Rhesus negative blood group
Rh factor blood test - Mayo Clinic
Overview
Rh factor is an inherited protein found on the surface of red blood cells. If your blood has the protein, you're Rh positive. If your blood doesn't have the protein, you're Rh negative. The "+" or "–" you might see after your blood type refers to Rh positive or Rh negative.
Rh positive is much more common than Rh negative. Having an Rh negative blood type is not an illness, and it usually does not affect your health. But it can affect pregnancy. Your pregnancy needs special care if you're Rh negative and your baby is Rh positive. That's called Rh incompatibility. A baby can inherit the Rh factor from either parent.
Your health care provider will advise that you have a blood type and Rh factor screening test during your first prenatal visit. This will show whether you are Rh positive or Rh negative.
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
During pregnancy, problems can happen if you're Rh negative and your baby is Rh positive. Usually, your blood doesn't mix with your baby's blood during pregnancy. However, a small amount of your baby's blood could come in contact with your blood when the baby is born. It can also happen if you have bleeding or trauma to your abdomen during pregnancy.
If you're Rh negative and your baby is Rh positive, your body might produce proteins called Rh antibodies if your blood and the baby's blood mix. Those antibodies aren't a problem during the first pregnancy. But problems can happen if you become pregnant again.
If your next baby is Rh positive, the Rh antibodies can cross the placenta and damage the baby's red blood cells. This could lead to life-threatening anemia, a condition in which red blood cells are destroyed faster than the baby's body can replace them. Red blood cells are needed to carry oxygen throughout the body.
If you're Rh negative, you might need to have another blood test — called an antibody screen — several times: during your first trimester, during week 28 of pregnancy and when your baby is born.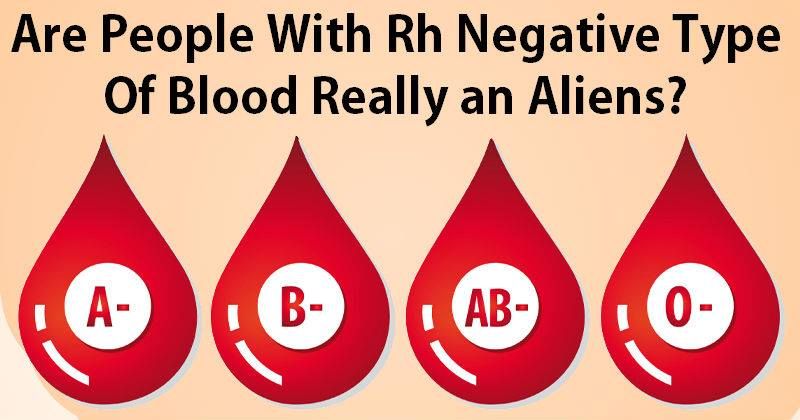 Some people need the test more often.
Some people need the test more often.
That test is used to detect antibodies to Rh positive blood. If you haven't started to produce Rh antibodies, you'll likely need a shot (injection) of a blood product called Rh immune globulin. This prevents your body from producing Rh antibodies during your pregnancy.
If your baby is born Rh negative, you don't need any other treatment. If your baby is born Rh positive, you'll need another injection shortly after delivery.
If you're Rh negative and your baby might be or is Rh positive, your health care provider may recommend an Rh immune globulin injection after situations in which your blood could come into contact with the baby's blood, including:
- Miscarriage
- Ectopic pregnancy — when a fertilized eggs implants somewhere outside the uterus, usually in a fallopian tube
- Abortion
- Removal of a molar pregnancy — a noncancerous (benign) tumor that develops in the uterus
- Amniocentesis — a prenatal test in which a sample of the fluid that surrounds and protects a baby in the uterus (amniotic fluid) is removed for testing or treatment
- Chorionic villus sampling — a prenatal test in which a sample of the wispy projections that make up most of the placenta (chorionic villi) is removed for testing
- Cordocentesis — a prenatal test in which a sample of the baby's blood is removed from the umbilical cord for testing
- Bleeding during pregnancy
- Injury or other trauma to your abdomen during pregnancy
- The external manual rotation of a baby in a breech position — such as buttocks first — before labor
- Delivery
If the antibody screen shows that you're already producing antibodies, an injection of Rh immune globulin won't help. Your baby will be carefully monitored during your pregnancy. The baby might be given a blood transfusion through the umbilical cord during pregnancy or immediately after delivery if necessary.
Your baby will be carefully monitored during your pregnancy. The baby might be given a blood transfusion through the umbilical cord during pregnancy or immediately after delivery if necessary.
| Mother's Rh factor | Father's Rh factor | Baby's Rh factor | Precautions |
|---|---|---|---|
| Rh positive | Rh positive | Rh positive | None |
| Rh negative | Rh negative | Rh negative | None |
| Rh positive | Rh negative | Could be Rh positive or Rh negative | None |
| Rh negative | Rh positive | Could be Rh positive or Rh negative | Rh immune globulin injections |
What you can expect
An Rh factor test is a basic blood test.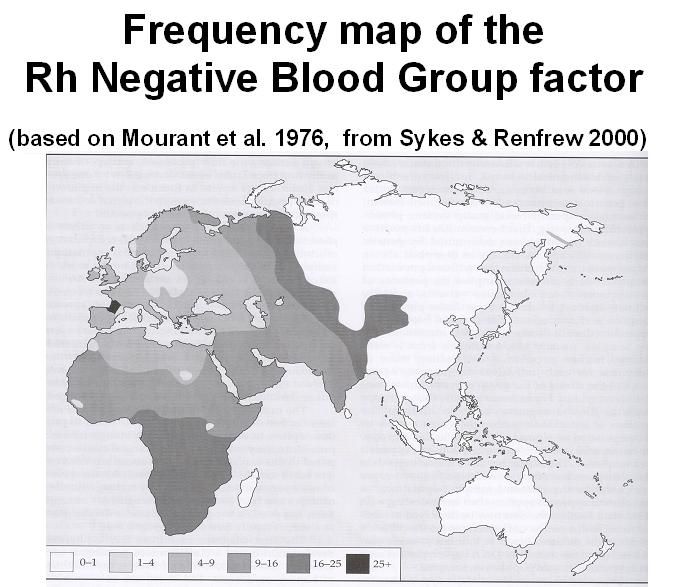 The blood sample usually is taken during the first prenatal visit and sent to a lab for testing. No special preparation is necessary.
The blood sample usually is taken during the first prenatal visit and sent to a lab for testing. No special preparation is necessary.
Results
If you're Rh positive, you don't need to do anything.
If you're Rh negative and your baby is Rh positive, your body could make antibodies that might be harmful during another pregnancy. Take these steps:
- If you have vaginal bleeding any time during pregnancy, contact your health care provider right away.
- Talk with your health care provider about scheduling an Rh immune globulin injection during your pregnancy.
- Remind your health care team during labor that you're Rh negative.
By Mayo Clinic Staff
Related
Products & Services
Blood groups - NHS
There are 4 main blood groups (types of blood) – A, B, AB and O. Your blood group is determined by the genes you inherit from your parents.
Each group can be either RhD positive or RhD negative, which means in total there are 8 blood groups.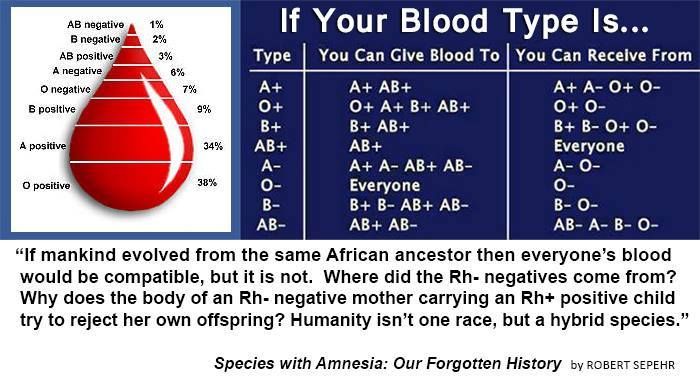
Antibodies and antigens
Blood is made up of red blood cells, white blood cells and platelets in a liquid called plasma. Your blood group is identified by antibodies and antigens in the blood.
Antibodies are proteins found in plasma. They're part of your body's natural defences. They recognise foreign substances, such as germs, and alert your immune system, which destroys them.
Antigens are protein molecules found on the surface of red blood cells.
The ABO system
There are 4 main blood groups defined by the ABO system:
- blood group A – has A antigens on the red blood cells with anti-B antibodies in the plasma
- blood group B – has B antigens with anti-A antibodies in the plasma
- blood group O – has no antigens, but both anti-A and anti-B antibodies in the plasma
- blood group AB – has both A and B antigens, but no antibodies
Blood group O is the most common blood group.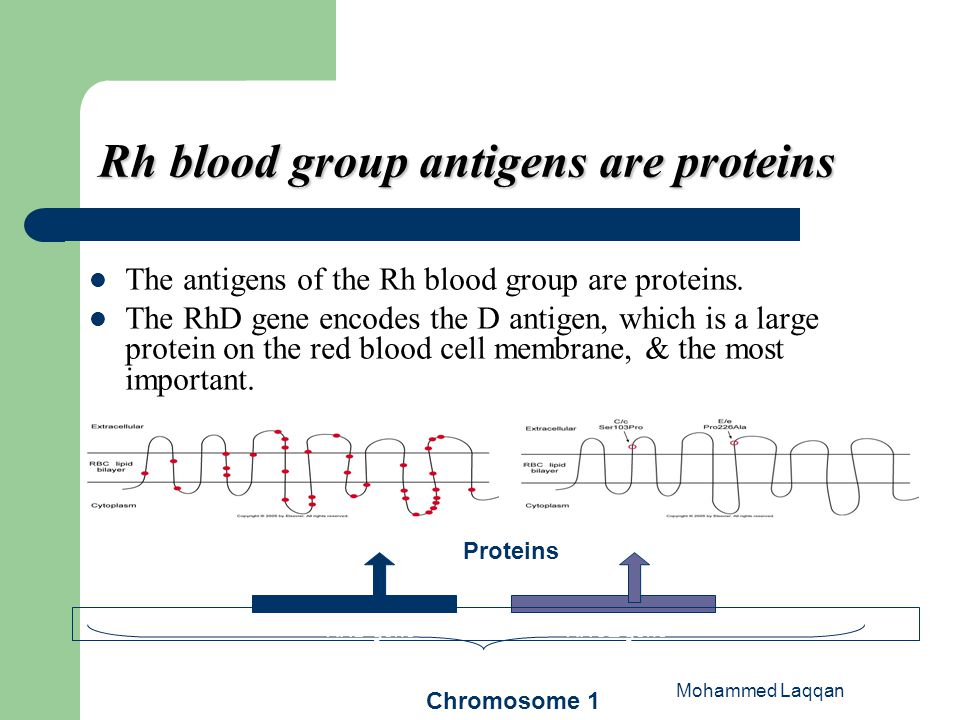 Almost half of the UK population (48%) has blood group O.
Almost half of the UK population (48%) has blood group O.
Receiving blood from the wrong ABO group can be life-threatening. For example, if someone with group B blood is given group A blood, their anti-A antibodies will attack the group A cells.
This is why group A blood must never be given to someone who has group B blood and vice versa.
As group O red blood cells do not have any A or B antigens, it can safely be given to any other group.
The NHS Blood and Transplant (NHSBT) website has more information about the different blood groups.
The Rh system
Red blood cells sometimes have another antigen, a protein known as the RhD antigen. If this is present, your blood group is RhD positive. If it's absent, your blood group is RhD negative.
This means you can be 1 of 8 blood groups:
- A RhD positive (A+)
- A RhD negative (A-)
- B RhD positive (B+)
- B RhD negative (B-)
- O RhD positive (O+)
- O RhD negative (O-)
- AB RhD positive (AB+)
- AB RhD negative (AB-)
About 85% of the UK population is RhD positive (36% of the population has O+, the most common type).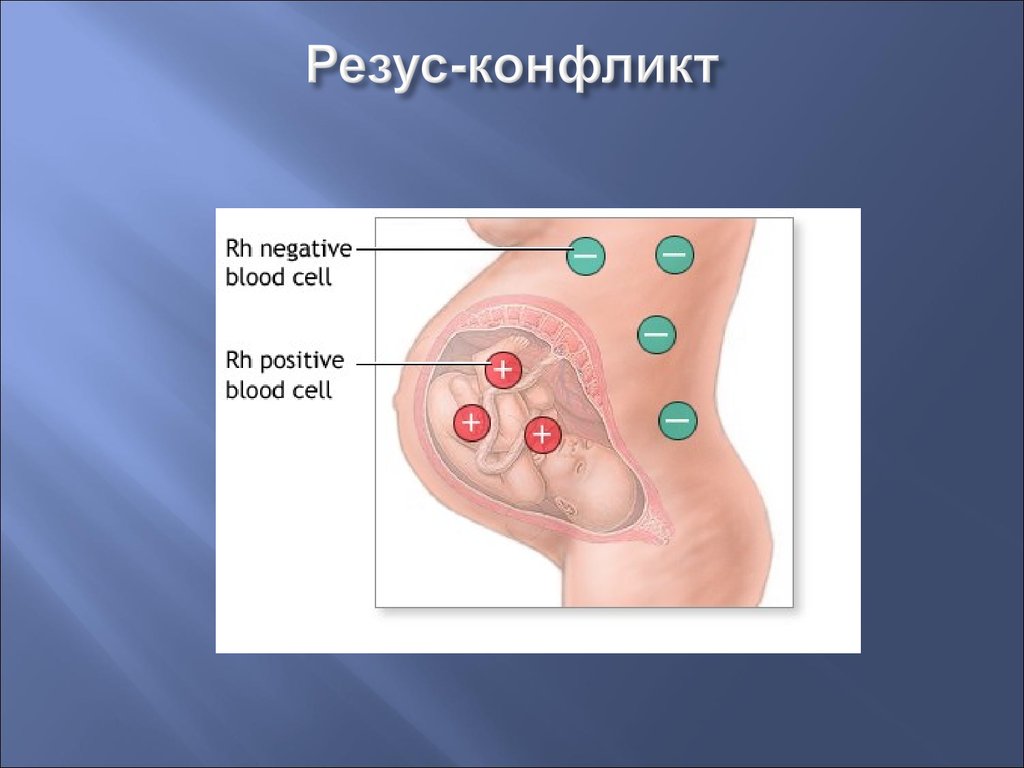
In most cases, O RhD negative blood (O-) can safely be given to anyone. It's often used in medical emergencies when the blood type is not immediately known.
It's safe for most recipients because it does not have any A, B or RhD antigens on the surface of the cells, and is compatible with every other ABO and RhD blood group.
The NHS Blood and Transplant (NHSBT) website has more information about the Rh system.
Blood group test
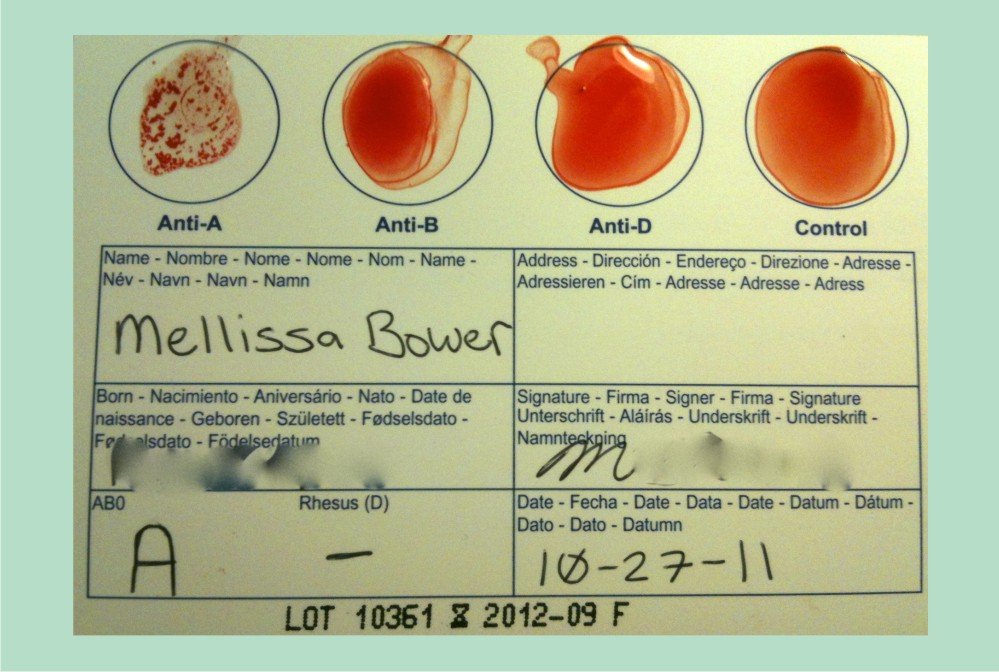
To work out your blood group, your red cells are mixed with different antibody solutions. If, for example, the solution contains anti-B antibodies and you have B antigens on your cells (you're blood group B), it will clump together.
If the blood does not react to any of the anti-A or anti-B antibodies, it's blood group O. A series of tests with different types of antibody can be used to identify your blood group.
If you have a blood transfusion – where blood is taken from one person and given to another – your blood will be tested against a sample of donor cells that contain ABO and RhD antigens. If there's no reaction, donor blood with the same ABO and RhD type can be used.
Pregnancy
Pregnant women are always given a blood group test. This is because if the mother is RhD negative but the child has inherited RhD-positive blood from the father, it could cause complications if left untreated.
RhD-negative women of child-bearing age should always only receive RhD-negative blood.
Read more about Rhesus disease.
Giving blood
Most people are able to give blood, but only 1 in 25 people actually do. You can donate blood if you:
- are fit and healthy
- weigh at least 50kg (7st 12lb)
- are 17-66 years old (or 70 if you've given blood before)
- are over 70 and have given blood in the last 2 years
Read more about who can give blood.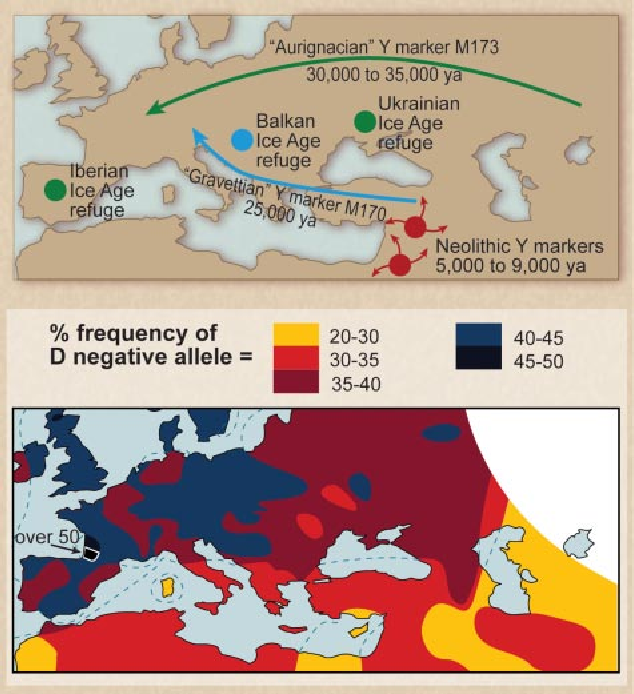
Find your nearest blood donor centre in England and North Wales
You can book an appointment online, or you can call 0300 123 23 23 to book an appointment.
Page last reviewed: 20 April 2020
Next review due: 20 April 2023
Rh factor
Rh factor is a protein that can be found on the surface of human red blood cells. It is of great importance in the management of pregnancy and blood transfusion.
Synonyms Russian
Rh-affiliation, Rh.
Synonyms English
Rh, Rh type, Rh typing, Rh-factor, rhesus factor.
Test method
Agglutination test.
What biomaterial can be used for research?
Venous blood.
How to properly prepare for an examination?
- Eliminate fatty foods for 24 hours before the test.
- Do not smoke for 30 minutes before the test.

General information about the study
Rh factor is a protein found on the surface of red blood cells in some people. The blood of those who have it is called Rh-positive, those who do not - Rh-negative. The presence or absence of this protein is an individual feature, not a pathology. Positive Rh factor occurs in 85% of people, respectively, negative - in 15%.
The Rh factor is of particular importance during pregnancy. If the mother has a positive Rh factor, then her blood will in any case be compatible with the blood of the child, if it is negative, options are possible: in the case when the father of the child also has a negative Rh factor, the mother’s blood will be compatible with the will inherit a negative Rh, but when the father has a positive Rh factor, and the mother has a negative one, with a probability of 50%, incompatibility of the blood of the mother and child may occur - an Rh conflict that threatens with complications.
This happens as follows: when the blood of the fetus enters the mother's bloodstream, antibodies to its positive Rh in her body begin to be produced, since the proteins on the erythrocyte molecules are perceived by the mother's body as something alien. This is not dangerous for a woman, but antibodies through the placenta penetrate the fetal bloodstream, which threatens him with negative consequences: the antibodies “stick” to the fetal red blood cells and can cause them to stick together. This process is called hemolysis. Hemolysis during pregnancy can lead to fetal developmental disorders and, in some cases, to miscarriage, and after birth, to the so-called hemolytic jaundice of the newborn, in which a significant number of red blood cells are destroyed in the baby's blood. At the same time, the skin of the newborn turns yellow, since the breakdown products of red blood cells are colored precisely in yellow. Most often the brain is affected, dropsy may develop. In severe cases, the baby needs a blood transfusion.
What is research used for?
- To determine a possible Rh conflict between mother and fetus. If its high probability is determined, the woman is given injections of a serum containing anti-Rh immunoglobulin, which binds to the fetal red blood cells and "hides" them from the mother's immune system, which prevents the production of antibodies to the fetal red blood cells.
- To find a donor for a safe blood transfusion. It is important to make sure that the donated blood is compatible with the recipient's blood. If the donor blood or its components contain antibodies to the protein contained on the recipient's erythrocytes, a severe transfusion reaction may develop, caused by the destruction of erythrocytes in the vascular bed. Currently, only the transfusion of blood that matches the group and Rh factor of the donor and the recipient is allowed.
When is the examination scheduled?
- During pregnancy, to confirm the woman's blood type, Rh factor and anti-Rh antibodies.
 This information is of great importance in the management of pregnancy.
This information is of great importance in the management of pregnancy. - When donating blood. Most often, a blood transfusion is needed for:
- severe anemia,
- bleeding occurring in a patient during or after surgery,
- severe injuries,
- significant blood loss,
- cancer and side effects of chemotherapy,
- bleeding disorders, in particular hemophilia.
What do the results mean?
If the woman is Rh-negative and positive for anti-Rh antibodies, the blood type and Rh factor of the child's father must be determined. If the father has a negative Rh factor, no further examination is required, if it is positive, further monitoring of the dynamics of the level of anti-Rh antibodies in the mother's blood is carried out. With its increase, a timely decision on therapy should be made.
Important notes
- Rh incompatibility between mother and fetus is currently not an obstacle to the birth of a healthy child.
- During the first pregnancy, Rh conflict usually does not occur, since antibodies are produced slowly and in small quantities. With repeated pregnancy and subsequent, the likelihood of a Rh conflict increases.
Also recommended
- Blood type AB0
- Alloimmune anti-erythrocyte antibodies (including anti-Rhesus), titer
Who orders the examination?
Obstetrician-gynecologist, therapist, general practitioner, hematologist, transfusiologist, surgeon.
About Blood Types - Blood Center
When a doctor talks about your blood type, he usually means two things: your ABO blood type and your Rh (rhesus factor).
A person's blood group is determined by antigens found on his red blood cells. An antigen is a structure on the surface of a cell. If it is foreign to the body, then the human defense system will react to it. Therefore, it is necessary to take into account blood groups when transfusing: the donor's blood group is determined at the Blood Center, and the patient's blood group is determined before transfusion.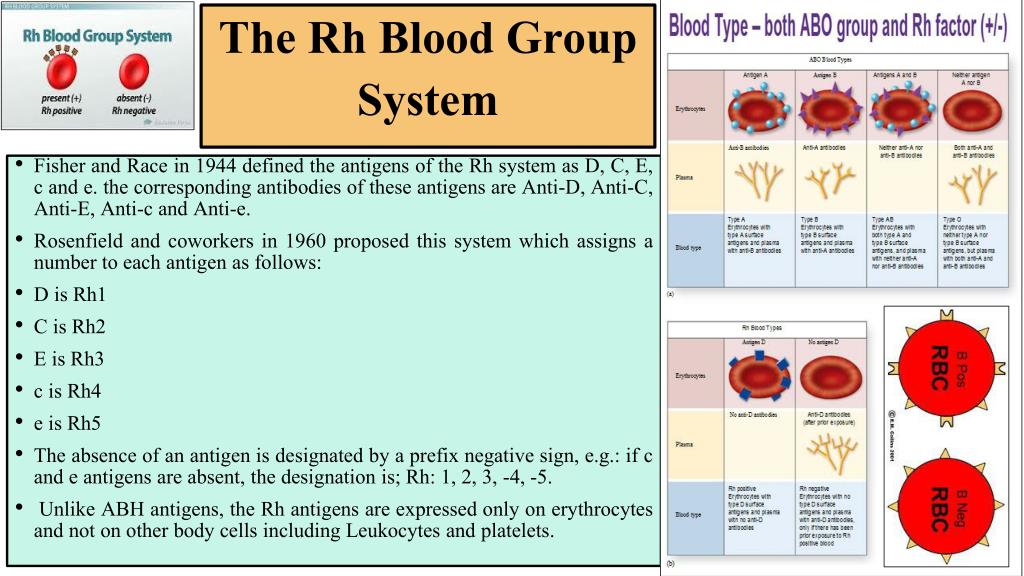
AB0 system
The most important is the ABO blood group system, according to which blood is divided into groups A, B, O and AB. It is determined by two antigens located on the surface of red blood cells:
- group A - only antigen A is present on the surface of erythrocytes
- group B - only antigen B is present on the surface of erythrocytes
- group AB - both A and B antigens are on the surface of erythrocytes
- group O - on the surface of erythrocytes there is neither antigen A nor antigen B.
If a person has blood type A, B or 0, then in his blood plasma there are also antibodies that destroy those antigens that the person himself does not have. Examples: If you have type A blood, then you cannot be transfused with type B blood, because in this case there are antibodies in your blood that fight against B antigens. If you have blood type 0, then your blood contains antibodies that fight like against antigens A and against antigens B.
If a person has blood type AB, then he does not have such antibodies, so he can be transfused with blood of any group. Therefore, the carrier of the AB blood group can be called universal patient.
A carrier of blood group 0 with a negative Rh factor, in turn, is called a universal donor, , since his red blood cells are suitable for all patients.
Rhesus (Rh ) accessory
Rh factor (Rh) can be positive (+) and negative (-). It depends on the presence of the D antigen on the surface of the red blood cells. If the D antigen is present, the person is considered Rh-positive, and if the D antigen is absent, then the person is Rh-negative.
If a person is Rh negative, contact with Rh positive blood (for example, during pregnancy or blood transfusion) may form antibodies. These antibodies can cause pregnancy problems in an Rh-negative woman if she is carrying an Rh-positive baby.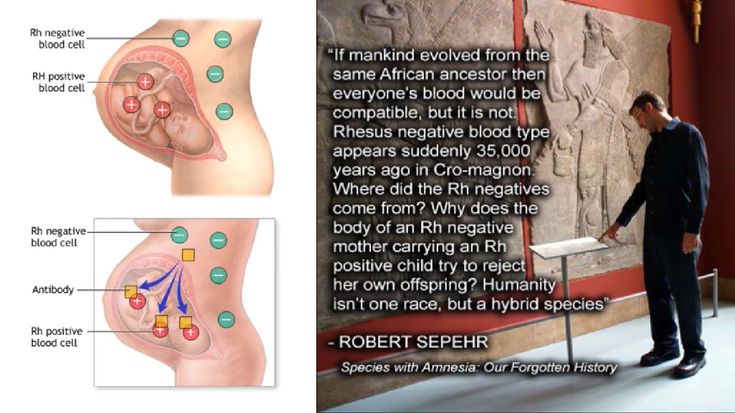
In addition to the ABO and Rh systems, about thirty more blood group systems have been discovered to date. Clinically, the most important of these are the Kell, Kidd and Duffy systems. According to the Kell system, donor blood is also examined.
How is blood type determined?
To determine the blood type, it is mixed with a reagent containing known antibodies.
Three drops of blood taken from one person are applied to the base: the anti-A test reagent is added to one drop, the anti-B test reagent to the other, and the anti-D test reagent to the third, i.e. Rh test reagent. If blood clots form in the first drop, i.e. erythrocytes stick together (agglutination), then the person has antigen A. If erythrocytes do not stick together in another drop, therefore the person does not have antigen B; and if agglutination occurs in the third drop, then this indicates a positive Rh factor. In this example, the donor has blood type A and is Rh positive.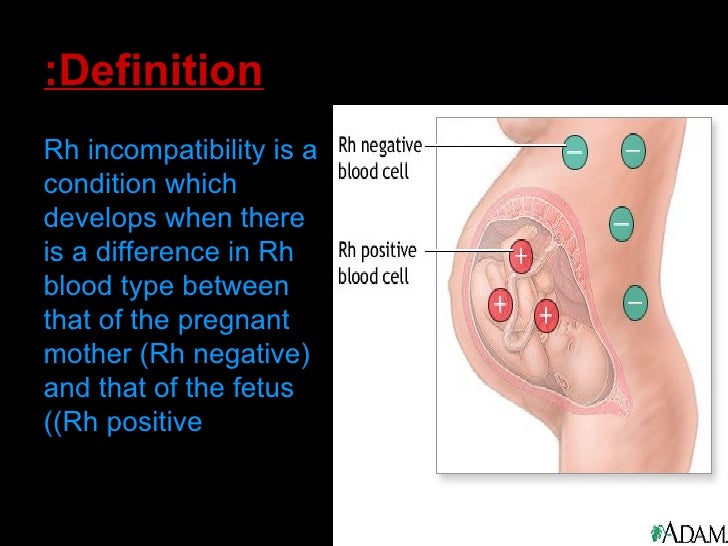
Donor and recipient blood group compatibility is extremely important, otherwise the recipient may have dangerous reactions to the blood transfusion.
Inheritance of blood groups
A person inherits from his father and from his mother to the same extent. Therefore, the hereditary substance has a double structure: one part from the mother and the other from the father. Speaking about the inheritance of blood groups, it must be borne in mind that:
- Most of our genes exist in two copies
- Each parent gives (based on random selection) one of these copies to their children.
- Genes occur in different versions (alleles)
- Some versions of the gene are stronger than others
| ABO system | System Rh | ||||||||||||||||||||||||||||||||||
In the AB0 system, antigens are presented in three versions A, B and 0. Given that the hereditary substance includes two parts, six different combinations can occur:
The stronger part appears, both equally or a combination of them.
Example: The mother has a combination of A0 genes in hereditary substance, and her blood type is A (at the same time, she is a carrier of the blood type 0 gene, and there is a possibility that she will pass it on to her child). The father's blood type has the designation 0, and in his hereditary substance there is a combination of genes 00. Accordingly, he can only pass 0 to the child, i.e. absence of antigens. Thus, their child may have an A (A0) or 0 (00) blood type. | |||||||||||||||||||||||||||||||||||
 In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows:
In the AB0 system, genes A and B are stronger than 0, which affects the formation of the blood group as follows: