Problem with conceiving
Having trouble conceiving | Jean Hailes
Endometriosis
Endometriosis is a common and often painful condition that affects approximately ten per cent of women. It occurs when the tissue that normally lines the uterus (the endometrium) grows outside the lining of the uterus. The misplaced tissue commonly grows on the uterine (fallopian) tubes, the ovaries or the tissue lining the pelvis (the peritoneum).
How does endometriosis affect fertility?
It is thought that around 30% of women with endometriosis are infertile, however further research is needed to confirm this.
In mild endometriosis there is no obvious reason why infertility occurs. It may be because the endometriosis cells release chemicals that interfere with the ability to conceive or affect early normal development of the embryo.
In moderate to severe endometriosis, scarring may cause interference with ovulation and the passage of the egg along the tube because of damage or blockage. It can also prevent the sperm from reaching the egg.
Not all women with endometriosis are infertile. Many women have children without difficulty, have already had children before they are diagnosed, or eventually have a successful pregnancy.
Treatment options
Surgical treatment of endometriosis, such as an operation called a laparoscopy to remove the endometriosis, is believed to increase the chances of pregnancy.
In an operation using laparoscopy the overall pregnancy rate was approximately 42% of women with endometriosis [1]. Approximately 45% of women will develop a recurrence of endometriosis after laparoscopic surgery for endometriosis [2].
If surgical treatment is unsuccessful, in vitro fertilisation (IVF) treatments may also be considered. However, before trying this form of treatment it is important that your endometriosis is properly treated, as the oestrogen levels involved may flare up any existing endometriosis.
Adenomyosis
Adenomyosis is a condition of the uterus (womb) where the cells which normally form a lining on the inside of the uterus also grow in the muscle wall of the uterus. If adenomyosis is centred in one area, it can lead to a mass of adenomyosis called an adenomyoma.
If adenomyosis is centred in one area, it can lead to a mass of adenomyosis called an adenomyoma.
Adenomyosis is only seen in women in their reproductive years because its growth requires oestrogen. After menopause, adenomyosis lessens because of the lack of oestrogen.
Does adenomyosis affect fertility?
Studies suggest there may be changes in the ability of the uterine muscles to contract appropriately. Also, these endometrial cells inside the muscle may release body chemicals which lead to subfertility.
Fibroids
Fibroids (also known as uterine fibromyomas, leiomyomas or myomas) are non-cancerous growths or lumps of muscle tissue that form within the walls of the uterus (womb).
Fibroids can vary in size ranging from the size of a pea to the size of a rock melon or larger.
It is not known exactly why fibroids occur. However, we do know that the female hormones, oestrogen (estrogen) and progesterone play a significant role in stimulating the growth of fibroids.
Fibroids occur in women of reproductive age, growing at varying rates until the onset of menopause, when they tend to decrease in size and may slowly shrink in size due to the loss of oestrogen and progesterone.
Do fibroids affect fertility?
Infertility is not a common problem for women with fibroids, less than 3% of women may have fertility problems as a result of fibroids. Fibroids can interfere with implantation of the embryo into the uterus, increase the risk of miscarriage or impact the progress of labour depending on the size and position.
Polycystic Ovary Syndrome (PCOS)
PCOS is the most common endocrine (hormonal) disorder in women. Symptoms include menstrual problems such as irregular periods and anovulation (lack of ovulation), high androgen (testosterone) levels which can cause male patterned hair growth and acne and metabolic problems which cause weight gain and an increased risk of type 2 diabetes.
PCOS and fertility
One of the first things you may have been told when diagnosed with PCOS was that the condition can affect your ability to have children. Whilst this is true for some women who have PCOS, 60% of women with PCOS become pregnant naturally. Some women may experience reduced fertility or it may take longer to conceive.
Whilst this is true for some women who have PCOS, 60% of women with PCOS become pregnant naturally. Some women may experience reduced fertility or it may take longer to conceive.
In women with PCOS the hormone changes that can cause irregular cycles may also affect ovulation and therefore affect fertility. Lack of ovulation is the most common cause of infertility in PCOS. An anovulatory cycle is a menstrual cycle in which ovulation fails to occur. This means that you do bleed but do not release an egg or ovulate.
In addition, body weight has an impact on fertility for women especially for those with PCOS.
Further help
There are many things you can do to improve your fertility and treatments are available if you have difficulty conceiving. See your doctor to first discuss treatment of your PCOS symptoms tailored to your individual needs. This might include some changes to lifestyle and/or medication.
Premature & early menopause
Premature menopause
Premature menopause is when the final period occurs before a woman is 40. The reason for premature menopause may be because:
The reason for premature menopause may be because:
- your periods stopped spontaneously but early (premature ovarian failure)
- you have had surgery to remove both ovaries (oophorectomy)
- chemotherapy has caused ovaries to fail
Early menopause
Early menopause is when the final period occurs before a woman is 45. Again the reasons may be spontaneous, surgical or chemical.
Effect on fertility
With premature and early menopause, the ovaries run out of eggs earlier than expected and they are unable to produce an egg or the hormones required for pregnancy.
Very rarely, (about a 2-5% lifetime chance), a woman may have a spontaneous pregnancy after a diagnosis of premature/early menopause.
Sometimes, premature/early menopause is diagnosed when a woman has sought help for fertility. If the ovaries fail to respond to the hormones used to produce eggs or if eggs fail to fertilise, these may be signs of premature/early menopause developing.
For a woman who has gone through premature/early menopause, depending on her circumstance her options for having children include:
- a donor egg
- surrogacy with a donor egg
- adoption
To explore the best option for you, ask your doctor for a referral to a fertility specialist who is a member of one of the in vitro fertilisation (IVF) clinics.
Fertility & chemotherapy
If you have been diagnosed with cancer and premature/early menopause is likely to occur because of treatment for cancer, there are some things you can do before you have the treatment.
Before chemotherapy and/or radiotherapy, you could investigate your options for trying to preserve eggs for conception. There are a number of options including:
- egg preservation
- ovarian preservation
- ovarian biopsy and freezing
Egg preservation
This takes place before chemotherapy.
The ovaries are hormonally stimulated to produce eggs and the eggs are then collected.
If you have a male partner, the eggs can be fertilised with your partner's sperm and the embryos are then frozen. When you are ready for pregnancy, the embryos are transferred into the uterus.
If you do not have a partner, the unfertilised eggs may be frozen. When you are ready for pregnancy, the eggs are thawed and a male partner's sperm or donor sperm is used to fertilise them. (This technology is still in development and sadly the success is limited).
Ovarian preservation
Some women are given therapy with a GnRH agonist – a hormone that causes a chemical reaction to control the ovary and eggs temporarily. This therapy is given during chemotherapy. After the chemotherapy stops, the GnRH agonist stops and the menstrual cycle should return. This therapy is not well developed or researched.
Ovarian biopsy & freezing
This procedure takes place before chemotherapy starts. A piece of ovary is excised (cut away) and frozen. After the chemotherapy is complete, the ovarian tissue is transplanted under skin and with hormone stimulation, eggs are collected. This technique has recently shown some success although is still in the research phase.
This technique has recently shown some success although is still in the research phase.
Thyroid problems
Your thyroid is a small bowtie or butterfly-shaped gland, located in your neck, wrapped around the windpipe. The thyroid gland takes iodine (mostly found in foods such as seafood and salt) to produce thyroid hormones. Two key thyroid hormones are triiodothyronine (T3) and thyroxine (T4). These hormones help oxygen get into cells and regulate the body's metabolism. The thyroid hormones also affect other important functions of the body such as growth.
There are number of factors that can put you at a higher risk of thyroid disease:
- A personal history of autoimmune conditions, including Type 1 diabetes
- If you have grown up in an area that was iodine deficient
- If you have been exposed to head and neck radiation in the past
Thyroid conditions affect women five times more often than men.
If the thyroid is underactive, symptoms of hypothyroidism may occur. An overactive thyroid gland produces excess thyroid hormones and is called hyperthyroidism.
An overactive thyroid gland produces excess thyroid hormones and is called hyperthyroidism.
How a problem thyroid affects fertility and pregnancy
According to Dr Jennifer Wong, a consultant endocrinologist at Monash Health, a number of health problems are associated with a problematic thyroid:
- Decreased fertility making it much harder to become pregnant
- Increased risk of miscarriage
- Increased risk of pre-term or early delivery
- Hypertension (high blood pressure)
- Premature birth
Diagnosing thyroid dysfunction
It is very important to detect thyroid problems in women pre-pregnancy and during the first 12 weeks of pregnancy as the foetus is dependent on the mother's thyroid hormone in the first trimester.
A simple, specific blood test will determine whether you have thyroid dysfunction. You can see your doctor for this test.
Thyroid treatment
If you are diagnosed with a thyroid condition, treatment is quite easy and manageable.
Premature & early menopause
Premature menopause
Premature menopause is when the final period occurs before a woman is 40. The reason for premature menopause may be because:
- your periods stopped spontaneously but early (premature ovarian failure)
- you have had surgery to remove both ovaries (oophorectomy)
- chemotherapy has caused ovaries to fail
Early menopause
Early menopause is when the final period occurs before a woman is 45. Again the reasons may be spontaneous, surgical or chemical.
Effect on fertility
With premature and early menopause, the ovaries run out of eggs earlier than expected and they are unable to produce an egg or the hormones required for pregnancy.
Very rarely, (about a 2-5% lifetime chance), a woman may have a spontaneous pregnancy after a diagnosis of premature/early menopause.
Sometimes, premature/early menopause is diagnosed when a woman has sought help for fertility. If the ovaries fail to respond to the hormones used to produce eggs or if eggs fail to fertilise, these may be signs of premature/early menopause developing.
If the ovaries fail to respond to the hormones used to produce eggs or if eggs fail to fertilise, these may be signs of premature/early menopause developing.
For a woman who has gone through premature/early menopause, depending on her circumstance her options for having children include:
- a donor egg
- surrogacy with a donor egg
- adoption
To explore the best option for you, ask your doctor for a referral to a fertility specialist who is a member of one of the in vitro fertilisation (IVF) clinics.
Turner's syndrome
The most common genetic cause of infertility in women is Turner's syndrome.
Turner's syndrome is a chromosomal condition that alters development in females. This condition occurs in about 1 in 2,500 female births worldwide.
It is caused by the complete or partial lack of one of the X chromosomes (female sex chromosome). This results in a range of complications, including stunted growth and development, deafness, an increased risk of heart and kidney problems and infertility. Women with this condition tend to be shorter than average and are usually unable to conceive a child because of an absence of ovarian function.
Women with this condition tend to be shorter than average and are usually unable to conceive a child because of an absence of ovarian function.
The majority of women with Turner's syndrome are infertile. There are two types of Turner's syndrome – XO who never have periods and XX/XO Mosaic who can have periods but have an early menopause. Spontaneous pregnancies (less than 5% of women) are associated with a high risk of miscarriage, and chromosomal and congenital abnormalities.
Pregnancy can be achieved at present through IVF technology with donor egg or embryo.
Due to early menopause, women with Turner Mosaic syndrome should not delay exploring their pregnancy options for too long, if this is possible.
Counselling regarding fertility and pregnancy is highly recommended for all women with Turner's syndrome.
Problems Conceiving | Reproductive Science Center of New Jersey
Getting pregnant may seem simple, but the act of conceiving a child can often be very difficult. It involves many bodily functions and systems being in good condition in both the male and the female, all of which must happen in the right sequence and at the right time.
It involves many bodily functions and systems being in good condition in both the male and the female, all of which must happen in the right sequence and at the right time.
Consider that the average woman of reproductive age only has a 20 percent chance of getting pregnant in any month of trying. And if conditions are hampering male and/or female reproductive systems, the chances are much worse. Infertility – defined as not conceiving after 12 months of having sex on a regular basis with no contraception – affects as many as 1 in 8 couples.
Causes of infertility can range from not timing intercourse properly to being overweight to structural problems with the reproductive organs. Reproductive Science Center of New Jersey’s goal is to find out what factors are causing infertility in a woman or couple and develop a personalized treatment plan to help them achieve pregnancy.
The primary causes of failure to achieve pregnancy fall into three categories: medical issues, lifestyle factors and genetics. Patients can address some of these lifestyle issues and our reproductive endocrinologists can address most medical conditions. Genetic issues have no direct solution as far as correcting the genetic problem, but that doesn’t mean we can’t work around them.
Patients can address some of these lifestyle issues and our reproductive endocrinologists can address most medical conditions. Genetic issues have no direct solution as far as correcting the genetic problem, but that doesn’t mean we can’t work around them.
In this section
Sexual dysfunction may be a cause of a couple's infertility. RSC can help evaluate an individual’s or couple’s sexual health and improve it.
Read More
By Susan Scott MSW, LCSW - Most couples will face some degree of emotional distress when they are diagnosed and being treated for infertility. Contact the Reproductive Science Center of New Jersey for more information mental health professionals who deal with infertility.
Read More
Families experiencing infertility may be affected by or at risk of genetic disorders & miscarriage. RSC genetic counselors provide explanation and testing.
Read More
Lifestyle issues affecting conception
Lifestyle issues that impede fertility are factors that one can often change by choices and behaviors. As such, we encourage people having troubling getting pregnant to try these changes first, if they are applicable. Most of the lifestyle issues can affect both men and women.
Weight. This is one of the primary lifestyle issues that can cause infertility in both men and women. Women who are obese or overweight may experience problems with ovulation, which reduces the effectiveness of in vitro fertilization (IFV). In men, obesity can harm sperm production.
While consistent exercise is important to a healthy weight, women who are trying to get pregnant should avoid excessively strenuous workouts.
Diet. Without proper nutrients, a woman’s body doesn’t perform tasks efficiently, including reproduction. In particular, women should limit caffeine intake. Poor nutrition can also limit sperm production in men.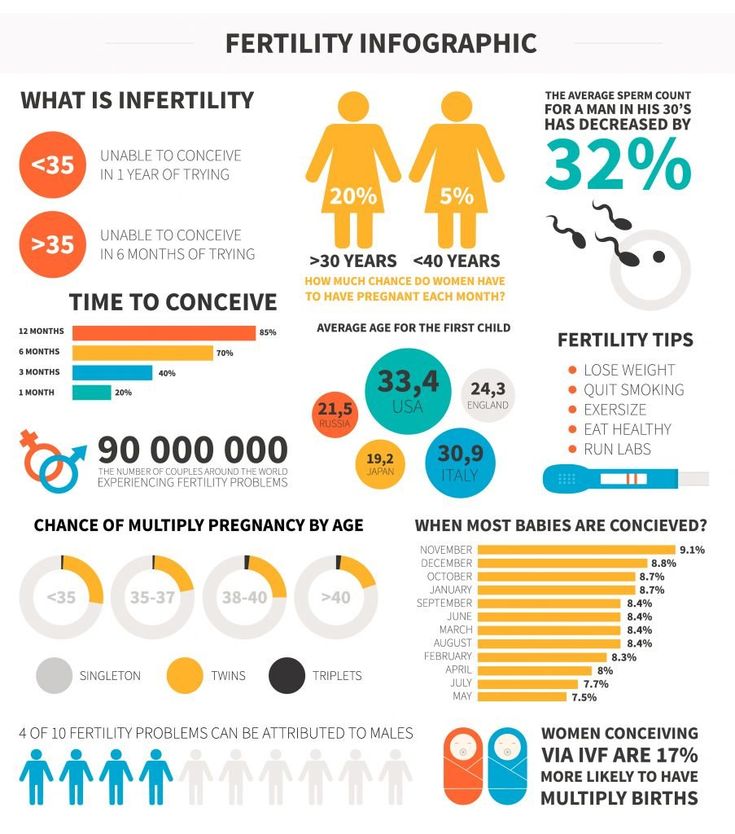
STDs. Sexually transmitted diseases (STDs) can cause infertility in women, and some STDs can block delivery of sperm in men. Safe sex with a limited number of partners is the best way to prevent infection.
Stress. This can disrupt hormone activity in women that regulates ovulation and can cause similar hormonal issues in men that inhibits healthy sperm.
Alcohol. Men should limit consumption, and women trying to get pregnant should avoid drinking altogether.
Illicit drug use. This can cause varied reproductive related problems in both sexes.
Exposure to toxins. Whether through work, outdoor activities or unhealthy indoor environments, chemicals, pesticides and other toxins can alter the hormonal balance in men and women, affecting fertility.
Temperature. Men should avoid things that raise the temperature of their scrotum, such as a laptop computer placed there.
Age. While not an adjustable factor, age is also a major influence in infertility, affecting females more dramatically than males. Men generally experience infertility issues later in life due to injury or illness.
Medical conditions that cause problems conceiving
Males and females have different medical issues and conditions, some present at birth, that can cause trouble getting pregnant. One medical condition may also lead to another illness or disorder that inhibits infertility.
Male medical issues
- Sperm problems are the primary medical cause of male infertility
- Infections, tumors, medications, surgeries
- Hormonal problems
- Erectile dysfunction and ejaculation issues
- Structural problems, including undescended testicles and varicocele
Female medical issues
- Ovulation disorders are the most common medical cause of infertility in women
- Structural defects
- Fallopian tube issues (hydrosalpinx)
- Uterine fibroids
- Ovarian cysts
- Anatomical uterine abnormalities
- Diseases and conditions that can result in some of the causes above
- Endometriosis
- Polycystic ovary syndrome
- Factors that make a woman prone to miscarriage
Genetic issues affecting conception
Genetic problems generally relate to chromosomal abnormalities and single gene issues. These often cause embryo implantation failure and pregnancy loss, as well as possibly resulting in birth defects when a child is born with a chromosomal or single gene defect.
These often cause embryo implantation failure and pregnancy loss, as well as possibly resulting in birth defects when a child is born with a chromosomal or single gene defect.
Chromosomal disorders can relate to one or more of an embryo’s chromosome pairs containing either one too many or one too few chromosomes. When the chromosome is not paired correctly, it is called aneuploidy. A chromosome may also have an abnormal structure. Both kinds of chromosome problems can be present in the female egg and/or the male sperm.
Single gene defects result from the embryo inheriting a genetic flaw from one or both parents. The gene could be one that results in cystic fibrosis or muscular dystrophy in birth. These single-gene defects can also cause embryo implantation failure or pregnancy loss.
Genetic issues often can be identified through preimplantation genetic screening, two types of embryo evaluation during IVF that can identify either form of genetic issues.
Unexplained infertility
Unexplained infertility is the diagnosis that fertility specialists give an individual or couple when fertility tests can not confirm a definitive cause for infertility.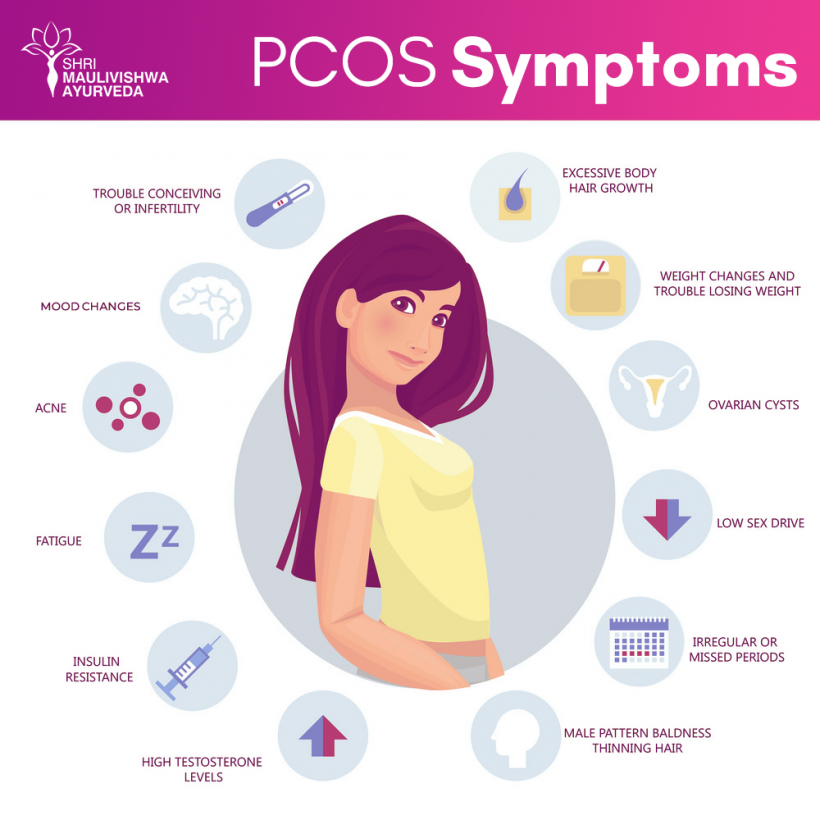 Unexplained infertility does not mean that there is not a cause for infertility; it simply means that the tests and examinations are not able to detect the reason an individual or couple is struggling to conceive.
Unexplained infertility does not mean that there is not a cause for infertility; it simply means that the tests and examinations are not able to detect the reason an individual or couple is struggling to conceive.
Unexplained infertility is the diagnosis in about 10-15% of infertility cases.
When is unexplained infertility the diagnosis?
Individuals and couples will receive an unexplained infertility diagnosis when the following conditions exist.
- The woman is ovulating regularly and has an appropriate ovarian reserve (antral follicle count).
- The female or female partner has at least one open fallopian tube (evaluated using a hysterosalpingogram).
- The male or male partner’s semen analysis is normal (including sperm count, shape and movement).
- Exams of the individual or of both partners did not result in the diagnosis of conditions or structural abnormalities that can cause infertility, such as uterine fibroids in women or varicoceles in men.

Unexplained infertility treatment
The inability to pin down a diagnosis with current fertility testing technology does not mean that a couple cannot get pregnant. In some cases, simple lifestyle changes or weight loss can improve the chances of pregnancy.
Fertility treatments such as fertility medications combined with IUI (intrauterine insemination) or in vitro fertilization (IVF) can dramatically improve the chances of pregnancy for those struggling with unexplained infertility.
Fomin's clinic — a network of multidisciplinary clinics
If pregnancy does not occur within six months of active sexual life, then this is one of the signs of infertility. But don't panic. This does not mean at all that you have infertility, perhaps it is enough for you, for example, to adjust your diet. Second, infertility is treated. Well, you should not immediately cheat yourself on the subject of IVF. Remember, infertility is not the same as IVF.
Infertility is a diagnosis that 10% of women all over the world have to live with: according to statistics, every fourth married couple is infertile. In this article we will talk about what female infertility is, how to live with it and whether it can be overcome.
Female infertility is a diagnosis made after a year of unsuccessful attempts to have children, subject to regular sex with a partner without contraception. If a woman is older than 35 years, the diagnosis is made faster - after 6 months. After 35 years, the ability to conceive gradually decreases, so older women should not delay treatment.
However, one should not rush to sad conclusions either. According to statistics, even completely healthy couples under the age of 30 manage to conceive a child in the first three months only in 20-37% of cases. At the same time, after six months, pregnancy occurs already in 80% of couples. Until a year has passed from the first attempt, there is no need to worry, be examined, and even more so, to be treated.
Pregnancy depends on many reasons - in order for the "stars to align" and all the factors to coincide, sometimes it takes some time.
For example, it is known that the easiest way to get pregnant is to make love 3-4 times a week. But a break of more than 5 days can adversely affect the quality of spermatozoa.
In addition, much depends on the lifestyle of parents - stress and heavy workload reduce fertility in both men and women. It's no surprise that many successful pregnancies have started during family vacations.
If less than 6-12 months have passed since the first attempt, you can try several "life hacks":
Choose the best time to conceive. According to some reports, the day of ovulation and 2-3 days before it are best suited for conception. To find out when ovulation occurs, a urinary express test for luteinizing hormone will help - a day or two before ovulation it will become positive. However, calculating the optimal time is not always the best option.
I always oppose the calculation of the optimal time for conception, because because of this, sex begins on a schedule in a couple's life, and this is one continuous stress. It seems to me that it is more reasonable to have sex 2-3 times a week during the entire cycle.
Kosolapova Inna Vladimirovna, gynecologist-reproductologist of the Fomina Clinic, chief physician
Do not use lubricants. Water-based, oil-based and silicone-based lubricants reduce sperm survival. But lubricants based on hydroxyethylcellulose have less effect on sperm survival - so if there is a lack of lubrication, you can continue to use them.
Stop dieting. Good nutrition is the key to a successful pregnancy. But don't overeat either. There is evidence that a body mass index (BMI) of 19 is ideal for pregnancy.-thirty. In women who have a BMI greater or less, the time to conception increases.
You can calculate your BMI manually by dividing your weight by your height squared. Alternatively, you can use the built-in calculator on the website of the medical organization, or download a special application.
Quit smoking and alcohol. Smoking increases the risk of infertility by 1.6 times. It is also better not to abuse alcohol - eat more than 20 grams of ethanol per day, the risks of "earning" infertility increase by 60%.
On the other hand, the position of the body during sex, based on the available data, does not affect the result in any way. The "missionary" position is suitable for conception just like any other.
If more than a year has passed and nothing helps, it's time to see a doctor. The diagnosis of "infertility" has the right to make only an obstetrician-gynecologist (reproductologist).
It is important to understand that infertility is not only a woman's problem. According to statistics, in the absence of children in a third of cases, the mother is “to blame”, in a third - the father, and in another third of cases the cause of infertility cannot be established. This means that with the diagnosis of "infertility" it is necessary to examine both partners.
Male infertility is diagnosed by a urologist/andrologist. But if you go to a family planning center, a reproductologist can make a diagnosis.
Most often, female infertility is associated with problems in the reproductive system: in the ovaries, fallopian (or fallopian) tubes, through which the egg passes from the ovaries to the uterus, and in the uterus itself. To figure out what exactly “broke down” in the female reproductive system, the doctor will collect an anamnesis, carefully examine the patient and prescribe tests. We talk more about this in the article "Diagnostics of female infertility".
Infertility is treated, and quite successfully — according to statistics, after diagnosis and therapy, children appear in 50% of women (without the use of assisted reproductive technologies: IVF, etc.). On the other hand, success depends on many factors, from the age and history of previous pregnancies to problems with the partner's sperm. Many factors influence the possibility of getting pregnant, so it can be difficult to predict the result.
If the problem is overweight or underweight, it is often enough to normalize the weight for a successful pregnancy. True, much more often the problem is associated with sex hormones - in this situation, the doctor will select the appropriate medication. And if the problem is in the obstruction of the fallopian tubes or in the uterus itself, surgery may be required.
In vitro fertilization (IVF) is available for patients for whom these treatments are not suitable or have not worked.
The essence of IVF is that the patient's ovaries are stimulated with the help of hormones, then the egg is taken and fertilized with the husband's sperm, then the embryo is "grown" for some time in a special incubator and transplanted into the mother's uterus. A baby is born in the same way as other children conceived "naturally".
In Russia, the IVF procedure can be done free of charge under the CHI policy. However, it is important to understand that this is a complex treatment method that requires serious preparation and gives the best result until the age of 40-45.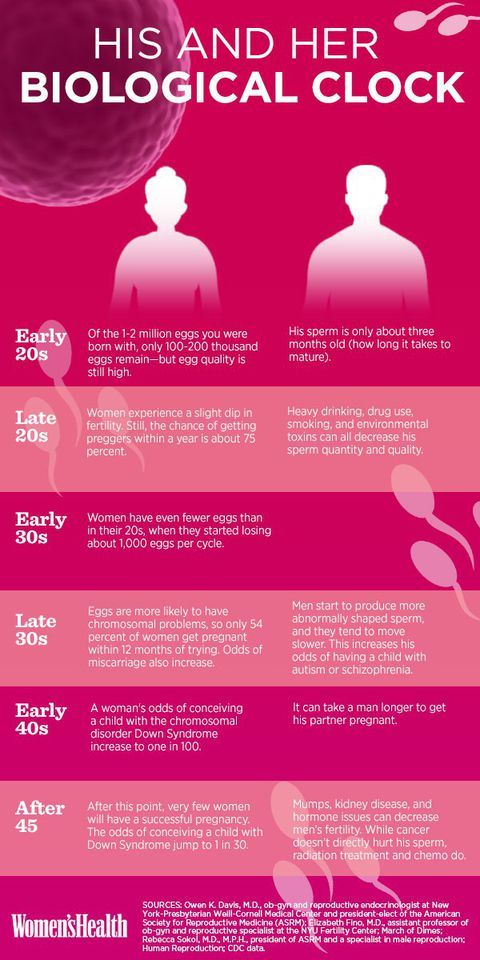 It is difficult to predict how successful IVF will be. According to statistics, the procedure ends with the birth of a live and healthy baby in about 27% of cases.
It is difficult to predict how successful IVF will be. According to statistics, the procedure ends with the birth of a live and healthy baby in about 27% of cases.
At the same time, IVF success rates vary greatly not only in different countries, but also in different clinics in the same city. There are clinics in which in 30-40% of cases it is possible to achieve a positive result on the first try.
Very often, mothers are concerned about possible health problems that may occur in children conceived through IVF. But in recent times there has been much less cause for concern than 20 years ago.
When the method was first created, all viable embryos that were obtained after fertilization were placed into the uterus of mothers “just in case”. If everyone took root, the mother often gave birth to twins or triplets, and sometimes “quadruples”. It is much harder to bear several children than one - and after all, mothers already had problems with pregnancy, otherwise IVF would simply not have been required.![]()
Today, the goal of the procedure is the birth of one healthy baby, so mothers transfer only one, maximum two of the best embryos. As a result, most children born after IVF do not differ much from their peers.
- Female infertility is as common as male infertility. If you can’t get pregnant within a year, you need to be examined, and sometimes treated together with your spouse.
- Infertility is a complex diagnosis that can have many causes. However, after treatment, about half of women successfully become pregnant and give birth to healthy babies (without IVF).
- IVF is a fairly effective way to give birth to a healthy baby. However, this method (like any other) has pros and cons, so you need to make a decision after consulting with an obstetrician-gynecologist or reproductologist.
Follow us
Why can't get pregnant | "Ivimed"
Such a topic often pops up in women's conversations, sections of forums on the Internet are full of this name, doctors often hear such a question at an appointment.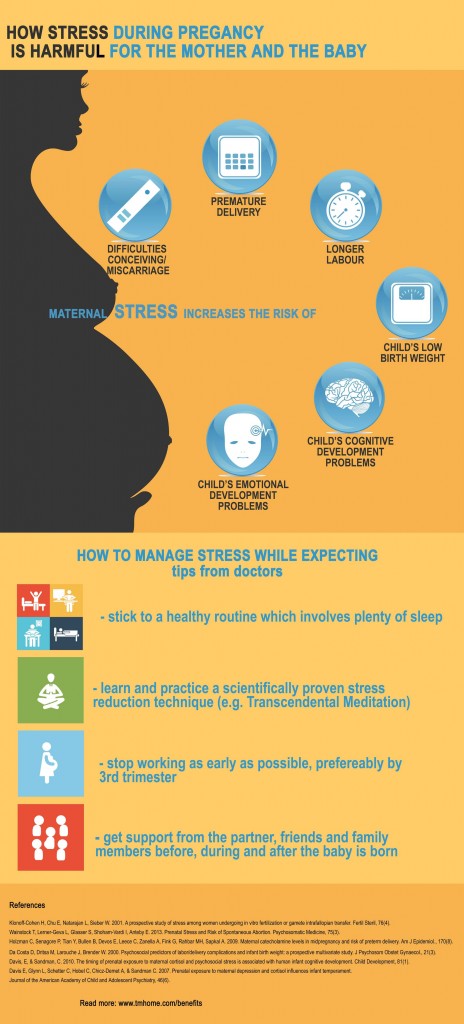 Why is it impossible to get pregnant with the great desire of the spouses? What are women and men doing wrong? Where is the problem that prevents the couple from becoming happy parents?
Why is it impossible to get pregnant with the great desire of the spouses? What are women and men doing wrong? Where is the problem that prevents the couple from becoming happy parents?
First of all, you need to decide when to sound the alarm. If conception does not occur within a year of regular unprotected sex, then a problem can be assumed.
The next important point is an adequate attitude to pregnancy planning and the birth of a child. It may seem to you that others manage to become parents quickly, and after 2-3 months of unsuccessful attempts, you start to panic. And in this state, you can make mistakes, because of which it is not possible to conceive a child.
Mistakes that interfere with becoming parents
Why a woman fails to get pregnant - usually this is how the question is formulated. In fact, the cause of problems with conception can lie both in the female and in the male body. Therefore, the first mistake is the belief that the inability to conceive a child is associated exclusively with the “female” factor.
The second mistake of future parents is not to take care of their health. “I can’t get pregnant,” complain women who have not visited a gynecologist for a long time, did not take tests, did not check the thyroid gland, etc. Men who continue to smoke, drink alcohol, ignore ailments and symptoms of chronic diseases, just as often do not see the connection between their attitude to health and the fact that they fail to conceive a child.
Stressed life is another mistake modern couples make. Women are especially prone to experiences when they fail to get pregnant. Unrest negatively affects health and further delays the desired pregnancy.
Despite the enlightenment of modern society, some of the fair sex still do not know that it is necessary to monitor the menstrual cycle and know the time of ovulation, when the probability of conception is maximum. You can calculate the time of ovulation yourself or ask your gynecologist for help. Usually, a mature and ready-to-fertilize egg leaves the ovary in the middle of the menstrual cycle (with an average cycle of 28 days, this happens approximately on day 14).
Another mistake that parents-to-be make is using dubious recipes or traditional methods. Instead of signing up for a consultation with a gynecologist or reproductologist, people look for advice on the Internet, among friends, use tools that not only do not bring results, but also harm.
For example, women douche with herbal decoctions or soda solution. Such procedures wash out the natural microflora of the internal reproductive organs, and can lead to inflammation or erosion. Someone goes to the bathhouse to relax and create a psychological mood favorable for conception. However, high temperatures are not as beneficial for the body as they seem, especially they harm men by worsening the quality of sperm.
What to do?
If you have managed to eliminate all of the above errors, but you are not able to get pregnant within a year, you need to consult a doctor. Reproductologist deals with issues of human reproductive health. Both spouses are welcome to attend.