Procedure to turn a breech baby
External cephalic version (ECV) | Pregnancy Birth and Baby
External cephalic version (ECV) | Pregnancy Birth and Baby beginning of content4-minute read
Listen
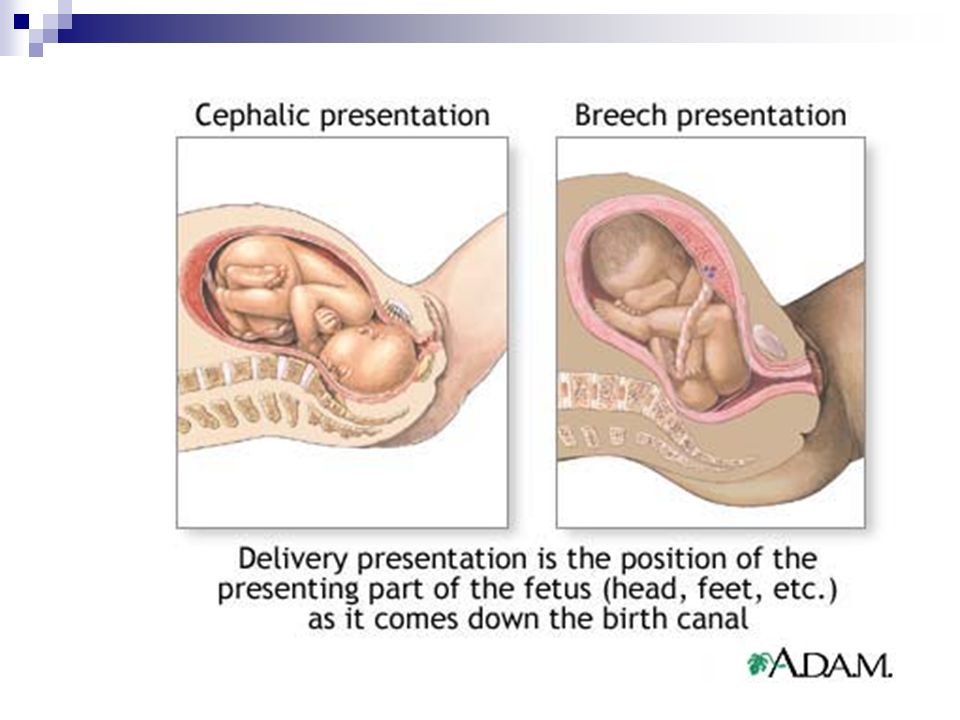
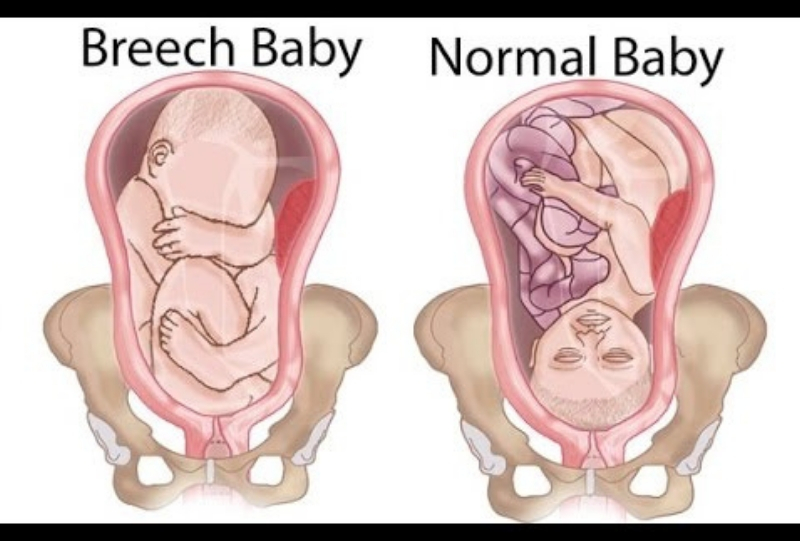
Giving birth is more challenging for babies who are bottom-down, or breech, when labour starts. This page explains external cephalic version (ECV), which tries to turn breech babies to the head-down position ready for a normal vaginal birth.
The breech position
Throughout your pregnancy, your baby repeatedly turns around and changes position. Most babies will settle into a head-down, or 'cephalic', position by 36 weeks of pregnancy. But about 3 in 100 babies are in a breech position at 36 weeks. For these babies, birth would be more difficult than if they were in the cephalic position.
Some breech babies turn naturally in the last month of pregnancy. If this is your first baby, the chance of the baby turning itself after 36 weeks is about 1 in 8. If this is your second or subsequent baby, the chance is about 1 in 3.
If your baby is still in a breech position at 36 weeks, your doctor or midwife might suggest you consider an external cephalic version, or ECV. The aim is to turn your baby so that it is head-down when labour starts.
An ECV is performed after 37 weeks of pregnancy.
Can anyone have an ECV?
Most women can have an ECV if they have a healthy pregnancy with a normal amount of amniotic fluid. However, an ECV is not recommended if:
- you need a caesarean for other reasons
- you have had vaginal bleeding in the previous 7 days
- the baby's heart rate is not normal
- a complicated pregnancy
- you are having twins or triplets
- you have an unusually shaped uterus
- you recently had vaginal bleeding
- you have placenta praevia (your placenta is growing close to, or on, your cervix)
- other health conditions, like high blood pressure or diabetes
ECV might also not be recommended if your unborn baby is unwell or not growing well.
If you have had a caesarean section before, an ECV can still be performed but there are special considerations that need to be discussed with your doctor.
How is an ECV performed?
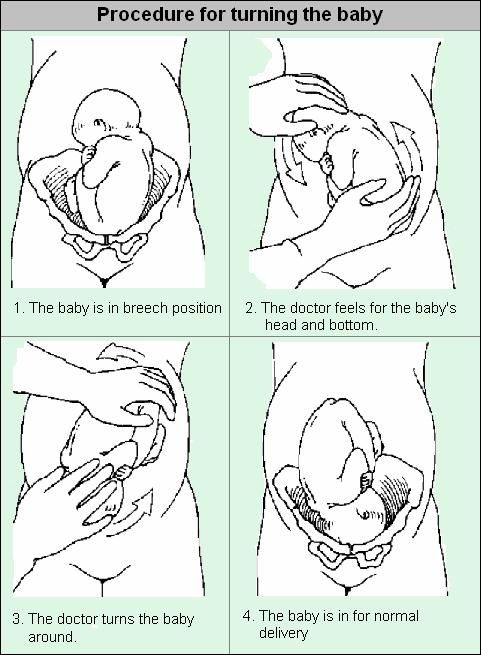
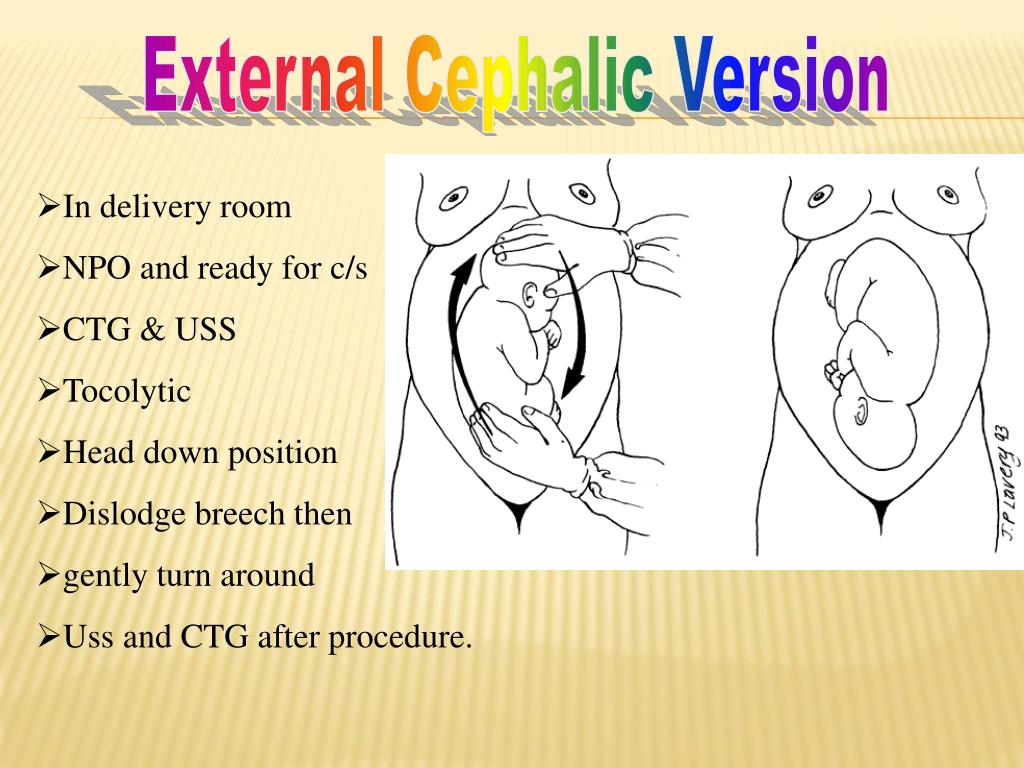
A health professional with appropriate expertise, usually an obstetrician, puts their hands on your abdomen to try to turn your baby into a head-down position.
A cardiotocograph, or CTG, will monitor your baby’s wellbeing for 20 to 30 minutes before the procedure.
A small needle will be inserted into your hand so that medication to relax your uterus can be administered directly into your vein.
An obstetrician will then perform an ultrasound to confirm the position of the baby, and then attempt to turn the baby by pressing their hands firmly on your abdomen. Some women find this uncomfortable, while others don’t. The pressure on your abdomen lasts a few minutes. If the first attempt is unsuccessful, the obstetrician might try again.
The CTG might be applied again after the procedure to assess your baby’s wellbeing before you leave.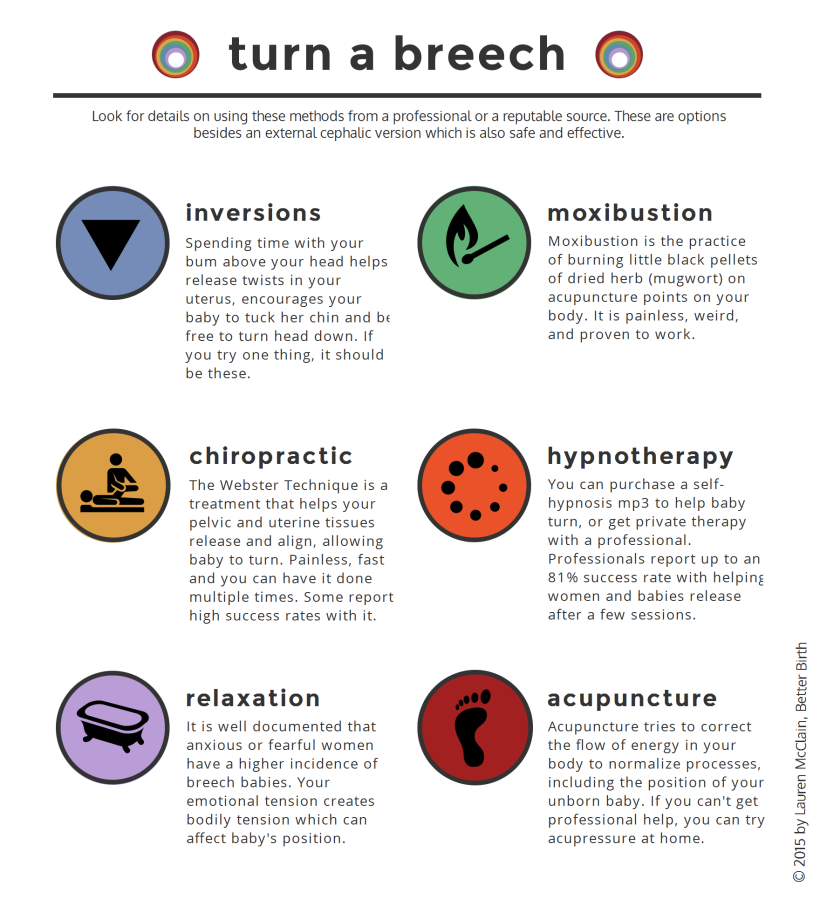
It usually takes about 3 hours from start to finish.
Where would I have an ECV?
Although complications from an ECV are rare, it is recommended that the procedure is done by an experienced health professional, in a hospital where there are facilities for emergency caesarean section. About 1 in 1,000 women go into labour after an ECV. About 1 in 200 women need an immediate caesarean section.
Will ECV work?
ECV can work, although there is no guarantee of success. If it does work, there is a small chance the baby will turn again to the breech position. But overall, ECV improves a woman’s chances of having a vaginal birth.
What happens if ECV doesn’t work?
A vaginal birth may still be possible, depending on your individual clinical circumstances and the type of breech position your baby is in. Talk to your doctor or midwife about your options.
What other methods are there to potentially turn my baby from a breech position?
Some people think that you might be able to encourage your baby to turn by holding yourself in certain positions, such as kneeling with your bottom in the air and your head and shoulders flat to the ground. Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work. Discuss with your doctor or midwife before having any treatment during pregnancy.
Other options you might hear include acupuncture, a Chinese herb called moxibustion and chiropractic treatment. There is no good evidence that these work. Discuss with your doctor or midwife before having any treatment during pregnancy.
Sources:
Mater Hospital Brisbane (Pregnancy: External Cephalic Version), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy), BioMed Central (Does moxibustion work? An overview of systematic reviews (BMC Research Notes 20103:284)), Department of Health (Clinical practice guidelines: Pregnancy care), SA Department for Health and Ageing (Perinatal practice guideline: Breech presentation), NSW Health (External Cephalic Version (ECV) for Breech Presentation)Learn more here about the development and quality assurance of healthdirect content.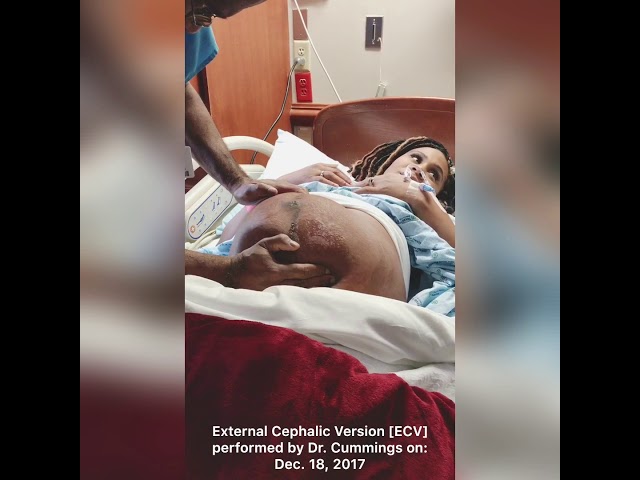
Last reviewed: April 2020
Back To Top
Related pages
- Breech birth
- Breech pregnancy
Need more information?
External Cephalic Version for Breech Presentation - Maternal, child and family health
This information brochure provides information about an External Cephalic Version (ECV) for breech presentation
Read more on NSW Health website
Breech presentation and turning the baby
In preparation for a safe birth, your health team will need to turn your baby if it is in a bottom first ‘breech’ position.
Read more on WA Health website
Breech pregnancy
When a baby is positioned bottom-down late in pregnancy, this is called the breech position.
Read more on Pregnancy, Birth & Baby website
Malpresentation
Malpresentation is when your baby is in an unusual position as the birth approaches. Sometimes it’s possible to move the baby, but a caesarean maybe safer.
Read more on Pregnancy, Birth & Baby website
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems. Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 35
You'll probably be having lots of Braxton Hicks contractions by now. It's your body's way of preparing for the birth. They should stop if you move position.
They should stop if you move position.
Read more on Pregnancy, Birth & Baby website
Anatomy of pregnancy and birth - pelvis
The pelvis helps carry your growing baby and is especially tailored for vaginal births. Learn more about the structure and function of the female pelvis.
Read more on Pregnancy, Birth & Baby website
Rhesus D negative in pregnancy
Find out what being Rhesus D negative could mean for your baby and how it is treated.
Read more on Pregnancy, Birth & Baby website
Placental abruption - Better Health Channel
Placental abruption means the placenta has detached from the wall of the uterus, starving the baby of oxygen and nutrients.
Read more on Better Health Channel website
Glossary of pregnancy and labour
Glossary of common terms and abbreviations used in pregnancy and labour.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.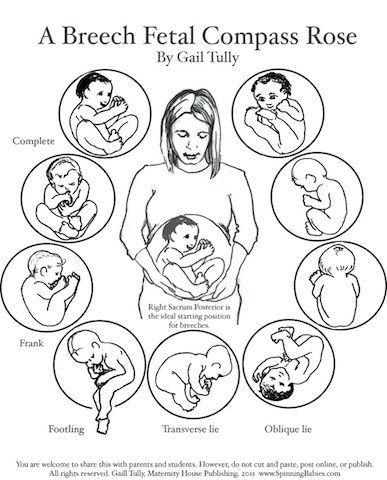
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
What Can I Do if My Baby is Breech?
Right before birth, most babies are in a headfirst position in the mother’s uterus. Sometimes, the baby is in a bottom-first (or feet-first) position. This is called a breech birth or breech baby. Babies can be breech early in pregnancy. Most of them turn on their own to be headfirst by the time of delivery.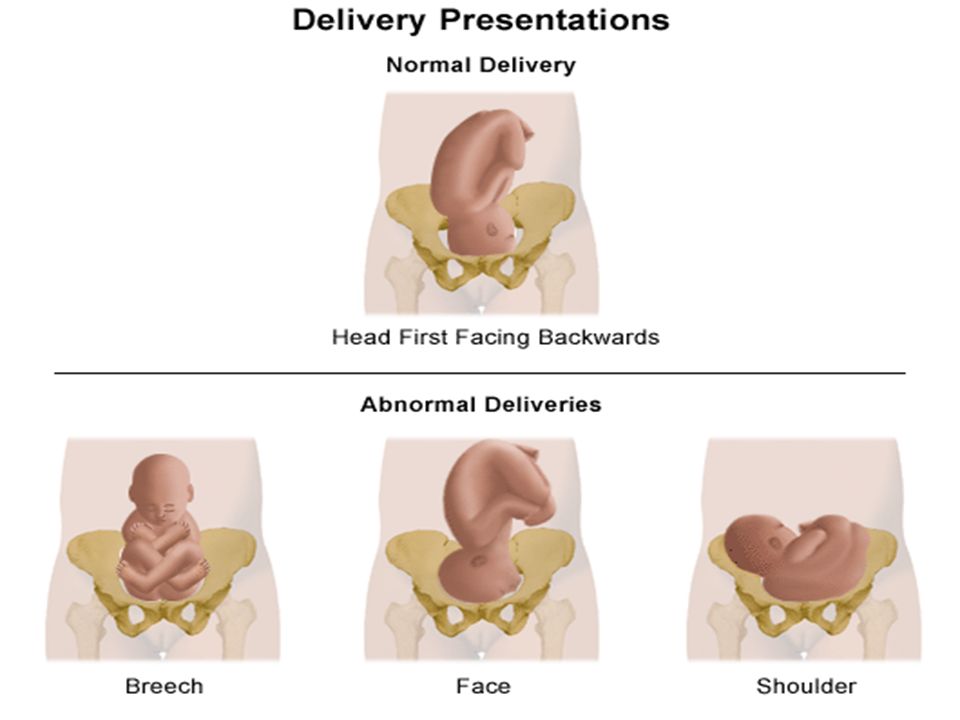 As you get closer to your due date, your doctor will be able to tell if your baby is breech. They can check by a physical exam, ultrasound, or both.
As you get closer to your due date, your doctor will be able to tell if your baby is breech. They can check by a physical exam, ultrasound, or both.
Babies are more likely to be breech if:
- They are early, or premature.
- They are part of a multiple birth (two or more babies).
- There is an abnormal level of amniotic fluid.
- The mother has an abnormal shaped uterus.
It’s important to see your doctor regularly throughout your pregnancy. Your doctor can tell if your baby is breech and help plan what to do. There are several ways to try and turn your baby. Your doctor may suggest methods to help turn the baby naturally. These could be the first attempt if it is still early and there are no health problems or concerns. Another option is to do a procedure called external cephalic version. Or your doctor may want to schedule a cesarean delivery (C-section).
External cephalic version (ECV)ECV is one way to turn a baby from breech position to head down position while it’s still in the uterus. It involves the doctor applying pressure to your stomach to turn the baby from the outside. Sometimes, they use ultrasound as well.
It involves the doctor applying pressure to your stomach to turn the baby from the outside. Sometimes, they use ultrasound as well.
Many women who have normal pregnancies can have ECV. You should not have ECV if you have:
- Vaginal bleeding.
- A placenta that is near or covering the opening of the uterus.
- A low level of fluid in the sac that surrounds and protects the baby.
- An abnormal fetal heart
- Premature rupture of the membranes.
- Twins or other multiples pregnancy.
ECV usually is done in a hospital toward the end of pregnancy, around 37 weeks. Before the procedure, the doctor will do an ultrasound to confirm that your baby is breech. They also will monitor your baby’s heart rate to make sure it is normal. The doctor may give you medicine to relax the muscles in your uterus. This can help decrease discomfort and increase the success of turning your baby. The medicine may be given as a shot or through a vein (IV). It is very safe, with no risk to your baby.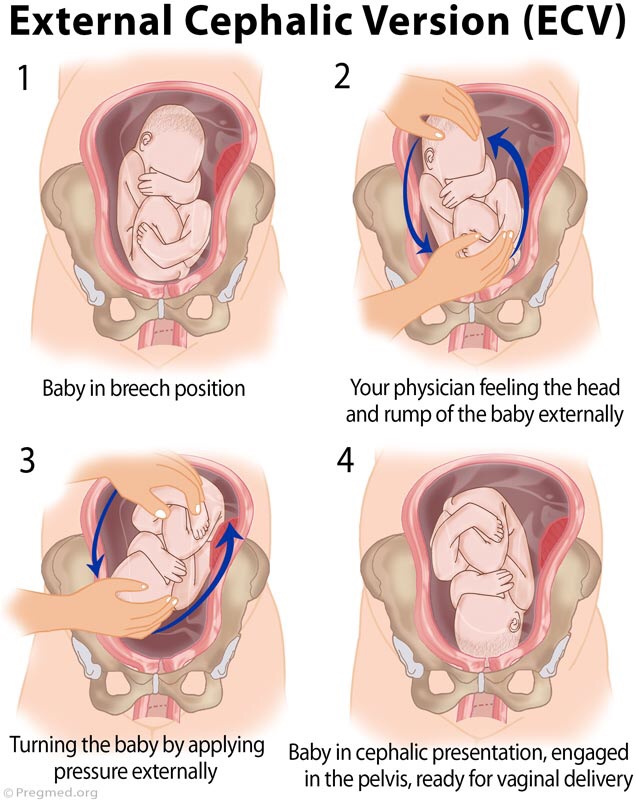
During the ECV, you will lie down and the doctor will place his or her hands on your stomach. After locating the baby’s head, the doctor will gently try to turn the baby to the headfirst position.
After the procedure, your doctor will monitor your baby’s heart rate again. If the procedure is successful, you shouldn’t have to stay in the hospital. Your chance of having a normal vaginal delivery is high. However, there is a chance that the baby can turn back around to the breech position. The success rate of ECV depends on several factors:
- How close you are to your due date.
- How much fluid is around your baby.
- How many pregnancies you have had.
- How much your baby weighs.
- How the placenta is positioned.
- How your baby is positioned.
If the procedure is not successful, your doctor will talk to you about delivery. He or she will discuss the pros and cons of having a vaginal delivery or a C- section. The doctor may suggest repeating the ECV.
The risks of ECV are small, but include:
- Early onset labor.
- Premature rupture of the membranes.
- Minor blood loss for either the baby or the mother.
- Fetal distress leading to an emergency C-section.
Some people look to natural ways to try and turn their baby. These methods include exercise positions, certain stimulants, and alternative medicine. They may help but there is no scientific evidence that they work.
- Breech tilt, or pelvic tilt: Lie on the floor with your legs bent and your feet flat on the ground. Raise your hips and pelvis into a bridge position. Stay in the tilt for about 10 to 20 minutes. You can do this exercise three times a day. It may help to do it at a time when your baby is actively moving in your uterus.
- Inversion: There are a few moves you can do that use gravity to turn the baby. They help relax your pelvic muscles and uterus.
 One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity.
One option is to rest in the child’s pose for 10 to 15 minutes. A second option is to gently rock back and forth on your hands and knees. You also can make circles with your pelvis to promote activity. - Music: Certain sounds may appeal to your baby. Place headphones or a speaker at the bottom of your uterus to encourage them to turn.
- Temperature: Like music, your baby may respond to temperature. Try placing something cold at the top of your stomach where your baby’s head is. Then, place something warm (not hot) at the bottom of your stomach.
- Webster technique: This is a chiropractic approach. It is meant to align your pelvis and hips, and relax your uterus. The goal is to promote your baby to turn.
- Acupuncture: This is a form of Chinese medicine. It involves placing needles at pressure points to balance your body’s energy. It can help relax your uterus and stimulate your baby’s movement.
It is not always possible to turn your baby from being breech. Some breech babies can be safely delivered through the vagina, but usually doctors deliver them by C-section. Risks involved with a C-section include bleeding and infection. There also can be a longer hospital stay for both the mother and her baby.
Other risks can occur for breech babies who are born vaginally. These include:
- An injury during or after delivery.
- An injury where the baby’s hip socket and thigh bone become separated.
- Problems with the umbilical cord. For example, the umbilical cord can be flattened during delivery. This can cause nerve and brain damage due to a lack of oxygen.
- How can I tell if my baby is breech?
- If my baby is breech, does it mean there is something wrong with them?
- What are the benefits and risks of ECV?
- What are my options for delivery if my baby remains in the breech position?
- What are the health risks to my baby and me if they are born breech?
Copyright © American Academy of Family Physicians
This information provides a general overview and may not apply to everyone.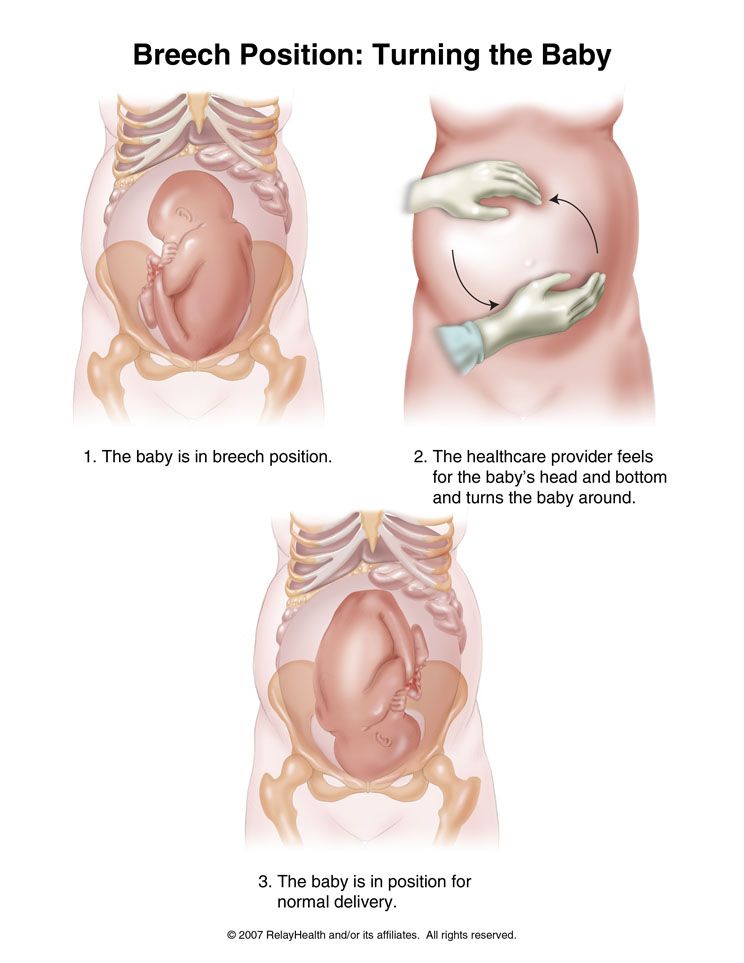 Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
Talk to your family doctor to find out if this information applies to you and to get more information on this subject.
The problem of breech presentation of the fetus. External obstetric rotation of the fetus on the head.
Breech presentation of the fetus occurs in 3% -5% of cases at full-term pregnancy. Vaginal delivery with breech presentation is associated with high risks both on the mother's side and on the fetus's side. Thus, breech presentation is currently considered pathological, even if the conditions necessary for childbirth through the birth canal are ideally met, and the fetus is relatively small relative to the size of the mother's pelvis. During vaginal delivery, the arms and head of the fetus may tilt back, which can lead to injury.
Currently the most common method of delivery in breech presentation is a caesarean section (90%). Among the indications for the use of caesarean section, breech presentation ranks third among others in the world. However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
However, this the operation does not make it possible to completely eliminate the risk of trauma to the fetus, since when it is removed, it is also possible to tilt the arms and head of the fetus, and their release requires the use of complex manipulations.
To correct breech presentation today, the world is using EXTERNAL OBTETAL TURNING OF THE FETUS ON THE HEAD proposed at the end the century before last by the Russian obstetrician Arkhangelsky B.A.
External obstetric cephalic rotation (EFRT) is a procedure during which the doctor turns the fetus from the outside through the wall of the uterus breech presentation in the head. A successful attempt at NAPP allows women to give birth on their own, avoiding a caesarean section.
What is required for external cephalic fetal rotation?
External obstetric rotation of the fetus on the head is performed before the onset of labor, usually starting from 36 weeks of pregnancy.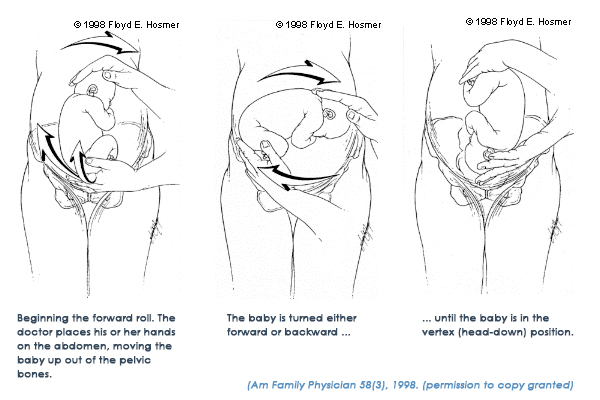
It is necessary to consult a doctor and conduct an ultrasound examination to confirm the fact breech presentation of the fetus and determine the conditions for NAPP, starting from 34-35 weeks of pregnancy.
| The operation of external rotation of the fetus on the head in breech presentation |
When NAPP is possible:
- From 36 to 37 weeks, since with earlier use, it is likely that it will return to the breech presentation.
- In the presence of a singleton pregnancy.
- Subject to the mobility of the buttocks of the fetus (if they are tightly pressed against the entrance to the mother's pelvis, it will be extremely difficult to change the position of the fetus).
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Sufficient amount of amniotic fluid. With oligohydramnios, this manipulation can be traumatic for the fetus, while with polyhydramnios there is a high probability of a reverse rotation of the fetus in a breech presentation.
- Fetal head flexed
When NAPP is not possible:
- With the outflow of amniotic fluid.
- If the patient has contraindications to the use of drugs used to relax the uterus (tocolysis).
- In the presence of obstetric indications or indications from the health of the mother for delivery by caesarean section.
- With the extensor position of the fetal head.
- If the fetus has congenital developmental features.
- With multiple pregnancy.
- In the presence of structural features of the uterus in a pregnant woman
However, in addition to this, there are a number of factors that may favor or, on the contrary, serve as a contraindication to external obstetric turning the fetus on the head, and which can only be determined by a doctor during a direct examination of a pregnant woman.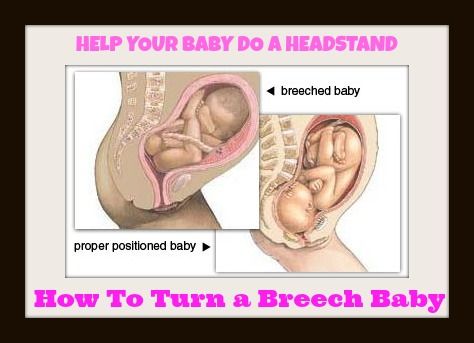
How NAPP is conducted
For manipulation, hospitalization in the maternity hospital is necessary. Preliminarily, an additional examination of the pregnant woman is carried out in the required volume, including ultrasound.
During the NAPP:
Immediately before the start of the manipulation, a CTG is recorded to assess the condition of the fetus.
Drugs are administered to prevent uterine contractions (tocolytics).
Further, under constant ultrasound and KGT control, as well as the continued administration of drugs that relax the uterus, the doctor performs a turn.
Holding both hands on the surface of the pregnant woman's abdomen, one on the head of the fetus, and the other on the buttocks of the fetus, the doctor pushes and rotates the fetus to the upside down position. A pregnant woman may feel some discomfort during the procedure.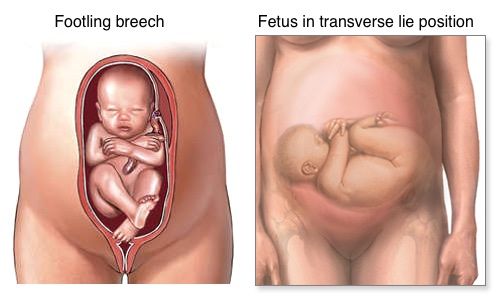 The degree of discomfort depends on the individual sensitivity of each patient.
The degree of discomfort depends on the individual sensitivity of each patient.
After the procedure is successfully completed, the CTG is recorded again, to make sure that the fetus feels well and has successfully undergone the procedure. Usually during the day, the condition of the mother and fetus is monitored, after which the patient is discharged and continues the pregnancy until spontaneous delivery occurs.
If the doctor notices a deterioration in the condition of the fetus according to the monitoring data, then the procedure is immediately stopped.
If the first attempt was not successful, your doctor may suggest another attempt if the fetus is in good health.
APP is performed ONLY in a maternity ward where there is an opportunity for an emergency delivery, if necessary.
Risks associated with NAPP
Subject to constant monitoring of the condition of the fetus, constant tocolysis (administration of drugs that relax the uterus) The risks associated with this procedure are minimal.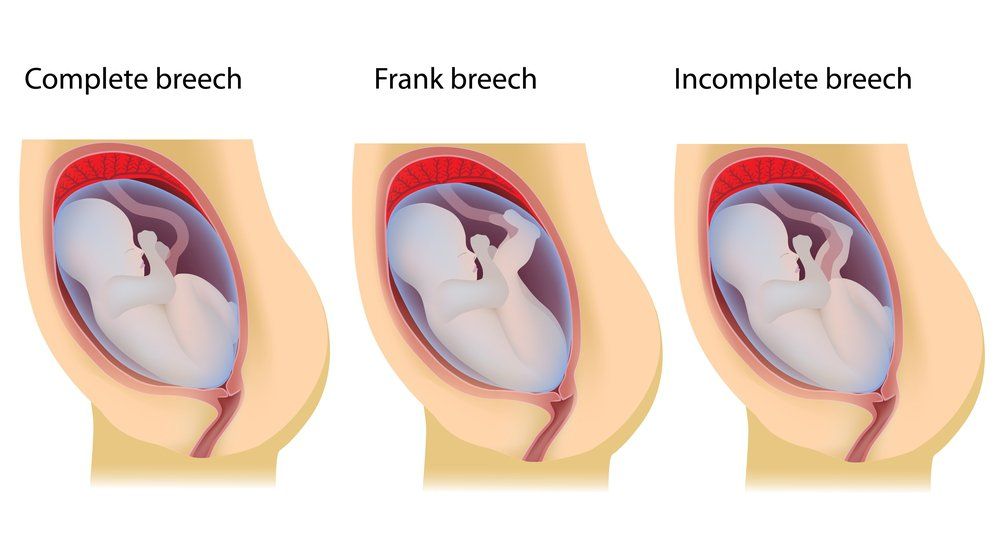 Complications from its use occur in less than 1-2% of cases.
Complications from its use occur in less than 1-2% of cases.
Complications of NAPP include:
- compression or "twisting" of the umbilical cord. In this case, constant monitoring of the condition of the fetus allows you to immediately fix its deterioration and stop the procedure.
- discharge of amniotic fluid or the development of labor. This complication can be considered relative, since the rotation in most cases is carried out at full-term pregnancy.
Any deviation from the normal course of the procedure serves as a reason to stop the manipulation and decide on the choice of further management tactics.
Carrying out NAPP with Rh-negative mother's blood.
The presence of Rh isoimmunization (that is, the presence of anti-Rh antibodies in the mother's blood) is a contraindication to this procedure, as it increases the risk of anemia in the fetus.
In the absence of isoimmunization (absence of anti-Rhesus antibodies) it is possible to carry out NAPP with prophylaxis by introducing anti-Rhesus immunoglobulin.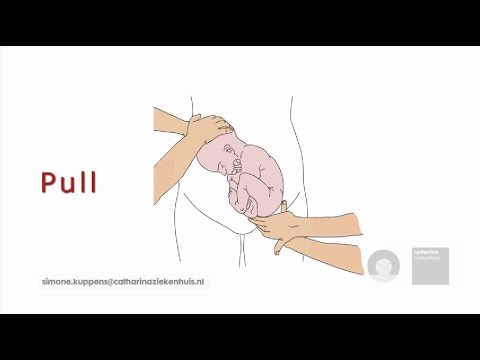
If you have a breech presentation of the fetus and you want to know about further options for pregnancy management, delivery, external obstetric rotation of the fetus on the head, the presence of indications and contraindications for its implementation, please consult our specialists.
Outer Fetus Rotation
- Material Information
It is known that in some pregnant women the fetus is in breech presentation. There are many opinions about what kind of help such women need. And at the same time, there is a single position supported by all the leading obstetricians in the world and voiced by the World Health Organization.
Births in breech presentation have a greater risk to the health of the fetus.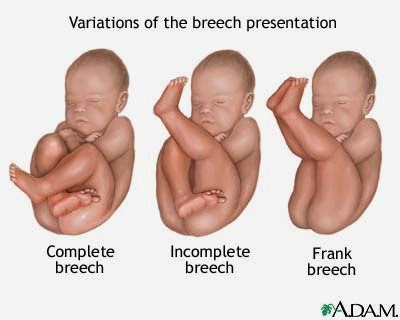 First, you should not worry about how the fetus is located in the uterus until 36-37 weeks. It is likely that he can completely independently take the head presentation before this time. Gymnastics, which is often offered to pregnant women, turned out to be ineffective (the frequency of fetal rotations in those who perform and do not perform special exercises is the same). As a method of delivery, a caesarean section is usually offered, but independent childbirth is also possible (this can only be said after an ultrasound on the eve of childbirth and an analysis of the clinical situation by an experienced obstetrician).
First, you should not worry about how the fetus is located in the uterus until 36-37 weeks. It is likely that he can completely independently take the head presentation before this time. Gymnastics, which is often offered to pregnant women, turned out to be ineffective (the frequency of fetal rotations in those who perform and do not perform special exercises is the same). As a method of delivery, a caesarean section is usually offered, but independent childbirth is also possible (this can only be said after an ultrasound on the eve of childbirth and an analysis of the clinical situation by an experienced obstetrician).
Many clinics in the world have completely abandoned independent birth in breech presentation, delivering such pregnant women by caesarean section. However, the argument often offered in the Russian Federation that breech birth in boys leads to male infertility has no scientific evidence. This story about male infertility is a topic exaggerated in Russian obstetric literature, and it was not heard about outside the USSR.
To avoid caesarean section in all industrialized countries, pregnant women are encouraged to perform an external rotation of the fetus on the head. The obstetrician, by light pressure on the abdomen, rotates the fetus, and it becomes head presentation. This is the safest and most frequently performed procedure in obstetrics, which is practiced throughout the world. The method of turning is different from previously performed, and most importantly, it is carried out under the control of ultrasound and CTG, which means that the obstetrician has a good idea of what is happening inside.
The most common fear expressed by a pregnant woman is that the fetus can be injured or damaged. It is impossible to injure the fetus during the rotation, it is in a state of hydroweightlessness and is protected by amniotic fluid, and the rotation is carried out with light movements. In the world, such a complication has not been reported, although the manipulation is performed in large numbers.