Rashes on 5 year old
Rashes on Children: When Should I Worry?
Childhood rashes are common, but that doesn’t mean they don’t freak you out any less as a parent. While most rashes do get better on their own, you may not be sure, especially if your child’s rash is accompanied by a fever or other symptoms.
“Rashes can be caused or associated with a variety of conditions, from mild conditions like heat rashes to serious conditions like meningitis,” said Nurul Hariadi, MD, a pediatric infectious diseases specialist at Banner Health Center. “Because of this, it’s important to know which should prompt a call to your child’s doctor or a visit to the ER.”
A good rule of thumb to remember is that a local rash is most likely caused by skin contact, exposure to certain materials or substances, and sometimes germs, such as diaper rash or an insect bite. A widespread rash is usually associated with a cause that affects the entire body such as measles.
Because many illnesses cause rashes, we put together a list of eight of the most common ones that occur in children, signs and symptoms that should prompt a visit to your child’s doctor or the ER, and an illustrative guide to keep on hand for quick reference.
8 common types of childhood rashes
Roseola
Roseola is one of the most common viral infections among children 6 months to 3 years of age. It starts with a fever for 2 to 3 days, followed by a rash after the fever is gone. Once the rash appears, your child is usually fine and doesn’t require treatment.
Fifth disease
Fifth disease, often called slapped cheek disease, is a common childhood infection caused by parvovirus. The symptoms are usually mild and include fever, upset stomach, headache and a rash that looks like the cheeks were slapped. It may be followed by a lacelike rash on the stomach, legs or arms. Older children or adults may experience joint pain. The virus clears up on its own, but your child may require pain reliever to treat symptoms.
Hand, foot & mouth disease
Hand, foot and mouth disease is caused by a group of viruses called enteroviruses and is a self-limiting disease, which means it will resolve without specific medication. It is spread by saliva, nasal mucus or fluid from an erupted blister. It causes tiny bumps, blisters or sores on the hands, feet, diaper area and in the mouth. It may also be associated with a fever and sore throat. If your child is able to take and keep fluids down and is active, you may observe them at home after discussing it with their doctor or triage nurse.
It is spread by saliva, nasal mucus or fluid from an erupted blister. It causes tiny bumps, blisters or sores on the hands, feet, diaper area and in the mouth. It may also be associated with a fever and sore throat. If your child is able to take and keep fluids down and is active, you may observe them at home after discussing it with their doctor or triage nurse.
Impetigo
Impetigo is one of the most common superficial bacterial skin infections in children. It usually appears as red bumps on the face that develop honey-colored crusts when they burst. Depending on the severity, it may require an antibiotic that is applied to the skin or taken by mouth.
MRSA
MRSA skin infection is caused by a type of Staphylococcus bacteria called Staphylococcus aureus that unfortunately causes infections that don’t respond well to antibiotics that treat less resistant S. aureus. Therefore, your child may need a different antibiotic. Recurrent boils can form and may require incision and drainage. Your child’s doctor may need to send the pus to a lab to check for MRSA.
Your child’s doctor may need to send the pus to a lab to check for MRSA.
Ringworm
Ringworm, or tinea corporis, is one of the most common fungal skin infections in children. It is scaly, red and itchy and may sometimes look like eczema. Depending on the location (skin versus scalp or nails), it may need antifungal medication that is applied on the skin or taken by mouth.
Scarlet fever
Scarlet fever, or scarlatina, is a bacterial infection that develops in some children who have Strep throat. It is most common in children 5 to 15 years old. Symptoms include a scarlet-colored rough rash that covers most of the body and feels like sandpaper, sore throat and high fever. Antibiotic is given to treat the illness.
Atopic dermatitis
Atopic dermatitis or eczema is not an infectious disease, it is a chronic skin condition. About 5% to 20% of children may have it, but many outgrow it by late childhood. Depending on age, it can appear on different areas of the body.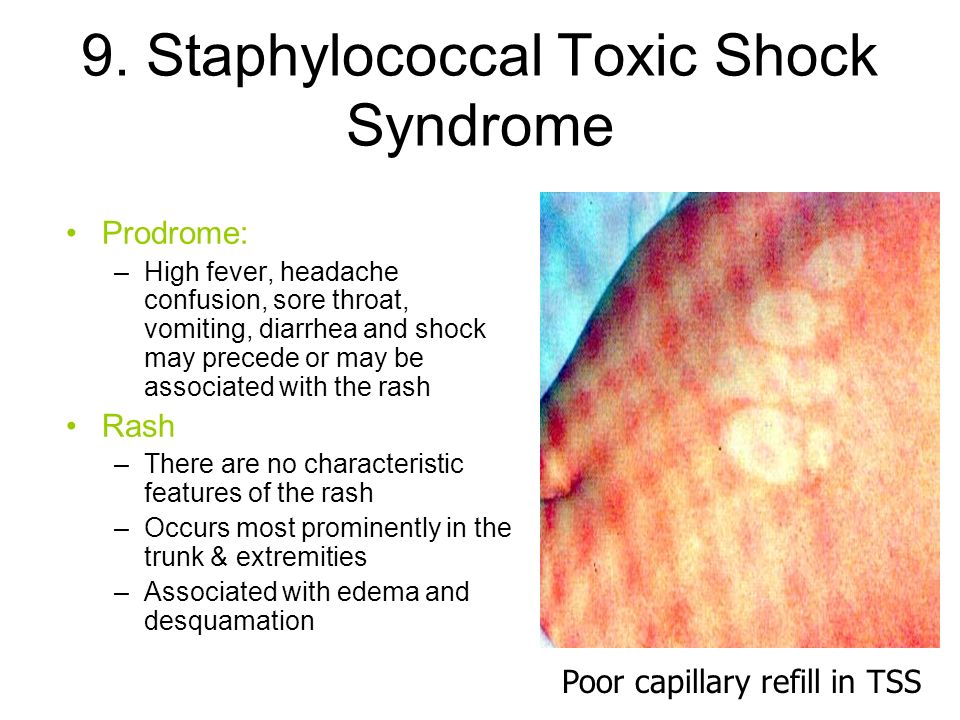 Common symptoms are red, inflamed and dry, itchy skin patches. Treatment will depend on your child’s symptoms and age.
Common symptoms are red, inflamed and dry, itchy skin patches. Treatment will depend on your child’s symptoms and age.
Got questions? Call your doctor
If your child has an unexplained rash, don’t hesitate to call their doctor. It’s better to talk to them about a rash (even if it ends up being nothing serious) than missing symptoms of a serious illness. To schedule an appointment, visit bannerhealth.com.
If you can’t reach the doctor, you can also call the Banner Nurse Now line at 844-259-9494 for free health care advice 24/7.
Other useful articles:
- Dermatologist-Recommended Skin Care Tips for Teens and Young Adults
- How Often Should My Child Really Bathe or Shower?
- Do's and Don'ts of Diaper Rashes (And How to Prevent Them)
Parenting Children's Health Infographics
Join the Conversation
12 Common Summertime Skin Rashes in Children
Sunny days and starlit evenings spent playing, splashing, and exploring can leave kids with more than warm summertime memories. Balmy weather also can lead to itchy, irritated skin.
Balmy weather also can lead to itchy, irritated skin.
Check out the list from the American Academy of Pediatrics (AAP) to see how you can help prevent, identify, and soothe these common summertime skin rashes.
1. Heat Rash
Heat rash (also known as prickly heat or miliaria) is seen most often in babies and young children when sweat gland pores become blocked and perspiration can't escape. The rash looks like patches of small pink or red bumps or blisters under clothing or spots where skin tends to fold—on the neck, elbows, armpits, or thighs—although heat rash can occur on other covered areas.
What parents can do:
Keep kids cool. Dress your child in clothing that keeps the skin cool and dry. If possible, use fans and air conditioning to avoid overheating.
Pay attention to hot spots. Wash areas of the skin that stay wet with sweat, urine, or drool with cool water. Pat them dry.

Keep skin bare. Leave areas open to air without clothing. Do not apply skin ointments.
2. Poison Ivy & Other Plant Rashes
Many children get a burning, intensely itchy rash where their skin touches plants—such as poison ivy, poison oak, sumac—containing a sticky oil called urushiol. An allergic skin reaction causes redness, swelling and blisters. Other plants—such as wild parsnip, giant hogweed, and citrus—contain chemicals that make skin hypersensitive to sunlight and cause a phytophotodermatitis rash.
What parents can do:
Prevent exposure. Teach your child what these plants look like and how to avoid them. Both poison ivy and poison oak have shiny green leaves that grow three to a stem, so you might share the rhyme: "Leaves of three, let them be." The sumac shrub has stems that contain 7-13 leaves arranged in pairs, while wild parsnip and giant hogweed have clusters of small, flat-topped yellow and white flowers.
 If you have younger children, inspect the parks they play in and have rash-causing plants removed.
If you have younger children, inspect the parks they play in and have rash-causing plants removed.Wash and trim. If your child comes into contact with these plants, wash all of his or her clothes and shoes in soap and water. Also, wash the area of the skin that was exposed with soap and water for at least 10 minutes after the plant or the oil is touched. To discourage scratching and further damage to the skin, keep your child's fingernails trimmed. This will also prevent the rash from spreading if there is still a small amount of oil under the fingernails.
Soothing salves. If the rash is mild, apply calamine lotion to cut down on the itching. Avoid ointments containing anesthetics or antihistamines—they can cause allergic reactions themselves. Another good option to reduce skin inflammation is 1% hydrocortisone cream.
Talk with your pediatrician. While mild cases can be treated at home, talk with your pediatrician if your child is especially uncomfortable, the rash is severe and/or isn't going away, if the rash is on your child's face or groin area, or if you notice signs of infection (i.
 e., fever, redness, swelling beyond the poison ivy or oak lesions).
e., fever, redness, swelling beyond the poison ivy or oak lesions).
3. Eczema
Eczema (also called atopic dermatitis or AD) is a chronic condition common in children that causes patches of dry, scaly red skin and tends to flare up during colder months when there's less moisture in the air. But dryness caused by air conditioning and pressurized planes during summer travel can cause problems, too. Overheating, sweating and chlorine in swimming pools also can trigger eczema.
What parents can do:
Moisturize. Apply fragrance-free creams or ointments at least once a day or more often if needed. After a bath or swimming, gently pat your child's skin with a towel and then apply moisturizer to his or her damp skin.
Dress wisely. Choose clothing made of soft, breathable fabrics like cotton when possible. Wash clothes in a detergent free of irritants such as perfumes and dyes.
Don't scratch.
 Keep your child's fingernails short and smooth, and remind him or her not to scratch. Scratching can make the rash worse and lead to infection.
Keep your child's fingernails short and smooth, and remind him or her not to scratch. Scratching can make the rash worse and lead to infection. Talk with your pediatrician. Ask your child's pediatrician if allergies, sometimes triggered by trees and plants that bloom during summer, could be a cause of the eczema. Your child's pediatrician may recommend medicines to help your child feel better and to keep the symptoms of eczema under control.
4. Insect Bites & Stings
Insects such as bees, wasps, mosquitos, fire ants, and ticks can cause itching and minor discomfort where they prick the skin. For some children, insect bites and stings can cause a severe allergic reaction called anaphylaxis—which includes a rash or hives and life-threatening symptoms such as airway swelling. (For children with a known allergy to insect bites and stings, it is important to have anaphylaxis emergency care plan in place). Other times, diseases spread by insects such as Lyme Disease, Rocky Mountain Spotted Fever, and Zika Virus can cause rashes and other health problems.
Other times, diseases spread by insects such as Lyme Disease, Rocky Mountain Spotted Fever, and Zika Virus can cause rashes and other health problems.
What parents can do:
Avoidance. When spending time outdoors, avoid scented soaps and shampoos and brightly colored clothing—they can attract insects. If possible, steer clear of areas where insects nest and gather (i.e., stagnant pools of water, uncovered food, and blooming flowers).
Use insect repellent. Products with DEET can be used on the skin, but look for family-friendly products that contain concentrations of no more than 30% DEET. Wash the insect repellent off with soap and water when your child returns indoors.
Cover up. When in wooded areas or in or near tall grass, stay on cleared trails as much as possible. Have your child wear a long-sleeved shirt, pants, and hat. Avoid wearing sandals in an area where ticks may live.

Look closely. Wear light-colored clothing to make it easier to spot ticks. After coming indoors, check for ticks on your child's skin—they often hide behind the ears or along the hairline.
Remove stingers and ticks. To remove a visible stinger from skin, gently scrape it off horizontally with a credit card or your fingernail. If you find a tick, gently grasp it with fine-tipped tweezers as close to the skin as possible. Without squeezing the tick's body, slowly pull it away from the skin. See How To Remove A Tick for more information.
Clean the skin. After the stinger or tick is out, clean the bitten area with rubbing alcohol or other first aid ointment.
Treat swelling. Apply a cold compress or an ice pack to any swelling for at least 10 minutes.
Help relieve the itch. Applying ice, along with calamine lotion or 1% hydrocortisone cream, can also help relieve itching.

5. Impetigo
Impetigo is a bacterial skin infection that's more common during hot, humid weather. It causes a rash that may have fluid-filled blisters or an oozing rash covered by crusted yellow scabs. Impetigo is more likely to develop where there is a break in the skin, like around insect bites.
What parents can do:
Clean and cover. Clean the infected area with soap and water. Cover the infected area loosely to help prevent contact that would spread the infection to others or to other parts of the body. Wash your own hands well after treating your child's sores.
Avoid scratching. Trim your child's fingernails and discourage scratching. A child can spread the infection to other parts of his or her body by scratching. You can cover the rash loosely with a bandage to discourage your child from touching the rash, but make sure air can flow through so the skin can heal.
Talk with your pediatrician.
 While mild cases may respond to over-the-counter antibiotics such as bacitracin or bacitracin-polymyxin, impetigo is usually treated with prescription antibiotics—either a skin cream or oral medication. Your pediatrician may order a skin culture (test of your child's skin) to determine which bacteria are causing the rash.
While mild cases may respond to over-the-counter antibiotics such as bacitracin or bacitracin-polymyxin, impetigo is usually treated with prescription antibiotics—either a skin cream or oral medication. Your pediatrician may order a skin culture (test of your child's skin) to determine which bacteria are causing the rash.
6. Swimmer's Itch
Swimmer's itch (also called clam digger's itch or cercarial dermatitis) may appear after playing in lakes, oceans, and other bodies of water. The rash is caused by microscopic parasites found in shallow, warmer water near the shoreline where children tend to stay. The parasites burrow into skin, and cause tiny reddish, raised spots on skin not covered by the swimsuit to appear. Welts and blisters may also form.
What parents can do:
Be aware. Don't swim near or wade in marshy areas where snails are commonly found. Try not to attract birds (by feeding them, for example) where your family swims.
 Birds may eat the snails and spread the parasites in the water.
Birds may eat the snails and spread the parasites in the water. Shower or towel dry. Shower or briskly rub the skin with a towel immediately after getting out of the water. The parasites start to burrow when the water on skin begins evaporating. If your skin child's skin stings with rubbing—and the rash appears under the swimsuit—he or she may instead have Seabather's Eruption from stinging larvae of sea critters such as jellyfish or sea anemone. Stop rubbing and shower instead.
Don't scratch. Trim your child's fingernails and discourage scratching. Home treatments such cool compresses on the affected areas, Epsom salt or oatmeal baths, or baking soda paste may help to relieve the discomfort. If itching is severe, talk with your child's pediatrician. He or she may suggest prescription-strength lotions or creams to reduce your child's symptoms.
7. Cutaneous Larva Migrans (Sandworms)
Sandworms may be present in sand contaminated with feces from pets or stray animals. When a child stands or sits in contaminated sand on a beach or in a sandbox, the worms may burrow under the skin, usually around the feet or buttocks. Lines of itchy, reddish rash known as a creeping eruption appear as the worms move under the skin, up to a few centimeters a day. The condition is more common subtropical and tropical areas such as the Caribbean, as well as parts of the southwestern United States.
When a child stands or sits in contaminated sand on a beach or in a sandbox, the worms may burrow under the skin, usually around the feet or buttocks. Lines of itchy, reddish rash known as a creeping eruption appear as the worms move under the skin, up to a few centimeters a day. The condition is more common subtropical and tropical areas such as the Caribbean, as well as parts of the southwestern United States.
What parents can do:
Keep shoes on. Don't let your child play on beaches where people walk their dogs. If your family goes on an outing to a designated pet-friendly beach, make sure your child keeps shoes on and doesn't sit in the sand without a blanket or towel.
Talk with your pediatrician. Your pediatrician can prescribe anti-parasitic medications such as albendazole or ivermectin to treat the rash. Without treatment, the larvae usually will die off in 5 to 6 weeks. Your pediatrician may suggest a cream to help relieve itching.

8. Folliculitis (Hot Tub Rash)
Folliculitis (hot tub rash) is an itchy, pimply rash that occurs when bacteria in unclean pools and hot tubs gets into hair follicles on the skin. The area where hairs grow from the skin becomes infected and inflamed, sometimes forming small, pus-filled blisters. A similar rash may come from wearing a damp swimsuit that wasn't washed and dried well after previous use. Hot rub rash typically starts 12-48 hours after being in a hot tub.
What parents can do:
Avoid dirty pools. If you're unsure whether the acid and chlorine levels are properly controlled in a heated pool, don't allow your child to go in.
Don't allow young children in spas or hot tubs. In addition to the risk for drowning and overheating, young children are also at higher risk of bacterial skin infection because they tend to spend more time in the water than teens or adults.
Talk with your pediatrician.
 Hot tub rash usually clears up without medical treatment. In the meantime, warm compresses and an over-the-counter anti-itch cream recommended by your pediatrician can help your child be more comfortable. If your child's rash lasts more than a few days, talk with your pediatrician.
Hot tub rash usually clears up without medical treatment. In the meantime, warm compresses and an over-the-counter anti-itch cream recommended by your pediatrician can help your child be more comfortable. If your child's rash lasts more than a few days, talk with your pediatrician.
9. Molluscum Virus
Molluscum contagiosum is a viral infection that causes pearly bumps on the skin on a child's chest, back, arms or legs. The dome-shaped bumps, also known as "water warts," may have a dimple in the center. The poxvirus that causes the bumps is more common in hot, humid climates. Some studies suggest the infection may spread in contaminated swimming pools.
What parents can do:
Wait it out. In most cases, molluscum contagiosum does not need treatment. The bumps usually will go away in 6 to 12 months.
Stop the spread. A child with molluscum contagiosum should not share towels, bedding, or clothing with others to avoid spreading the virus.
 The bumps are contagious as long as they are present.
The bumps are contagious as long as they are present.Avoid scratching. Scratching the bumps can spread the virus and cause a second, bacterial infection where the skin is open.
10. Juvenile Plantar Dermatosis (Sweaty Sock Syndrome)
A smooth, reddened rash on your child's feet, sometimes with peeling, cracking skin or scaly skin, could be from a condition called Juvenile Plantar Dermatosis (Sweaty Sock Syndrome). It happens when feet get wet and then dry quickly, again and again—like when shoes are taken on and off coming in and out of the house during summer.
What parents can do:
Breathable footwear. Reduce how often the feet go from wet to dry quickly by having your child wear open or more breathable footwear made of materials like mesh or cotton (i.e., water shoes) and/or thicker more absorbent socks.
Apply ointment. Applying moisturizing ointment or an over-the-counter steroid cream to the affected areas of your child's foot immediately after taking shoes off or getting out of water can help.
 If the condition does not improve, or if you notice any sign of infection where your child's skin is cracking, talk to your pediatrician.
If the condition does not improve, or if you notice any sign of infection where your child's skin is cracking, talk to your pediatrician.
11. Tinea (Ringworm)
Despite having "worm" in its misleading name, tinea (ringworm) is an infection caused by a fungus that thrives in warm, damp conditions. It is similar to athlete's foot and jock itch and can appear on a child's scalp or other parts of the body. It's called ringworm because the rash from the infection tends to form round or oval spots that become smooth in the center as they grow while the border remains red and scaly. The fungus can spread quickly among student athletes, especially during sweaty, summertime practices and games, when they share sports equipment and locker rooms.
What parents can do:
Stop the spread. Check and treat any pets that may have the fungus—look for scaling, itchy, hairless areas on their fur. Family members, playmates, or schoolmates who show symptoms also should be treated.
 Do not allow your child to share combs, brushes, hair clips, barrettes, or hats. Make sure mats used in sports like wrestling and gymnastics are properly disinfected after use.
Do not allow your child to share combs, brushes, hair clips, barrettes, or hats. Make sure mats used in sports like wrestling and gymnastics are properly disinfected after use.Talk with your pediatrician. A single ringworm patch on the body can be treated with an over-the-counter cream recommended by your pediatrician. If there are any patches on the scalp or more than one on the body, or if the rash is getting worse while being treated, your pediatrician may prescribe a stronger medication and special shampoo.
12. Hand, Foot & Mouth Disease
Many parents assume virus season winds down after winter. But some viral illnesses, such as hand, foot, and mouth disease, are more common during summer and early fall. Outbreaks are most common in younger children and can spread in child care centers, preschools, and summer camps. Caused by Enterovirus coxsackie, the illness starts with a fever, sore throat, and runny nose—much like the common cold—but then a rash with tiny blisters may appear on any or all the following places on the body:
In the mouth (inner cheeks, gums, sides of the tongue or back of the mouth)
Fingers or palms of hands
Soles of feet
Buttocks
Symptoms are the worst in the first few days, but they are usually gone within a week.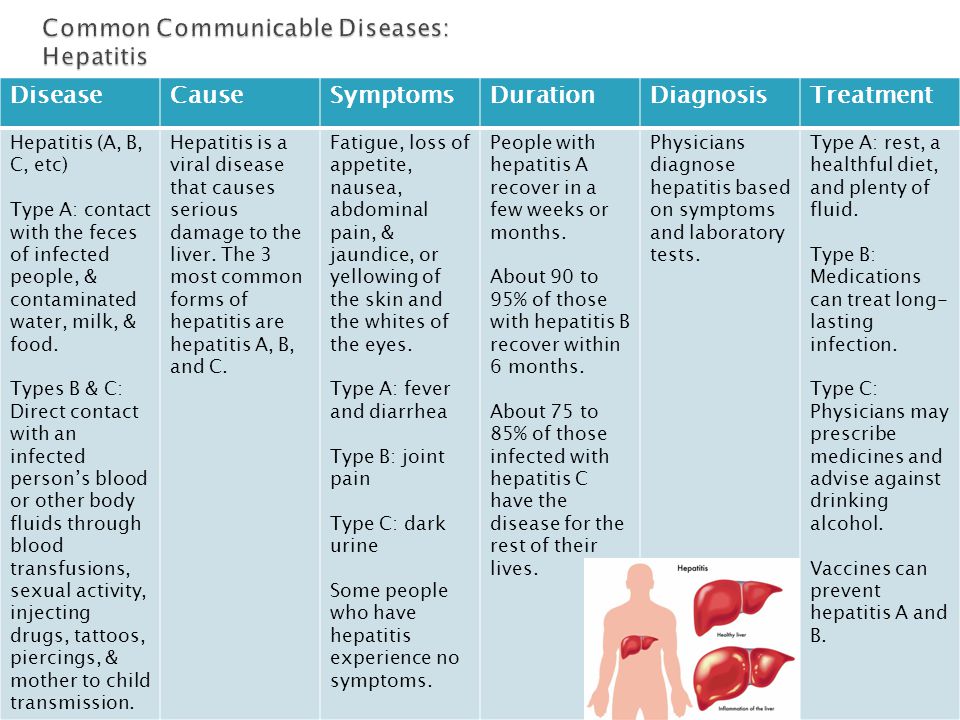 Peeling skin on the fingers, toes, and nails may begin after a week or two, but it is harmless. Parents of children with a history of atopic dermatitis or eczema should be aware that their children may be prone to a more severe outbreak.
Peeling skin on the fingers, toes, and nails may begin after a week or two, but it is harmless. Parents of children with a history of atopic dermatitis or eczema should be aware that their children may be prone to a more severe outbreak.
What parents can do:
Monitor symptoms. Be sure to call your pediatrician if your child's fever lasts more than 3 days or if he or she is not drinking fluids. If symptoms are severe, your pediatrician may collect samples from your child's throat for lab testing.
Ease the pain. For fever and pain, the pediatrician may also recommend acetaminophen or ibuprofen. Liquid mouth-soothing remedies may be useful to alleviate mouth ulcer pain. Do not use regular mouthwashes, because they sting.
Avoid dehydration: Children with hand, foot, and mouth disease need to drink plenty of fluids. Call your pediatrician or go to the ER if you suspect your child is dehydrated.
 See Signs of Dehydration in Infants & Children for more information.
See Signs of Dehydration in Infants & Children for more information. Inform others. Tell child care providers and playmates' parents to watch for symptoms of the illness. Children with hand, foot, and mouth disease may spread the virus through the respiratory tract (nose, mouth and lungs) for 1-3 weeks, and in the stool for weeks to months after the infection starts. Once a child's fever has gone away and he or she is feeling better, there is no need to keep him or her home unless there are still open and oozing blisters. See When to Keep Your Child Home from Child Care for more information.
Remember…
Protecting your child's skin is a year-round concern, but it's especially important in the summer months when so much skin is exposed and vulnerable. Fortunately, many summertime rashes clear up quickly on their own. Be sure to talk with your pediatrician about any rash that you're unsure about—especially if you don't know what caused it, if it is making your child feel miserable or doesn't clear up quickly, or if it shows signs of infection or is accompanied by any shortness of breath.
Additional Information:
- Summer Safety Tips: Staying Safe Outdoors
- Antibiotic Prescriptions for Children: 10 Common Questions Answered
- American Academy of Dermatology
- American College of Allergy, Asthma & Immunology
- Society for Pediatric Dermatology
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and medicines! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies. Doctors constantly improve their qualifications, undergo internships abroad.
Ultimate treatment safety
We made pediatric medicine safe! All our staff work according to the most stringent international standards JCI
We have fun, like visiting best friends
Game room, cheerful animator, gifts after the reception. We try to make friends with the child and do everything to make the little patient feel comfortable with us.
You can make an appointment by calling or by filling out the form on the site
Other Pediatric services
- Pediatrician's consultation
- Child Health Management Program
Frequent calls
- Acute bronchiolitis in children: diagnosis and treatment
- SARS
- Angina streptococcal tonsillitis
- Frequently ill child
- Intestinal infections
- Pneumonia (pneumonia) in children
- Colic
- Feeding problems
- Prolonged cough in a child: diagnosis and treatment
- Acute bronchitis in children: diagnosis and treatment
- Pneumonia (pneumonia) in children: diagnosis and treatment
- False croup in a child
- Coxsackie virus in a child
- The child was bitten by a tick! What to do?
Online payment
Documents online
Online services
Have you noticed a rash on your child's skin? Contact your pediatrician to find out the reason. Redness itself is not a disease, but can signal internal disorders in the body.
In the article we will talk about the causes, types and methods of treating rash in children.
What causes a rash?
Rashes on the skin of a child do not appear just like that. In any case, this is the body's immune response to the influence of external or internal factors.
Different types of rashes are similar in appearance, especially for parents who are faced with a problem for the first time. But if some spots are completely harmless, then others can threaten health. That is why it is important to understand their origin.
The main causes of the rash:
- Reaction to stimuli. If the child is dressed too warmly, the rash may be due to overheating and excessive sweating. Most often, prickly heat occurs on the back, neck, chest and abdomen.
The same goes for the diaper. If you do not arrange air baths and do not change it to a new one in time, the skin in the inguinal region and on the buttocks will disappear.
Prickly heat does not require special treatment, it is only important to eliminate the irritating factor. - Physiological. In the first months of life, breastfed babies are often diagnosed with infantile acne. With milk, maternal hormones enter the body, which activate the sebaceous glands. As a result, small comedones and pimples appear on the face. Over time, they disappear.
- Viral and bacterial infections. Measles, chicken pox, rubella, herpes simplex virus, roseola, scarlet fever, meningococcal infection, fungus and streptoderma. These diseases are characterized by specific rashes on the arms, legs and other parts of the body. Many are accompanied by itching and a steady increase in body temperature for 3-5 days.
- Allergy. Urticaria and various types of atopic dermatitis: eczema, diathesis, neurodermatitis.
Spots without suppuration may cover the head, face, shoulders, armpits, back and groin.
- Comorbidities. Rash may indicate gastrointestinal, vascular, or kidney problems.
Eruptions in children
Depending on the appearance, localization and size, the following types are distinguished:
- Tubercles.
- Vesicles.
- Blisters.
- Purples.
- Pustules.
- Stains.
- Erythema.
Why are rashes dangerous?
With any kind of redness, it is important to consult a doctor to determine the cause. The most dangerous rash of viral and bacterial origin, especially if there are other symptoms:
- cough;
- sore throat;
- enlarged tonsils and lymph nodes;
- tearing;
- temperature increase.
Without timely treatment, complications are possible. For example, measles can lead to pneumonia, meningitis, and hearing loss.
With skin allergic reactions, it is important to determine the source of the problem. A neglected allergy can cause swelling and suffocation.
What should parents do?
If you find bumps, vesicles or redness on the child's body, proceed in sequence:
- examine the entire skin;
- estimate the area and number of lesions;
- check throat, tonsils and take temperature;
- remember what the child ate, did or touched before the redness appeared.
Is the baby already talking? Then try to figure out what's bothering him. Ask about the sensations (spots hurt, itch) and general well-being.
If you have a high temperature, call your doctor at home. It could be a contagious infectious disease that definitely shouldn't be spread. But even if the child looks healthy and vigorous, do not postpone a visit to a specialist - make an appointment at a medical facility.
It is strictly forbidden to self-medicate, comb or squeeze out neoplasms.
Diagnostics
Diagnostic measures help to choose the right therapy. First, the pediatrician prescribes to small patients:
- blood, urine and feces analysis;
- skin scrapings;
- collection of exudate samples, in the presence of watery formations.
Based on the results, the doctor makes a preliminary conclusion and sends the parents with the child for examination to narrow specialists: an allergist, dermatologist, endocrinologist or gastroenterologist.
Treatment
Treatment of rashes is carried out in a complex way to eliminate both the symptoms and the cause. A young patient is prescribed anti-allergic, anti-inflammatory or hormonal drugs in the form of tablets, ointments or suspensions.
Along with this, parents are advised to reconsider nutrition and living conditions:
- exclude potentially allergenic products;
- use gentle detergents for the body, dishes and laundry;
- wear loose clothing made from natural fabrics;
- dress the child according to the weather, do not wrap too tightly to avoid overheating;
- change the diaper in a timely manner, arrange air baths and lubricate the groin area with a special cream.