Pregnant women going into labor
Pregnancy – labour - Better Health Channel
Labour is divided into 3 stages. The first stage is the dilation of the cervix, the second stage is the birth of the baby, and the third stage is the delivery of the placenta. For first-time mothers, labour takes around 12 to 14 hours. Women who have undergone childbirth before can expect about 7 hours of labour.
Recognising the start of labour
Braxton-Hicks contractions are sometimes mistaken for labour. These ‘false’ contractions usually start halfway through the pregnancy and continue all the way through. You may find these contractions visibly harden and lift your pregnant belly.
It is not known what triggers the onset of labour, but it is thought to be influenced by the hormone oxytocin, which is responsible for causing uterine contractions.
Symptoms of going into labour
Some of the signs and symptoms of going into labour may include:
- period-like cramps
- backache
- diarrhoea
- a small bloodstained discharge as your cervix thins and the mucus plug drops out (this is called a ‘show’)
- a gush or trickle of water as the membranes break
- contractions.
First stage of labour
The first stage of labour involves the thinning of the cervix and its dilation to around 10 cm. The first stage is made up of three different phases:
- The latent phase – Generally, this stage is the longest and the least painful part of labour. The cervix thins out and dilates zero to three centimetres. This may occur over weeks, days or hours and be accompanied by mild contractions. The contractions may be regularly or irregularly spaced, or you might not notice them at all.
- The active phase – The next phase is marked by strong, painful contractions that tend to occur three or four minutes apart, and last from 30 to 60 seconds. The cervix dilates from 3 to 7–8 centimetres.
- The transition phase – During transition, the cervix dilates from 8 to 10 centimetres (that is, fully dilated). These contractions can become more intense, painful and frequent. It may feel as though the contractions are no longer separate, but running into each other.
 It is not unusual to feel out of control and even a strong urge to go to the toilet as the baby’s head moves down the birth canal and pushes against the rectum.
It is not unusual to feel out of control and even a strong urge to go to the toilet as the baby’s head moves down the birth canal and pushes against the rectum.
Throughout the first stage of labour, careful monitoring and recording of your wellbeing and that of your baby, and the progress of your labour, is important. This is to ensure that labour is progressing normally and that any problems are recognised early and well communicated.
Second stage of labour
The second stage of labour is from when your cervix is fully dilated to the time your baby is born. The contractions during this time are regular and spaced apart. As each contraction builds to a peak, you may feel the urge to bear down and push. The sensation of the baby moving through the vagina is described as a stretching or burning, particularly as the baby’s head crowns (appears at the vaginal entrance).
At the time of birth, a doctor or midwife may guide your pushing to enable a gentle, unhurried birth of your baby's head. Sometimes the umbilical cord is wound around the baby's neck. If possible, the doctor or midwife will loosen it, loop it over your baby's head, or clamp and cut it to allow your baby to be born safely.
Sometimes the umbilical cord is wound around the baby's neck. If possible, the doctor or midwife will loosen it, loop it over your baby's head, or clamp and cut it to allow your baby to be born safely.
Once the head has emerged, your midwife or doctor will guide your baby’s body so the shoulders come out. The rest of the baby will then follow.
If this is your first baby, the second stage of labour can last up to 1 to 2 hours, particularly if you have had an epidural. If you have had a baby before, this stage is often much quicker.
Monitoring of your condition and that of your baby is increased during the second stage of labour. A long second stage of labour can result in risks for you and your baby. If your labour is not progressing, it is important that the reason is worked out and steps are taken to help you.
Third stage of labour
After the birth of your baby your uterus gently contracts to loosen and push out the placenta, although you may not be able to feel these contractions. This may occur 5 to 30 minutes after the birth of your baby.
This may occur 5 to 30 minutes after the birth of your baby.
The muscles of the uterus continue to contract to stop the bleeding. This process is always associated with a moderate blood loss – up to 500 ml.
In this stage of labour, one of the potential problems is excessive bleeding (postpartum haemorrhage), which can result in anaemia and fatigue. This is why the third stage is carefully supervised.
There are two approaches to managing the third stage:
- Active management – this is the common practice in Australia. After the birth of your baby, the midwife or doctor gives you (with your consent) an injection of oxytocin, clamps and cuts the umbilical cord, and then carefully pulls on the cord to speed up delivery of the placenta. Active management has been found to reduce excessive blood loss and other serious complications.
- Expectant management – the placenta is allowed to deliver on its own, aided by gravity or nipple stimulation only.
 In this approach the umbilical cord stays connected to the baby until the cord stops pulsating.
In this approach the umbilical cord stays connected to the baby until the cord stops pulsating.
Monitoring your baby during labour
During labour, your baby's heart rate will be checked regularly. If you have had a low risk pregnancy and there are no problems at the onset of labour, your baby's heart will be listened to every 15 to 30 minutes using a small hand-held Doppler ultrasound device or Pinard (fetal stethoscope). This equipment can be used regardless of the position you are in.
If you had problems during pregnancy or if problems arise during your labour, your baby’s heart rate may be monitored continuously using a cardiotocograph (CTG).
A CTG involves having two plastic disks (receivers) strapped to your abdomen and held in place by two belts. The receivers are attached to a machine, which may limit your movement. Some hospitals have machines that enable you to move around freely while you are being monitored. This is known as telemetry.
Care of the perineum during birth
The area between the vagina and anus is called the perineum. Once the baby's head starts to crown (appear) the perineum will tear if it can't stretch enough. These naturally occurring tears can be difficult to stitch and may not heal very well. In around 3–4 per cent of cases, the vagina tears right through to the anus.
Once the baby's head starts to crown (appear) the perineum will tear if it can't stretch enough. These naturally occurring tears can be difficult to stitch and may not heal very well. In around 3–4 per cent of cases, the vagina tears right through to the anus.
An episiotomy is an intentional cut of the perineum, using a pair of scissors. This clean cut is much easier to control and repair, tends to heal better than a tear, and is less traumatic to the underlying muscle and tissue. An episiotomy may be needed during the last part of the second stage of labour if:
- the birth needs to be quicker if you or your baby show signs of distress
- you need an assisted vaginal birth
- you are showing signs that you may tear badly.
If you are having your first baby, you may help prevent tearing by massaging the perineum during the weeks prior to the birth. Massaging the perineum during the second stage of labour has not been shown to stretch tissues and therefore does not reduce perineal injury.
Episiotomies should be performed only if needed. They should not be 'routine' as they do not reduce the risk of severe perineal injury, urinary stress incontinence or trauma to the baby.
Suggestions for preparing for labour
Some women may find the following activities helpful in preparing for labour:
- choose your support person – someone you are comfortable with and who will help you rather than distract you during the different stages of labour
- yoga
- relaxation exercises
- hypnotherapy (a state of relaxation)
- childbirth education – for you and your support person.
Early stages of labour
Be guided by your doctor or midwife, but general suggestions for a woman approaching labour include:
- Once you go into early labour, take the opportunity to rest and relax at home. There is no need to be in hospital until the contractions are regular and painful.
- Call your support person to let them know your labour is beginning.

- Once the contractions are around 7 to 10 minutes apart, start timing them. Do this by noting how many minutes elapse between the start of one contraction and the start of the next.
- If you are unsure whether to stay home or go to the hospital, ring and speak to one of the midwives. They will ask you a number of questions and help you decide what to do.
- Once your contractions are 5 minutes apart, or if you live a long distance from the intended place of birth (often the hospital), or if you no longer feel comfortable being at home, go to the intended place of birth.
- If your waters break or if you start bleeding from the vagina, go immediately to hospital.
Once you are in your intended place of birth
Suggestions for labour once you are in your intended place of birth include:
- Drink plenty of fluid (water, juice or iceblocks).
- Suck on sweets to keep up your energy.
- Vary your position to keep as comfortable as possible (standing, kneeling, lying down, straddling a chair, or on all fours).
- Have a bath or hot shower.
- Ask your support person for a back rub or massage.
- Try to relax between contractions.
- If you need or want it, discuss having some pain relief.
- Resist any urge to push until your cervix is fully dilated (your midwife will let you know when this has occurred).
- The pressure of your baby’s head helps to widen your cervix, so use gravity and walk around, stand or sit upright.
- Don’t feel embarrassed or inhibited by your appearance or behaviour – your midwife has seen it all before. If you want to grunt, yell or swear – go ahead.
- Remember that passing a bowel motion during labour is normal and nothing to be concerned about.
Having a support person
Having a support person with you can help enormously during labour. Your support person can:
- encourage you
- give emotional support
- help to make you comfortable
- help with breathing techniques
- provide ice to suck if you are thirsty
- provide a heat pack for your back or a cool face washer for your forehead
- massage your back
- celebrate the arrival of your baby with you.

Where to get help
- Your GP (doctor)
- Your hospital or birth centre
- Obstetrician
- Midwife
Labor | Johns Hopkins Medicine
What You Need to Know
- Labor is a series of continuous, progressive contractions of the uterus that help the cervix dilate (open) and efface (thin). This allows the fetus to move through the birth canal.
- Labor usually starts two weeks before or after the estimated date of delivery. However, the exact trigger for the onset of labor is unknown.
- While the signs of labor may vary, the most common are contractions, rupture of the amniotic sac (“breaking your water”) and bloody show.
- Labor is typically divided into three stages: dilation and effacement of the cervix, pushing and the delivery of the placenta.

- Pain management options during labor include nonmedicated measures, analgesics and anesthesia.
Definition of Labor
Labor is a series of continuous, progressive contractions of the uterus that help the cervix dilate and efface (thin out). This lets the fetus move through the birth canal. Labor usually starts two weeks before or after the estimated date of delivery. However, the exact trigger for the onset of labor is unknown.
Signs of Labor
While each woman experiences labor differently, some common signs of labor may include:
-
Bloody show. A small amount of mucus, slightly mixed with blood, may be expelled from the vagina.
-
Contractions. Uterine muscle spasms that occur at intervals of less than 10 minutes may signify that labor has started. These may become more frequent and severe as labor progresses.
-
Rupture of the amniotic sac (bag of water).
 If you experience amniotic fluid gushing or leaking from your vagina, go to the hospital immediately and contact your health care provider. Most women go into labor within hours of the amniotic sac breaking. If labor does not begin soon after rupturing your amniotic sac, you will be given medications to induce your labor. This step is often taken to prevent infection and other delivery complications.
If you experience amniotic fluid gushing or leaking from your vagina, go to the hospital immediately and contact your health care provider. Most women go into labor within hours of the amniotic sac breaking. If labor does not begin soon after rupturing your amniotic sac, you will be given medications to induce your labor. This step is often taken to prevent infection and other delivery complications.
If you are unsure about the start of your labor, call your health care provider.
Different Stages of Labor
Typically, labor is divided into three stages:
-
First stage. During the onset of labor, your cervix will complete dilation. Early in this stage, you may not recognize that you are in labor if your contractions are mild and irregular. Early labor is divided into two phases:
-
The latent phase is marked by strong contractions that usually occur at five- to 20-minute intervals.
 During this phase, your cervix will dilate approximately 3 to 4 centimeters and efface. This is usually the longest and least intense phase of labor. You may be admitted to the hospital during this phase. Your doctor will perform pelvic exams to determine the dilation of the cervix.
During this phase, your cervix will dilate approximately 3 to 4 centimeters and efface. This is usually the longest and least intense phase of labor. You may be admitted to the hospital during this phase. Your doctor will perform pelvic exams to determine the dilation of the cervix. -
The active phase is signaled by the dilation of the cervix from 4 to 10 centimeters. Your contractions will likely increase in length, severity and frequency, occurring at three- to four-minute intervals. In most cases, the active phase is shorter than the latent phase.
-
-
Second stage. Often referred to as the pushing stage of labor, this stage starts when your cervix is completely opened and ends with the delivery of your baby. During the second stage, you become actively involved by pushing the baby through the birth canal. Crowning occurs when your baby’s head is visible at the opening of the vagina.
 The second stage is usually shorter than the first stage, and may take between 30 minutes and three hours for your first pregnancy.
The second stage is usually shorter than the first stage, and may take between 30 minutes and three hours for your first pregnancy. -
Third stage. After your baby is delivered, you will enter the third and final stage of labor. This stage involves the passage of the placenta (the organ that nourished your baby inside of the uterus) out of the uterus and through the vagina. The delivery of the placenta may take up to 30 minutes.
Since each labor experience is different, the amount of time required for each stage will vary. If labor induction is not required, most women will deliver their baby within 10 hours of being admitted to the hospital. Labor is generally shorter for subsequent pregnancies.
Johns Hopkins Hospital Designated as Baby-Friendly
The Baby-Friendly Hospital Initiative, a global program launched by the World Health Organization and the United Nations Children’s Fund, has designated The Johns Hopkins Hospital as Baby-Friendly. This designation is given to hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding.
This designation is given to hospitals and birthing centers that offer an optimal level of care for infant feeding and mother-baby bonding.
Learn more
Induction of Labor
In some cases, labor has to be induced or stimulated to begin. The reasons for induction vary. Labor induction is not initiated before 39 weeks of pregnancy unless there is a problem. The most common reasons for induction include the following:
-
The mother or fetus is at risk due to complications.
-
The pregnancy has continued too far past the due date.
-
The mother has pre-eclampsia, eclampsia or chronic high blood pressure.
-
The fetus has been diagnosed with poor growth.
Labor may be induced by:
-
Inserting vaginal suppositories that contain prostaglandin to stimulate contractions.
-
Giving an intravenous (IV) infusion of oxytocin (a hormone produced by the pituitary gland that stimulates contractions) or a similar drug.

-
Artificially rupturing the amniotic sac.
Hospital Care During Labor
When you first arrive at the hospital in labor, the nursing staff may perform a physical exam of your abdomen to determine the size and position of the fetus. The nurses may also examine your cervix for dilation and effacement.
To monitor your health, the nursing staff may check the following:
In addition, your baby’s health is carefully monitored during labor. A monitor may be placed over your abdomen to keep track of the fetal heart rate.
You may receive IV fluids during labor. The IV line, a thin, plastic tube inserted into a vein (usually in your forearm), can also be used to give medicine. IV fluids are usually given once active labor has begun and when you have epidural anesthesia.
Pain Management Options During Labor
You have many options to relieve pain during labor and delivery. In general, you and your health care provider should choose the safest, most effective method of pain relief available. This decision will be determined by your:
This decision will be determined by your:
The following are the most common natural and medication-based methods for managing the pain associated with labor and delivery:
Nonmedicated Pain Management
As part of natural childbirth, these pain management strategies provide comfort and relieve stress without the use of medication. Many women have successfully learned natural techniques to help them feel more comfortable and in control during labor and birth. These techniques include:
-
Relaxation. This technique can improve your ability to detect and release tension. During progressive relaxation, you can learn to relax various muscle groups in series.
-
Touch. This may include massage or light stroking to relieve tension. A jetted bath or a shower during labor may also help relieve pain or tension. Ask your health care provider before taking a tub bath during labor.
-
Hot or cold therapy.
 A warm towel or a cold pack may help relax tense or painful areas.
A warm towel or a cold pack may help relax tense or painful areas. -
Imagery. Using the mind to form mental pictures may help create and promote relaxed feelings.
-
Meditation or focused thinking. Meditation helps your mind focus on an object or task, such as breathing, instead of discomfort.
-
Breathing. These techniques use different patterns and types of breathing to help direct your mind away from discomfort.
-
Positioning and movement. Many women find that changing positions and moving around during labor helps to relieve discomfort and may even accelerate the process. Rocking in a rocking chair, sitting in the Tailor sit position, sitting on a special birthing ball, walking or swaying may also help relieve discomfort. Your health care provider can help you find comfortable positions that are safe for you and your baby.

Medicated Pain Management
Analgesics. Pain relief medications, such as meperidine, may be used during labor in small amounts with very few complications. However, if given in large amounts or in repeated doses, analgesics can slow the activity of the breathing center in the brain of the mother and child.
Anesthesia. This type of medicine is designed to cause a loss of sensation in various areas of the body. Anesthesia medications include:
-
Local block. Anesthesia injected in the perineal area (the area between the vagina and rectum) numbs the area for repair of a tear or episiotomy after delivery.
-
Pudendal block. Used for vaginal deliveries, this type of local anesthesia is injected into the vaginal area affected by the pudendal nerve. Since it causes complete numbness in the vaginal area without affecting the contractions of the uterus, you can remain active in pushing the baby through the birth canal.

-
Epidural anesthesia (epidural block). This type of anesthesia involves infusing numbing medications through a thin catheter that has been inserted into the space that surrounds the spinal cord in the lower back, causing a loss of sensation in the lower body. Infusions of medications may be increased or stopped as needed. This type of anesthesia is used during labor and for vaginal and cesarean deliveries.
The most common complication of epidural anesthesia is low blood pressure in the mother. Because of this, most women need to have an intravenous infusion of fluids before epidural anesthesia is given. Another risk of epidural anesthesia is a postpartum headache. It may develop if the epidural needle enters the spinal canal rather than staying in the space surrounding the canal. Your anesthesiologist will discuss the risks, benefits and alternatives to this method of pain management.
-
Epidural analgesia.
 This is sometimes called a walking epidural because the medication infused through the epidural is an analgesic. While it does help relieve pain, it does not numb your body or prohibit movement. Combinations of medications may be used in this type of epidural to provide both analgesic and anesthetic effects. This type of epidural may be used to relieve pain during labor and vaginal deliveries.
This is sometimes called a walking epidural because the medication infused through the epidural is an analgesic. While it does help relieve pain, it does not numb your body or prohibit movement. Combinations of medications may be used in this type of epidural to provide both analgesic and anesthetic effects. This type of epidural may be used to relieve pain during labor and vaginal deliveries.Similar to epidural anesthesia, the most common complication of epidural analgesia is low blood pressure in the mother. Another risk of epidural analgesia is a postpartum headache caused by the epidural needle entering the spinal canal.
-
Spinal anesthesia. This type of anesthesia involves injecting a single dose of the anesthetic agent directly into your spinal fluid. Spinal anesthesia acts very quickly and causes complete loss of sensation and loss of movement in your lower body. This type of anesthesia is often used for cesarean deliveries.

-
Spinal analgesia. This involves injecting an analgesic medication into the spinal fluid to provide pain relief without numbing. Spinal analgesia may be used in combination with epidural anesthesia or analgesia to provide pain relief during labor or after delivery.
-
General anesthesia. Often used in emergency cesarean deliveries, this type of pain relief involves administering an anesthetic agent that causes you to go to sleep.
Pregnancy and childbirth \ Acts, samples, forms, contracts \ Consultant Plus
- Main
- Legal resources
- Collections
- Pregnancy and childbirth
This resource contains collections of the most important and relevant documents on various topics. Here you will find regulations, articles and expert advice, forms of documents on topics of interest to you:
113-rz Komi benefits
12 weeks of pregnancy
Abortion
Act of the form of Wu-25
Apostille Certificate
Certificate of civil servants Pregnant women
Pregnant on the Labor Exchange
Pregnant, pregnant woman refuses to transfer
Pregnancy Pregnancy MASTRICALS PENTERS Free medicines for pregnant women
Sick leave for stillbirth
In what cases can a pregnant woman be fired
In what case is a certificate of birth of a child issued form 4
Veterinary certificate form 4
Amendments to the birth certificate
Intrahepatic cholestasis during pregnancy
Reinstatement of a pregnant woman upon dismissal at her own request
9001 Medical conclusion pregnant woman to another jobTemporary transfer of a pregnant woman
Temporary transfer of a pregnant woman to light work
Temporary transfer to light work
Issuance of veterinary certificate
Issue of a certificate in proactive mode
Payments to unemployed
Pregnant women women upon dismissal
Guarantees for pregnant women upon liquidation
Guarantees for pregnant women upon liquidation of an organization
Documents for transfer to light work
Documents for obtaining a mother's certificate
Documents confirming pregnancy
Supplement up to average earnings when transferring to light work
Supplement to average light work
Supplementary agreement on transfer to light work
Supplementary agreement on the extension of a fixed-term employment contract due to pregnancy
Is it allowed to use the labor of pregnant women in jobs related to a computer
income on the generic certificates of KOSGU
Monthly cash payment to provide a full -fledged meals for pregnant women
Law on surrogate maternity
Fested pregnancy
Filling out the sick leave
Bulletproof banks
Preservation
certificates of pregnancy
Application of a pregnant woman for part-time work
Application for medical examination of a pregnant woman
Application for light work due to pregnancy
Application for a second birth certificate
Application for transfer of a pregnant woman
Application for transfer to remote work due to pregnancy
Application for transfer to light work
the fact of birth registration
Application form 25
Abuse of the right of a pregnant woman
Changes in birth certificate
Artificial termination of pregnancy
Probationary period for pregnant women
How to pay benefits for the burial of a stillborn child
How pregnant women are paid for the day of visiting a doctor
How to pay for self-isolation for pregnant women
How to apply for easy labor for pregnant women
How to arrange a visit to the doctor for pregnant women
How to transfer a pregnant woman to light work
How to calculate the average earnings of a pregnant employee transferred to light work
When can a pregnant woman be fired
Business trips for pregnant women
Commentary on article 113 of the Labor Code of the Russian Federation
Who is paid financial assistance upon the birth of a child
Laminated birth certificate
pregnant concept
Light work for minors
Light work for medical reasons
Light labor of the Labor Code of the Russian Federation
Financial assistance for the birth of a dead child
Financial assistance for the birth of a child
Financial assistance for the birth of a child 2020
Financial assistance for the birth of a child in the RSV
Financial assistance for the birth of a child deduction
deductible at the birth of a child documentsFinancial assistance at the birth of a child to each parent
Financial assistance at the birth of a child personal income tax code
Financial assistance at the birth of a child Income tax
Financial assistance at the birth of a child Personal income tax
Financial assistance at the birth of a child Personal income tax and insurance premiums
Financial assistance at the birth of a child is not subject to personal income tax
Financial assistance at the birth of a child is reflected in 90 in Rs3
Financial assistance at the birth of a child postings
Financial assistance at the birth of a child insurance premiums
Financial assistance at the birth of a child accounting
Maternity capital surrogate mother
Medical termination of pregnancy
Medical report of a pregnant woman on transfer to another job
Can a pregnant woman establish part-time work
Is it possible to change the working conditions of a pregnant woman
Can a pregnant woman be refused a job 9013 9013 Is it possible to lay off a pregnant employee
Is it possible to dismiss a pregnant woman from a temporary position
Is it possible to dismiss a pregnant woman on probation
Is it possible to dismiss the pregnant woman under Article
Moatorial for issuing a specialist certificate
Moatorial for issuing certificates
Moratorial for certificates
Charges of material assistance at the birth of a child
POPL MATPOMENT AT THE BREADING DIARE
9001 NDFLS with materialPersonal income tax from certificates
Cannot be transferred to light work
Illegal termination of pregnancy
Illegal abortion
Non-preferential certificate
No easy work for a pregnant woman. What to do
What to do
new forms from 11.11.2020
Certificate Nominal
Normal pregnancy
The time of visiting the doctor
Pregnant work for pregnant women
Mandatory dispensary of the pregnant woman
Limit on the computer
restrictions in the work pregnant
Restrictions on working at a computer for a pregnant woman
Single mother certificate 25
Payment for sick leave for pregnancy and childbirth
Payment for the average pregnant woman upon suspension
Payment for birth certificate coupons
Paid hours for pregnant women to visit a doctor on leave
night work for pregnant women
Grounds for transfer to light work
Grounds for transfer of a pregnant woman to light work
Responsibility for the dismissal of a pregnant woman
Responsibility under a surrogacy contract
Refusal of a pregnant woman from transfer to light work
Refusal to transfer to light work
Maternity leave surrogate motherhood
Suspension due to pregnancy of a pregnant woman
Suspension of a pregnant woman from work due to coronavirus
Suspension of a pregnant woman report card
Absence of a pregnant woman at work
Registration of easy work for a pregnant woman
Labor protection of pregnant women
Transfer of a pregnant woman to remote work
Transfer of a pregnant woman for medical reasons
Transfer to lighter work due to pregnancy
Transfer to a difficult job SUPPLEMENTARY AGREEMENT
Transfer to light work for a pregnant woman Application
Transfer to light work for medical reasons
Translation to light work after operation
Form Form 25
Obtaining housing certificate
Obtaining a birth certificate
Number to the dismissal of a pregnant woman
The concept of maximum labor certificates
pregnancy
Procedure for spending money on birth certificates
Visiting a doctor by a pregnant woman during working hours
Visiting a home arrest
A manual for burial of a stillborn baby
Pressure allowance 2021
Useful Greetings
Guide to a student
Giving birth to a dead child
registration registration
SPU maternity
Provision of light labor for pregnant women
Termination of pregnancy
Termination of pregnancy for medical reasons
Termination of pregnancy for social reasons
When undergoing a mandatory dispensary examination in medical organizations, pregnant women retain their average earnings at their place of work.
Employment of pregnant women
Employment of pregnant women on days off
Employment of pregnant women on weekends and holidays
Employment of pregnant women
Acknowledgment of paternity in surrogacy
Order on the payment of financial assistance in connection with the birth of a child
Order on the transfer to light work of a pregnant woman
Order on the extension of a fixed-term employment contract with a pregnant woman
Acquisition of certificates of kosgu
Problems of surrogacy
Verification of birth certificates
Extension of medical certificates
Extension of a fixed-term employment contract until the end of pregnancy
Extension of a fixed-term employment contract until the end of maternity leave
Extension of a fixed-term employment contract with a pregnant woman
Prevention of abortions
Medical examination for pregnant women
Work of a pregnant woman in shift work
Work of pregnant women in remote mode 9012
Work of pregnant women at a computer
Work at a computer of pregnant women
Part-time work of pregnant women
The employee brought a certificate for light work
The employee brought a certificate of transfer to light work
Distribution of funds according to maternity certificates
Termination of a fixed-term employment contract with a pregnant woman
Termination of a fixed-term employment contract with an employee on maternity leave
Expense means of birth certificatesRegistration of a stillborn child
Registration of a newborn
Registration of a child born by a surrogate mother
Certificate registry office Form 4
Help for a pregnant woman
Certificate to transfer to light work
Certificate to transfer to a pregnant woman
Certificate of visiting a doctor
Giving birth certificate
Giving birth to a dead child
22222 Birth certificate form
Birth certificate form 2
Birth certificate form 24
Birth certificate form 3
Certificate form 25
Funds of generic certificates
Final employment contract Pregnancy
Final employment contract for the duration of the Decree Sample
Article 56. Artificial termination of pregnancy
Artificial termination of pregnancy
Cost of the birth certificate
Surroganic motherhood, Lonely Material Materials Lonely Materials Lonely Mother of Surrogate Materials Lonely Mother Coupons of birth certificates
Labor Code of the Russian Federation guarantees for pregnant women
Notification of a pregnant woman about the expiration of the employment contract
The dismissal of the pregnant director
Disruption of the pregnant woman Disciplinary sanction
Dismissal of the pregnant woman
The dismissal of a pregnant woman upon liquidation of an individual entrepreneur
The dismissal of the pregnant woman for theft
The dismissal of the pregnant woman
The dismissal of the pregnant woman as not passed the test of the testing period as not passed the test of the testing period on probation
Dismissal of a pregnant woman at the end of the contract
The dismissal of the pregnant woman at his own request
The dismissal of the pregnant woman by agreement of the parties
The dismissal of the pregnant woman upon liquidation of the organization
The dismissal of the pregnant woman adopted under an urgent employment contract
The dismissal of the pregnant woman
The dismissal of the pregnant woman from the time rate
from the civil serviceDismissal of pregnant women
Withholding personal income tax from material assistance for the birth of a child
Deductions from material assistance at the birth of a child
Working conditions for pregnant women
Ownership of a birth certificate
Form 24-FSS
Form VU-25
Form 9 of a medical report on transfer to light work
FormPregnancy certificate form
Citizenship stamp on birth certificate
- "Hot" documents
- Codes and most requested laws
- Legislative Reviews
- Federal law
- Regional legislation
- Draft legal acts and legislative activities
- Other reviews
- Reference information, calendars, forms
- Calendars
- Forms of documents
- Helpful Hints
- Financial advice
- Journals of the publishing house "Glavnaya kniga"
- Internet interview
- Classics of Russian law
- Useful links and online services
- Subscribe to newsletters
- News informer ConsultantPlus
- News RSS feeds
- Export of materials
- Documents
- Collections
Pregnancy in questions and answers - Useful articles
What to expect? How to eat? How to deal with difficulties? How to do everything right? These and many questions will be answered by Irina Alexandrovna Soleeva, an obstetrician-gynecologist at the Sadko clinic.
- How is due date calculated?
From the first day of the last menstruation. To determine the due date, 280 days are added to the first day of the last menstruation, i.e. 10 obstetric, or 9 calendar months.
Usually, the calculation of the due date is simpler: from the date of the first day of the last menstruation, count back 3 calendar months and add 7 days. So, if the last menstruation began on October 2, then, counting back 3 months (September 2, August 2 and July 2) and adding 7 days, determine the expected date of birth - 9July; if the last menstruation began on May 20, then the expected due date is February 27, etc.
Expected due date can be calculated by ovulation: 14-16 days are counted back from the first day of the expected but not arrived menstruation and 273-274 days are added to the found date.
- And if you know the exact date of conception, how many days to add?
A large-scale study was conducted with a large number of pregnant women, according to various indicators, the gestational age and, accordingly, the date of birth were determined. It turned out that the woman most often remembers the date of the last menstruation. And from this fixed date, as the study showed, childbirth occurs at the 40th week ± a couple of weeks. Obstetrician-gynecologists are guided precisely by this system of calculations.
It turned out that the woman most often remembers the date of the last menstruation. And from this fixed date, as the study showed, childbirth occurs at the 40th week ± a couple of weeks. Obstetrician-gynecologists are guided precisely by this system of calculations.
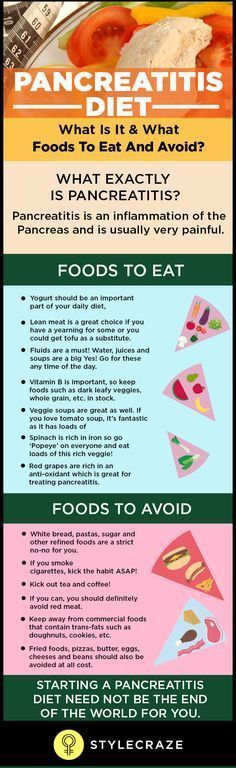
- Should I change my diet, if so, how?
4 meals a day are recommended in the first half of pregnancy, 5-6 meals a day in the second. It is better to eat often, but little by little. For healthy women, there are no forbidden foods (except alcoholic beverages), only more or less preferred ones.
So, the body absorbs easily digestible milk fats and vegetable oils better. The latter are not only a source of essential linoleic acid, but also vitamin E, which has a positive effect on the course of pregnancy.
To eliminate constipation, it is worth enriching the diet with sources of dietary fiber (fiber, pectins) - vegetables and fruits, buckwheat and oatmeal.
In the second half of pregnancy, sugar, confectionery and flour products, rice should be eaten in very small quantities. Do not get carried away with fried, spicy, salty foods, because. during this period, the liver and kidneys of a pregnant woman function with tension. It is better to prefer boiled and steamed dishes.
Do not get carried away with fried, spicy, salty foods, because. during this period, the liver and kidneys of a pregnant woman function with tension. It is better to prefer boiled and steamed dishes.
The main thing is to include in your diet a variety of foods: vegetables, fruits, juices - and you will provide yourself and your unborn child with everything necessary for normal development.
- I really want olives, but they are canned. Can?
It depends on the gestational age. After 20 weeks, I would not recommend eating too salty foods, including olives. And in general, any canned food is not the most suitable food for a pregnant woman. Although olives, in themselves, the product is very useful. Therefore, within reasonable limits, say, a jar can be eaten in two days.
- And the grapes?
Grapes are very well digestible. It's fructose. It is immediately absorbed and quickly raises blood sugar. But if you are overweight, it is either not recommended at all, or it is allowed in small quantities. It is allowed to eat a small brush, or you can treat yourself to something else.
It is allowed to eat a small brush, or you can treat yourself to something else.
For some reason, it is customary for us to believe that if you are pregnant, you have to eat for three or whatever you want. As a result, pregnant women buy grapes in boxes and eat them in kilograms. Such a diet does not lead to anything good: sugar appears in the urine, blood sugar rises, babies are born large. Moreover, a large load falls not only on the mother's pancreas, but also on the child's pancreas - the baby from birth will be predisposed to being overweight.
- Is it possible to reduce excess weight during pregnancy and cleanse your body with the help of special teas?
All cleansing teas are contraindicated during pregnancy. We have drugs that improve the functions of the liver and kidneys, which have a diuretic effect. We assign everything individually. There are no special cleansing procedures during pregnancy. However, we have fasting days - here is the best cleansing procedure for you.
- Which vitamins are better to choose during pregnancy?
Now there is a huge selection of various vitamin complexes for pregnant women. Of course, they are all close to each other in composition. One or two components or the dosage of some vitamin differ. In order not to harm yourself and the baby, to achieve the maximum effect, each patient needs to select vitamins, based on the advice of her doctor, who controls the course of pregnancy.
- How long should I take them?
Do not take multivitamin preparations continuously. The necessary course can be selected only by a doctor, taking into account the state of your body. We have different periods when it is better to stop taking vitamins altogether. In certain weather seasons, when there is enough sun, fresh vegetables and fruits, there is no need to take vitamin complexes.
- Can I continue playing sports?
Not only possible, but necessary. From the first months of pregnancy. They will help to maintain good physical shape, and this will definitely help during childbirth, relieve excessive tension and improve mood. The main thing that you should not forget is that the training program should be specially adapted for pregnant women and should be carried out under the supervision of a doctor or an experienced instructor.
From the first months of pregnancy. They will help to maintain good physical shape, and this will definitely help during childbirth, relieve excessive tension and improve mood. The main thing that you should not forget is that the training program should be specially adapted for pregnant women and should be carried out under the supervision of a doctor or an experienced instructor.
- Do I really have to push in prenatal classes? Will not diligence create the danger of premature birth?
No, there is no danger in this exercise. If there is anything to beware of, it is cycling, horseback riding, roller skating - all sports with an increased risk of injury.
- Can I take a contrast shower?
If a woman used this procedure before pregnancy. But during pregnancy, the water should not be too hot. By the way, hot baths and a bath should also be excluded.
- Can I continue to have sex while pregnant?
Each couple decides for themselves. If it gives pleasure to both, if the woman is comfortable, then you can keep your sex life almost until childbirth. Of course, too active sex will have to be excluded, and completely stopped 2-3 weeks before the birth: too vigorous sexual intercourse: it can provoke premature birth.
If it gives pleasure to both, if the woman is comfortable, then you can keep your sex life almost until childbirth. Of course, too active sex will have to be excluded, and completely stopped 2-3 weeks before the birth: too vigorous sexual intercourse: it can provoke premature birth.
If earlier it was very strict: from 30-32 weeks, sexual life stops, now sex life is excluded by the doctor only if there are any deviations. After a while, he may allow you to resume intimacy. There are cases when sexual life is excluded for all 40 weeks.
- Is it necessary to use protection during pregnancy in order not to get pregnant again?
Very funny question. If one pregnancy has already occurred, re-conception during this period can no longer occur. The need for protection is therefore eliminated.
- Can I sleep on my stomach?
On short terms it is possible. The uterus comes out of the pelvic cavity after 12-13 weeks. Before that, it is protected by the pelvic bones, which means that we will not cause any harm to the fetus.
- So, the work of the expectant mother. Is it worth revising your working day, taking into account the new state?
Work during pregnancy is perfectly acceptable if there are no abnormalities. It is important to remember that pregnant women should not lift weights, work in heat and high humidity. Contact with harmful substances and prolonged standing should be avoided.
- Can motorists continue to drive?
You can drive a car if there are no contraindications from the doctor who monitors you during pregnancy. And it is not desirable in the later stages after 30 weeks, because there is a very strong load on the muscles of the pelvic floor, legs and arms work, concentration of attention is required - this is an additional stressful situation for your body. And of course, do not neglect the seat belt. He will not pull your stomach, but will pass under it and under your arm obliquely.
- How to deal with the symptoms of varicose veins?
It depends on the degree of varicose veins, its severity. Despite the rich selection of various drugs for internal and local action - tablets, drops, ointments - the most effective method of struggle is, nevertheless, wearing compression underwear. By the way, those who spend most of their working time sitting at a table, or vice versa, standing on their feet, should also think about the prevention of varicose veins.
Despite the rich selection of various drugs for internal and local action - tablets, drops, ointments - the most effective method of struggle is, nevertheless, wearing compression underwear. By the way, those who spend most of their working time sitting at a table, or vice versa, standing on their feet, should also think about the prevention of varicose veins.
It is better to stop your choice on tights: an elastic band or a stocking squeezes the leg too much, and when bandaging the legs, it is difficult to determine the necessary compression.
Tights should be selected by a doctor. A phlebologist works in our clinic. He will be able to choose the desired degree of compression.
Do not be afraid that underwear will be too tight on both legs and stomach: there are special tights for pregnant women. A special insert on the stomach fits him, supporting him, without squeezing at all.
- How to be smokers: won't quitting a bad habit cause stress for the body if the smoking experience before pregnancy was quite long?
Smoking during pregnancy is very bad. This applies equally to active and passive smokers. The fetus develops chronic hypoxia - a constant lack of oxygen. And it primarily affects the development of brain structures. The result is deviations from the norm in mental development. Even if the violations are minor at first, in infancy, most likely, they will manifest themselves in kindergarten or school, when the maximum load falls on the child's intellect. It will be difficult for the baby to learn, to perceive some information.
This applies equally to active and passive smokers. The fetus develops chronic hypoxia - a constant lack of oxygen. And it primarily affects the development of brain structures. The result is deviations from the norm in mental development. Even if the violations are minor at first, in infancy, most likely, they will manifest themselves in kindergarten or school, when the maximum load falls on the child's intellect. It will be difficult for the baby to learn, to perceive some information.
Moreover, there is a growing risk of premature births, miscarriages at different stages of pregnancy. Babies are often born small.
Stories that giving up habitual smoking will become a strong stress for the body are far from the truth. Our expectant patients break this bad habit without much difficulty. Even if you regularly inhaled tobacco smoke both before and after conception, you should not think that it is still too late to quit. The harm you will do to your baby if you continue to smoke is incomparable to the reluctance to part with a cigarette.