hot pot and a cup of boiling water on the table - this is a far from complete list of areas dangerous for a small child. Therefore, it is necessary to have an idea about possible domestic injuries and know how to act in a particular case.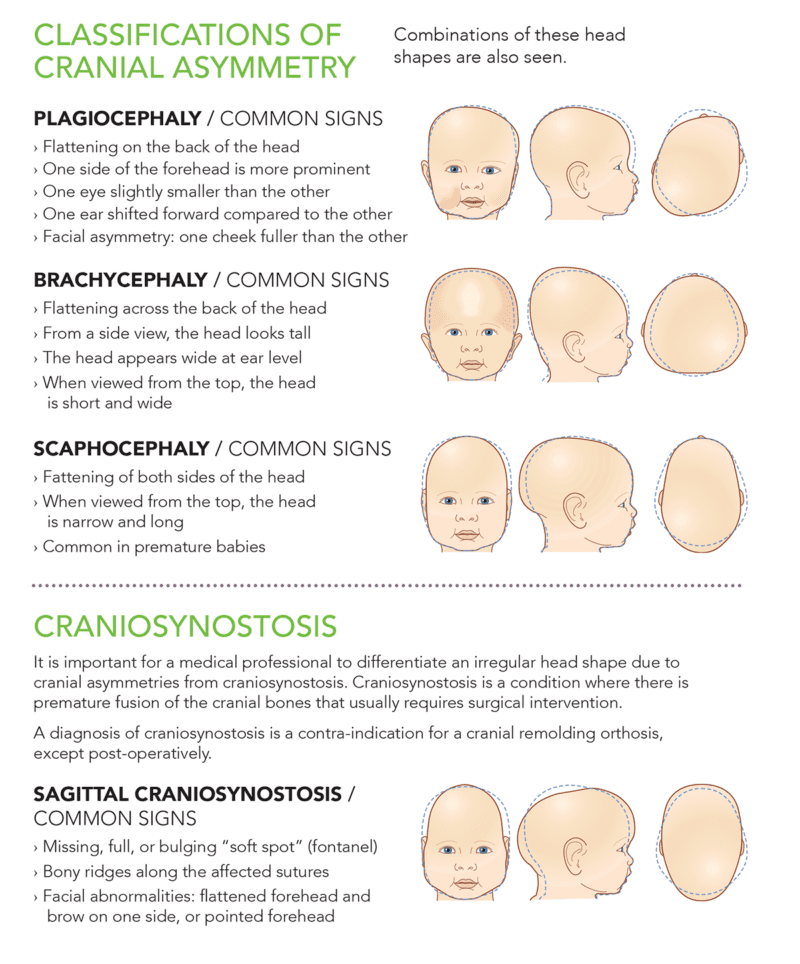 The first thing parents should do if the baby is injured is not to panic themselves, not to be helpless and unable to help the baby. Then you need to calm the child, give him first aid and show the baby to the doctor as soon as possible.
The first thing parents should do if the baby is injured is not to panic themselves, not to be helpless and unable to help the baby. Then you need to calm the child, give him first aid and show the baby to the doctor as soon as possible.
Bruise
Contusion is perhaps the most common childhood injury. Whether the child fell or hit something - swelling and bruising appear at the site of the bruise. With bruises, the integrity of the tissues is not violated, the main damage occurs in the vessels that burst, forming a hematoma (hemorrhage).
In this case, you need to put something cold on the site of injury: an ice bag, a towel moistened with ice water. Cooling the site of injury will relieve pain and prevent swelling or hematoma from building up. If the bruise is rapidly increasing in size and volume, you need to call a doctor or take the child to a traumatologist. Most likely, there is an increase in the hematoma, and it is necessary to evacuate the blood by puncture (the doctor will puncture the skin and suck out the blood).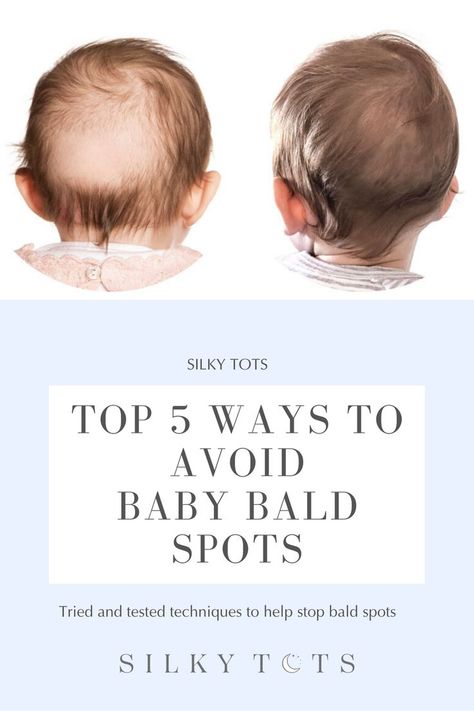
Dislocation
The joints of children are not as strong as those of adults, since the connective tissue in a child is more elastic and less dense. Therefore, any careless, abrupt movement or fall can lead to subluxations or dislocations. More often in children there are dislocations of the head of the radius, shoulder, fingers. Such an injury is accompanied by pain, the child cannot move the dislocated arm or leg, sometimes the limb takes an unnatural position due to “springy” fixation (when the dislocated part of the limb exerts springy resistance when trying to return it to its natural position and cannot “get back in place”).
If the arm is injured, it must be immobilized by applying a scarf bandage. The bandage is made from a square scarf, which is folded into a triangle, and the two extreme corners are tied around the child's neck. The forearm is laid on the plane of the handkerchief at an angle of 90°C. The middle corner of the fabric wraps around the shoulder and elbow and is fixed with a pin on the front side of the bandage.
In case of dislocation, the leg can be fixed with a bandage to an impromptu splint: thick cardboard, plywood, board, etc. The main thing is to achieve a comfortable, painless position of the limb, without trying to overcome the springy resistance. To do this, you can use pillows, rolled up diapers or blankets. Then you should put an ice pack (or other cold object) on the sore spot, give the child pain medication. And then, as soon as possible, show the injured baby to the traumatologist. The dislocation must be repaired as quickly as possible. Then, for 2-3 weeks, a bandage fixing the joint is applied to the child.
Stretching
Symptoms of sprain may not appear immediately, but after some time. In this case, swelling usually occurs at the site of the sprain, and the child feels severe pain.
In this case, it is necessary to immobilize or reduce the load on the damaged joint, apply cold to the pain site. Then you can apply a fixing cruciform bandage at the site of sprain (with oblique bandage moves, alternately apply it above and below the injured joint) and contact a traumatologist. If the injury happened late in the evening, and you can only see a doctor in the morning, no bandages should be applied to the injured joint. Give the limbs of the baby an elevated position. Give your child pain medication and go to the traumatologist in the morning. Often, with symptoms of sprain, a baby is diagnosed with a fracture.
If the injury happened late in the evening, and you can only see a doctor in the morning, no bandages should be applied to the injured joint. Give the limbs of the baby an elevated position. Give your child pain medication and go to the traumatologist in the morning. Often, with symptoms of sprain, a baby is diagnosed with a fracture.
Fracture
It is quite difficult to recognize a closed fracture without special skills and X-rays. Pain sensations occur in the child at the very moment of the fracture and appear when trying to move or when touching the affected area. Also, a fracture can be accompanied by a tumor (due to tissue edema) and rupture of soft tissues. More often in children, fractures of the fingers, bones of the forearm, shoulder, collarbone, and also the lower leg occur. First of all, you need to immobilize the broken limb with the help of improvised means (thick cardboard, ruler, board, etc.), give it an elevated position and apply cold to the place of pain.
If the leg is injured - eliminate any vertical or horizontal load on it. Fix the joints located above and below the site of a possible fracture with a long splint, bandaging it to the leg. Give your child pain medication and call an ambulance.
In case of tissue damage, in no case should you touch the wound above the fracture site with your hands to avoid infection. Cover it with a clean cloth moistened with an antiseptic. Do not bandage tightly, it is better to secure the napkin with a band-aid. Do not try to eliminate the displacement of bone fragments yourself, so as not to aggravate the injury. Take the injured child to a traumatologist as soon as possible. He will choose an adequate surgical or conservative treatment tactics (for example, apply a cast).
Injuries with damage to the skin
Splinter
A small foreign body (a sliver, a thorn, etc.) that has entered under the skin gives the baby discomfort. If the splinter is not removed, suppuration may begin.
If possible, carefully, using tweezers, pull out the splinter and treat the wound with hydrogen peroxide and any other available antiseptic (zelenil, iodine). If you can’t get a splinter with tweezers, in no case should you expand the wound with a needle - you need to contact a surgeon or traumatologist at the clinic. The doctor, using special tools, quickly, without causing pain and additional injury to the child, will remove the foreign body and, if necessary, prevent possible infectious complications by prescribing antibiotics in the form of tablets or ointments.
Scratch or abrasion
These are superficial skin lesions. It is almost impossible to protect a child from them. But you can teach him to seek help from his parents in case of injury and in no case touch the wound with his hands so as not to infect.
A scratch or abrasion should be treated with any drying antiseptic. When the wound is healing, do not allow the baby to tear off the dry crust so that a rough scar does not form, which can remain for a long time. If inflammation is suspected (redness around the abrasion, swelling, fluid release), it is necessary to show the child to a surgeon or traumatologist.
If inflammation is suspected (redness around the abrasion, swelling, fluid release), it is necessary to show the child to a surgeon or traumatologist.
Cut
This is a fairly deep skin injury, accompanied by bleeding.If the wound was caused by a broken cup or glass, or a Christmas toy, or any other fragile object, if possible, remove the fragments remaining in the wound of the baby. The main thing is not to drive the fragments deeper. After washing the wound under running water, treat the edges with an antiseptic and apply a pressure bandage (tightly bandaging a gauze napkin to the wound).
For cuts, regardless of their depth, the main thing is to stop the bleeding. If the pressure bandage does not help, you need to apply a tourniquet above the injury site and show the baby to the doctor no more than 60 minutes later. A tourniquet is applied to the leg in the upper third of the thigh or lower leg, and to the arm - in the upper part of the shoulder or forearm. Under the tourniquet, be sure to put cotton wool or a napkin. It is dangerous to overexpose the tourniquet - this can lead to tissue necrosis, since blood is temporarily not supplied to them.
Under the tourniquet, be sure to put cotton wool or a napkin. It is dangerous to overexpose the tourniquet - this can lead to tissue necrosis, since blood is temporarily not supplied to them.
To avoid the possibility of wound infection, poor healing, rough scarring and, of course, tetanus infection, show any cuts to a doctor. Otherwise, the responsibility for possible complications lies with you.
Only the doctor decides whether to suture or strengthen the edges of the wound with a band-aid, or it is enough to treat it with medicines.
Tetanus prophylaxis is carried out in children who are not vaccinated against this infection in trauma centers or hospitals. Antitoxin from tetanus is administered urgently once to those babies whose wound was contaminated during trauma.
Tetanus vaccination is included in the National Immunization Schedule and is given to all children at 3-4.5-6 months. Revaccination is carried out at 1.5 years, at 7 and at 14 years. After age 18, the vaccine is given every 10 years.
After age 18, the vaccine is given every 10 years.
Burn
A baby can get burned not only by fire, but also by boiling water. In this case, burns are of three categories: light, characterized by reddening of the skin; medium, when a bubble is formed filled with liquid; as well as severe, in which there is charring of the skin and underlying tissues - to the bone. In either case, the child will experience pain ranging from tingling to sharp.In these cases, firstly, it is necessary to stop the effect of heat as soon as possible and cool the affected area either under a stream of cold water or with a damp and cold cloth, often replaced. A good effect with mild and moderate burns is given by alcohol applications - applying a napkin soaked in alcohol to the burn site until it warms up and dries. Alcohol, evaporating from the skin, will carry away heat from the burnt surface, and the tissues will gradually cool.
After 5-10 minutes of cooling (during this time, not only the surface tissues, but also the deep layers of the affected skin cool down), you need to assess the baby's condition, give him an anesthetic, calm him down and, applying a bandage moistened with an antiseptic, contact a surgeon or traumatologist. It is better to show a child even with a mild, in your opinion, degree of burn to a specialist in a clinic.
It is better to show a child even with a mild, in your opinion, degree of burn to a specialist in a clinic.
In case of burns, do not apply ointment dressings and do not treat the skin of the crumbs with coloring antiseptics - such as brilliant green, fukartsin, etc. This will make it difficult for a doctor to assess the degree of tissue damage. Only he can correctly determine the degree of the burn, remove necrotic (dead) tissues and choose further tactics for treating the child.
It is not necessary to lubricate the burn site with oil or urine, since in the first case a film is formed that disrupts the thermal exchange in the tissues (the burned layers of the skin cannot cool), and the urine dehydrates the tissues that have already lost water as a result of the burn.
Other injuries
Nosebleed
Children tend to break the nose, thereby violating the integrity of the capillaries (the smallest vessels), which is why the nose bleeds. At an early age, this is mainly due to a fall. Older children may develop nosebleeds due to damage to the nose in a fight.
At an early age, this is mainly due to a fall. Older children may develop nosebleeds due to damage to the nose in a fight.
A common mistake in helping with a nosebleed is tilting the baby's head back. This can not be done, as the baby can simply choke on blood entering the throat. The child needs to be seated and asked to tilt his head slightly forward, pressing the injured nostril against the nasal septum with his finger for a few seconds.
If blood continues to flow, place a piece of cotton wool or a piece of bandage moistened with hydrogen peroxide in the nostril and apply ice or something cold to the nose. If this does not help, you need an examination by an otolaryngologist, surgeon or traumatologist who can stop the bleeding.
Items in the nose
Sometimes it's not easy to tell if a child has put something up its nose. If nothing is visible in the nostril, and there is also no unnatural protrusion of one of the nasal passages, but at the same time a healthy baby breathes with a whistle, it is possible that there is a foreign object in the nasal cavity.
If you have not seen how the child put something in his nose, but at the same time do not exclude such a possibility, ask him about it if the baby already knows how to talk. In any case, even if you think that you can remove the object from the child's nose yourself, do not do this so as not to damage the nasal septum.
If you find (or suspect) something foreign in the nose, show the baby to a surgeon, traumatologist or otolaryngologist. With special tools, the doctor will remove the foreign object from the nose.
Swallowed toy
Signs that a toy is not completely swallowed or lodged in a child's airway may include: choking, wheezing, coughing, voice change or loss.
In these cases, call an ambulance immediately. If a child is choking, you need to act immediately! Lay the baby face down, supporting him with his hand, for example, in the waist so that his head is lower than the body level, and pat a few times on the back between the shoulder blades or, lowering the child upside down, shake him.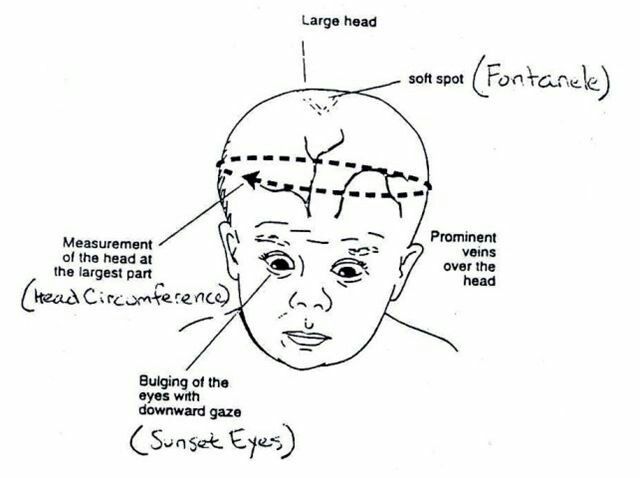
If the foreign body does not come out, try to open the baby's mouth and, pulling back the tongue, assess the situation: if there is a toy in your field of vision, it is advisable to remove it as soon as possible. But only if you are sure that it can be done with a finger or long tweezers.
If all else fails and the child continues to choke, begin artificial respiration until the ambulance arrives. The child must be laid on his back on a hard surface; throw his head back; closing your nose with your fingers, inflate the lungs of the child with your breath, combining this with a closed heart massage (pressing on the sternum). Ha 1 breath perform 5 pressure on the sternum. If the child is very small, press with two crossed fingers. For an older baby, an indirect heart massage is performed by pressing on the sternum with several fingers. Remember, all these manipulations must be done very quickly!
If the child has swallowed a small object and does not show any complaints, it is better to discuss further actions with the doctor after the x-ray of the gastrointestinal tract. Buttons, beads and other small smooth objects are usually evacuated from the intestines along with feces on their own. In other cases, surgery may be required.
Buttons, beads and other small smooth objects are usually evacuated from the intestines along with feces on their own. In other cases, surgery may be required.
Electric shock
Modern parents know that with the advent of a child, all sockets in the house must be closed, and electrical appliances must be removed to a distance inaccessible to the baby. However, it is not always possible to follow all precautions, and children often get electrical injuries while examining sockets or electrical appliances.
In the event of an electrical injury, a child may be found to have a burn at the point of contact with the wire, a weak or arrhythmic heartbeat, and shortness of breath.
In this case, parents should ensure that the injured baby is calm and immediately call an ambulance, even if at first glance it seems that the electric shock was not strong. Often, the heart suffers from an electrical discharge, so do not delay calling a doctor for a child. You need to see a doctor for a few days.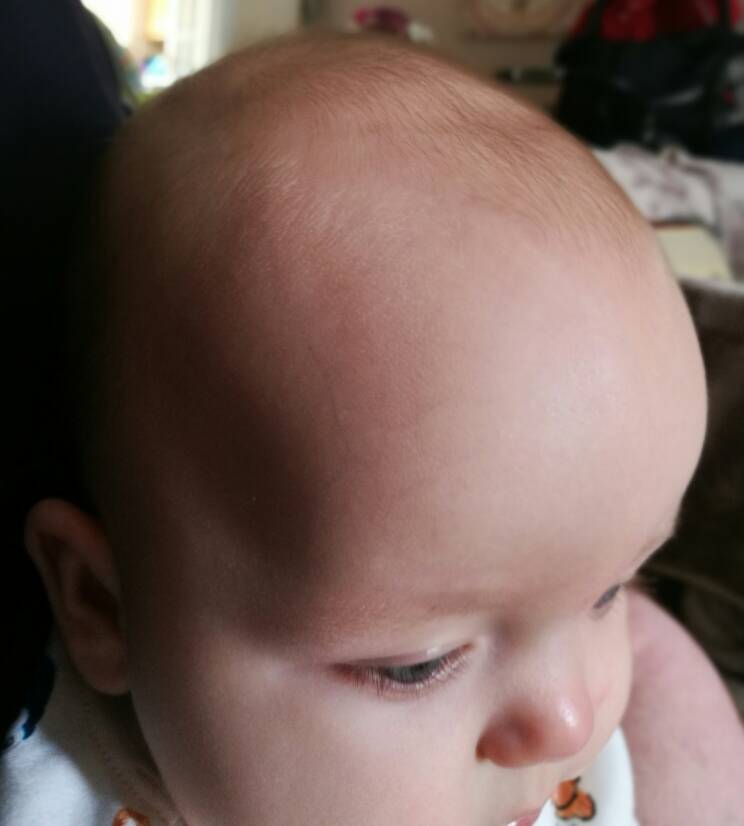
Bite
Bites are different: insects or animals. Minor insect bites (for example, mosquitoes) should be treated with special antihistamines (antiallergic), antipruritic agents and the child should not be allowed to comb the damaged area.
When bitten by a stinging insect (wasp, bee), it is necessary to remove the entire sting with tweezers and treat the wound with any antiseptic (brilliant green, iodine).
If bitten by a tick, be sure to consult a surgeon. In no case do not try to remove it from the baby's skin with your fingers, since the contents of the internal organs of the tick (and if it is infected, then the encephalitis virus), as from a syringe, is released into the wound. And this significantly increases the risk of infection with tick-borne encephalitis. Remember: the rate of its spread and the severity of the course of the disease depend on the dose of the virus that enters the body.
If bitten by an animal, including a domestic animal, wash the bite site very thoroughly with soap and water to remove the animal's saliva. Through pinpoint skin wounds, microbes can get deep under the skin and cause inflammation. After washing, apply a loose, clean and dry aseptic (sterile) bandage to this place and immediately show the child to the doctor.
Through pinpoint skin wounds, microbes can get deep under the skin and cause inflammation. After washing, apply a loose, clean and dry aseptic (sterile) bandage to this place and immediately show the child to the doctor.
When bitten by an animal suspected of rabies, children are given specific prophylaxis with anti-rabies gamma globulin and anti-rabies vaccine.
Hazardous areas
A child, especially a small one, can be injured, it would seem, out of the blue. In residential premises, the main danger is represented by sharp corners of furniture, sockets, household electrical appliances, sharp and cutting objects, slippery carpets or parquet - in general, almost any interior and household items.A playground in the yard can also be a threat: slides, ladders, swings and trees often cause various childhood injuries. Even a seemingly safe park bench can turn into the cause of splinters or become the culprit of a fracture due to an unsuccessful jump.
The first line in the list of causes of childhood injuries is transport.