Pregnant with spina bifida baby
Spina bifida | Pregnancy Birth and Baby
Spina bifida | Pregnancy Birth and Baby beginning of content4-minute read
Listen
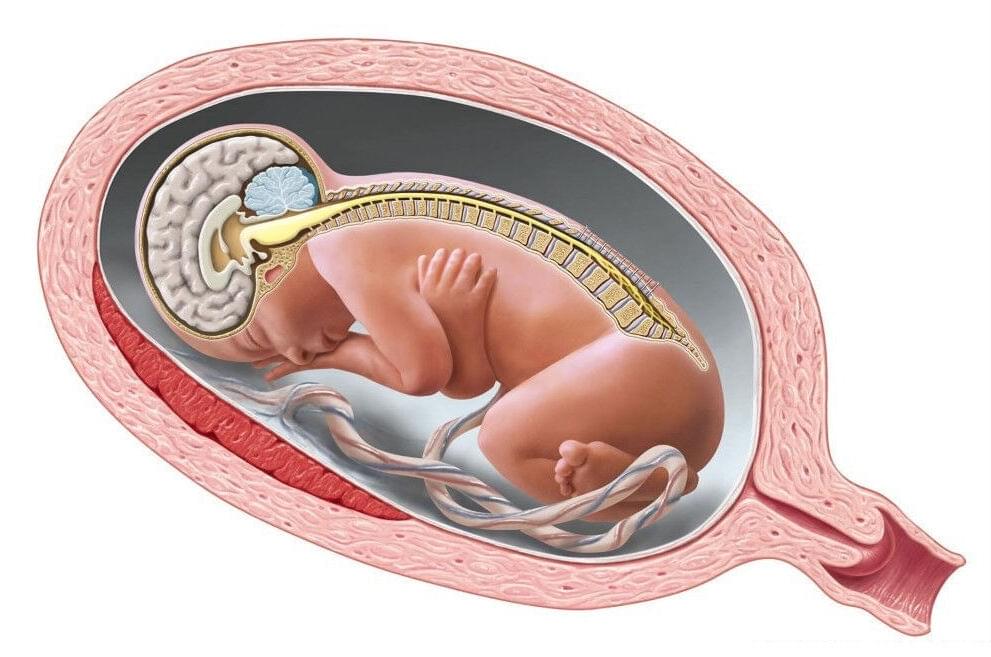
Spina bifida is a condition that affects the normal development of a baby’s spine early in pregnancy. This page provides information about spina bifida and how it might affect a baby born with the condition.
About spina bifida
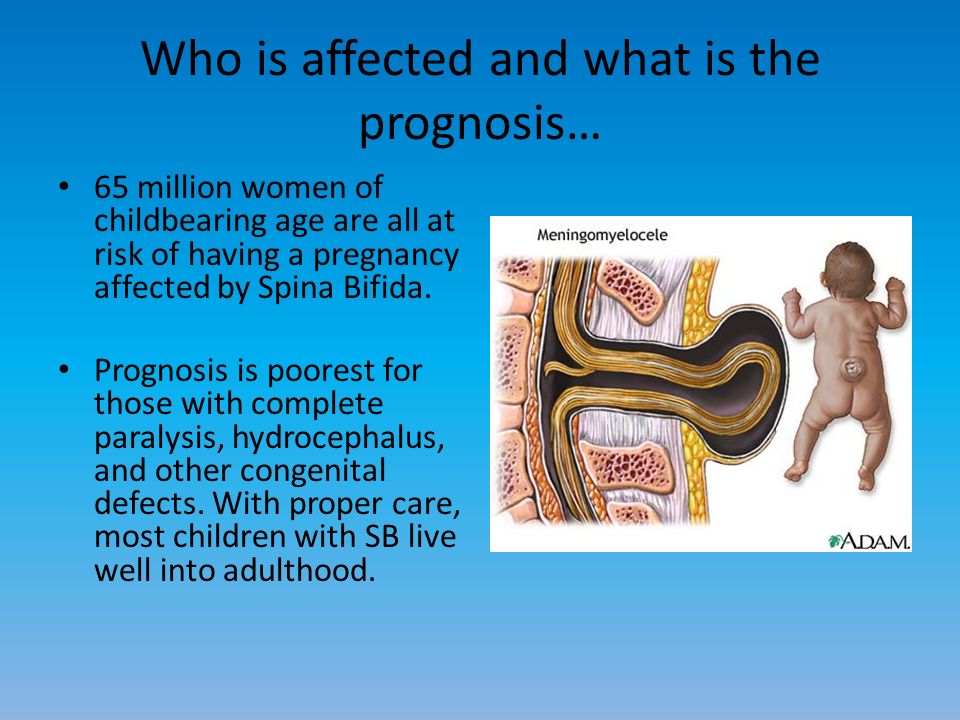
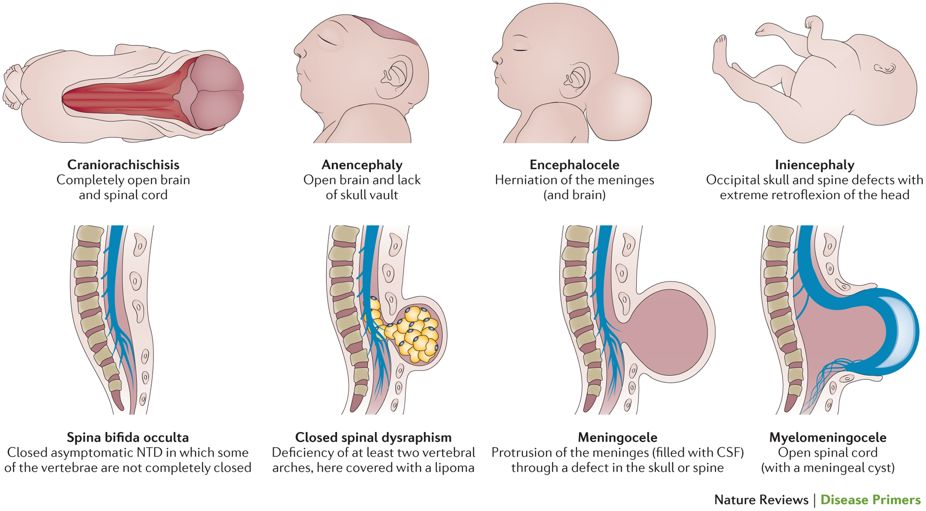
A baby’s spine and brain begin to develop from the neural tube of the embryo during the first month of pregnancy. Spina bifida occurs when the neural tube has a defect and fails to close completely, leaving a gap in the baby’s spine.
This gap can interfere with messages that pass between the body, the nerves within the spine and the brain.
Spina bifida only affects the part of the body that receives its nerve supply from the open area of the spine or below that area. It doesn’t affect the brain, heart, chest or arms.
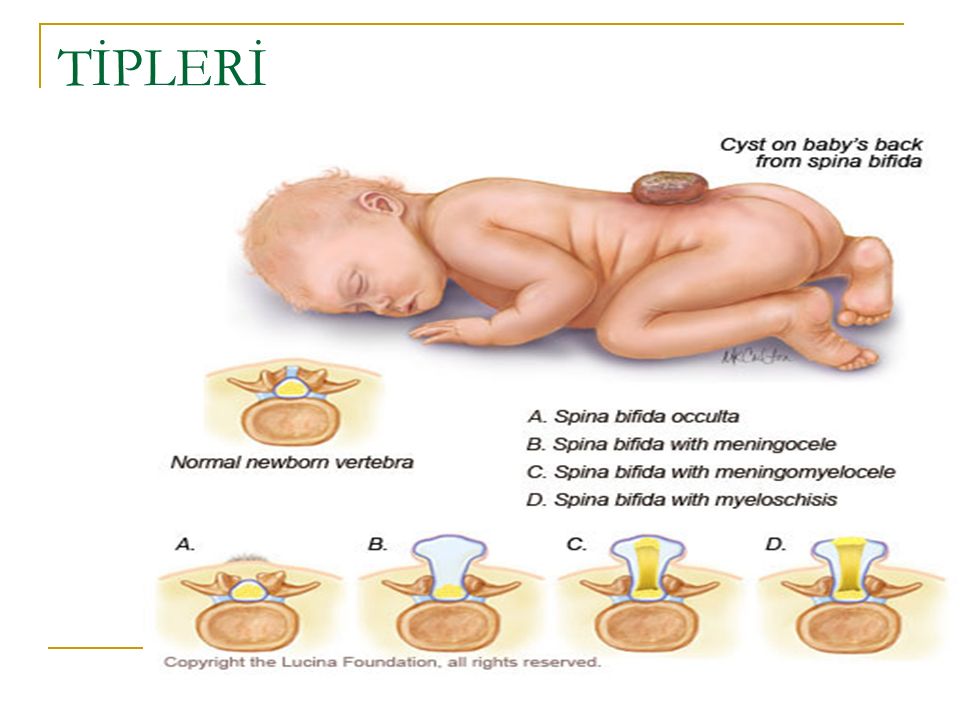
There are different types of spina bifida. The mildest form is a defect in the fusion of the bones of the spine that surround an otherwise healthy spinal cord. A person with mild spina bifida might have few or no symptoms.
In the most serious form, the spinal cord and its protective covering bulge through the gap in the baby's spine. It can lead to a number of problems with things like leg weakness and movement, sensation, bladder and bowel control and learning difficulties.
What causes spina bifida?
The cause of spina bifida is not fully understood. It appears to be a combination of genetic, environmental and nutritional factors.
Your baby is more at risk of spina bifida if your family has a history of neural tube defects. There is also greater risk if you have insulin-dependent diabetes and don't control your blood sugar well, are obese, or take certain medications such as valproate or carbamazepine. It’s important to speak to your doctor about medications if you are planning to become pregnant.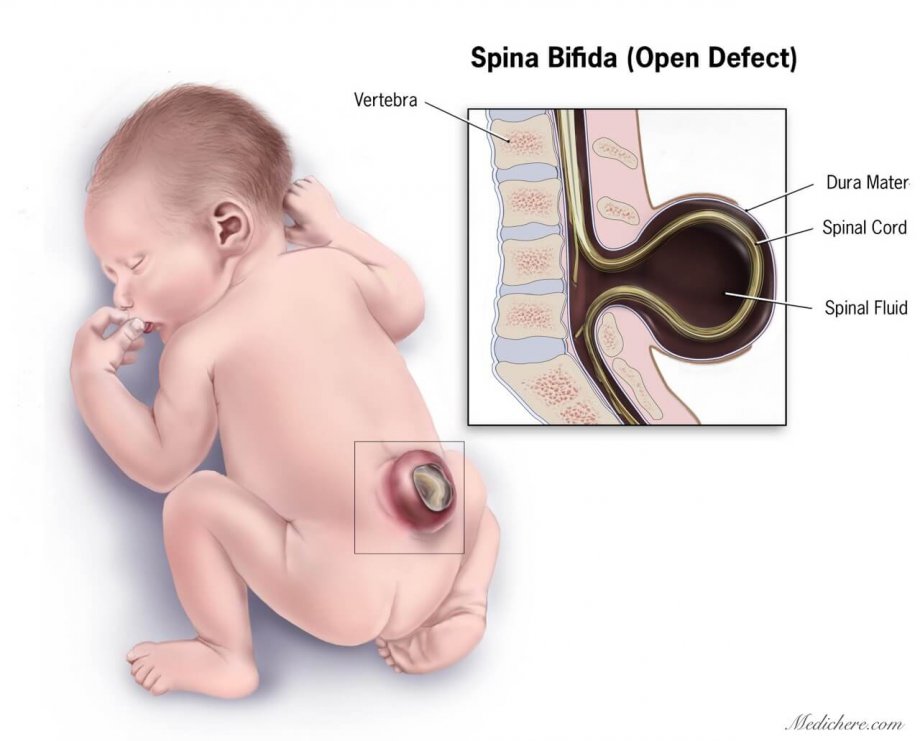
One way you can reduce the risk of your baby having spina bifida is to take a folate supplement and eat folate-rich foods if you are planning to become pregnant. You should take a folate supplement for at least 1 month before becoming pregnant and for the first 12 weeks of pregnancy.
How do I know if my baby might have spina bifida?
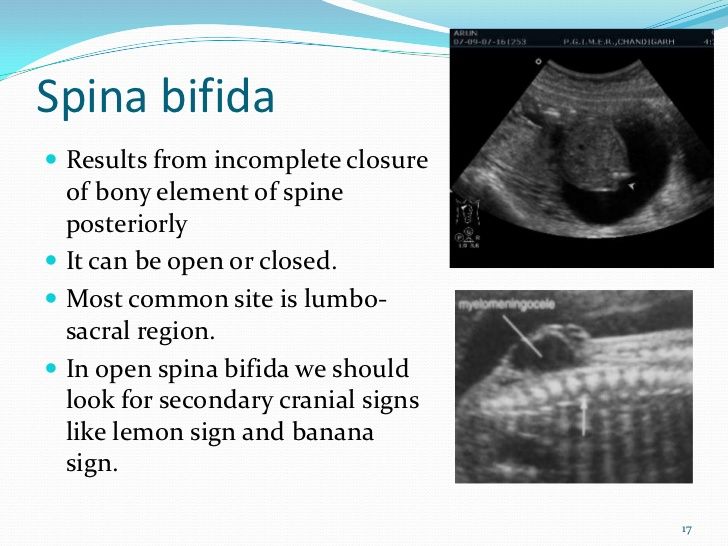
Spina bifida can be diagnosed with an ultrasound or blood test around the 16th and 18th weeks of pregnancy.
What if my baby has spina bifida?
If your baby has spina bifida, you will need to find out as much as you can about what it will mean for you and your unborn child.
Talk to your doctor about what the diagnosis means for both you and your baby. If the condition is serious enough, you might also wish to seek advice and information on whether to have the baby or to consider terminating the pregnancy. Pregnancy, Birth and Baby on 1800 882 436 can also offer advice.
You may also want to ask your doctor for a referral to a genetic counsellor who can help you understand more about the spina bifida and to plan for the future.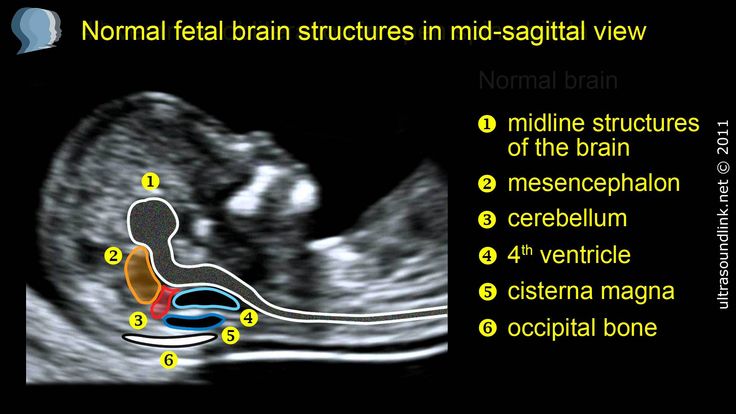
What happens when my baby is born?
Your baby will need special care at the time of birth. Medical staff will usually wrap the spinal opening with sterile dressings and plastic wrap and attach a drip to a vein in your baby’s arm to provide fluids and antibiotics. Your baby will be placed in an incubator for warmth.
If severely affected, your baby may be transferred to the hospital’s neonatal intensive care unit. If necessary, an operation can be done within the first few days to repair the spine or drain fluid from the baby’s brain.
Depending on the type of spina bifida, your baby might need continuing care from different specialists working in a hospital or your community. They might need to help your child with practical matters such as movement and learning how to go to the toilet.
What assistance is available?
If you are caring for a child with spina bifida, there are support groups in the different states. You can also get practical advice from a maternal child health nurse at Pregnancy, Birth and Baby on 1800 882 436.
The Australian Government’s Carer Gateway provides general advice and different states have support groups. Your child may qualify for support from the National Disability Insurance Scheme.
Sources:
Centre for Genetics Education, NSW Health (Fact Sheet No. 60 - Neural tube defects – spina bifida and anencephaly), Cochrane (Folic acid supplements before conception and in early pregnancy (up to 12 weeks) for the prevention of birth defects), Cochrane (Spina bifida repair and infant and maternal health), Sydney Children’s Hospitals Network (Spina bifida)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: June 2020
Back To Top
Related pages
- Disability and chronic illness
- Prenatal screening and testing
Need more information?
Spina bifida | Novita
Major effects of spina bifida Paralysis of the legs There may be complete paraplegia, or partial or minor paralysis depending on the level of the spinal injury
Read more on Novita Services website
Spina Bifida | Sydney Children's Hospitals Network
Spina Bifida comes from a latin term which means “split spine”
Read more on Sydney Children's Hospitals Network website
Hydrocephalus and Spina Bifida | Sydney Children's Hospitals Network
Many people living with Spina Bifida also have a condition called Hydrocephalus
Read more on Sydney Children's Hospitals Network website
Spina Bifida - Adolescents and adults with Spina Bifida | Sydney Children's Hospitals Network
Independence Being independent is an important life skill
Read more on Sydney Children's Hospitals Network website
Maternal screening - Pathology Tests Explained
Why and when to get tested for maternal screening
Read more on Pathology Tests Explained website
Why do you need to take folic acid when pregnant? | Queensland Health
Learn about why folic acid is important in pregnancy.
Read more on Queensland Health website
Pregnancy checkups, screenings and scans
Knowing what check-ups, screenings and scans to have and when to have them during your pregnancy is important information for every pregnant woman.
Read more on Pregnancy, Birth & Baby website
Neural tube defects: children & teens | Raising Children Network
Neural tube defects are brain and spinal cord abnormalities, including spina bifida, encephalocele and anencephaly. Read how they affect children.
Read more on raisingchildren.net.au website
Folate and pregnancy
Folate and folic acid are important for pregnancy since they can help prevent birth defects known as neural tube defects, such as spina bifida.
Read more on Pregnancy, Birth & Baby website
Sweat Chloride Test - Pathology Tests Explained
Prenatal screening provides pregnant women with the option to refine the probability of having a fetus with a common fetal chromosomal anomaly such as Down syndrome or a structural defect such as spina bifida.
Read more on Pathology Tests Explained website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.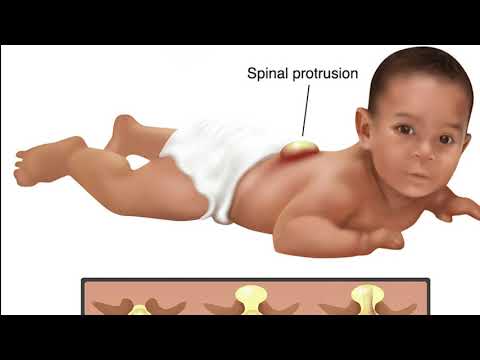
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
A Pregnant Woman with Spina Bifida: Need for a Multidisciplinary Labor Plan
Introduction
Spina bifida is caused by the failure of the neural tube to close during the first month of embryonic development. There are three main types: spina bifida occulta, meningocele, and myelomeningocele. In spina bifida occulta, the outer part of the vertebrae is not completely closed.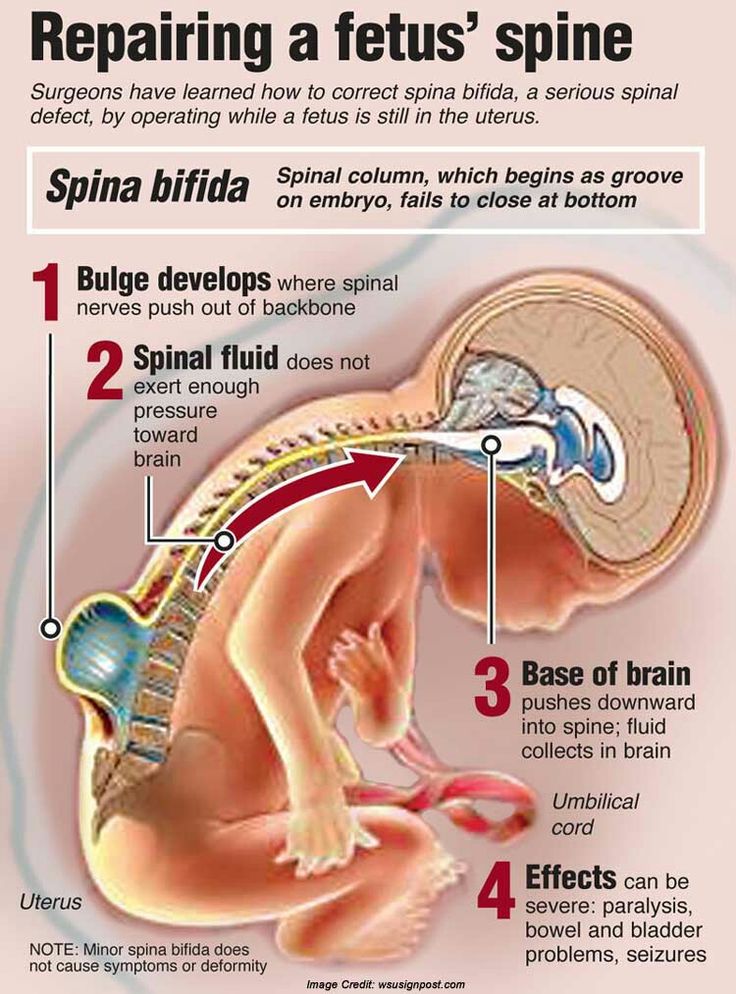 The splits in the vertebrae are so small that the spinal cord does not protrude. A meningocele involves a defect in bony closure, which allows the meninges to herniate between the vertebrae. This is a closed spinal dysraphism where the skin is intact, but the underlying spinal cord and associated structures are abnormal. In the patient presented, there was an associated lipomatous mass. Last, in individuals who have a myelomeningocele, the unfused portion of the spinal column allows the spinal cord elements to protrude through the opening. This is an open spinal dysraphism where the malformed spinal cord segment and meninges are not covered by skin.
The splits in the vertebrae are so small that the spinal cord does not protrude. A meningocele involves a defect in bony closure, which allows the meninges to herniate between the vertebrae. This is a closed spinal dysraphism where the skin is intact, but the underlying spinal cord and associated structures are abnormal. In the patient presented, there was an associated lipomatous mass. Last, in individuals who have a myelomeningocele, the unfused portion of the spinal column allows the spinal cord elements to protrude through the opening. This is an open spinal dysraphism where the malformed spinal cord segment and meninges are not covered by skin.
A tethered cord is defined as an abnormal attachment of the spinal cord to its surrounding tissues. This can occur because of abnormalities in the development in the end of the spinal cord, such as a thickened filum terminale or because of surgery for the spinal dysraphism. The radiologic diagnosis requires a low-lying conus medullaris and a thickened (more than 2 mm) filum terminale.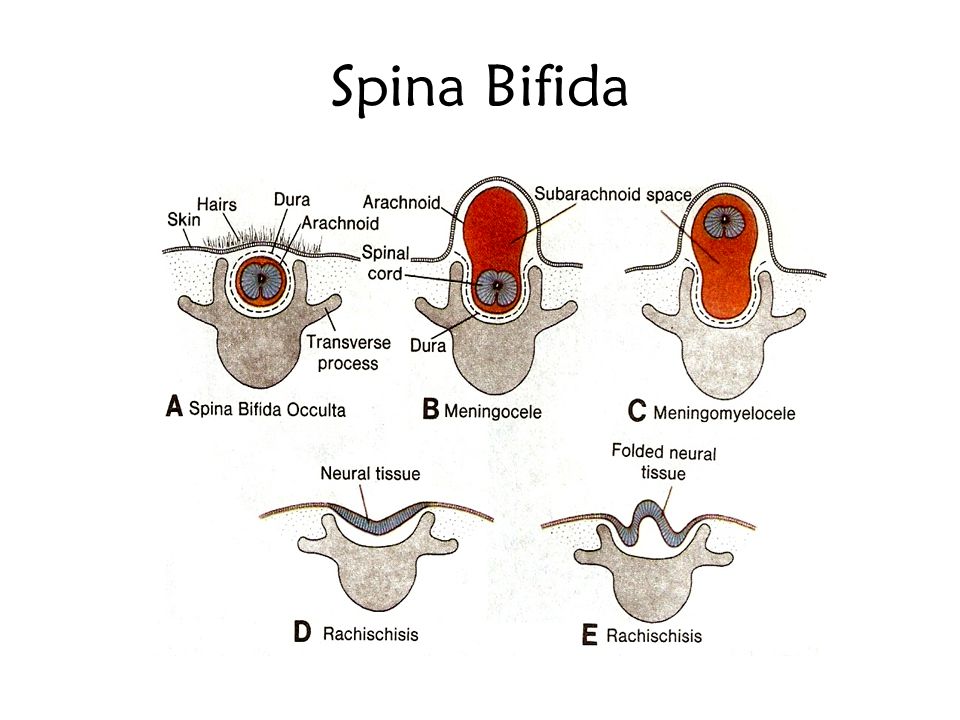 This is distinct from the tethered cord syndrome, which refers to the neurologic symptoms such patients may display. The symptoms typically may include pain, which may be worse with exercise or flexion, lower extremity weakness, and sensory loss and bladder dysfunction (1). Patients with spina bifida often have other associated anomalies of the neural tube particularly Chiari II malformations. This malformation is characterized by cerebellar hypoplasia and caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This leads to impairment of cerebrospinal fluid flow causing hydrocephalus. Chiari II malformations occur in more than 90% of infants with myelomeningocele. Other frequent anomalies include cortical dysplasias and abnormalities involving the corpus callosum and thalami (2).
This is distinct from the tethered cord syndrome, which refers to the neurologic symptoms such patients may display. The symptoms typically may include pain, which may be worse with exercise or flexion, lower extremity weakness, and sensory loss and bladder dysfunction (1). Patients with spina bifida often have other associated anomalies of the neural tube particularly Chiari II malformations. This malformation is characterized by cerebellar hypoplasia and caudal displacement of the lower brainstem into the upper cervical canal through the foramen magnum. This leads to impairment of cerebrospinal fluid flow causing hydrocephalus. Chiari II malformations occur in more than 90% of infants with myelomeningocele. Other frequent anomalies include cortical dysplasias and abnormalities involving the corpus callosum and thalami (2).
Case
A 34-year-old lady G1 P0, 35 weeks pregnant who had a history of surgery for spina bifida and a tethered cord was sent for neurologic evaluation to define both obstetric risks and safety of neuraxial anesthesia.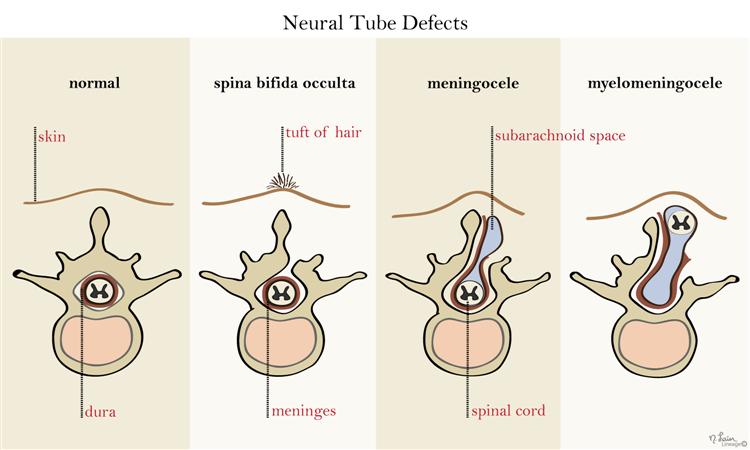 She had a lipomeningocele operated on at 3 months of age. At age 10, she developed a tethered cord syndrome, which required surgery. Unfortunately, due to progressive neurologic symptoms, she required a second untethering procedure. Her neurologic impairments included weakness in legs, distal more than proximal, distal lower extremity numbness, and urinary incontinence. She required braces and crutches to walk and needed to self-catheterize.
She had a lipomeningocele operated on at 3 months of age. At age 10, she developed a tethered cord syndrome, which required surgery. Unfortunately, due to progressive neurologic symptoms, she required a second untethering procedure. Her neurologic impairments included weakness in legs, distal more than proximal, distal lower extremity numbness, and urinary incontinence. She required braces and crutches to walk and needed to self-catheterize.
Pertinent Findings on Neurologic Examination
Her right leg was shorter than the left with a smaller right foot. She had bilateral pes cavus deformities and hammer toes. Lower extremity strength: 4/5 hip flexors on the left, 4-/5 on the right, full hip adductors, abductors were 4/5 bilaterally. She had full knee flexion and extension strength. She has no movement of either foot with distal atrophy. Reflexes: 1+ right knee jerk, no left knee jerk, absent ankle jerks. Toes were mute. Sensation showed diminished pinprick right greater than left in an L5-S1 distribution.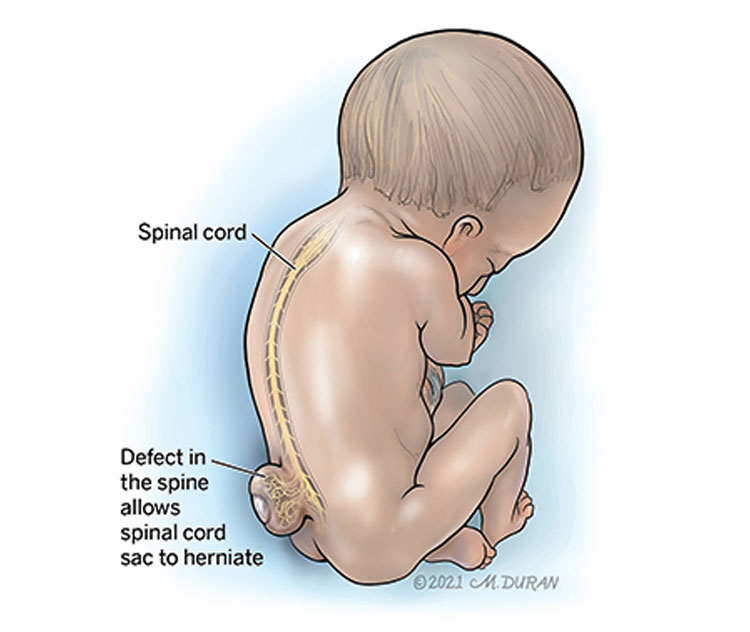 She could transfer from her wheelchair.
She could transfer from her wheelchair.
Lumbar MRI showed cord dysraphism from L4-L5 with a lipomeningocele. There were surgical changes at L3-L5. Neural elements were present to the sacrum. See Figure 1; obstetrical anesthesia was also consulted. After review of her imaging and joint consultation, the patient was offered epidural anesthesia with the plan to perform the procedure above the level of her previous surgeries. It was explained that due to her prior surgeries that the block might not be as effective and technically difficult. In addition, she understood that it was likely given her significant lower extremity weakness that she would require a caesarian delivery.
Figure 1. Axial and sagittal T2 lumbar MRI showing postsurgical changes from L3-L5 with neural elements present to the sacrum with an associated syrinx.
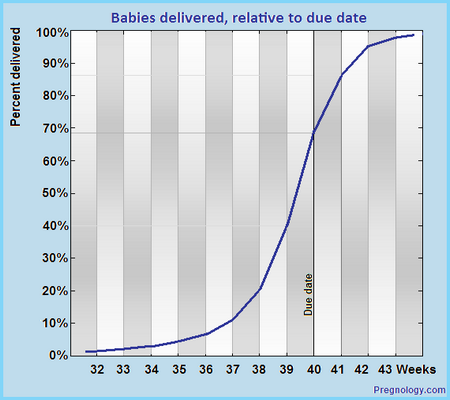
She presented at 39 weeks in labor. Epidural anesthesia was successfully placed at T12-L1 using ultrasound guidance. Due to failure to progress, the patient had a caesarian delivery. The epidural anesthesia provided good analgesia. A healthy baby girl was delivered.
The epidural anesthesia provided good analgesia. A healthy baby girl was delivered.
Discussion
Obstetric Concerns
Fertility is felt to be normal in these women. However, there are no studies looking at fertility in this group of women specifically, so the best information is that extrapolated from studies of women with spinal cord injury (3). In one series of 17 women (14 had a myelomeningocele, 3 had a meningocele), antenatal complications occurred in 14/17 patients. Antenatal admissions were less frequent in women who could ambulate independently as compared with those who were wheelchair dependent. The most frequent complications related to spinal bifida include urinary tract infections, stoma complications, decubitus ulcers, and worsening back pain. Severe thoracic scoliosis in the setting of pregnancy can contribute to restrictive lung disease. Many of these women may have undergone urologic procedures to improve their bladder function. This may complicate performing a caesarian delivery due to the abnormal and complex anatomy.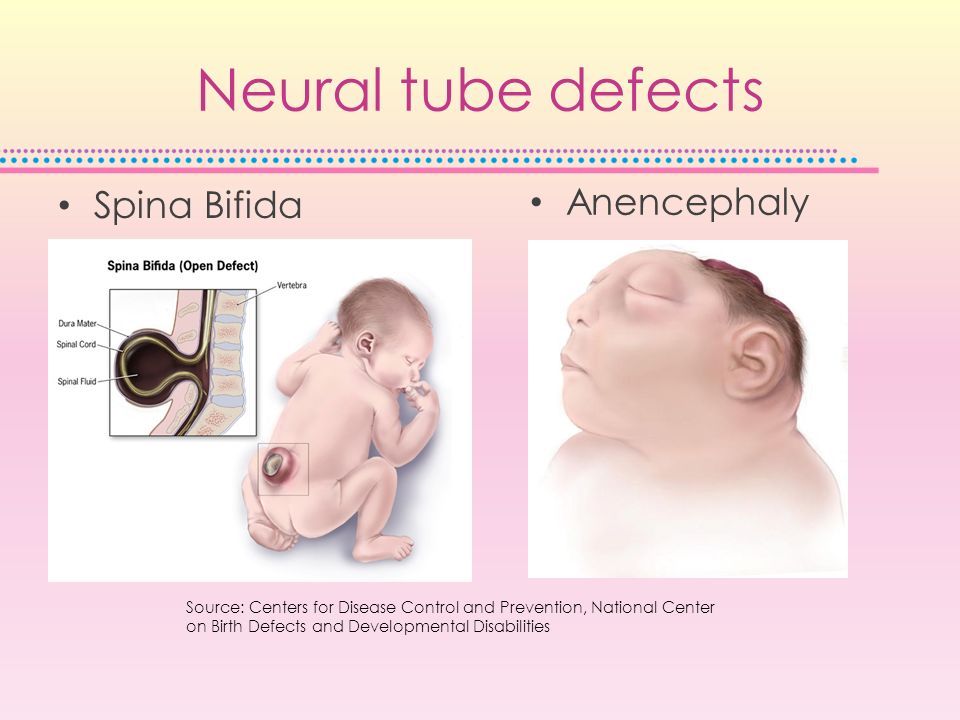 These women also had obstetric complications with a higher frequency of hypertension and preeclampsia. Nearly half of these women required caesarian delivery; this was especially common in women who were wheelchair dependent (4).
These women also had obstetric complications with a higher frequency of hypertension and preeclampsia. Nearly half of these women required caesarian delivery; this was especially common in women who were wheelchair dependent (4).
Neuraxial Anesthesia
There are several case reports in the literature of using epidural or combined spinal and epidural anesthesia in women who had prior surgery for their spina bifida. The complications encountered are related to the altered anatomy. These include difficulty locating the epidural space, an asymmetric block likely related to scarring, dural punctures, and the need for multiple operator attempts to place the anesthesia (5). However, reports of permanent neurologic injury after neuraxial anesthesia in such patients are rare (6).
Following surgery in patients, like the one presented, the epidural space is not going to be normal. In addition, even after a detethering procedure, the conus medullaris will likely still be in an abnormally low position (as in our patient).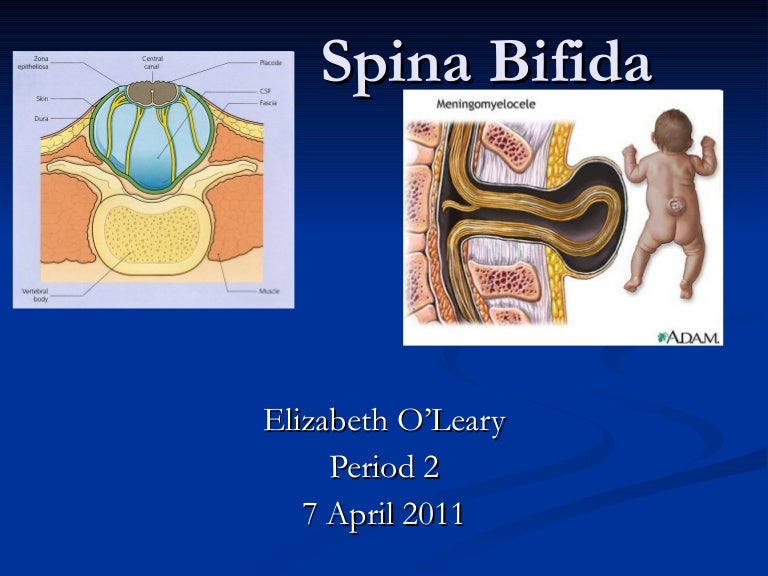 Scoliosis with or without associated corrective surgery can further complicate the spine anatomy. These factors make the ability to perform a safe and efficacious block difficult. Careful analysis of such a patient requires a careful pre-labor analgesic plan. The plan should include a detailed neurologic exam to establish baseline motor and sensory deficits as well as an obstetrical anesthesia consult. The consultants should then discuss the best patient care algorithm.
Scoliosis with or without associated corrective surgery can further complicate the spine anatomy. These factors make the ability to perform a safe and efficacious block difficult. Careful analysis of such a patient requires a careful pre-labor analgesic plan. The plan should include a detailed neurologic exam to establish baseline motor and sensory deficits as well as an obstetrical anesthesia consult. The consultants should then discuss the best patient care algorithm.
Imaging is important to look at the anatomy in detail, to locate the best level for neuraxial anesthesia. The most appropriate imaging modality is lumbar magnetic resonance imaging. The level where the cord is not too posteriorly located and the epidural space is likely to be normal is the area where a block should be attempted. Finally, a backup analgesic plan should be formulated in case the block is incomplete or unsuccessful.
Conclusion
1. Women with spina bifida have an increased risk of obstetric complications.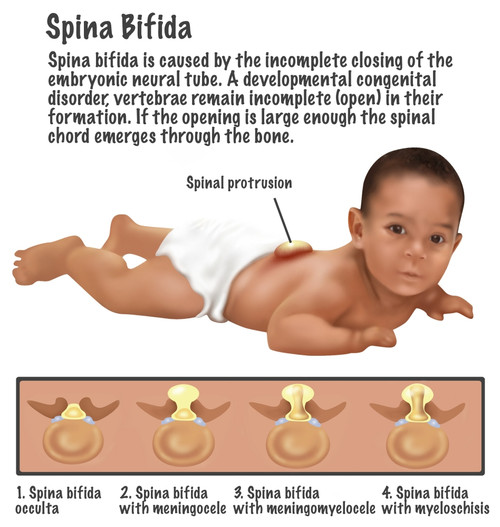 The inability to ambulate is highly correlated with the need for a caesarian delivery.
The inability to ambulate is highly correlated with the need for a caesarian delivery.
2. Neuraxial anesthesia can be performed safely and effectively in women with spina bifida.
3. Consultations with neurology and obstetric anesthesia should occur to document a baseline neurologic exam and coordinate an appropriate pre-labor analgesic plan.
Ethics Statement
Written informed consent was obtained from the patient for the publication of this case report.
Author Contributions
The author confirms being the sole contributor of this work and approved it for publication.
Conflict of Interest Statement
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Agaralla PK, Dunn IF, Scot RM, Smith ER. Tethered cord syndrome. Neurosurg Clin N Am (2007) 18:1–547.
Google Scholar
2. Gilbert JN, Jones KL, Rorke LB, Chernoff GF, James HE.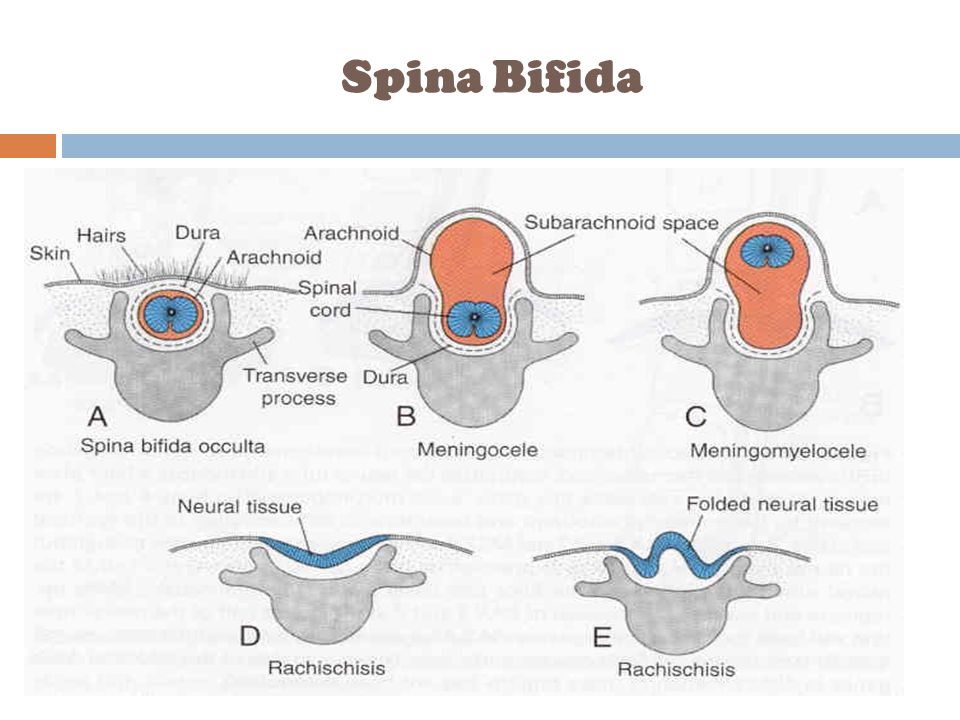 Central nervous system anomalies associated with meningomyelocele, hydrocephalus, and the Arnold-Chiari malformation: reappraisal of theories regarding the pathogenesis of posterior neural tube closure defects. Neurosurgery (1986) 18(5):559–64. doi:10.1097/00006123-198605000-00008
Central nervous system anomalies associated with meningomyelocele, hydrocephalus, and the Arnold-Chiari malformation: reappraisal of theories regarding the pathogenesis of posterior neural tube closure defects. Neurosurgery (1986) 18(5):559–64. doi:10.1097/00006123-198605000-00008
PubMed Abstract | CrossRef Full Text | Google Scholar
3. Jackson AB, Mott PK. Reproductive health care for women with spina bifida. Sci World J (2007) 7:1875–83. doi:10.1100/tsw.2007.304
CrossRef Full Text | Google Scholar
4. Arata M, Grover S, Dunne K, Bryan D. Pregnancy outcome and complications in women with spina bifida. J Reprod Med (2000) 43(9):743–8.
PubMed Abstract | Google Scholar
5. Murphy CJ, Stanley E, Kavanagh E, Lenane PE, McCaul CL. Spinal dysraphisms in the parturient: implications for perioperative anaesthetic care and labour analgesia. Int J Obstet Anesth (2015) 24:252–63. doi:10.1016/j.ijoa.2015.04.002
PubMed Abstract | CrossRef Full Text | Google Scholar
6. Hebl JR, Horlocker TT, Schroeder DR. Neuraxial anesthesia and analgesia in patients with preexisting central nervous system disorders. Anesth Analg (2006) 103(1):223–8. doi:10.1213/01.ane.0000220896.56427.53
Hebl JR, Horlocker TT, Schroeder DR. Neuraxial anesthesia and analgesia in patients with preexisting central nervous system disorders. Anesth Analg (2006) 103(1):223–8. doi:10.1213/01.ane.0000220896.56427.53
PubMed Abstract | CrossRef Full Text | Google Scholar
Fetal spina bifida - symptoms, causes, who treats
What should be done to diagnose the causes of spina bifida in a fetus? To solve this problem, the first step for the patient is to make an appointment with an obstetrician-gynecologist.
After the initial examination, the doctor may prescribe additional examinations using:
- ultrasound
- ultrasound brain scan
- computed tomography of the brain or magnetic resonance imaging of the brain
- bladder ultrasound
- ultrasound scan of the kidneys.
Spina bifida is a birth defect in which the baby's spine and spinal cord do not develop properly in the womb, causing damage to the integrity of the spinal column. This pathology of the spine is a type of neural tube defect - the structure that eventually transforms into the brain and spinal cord. The neural tube begins to form early in pregnancy and closes about 4 weeks after conception. In spina bifida, part of the neural tube does not develop or close, resulting in defects in the spinal cord and vertebrae. nine0011
This pathology of the spine is a type of neural tube defect - the structure that eventually transforms into the brain and spinal cord. The neural tube begins to form early in pregnancy and closes about 4 weeks after conception. In spina bifida, part of the neural tube does not develop or close, resulting in defects in the spinal cord and vertebrae. nine0011
Causes of spina bifida
The exact cause of spina bifida is not known, but a number of factors can increase a child's risk of developing the condition.
Folic Acid Deficiency
Folic acid (also known as vitamin B9) is found naturally in certain foods such as broccoli, peas, brown rice, and breakfast cereals. All pregnant women, as well as those planning a pregnancy, are recommended to take a mandatory folic acid preparation. It is estimated that taking this vitamin before conception and during pregnancy can prevent up to 7 out of 10 neural tube defects. It is not clear how folic acid helps reduce the risk of spina bifida, but it is likely necessary for important biochemical reactions in the body. nine0011
nine0011
Family history
The presence of neural tube defects in close relatives increases the chances of having a child with a spinal fissure. Also, if parents previously had a child with this defect, the chances of having other sick children also increase.
Medical factors
Taking certain medications during pregnancy is associated with an increased risk of having a baby with a spina bifida or other birth defects. Valproate and carbamazepine are the drugs most commonly associated with spina bifida. They are often used to treat epilepsy and certain mental illnesses such as bipolar disorder. Doctors will try to avoid prescribing these drugs if there is a possibility that a woman may become pregnant while taking them, but they may still be needed if other alternative methods are ineffective. In this case, the specialist will reduce the dose and prescribe folic acid supplements in a large dose. nine0011
Genetic factors
It is very common for a child to have spina bifida in combination with certain genetic diseases such as Patau syndrome, Edwards syndrome or Down syndrome.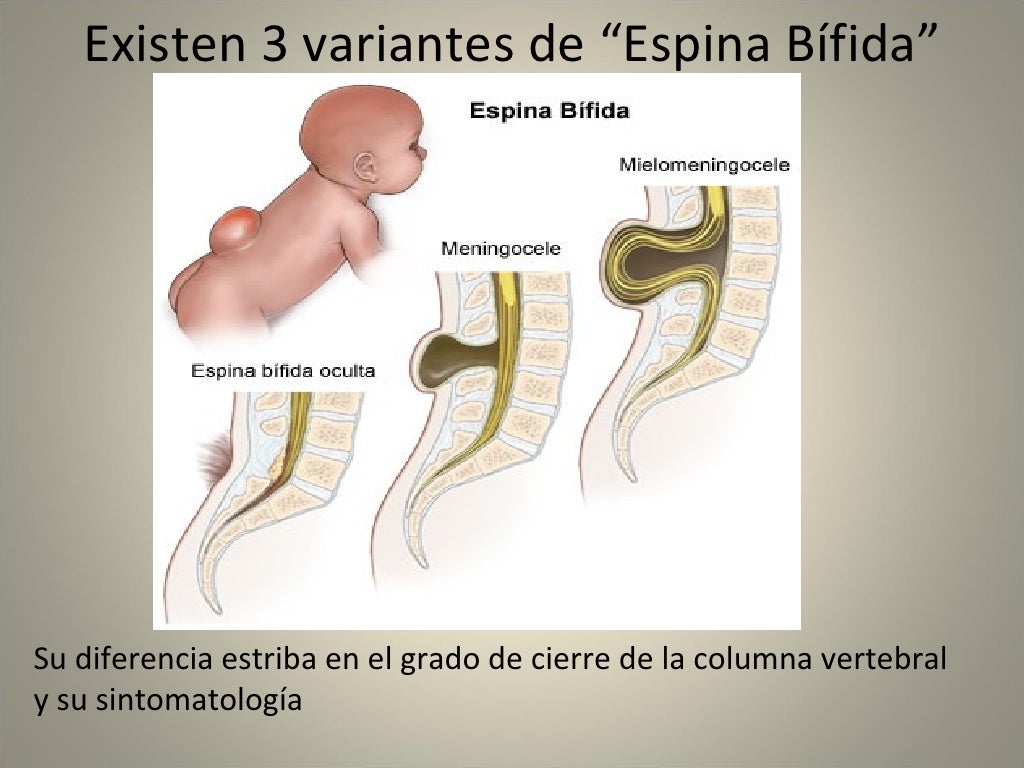
Other risk factors
Other risk factors for spina bifida include:
obesity - obese women are more likely to have a child with spina bifida than women of average weight; Diabetes - Women with diabetes may have an increased risk of the defect in their children. nine0011
Types of spina bifida
There are several different types of spina bifida:
- myelomeningocele is the most severe form of spina bifida, where a child's spinal canal remains open for several vertebrae, allowing the spinal cord and protective membranes around it to bulge out and form a hernial sac ;
- Meningocele is another serious type of spina bifida in which the protective membranes of the spinal cord protrude outward through the spine, with the spinal cord usually developing normally; nine0004
- spina bifida occulta is the most common and mildest form of spina bifida, in which one or more vertebrae are malformed but the gap in the spine is very small; this type of disease usually does not cause serious problems.

Symptoms of spina bifida
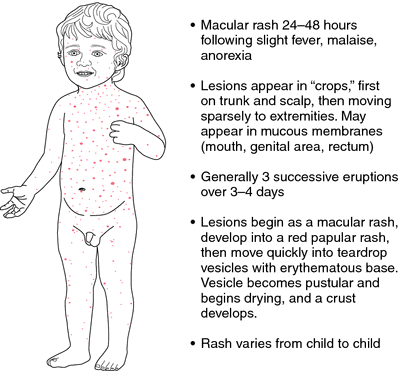
Spina bifida can cause a wide range of symptoms, including movement problems, bladder and bowel problems, and hydrocephalus. The severity of the symptoms of this anomaly varies significantly, largely depending on the location of the cleft in the spine. An upper spinal defect is more likely to cause leg paralysis and difficulty with mobility than a cleft in the middle or base of the spinal column. nine0011
Movement problems
Most children with spina bifida have weakness or paralysis in the lower extremities. They may need to use ankle supports or crutches to get around, or in severe cases they may need a wheelchair. Paralysis can also cause other related problems. For example, if the leg muscles are not used regularly, they can become very weak (atrophy). Muscles support bones, so muscle weakness can in turn cause dislocation or deformity of joints, bone fractures, bone deformity, and abnormal curvature of the spine. nine0011
nine0011
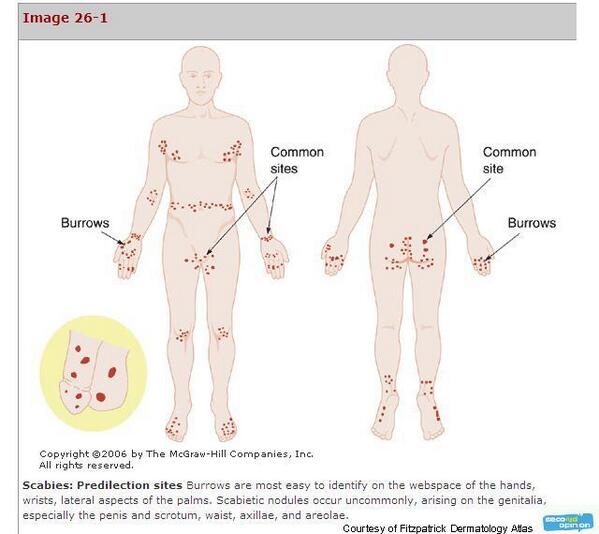
Bladder problems
Many patients with spina bifida have problems urinating. This is caused by improper formation of the nerves that control the bladder and can lead to:
- urinary incontinence;
- urinary tract infections;
- hydronephrosis - when one or both kidneys increase in size due to the accumulation of urine inside them;
- scarring of the kidneys; nine0015 kidney stones.
Bowel problems
The nerves that run through the spinal cord also control bowel movements and the sphincter muscles that keep feces in the bowel. Many people with spina bifida have little or no control of the sphincter muscles. Bowel incontinence often leads to periods of constipation followed by episodes of diarrhea.
Hydrocephalus
Some children with spina bifida have hydrocephalus, a buildup of excess fluid in the brain that can damage brain matter and cause further problems.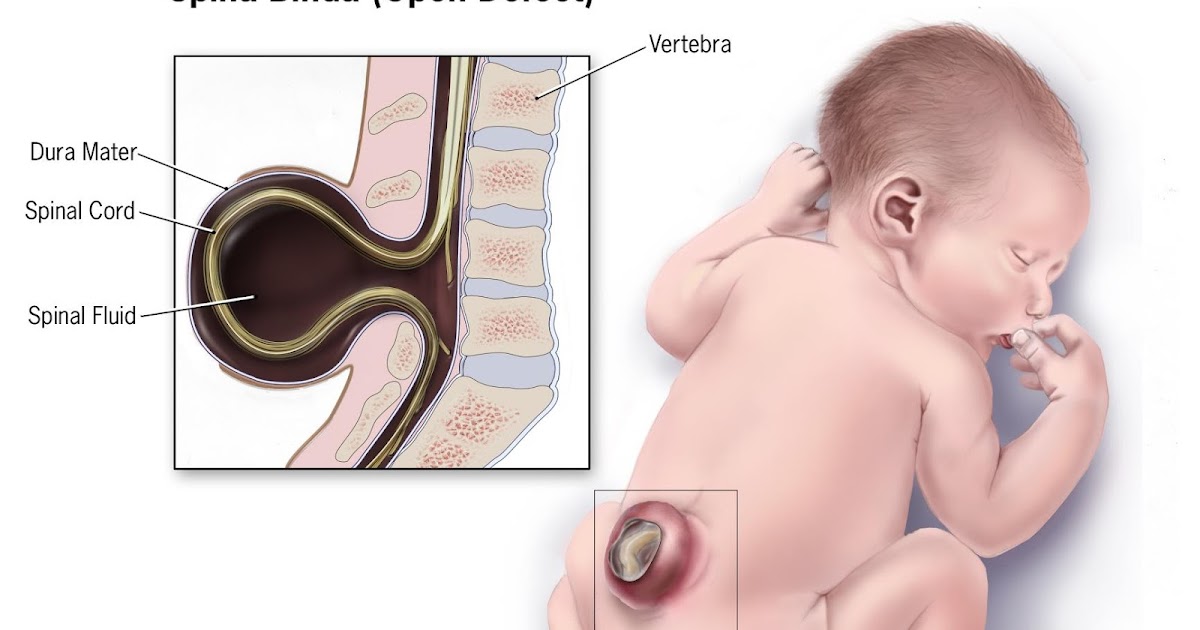 Many patients with hydrocephalus will have normal intelligence, although some will have learning difficulties such as:
Many patients with hydrocephalus will have normal intelligence, although some will have learning difficulties such as:
- short attention span;
- difficulty solving problems;
- difficulty reading;
- difficulty understanding spoken language - especially fast conversations between a group of people;
- difficulty organizing events or making detailed plans;
- problems with visual and physical coordination;
- irritability;
- convulsions; nine0004
- drowsiness;
- nausea.
In some infants, hydrocephalus causes the lower portions of the brain to move down towards the spinal cord - this is called Arnold-Chiari type 2 malformation.
Other problems
Other problems associated with spina bifida include:
- skin problems - decreased sensation;
- this can make it difficult to determine the location of damage to the skin on the legs with burns on the radiator, with injuries or infections; nine0004
- latex allergy - symptoms can range from a mild allergic reaction (watery eyes and skin rash) to a severe allergic reaction known as anaphylactic shock, which requires immediate medical attention.

How a Doctor Diagnoses Spina Bifida
Spina bifida is often discovered during a routine ultrasound scan, which is offered to all pregnant women between 18 and 21 weeks of pregnancy. If a neural tube defect is detected, the woman will be consulted by a medical commission on the possibility of prolonging or terminating the pregnancy. nine0011
Tests after birth
After the baby is born, a number of additional tests may be done to determine the severity of the condition and choose the most effective treatment. Tests may include:
- observing the baby's head growth and performing an ultrasound scan of the brain,
- computed tomography of the brain or magnetic resonance imaging of the brain to look for signs of hydrocephalus; nine0004
- bladder ultrasound
- ultrasound scan of the kidneys;
- assessment of the child's movements for signs of paralysis.
How a doctor treats spina bifida
Treatment of symptoms or conditions associated with spina bifida includes:
- surgery to close a hole in the spine and treat hydrocephalus;
- treatments that help ease the daily life of the patient; nine0004
- mobility aids and equipment;
- treatment of bowel and urinary problems.
With the right treatment and support, many children with spina bifida survive into adulthood.
Primary spinal repair surgery
Babies with a spinal fissure may have tissue and membranes coming out of the hole in the spine, damaging the nerves and can lead to serious infections, so the baby usually has spinal repair surgery within 48 hours of birth. During the operation, the surgeon will return the anatomically correct location of the spinal cord and exposed tissues or nerves, then close the cleft in the spine with muscles and skin. While this will fix the defect, unfortunately it cannot completely fix nerve damage. nine0011
Treatment of hydrocephalus
To treat hydrocephalus surgically, a surgeon implants a thin tube (shunt) to drain excess fluid from the brain to another part of the body, usually the abdomen. The shunt most often remains in place for the rest of the child's life. Further surgery may be required if:
- the shunt is blocked or infected;
- the child is growing out of the shunt and needs a larger size.
Physiotherapy
Physiotherapy is a method of treatment aimed at helping the patient to move, prevent deformity and stop further weakening of the leg muscles. It may include daily exercise to maintain muscle tone, as well as the wearing of special splints to support the legs. nine0011
Treatment for bladder problems
Treatment for bladder problems includes:
- antibiotic therapy - sometimes lifelong antibiotics are needed to prevent kidney and urinary tract infections;
- medicines to help relax the bladder so it can store more urine;
- bladder catheterization - using a catheter, urine is removed from the bladder several times a day to prevent urinary stasis and infection; nine0004
- Bladder surgery - may involve enlarging the bladder so it can hold more urine, or connecting the appendix to the bladder and creating an opening in the abdomen for easier catheter insertion.
Treatment of bowel problems
Treatment of bowel problems includes:
- laxatives - medicines to help empty the bowels;
- suppositories and enemas for constipation; nine0015 colostomy - an operation to retract the end of the large intestine through an opening to the abdomen;
- Attaches a stool bag to the opening.
A colostomy may be recommended if other treatments fail.
Prevention of spina bifida with folic acid
The best way to prevent spina bifida is to take folic acid supplements before and during pregnancy. A woman is usually given a 400 mcg folic acid tablet every day during the planning period and up to 12 weeks of pregnancy. A diet rich in foods containing folic acid is also recommended. nine0011
Recommendations for women at increased risk of spina bifida
Women at increased risk of having a child with spina bifida should be given a higher dose of folic acid (5 mg).
The best doctors in St. Petersburg
Vinogradova Galina Vasilievna
Rating: 5 / 5
Enroll
Klimanova Daria Alexandrovna
Rating: 4.6 / 5
Enroll
Share:
Scientific sources:
- Altynnik H.A.
 The value of ultrasound assessment of the thickness of the nuchal space of the fetus in early pregnancy for prenatal diagnosis of chromosomal abnormalities: Diss. . cand. honey. Sciences. M., 2002.
The value of ultrasound assessment of the thickness of the nuchal space of the fetus in early pregnancy for prenatal diagnosis of chromosomal abnormalities: Diss. . cand. honey. Sciences. M., 2002. - Medvedev M.V., Altynnik H.A. On the issue of ultrasound assessment of fetal anatomy in early pregnancy // Prenat. Diagn. 2002. V. 1. No. 2. S. 158-159.
- Fundamentals of prenatal diagnosis / Ed. Yudina E.V., Medvedeva M.V. M.: RAVUZDPG, Realnoe Vremya, 2002. 184 p. nine0004
- Sinitsin, V.E.: Magnetic resonance angiography of today. The level of development and new opportunities / V.E. Sinitsin, E.A. Timonina, O.V. Stukalova // Med. visualization. - 1996. - No. 4. - S. 36-44.
- Turkin A.M. MRI in the diagnosis of the brain. Diss. candidate of medical sciences - M., 1990.-158 p.
Useful information
Hemolytic disease of the fetus
What should be done to diagnose the causes of fetal hemolytic disease (erythroblastosis, Rh incompatibility)? To solve this problem, the first step for the patient is to make an appointment with an obstetrician-gynecologist.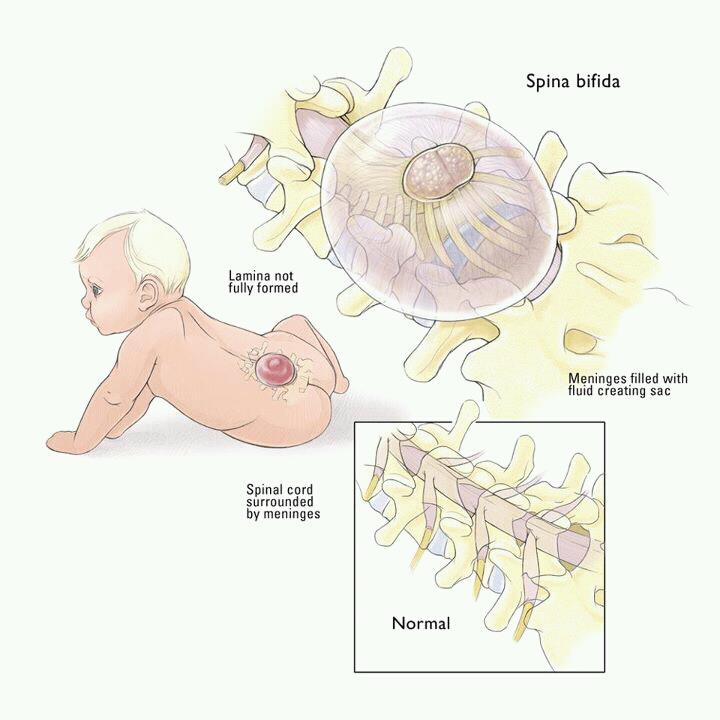 After the initial examination, the doctor may prescribe additional examinations: Blood test Checking the child's blood group. nine0011
After the initial examination, the doctor may prescribe additional examinations: Blood test Checking the child's blood group. nine0011
read more +
female infertility
What needs to be done to diagnose and treat female infertility? To solve this problem, the first step for the patient is to make an appointment with a gynecologist. After the initial examination, the doctor may prescribe additional studies: pelvic ultrasound MRI of the pelvis MRI of the pituitary gland CT pituitary Laboratory research Ultrasound of the adrenal glands Ultrasound of the thyroid gland. nine0011
read more +
How often can an MRI of the brain be done?
When receiving a referral for magnetic resonance imaging, patients often ask themselves how often they can have an MRI of the brain, especially if a child, a woman in the last stage of pregnancy, a cancer patient, a person who has just undergone surgery is to be examined. In this article, we will discuss the safety of magnetic resonance imaging, the recommended frequency of its implementation and possible side effects. nine0011
nine0011
read more +
SPIN BIFID (CONGENITAL DISTURBANCE OF THE SPINE) – ROMMER International Fizik Tedavi ve Rehabilitasyon Tıp Merkezi
What is Spina Bifida ?
Spina Bifida means a split or open spine. This is one of the most common congenital diseases. The baby is born with a hole in the back. Depending on the location of the hole, paralysis of varying degrees can occur. The higher the hole, the more severe the paralysis will be. For this reason, some spina bifida patients require fewer assistive devices (some cannot use them at all), and others may even need to use a wheelchair. nine0011
Affected muscles may not only be muscles that allow movement. Many patients may have problems with the muscles that control urine and stool.
More than 85% of spina bifida patients experience fluid accumulation in the brain (large head size). Since the bones of the skull in babies have not yet hardened, the head grows and tries to relieve pressure.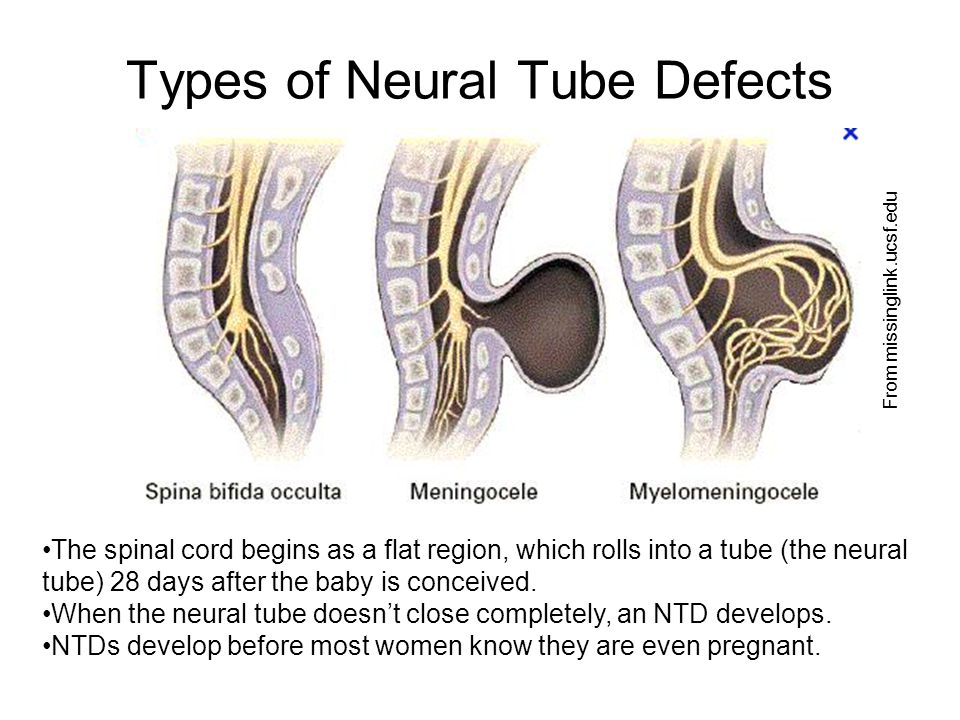 Therefore, intervention in hydrocephalus before brain damage occurs will not affect the IQ of children diagnosed with Spina Bifida. nine0011
Therefore, intervention in hydrocephalus before brain damage occurs will not affect the IQ of children diagnosed with Spina Bifida. nine0011
What causes Spina Bifida disease ?
Spina bifida is an anomaly that occurs in the first month of pregnancy in the womb. While a child's spine is taking shape, it does not close completely, and for this reason, a picture known as "spina bifida" arises among the population. It is not known exactly what causes it.
In Spina Bifida disease, the nerves and sheaths come out of the vertebrae, which remain open, forming a lump on the child's back. nine0011
Folic acid deficiency is primarily blamed. Therefore, precautions should be observed for pregnant women, as well as women who plan to become pregnant.
Spina Bifida is more common in Caucasians and more common in women. The higher frequency of Spina Bifida in the family resembles hereditary causes. The risk of having a child with spina bifida in future pregnancies is 15%.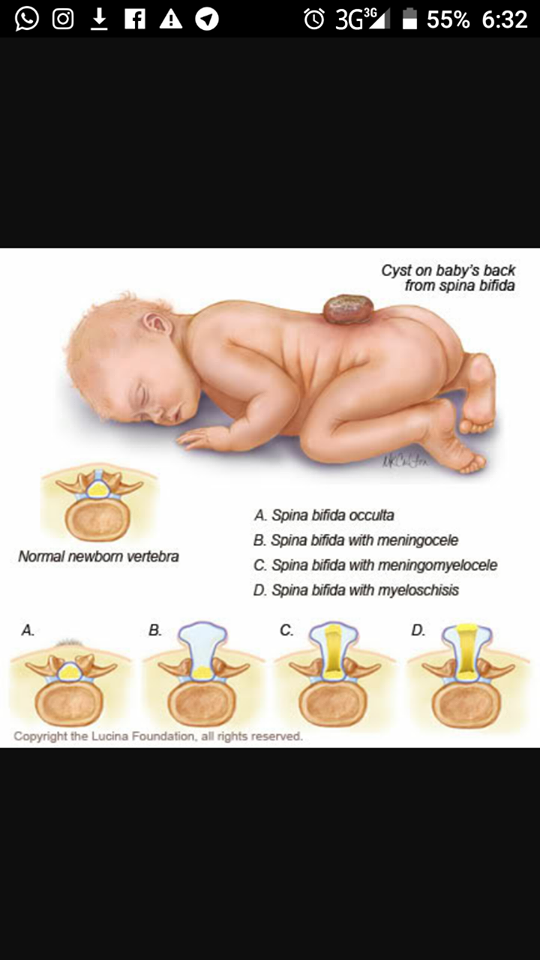 Some medications used for epilepsy, such as valproic acid, are said to increase the risk of having a baby with spina bifida. nine0011
Some medications used for epilepsy, such as valproic acid, are said to increase the risk of having a baby with spina bifida. nine0011
How many types are there Spines of Bifida ?
Spina bifida appears in the first 3 weeks of pregnancy and is approximately 0.15-0.3%. Although there are three types depending on the severity of the disease and the problems it causes, when Spina Bifida is mentioned, the most severe type, myelomeningocele, comes to mind first.
- Spina Bifida Occult is the most common and mild form of the disease. Many people are not even aware of the disease. The result of a film shot with a different purpose is often noticed. A small portion of the bones of the spine are exposed, which is why the condition is also called closed spina bifida. It usually does not cause discomfort and does not require surgery. nine0004
In rare cases, the spinal cord can be compressed and stretched. As a result, leg weakness and urinary incontinence may occur.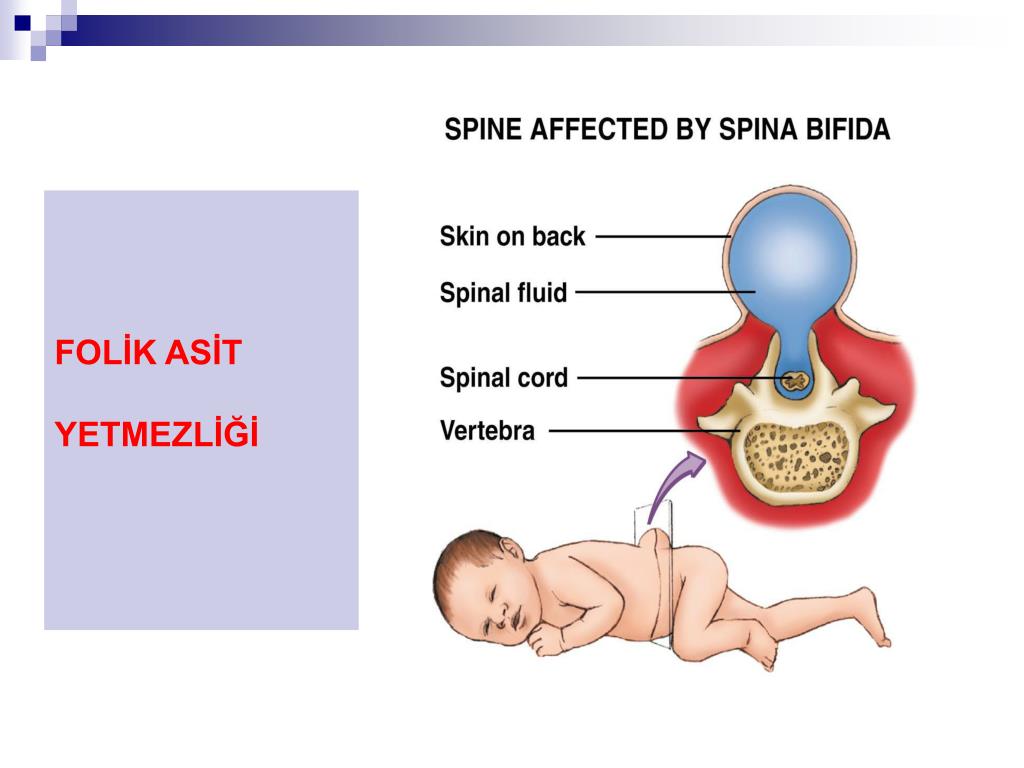 This is called the strained spine syndrome
This is called the strained spine syndrome
- Meningocele is the rarest type of spina bifida. Since there are no nerves in this part that come out in the form of a cavity, this does not cause serious problems. Some children develop bladder and bowel problems and, in rare cases, hydrocephalus.
- Myelomeningocele is the most serious and common type of spina bifida. The cavity emerging from the bones of the spine also contains the spinal nerves. As a result, it can cause some problems such as partial paralysis, difficulty walking, hydrocephalus, urinary/fecal incontinence, severe kidney failure, and scoliosis. nine0004
What are the symptoms of Spina Bifida?
Damage to the area, spinal cord membranes and nerves are among the factors that determine clinical symptoms.
Spina Bifida Occult usually has no symptoms. Sometimes visible traces can be found over the defect, such as an abnormal strand of hair, a small depression, or a mole at the site of the anomaly.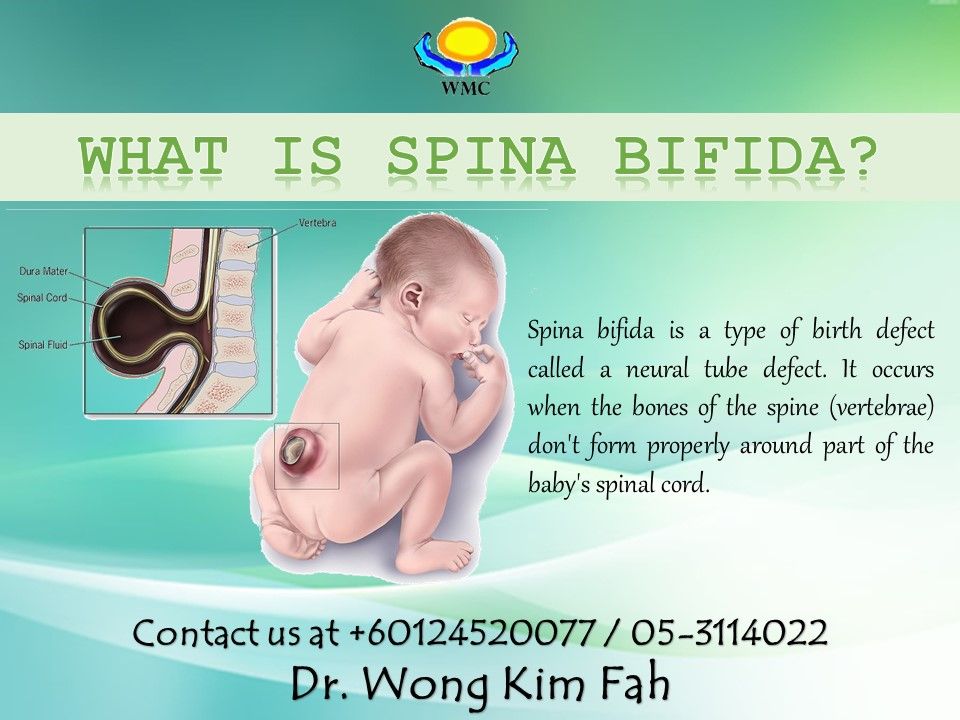
In meningocele, the meninges of the spinal cord protrude from the opening in the spine. Since the cavity contains only fluid, this factor can rarely cause hydrocephalus and even more rarely problems with the bladder and intestines. nine0011
Myelomeningocele leaves the spinal canal open in the lower or middle back, along many of the vertebrae. Inside this cavity are both the membranes surrounding the spinal cord and the spinal cord or nerves. In the later stages of life, severe symptoms may appear, such as problems with walking, leg deformities, and bladder dysfunction. Symptoms are characterized by localization in patients. Partial paralysis, difficulty walking, and hydrocephalus may occur.
How is spina bifida diagnosed?
Spina bifida can be diagnosed by amniocentesis, ultrasound and blood tests. Higher-than-expected AFP (alpha-fetoprotein) values in a triple test increase the likelihood of Spina Bifida.
Triple test performed between 16 and 18 weeks of pregnancy.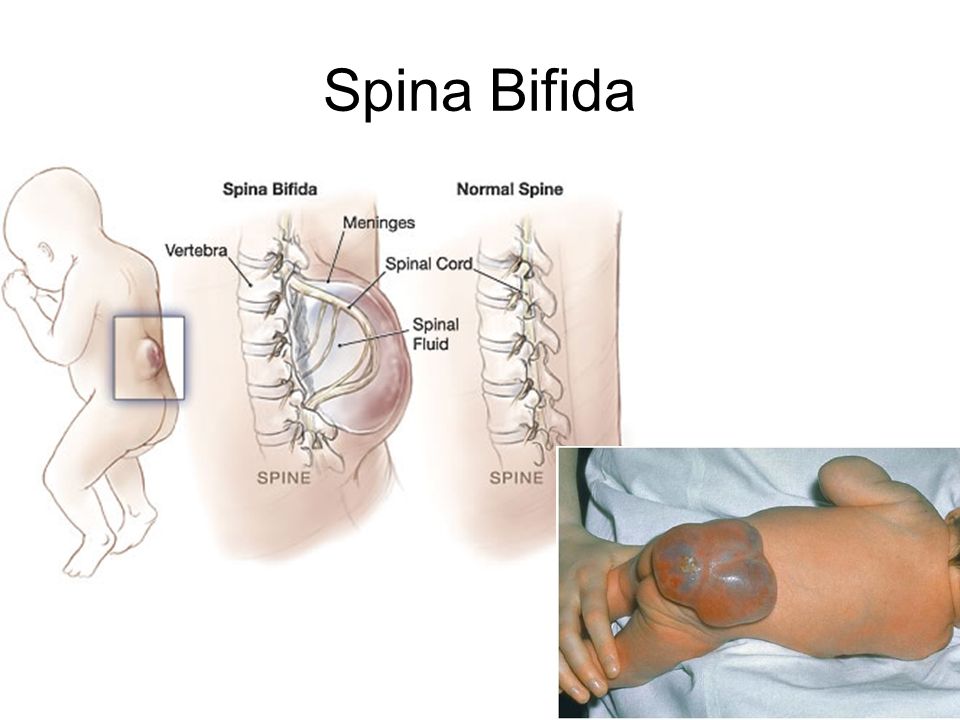 In addition, Spina Bifida can be detected with a detailed ultrasound examination to be carried out in these weeks. When making a diagnosis of Spina Bifida, it is necessary to examine in detail the skull, spine and other organs. nine0011
In addition, Spina Bifida can be detected with a detailed ultrasound examination to be carried out in these weeks. When making a diagnosis of Spina Bifida, it is necessary to examine in detail the skull, spine and other organs. nine0011
How is Spina Bifida treated?
If a baby with Spina Bifida is allowed, it should usually be operated on within 36 hours of birth. During the operation, the cavity on the back must be closed. Those who develop hydrocephalus should have a drainage system called bypass surgery to drain excess brain fluid into the bloodstream.
Operations are often used to protect the current situation and prevent future problems. Patients may not fully recover after surgery. However, even if Spina Bifida patients cannot become completely healthy, they can live on their own. nine0011
The use of some physiotherapy methods in the postoperative period will be especially useful for strengthening the muscles of the legs and lower back.
Rehabilitation should include exercises (sitting, balance, walking) to strengthen muscles and prevent joint stiffness.