Red raised birthmarks
Infantile Hemangiomas: About Strawberry Baby Birthmarks
Hemangiomas are clusters of extra blood vessels on a baby's skin. They may be there when a baby is born, or form within a few weeks or months of birth. Some may look like rubbery, bumpy red "strawberry" patches while others resemble deep bruises. Seeing a hemangioma develop can be worrisome for new parents.
The American Academy of Pediatrics (AAP) guidelines say it's important to identify and begin monitoring infantile hemangiomas right after they appear―when they tend to change most quickly.
While hemangiomas can vary a lot in size, appearance, and placement, they are universally benign (non-cancerous). Most will go away on their own without causing any problems. Some hemangiomas―particularly those on the face or those that are very large―need treatment early to prevent them from interfering with body functions or causing permanent scars. Thankfully, there are excellent treatments available today to can prevent these problems if treated early on.
About Infantile Hemangiomas:
Infantile hemangiomas appear after a baby is born, typically within a month. Roughly 4% to 5% of all infants get them, although they are more common in Caucasians, girls, twins, and preterm or low-birth-weight babies. Infantile hemangiomas typically go through a period of rapid growth, followed by more gradual fading and flattening.
There are different types of infantile hemangiomas:
Superficial hemangiomas have been called "strawberry marks," because they can resemble the surface of berries. They may begin as small white, pink, or red areas on the skin that quickly change into brighter red, raised lesions. Superficial hemangiomas may be focused in one spot or spread out over a larger area.
Deep hemangiomas have a smooth surface and form under the skin. They may have a bluish tint and resemble bruises. Some cause the skin to look swollen.
Mixed hemangiomas are a combination of superficial and deep growths.
Are there other birthmarks like it?
Some of the other marks that can show up on a baby's skin include port wine stains and "stork bites." These also are caused when more blood than usual floods the capillaries under the skin. Port wine stains turn a reddish-purple and are often permanent; like hemangiomas, stork bites usually disappear, but can remain if they're on the back of the neck.
What to do if you think your baby has an infantile hemangioma:
Infantile hemangiomas usually become noticeable by 4 weeks of age. They may start out looking like a tiny bump or scratch. But many then grow especially fast between 5 and 7 weeks old. If you think your baby might have a hemangioma, it's best to contact your baby's pediatrician right away. He or she probably will want to see your baby within a short timeframe. According to the AAP, the best "window of opportunity" to be evaluated and start treatment if needed is about 1 month of age.
Your pediatrician will want to know:
Size: Is the hemangioma small (3/4" or less across) or larger?
Location: Is it located on the face or in the diaper area, or in a different area?
Number: Is there one or more than one? If more than one, how many?
If your doctor can't see you in the office right away, they may ask you to send photos or recommend a telemedicine visit to have a look without delay.
What to expect next:
It's important to continue monitoring the hemangioma until it stops growing.
Superficial hemangiomas typically reach their full size by 5 months of age, although
deep hemangiomas sometimes keep growing a while longer. In some cases, your pediatrician may give a referral to an infantile hemangioma specialist with expertise in
pediatric dermatology, hematology-oncology, otolaryngology, or
plastic surgery.
By the time a baby is 6-18 months old, most hemangiomas begin to slowly improve. In a process called "involution," the hemangioma will become less red and more grey or whitish and gradually flatten and shrink from the center outward.
Each case is different. Most hemangiomas have finished or almost finished flattening and shrinking by 4 to 5 years of age. |
When does a hemangioma need to be treated?
Whether a hemangioma needs treatment depends on the age of the baby, where the hemangioma is located and how fast it is growing, whether it becomes sore or scabby, and the risk of it causing medical complications with a child's health and well-being.
There are 3 main reasons for treatment:
Medical problems. In rare cases and depending where they are located and how fast they are growing, hemangioma may begin to interfere with vital functions.
 Hemangiomas near the child's eyes, nose or mouth, for example, can affect the child's ability to see, eat, breath or hear well. In rare cases, hemangiomas grow inside the body, which may need to be monitored with imaging tests.
Hemangiomas near the child's eyes, nose or mouth, for example, can affect the child's ability to see, eat, breath or hear well. In rare cases, hemangiomas grow inside the body, which may need to be monitored with imaging tests.Skin breakdown. Sometimes, skin on the hemangioma's surface breaks down and becomes an open sore (called an ulcer) that could lead to bleeding, infection, or scarring.
Permanent skin changes. Changes in the skin's texture or color can remain even after the hemangioma has gone away. This can be a concern, especially for hemangiomas on the child's face. Large hemangiomas on facial features such as the nose or lip can also distort growth.
What kinds of treatments are available for hemangiomas?
If a baby's hemangioma risks causing problems, medications can be applied directly to the skin or taken by mouth. The goal is to keep them from getting any bigger during their period of rapid growth, or to make them shrink more quickly. Laser procedures or surgery may be an option in some cases, although it generally is avoided during early infancy to avoid increased anesthesia risks.
Laser procedures or surgery may be an option in some cases, although it generally is avoided during early infancy to avoid increased anesthesia risks.
Systemic treatments
Propranolol, a beta blocker medication used for many years to treat high blood pressure, is now commonly given by mouth as an effective treatment for problem hemangiomas. To avoid a growth rebound, the pediatrician may recommend therapy continue until your child's first birthday. The drug must be used with close observation by your healthcare provider to watch for possible side effects and complications.
Oral steroids have been largely replaced by safer and more effective options, but are still used in select cases, determined by the healthcare provider.
Localized treatments
Topical medications applied directly on the skin may be used for small, superficial hemangiomas. Prescription creams or ointments containing beta-blockers are the most effective topical treatment option to help stop growth and sometimes shrink and fade hemangiomas.
 In some cases, steroid creams may be prescribed for smaller, thinner hemangiomas.
In some cases, steroid creams may be prescribed for smaller, thinner hemangiomas.Steroid injections can be given directly into the hemangioma to help slow its growth. This works best for smaller, localized hemangiomas.
Other treatments
Surgery is usually only considered for smaller hemangiomas in areas where they may cause problems, or for small hemangiomas with broken skin. Because surgery will always leave a scar itself--and because most hemangiomas get better with time--early surgery is only recommended for a small minority of cases. Surgery can also repair extra skin or scars left by a hemangioma, but usually is delayed until a child is between 3 and 5 years old.
Laser treatment may be helpful in some cases to stop bleeding or to help heal hemangiomas with open sores (ulcers). They can also help to remove some of the redness or texture changes that may be left behind after the hemangioma improves.

Remember:
Contact your pediatrician if you notice anything developing on your baby's skin. Your baby's first few well-child visits are also a great time to bring it up. Few hemangiomas cause any trouble, and most go away on their own. But prompt evaluation, monitoring and treatment, when needed, can help ensure problem hemangiomas have as little impact as possible on your child.
Additional Information:
Baby Birthmarks & Rashes
Management of Infantile Hemangiomas (AAP Clinical Practice Guideline)
HemangiomaEducation.org
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Birthmarks - red Information | Mount Sinai
Strawberry mark; Vascular skin changes; Angioma cavernosum; Capillary hemangioma; Hemangioma simplex
Red birthmarks are skin markings created by blood vessels close to the skin surface. They develop before or shortly after birth.
They develop before or shortly after birth.
A stork bite is a vascular lesion quite common in newborns consisting of one or more pale red patches of skin. Most often stork bites appear on the forehead, eyelids, tip of the nose, upper lip or back of the neck. They are usually gone within 18 months of birth.
Hemangiomas are tumors made up of dilated blood vessels that usually appear shortly after birth, although they may be present at birth. Hemangiomas on the face can be disfiguring and may interfere with visual development or cause obstruction of the airway.
Hemangiomas on the face can be disfiguring and may interfere with visual development or cause obstruction of the airway.
This child has a juvenile hemangioma (strawberry hemangioma) on the chin. These may begin as flat, red spots and later become larger and elevated. Juvenile hemangiomas often go away (involute) spontaneously.
Causes
There are two main categories of birthmarks:
- Red birthmarks are made up of blood vessels close to the skin surface. These are called vascular birthmarks.
- Pigmented birthmarks are areas in which the color of the birthmark is different from the color of the rest of the skin.
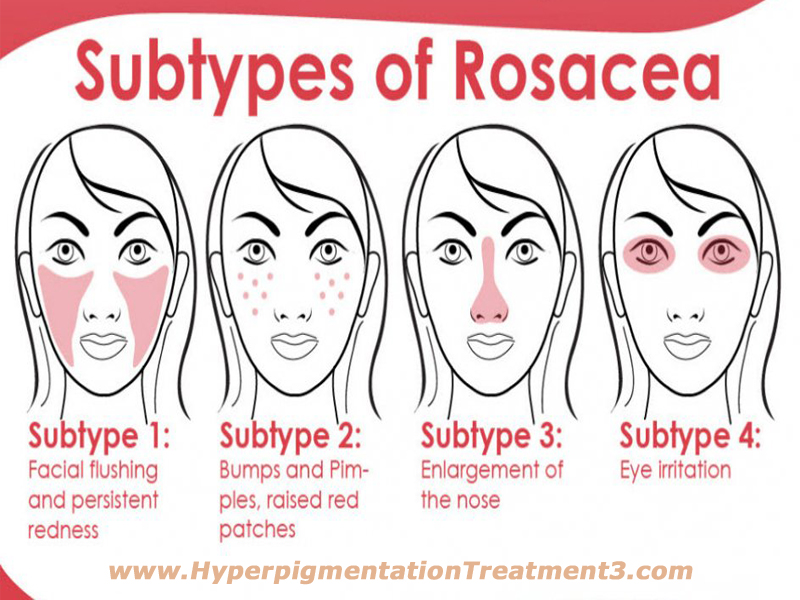
Hemangiomas are a common type of vascular birthmark. Their cause is unknown. Their color is caused by the growth of blood vessels at the site. Different kinds of hemangiomas include:
- Strawberry hemangiomas (strawberry mark, nevus vascularis, capillary hemangioma, hemangioma simplex) may develop several weeks after birth.
 They may appear anywhere on the body, but are most often found on the neck and face. These areas consist of small blood vessels that are very close together.
They may appear anywhere on the body, but are most often found on the neck and face. These areas consist of small blood vessels that are very close together. - Cavernous hemangiomas (angioma cavernosum, cavernoma) are similar to strawberry hemangiomas, but they are deeper and may appear as a red-blue spongy area of tissue filled with blood.
- Salmon patches (stork bites) are very common. Up to half of all newborns have them. They are small, pink, flat spots made up of small blood vessels that can be seen through the skin. They are most common on the forehead, eyelids, upper lip, between the eyebrows, and on the back of the neck. Salmon patches may be more noticeable when an infant cries or during temperature changes.
- Port-wine stains are flat hemangiomas made of expanded tiny blood vessels (capillaries). Port-wine stains on the face may be associated with Sturge-Weber syndrome. They are most often located on the face. Their size varies from very small to over half of the body's surface.
Symptoms
The main symptoms of birthmarks include:
- Marks on the skin that look like blood vessels
- Skin rash or lesion that is red
Exams and Tests
A health care provider should examine all birthmarks. Diagnosis is based on how the birthmark looks.
Tests to confirm deeper birthmarks include:
- Skin biopsy
- CT scan
- MRI of the area
Treatment
Many strawberry hemangiomas, cavernous hemangiomas, and salmon patches are temporary and do not need treatment.
Port-wine stains may not need treatment unless they:
- Affect your appearance
- Cause emotional distress
- Are painful
- Change in size, shape, or color
Most permanent birthmarks are not treated before a child reaches school age or the birthmark is causing symptoms. Port-wine stains on the face are an exception. They should be treated at a young age to prevent emotional and social problems. Laser surgery can be used to treat them.
Concealing cosmetics may hide permanent birthmarks.
Oral or injected cortisone may reduce the size of a hemangioma that is growing quickly and affecting vision or vital organs.
Other treatments for red birthmarks include:
- Beta-blocker medicines
- Freezing (cryotherapy)
- Laser surgery
- Surgical removal
Outlook (Prognosis)
Birthmarks rarely cause problems, other than changes in appearance. Many birthmarks go away on their own by the time a child reaches school age, but some are permanent. The following development patterns are typical for the different types of birthmarks:
Many birthmarks go away on their own by the time a child reaches school age, but some are permanent. The following development patterns are typical for the different types of birthmarks:
- Strawberry hemangiomas usually grow quickly and stay the same size. Then they go away. Most strawberry hemangiomas are gone by the time a child is 9 years old. However, there may be a slight change in color or puckering of the skin where the birthmark was.
- Some cavernous hemangiomas go away on their own, usually as a child is about school age.
- Salmon patches often fade as the infant grows. Patches on the back of the neck may not disappear. They usually are not visible as hair grows.
- Port-wine stains are often permanent.
Possible Complications
The following complications can occur from birthmarks:
- Emotional distress because of appearance
- Discomfort or bleeding from vascular birthmarks (occasional)
- Interference with vision or bodily functions
- Scarring or complications after surgery to remove them
When to Contact a Medical Professional
Have your provider look at all birthmarks.
Prevention
There is no known way to prevent birthmarks.
Dinulos JGH. Vascular tumors and malformations. In: Dinulos JGH, ed. Habif's Clinical Dermatology. 7th ed. Philadelphia, PA: Elsevier; 2021:chap 23.
Folpe AL, Kozakewich HP. Benign vascular tumors and malformations. In: Goldblum JR, Folpe AL, Weiss SW, eds. Enzinger and Weiss's Soft Tissue Tumors. 7th ed. Philadelphia, PA: Elsevier; 2020:chap 20.
Patterson JW. Vascular tumors. In: Patterson JW, ed..jpg) Weedon's Skin Pathology. 5th ed. Philadelphia, PA: Elsevier Limited; 2021:chap 39.
Weedon's Skin Pathology. 5th ed. Philadelphia, PA: Elsevier Limited; 2021:chap 39.
Last reviewed on: 11/10/2020
Reviewed by: Ramin Fathi, MD, FAAD, Director, Phoenix Surgical Dermatology Group, Phoenix, AZ. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Why red moles appear on the body. How to get rid of them.
Moles are benign skin growths. Red moles (angiomas) are the result of malfunctioning subcutaneous capillaries. Although the vast majority of them are not dangerous to health, their unexpected appearance, strange color and unusual shape often frighten people. Ignorance and misunderstanding of the problem can lead to sad consequences.
To avoid this, let's talk more about red moles and dot the i's. nine0003
The etiology of red moles has not yet been studied. No one can name the exact reasons why they appear on the skin. However, there is a widespread belief that angiomas occur as a result of a malfunction of the subcutaneous capillaries.
This assumption is partly proved by the structure of the red mole. Under a microscope, a neoplasm is a mass of glued or intertwined blood vessels that are localized in the upper layers of the skin, or on its surface. This is probably why red moles most often occur in early childhood. nine0003
The child's circulatory system changes periodically. Vessels grow, develop and often form entire networks of angiomas on the skin. Most often on the face.
In adulthood, red moles appear less frequently. They occur suddenly on any part of the body as a reaction to an external or internal stimulus. In particular, the following can provoke the appearance and growth of angiomas:
- prolonged insolation;
- hormonal disruptions;
- violation of microcirculation in skin cells; nine0016
- age-related changes in the body.
What do red moles look like?
Angiomas are small neoplasms in the red color spectrum (from pale pink to brown). They do not hurt and are not felt in any way by the wearer under normal conditions. Below are the possible types of red moles:
Are red moles dangerous?
The short answer is no. Not dangerous. Angiomas do not threaten human life and health. Cases when these neoplasms degenerate into cancer are extremely rare and are usually associated with some genetic prerequisites. Or with exposure to carcinogens. nine0003
But, you should consult a doctor if:
- the red mole itches or grows;
- you damaged (or tore off) a red mole;
- too many angiomas;
- they bleed and ulcerate.
Why it matters.
Itching, rapid growth, scaling, bleeding and ulceration are not typical behaviors for angioma. Therefore, it is possible that malignancy processes have started in the neoplasm, or it was initially malignant. nine0003
Damage to a red mole is usually accompanied by profuse bleeding. It is fraught. If you have torn off a red mole, you can find out how to provide first aid in our separate article "What to do if you have damaged a mole?". And after all the measures taken, visit at least a dermatologist (for greater persuasiveness, read about "How dangerous is a damaged mole?").
And after all the measures taken, visit at least a dermatologist (for greater persuasiveness, read about "How dangerous is a damaged mole?").
Removal of red moles
Angiomas respond well to treatment. They can be removed. But it is better to do this in a specialized institution (preferably in a clinic, in extreme cases, in a beauty parlor). By no means at home! nine0003
Removal of any growths at home is dangerous. Acidic products that are used for these purposes contain carcinogens. Carcinogens can provoke the development of malignant pathology, as well as disrupt the integrity of tissues. A scar is the most harmless thing that can be obtained by resorting to such methods of removing red moles.
How to remove red moles?
Laser. Or any other safe method. It is better to avoid direct surgical intervention and strive for the most bloodless and non-contact methods. nine0003
Why?
Non-contact ways to remove tumors are safe. You do not risk infection during the procedure. In addition, the rehabilitation period is significantly reduced - the treated area heals quickly and, as a rule, without consequences.
You do not risk infection during the procedure. In addition, the rehabilitation period is significantly reduced - the treated area heals quickly and, as a rule, without consequences.
If we are talking about red moles, then we recommend laser removal, preferably CO2 laser (if the neoplasm is large or deeply located). If the angiomas are small, then an erbium or so-called “cold” laser is suitable for removal. The difference is only in power and depth of impact. nine0003
Read more about how CO2 laser works in the article "Carbon dioxide laser as the most common laser in cosmetology.".
In conclusion
In conclusion, I would like to add that angiomas or red moles should not be frightened. Yes, they appear suddenly and also suddenly disappear. They can appear on the chest, face, arms and other parts of the body. Aesthetic discomfort is perhaps the only reason why patients decide to have it removed. But often, it is enough to wait a short time, and the neoplasm will disappear by itself. nine0003
nine0003
Most importantly, don't try to self-medicate. Is it dangerous!
Red moles: treatment, causes.
Contents
Causes of red moles
Locations
Types and classification
Are red moles dangerous?
Red moles in children
Red moles during pregnancy
Should red moles be removed?
Diagnostics
Methods for removing red moles
This type of growth is usually not a cause for concern. Provided they do not bleed or change in size, shape or color. Otherwise, it would be better to consult a doctor. Any changes in the mole can be the first signals of skin cancer, provided that there was no mechanical damage, from which they can also bleed and itch, which can lead to wrong conclusions.
Causes of red moles
The exact reason why red moles appeared on the body is unknown, it may be a predisposition due to a genetic factor. But there are other reasons too:
- pregnancy;
- exposure to chemicals;
- certain diseases, including infectious ones;
- unsuitable climate (too hot or cold)
- mechanical damage to the skin, such as bites or cuts, in which pieces of skin are not completely torn off.
 nine0016
nine0016
Their manifestations at a more mature age are also possible, this is due to a gradual decrease in immunity. Neoplasms appear in 75% of the population over the age of 60 years.
It is impossible to somehow influence the appearance or non-appearance of red moles on the body, since they are inherent in us at the genetic level, if one of the parents had a lot of them, then the children will have a similar situation, and even identical maps of the location of nevi are possible. nine0003
Locations
An increase in the growth of moles is observed in people aged 0 to 20 years, and then from 45 years and older. The rest of the time they appear, but not as actively as in the first and last phase of life. Typically, red moles occur on the upper body, arms, legs, and shoulders. Also their favorite place is the head, feet, hands. They can be located throughout the body, and it is impossible to predict their subsequent locations. The red color is given to them by the accumulation of small blood vessels at the base, which feed them with blood. nine0003
The red color is given to them by the accumulation of small blood vessels at the base, which feed them with blood. nine0003
Types and classification
Moles have two main types:
- Pigmented. These include flat, often brown, nevi.
- Vascular, which are formed from changes in the structure of blood vessels.
They are also:
- Congenital - dividing by size: small, medium and large.
- Acquired, divided into three types depending on the presence of melanocytes in the layers of the epidermis. nine0016
- Hanging, they are also called papillomas.
There are invisible nevi, which appear over time changing color. Also wandering, which change their location, appearing in one place or another. It is advisable to follow the map of the location of your moles.
Are red moles dangerous?
Signs to look out for if small red moles appear: nine0003
- Colour.
 If it is uneven and begins to change, this is a reason to visit a doctor.
If it is uneven and begins to change, this is a reason to visit a doctor. - Inflammation around the growth, that is, redness in the form of a halo around the mole.
- An increase in the size of a mole or its induration.
- The appearance of cracks and ulcers on the body of a mole.
- Loss of hair if it has grown from a mole.
- Itching, burning or tingling at the site of the mole. nine0015 Changing the edges of the nevus also indicates that it is time to visit a specialist.
An accurate diagnosis can be made by a dermatologist or an oncologist, who can and should be contacted for help. Nevi are not dangerous as long as they are in a stable condition, in which case you can wait with your doctor.
Red moles in children
In most people, the main part of moles appears in the first 20 years of life, then the formation of moles (nevi) subsides. They also have the ability to sometimes disappear on their own, and this happens due to the fact that the blood vessels that feed the mole dry out or become clogged. One in 100 newborns is already born with small red moles on the body, and they are considered more prone to changes and the transition to melanoma. This neoplasm of red color, slightly rising above the surface of the skin, is called the Spitz nevus. nine0028
One in 100 newborns is already born with small red moles on the body, and they are considered more prone to changes and the transition to melanoma. This neoplasm of red color, slightly rising above the surface of the skin, is called the Spitz nevus. nine0028
Children can also be born with large blue spots on their backs, they are called Mongolian and are most often found in children with Asian roots. Any moles are often injured, especially in childhood. This can cause complications, so it is advisable to occasionally see a doctor, and also try to protect children from such injuries.
Red moles during pregnancy
During pregnancy, the female body is undergoing hormonal changes, and at this time new nevi may appear, or old ones may grow. In 85%, this may be the norm and the body's normal reaction to pregnancy. Such moles are most likely harmless. In the remaining 15%, it is still better to consult a specialist and find out why red moles appear on the body.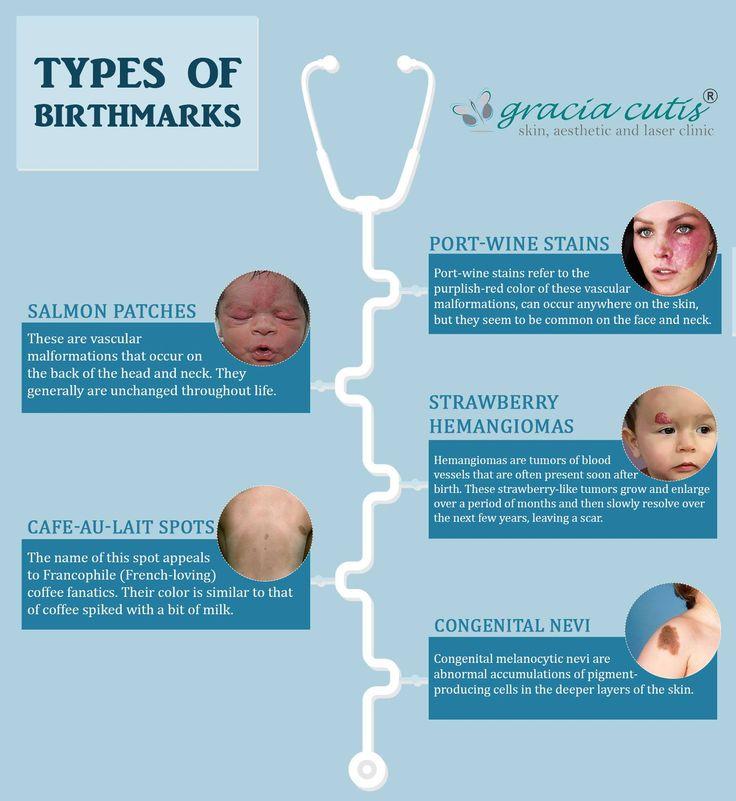 nine0003
nine0003
Should red moles be removed?
Not only possible, but necessary. If the hemangioma increases in size, changes shape or color - this, of course, is a direct indication to get an appointment with an oncologist as soon as possible for further research, if necessary, and removal. Of course, not by artisanal or folk methods, but with the help of modern specialists. If the mole behaves calmly enough and does not change its shape and color, then most likely you should not be afraid and you can wait a bit with the removal of moles. nine0003
Diagnostics
In medicine, there is a general method for diagnosing neoplasms on the skin. These include a primary examination and a record of all patient complaints (anamnesis). If a malignant tumor is suspected, an MRI or x-ray is prescribed. All the data obtained are analyzed and conclusions are drawn, on the basis of which a preliminary diagnosis is made. The main and final point in the diagnosis is the histological method (biopsy). It is a microscopic sampling of tissue from the body of a mole, and is done in order to identify cell pathology in the neoplasm. nine0003
It is a microscopic sampling of tissue from the body of a mole, and is done in order to identify cell pathology in the neoplasm. nine0003
Methods for removing red moles
If the mole does not bother you and is not located in places of increased risk, that is, on the hands, feet or head and back, then it may well not be removed.
If the hemangioma worries, then it can only be removed by specialists, a dermatologist or an oncologist. You should not take risks by removing a nevus from a cosmetologist and endangering the growth of an incorrectly removed hemangioma or the risk of infection.
There are several common procedures for removing them. nine0003
- Electrocautery. The nevus is burned with an electric current applied with a small tool. The grounding block will be placed somewhere so that the rest of the body is not exposed to electricity.
- Cryosurgery. The mole is frozen with liquid nitrogen. It is destroyed by intense cold. Liquid nitrogen is sprayed within 10 seconds, the problem is solved within one session.