How does autism affect a child development
Autism Spectrum Disorder (ASD) - Developmental and Behavioral Pediatrics - Golisano Children's Hospital
Golisano Children's Hospital / / / ASD
What is autism spectrum disorder in children?
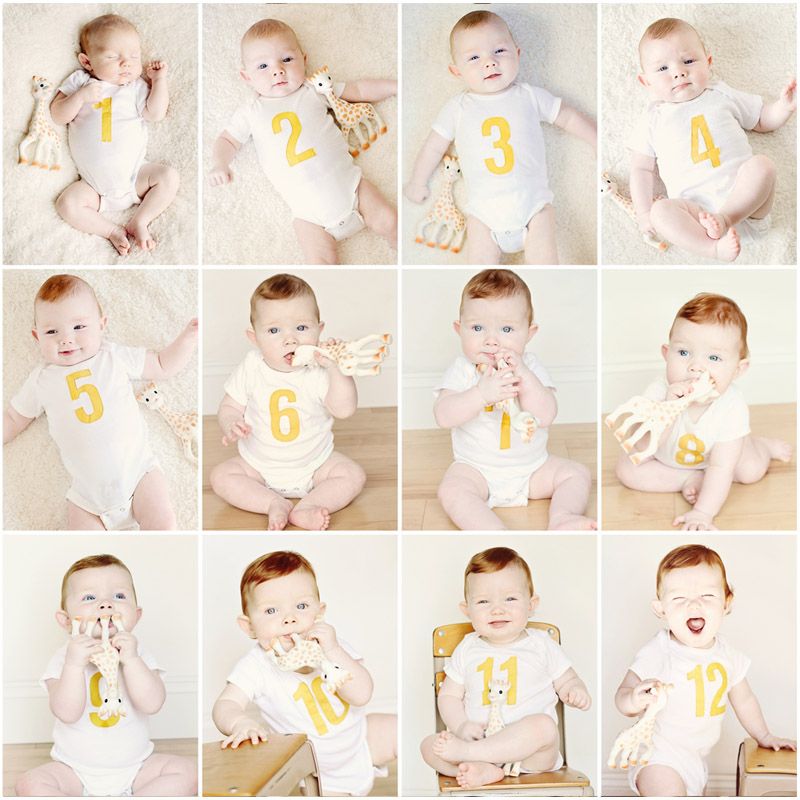
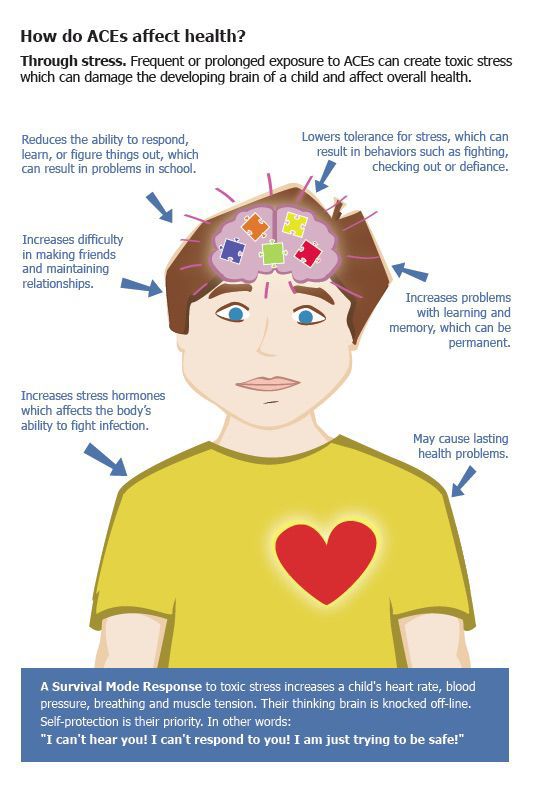
Autism spectrum disorder (ASD) is a problem that affects a child’s nervous system and growth and development. It often shows up during a child’s first 3 years of life.
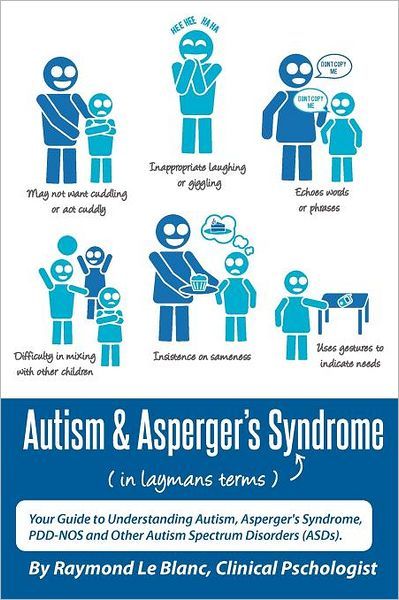
Some children with ASD seem to live in their own world. They are not interested in other children and lack social awareness. A child with ASD focuses on following a routine that may include normal behaviors. A child with the disorder also often has problems communicating with others. He or she may not start speaking as soon as other children. He or she may not want to make eye contact with other people.
ASD can keep a child from developing social skills. This is in part because a child with ASD may not be able to understand facial expressions or emotions in other people. A child with ASD may:
A child with ASD may also repeat movements. This might be flapping his or her hands or rocking. He or she may also have abnormal attachments to objects. But a child with ASD may also do certain mental tasks very well. For example, the child may be able to count or measure better than other children. Children with ASD may do well in art or music, or be able to remember certain things very well.
What causes ASD in a child?
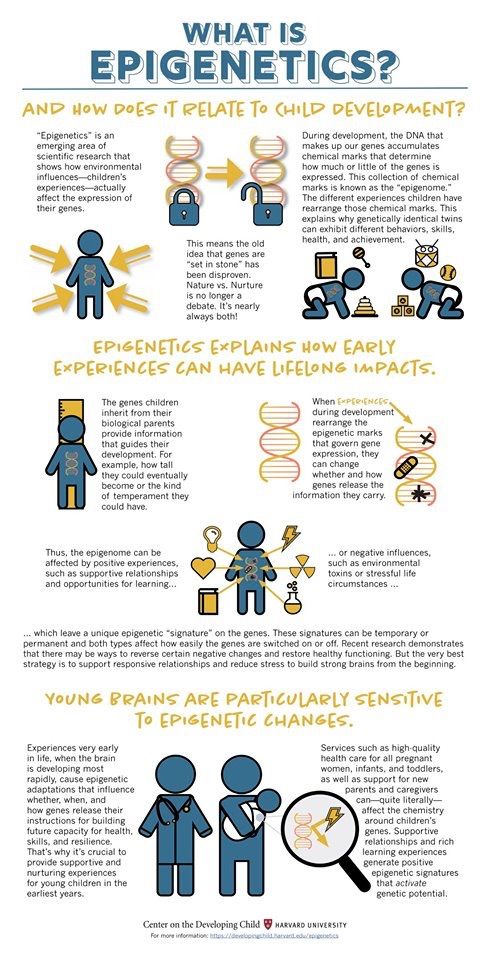
Experts don’t know what causes ASD. It may be caused by certain genes. A child with ASD may also have problems with their brain structure or with certain chemicals in the brain. Researchers do know that ASD is not caused by what a parent does to raise a child. It is also not linked to any vaccines given to children.
Much less often, other things that may cause ASD include:
-
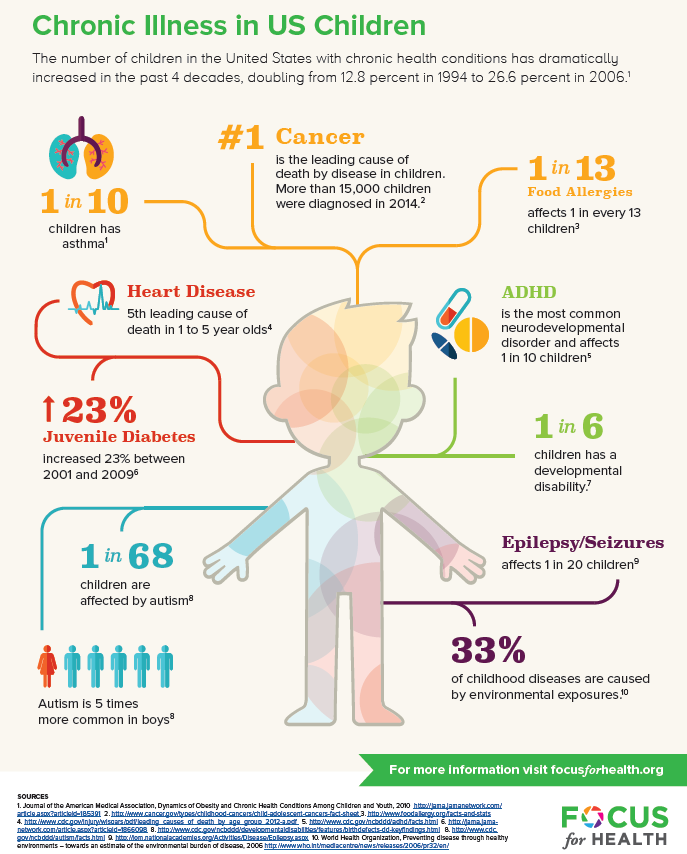
Being exposed to toxins in the environment before or after birth
-
Severe infections such as meningitis or encephalitis that result in brain damage
-
Problems during delivery
-
Infections before birth
Which children are at risk for ASD?
ASD occurs in all racial, ethnic, and socioeconomic groups.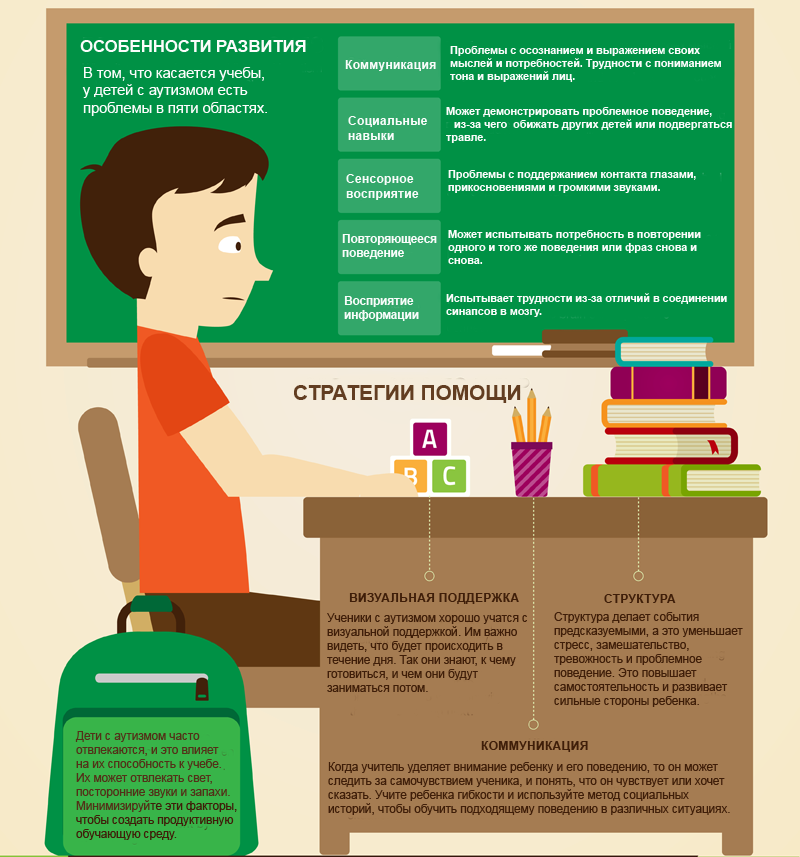 The disorder happens much more often in boys than girls. Four to 5 times as many boys as girls have ASD.
The disorder happens much more often in boys than girls. Four to 5 times as many boys as girls have ASD.
Certain gene disorders that run in families can raise a child’s risk for ASD. These include:
Your child may need genetic testing to help find out if another problem has contributed. The testing is done by a medical geneticist. This is a healthcare provider with special training in genetics and inherited problems. They can let you know the chances of having another child with the gene problem. For example, PKU carries a 1 in 4 chance of happening in another pregnancy. For tuberous sclerosis, the chances are 1 in 2.
Even when no gene problem is found, you are at a slightly higher chance of having another child with ASD. Experts think this is because several genes from both parents may act together to cause ASD.
What are the symptoms of ASD in a child?
Each child may have different symptoms. Below are the most common symptoms of ASD.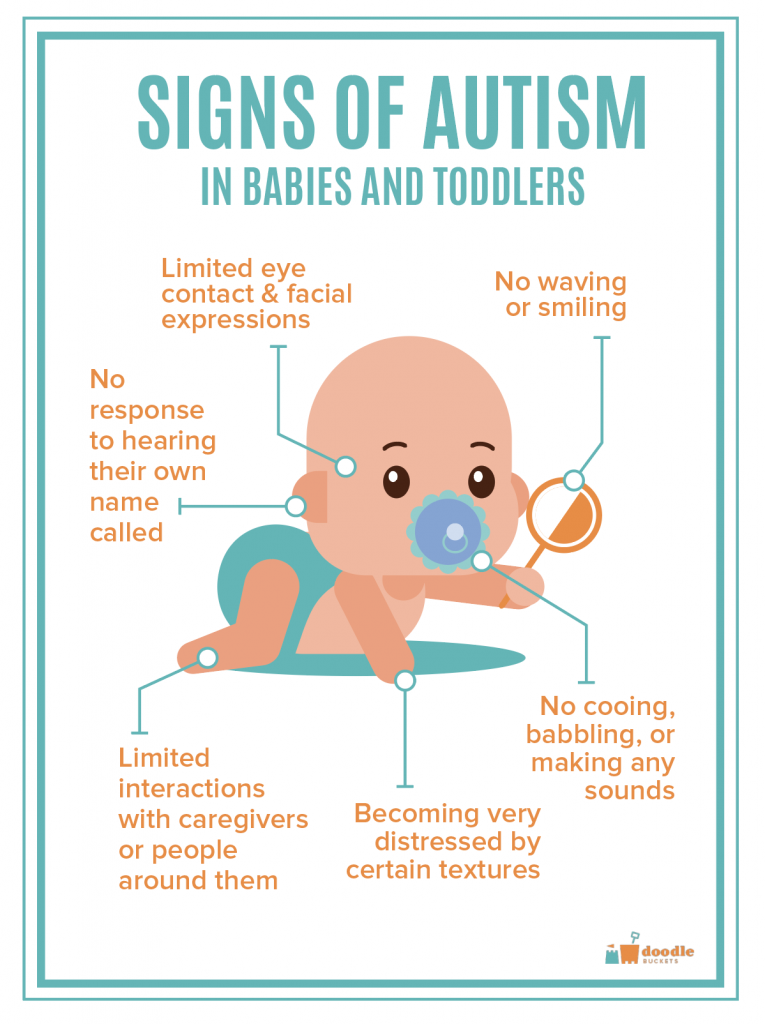
Social symptoms
Communication symptoms
-
Does not communicate well with others
-
Starts speaking at a later age than other children or doesn’t speak at all
-
When the child is able to speak, doesn’t use speech in social settings
-
Repeats words or phrases (echolalia) or repeats parts of dialogue from TV or movies
Behavior symptoms
-
Does repeated movements, such as rocking or flapping fingers or hands
-
May be too sensitive or less sensitive to certain things around him or her, such as lights, sounds, touch, or taste
-
Has rituals
-
Needs routines
The symptoms of ASD may look like other health conditions. Make sure your child sees their healthcare provider for a diagnosis.
How is ASD diagnosed in a child?
No single medical test can diagnose ASD.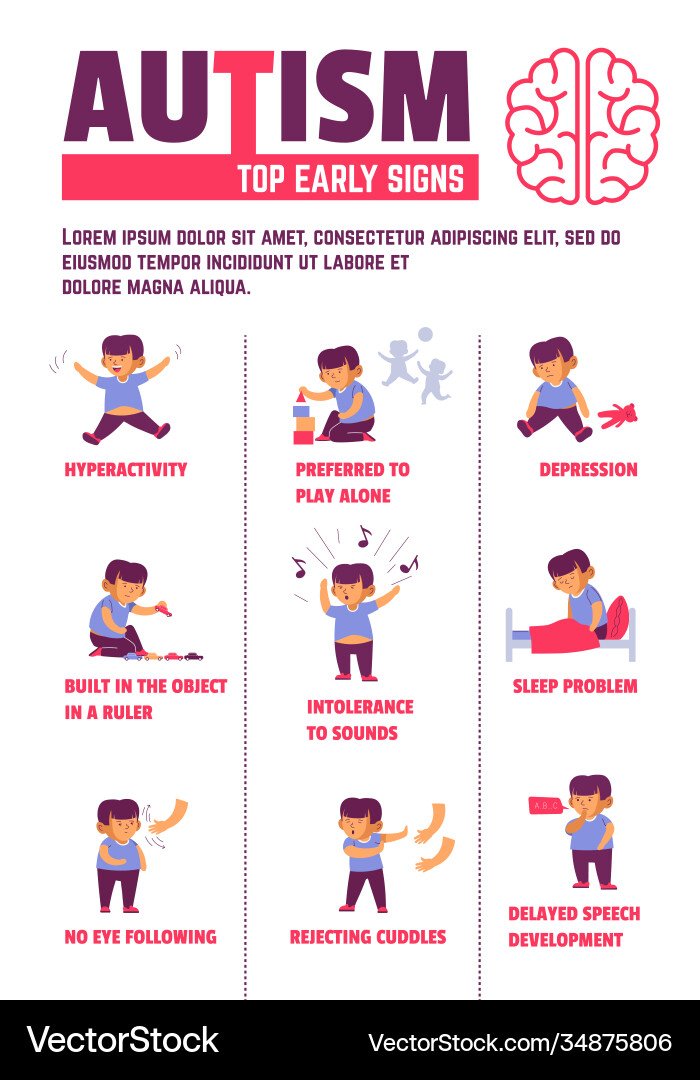 Healthcare providers use certain guidelines to help diagnose ASD in children before age 2. The guidelines can help diagnose the disorder early. Children diagnosed with ASD early can be treated right away.
Healthcare providers use certain guidelines to help diagnose ASD in children before age 2. The guidelines can help diagnose the disorder early. Children diagnosed with ASD early can be treated right away.
The guidelines say that all children should be screened for ASD and other development disorders before age 2. The screening is done at well-child checkups. Children who have symptoms of development or behavior disorders will need to get more testing for ASD.
Healthcare providers look for the following problems during well-child visits before age 2:
-
No babbling, pointing, or gesturing by age 12 months
-
No single words spoken by age 16 months
-
No 2-word phrases by age 24 months, just repeating words or sounds of others
-
Loss of any language or social skills at any age
-
No eye contact at 3 to 4 months
If a child has any of the above problems, the healthcare provider will do more screening.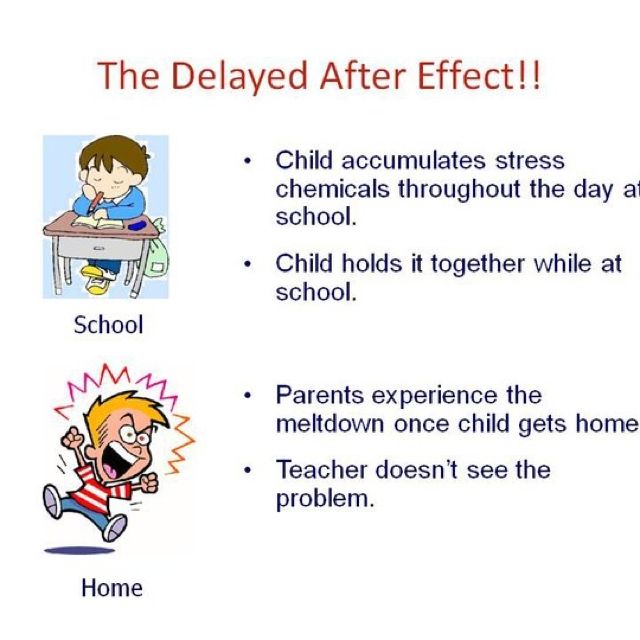 This will help show if your child has ASD or another developmental disorder. Your child may need to see a healthcare provider with special training to diagnose and treat ASD. Your child may also need these screening tests:
This will help show if your child has ASD or another developmental disorder. Your child may need to see a healthcare provider with special training to diagnose and treat ASD. Your child may also need these screening tests:
-
Nervous system exam
-
Imaging tests such as CT scan, MRI, or PET scan
-
Mental health tests
-
Genetic tests to look for gene problems that cause ASD or other developmental disorders
How is ASD treated in a child?
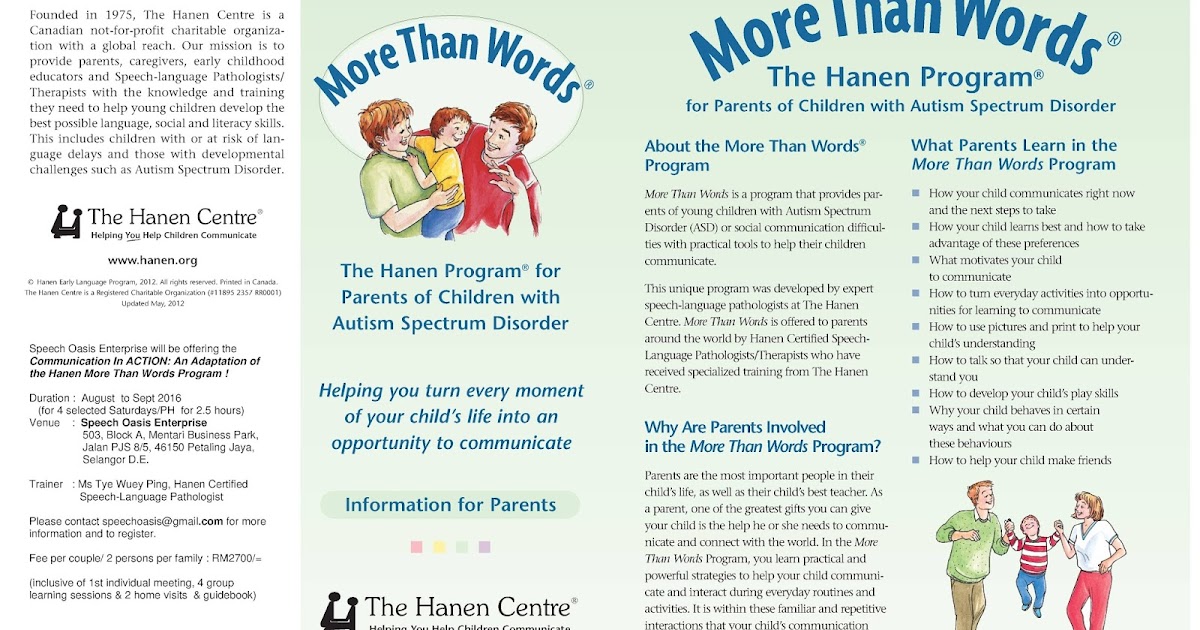
Each child with ASD needs their own special treatment program. This is because children with ASD can vary a lot in how much help they need. Programs that work best are those that are started as early as possible and include the parents.
Treatment for ASD includes:
-
Behavior change programs. These programs teach social skills, movement skills, and thinking (cognitive) skills.
 They can help a child change problem behaviors.
They can help a child change problem behaviors. -
Special education programs. These focus on social skills, speech, language, self-care, and job skills.
-
Medicine. Some children need medicine to help treat some of the symptoms of ASD.
Your child and your family may also need to see a mental health provider. This provider can give you parent counseling, social skills training, and one-on-one therapy. This provider can also help you find the treatment programs that are best for your child.
How can I help prevent ASD in my child?
Experts don’t know how to prevent ASD in children. They do know that it is not caused by what a parent does to raise a child, nor is it linked to childhood vaccines. Spotting and treating ASD early can reduce symptoms and enhance your child’s normal development. It can also improve your child’s quality of life.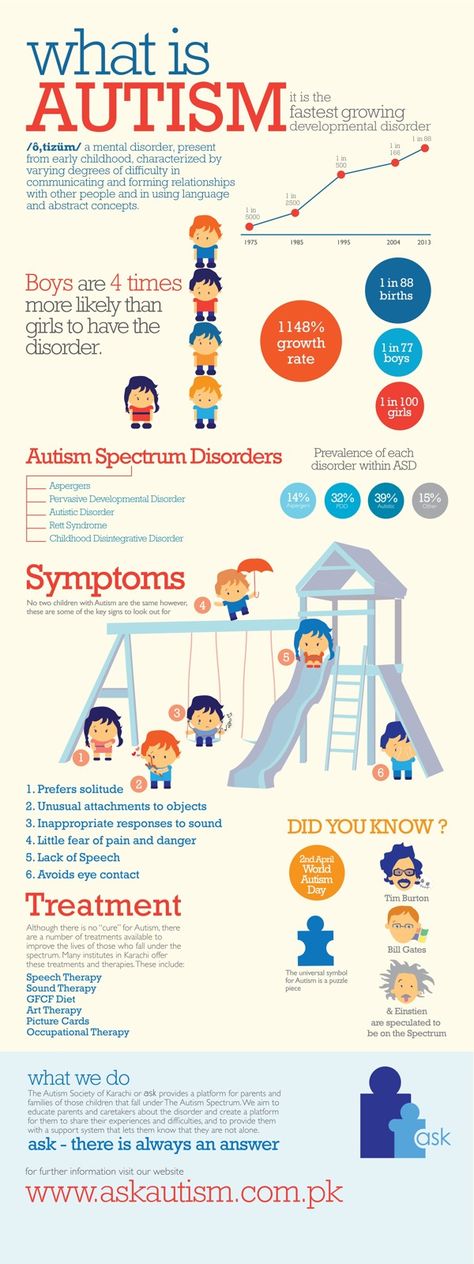
How can I help my child live with ASD?
ASD is a lifelong condition that can put great stress on both the person with ASD and their family. Your child’s primary care provider will play a key role in supporting you and your child. They will help you understand treatment and how to care for your child. You play a critical part in your child’s treatment and well-being. Here are things you can do to help your child:
-
Keep all appointments with your child’s healthcare provider.
-
Talk with your child’s healthcare provider about other providers who will be included in your child’s care. Your child may get care from a team that may include neurologists, speech-language pathologists, occupational and physical therapists, social workers, psychologists, and psychiatrists. Your child’s care team will depend on your child’s needs and how serious the ASD is.
-
Tell others about your child’s ASD.
 Work with your child’s healthcare provider and schools to create a treatment plan.
Work with your child’s healthcare provider and schools to create a treatment plan. -
Check for school resources for your child. Many times a child’s ASD seriously interferes with their ability to manage regular school settings. The Americans with Disabilities Act (ADA) and Section 504 of the Civil Rights Act can help protect children with special educational needs. Talk with your child's teacher or school principal for more information.
-
Have your child wear a medical alert bracelet or necklace if they wander or have communication problems,. Also think about having them carry an emergency form with contact information and communication symbols.
-
Reach out for support from local community services. ASD can be stressful. Being in touch with other parents who have a child with ASD may be helpful.
-
Take care of yourself and watch for signs of stress in you or your family members.
 The physical and emotional demands of caregiving can be overwhelming. Let family and friends help and provide respite care. A break can be helpful for both you and your child. Get additional professional support if needed.
The physical and emotional demands of caregiving can be overwhelming. Let family and friends help and provide respite care. A break can be helpful for both you and your child. Get additional professional support if needed.
Key points about autism spectrum disorder in children
-
Autism spectrum disorder (ASD) is a problem that affects a child’s nervous system and growth and development.
-
A child with ASD often has problems communicating. They may have trouble developing social skills.
-
Genes may play a role in ASD.
-
All children should be screened for ASD before age 2.
-
Diagnosis may include imaging and genetic tests.
-
Children with ASD need a special, long-term treatment plan. It may include programs that change behavior and teach social skills.

-
Each child with ASD is unique and has unique experiences. Families can get help from community-based resources.
Next steps
Tips to help you get the most from a visit to your child’s healthcare provider:
-
Know the reason for the visit and what you want to happen.
-
Before your visit, write down questions you want answered.
-
At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you for your child.
-
Know why a new medicine or treatment is prescribed and how it will help your child. Also know what the side effects are.
-
Ask if your child’s condition can be treated in other ways.
-
Know why a test or procedure is recommended and what the results could mean.
-
Know what to expect if your child does not take the medicine or have the test or procedure.
-
If your child has a follow-up appointment, write down the date, time, and purpose for that visit.
-
Know how you can contact your child’s provider after office hours. This is important if your child becomes ill and you have questions or need advice.
Online Medical Reviewers:
- L Renee Watson MSN RN
- Marianne Fraser MSN RN
- Paul Ballas MD
Related Services
We provide many services to support families of children newly diagnosed with ASD and ongoing specialty care. This includes state of the art diagnostic evaluation for children suspected of having an ASD. We also provide resources and information and referral services.
University of Rochester is one of 17 sites of the Autism Treatment Network and has one of the largest research programs on ASD in the United States! Many families of children with ASD choose to participate in research which offers children the opportunity to participate in new treatments.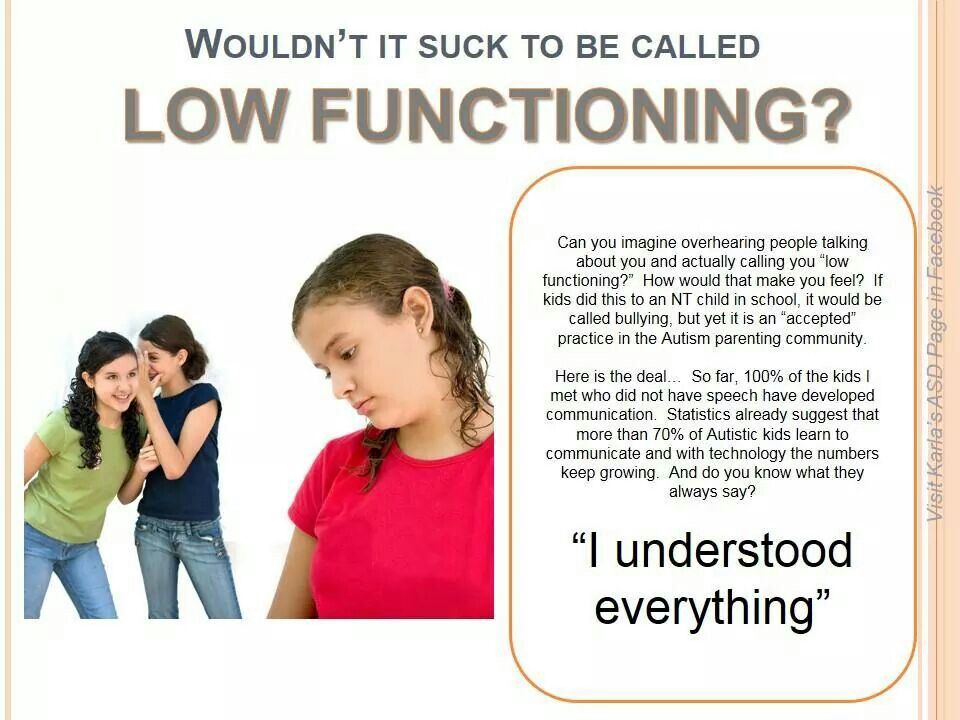
URMC Collaborations
- Child Neurology - Assures children have the evaluation and treatment they need for seizures or other neurologic issues.
- Pediatric Gastroenterology - Evaluates and offers suggestions for treatment for problems with slow bowel motility, constipation, or gastroesophageal reflux (GER).
- Pediatric Sleep Medicine Service - Evaluates and treats sleep problems.
- Physical Medicine and Rehabilitation - Provides outpatient evaluation and intense and targeted therapy programs for children and teens. Pediatric physical therapists provide evaluation and treatment of independent daily living skills and equipment needs. Pediatric occupational therapists provide evaluation and treatment of fine motor skills, handwriting, daily living skills, sensory processing, and adaptive equipment needs.
- Speech Pathology Department - Meets the needs of children who have difficulties with speech, communication, oral-motor control, and feeding/swallowing.
Resources
Visit the Autism Spectrum Disorder LibGuide for resources.
Brain and behavior development in autism from birth through infancy
1. Centers for Disease Control and Prevention (CDC). Prevalence of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 sites. United States, 2010. MMWR Surveill Summ. 2014;63(2):1–21. [PubMed] [Google Scholar]
2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013 [Google Scholar]
3. Rogers SJ. What are infant siblings teaching us about autism in infancy? Autism Res. 2009;2(3):125–137. [PMC free article] [PubMed] [Google Scholar]
4. Ozonoff S., losif AM., Baguio F., et al. A prospective study of the emergence of early behavioral signs of autism. J Am Acad Child Adolesc Psychiatry.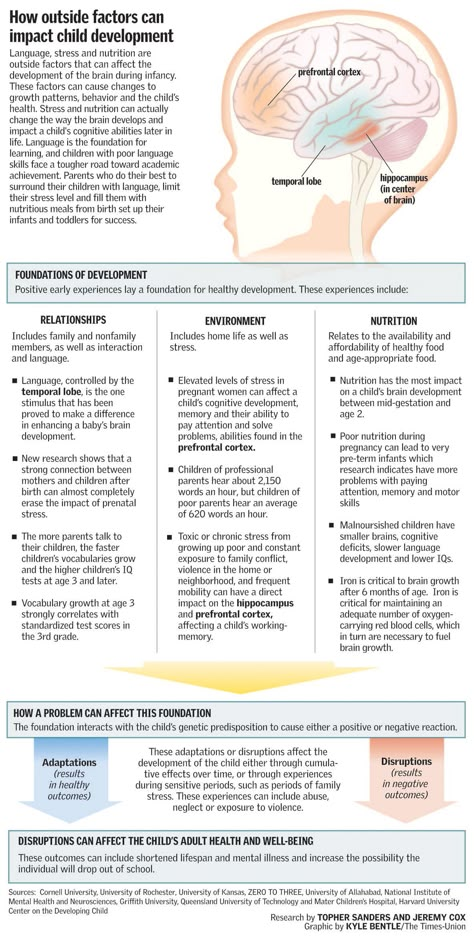 2010;49(3):256–66. [PMC free article] [PubMed] [Google Scholar]
2010;49(3):256–66. [PMC free article] [PubMed] [Google Scholar]
5. Landa RJ., Gross AL., Stuart EA., Faherty A. Developmental trajectories in children with and without autism spectrum disorders: the first 3 years. Child Dev. 2013;84(2):429–442. [PMC free article] [PubMed] [Google Scholar]
6. Zwaigenbaum L., Bryson S., Rogers T., Roberts W., Brian J., Szatmari P. Behavioral manifestations of autism in the first year of life. Int J Dev Neurosci. 2005;23(2-3):143–152. [PubMed] [Google Scholar]
7. Dawson G., Rogers S., Munson J., et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1):e17–e23. [PMC free article] [PubMed] [Google Scholar]
8. Rogers SJ., Vismara LA. Evidence-based comprehensive treatments for early autism. J Clin Child Adolesc Psychol. 2008;37(1):8–38. [PMC free article] [PubMed] [Google Scholar]
9. Clark MLE., Vinen Z., Barbaro J. , Dissanayake C. School age outcomes of children diagnosed early and later with autism spectrum disorder. J Autism Dev Disord. 2017 Sep 14. doi:10.1007/s10803-017-3279-x. [PubMed] [Google Scholar]
, Dissanayake C. School age outcomes of children diagnosed early and later with autism spectrum disorder. J Autism Dev Disord. 2017 Sep 14. doi:10.1007/s10803-017-3279-x. [PubMed] [Google Scholar]
10. Ozonoff S., Young GS., Carter A., et al. Recurrence risk for autism spectrum disorders: a Baby Siblings Research Consortium study. Pediatrics. 2011;128(3):e488–e495. [PMC free article] [PubMed] [Google Scholar]
11. Constantino JN., Zhang Y., Frazier T., Abbacchi AM., Law P. Sibling recurrence and the genetic epidemiology of autism. Am J Psychiatry. 2010;167(11):1349–1356. [PMC free article] [PubMed] [Google Scholar]
12. Gamliel I., Yirmiya N., Sigman M. The development of young siblings of children with autism from 4 to 54 months. J Autism Dev Disord. 2007;37(1):171–183. [PubMed] [Google Scholar]
13. Georgiades S., Szatmari P., Zwaigenbaum L., et al. A prospective study of autistic-like traits in unaffected siblings of probands with autism spectrum disorder. JAMA Psychiatry. 2013;70(1):42–47. [PubMed] [Google Scholar]
JAMA Psychiatry. 2013;70(1):42–47. [PubMed] [Google Scholar]
14. Ozonoff S., Heung K., Byrd R., Hansen R., Hertz-Picciotto I. The onset of autism: patterns of symptom emergence in the first years of life. Autism Res. 2008;1(6):320–328. [PMC free article] [PubMed] [Google Scholar]
15. Elison JT., Wolff JJ., Reznick JS., et al. Repetitive behavior in 12-month-olds later classified with autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2014;53(11):1216–1224. [PMC free article] [PubMed] [Google Scholar]
16. Wolff JJ., Botteron KN., Dager SR., et al. Longitudinal patterns of repetitive behavior in toddlers with autism. J Child Psychol Psychiatry. 2014;55(8):945–953. [PMC free article] [PubMed] [Google Scholar]
17. Filliter JH., Longard J., Lawrence MA., et al. Positive affect in infant siblings of children diagnosed with autism spectrum disorder. J Abnorm Child Psychol. 2014;43(3):567–575. [PubMed] [Google Scholar]
18. Estes A., Zwaigenbaum L., Gu H., et al. Behavioral, cognitive, and adaptive development in infants with autism spectrum disorder in the first 2 years of life. J Neurodev Disord. 2015;7(1):24. [PMC free article] [PubMed] [Google Scholar]
Estes A., Zwaigenbaum L., Gu H., et al. Behavioral, cognitive, and adaptive development in infants with autism spectrum disorder in the first 2 years of life. J Neurodev Disord. 2015;7(1):24. [PMC free article] [PubMed] [Google Scholar]
19. Flanagan JE., Landa R., Bhat A., Bauman M. Head lag in infants at risk for autism: a preliminary study. Am J Occup Ther. 2012;66(5):577–585. [PubMed] [Google Scholar]
20. Swanson MR., Shen MD., Wolff JJ., et al. Subcortical brain and behavior phenotypes differentiate infants with autism versus language delay. Biol Psychiatry Cogn Neurosci Neuroimaging. 2017;2(8):664–672. [PMC free article] [PubMed] [Google Scholar]
21. Chawarska K., Macari S., Shic F. Decreased spontaneous attention to social scenes in 6-month-old infants later diagnosed with autism spectrum disorders. Biol Psychiatry. 2013;74(3):195–203. [PMC free article] [PubMed] [Google Scholar]
22. Jones W., Klin A. Attention to eyes is present but in decline in 2-6-month-old infants later diagnosed with autism. Nature. 2014;504(7480):427–431. [PMC free article] [PubMed] [Google Scholar]
Nature. 2014;504(7480):427–431. [PMC free article] [PubMed] [Google Scholar]
23. Shic F., Macari S., Chawarska K. Speech disturbs face scanning in 6-month-old infants who develop autism spectrum disorder. Biol Psychiatry. 2014;75(3):231–237. [PMC free article] [PubMed] [Google Scholar]
24. Ozonoff S., Young GS., Steinfeld MB., et al. How early do parent concerns predict later autism diagnosis? J Dev Behav Pediatr. 2009;30(5):367–375. [PMC free article] [PubMed] [Google Scholar]
25. Chawarska K., Shic F., Macari S., et al. 18-Month predictors of later outcomes in younger siblings of children with autism spectrum disorder: a Baby Siblings Research Consortium Study. J Am Acad Child Adolesc Psychiatry. 2014;53(12):1317–1327.e1. [PMC free article] [PubMed] [Google Scholar]
26. Robins DL., Fein D., Barton ML., Green JA. The Modified Checklist for Autism in Toddlers: an initial study investigating the early detection of autism and pervasive developmental disorders.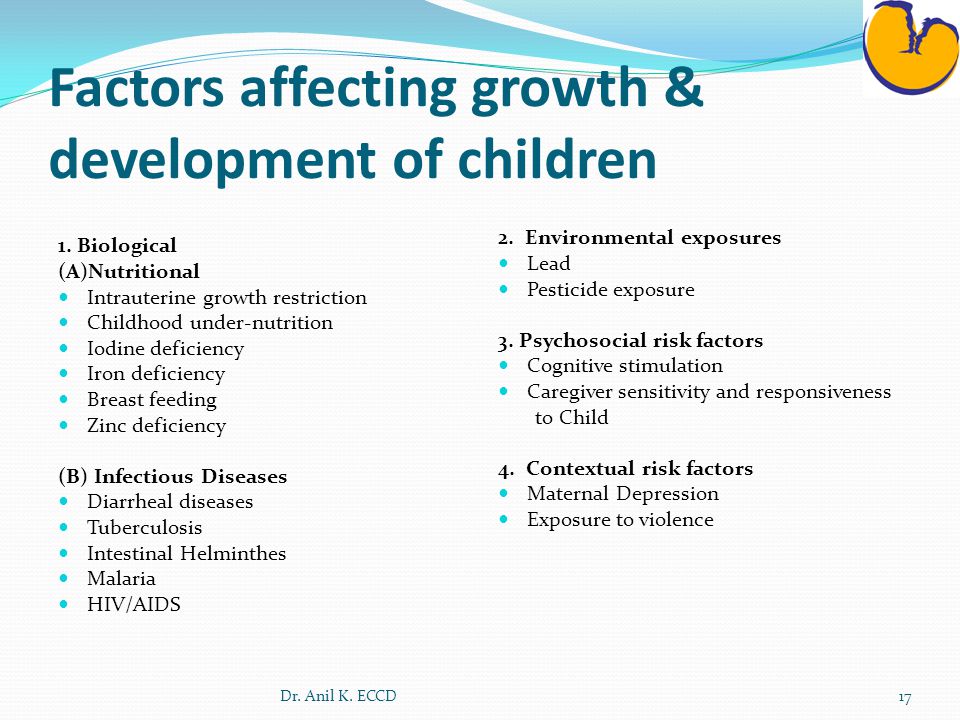 J Autism Dev Disord. 2001;31(2):131–144. [PubMed] [Google Scholar]
J Autism Dev Disord. 2001;31(2):131–144. [PubMed] [Google Scholar]
27. Pandey J., Verbalis A., Robins DL., et al. Screening for autism in older and younger toddlers with the Modified Checklist for Autism in Toddlers. Autism. 2008;12(5):513–535. [PubMed] [Google Scholar]
28. Zwaigenbaum L., Bryson S., Lord C., et al. Clinical assessment and management of toddlers with suspected autism spectrum disorder: insights from studies of high-risk infants. Pediatrics. 2009;123(5):1383–1391. [PMC free article] [PubMed] [Google Scholar]
29. Hazlett HC., Poe MD., Gerig G., et al. Early brain overgrowth in autism associated with an increase in cortical surface area before age 2 years. Arch Gen Psychiatry. 2011;68(5):467. [PMC free article] [PubMed] [Google Scholar]
30. Hazlett HC., Poe M., Gerig G., et al. Magnetic resonance imaging and head circumference study of brain size in autism: birth through age 2 years. Arch Gen Psychiatry. 2005;62(12):1366–1376.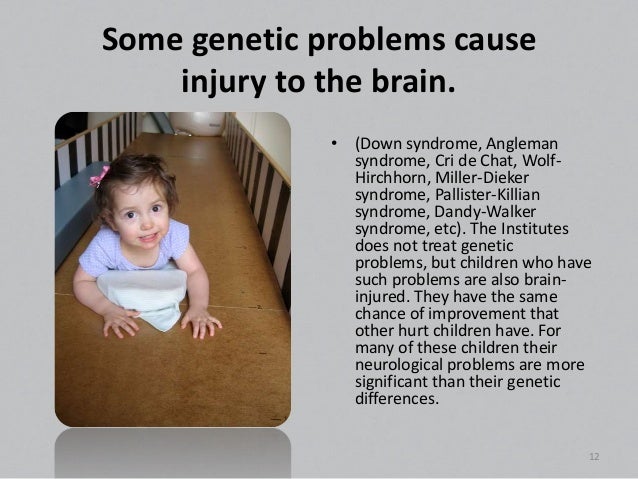 [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
31. Courchesne E., Karns CM., Davis HR., et al. Unusual brain growth patterns in early life in patients with autistic disorder: an MRI study. Neurology. 2001;57(2):245–254. [PubMed] [Google Scholar]
32. Nordahl CW., Lange N., Li DD., et al. Brain enlargement is associated with regression in preschool-age boys with autism spectrum disorders. Proc Natl Acad Sci U S A. 2011;108(50):20195–20200. [PMC free article] [PubMed] [Google Scholar]
33. Sparks BF., Friedman SD., Shaw DW., et al. Brain structural abnormalities in young children with autism spectrum disorder. Neurology. 2002;59(2):184. [PubMed] [Google Scholar]
34. Shen MD., Nordahl CW., Young GS., et al. Early brain enlargement and elevated extra-axial fluid in infants who develop autism spectrum disorder. Brain. 2013;136(pt 9):2825–2835. [PMC free article] [PubMed] [Google Scholar]
35. Hazlett HC., Gu H., Munsell BC., et al. Early brain development in infants at high risk for autism spectrum disorder.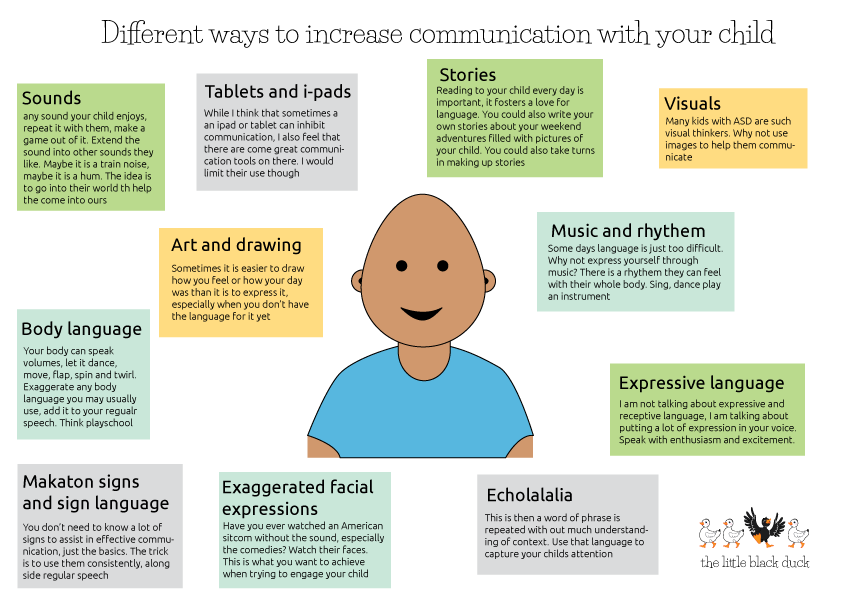 Nature. 2017;542(7641):348–351. [PMC free article] [PubMed] [Google Scholar]
Nature. 2017;542(7641):348–351. [PMC free article] [PubMed] [Google Scholar]
36. Panizzon MS., Fennema-Notestine C., Eyler LT., et al. Distinct genetic influences on cortical surface area and cortical thickness. Cerebral Cortex. 2009;19(11):2728–2735. [PMC free article] [PubMed] [Google Scholar]
37. Ohta H., Nordahl CW., Iosif AM., Lee A., Rogers S., Amaral DG. Increased surface area, but not cortical thickness, in a subset of young boys with autism spectrum disorder. Autism Res. 2016;9(2):232–248. [PMC free article] [PubMed] [Google Scholar]
38. Shen MD., Kim SH., McKinstry RC., et al. Increased extra-axial cerebrospinal fluid in high-risk infants who later develop autism. Biol Psychiatry. 2017;82(3):186–193. [PMC free article] [PubMed] [Google Scholar]
39. Elison JT., Paterson SJ., Wolff JJ., et al. White matter microstructure and atypical visual orienting in 7-month-olds at risk for autism. Am J Psychiatry. 2013;170(8):899–908.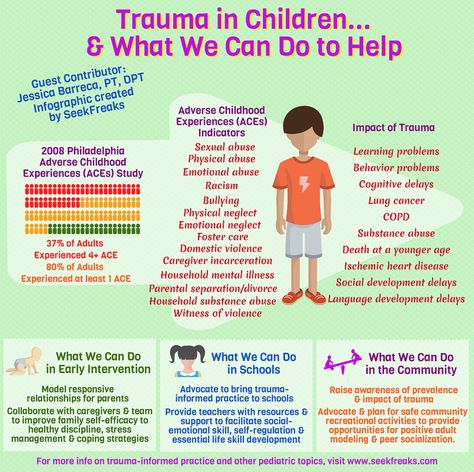 [PMC free article] [PubMed] [Google Scholar]
[PMC free article] [PubMed] [Google Scholar]
40. Johanson CE., Duncan JA., Klinge PM., Brinker T., Stopa EG., Silverberg GD. Multiplicity of cerebrospinal fluid functions: new challenges in health and disease. Cerebrospinal Fluid Res. 2008;5:10. [PMC free article] [PubMed] [Google Scholar]
41. Xie L., Kang H., Xu Q., et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–377. [PMC free article] [PubMed] [Google Scholar]
42. Del Bigio MR. Neuropathology and structural changes in hydrocephalus. Dev Disabil Res Rev. 2010;16(1):16–22. [PubMed] [Google Scholar]
43. Iliff JJ., Wang M., Liao Y., et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111. [PMC free article] [PubMed] [Google Scholar]
44. Lehtinen MK., Walsh CA. Neurogenesis at the brain-cerebrospinal fluid interface. Annu Rev Cell Dev Biol. 2011;27:653–679. [PMC free article] [PubMed] [Google Scholar]
Annu Rev Cell Dev Biol. 2011;27:653–679. [PMC free article] [PubMed] [Google Scholar]
45. Swanson MR., Piven J. Neurodevelopment of autism: the first three years of life. In: Autism Imaging and Devices. Casanova MF, El-Baz AS, Suri JS, eds. Boca Raton, FL: Taylor & Francis Group; 2016 [Google Scholar]
46. Lehtinen MK., Zappaterra MW., Chen X., et al. The cerebrospinal fluid provides a proliferative niche for neural progenitor cells. Neuron. 2011;69(5):893–905. [PMC free article] [PubMed] [Google Scholar]
47. Mashayekhi F., Draper CE., Bannister CM., Pourghasem M., Owen-Lynch PJ., Miyan JA. Deficient cortical development in the hydrocephalic Texas (H-Tx) rat: a role for CSF. Brain. 2002;125(pt 8):1859–1874. [PubMed] [Google Scholar]
48. Chazal J., Tanguy A., Irthum B., Janny P., Vanneuville G. Dilatation of the subarachnoid pericerebral space and absorption of cerebrospinal fluid in the infant. Anat Clin. 1985;7(1):61–66. [PubMed] [Google Scholar]
[PubMed] [Google Scholar]
49. Briner S., Bodensteiner J. Benign subdural collections of infancy. Pediatrics. 1981;67(6):802–804. [PubMed] [Google Scholar]
50. Wolff JJ., Gu H., Gerig G., et al. Differences in white matter fiber tract development present from 6 to 24 months in infants with autism. Am J Psychiatry. 2012;169(6):589–600. [PMC free article] [PubMed] [Google Scholar]
51. Wolff JJ., Gerig G., Lewis JD., et al. Altered corpus callosum morphology associated with autism over the first 2 years of life. Brain. 2015;138(pt 7):2046–2058. [PMC free article] [PubMed] [Google Scholar]
52. Wolff JJ., Swanson MR., Elison JT., et al. Neural circuitry at age 6 months associated with later repetitive behavior and sensory responsiveness in autism. Mol Autism. 2017;8:8. [PMC free article] [PubMed] [Google Scholar]
53. Bashat DB., Kronfeld-Duenias V., Zachor DA., et al. Accelerated maturation of white matter in young children with autism: a high b value DWI study.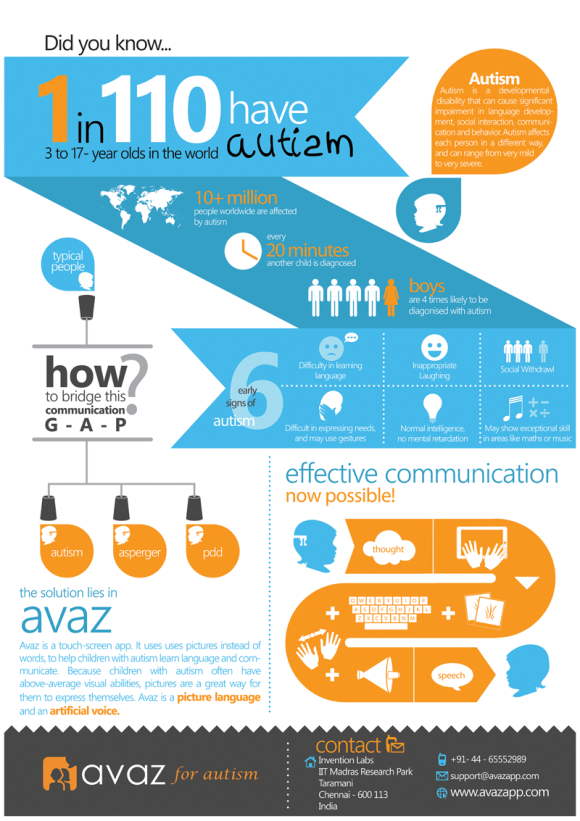 Neuroimage. 2007;37(1):40–47. [PubMed] [Google Scholar]
Neuroimage. 2007;37(1):40–47. [PubMed] [Google Scholar]
54. Solso S., Xu R., Proudfoot J., et al. Diffusion tensor imaging provides evidence of possible axonal overconnectivity in frontal lobes in autism spectrum disorder toddlers. Biol Psychiatry. 2015;79(8):676–684. [PMC free article] [PubMed] [Google Scholar]
55. Emerson RW., Adams C., Nishino T., et al. Functional neuroimaging of high-risk 6-month-old infants predicts a diagnosis of autism at 24 months of age. Sci Transl Med. 2017;9(393):eaag2882. [PMC free article] [PubMed] [Google Scholar]
56. Elsabbagh M., Mercure E., Hudry K., et al. Infant neural sensitivity to dynamic eye gaze is associated with later emerging autism. Curr Biol. 2012;22(4):338–342. [PMC free article] [PubMed] [Google Scholar]
57. Jones EJ., Venema K., Earl R., et al. Reduced engagement with social stimuli in 6-month-old infants with later autism spectrum disorder: a longitudinal prospective study of infants at high familial risk. J Neurodev Disord. 2016;8:7. [PMC free article] [PubMed] [Google Scholar]
J Neurodev Disord. 2016;8:7. [PMC free article] [PubMed] [Google Scholar]
58. Vivanti G., Dissanayake C. Outcome for children receiving the early start Denver model before and after 48 months. J Autism Dev Disord. 2016;46(7):2441–2449. [PubMed] [Google Scholar]
59. Rogers SJ., Vismara L., Wagner AL., McCormick C., Young G., Ozonoff S. Autism treatment in the first year of life: a pilot study of infant start, a parent-implemented intervention for symptomatic infants. J Autism Dev Disord. 2014;44(12):2981–2995. [PMC free article] [PubMed] [Google Scholar]
60. Green J., Charman T., Pickles A., Wan MW. Parent-mediated intervention versus no intervention for infants at high risk of autism: a parallel, single-blind, randomised trial. Lancet Psychiatry. 2015;2(2):133–140. [PMC free article] [PubMed] [Google Scholar]
61. Jones EJH., Dawson G., Kelly J., Estes A., Jane Webb S. Parent-delivered early intervention in infants at risk for ASD: effects on electrophysiological and habituation measures of social attention. Autism Res. 2017;10(5):961–972. [PMC free article] [PubMed] [Google Scholar]
Autism Res. 2017;10(5):961–972. [PMC free article] [PubMed] [Google Scholar]
62. NIH Biomarkers Definitions Working Group. Biomarkers and surrogate endpoints: preferred definitions and conceptual framework. Clin Pharmacol Ther. 2001;69(3):89–95. [PubMed] [Google Scholar]
63. Knickmeyer RC., Gouttard S., Kang C., et al. A structural MRI study of human brain development from birth to 2 years. J Neurosci. 2008;28(47):12176–12182. [PMC free article] [PubMed] [Google Scholar]
64. Insel TR. Translating scientific opportunity into public health impact: a strategic plan for research on mental illness. Arch Gen Psychiatry. 2009;66(2):128–133. [PubMed] [Google Scholar]
65. Ozonoff S., Young GS., Landa RJ., et al. Diagnostic stability in young children at risk for autism spectrum disorder: a baby siblings research consortium study. J Child Psychol Psychiatry. 2015;56(9):988–998. [PMC free article] [PubMed] [Google Scholar]
66. Zwaigenbaum L., Bryson SE., Brian J., et al. Stability of diagnostic assessment for autism spectrum disorder between 18 and 36 months in a high-risk cohort. Autism Res. 2016;9(7):790–800. [PubMed] [Google Scholar]
67. Brian J., Bryson SE., Smith IM., et al. Stability and change in autism spectrum disorder diagnosis from age 3 to middle childhood in a high-risk sibling cohort. Autism. 2016;20(7):888–892. [PubMed] [Google Scholar]
68. Chung J., Smith AL., Hughes SC., et al. Twenty-year follow-up of newborn screening for patients with muscular dystrophy. Muscle Nerve. 2016;53(4):570–578. [PubMed] [Google Scholar]
69. MacLeod R., Beach A., Henriques S., Knopp J., Nelson K., Kerzin-Storrar L. Experiences of predictive testing in young people at risk of Huntington's disease, familial cardiomyopathy or hereditary breast and ovarian cancer. Eur J Hum Genet. 2014;22(3):396–401. [PMC free article] [PubMed] [Google Scholar]
70. Crozier S.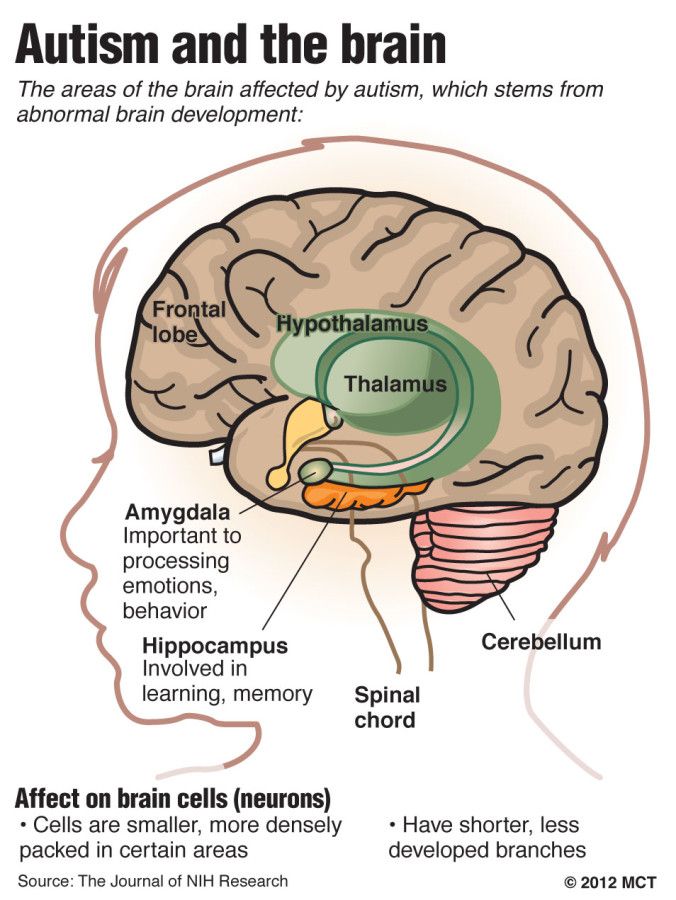 , Robertson N., Dale M. The psychological impact of predictive genetic testing for Huntington's disease: a systematic review of the literature. J Genet Couns. 2015;24(1):29–39. [PubMed] [Google Scholar]
, Robertson N., Dale M. The psychological impact of predictive genetic testing for Huntington's disease: a systematic review of the literature. J Genet Couns. 2015;24(1):29–39. [PubMed] [Google Scholar]
71. Broadstock M., Michie S., Marteau T. Psychological consequences of predictive genetic testing: a systematic review. Eur J Hum Genet. 2000;8(10):731–738. [PubMed] [Google Scholar]
72. Michie S., Bobrow M., Marteau TM. Predictive genetic testing in children and adults: a study of emotional impact. J Med Genet. 2001;38(8):519–526. [PMC free article] [PubMed] [Google Scholar]
73. Sparbel KJ., Tluczek A. Patient and family issues regarding genetic testing for cystic fibrosis: a review of prenatal carrier testing and newborn screening. Annu Rev Nurs Res. 2011;29:303–329. [PubMed] [Google Scholar]
74. Bailey DB., Wheeler A., Berry-Kravis E., et al. Maternal consequences of the detection of fragile X carriers in newborn screening. Pediatrics. 2015;136(2):e433–e440. [PMC free article] [PubMed] [Google Scholar]
2015;136(2):e433–e440. [PMC free article] [PubMed] [Google Scholar]
75. Hendriks KS., Grosfeld FJ., Wilde AA., et al. High distress in parents whose children undergo predictive testing for long QT syndrome. Community Genet. 2005;8(2):103–113. [PubMed] [Google Scholar]
76. Lerman C., Croyle RT., Tercyak KP., Hamann H. Genetic testing: psychological aspects and implications. J Consult Clin Psychol. 2002;70(3):784–797. [PubMed] [Google Scholar]
77. Bailey DB., Skinner D., Davis AM., Whitmarsh I., Powell C. Ethical, legal, and social concerns about expanded newborn screening: fragile X syndrome as a prototype for emerging issues. Pediatrics. 2008;121(3):e693–e704. [PubMed] [Google Scholar]
78. Green RC., Roberts JS., Cupples LA., et al. Disclosure of APOE genotype for risk of Alzheimer's disease. N Engl J Med. 2009;361(3):245–254. [PMC free article] [PubMed] [Google Scholar]
79. Walsh P., Elsabbagh M., Bolton P., Singh I. In search of biomarkers for autism: scientific, social and ethical challenges. Nat Rev Neurosci. 2011;12(10):603–612. [PubMed] [Google Scholar]
In search of biomarkers for autism: scientific, social and ethical challenges. Nat Rev Neurosci. 2011;12(10):603–612. [PubMed] [Google Scholar]
80. Insel TR., Cuthbert BN. Medicine. Brain disorders? Precisely. Science. 2015;348(6234):499–500. [PubMed] [Google Scholar]
Autism: what can parents do to help their child?
The first 2-3 years are especially difficult for a couple who have had their first child. Young mothers and fathers are still learning to be parents, and it is quite difficult to understand that the development of their child is different from others. It's even harder to accept that your baby may have a mental disorder. Childhood autism, or as it is now also called, autism spectrum disorders (ASD), today occurs in every 88th child. How to recognize the disease and what should parents pay attention to? These and other questions related to autism were answered by the Head of the Department of Psychiatry and Narcology, Doctor of Medical Sciences, Associate Professor Grechany Severin Vyacheslavovich.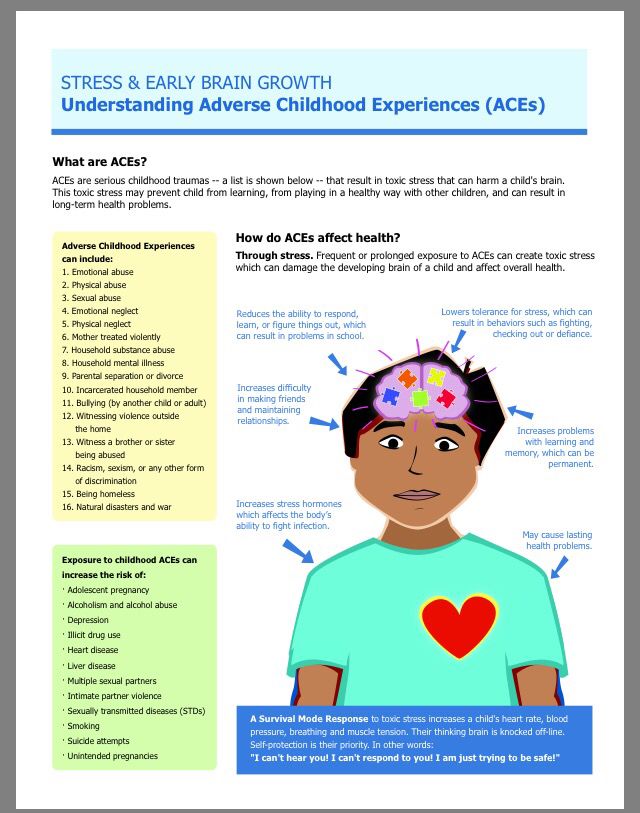 nine0004
nine0004
What is autism? Is this disease born or is it an acquired condition in the environment in which the child grows up?
Childhood autism is a congenital disease. The fact of its occurrence cannot be the result of such external causes as, for example, the social or cultural level of the family. The decisive role is played by the biological factor that determines the birth of such a child. Of course, there are external circumstances that, ceteris paribus, provoke the appearance of symptoms of this disorder - a severe viral infection, in some cases even a sharp change in the family situation, for example, a sudden separation from the mother, hospitalization of the child in the hospital and more. Often an autistic child is the firstborn in the family, and parents do not yet know how the child should develop. Subsequently, they recall that they often thought about why their child did not develop like other children, but still they did not suspect serious deviations.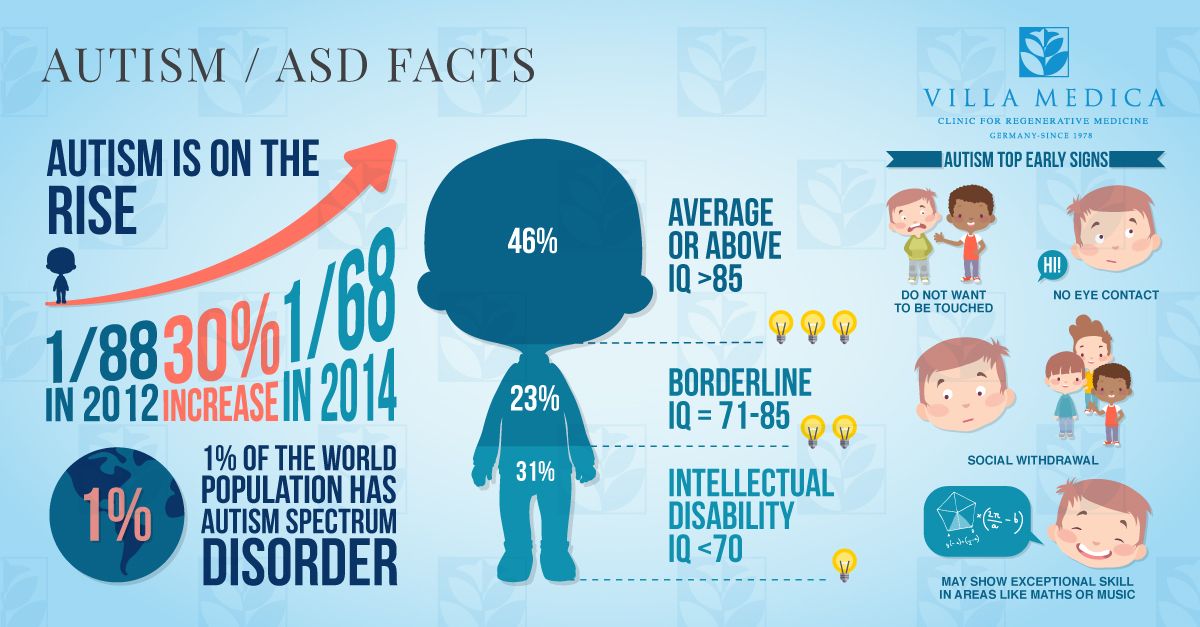 Therefore, this day - April 2 - just calls for adults to take a closer look at the child in general and notice any anomalies in his development as early as possible. And whether this is autism or some other disease - this should be decided by the doctor. nine0005
Therefore, this day - April 2 - just calls for adults to take a closer look at the child in general and notice any anomalies in his development as early as possible. And whether this is autism or some other disease - this should be decided by the doctor. nine0005
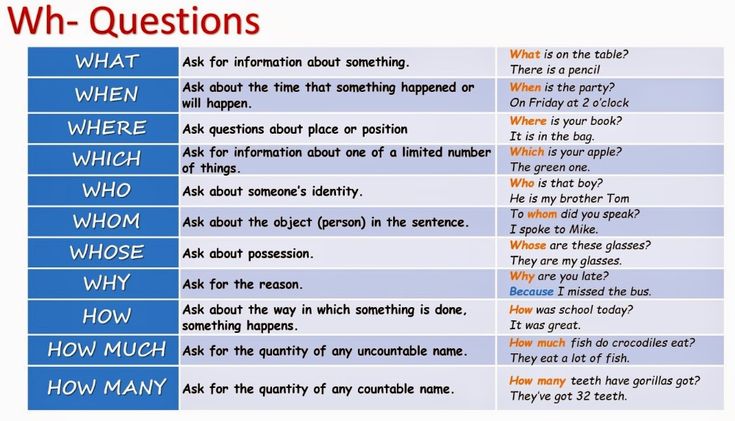
How can parents tell if their child has the condition?
Unfortunately, often parents do not immediately pay attention to the atypical, age-specific behavior of their child. This circumstance gave rise to some myths that autism can occur with the wrong parenting approach or after some medical interventions, including preventive vaccinations. This cannot be believed, since childhood autism also goes through a latent phase in its development, when its symptoms are almost imperceptible, but this does not mean that it was not there from birth. However, you need to know the so-called "red flags of autism", with the manifestation of which it is worth contacting a specialist. These include:
- child does not use pointing gesture,
- does not make eye contact, does not smile in response to a smile,
- does not respond to his name or to requests addressed to him,
- does not hear speech, does not understand why adults turn to him,
- does not say a 2-word phrase by age 2,
- does not use toys for its intended purpose.
Often the child does not develop a plot game. For example, a car for a boy is not an image of a car that he saw on the street, but only wheels that can be turned. With the help of a toy, a child cannot reproduce the plot seen in life. In the same way, for a girl, a doll is not an image of a little man whom she can put to sleep or feed, but an indifferent object with moving parts. It is also worth paying attention to how the child communicates, whether he can follow the simple instructions of an adult, and concentrate his attention. If parents notice these features, then you need to see a doctor. nine0005
Is it possible to cure autism or only bring adaptation to life to a certain level? Which doctor to contact in this case?
Any specialist can suspect autism. Suppose the district pediatrician assumes that the child has autism and advises parents to contact a psychiatrist. However, it is important to understand that the final diagnosis may differ from the initial one, and there are other mental disorders besides childhood autism at an early age. nine0005
nine0005
Is child autism treated at the Pediatric University Clinic?
We don’t have a separate department yet, besides, working with an autistic child is a long-term, often many-year work of a large team of different specialists, including not only doctors, but also correctional teachers, clinical psychologists and their varieties, rehabilitation specialists etc. However, we consult such children and their mothers at the stage of early diagnosis, when parents, for various reasons, are not yet ready to go to official psychiatric institutions. Thus, difficult and doubtful diagnostic cases are solved, the very first recommendations are given. For example, I receive at the Multidisciplinary Center, Vera Vladimirovna Pozdnyak takes at the Consultative and Diagnostic Center. We provide primary care to these children. We give advice on how to treat a possible disease in a child, how to behave with such children and what options for drug therapy exist. Most moms walk away grateful as they get answers to questions that have haunted them for a long time. nine0005
Most moms walk away grateful as they get answers to questions that have haunted them for a long time. nine0005
As far as treatment is concerned, we do not provide it. In addition, parents, faced with the problem of autism, must understand that it is impossible to completely cure it, and they will have to accept that throughout their life the child will be special, unlike all others. There has never been such a case that the same classic autism ended in complete adaptation in society, even if the child at some stage was able to master the profession. Although it is believed that with age the diagnosis of "autism" cannot be reconsidered for a child, but most of the actual "autistic" traits disappear on their own over time. And already at the age of 6-7, other problems related to behavior, underdevelopment of abstract concepts, misunderstanding of the context of communication, i.e. purely intellectual difficulties, come to the fore. In the future, parents will need to adapt the child to life with what is, including special requirements for the learning process. At home, you should also follow a special system of rules developed individually for a particular child. nine0005
At home, you should also follow a special system of rules developed individually for a particular child. nine0005
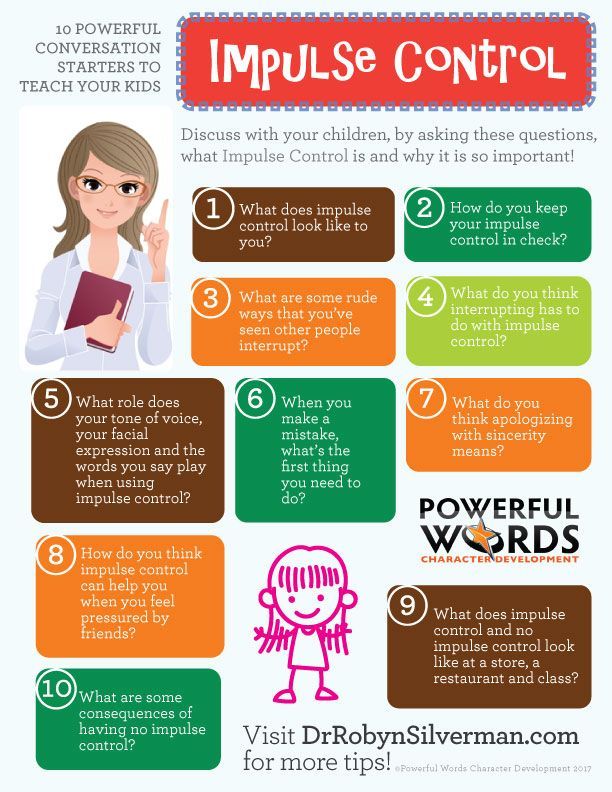
How can parents help their child cope with autism? Can you give any recommendations for them?
The most important recommendation, from our point of view, is to initially understand the child's capabilities, not to do too much and not to set too high goals. The biggest conflict arises precisely when parents are faced with a contradiction between the real abilities of the child and their own ambitions for him. And everything negative that can happen later - protests, disobedience, experiencing disappointment and despair - all this comes precisely from this conflict. nine0005
The main principle for parents is to gain a sense of confidence as a caregiver and get rid of excessive feelings of guilt. You need to know that an autistic child is very sensitive to the internal state of his parents, easily reacts to their anxiety, confusion. With regard to mental development, one should be prepared for the fact that it will take a long time to achieve success, even small ones. It does not happen that a child falls asleep with one person and wakes up with another person.
With regard to mental development, one should be prepared for the fact that it will take a long time to achieve success, even small ones. It does not happen that a child falls asleep with one person and wakes up with another person.
Another common mistake is the opinion that the most important thing for a child is to learn to talk. This is not true. If speech does not appear on its own, then there are objective reasons for this. As soon as the prerequisites for pronouncing words are formed, the child will begin to speak independently without our help. Therefore, you should not artificially try to accelerate the development of such a child. nine0005
Is it possible to say that modern communication devices, computers, gadgets, mobile phones can develop autism in a child? And do they somehow affect children who have already been diagnosed with this disease? (Can modern technology help to socialize or, on the contrary, contribute to the fact that the child withdraws more and more into himself?)
In autism, this is neither good nor bad.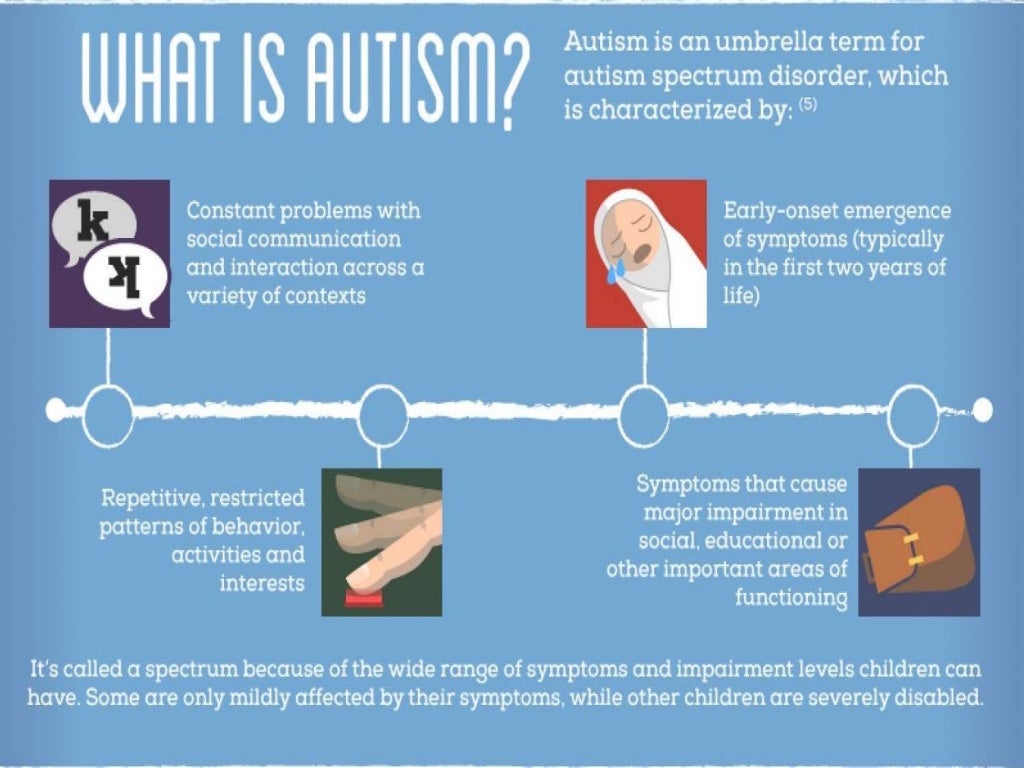 There can be no universal recommendation here, everything is individual. It is important for a mother to understand whether her child is now ready to master society or whether she still needs to wait, subsequently carefully “grafting” him to life. Here the advice of a defectologist, a psychiatrist will help. True, very often the mothers of such children are guided only by their own opinion, without accepting someone else's help. This happens if their relatives betrayed them, the father left, the grandparents did not accept the child, and the mother is left alone with the problem. nine0005
There can be no universal recommendation here, everything is individual. It is important for a mother to understand whether her child is now ready to master society or whether she still needs to wait, subsequently carefully “grafting” him to life. Here the advice of a defectologist, a psychiatrist will help. True, very often the mothers of such children are guided only by their own opinion, without accepting someone else's help. This happens if their relatives betrayed them, the father left, the grandparents did not accept the child, and the mother is left alone with the problem. nine0005
Why is autism thought to be more common in boys? And why is it more characteristic of them?
Indeed, this is a fundamental fact. And childhood autism is not the only example. A lot of mental disorders occur more often in boys. Why this is so is hard to say. There are many hypotheses for this, but an exhaustive explanation has not yet been received.
Maybe there is some relationship between the mother's condition during pregnancy and the child's subsequently diagnosed autistic disorder? Is it possible to somehow predict the birth of a child with autism? What are the medical reasons? nine0013
Mothers often ask me: “Tell me, please, where, at what stage did I make a mistake? What did I do wrong? Unfortunately, despite the fact that we live in the 21st century, there are no prerequisites to predict the birth of such a child.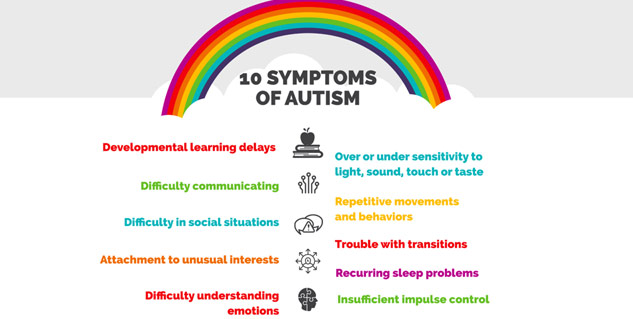 With the exception of the examination of the amniotic fluid for gross genetic anomalies. If this is observed, then we can say with a high degree of probability that a clinical picture of autism should be expected here. In all other cases, it is difficult to predict anything. There is no data for this. nine0005
With the exception of the examination of the amniotic fluid for gross genetic anomalies. If this is observed, then we can say with a high degree of probability that a clinical picture of autism should be expected here. In all other cases, it is difficult to predict anything. There is no data for this. nine0005
Is it true that autism is more common in children today than it was 10, 20, 30 years ago?
It is believed that the number of children with autism has not increased, diagnosis has improved. This happened due to the spread of information about autism and its manifestations. As a result, parents began to pay more attention to what they had not noticed before. And, as a result, the number of visits to doctors for the purpose of making a diagnosis has increased. What used to cause confusion and misunderstanding in parents, now prompts a search for answers in specialized literature, the Internet. As a result, the symptoms of autism began to be detected more often and at an earlier age.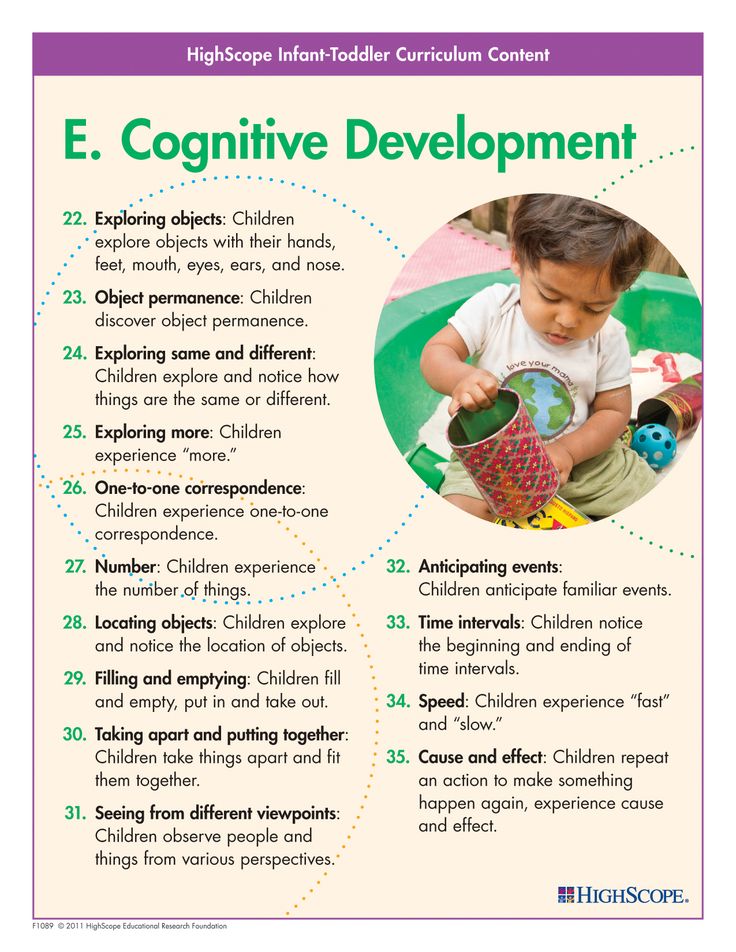 And here there is another extreme - the emerging trend towards overdiagnosis of this disorder. A special term has even appeared - autism spectrum disorders, the role of which is seen in drawing more attention of parents to any symptoms of deviant development, closely or remotely resembling childhood autism, in order to promptly apply for practical assistance. nine0005
And here there is another extreme - the emerging trend towards overdiagnosis of this disorder. A special term has even appeared - autism spectrum disorders, the role of which is seen in drawing more attention of parents to any symptoms of deviant development, closely or remotely resembling childhood autism, in order to promptly apply for practical assistance. nine0005
Can an autistic child go to a regular school, or is it better to send him to a special school?
There are inclusive types of education that allow such children to study in a regular school. A group of 3-4 such children is recruited, and most of the time they study with a separate teacher. Periodically, the teacher selectively leads, as far as possible, such children to classes with healthy children. But the need for such classes must be considered individually. All possible consequences should be taken into account. For example, in practice, children with autism are not very physically healthy, they are characterized by weak immunity - this increases their risk of getting respiratory and other infectious diseases, which usually occur in a more severe form in children with autism.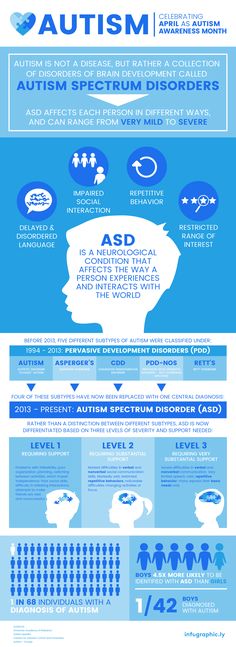 After all, even under normal conditions, autistic children get sick more often than other children. In addition, education in a mass school is possible if there is a special assistant or tutor nearby, a person who guides the child in each specific case and tells him what to do. Often such children, being in mass education, do not follow the school curriculum, but only formally attend the lessons. But what he will learn as a result is a separate question. More often it is a kind of “familiarization” with educational material. And in this situation, we have no right to demand that the child master the entire program. However, one should not forget that traditional defectological assistance in the conditions of ordinary correctional kindergartens and schools has great potential in terms of filling cognitive deficits, and the passage of inclusive education still does not eliminate the need to acquire specialized skills using routine correction methods. nine0005
After all, even under normal conditions, autistic children get sick more often than other children. In addition, education in a mass school is possible if there is a special assistant or tutor nearby, a person who guides the child in each specific case and tells him what to do. Often such children, being in mass education, do not follow the school curriculum, but only formally attend the lessons. But what he will learn as a result is a separate question. More often it is a kind of “familiarization” with educational material. And in this situation, we have no right to demand that the child master the entire program. However, one should not forget that traditional defectological assistance in the conditions of ordinary correctional kindergartens and schools has great potential in terms of filling cognitive deficits, and the passage of inclusive education still does not eliminate the need to acquire specialized skills using routine correction methods. nine0005
Whatever problems parents face on the difficult path of upbringing, it is important to remember that parental love is important at any stage of growing up.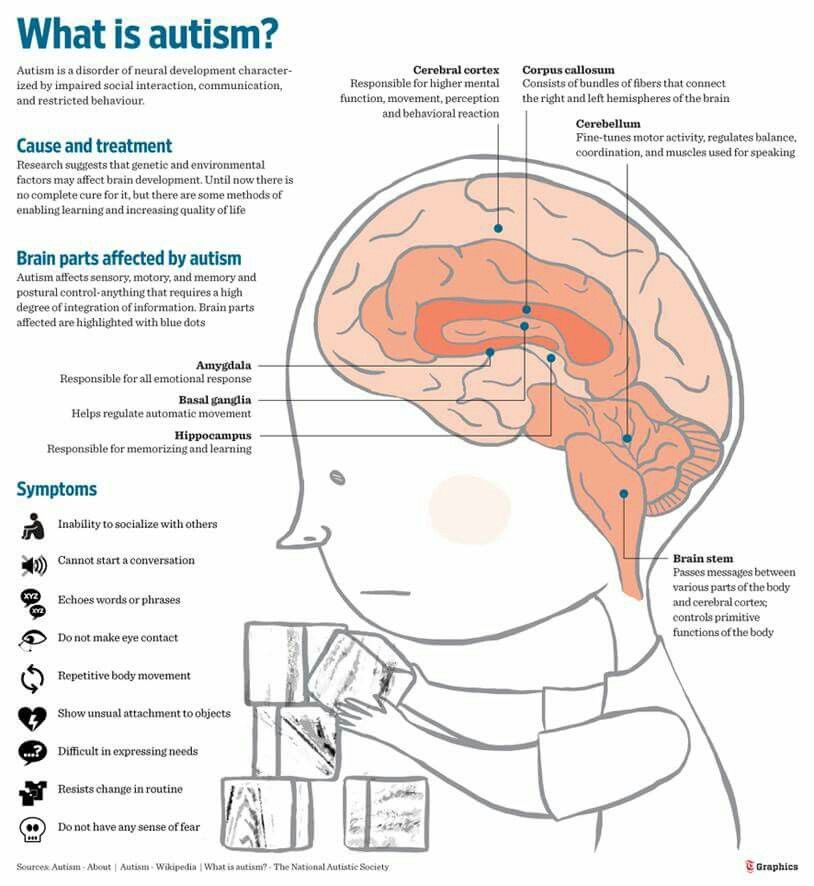
Publication date: 2.04.2020
"Children of the rain". What you need to know about autism
11 April 2019 12:01
Behind the poetic expression "children of the rain" lies the daily feat of people who are faced with a diagnosis of autism. Children who will never be able to perceive themselves as part of the world around them, and parents for whom every day is a series of battles and victories. First, fighting with yourself, accepting and realizing that their child will never be cured, and then fighting the disease for every gesture, every smile, every look and word of the child - small, but such important victories. nine0005
Scientists have not been able to reliably establish the causes of the disease. It is known about the genetic predisposition: signs of autism are more often manifested in people whose family already has an autistic person. Pregnancy in mothers of such children proceeds normally, and the children themselves are often very attractive in appearance - autism, as a rule, does not affect the physical development of the child.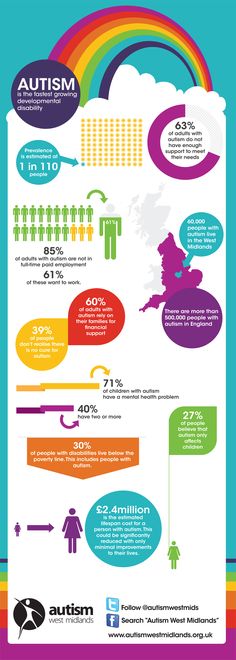 However, the development of autism is still in some cases associated with the manifestation of other diseases:
However, the development of autism is still in some cases associated with the manifestation of other diseases:
- cerebral palsy; nine0027 maternal rubella infection during pregnancy;
- tuberous sclerosis;
- impaired fat metabolism (the risk of having a baby with autism is greater in obese women).
All of these conditions can have a bad effect on the brain and, as a result, provoke symptoms of autism. However, what autism is, and what are the causes of its manifestation, is still not completely clear.
Early diagnosis plays an important role in the further development of an autistic child. Autism in children is manifested by certain signs. Early childhood autism is a condition that can manifest itself in children at a very early age - both at 1 year old and at 2 years old. What is autism in a child, and whether this disease occurs, is determined by a specialist. But you can independently figure out what kind of illness a child has and suspect him, based on information about the signs of such a condition.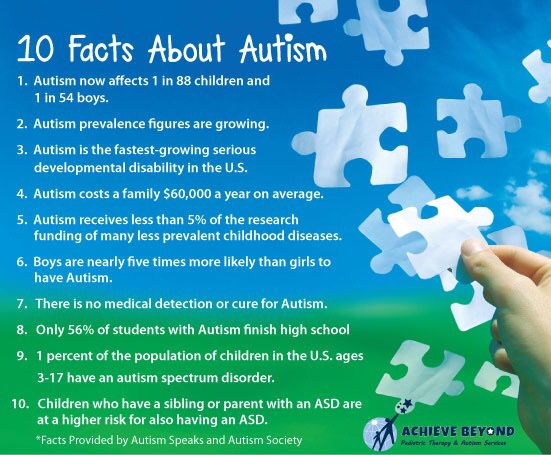 nine0005
nine0005
Early signs of autism in a child
This syndrome is characterized by 4 main signs. In children with this disease, they can be determined to varying degrees.
Signs of autism in children are:
- impaired social interaction;
- broken communication;
- stereotyped behaviour;
- early symptoms of childhood autism in children under 3 years of age.
The first signs of autistic children can be expressed as early as the age of 2 years. Symptoms may be mild when eye-to-eye contact is impaired, or more severe when it is completely absent. As a rule, autism manifests itself very early - even before the age of 1, parents can recognize it. In the first months, such children are less mobile, react inadequately to stimuli from the outside, they have poor facial expressions. nine0005
The child cannot perceive a holistic image of a person who is trying to communicate with him. Even in the photo and video, you can recognize that such a baby's facial expressions do not correspond to the current situation.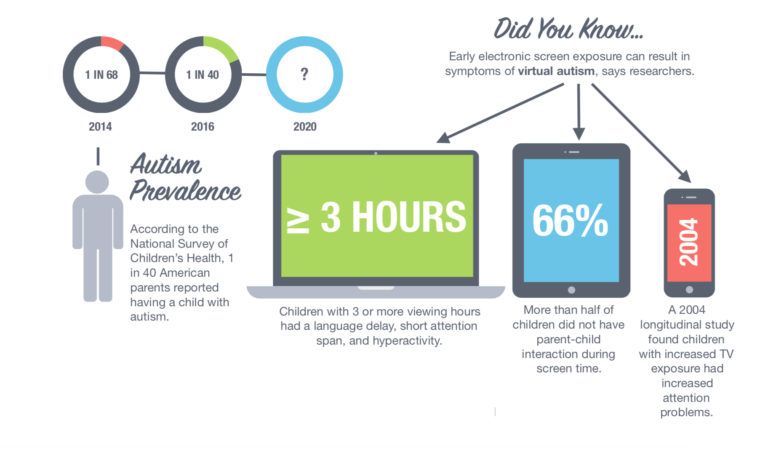 He does not smile when someone tries to amuse him, but he can laugh when the reason for this is not clear to anyone close to him. The face of such a baby is mask-like, grimaces periodically appear on it.
He does not smile when someone tries to amuse him, but he can laugh when the reason for this is not clear to anyone close to him. The face of such a baby is mask-like, grimaces periodically appear on it.
Baby uses gestures only to indicate needs. As a rule, even in children under one year old, interest is sharply shown if they see an interesting object - the baby laughs, points with a finger, and demonstrates joyful behavior. The first signs in children under 1 year old can be suspected if the child does not behave like this. Symptoms of autism in children under one year old are manifested by the fact that they use a certain gesture, wanting to get something, but do not seek to capture the attention of their parents by including them in their game. nine0005
An autistic person cannot understand other people's emotions. How this symptom manifests itself in a child can be traced already at an early age. If ordinary children have a brain designed in such a way that they can easily determine when they look at other people, they are upset, cheerful or scared, then an autistic person is not capable of this.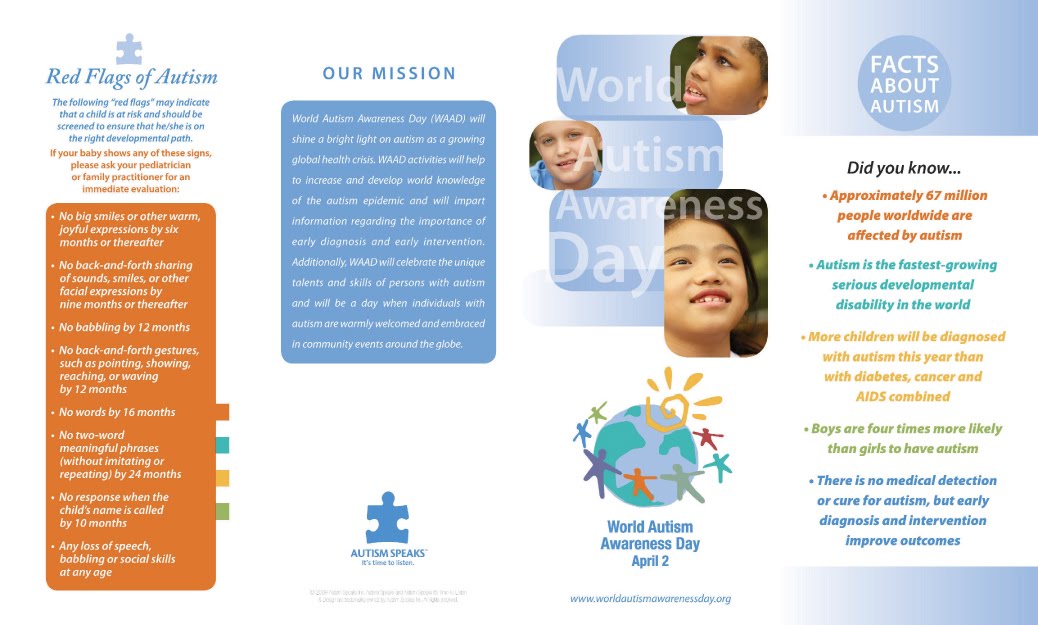
The child is not interested in peers. Already at the age of 2, ordinary children strive for company - to play, to get acquainted with their peers. Signs of autism in children of 2 years old are expressed by the fact that such a baby does not participate in games, but plunges into his own world. Those who want to know how to recognize a child 2 years old and older should simply look at the company of children: an autist is always alone and does not pay attention to others or perceives them as inanimate objects. nine0005
It is difficult for a child to play using imagination and social roles. Children 3 years old and even younger play, fantasizing and inventing role-playing games. In autistics, symptoms at 3 years old may be expressed by the fact that they do not understand what a social role in the game is, and do not perceive toys as integral objects. For example, signs of autism in a child of 3 years old can be expressed by the fact that the baby spins the wheel of a car for hours or repeats other actions.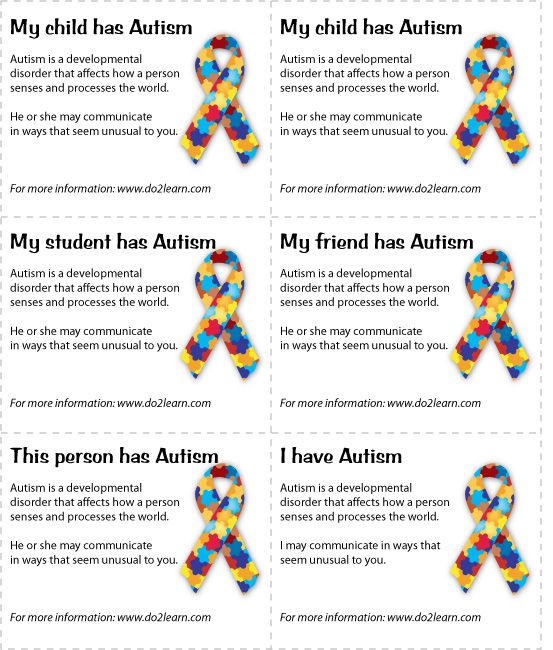
Child does not respond to emotions and communication from parents. Previously, it was believed that such children are not emotionally attached to their parents at all. But now scientists have proven that when a mother leaves, such a child at 4 years old and even earlier shows anxiety. If family members are around, he looks less obsessed. However, in autism, signs in children of 4 years old are expressed by a lack of reaction to the fact that parents are absent. The autist shows anxiety, but he does not try to return his parents. nine0005
In children under 5 years of age and later, there is a delay in speech or its complete absence (mutism). The speech is incoherent, the child repeats the same phrases, devoid of meaning, speaks of himself in the third person. He does not respond to other people's speech either. When the “age of questions” comes, parents will not hear them from the baby, and if they do, then these questions will be monotonous and without practical significance.
Stereotypic behavior includes obsession with one activity, repetition of daily rituals, development of fears and obsessions. At the same time, if the sequence of the ritual is violated, the child becomes hysterical or may show aggression or self-aggression. nine0005
Can autism be cured and is it curable at all? Unfortunately, there is no cure. How you can help your child depends on each individual case. Drug treatment is prescribed only in case of destructive behavior of a small patient. But, despite the fact that the disease is not curable, it is possible to correct the situation. The best "treatment" in this case is regular practice every day and the creation of the most favorable environment for the autistic. Classes are held in stages:
- To form the skills that are needed for training. If the child does not make contact, gradually establish it, not forgetting who it is - autistics. Gradually it is necessary to develop at least the rudiments of speech. nine0028
- Eliminate forms of behavior that are non-constructive: aggression, self-aggression, fears, withdrawing into oneself, etc.
- Learn to observe, imitate.
- Teaching social games and roles.
- Learn to make emotional contact.
The most common treatment for autism is practiced according to the principles of behaviorism (behavioral psychology). One of the subtypes of such therapy is ABA therapy. The basis of this treatment is to observe what the reactions and behavior of the baby look like. After all the features are studied, incentives are selected for a particular autist. Speech therapy practice is obligatory: if the kid regularly works with a speech therapist, his intonation and pronunciation are getting better. At home, parents help the child develop self-service and socialization skills. Since autists have no motivation to play, they get used to the daily routine, everyday affairs, cards are created where the order of performing this or that action is written or drawn. nine0005
Why is early diagnosis important? There are conditions that mimic autism that can be confused with its symptoms. But other methods are used to correct them.
But other methods are used to correct them.
ZPRR with autistic features
The symptoms of this disease are associated with a delay in psychoverbal development. They are in many ways similar to the signs of autism. Starting from a very early age, the baby does not develop in terms of speech in the way that existing norms suggest. In the first months of life, he does not babble, then he does not learn to speak simple words. At 2-3 years old, his vocabulary is very poor. Such children are often poorly developed physically, sometimes hyperactive. The final diagnosis is made by the doctor. It is important to visit a psychiatrist, speech therapist with the child. nine0005
Attention deficit hyperactivity disorder
This condition is also often mistaken for autism. With a lack of attention, children are restless, it is difficult for them to study at school. There are problems with concentration, such children are very mobile. Even in adulthood, echoes of this state remain, because it is difficult for such people to remember information and make decisions.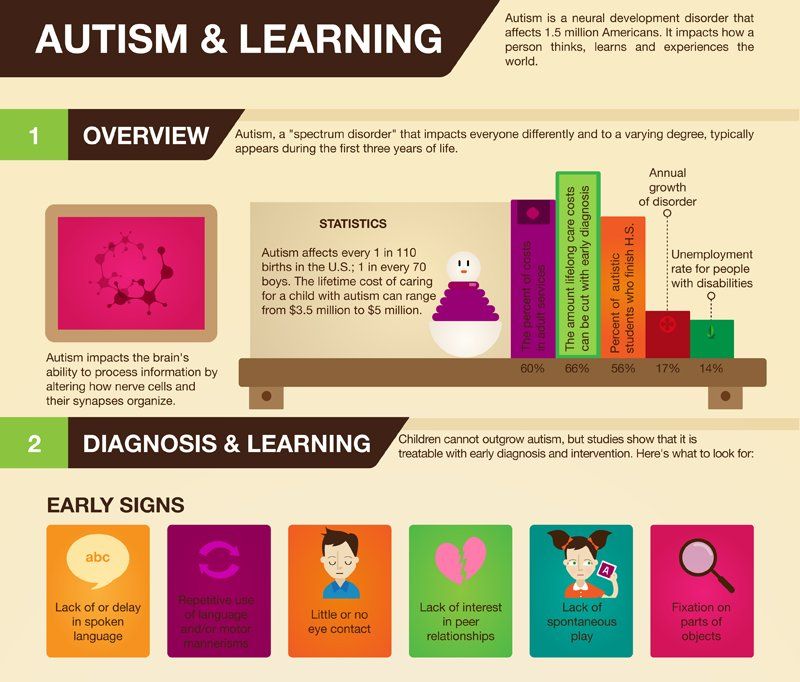 You should try to diagnose this condition as early as possible, practice treatment with psychostimulants and sedative drugs, and visit a psychologist. nine0005
You should try to diagnose this condition as early as possible, practice treatment with psychostimulants and sedative drugs, and visit a psychologist. nine0005
Hearing loss
These are various hearing impairments, both congenital and acquired. Hearing-impaired children also have speech delays. Therefore, such children do not respond well to the name, fulfill requests and may seem naughty. At the same time, parents may suspect autism in children. But a professional psychiatrist will definitely send the baby for an examination of auditory function.
Hearing aid helps solve problems.
Schizophrenia
Autism was previously considered one of the manifestations of schizophrenia in children. However, it is now clear that these are two completely different diseases. Schizophrenia in children begins later - at 5-7 years. The symptoms of this disease appear gradually. Such children have obsessive fears, talk to themselves, later delusions and hallucinations appear.