In vitro fertilization babies
In vitro fertilization (IVF) - Mayo Clinic
Overview
In vitro fertilization
In vitro fertilization
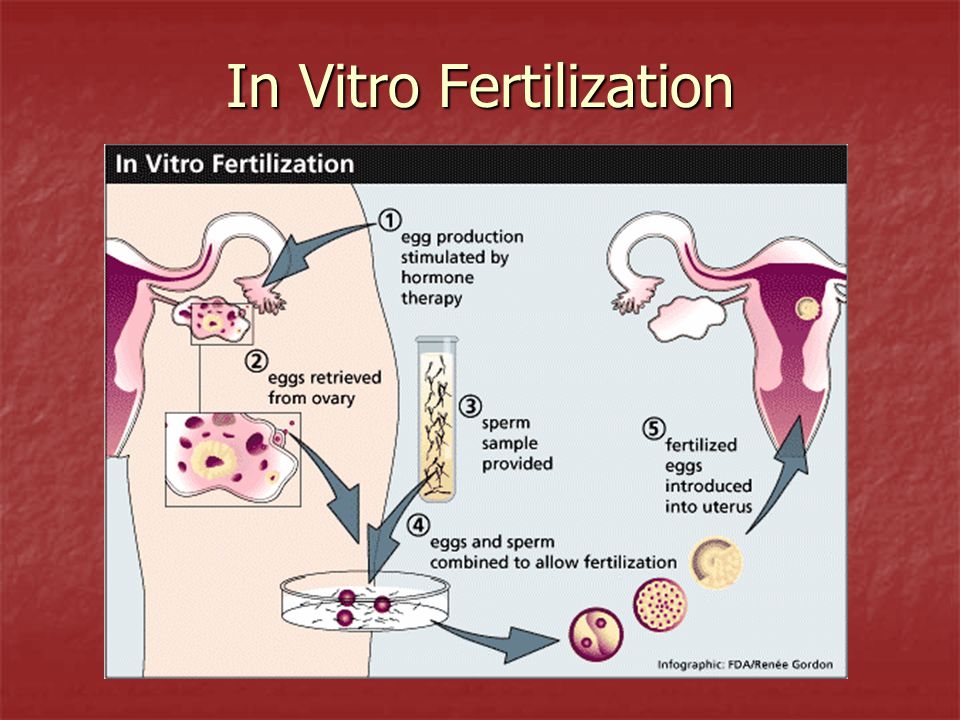
During in vitro fertilization, eggs are removed from mature follicles within an ovary (A). An egg is fertilized by injecting a single sperm into the egg or mixing the egg with sperm in a petri dish (B). The fertilized egg (embryo) is transferred into the uterus (C).
In vitro fertilization (IVF) is a complex series of procedures used to help with fertility or prevent genetic problems and assist with the conception of a child.
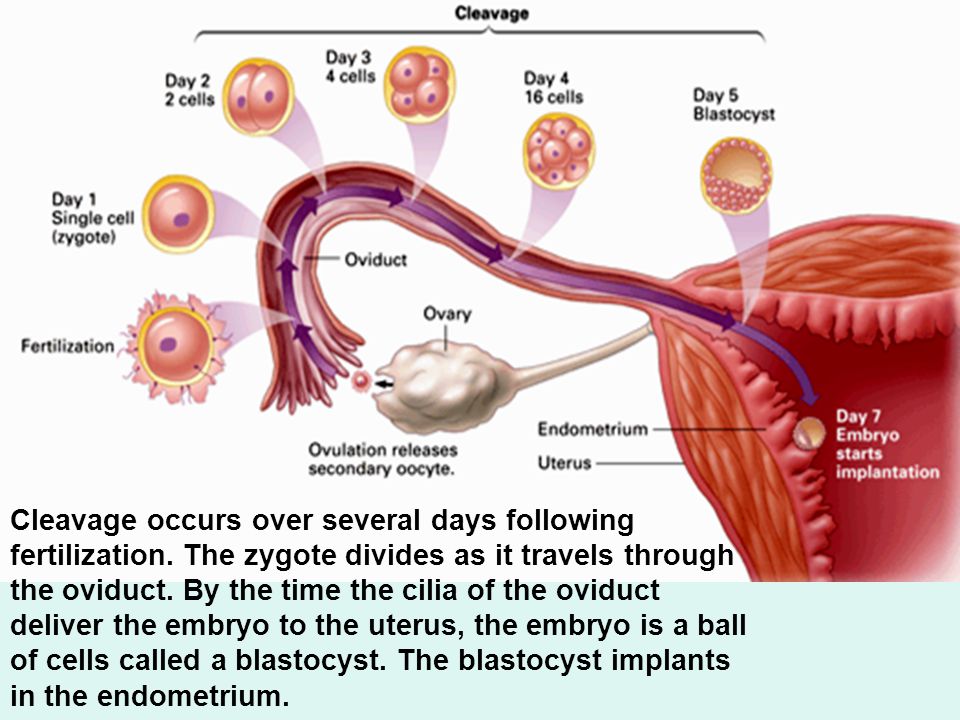
During IVF, mature eggs are collected (retrieved) from ovaries and fertilized by sperm in a lab. Then the fertilized egg (embryo) or eggs (embryos) are transferred to a uterus. One full cycle of IVF takes about three weeks. Sometimes these steps are split into different parts and the process can take longer.
IVF is the most effective form of assisted reproductive technology. The procedure can be done using a couple's own eggs and sperm. Or IVF may involve eggs, sperm or embryos from a known or anonymous donor. In some cases, a gestational carrier — someone who has an embryo implanted in the uterus — might be used.
Your chances of having a healthy baby using IVF depend on many factors, such as your age and the cause of infertility. In addition, IVF can be time-consuming, expensive and invasive. If more than one embryo is transferred to the uterus, IVF can result in a pregnancy with more than one fetus (multiple pregnancy).
Your doctor can help you understand how IVF works, the potential risks and whether this method of treating infertility is right for you.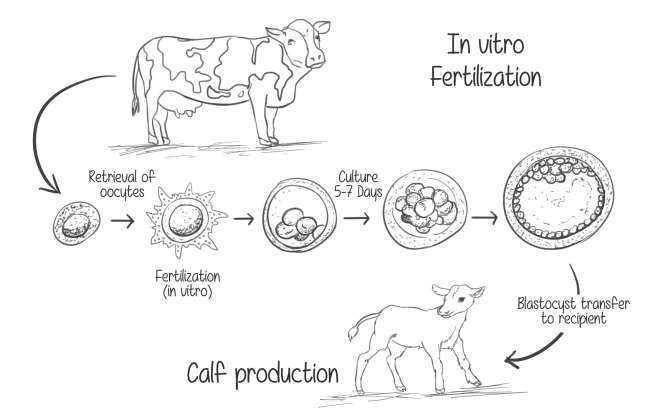
Products & Services
- Book: Mayo Clinic Family Health Book, 5th Edition
- Book: Mayo Clinic Guide to a Healthy Pregnancy
- Book: Mayo Clinic Guide to Fertility and Conception
- Newsletter: Mayo Clinic Health Letter — Digital Edition
Why it's done
In vitro fertilization (IVF) is a treatment for infertility or genetic problems. If IVF is performed to treat infertility, you and your partner might be able to try less-invasive treatment options before attempting IVF, including fertility drugs to increase production of eggs or intrauterine insemination — a procedure in which sperm are placed directly in the uterus near the time of ovulation.
Sometimes, IVF is offered as a primary treatment for infertility in women over age 40. IVF can also be done if you have certain health conditions. For example, IVF may be an option if you or your partner has:
For example, IVF may be an option if you or your partner has:
- Fallopian tube damage or blockage. Fallopian tube damage or blockage makes it difficult for an egg to be fertilized or for an embryo to travel to the uterus.
- Ovulation disorders. If ovulation is infrequent or absent, fewer eggs are available for fertilization.
- Endometriosis. Endometriosis occurs when tissue similar to the lining of the uterus implants and grows outside of the uterus — often affecting the function of the ovaries, uterus and fallopian tubes.
- Uterine fibroids. Fibroids are benign tumors in the uterus. They are common in women in their 30s and 40s. Fibroids can interfere with implantation of the fertilized egg.
- Previous tubal sterilization or removal. Tubal ligation is a type of sterilization in which the fallopian tubes are cut or blocked to permanently prevent pregnancy.
 If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery.
If you wish to conceive after tubal ligation, IVF may be an alternative to tubal ligation reversal surgery. - Impaired sperm production or function. Below-average sperm concentration, weak movement of sperm (poor mobility), or abnormalities in sperm size and shape can make it difficult for sperm to fertilize an egg. If semen abnormalities are found, a visit to an infertility specialist might be needed to see if there are correctable problems or underlying health concerns.
- Unexplained infertility. Unexplained infertility means no cause of infertility has been found despite evaluation for common causes.
- A genetic disorder. If you or your partner is at risk of passing on a genetic disorder to your child, you may be candidates for preimplantation genetic testing — a procedure that involves IVF. After the eggs are harvested and fertilized, they're screened for certain genetic problems, although not all genetic problems can be found.
 Embryos that don't contain identified problems can be transferred to the uterus.
Embryos that don't contain identified problems can be transferred to the uterus. -
Fertility preservation for cancer or other health conditions. If you're about to start cancer treatment — such as radiation or chemotherapy — that could harm your fertility, IVF for fertility preservation may be an option. Women can have eggs harvested from their ovaries and frozen in an unfertilized state for later use. Or the eggs can be fertilized and frozen as embryos for future use.
Women who don't have a functional uterus or for whom pregnancy poses a serious health risk might choose IVF using another person to carry the pregnancy (gestational carrier). In this case, the woman's eggs are fertilized with sperm, but the resulting embryos are placed in the gestational carrier's uterus.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your inbox
Sign up for free, and stay up to date on research advancements, health tips and current health topics, like COVID-19, plus expertise on managing health.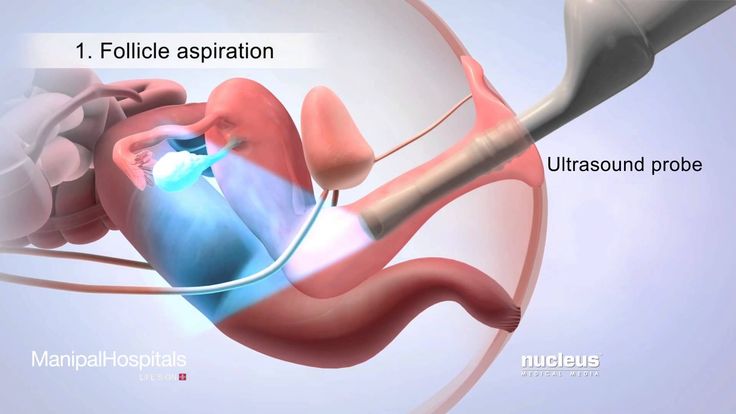
To provide you with the most relevant and helpful information, and understand which information is beneficial, we may combine your email and website usage information with other information we have about you. If you are a Mayo Clinic patient, this could include protected health information. If we combine this information with your protected health information, we will treat all of that information as protected health information and will only use or disclose that information as set forth in our notice of privacy practices. You may opt-out of email communications at any time by clicking on the unsubscribe link in the e-mail.
Risks
Risks of IVF include:
- Multiple births.
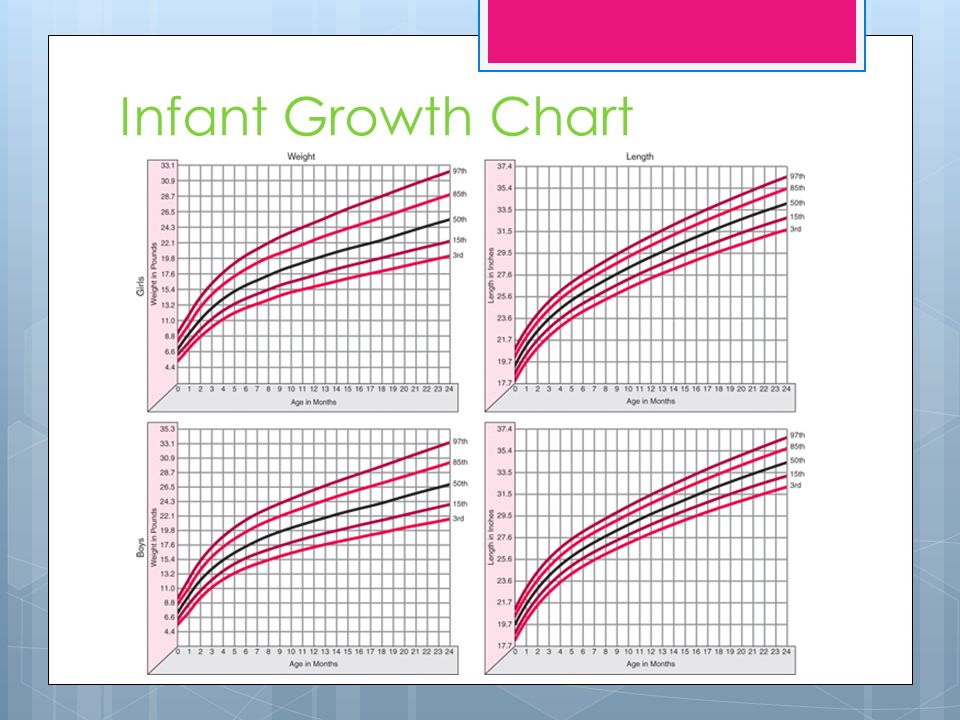
 IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does.
IVF increases the risk of multiple births if more than one embryo is transferred to your uterus. A pregnancy with multiple fetuses carries a higher risk of early labor and low birth weight than pregnancy with a single fetus does. - Premature delivery and low birth weight. Research suggests that IVF slightly increases the risk that the baby will be born early or with a low birth weight.
-
Ovarian hyperstimulation syndrome. Use of injectable fertility drugs, such as human chorionic gonadotropin (HCG), to induce ovulation can cause ovarian hyperstimulation syndrome, in which your ovaries become swollen and painful.
Symptoms typically last a week and include mild abdominal pain, bloating, nausea, vomiting and diarrhea. If you become pregnant, however, your symptoms might last several weeks. Rarely, it's possible to develop a more severe form of ovarian hyperstimulation syndrome that can also cause rapid weight gain and shortness of breath.
- Miscarriage. The rate of miscarriage for women who conceive using IVF with fresh embryos is similar to that of women who conceive naturally — about 15% to 25% — but the rate increases with maternal age.
- Egg-retrieval procedure complications. Use of an aspirating needle to collect eggs could possibly cause bleeding, infection or damage to the bowel, bladder or a blood vessel. Risks are also associated with sedation and general anesthesia, if used.
- Ectopic pregnancy. About 2% to 5% of women who use IVF will have an ectopic pregnancy — when the fertilized egg implants outside the uterus, usually in a fallopian tube. The fertilized egg can't survive outside the uterus, and there's no way to continue the pregnancy.
- Birth defects. The age of the mother is the primary risk factor in the development of birth defects, no matter how the child is conceived.
 More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects.
More research is needed to determine whether babies conceived using IVF might be at increased risk of certain birth defects. - Cancer. Although some early studies suggested there may be a link between certain medications used to stimulate egg growth and the development of a specific type of ovarian tumor, more-recent studies do not support these findings. There does not appear to be a significantly increased risk of breast, endometrial, cervical or ovarian cancer after IVF.
- Stress. Use of IVF can be financially, physically and emotionally draining. Support from counselors, family and friends can help you and your partner through the ups and downs of infertility treatment.
How you prepare
The Centers for Disease Control and Prevention and the Society for Assisted Reproductive Technology provide information online about U.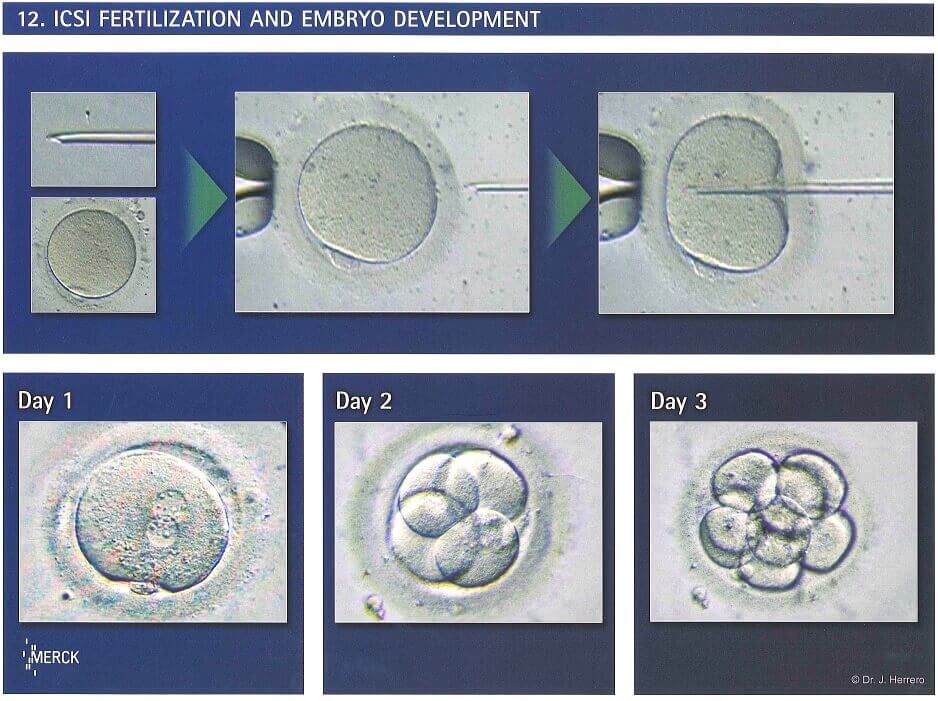 S. clinics' individual pregnancy and live birth rates.
S. clinics' individual pregnancy and live birth rates.
A clinic's success rate depends on many factors. These include patients' ages and medical issues, as well as the clinic's treatment population and treatment approaches. Ask for detailed information about the costs associated with each step of the procedure.
Before beginning a cycle of IVF using your own eggs and sperm, you and your partner will likely need various screenings, including:
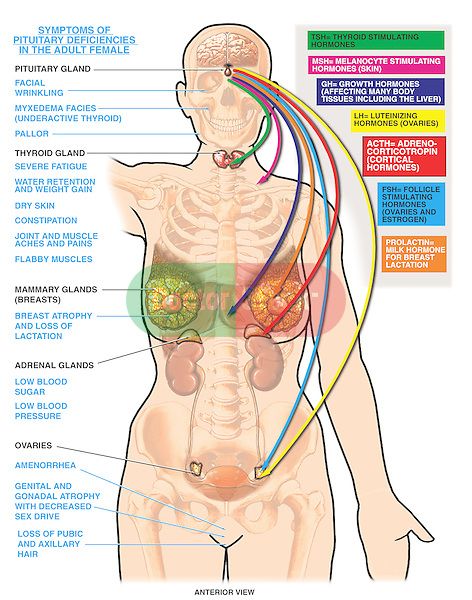
- Ovarian reserve testing. To determine the quantity and quality of your eggs, your doctor might test the concentration of follicle-stimulating hormone (FSH), estradiol (estrogen) and anti-mullerian hormone in your blood during the first few days of your menstrual cycle. Test results, often used together with an ultrasound of your ovaries, can help predict how your ovaries will respond to fertility medication.
- Semen analysis. If not done as part of your initial fertility evaluation, your doctor will conduct a semen analysis shortly before the start of an IVF treatment cycle.
- Infectious disease screening. You and your partner will both be screened for infectious diseases, including HIV.
- Practice (mock) embryo transfer. Your doctor might conduct a mock embryo transfer to determine the depth of your uterine cavity and the technique most likely to successfully place the embryos into your uterus.
- Uterine exam. Your doctor will examine the inside lining of the uterus before you start IVF. This might involve a sonohysterography — in which fluid is injected through the cervix into your uterus — and an ultrasound to create images of your uterine cavity. Or it might include a hysteroscopy — in which a thin, flexible, lighted telescope (hysteroscope) is inserted through your vagina and cervix into your uterus.
Before beginning a cycle of IVF, consider important questions, including:
-
How many embryos will be transferred? The number of embryos transferred is typically based on age and number of eggs retrieved.
 Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.
Since the rate of implantation is lower for older women, more embryos are usually transferred — except for women using donor eggs or genetically tested embryos.Most doctors follow specific guidelines to prevent a higher order multiple pregnancy, such as triplets or more. In some countries, legislation limits the number of embryos that can be transferred. Make sure you and your doctor agree on the number of embryos that will be transferred before the transfer procedure.
-
What will you do with any extra embryos? Extra embryos can be frozen and stored for future use for several years. Not all embryos will survive the freezing and thawing process, although most will.
Having frozen embryos can make future cycles of IVF less expensive and less invasive. Or, you might be able to donate unused frozen embryos to another couple or a research facility. You might also choose to discard unused embryos.

- How will you handle a multiple pregnancy? If more than one embryo is transferred to your uterus, IVF can result in a multiple pregnancy — which poses health risks for you and your babies. In some cases, fetal reduction can be used to help a woman deliver fewer babies with lower health risks. Pursuing fetal reduction, however, is a major decision with ethical, emotional and psychological consequences.
- Have you considered the potential complications associated with using donor eggs, sperm or embryos, or a gestational carrier? A trained counselor with expertise in donor issues can help you understand the concerns, such as the legal rights of the donor. You may also need an attorney to file court papers to help you become legal parents of an implanted embryo.
What you can expect
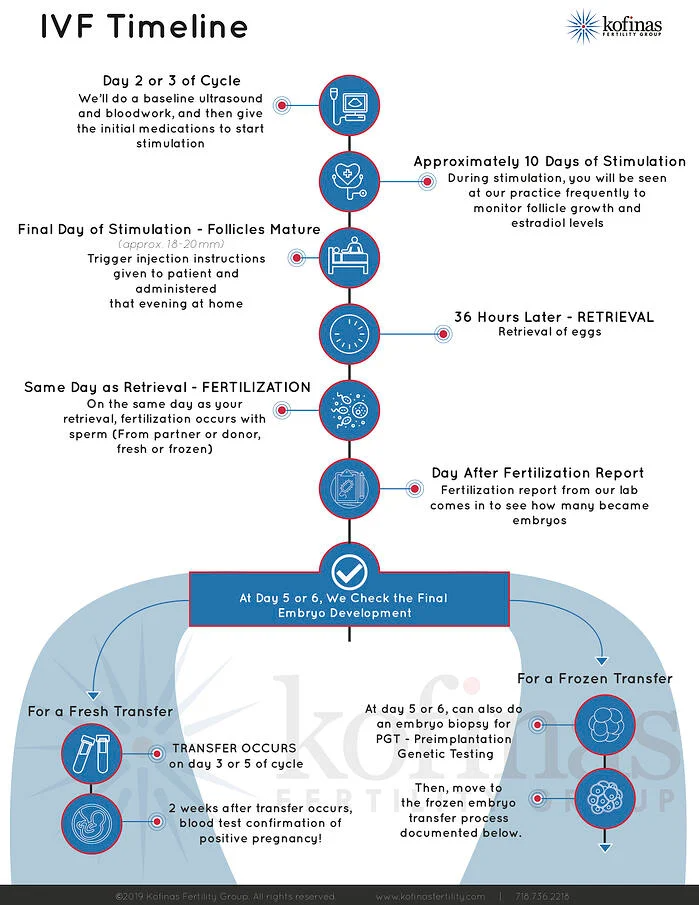
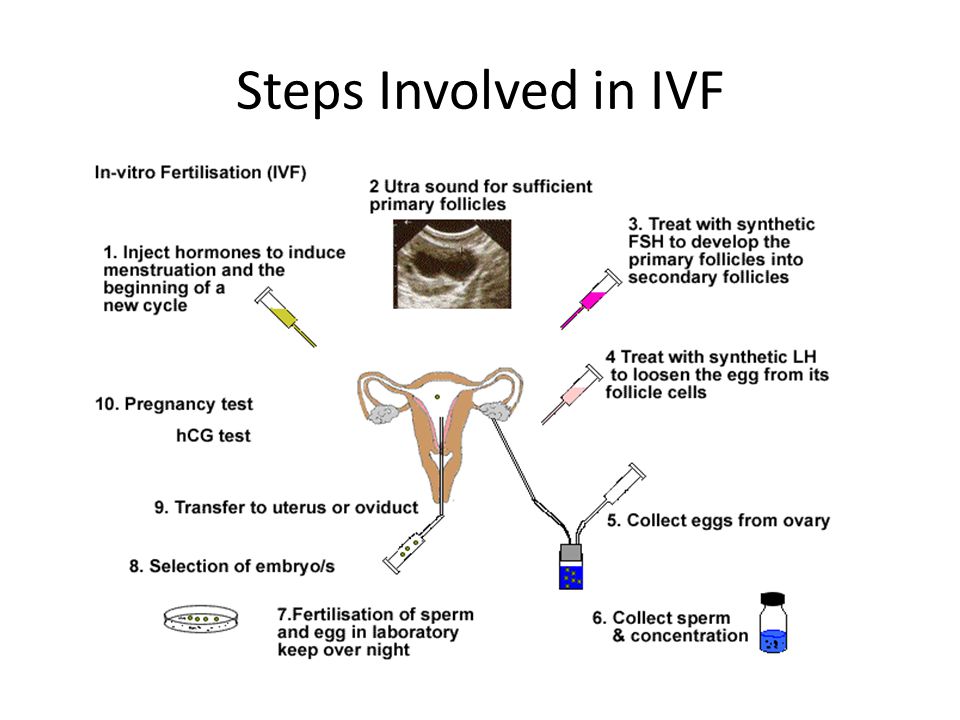
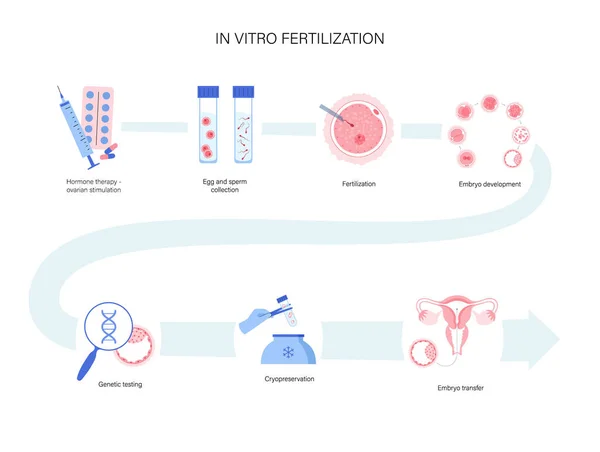
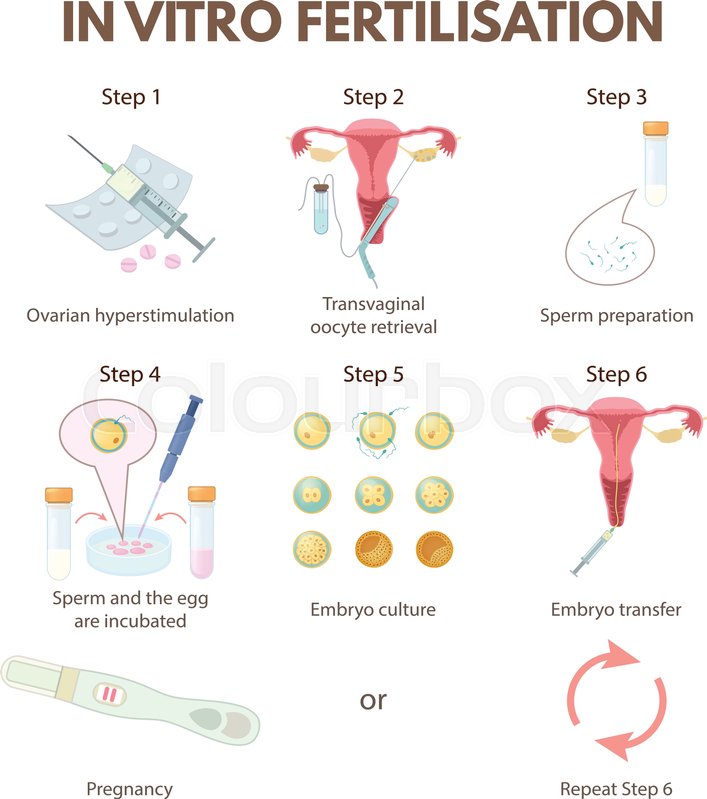
IVF involves several steps — ovarian stimulation, egg retrieval, sperm retrieval, fertilization and embryo transfer.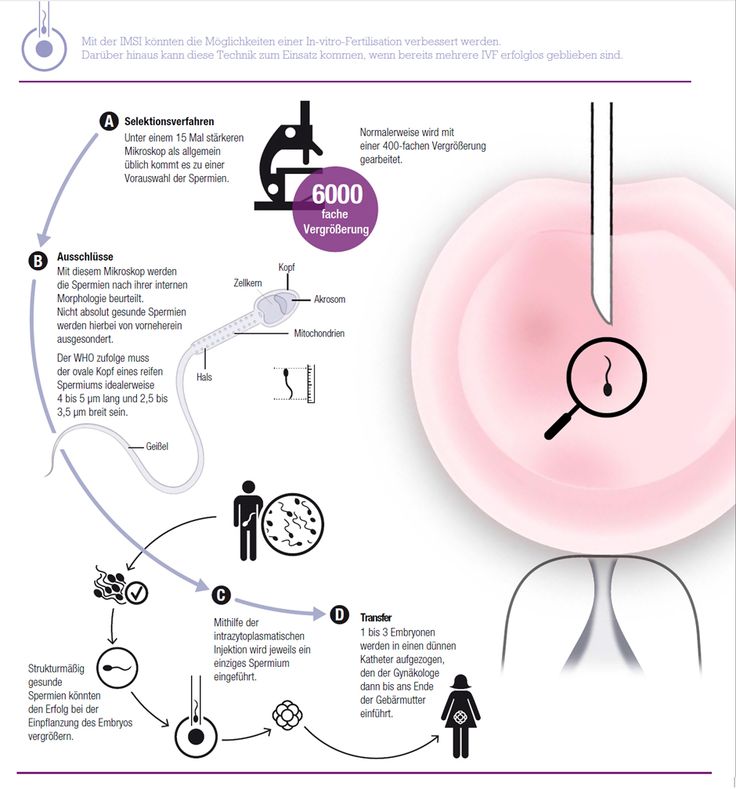 One cycle of IVF can take about two to three weeks. More than one cycle may be needed.
One cycle of IVF can take about two to three weeks. More than one cycle may be needed.
Ovulation induction
The start of an IVF cycle begins by using synthetic hormones to stimulate the ovaries to produce multiple eggs — rather than the single egg that typically develops each month. Multiple eggs are needed because some eggs won't fertilize or develop normally after fertilization.
Several different medications may be used, such as:
- Medications for ovarian stimulation. To stimulate your ovaries, you might receive an injectable medication containing a follicle-stimulating hormone (FSH), a luteinizing hormone (LH) or a combination of both. These medications stimulate more than one egg to develop at a time.
- Medications for oocyte maturation. When the follicles are ready for egg retrieval — generally after eight to 14 days — you will take human chorionic gonadotropin (HCG) or other medications to help the eggs mature.
- Medications to prevent premature ovulation. These medications prevent your body from releasing the developing eggs too soon.
- Medications to prepare the lining of your uterus. On the day of egg retrieval or at the time of embryo transfer, your doctor might recommend that you begin taking progesterone supplements to make the lining of your uterus more receptive to implantation.
Your doctor will work with you to determine which medications to use and when to use them.
Typically, you'll need one to two weeks of ovarian stimulation before your eggs are ready for retrieval. To determine when the eggs are ready for collection, you may have:
- Vaginal ultrasound, an imaging exam of your ovaries to monitor the development of follicles — fluid-filled ovarian sacs where eggs mature
- Blood tests, to measure your response to ovarian stimulation medications — estrogen levels typically increase as follicles develop, and progesterone levels remain low until after ovulation
Sometimes IVF cycles need to be canceled before egg retrieval for one of these reasons:
- Inadequate number of follicles developing
- Premature ovulation
- Too many follicles developing, creating a risk of ovarian hyperstimulation syndrome
- Other medical issues
If your cycle is canceled, your doctor might recommend changing medications or their doses to promote a better response during future IVF cycles. Or you may be advised that you need an egg donor.
Or you may be advised that you need an egg donor.
Egg retrieval
Egg retrieval can be done in your doctor's office or a clinic 34 to 36 hours after the final injection and before ovulation.
- During egg retrieval, you'll be sedated and given pain medication.
- Transvaginal ultrasound aspiration is the usual retrieval method. An ultrasound probe is inserted into your vagina to identify follicles. Then a thin needle is inserted into an ultrasound guide to go through the vagina and into the follicles to retrieve the eggs.
- If your ovaries aren't accessible through transvaginal ultrasound, an abdominal ultrasound may be used to guide the needle.
- The eggs are removed from the follicles through a needle connected to a suction device. Multiple eggs can be removed in about 20 minutes.
- After egg retrieval, you may experience cramping and feelings of fullness or pressure.
- Mature eggs are placed in a nutritive liquid (culture medium) and incubated.
 Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Eggs that appear healthy and mature will be mixed with sperm to attempt to create embryos. However, not all eggs may be successfully fertilized.
Sperm retrieval
If you're using your partner's sperm, a semen sample needs to be provided at your doctor's office or clinic the morning of egg retrieval. Typically, the semen sample is collected through masturbation. Other methods, such as testicular aspiration — the use of a needle or surgical procedure to extract sperm directly from the testicle — are sometimes required. Donor sperm also can be used. Sperm are separated from the semen fluid in the lab.
Fertilization
Fertilization can be attempted using two common methods:
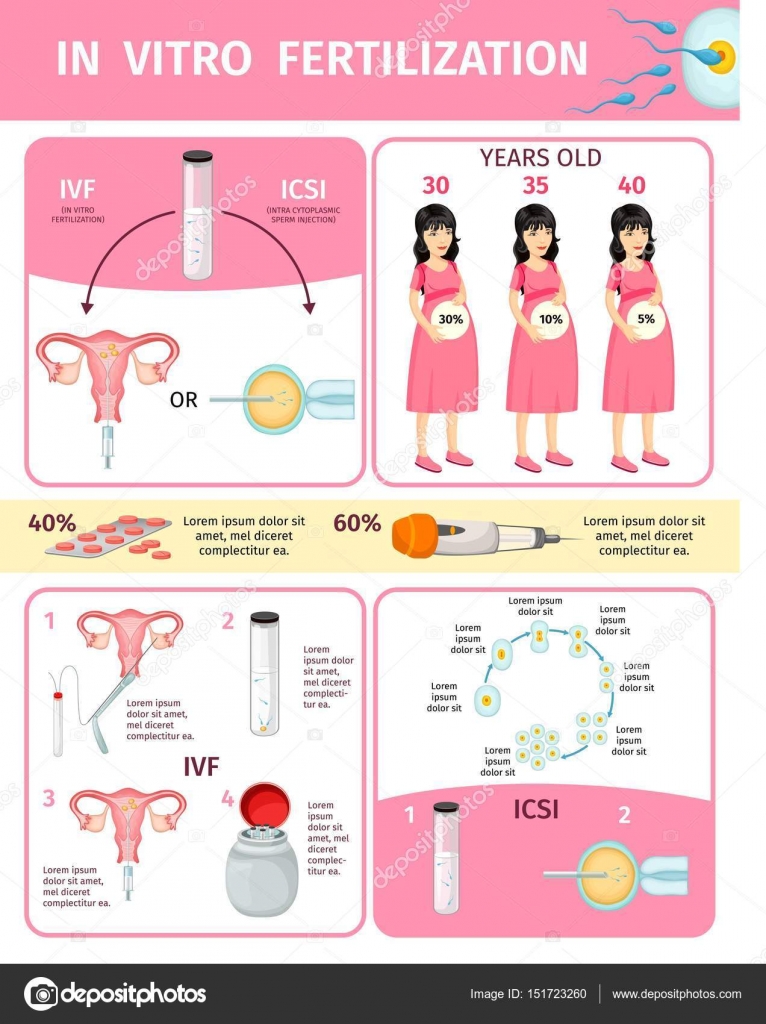
- Conventional insemination. During conventional insemination, healthy sperm and mature eggs are mixed and incubated overnight.
- Intracytoplasmic sperm injection (ICSI). In ICSI, a single healthy sperm is injected directly into each mature egg.
 ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior IVF cycles failed.
In certain situations, your doctor may recommend other procedures before embryo transfer.
- Assisted hatching. About five to six days after fertilization, an embryo "hatches" from its surrounding membrane (zona pellucida), allowing it to implant into the lining of the uterus. If you're an older woman, or if you have had multiple failed IVF attempts, your doctor might recommend assisted hatching — a technique in which a hole is made in the zona pellucida just before transfer to help the embryo hatch and implant. Assisted hatching is also useful for eggs or embryos that have been previously frozen as the process can harden the zona pellucida.
- Preimplantation genetic testing.
 Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryos are allowed to develop in the incubator until they reach a stage where a small sample can be removed and tested for specific genetic diseases or the correct number of chromosomes, typically after five to six days of development. Embryos that don't contain affected genes or chromosomes can be transferred to your uterus. While preimplantation genetic testing can reduce the likelihood that a parent will pass on a genetic problem, it can't eliminate the risk. Prenatal testing may still be recommended.
Embryo transfer
Egg-retrieval technique
Egg-retrieval technique
Typically, transvaginal ultrasound aspiration is used to retrieve eggs. During this procedure, an ultrasound probe is inserted into your vagina to identify follicles, and a needle is guided through the vagina and into the follicles. The eggs are removed from the follicles through the needle, which is connected to a suction device.
ICSI
ICSI
In intracytoplasmic sperm injection (ICSI), a single healthy sperm is injected directly into each mature egg. ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
ICSI is often used when semen quality or number is a problem or if fertilization attempts during prior in vitro fertilization cycles failed.
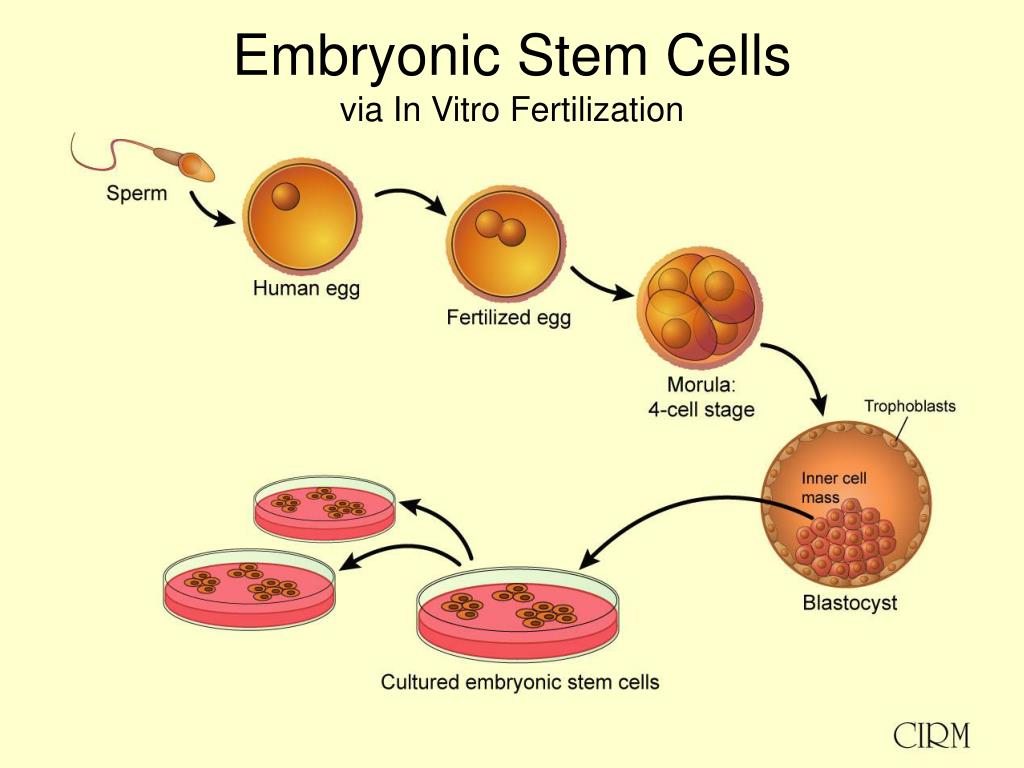
Blastocyst
Blastocyst
Three days after fertilization, a normally developing embryo will contain about six to 10 cells. By the fifth or sixth day, the fertilized egg is known as a blastocyst — a rapidly dividing ball of cells. The inner group of cells will become the embryo. The outer group will become the cells that nourish and protect it.
Embryo transfer is done at your doctor's office or a clinic and usually takes place two to five days after egg retrieval.
- You might be given a mild sedative. The procedure is usually painless, although you might experience mild cramping.
- The doctor will insert a long, thin, flexible tube called a catheter into your vagina, through your cervix and into your uterus.
- A syringe containing one or more embryos suspended in a small amount of fluid is attached to the end of the catheter.
- Using the syringe, the doctor places the embryo or embryos into your uterus.
If successful, an embryo will implant in the lining of your uterus about six to 10 days after egg retrieval.
After the procedure
After the embryo transfer, you can resume your usual daily activities. However, your ovaries may still be enlarged. Consider avoiding vigorous activity, which could cause discomfort.
Typical side effects include:
- Passing a small amount of clear or bloody fluid shortly after the procedure — due to the swabbing of the cervix before the embryo transfer
- Breast tenderness due to high estrogen levels
- Mild bloating
- Mild cramping
- Constipation
If you develop moderate or severe pain after the embryo transfer, contact your doctor. He or she will evaluate you for complications such as infection, twisting of an ovary (ovarian torsion) and severe ovarian hyperstimulation syndrome.
Results
About 12 days to two weeks after egg retrieval, your doctor will test a sample of your blood to detect whether you're pregnant.
- If you're pregnant, your doctor will refer you to an obstetrician or other pregnancy specialist for prenatal care.
- If you're not pregnant, you'll stop taking progesterone and likely get your period within a week. If you don't get your period or you have unusual bleeding, contact your doctor. If you're interested in attempting another cycle of in vitro fertilization (IVF), your doctor might suggest steps you can take to improve your chances of getting pregnant through IVF.
The chances of giving birth to a healthy baby after using IVF depend on various factors, including:
- Maternal age. The younger you are, the more likely you are to get pregnant and give birth to a healthy baby using your own eggs during IVF.
 Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success.
Women age 41 and older are often counseled to consider using donor eggs during IVF to increase the chances of success. - Embryo status. Transfer of embryos that are more developed is associated with higher pregnancy rates compared with less-developed embryos (day two or three). However, not all embryos survive the development process. Talk with your doctor or other care provider about your specific situation.
- Reproductive history. Women who've previously given birth are more likely to be able to get pregnant using IVF than are women who've never given birth. Success rates are lower for women who've previously used IVF multiple times but didn't get pregnant.
- Cause of infertility. Having a normal supply of eggs increases your chances of being able to get pregnant using IVF.
 Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility.
Women who have severe endometriosis are less likely to be able to get pregnant using IVF than are women who have unexplained infertility. - Lifestyle factors. Women who smoke typically have fewer eggs retrieved during IVF and may miscarry more often. Smoking can lower a woman's chance of success using IVF by 50%. Obesity can decrease your chances of getting pregnant and having a baby. Use of alcohol, recreational drugs, excessive caffeine and certain medications also can be harmful.
Talk with your doctor about any factors that apply to you and how they may affect your chances of a successful pregnancy.
Clinical trials
Explore Mayo Clinic studies of tests and procedures to help prevent, detect, treat or manage conditions.
By Mayo Clinic Staff
Related
Products & Services
Procedure & How It Works
Overview
Learn more about how the IVF process works.What is IVF?
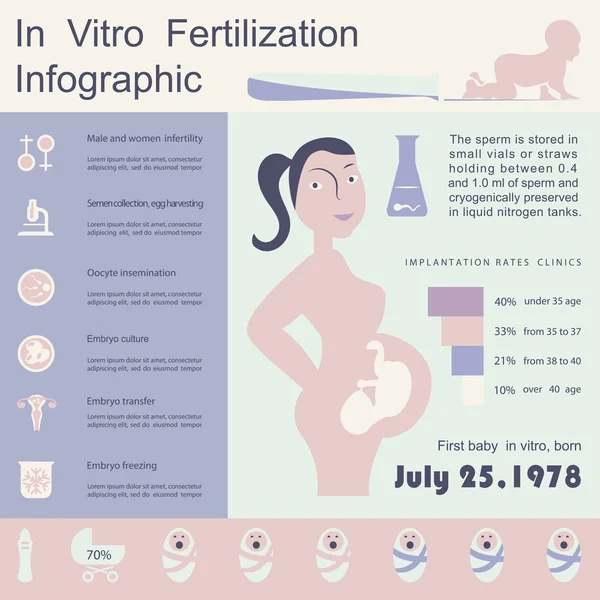
In vitro fertilization (IVF) is a type of assisted reproductive technology (ART) where sperm and an egg are fertilized outside of the human body. IVF is a complex process that involves retrieving eggs from ovaries and manually combining them with sperm in a lab for fertilization. Several days after fertilization, the fertilized egg (now called an embryo) is placed inside a uterus. Pregnancy occurs when this embryo implants itself into the uterine wall.
Why is IVF performed?
People choose IVF for many reasons, including infertility issues or when one partner has an existing health condition. Some people will try IVF after other fertility methods have failed or if they’re at an advanced maternal age. IVF is also a reproductive option for same-sex couples or people who wish to have a baby without a partner.
IVF is an option if you or your partner has:
- Blocked or damaged fallopian tubes.

- Endometriosis.
- Low sperm count or other sperm impairments.
- Polycystic ovary syndrome (PCOS) or other ovarian conditions.
- Uterine fibroids.
- Problems with your uterus.
- Risk of passing on a genetic disease or disorder.
- Unexplained infertility.
- Are using an egg donor or a gestational surrogate.
How long is the IVF process from beginning to end?
IVF is a complicated process with many steps. On average, you can expect the process to last four to six weeks. This includes the time before egg retrieval, when a person takes fertility medication until they’re tested for pregnancy.
How common is IVF?
Approximately 5% of couples with infertility will try IVF. More than 8 million babies have been born from IVF since 1978. It’s one of the most effective assisted reproductive technologies (ARTs) available.
What is the difference between IVF and IUI (intrauterine insemination)?
Intrauterine insemination (IUI) is different from in vitro fertilization (IVF) because in an IUI procedure, fertilization occurs in a person’s body.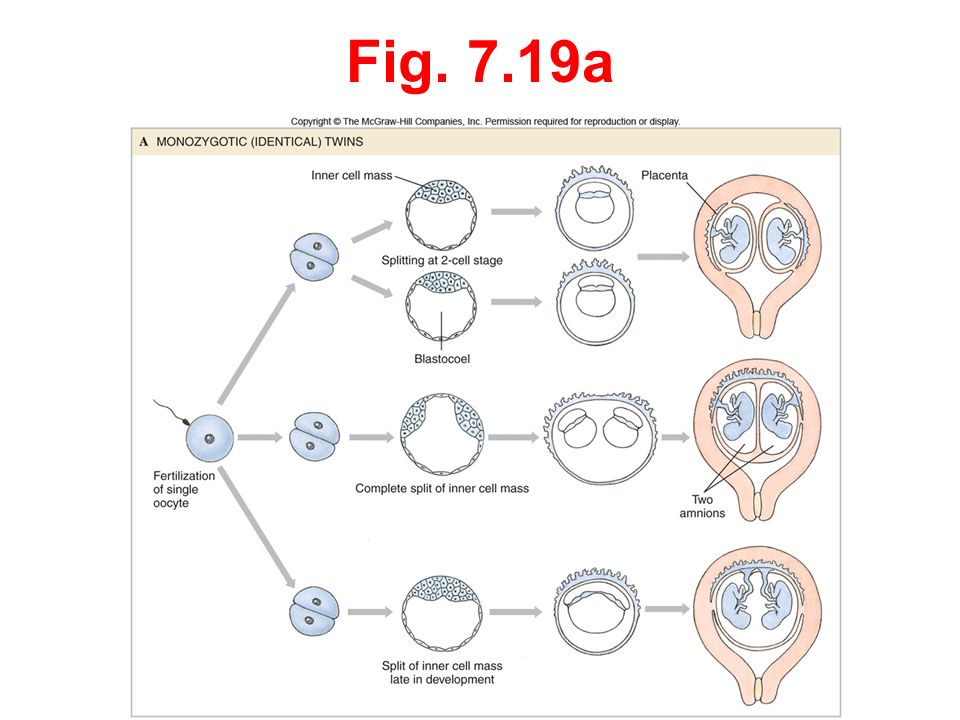 A sperm sample is collected and washed so only high-quality sperm are left. This sample is inserted into your uterus with a catheter (thin tube) during ovulation. This method helps the sperm get to the egg more easily in hope that fertilization will happen.
A sperm sample is collected and washed so only high-quality sperm are left. This sample is inserted into your uterus with a catheter (thin tube) during ovulation. This method helps the sperm get to the egg more easily in hope that fertilization will happen.
With IVF, the sperm and egg are fertilized outside of your uterus (in a lab) and then placed in your uterus as an embryo.
IUI is less expensive and less invasive than IVF. IUI has a lower success rate per cycle.
Procedure Details
What are the steps of IVF treatment?
IVF can be broken down into the following steps:
Birth control pills or estrogen
Before you start IVF treatment, your healthcare provider may prescribe birth control pills or estrogen. This is used to stop the development of ovarian cysts and control the timing of your menstrual cycle. It allows your healthcare provider to control your treatment and maximize the number of mature eggs during the egg retrieval procedure. Some people are prescribed combination birth control pills (estrogen and progesterone), while others are given just estrogen.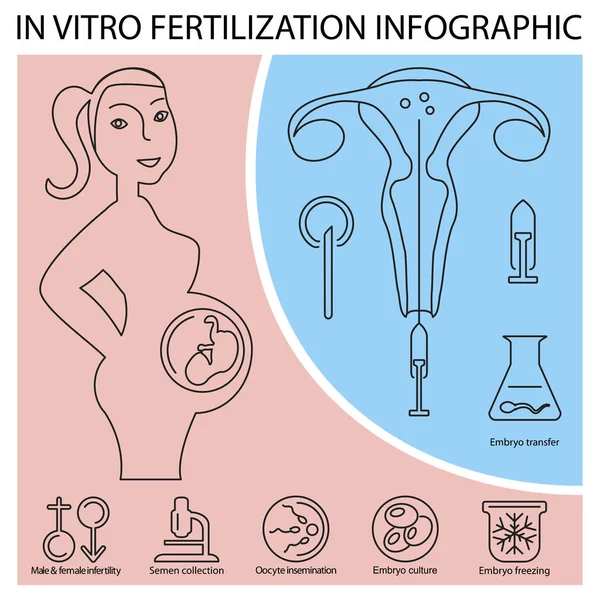
Ovarian stimulation
During each natural cycle in a healthy person of reproductive age, a group of eggs begins to mature each month. Typically, only one egg becomes mature enough to ovulate. The remaining immature eggs in that group disintegrate.
During your IVF cycle, you’ll take injectable hormone medications to encourage the entire group of that cycle’s eggs to mature simultaneously and fully. This means, instead of having just one egg (like in a natural cycle), you may have many eggs. The type, dosage and frequency of medications prescribed will be tailored to you as an individual based on your medical history, age, AMH (anti-mullerian hormone) level and your response to ovarian stimulation during previous IVF cycles.
The other steps in the ovarian stimulation process include:
- Monitoring: Your ovaries’ response to the medications is monitored by ultrasounds and blood hormone levels. Monitoring can occur daily or every few days over two weeks.
 Most stimulations last between eight and 14 days. At monitoring appointments, healthcare providers use ultrasound to look at your uterus and ovaries. The eggs themselves are too small to be visible with ultrasound. But, your healthcare providers will measure the size and number of growing ovarian follicles. Follicles are little sacks within your ovaries that should each contain a single egg. The size of each follicle indicates the maturity of the egg it contains. Most follicles greater than 14 millimeters (mm) contain a mature egg. The eggs contained within follicles less than 14 mm are more likely be immature and won’t fertilize.
Most stimulations last between eight and 14 days. At monitoring appointments, healthcare providers use ultrasound to look at your uterus and ovaries. The eggs themselves are too small to be visible with ultrasound. But, your healthcare providers will measure the size and number of growing ovarian follicles. Follicles are little sacks within your ovaries that should each contain a single egg. The size of each follicle indicates the maturity of the egg it contains. Most follicles greater than 14 millimeters (mm) contain a mature egg. The eggs contained within follicles less than 14 mm are more likely be immature and won’t fertilize. - Trigger shot: When your eggs are ready for final maturation (determined by your ultrasound and hormone levels), a “trigger shot” is given to finalize the maturation of your eggs in preparation for egg retrieval. You’ll be instructed to administer the trigger shot exactly 36 hours before your scheduled egg retrieval time.
Egg retrieval
- Your healthcare provider uses an ultrasound to guide a thin needle into each of your ovaries through your vagina.
 The needle is connected to a suction device used to pull your eggs out of each follicle.
The needle is connected to a suction device used to pull your eggs out of each follicle. - Your eggs are placed in a dish containing a special solution. The dish is then put in an incubator (controlled environment).
- Medication and mild sedation are used to reduce discomfort during this procedure.
- Egg retrieval is done 36 hours after your last hormone injection, the “trigger shot.”
Fertilization
The afternoon after your egg retrieval procedure, the embryologist will try to fertilize all mature eggs using intracytoplasmic sperm injection, or ICSI. This means that sperm will be injected into each mature egg. Immature eggs cannot have ICSI performed on them. The immature eggs will be placed in a dish with sperm and nutrients. Immature eggs rarely finish their maturation process in the dish. If an immature egg does mature, the sperm in the dish can then attempt to fertilize the egg.
On average, 70% of mature eggs will fertilize. For example, if 10 mature eggs are retrieved, about seven will fertilize.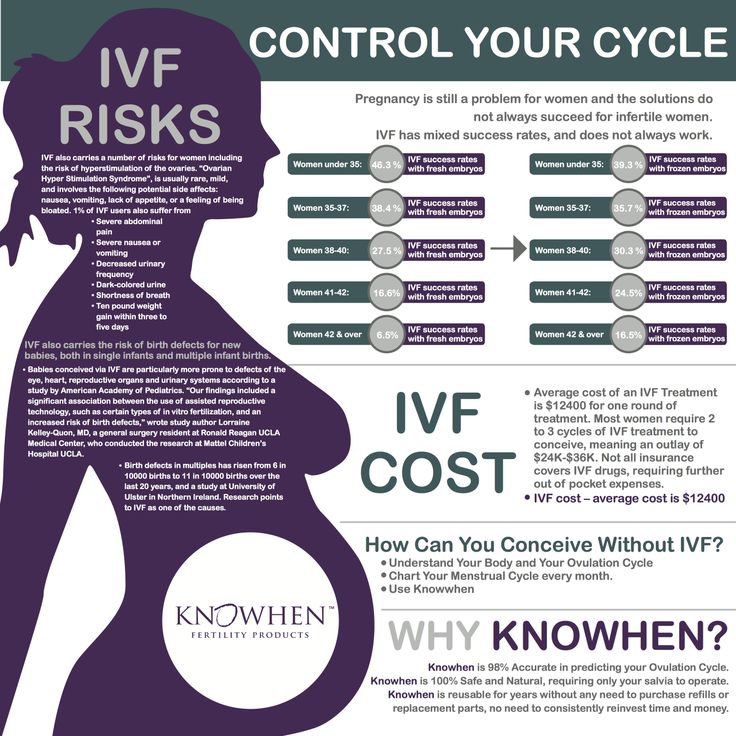 If successful, the fertilized egg will become an embryo.
If successful, the fertilized egg will become an embryo.
If there are an exceedingly large number of eggs or you don’t want all eggs fertilized, some eggs may be frozen before fertilization for future use.
Embryo development
Over the next five to six days, the development of your embryos will be carefully monitored.
Your embryo must overcome significant hurdles to become an embryo suitable for transfer to your uterus. On average, 50% of fertilized embryos progress to the blastocyst stage. This is the stage most suitable for transfer to your uterus. For example, if seven eggs were fertilized, three or four of them might develop to the blastocyst stage. The remaining 50% typically fail to progress and are discarded.
All embryos suitable for transfer will be frozen on day five or six of fertilization to be used for future embryo transfers.
Embryo transfer
There are two kinds of embryo transfers: fresh embryo transfer and frozen embryo transfer. Your healthcare provider can discuss using fresh or frozen embryos with you and decide what’s best based on your unique situation. Both frozen and fresh embryo transfers follow the same transfer process. The main difference is implied by the name.
Your healthcare provider can discuss using fresh or frozen embryos with you and decide what’s best based on your unique situation. Both frozen and fresh embryo transfers follow the same transfer process. The main difference is implied by the name.
A fresh embryo transfer means your embryo is inserted into your uterus between three and seven days after the egg retrieval procedure. This embryo hasn’t been frozen and is “fresh.”
A frozen embryo transfer means that frozen embryos (from a previous IVF cycle or donor eggs) are thawed and inserted into your uterus. This is a more common practice for logistical reasons and because this method is more likely to result in a live birth. Frozen embryo transfers can occur years after egg retrieval and fertilization.
As part of the first step in a frozen embryo transfer, you’ll take oral, injectable, vaginal or transdermal hormones to prepare your uterus for accepting an embryo. Usually, this is 14 to 21 days of oral medication followed by six days of injections. Typically, you’ll have two or three appointments during this time to monitor the readiness of your uterus with ultrasound and to measure your hormone levels with a blood test. When your uterus is ready, you’ll be scheduled for the embryo transfer procedure.
Typically, you’ll have two or three appointments during this time to monitor the readiness of your uterus with ultrasound and to measure your hormone levels with a blood test. When your uterus is ready, you’ll be scheduled for the embryo transfer procedure.
The process is similar if you’re using fresh embryos, except embryo transfer happens within three to five days of being retrieved.
The embryo transfer is a simple procedure that doesn’t require anesthesia. It feels similar to a pelvic exam or Pap smear. A speculum is placed within the vagina, and a thin catheter is inserted through the cervix into the uterus. A syringe attached to the other end of the catheter contains one or more embryos. The embryos are injected it the uterus through the catheter. The procedure typically takes less than 10 minutes.
Pregnancy
Pregnancy occurs when the embryo implants itself into the lining of your uterus. Your healthcare provider will use a blood test to determine if you’re pregnant approximately nine to 14 days after embryo transfer.
If donor eggs are being used, the same steps are taken. The egg donor will complete ovarian stimulation and egg retrieval. After fertilization takes place, the embryo is transferred to the person who intends to carry the pregnancy (either with or without various fertility medications).
There are many factors to take into consideration before starting IVF treatment. To get the best understanding of the IVF process and what to expect, it’s important to consult with your healthcare provider.
What do you do to prepare for IVF treatment?
Before starting IVF treatment, you’ll need a thorough medical exam and fertility tests. Your partner will be examined and tested as well. Some of the preparation you’ll go through includes:
- IVF consultation (meet with healthcare providers to discuss the details of the IVF process).
- A uterine exam, up-to-date Pap test and mammogram (if over 40).
- A semen analysis.
- Screening for sexually transmitted infections (STIs) and other infectious diseases.
- Ovarian reserve testing, and blood and urine tests.
- Instructions on how to administer fertility medications.
- Genetic carrier screening.
- Sign consent forms.
- Uterine cavity evaluation (hysteroscopy or saline-infused sonography (SIS)).
Your healthcare provider will have you start supplementing with folic acid at least three months before embryo transfer.
What can you expect after IVF treatment?
There are some mild symptoms that you can experience after embryo transfer:
- Mild bloating and cramping.
- Breast tenderness from high estrogen levels.
- Spotting.
- Constipation.
Many people will return to normal activities right after their egg retrieval procedure. However, you shouldn’t drive for 24 hours after having anesthesia. Around nine to 14 days after the embryos are transferred, you’ll return to the clinic for a pregnancy test using a blood sample.
How do IVF injections work?
During your IVF cycle, you’ll take injectable hormone medications to encourage the entire group of that cycle’s eggs to mature simultaneously and fully. Your healthcare provider will determine the type of drug, frequency and dosages you need for your treatment. This is based on your age, medical history, hormone levels and your response to previous IVF cycles if applicable. You can expect to inject fertility medicine for around eight to 14 days.
Your healthcare provider will determine the type of drug, frequency and dosages you need for your treatment. This is based on your age, medical history, hormone levels and your response to previous IVF cycles if applicable. You can expect to inject fertility medicine for around eight to 14 days.
What medications are used for IVF?
Several medications can be used during a cycle of IVF. Some are taken orally, while others are injected, absorbed through your skin or placed in your vagina. Your healthcare provider will outline the exact dosage and timing depending on your treatment plan.
During the ovarian stimulation phase, you can expect to be given injectable hormones:
- Follicle stimulating hormone (FSH): These hormones work to stimulate your ovaries to produce eggs. You may be given one or a combination of both during your treatment. This is done for approximately right to 14 days.
- Human chorionic gonadotropin (hCG): Usually given as one final shot to trigger your eggs to mature and set ovulation in motion.

- Leuprolide acetate: A type of gonadotropin-releasing hormone (GnRH) agonist (initiates a response) that’s given as an injection. It can help control the stimulation process or be used as a trigger shot.
You may be prescribed birth control pills or injections before starting IVF. This provides a level of control over your cycle and allows all of your eggs to start simultaneously. Most people are given estrogen supplements to take before and after embryo transfer. This hormone helps thicken the lining of their uterus. Progesterone is also added to improve the chances of an embryo implanting and growing into a successful pregnancy. Most continue this throughout their first trimester. These medications are either oral, injectable, transdermal or vaginal.
What is assisted hatching in IVF?
Assisted hatching is a technique used in IVF treatment. It involves making a hole in your embryo’s outer shell before embryo transfer into your uterus. This hole helps your embryo “hatch” from its outer shell more easily.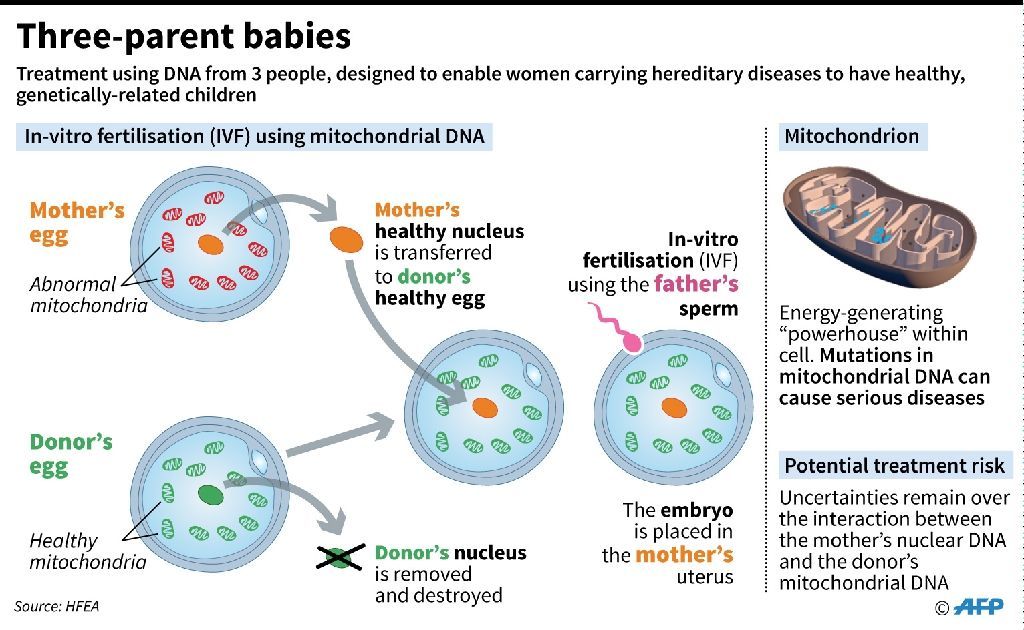 To get pregnant, your embryo must hatch and attach to the lining of your uterus. Think of assisted hatching like giving your embryo a head start and increasing its chances of hatching and implanting in your uterus. Assisted hatching is used primarily for those who’ve had several failed IVF cycles.
To get pregnant, your embryo must hatch and attach to the lining of your uterus. Think of assisted hatching like giving your embryo a head start and increasing its chances of hatching and implanting in your uterus. Assisted hatching is used primarily for those who’ve had several failed IVF cycles.
How much does IVF cost?
The average cost of an IVF cycle in the United States is $15,000. This doesn’t include the cost of medication, which can cost approximately $5,000 per cycle. It’s hard to give an exact amount because the cost depends on your health history and plan for treatment, insurance coverage (certain states may cover treatment) and the treatment center itself.
Risks / Benefits
What are the risks of IVF?
There are several risks associated with IVF treatment:
- Multiple births: A pregnancy with multiple babies carries a higher risk of premature labor.
- Premature delivery: You may have a slightly higher risk of your baby being born early or at a lower birth weight.
- Miscarriage: The rate of miscarriage is about the same as pregnancies from natural conception.
- Ectopic pregnancy: This is a condition where your fertilized egg implants outside of your uterus.
- Complications during egg retrieval: Bleeding, infection and damage to your bladder, bowel or reproductive organs during the egg retrieval process.
- Ovarian hyperstimulation syndrome (OHSS): A rare condition that causes abdominal pain, nausea, vomiting, diarrhea, rapid weight gain, bloating, shortness of breath and inability to urinate.
What are the most common side effects of IVF?
Some experience side effects from the fertility medications used during the ovulation stimulation phase of IVF. These include:
- Nausea and vomiting.
- Hot flashes.
- Headaches.
- Enlargement of their ovaries.
- Abdominal pain.
- Bruising from IVF injections.

After the transfer of your embryo, you should be able to resume normal activities. Your ovaries will be enlarged, and some discomfort may occur. Common side effects after embryo transfer are:
- Constipation.
- Bloating.
- Cramping.
- Breast tenderness (from high estrogen).
- Spotting.
IVF can be difficult — both physically and emotionally. Many people doing IVF treatment struggle with depression and anxiety. Infertility struggles and IVF can leave people feeling disappointed or overwhelmed. Talk with your healthcare provider about how you’re feeling so they can offer support through the process.
Are IVF pregnancies high risk?
An IVF pregnancy isn’t automatically considered high risk. An IVF pregnancy will be considered high-risk if there’s a medical condition that makes the birthing parent high risk. For example, advanced maternal age, expecting multiples or high blood pressure.
Recovery and Outlook
How effective is IVF in getting pregnant?
Your age is one of the strongest factors in the success of IVF. Your chance of becoming pregnant through IVF is much higher if you’re under 35 years old, and lower if you’re over 40 years old. The live birth rate also varies and is strongly associated with age. For example, the live birth rate when the birthing parent is under 35 and using their own eggs is around 46%, while the birth rate of a 38-year-old using their own eggs is about 22%.
Your chance of becoming pregnant through IVF is much higher if you’re under 35 years old, and lower if you’re over 40 years old. The live birth rate also varies and is strongly associated with age. For example, the live birth rate when the birthing parent is under 35 and using their own eggs is around 46%, while the birth rate of a 38-year-old using their own eggs is about 22%.
How long does it take to know you are pregnant after IVF?
It takes about nine to 14 days to test for pregnancy after embryo transfer. The exact timing may vary depending on the practice or fertility clinic. Your healthcare provider will most likely use a blood test to check for pregnancy. Blood tests measure hCG (human chorionic gonadotropin), which is the hormone produced by the placenta during pregnancy.
How soon after a failed IVF procedure can you try again?
Most treatment centers recommend you have one complete menstrual cycle between IVF cycles. The length of a menstrual cycle varies, but you can expect to wait four to six weeks after a negative test to start another cycle.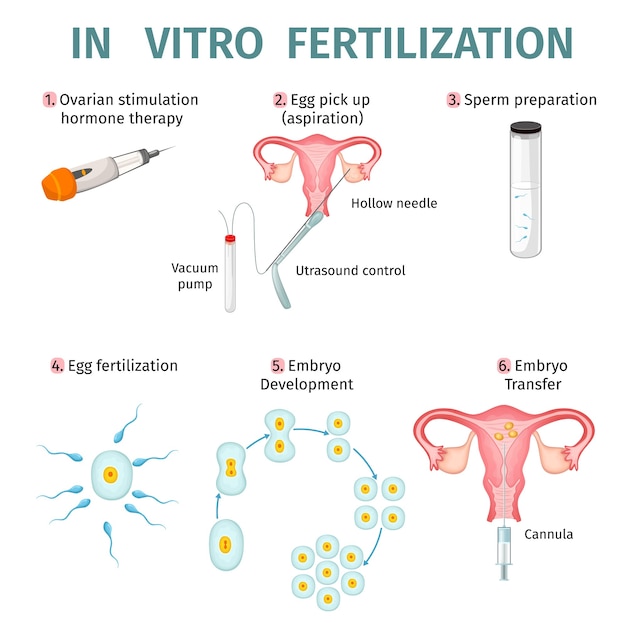 A small break between cycles is usually advised for health, financial and emotional reasons.
A small break between cycles is usually advised for health, financial and emotional reasons.
When to Call the Doctor
When should I contact my healthcare provider?
If you’re in the process of getting IVF treatment, you should contact your healthcare provider if any of the following happens:
- You develop a fever higher than 100.5 degrees Fahrenheit (or 38.05 Celsius).
- You have blood in your urine.
- There is heavy bleeding from your vagina.
- You have severe pelvic pain.
What questions should I ask the fertility clinic?
Selecting a fertility clinic and undergoing IVF is an important decision. Some questions you can ask are:
- What’s your success rate for couples like us?
- What’s your live birth rate per year?
- What’s your pregnancy rate per embryo transfer?
- How many live births are multiples?
- How much does the procedure cost?
- Can we freeze and store our embryos? For how long?
- Do you allow for gender/sex selection?
Additional Details
Can you select the gender during IVF?
Yes, it’s possible to select the sex of your baby during IVF.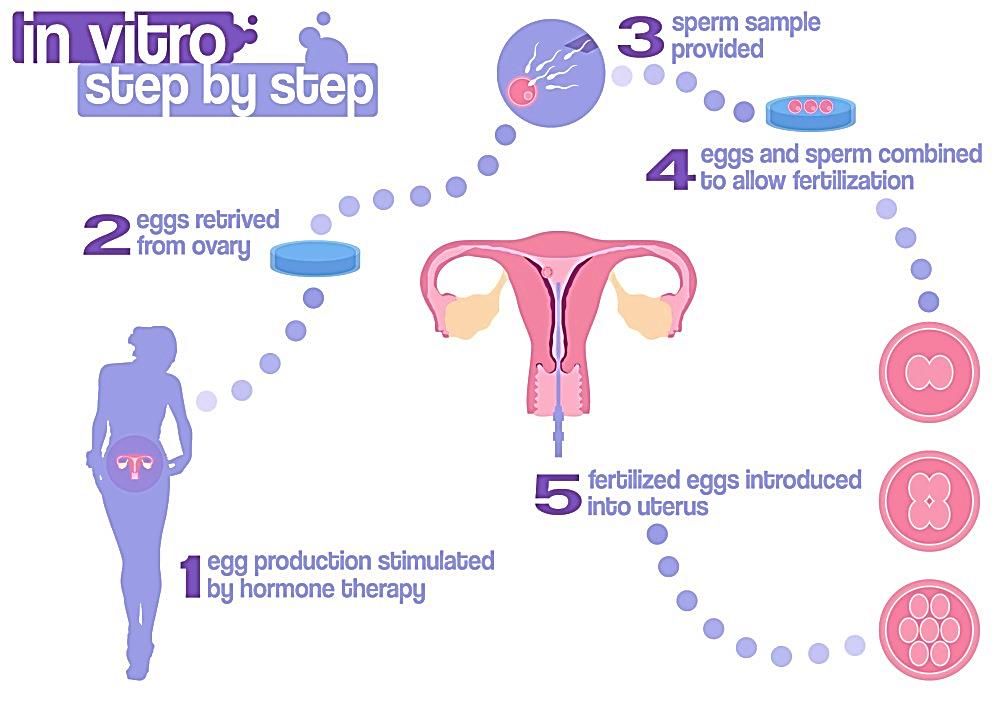 Before your embryo is implanted into your uterus, your embryo’s cells can be studied (embryonic testing) for either male or female chromosomes. Couples can choose to only implant the desired sex and discard the other embryos. This service is illegal in many countries outside the United States. Within the United States, not all practices or doctors provide this service.
Before your embryo is implanted into your uterus, your embryo’s cells can be studied (embryonic testing) for either male or female chromosomes. Couples can choose to only implant the desired sex and discard the other embryos. This service is illegal in many countries outside the United States. Within the United States, not all practices or doctors provide this service.
Is there anything I can do to increase my chances of pregnancy with IVF?
Several factors can determine the success of IVF — some within your control and others not. These factors include:
- Age.
- Height and weight.
- Number of previous births.
- Total number of pregnancies.
- Using your eggs or donor eggs.
- Number of IVF cycles.
- Success rate of the fertility clinic.
- Health conditions.
- Your cause of infertility.
Your healthcare provider will work with you to determine how you can increase your chances of becoming pregnant using IVF based on your situation and medical history.
What is the success rate of IVF by age?
Data collected in the U.S .is measured per egg retrieval, not per cycle. The average percentage of live births per egg retrieval in 2019 was:
- Younger than 35: 46.7%
- Ages 35 to 37: 34.2%
- Ages 38 to 40: 21.6%
- Ages 41 to 42: 10.6%
- Ages 43 and up: 3.2%
Why do IVF treatments fail?
IVF treatments can fail for many reasons and at any step in the IVF process. Some reasons an IVF cycle fails are:
- Premature ovulation.
- No eggs are developing.
- Too many eggs are developing.
- Egg isn’t fertilized by sperm.
- Sperm quality.
- Embryo stops growing or will not implant.
- Problems with egg retrieval or embryo transfer.
Your healthcare provider will be able to examine each step of the process with you and determine how to best move forward with future treatments.
Can IVF cause birth defects?
It’s not entirely known if IVF alone is responsible for birth defects. For non-IVF pregnancies, around 2% of all children will be born with a birth defect. Some studies show a slightly higher risk for babies born through IVF. This could be due to delayed conception or related to the underlying cause of infertility.
What is the best age to get IVF?
Research shows that your chances of getting pregnant or having a live birth after IVF treatment decreases beginning at age 35. The success rate declines significantly after age 40.
Should you freeze embryos during IVF treatment?
Embryo cryopreservation is done as part of most IVF programs. Some people choose to freeze and store embryos so they can have another chance at getting pregnant. Extra embryos can be frozen and stored for several years, although not all will survive the freezing and thawing process.
A note from Cleveland Clinic
IVF treatment is a personal and complicated process.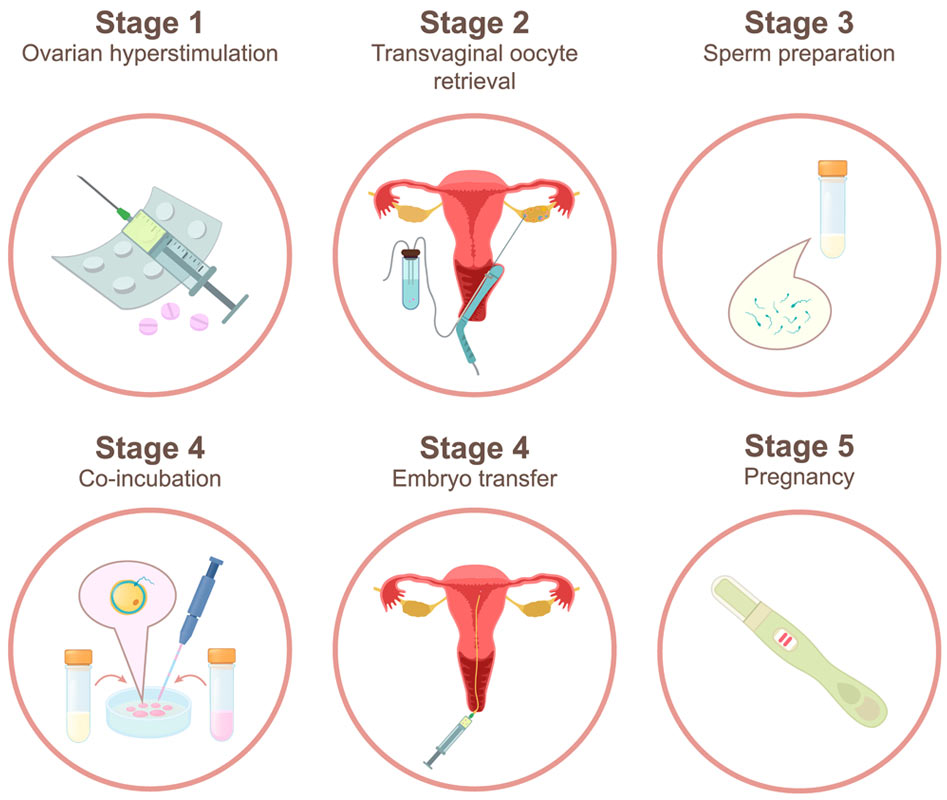 Speak openly with your healthcare provider so you understand all the steps involved. Your healthcare team is there to support you and your partner throughout your treatment.
Speak openly with your healthcare provider so you understand all the steps involved. Your healthcare team is there to support you and your partner throughout your treatment.
Children after IVF - the birth of children after IVF - Academician Grishchenko IVF Clinic and Infertility Treatment
Infertility has long been considered an insoluble problem for many couples who are faced with such a diagnosis. Today, with the development of reproductive technologies, in vitro fertilization has become a real salvation for thousands of families. However, despite the fact that IVF helps babies to be born into the world, disputes about how these very crumbs are born do not subside.
They arouse interest not only among parents who have decided to undergo the procedure, but also among doctors and even psychologists. Many of them argue that such children are at too high a risk of developing various pathologies.
Scientists' opinion
More than 35 years have passed since the birth of the very first child conceived through in vitro fertilization. And over the years, a lot of research has been done on the health of babies born after its use. According to the data obtained, it became known that IVF does not have a negative impact on the health of the child. That is, all those fears that many were worried about - an increased risk of oncology, deafness and other malformations, have no real basis. In children born after in vitro fertilization, the development of any intrauterine pathologies occurs no more often than when pregnancy occurs naturally. The probability of their occurrence is affected not by the method of conception, but by heredity, the gene pool, and even the individual characteristics of each particular woman.
And over the years, a lot of research has been done on the health of babies born after its use. According to the data obtained, it became known that IVF does not have a negative impact on the health of the child. That is, all those fears that many were worried about - an increased risk of oncology, deafness and other malformations, have no real basis. In children born after in vitro fertilization, the development of any intrauterine pathologies occurs no more often than when pregnancy occurs naturally. The probability of their occurrence is affected not by the method of conception, but by heredity, the gene pool, and even the individual characteristics of each particular woman.
The test of time
In addition to the scientifically proven facts about the "normality" of children born as a result of in vitro fertilization, one should take into account the fact that this method of conception is already showing real results. For more than 30 years, a huge number of children were born after IVF, and judging by their medical records, they are no different from the most ordinary babies.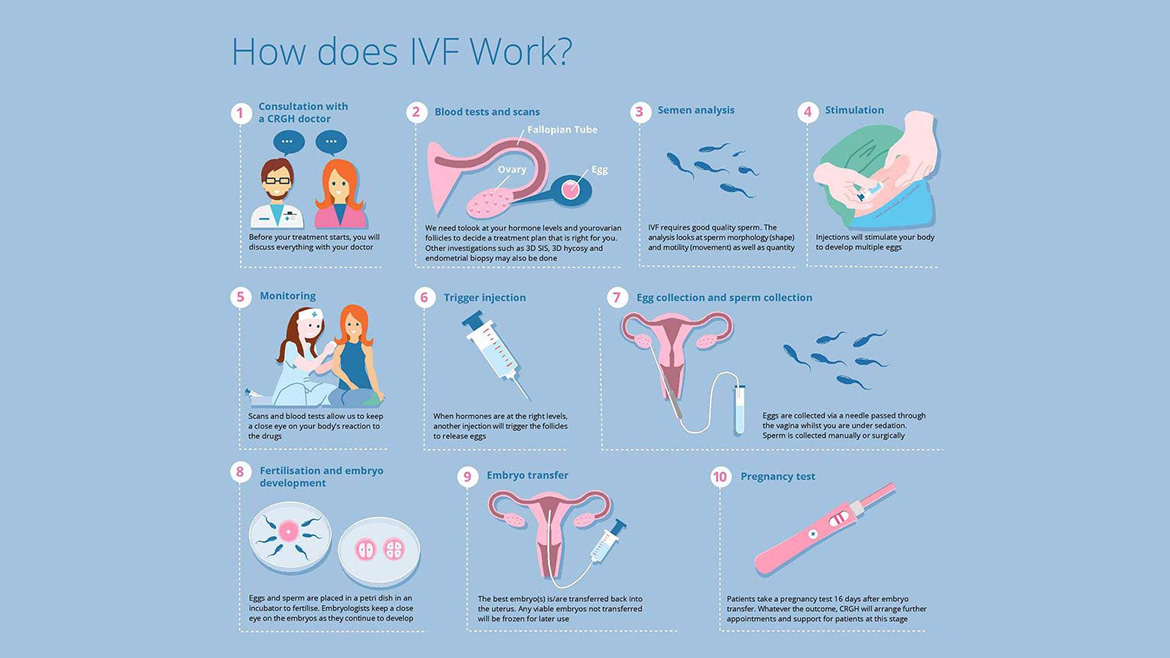 Moreover, some of the children after that had already reached childbearing age and in fact proved the falsity of the opinion that infertile couples can only give birth to infertile children - many people conceived “in a test tube” already have their own children.
Moreover, some of the children after that had already reached childbearing age and in fact proved the falsity of the opinion that infertile couples can only give birth to infertile children - many people conceived “in a test tube” already have their own children.
Benefits of IVF
There is an opinion that the use of in vitro fertilization not only does not harm the health of future babies, but can also have a beneficial effect on it. This opinion is based on the fact that before fertilization, embryologists carefully process the seminal fluid and select the most healthy and viable spermatozoa.
Some genetic diseases can also be avoided by using donor sperm for fertilization instead of the spouse's biological material, and the method of preimplantation genetic diagnosis allows only genetically normal embryos to be transferred into the uterine cavity.
Another important plus to this opinion is the fact that during IVF it is possible to determine the sex of the child in advance. And, despite the fact that in some countries such a service is prohibited, in some cases it is necessary for the birth of a healthy baby. For example, if parents have genetic diseases that are transmitted only through the male line.
And, despite the fact that in some countries such a service is prohibited, in some cases it is necessary for the birth of a healthy baby. For example, if parents have genetic diseases that are transmitted only through the male line.
Do children get sick more often after IVF?
Another myth associated with children born after in vitro fertilization is the sickness of such babies. But the fact that such children get sick more often is not actually revealed and remains only a rumor associated with this procedure.
IVF risks
There are certainly some risks associated with this type of insemination. For example, multiple pregnancy, which occurs after in vitro fertilization much more often than with a natural method of conception. Such a pregnancy is somewhat more complicated, since the load on the woman's body increases significantly. In addition, with such pregnancies, preeclampsia (preeclampsia), anemia, toxicosis and other unpleasant manifestations that do not have a positive effect on the fetus occur more often.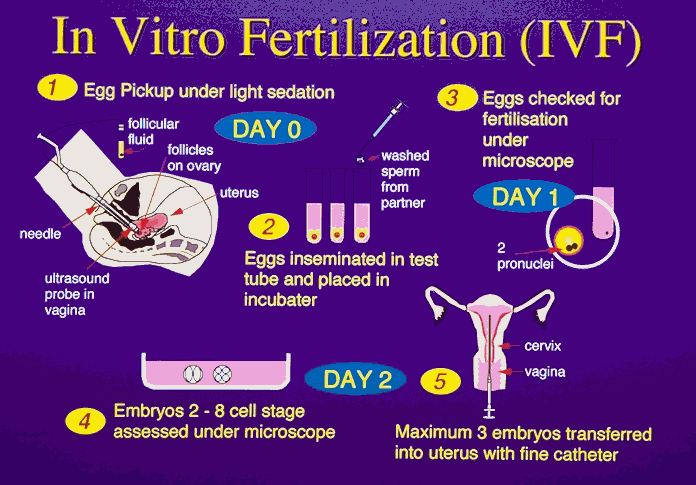 Also, multiple pregnancies are much more likely to end in premature birth, which is associated with a large load on the woman's body.
Also, multiple pregnancies are much more likely to end in premature birth, which is associated with a large load on the woman's body.
But it is worth remembering that all these complications can also occur when a multiple pregnancy occurs naturally. The only difference is that with IVF, such a pregnancy happens much more often.
Therefore, in order to avoid the risk of successful implantation of all embryos at once, today their number during replanting was reduced to two. And in some cases, when multiple pregnancy is contraindicated for a woman due to individual characteristics, only one embryo is implanted. This became possible thanks to the improvement of the work of embryologists and the increase in the efficiency of IVF.
Drawing a conclusion from the above, we can conclude that there is no difference between children after IVF and ordinary babies, except for the method of conception itself.
Children after IVF - myths and reality
Children after IVF - myths and reality | Clinic "IVF Center" in Kaliningrad- Infertility
- All about infertility
- Infertility treatment
- IVF cost
- ICSI
- Donation
- Donor eggs
- Donor sperm
- Surrogacy
- Laboratory
- Genetic diagnostics
- Diagnostics
- Cryopreservation
- Insemination
- Ultrasound
- Specialist consultations
- Gynecology
- Donor
- Become an oocyte donor
- Become a surrogate mother
Couples who decide to fight infertility with in vitro fertilization are faced with the question of whether their children will be healthy and will not be different from children whose conception occurred naturally.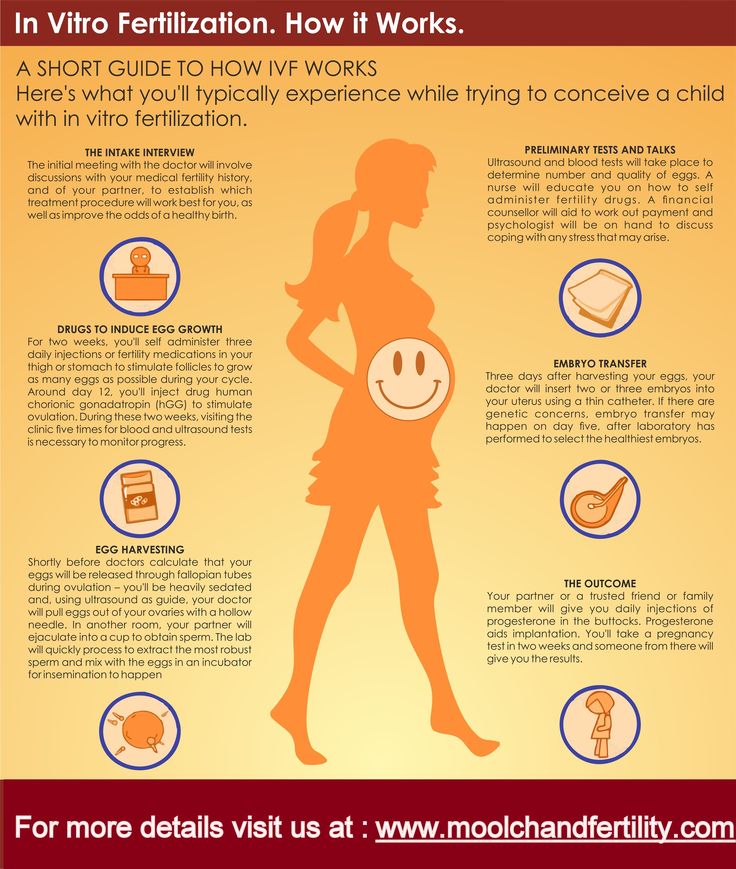 Today, IVF is a common and standard method of infertility treatment, but myths about children born through artificial insemination do not cease to arise. The only risk for a woman in the case of in vitro fertilization is the development of multiple pregnancy, accompanied by an increased burden on the mother's body and various complications.
Today, IVF is a common and standard method of infertility treatment, but myths about children born through artificial insemination do not cease to arise. The only risk for a woman in the case of in vitro fertilization is the development of multiple pregnancy, accompanied by an increased burden on the mother's body and various complications.
Children after IVF: the most common myths
- Children conceived through in vitro fertilization are not able to become parents themselves, as they are born sterile. The first child, whose birth was due to assisted reproductive technology, was born more than 30 years ago. After that, more than three million IVF children were born. Many of them themselves repeatedly became parents, while conception occurred naturally. The woman who became the first IVF child became a mother without the use of assisted reproductive technologies. All this is evidence that there is no connection between the way a child was conceived and the functioning of his reproductive system in the future.
- Children after in vitro fertilization are often born with malformations and genetic abnormalities. It is important to understand that the risk of having a child with genetic pathologies exists both in the case of a natural pregnancy and with the use of in vitro fertilization. It doesn't matter how the baby was conceived. As part of the in vitro fertilization program, specialists at the IVF Center clinic in Kaliningrad conduct pre-implantation genetic diagnostics of embryos, which makes it possible to identify genetic disorders even before the embryo is implanted in the uterus. Such measures help prevent the birth of a knowingly unhealthy child. In addition, in the case of IVF, doctors regularly monitor the health of the mother and the development of the fetus. It can be argued that the risk of having sick children after IVF is several times lower than during a pregnancy that occurred naturally. The health of a child, whose conception occurred due to this procedure or in a natural way, can be influenced by many factors - the age of the parents, their state of health, existing genetic diseases, and the environmental situation in the place of residence.

- Such children are characterized by poor health and get sick more often than naturally conceived babies. According to statistical observations, such children are not prone to frequent diseases. Babies receive all the necessary vaccinations after being discharged from the hospital and get sick with the same frequency as other children.
- Children after IVF lag behind in development. In this case, the situation is reversed. Children born after in vitro fertilization are always desired and long-awaited, parents pay a lot of attention to their physical and mental development.
Risks of IVF
Statistics show that the risks of giving birth to children after in vitro fertilization with any developmental pathologies or genetic abnormalities are not at all higher, but even lower than in the case of children whose conception occurred naturally.
The only risk in case of in vitro fertilization is multiple pregnancy. Twins in such cases are born several times more often than during natural pregnancy. Multiple pregnancy is accompanied by an increased burden on the body of the expectant mother.
Multiple pregnancy is accompanied by an increased burden on the body of the expectant mother.
Multiple pregnancy occurs due to the fact that as part of the in vitro fertilization program, in order to increase the likelihood of pregnancy, several healthy embryos are simultaneously placed in the uterus of a woman.
Multiple pregnancy develops in 50% of cases. In practice, patients are implanted with no more than two embryos. Due to this, the risk of multiple pregnancy and its accompanying complications is minimized. Only at the request of the woman, in the absence of contraindications from the doctor, a woman can transfer more than two embryos into the uterus.
Children after IVF: is there any difference
In fact, there are no differences between children born after IVF and naturally. Only the process of conception differs. As part of the in vitro fertilization program, medical intervention occurs only at the stage of the meeting of the germ cells of both partners, as well as when healthy embryos are transferred into the woman's uterus.