Child rash on top of hands
Skin rashes in children | NHS inform
Childhood rashes are common and aren't usually a cause for concern. Most rashes are harmless and disappear without the need for treatment.
However, see your GP if your child has a rash and seems unwell, or if you're worried. They'll be able to investigate the cause and recommend any necessary treatment.
This page may give you a better idea about what could be causing the rash, but don't use this to self-diagnose your child's condition – always see a GP for a proper diagnosis.
The most common causes of rashes in children are:
- cellulitis
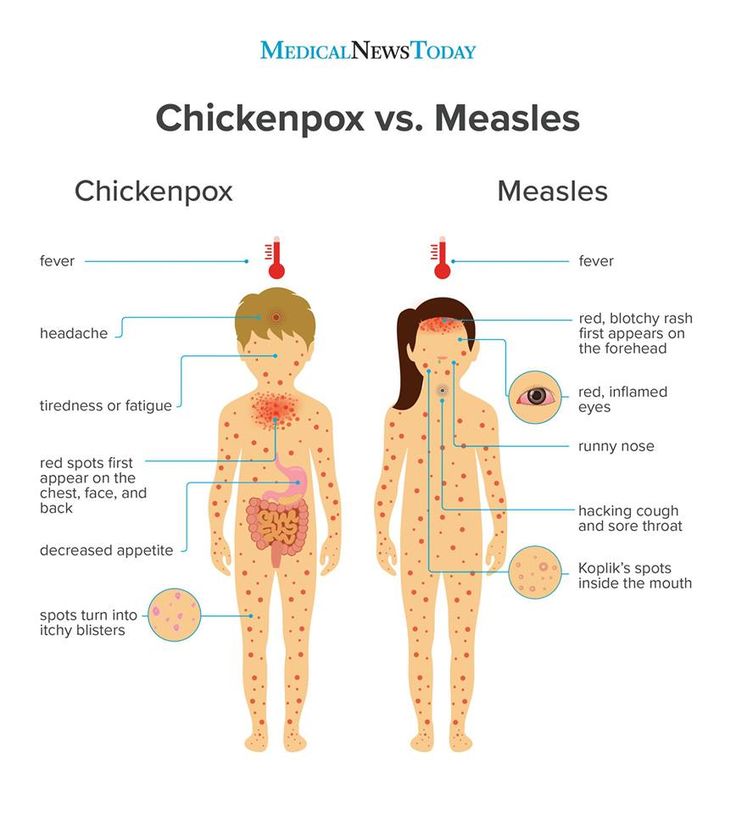
- chickenpox
- eczema
- erythema multiforme
- hand, foot and mouth disease
- impetigo
- keratosis pilaris ("chicken skin")
- measles
- molluscum contagiosum
- pityriasis rosea
- prickly heat
- psoriasis
- ringworm
- scabies
- scarlet fever
- slapped cheek syndrome
- urticaria (hives)
Although meningitis has become less common over recent years, it's important to be aware of the rash and the other signs and symptoms of meningitis.
Cellulitis
Cellulitis is an infection of the deeper layers of skin and underlying tissue. The affected area will be red, painful, swollen and hot. It often affects the legs, but can occur anywhere on the body. Your child will probably also have a fever.
See your GP immediately if an area of your child's skin suddenly turns red, hot and tender. If you can't see your GP on the same day, go to a walk-in centre or minor injuries unit.
Cellulitis can usually be diagnosed by assessing the symptoms and examining the skin. It usually responds well to treatment with antibiotics.
Chickenpox
Chickenpox is a viral illness that most children catch at some point. It most commonly affects children under 10 years of age.
A rash of itchy spots turns into fluid-filled blisters. They crust over to form scabs, which after a while drop off. Some children only have a few spots, whereas others have them over their entire body. The spots are most likely to appear on the face, ears and scalp, under the arms, on the chest and belly, and on the arms and legs.
There's no specific treatment for chickenpox, but you can take steps to relieve the symptoms. For example, paracetamol can help relieve fever (don't give aspirin to children under 16), and calamine lotion and cooling gels can be used to ease itching.
Read more about treating chickenpox.
Eczema
Eczema is a long-term condition that causes the skin to become itchy, red, dry and cracked. The most common type is atopic eczema, which mainly affects children but can continue into adulthood.
Atopic eczema commonly develops behind the knees or on the elbows, neck, eyes and ears. It isn't a serious condition, but if your child later becomes infected with the herpes simplex virus, it can cause the eczema to flare up into an outbreak of tiny blisters called eczema herpeticum, and will cause a fever.
About one in five children in the UK has eczema, and in eight out 10 cases it develops before the age of five, often before a child's first birthday.
Read about treating atopic eczema.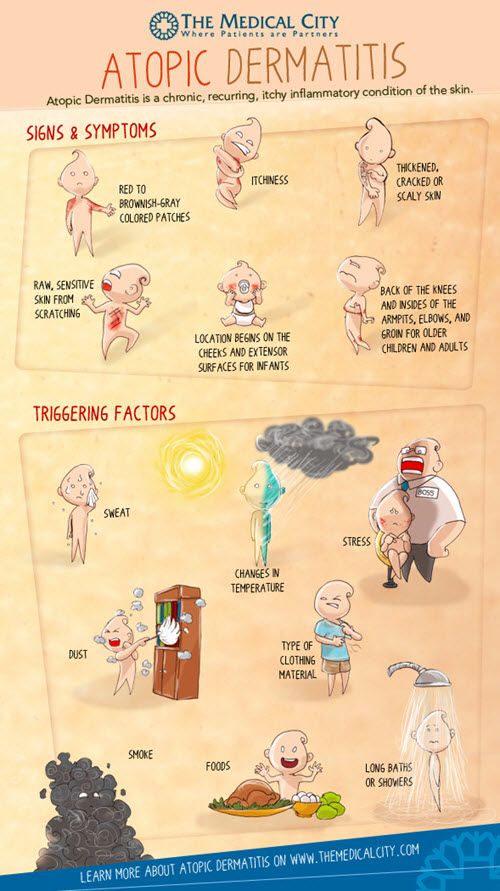
Erythema multiforme
Erythema multiforme is a skin rash (usually mild) that's caused by an allergic reaction to the herpes simplex virus.
The spots look like targets, with a dark red centre and paler ring around the outside. The hands or feet tend to be affected first, followed by the limbs, upper body and face.
Your child will probably feel unwell and may have a fever, which you should be able to treat with over-the-counter medicine. It may take from two to six weeks before they feel better. See your GP if your child has a rash and seems unwell.
In rare cases, erythema multiforme can be triggered by a reaction to certain medications, such as an antibiotic or anticonvulsant. This more severe form is called Stevens-Johnson syndrome and it can be life-threatening.
Hand, foot and mouth disease
Hand, foot and mouth disease is a common, contagious infection that causes mouth ulcers and spots and blisters on the palms of the hands and soles of the feet.
It's most common in young children (particularly those under 10), but it can also affect older children and adults.
There's no cure for hand, foot and mouth disease and it's easily spread, so you should keep your child away from school or nursery until they're better. Your child's immune system will fight the virus and it should clear up after about seven to 10 days.
Make sure your child drinks plenty of fluid, and if eating and swallowing is uncomfortable, give them soft foods, such as mashed potatoes, yoghurt and soup.
Impetigo
Impetigo is a common and highly contagious skin infection that causes sores and blisters. It isn't usually serious and often improves within a week of treatment. There are two types of impetigo called non-bullous and bullous.
Non-bullous impetigo typically affects the skin around the nose and mouth, causing sores that quickly burst to leave a yellow-brown crust.
Bullous impetigo typically affects the trunk (the area of the body between the waist and neck), and causes fluid-filled blisters that burst after a few days to leave a yellow crust.
See your GP or pharmacist if you think your child has impetigo. Antibiotics, in the form of a cream or tablets, will be prescribed. This should reduce the length of the illness to around seven to 10 days.
Keratosis pilaris ("chicken skin")
Keratosis pilaris is a common and harmless skin condition. The skin on the back of the upper arms becomes rough and bumpy, as if covered in permanent goose pimples. Sometimes, the buttocks, thighs, forearms and upper back can also be affected.
Keratosis pilaris typically begins in childhood and gets worse during puberty. Some people find it improves after this and may even disappear in adulthood.
There's no cure for keratosis pilaris, and it often gets better on its own without treatment. However, there are some measures you can take that may improve your child's rash, such as using non-soap cleansers rather than soap, and an emollient to moisturise their skin. Your GP or pharmacist will be able to recommend a suitable cream.
Measles
Measles is a highly infectious illness that most commonly affects young children. It's now rare in the UK because of the effectiveness of the measles, mumps and rubella (MMR) vaccine.
The measles rash is red-brown blotches. It usually starts on the head or upper neck and then spreads outwards to the rest of the body. Your child may also have a fever and cold-like symptoms.
Call your GP surgery immediately if you think your child has measles. It's best to phone before visiting because the surgery may need to make arrangements to reduce the risk of spreading the infection to others.
Measles usually passes in about seven to 10 days without causing further problems. Paracetamol or ibuprofen can be used to relieve fever, aches and pains (don't give aspirin to children under 16). Also, make sure your child drinks plenty of water to avoid dehydration.
Read more about treating measles.
Molluscum contagiosum
Molluscum contagiosum is a viral skin infection that causes clusters of small, firm, raised spots to develop on the skin.
It commonly affects young children aged one to five years, who tend to catch it after close physical contact with another infected child.
The condition is usually painless, although some children may experience some itchiness. It usually goes away within 18 months without the need for treatment.
Molluscum contagiosum is highly infectious. However, most adults are resistant to the virus, which means they're unlikely to catch it if they come into contact with it.
Pityriasis rosea
Pityriasis rosea is a relatively common skin condition that causes a temporary rash of raised, red scaly patches to develop on the body. Most cases occur in older children and young adults (aged between 10 and 35).
The rash can be very itchy. In most cases, it clears up without treatment in 2 to 12 weeks, although in rare cases it can last up to five months.
Emollients, steroid creams and antihistamines can be used to help relieve the itchiness. The rash doesn't usually leave scars, although the skin can sometimes be discoloured afterwards.
Prickly heat (heat rash)
Prickly heat (heat rash), also known as miliaria, is an itchy rash of small, raised red spots that causes a stinging or prickly sensation on the skin.
It occurs when the sweat ducts in the outer layer of skin (epidermis) are obstructed. You can get a heat rash anywhere on your body, but the face, neck, back, chest or thighs are most often affected.
Infants can sometimes get a prickly heat rash if they sweat more than usual – for example, when it's hot and humid or if they're overdressed. It isn't a serious condition and rarely requires any specific treatment.
Psoriasis
Psoriasis is a long-lasting (chronic) skin condition that causes red, flaky, crusty patches of skin covered with silvery scales.
The severity of psoriasis varies greatly from person to person. For some people, it's just a minor irritation, but for others it can have a major impact on their quality of life.
There's no cure for psoriasis, but there are a number of treatments that can help improve the symptoms and appearance of skin patches. For example, topical corticosteroids are creams and ointments that can be applied to the skin.
For example, topical corticosteroids are creams and ointments that can be applied to the skin.
Ringworm
Ringworm is a highly infectious fungal skin infection that causes a ring-like red or silvery patch on the skin that can be scaly, inflamed or itchy.
Ringworm often affects the arms and legs, but it can appear almost anywhere on the body. Other similar fungal infections can affect the scalp, feet, groin and nails.
Ringworm can usually be easily treated with antifungal medicines, which are available from a pharmacy. Ringworm of the scalp can cause scaling and patches of hair loss. It's treated with antifungal tablets, often combined with antifungal shampoo.
Scabies
Scabies is a contagious skin condition that's intensely itchy. It's caused by tiny mites that burrow into the skin.
In children, scabies is usually spread through prolonged periods of skin-to-skin contact with an infected adult or child – for example, during play fighting or hugging.
The mites like warm places, such as skin folds, between the fingers, under fingernails, or around the buttock creases. They leave small red blotches, which are often found on the palms of the hands or soles of the feet. In infants, blisters are commonly found on the soles of the feet.
See your GP if you think your child has scabies. It's not usually a serious condition, but it does need to be treated. Your GP will prescribe a lotion or cream. Read more about treating scabies.
Scarlet fever
Scarlet fever is a highly contagious bacterial infection that usually affects children between two and eight years of age. It causes a distinctive pink-red rash, which feels like sandpaper to touch and may be itchy.
It often starts with a sore throat, fever and headache, with the rash developing two to five days after infection. The rash usually occurs on the chest and stomach before spreading to other areas of the body, such as the ears and neck.
Scarlet fever usually clears up after about a week, but see your GP if you think your child may have it.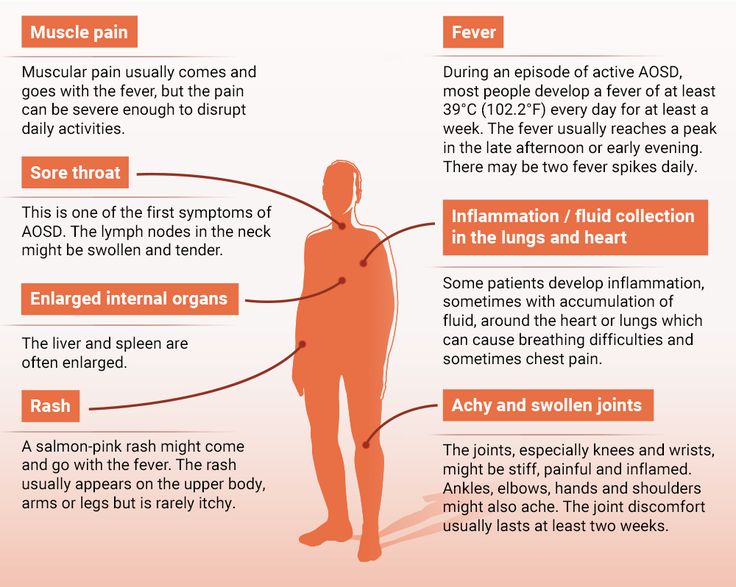 Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Antibiotics are used to treat it (liquid antibiotics, such as penicillin or amoxicillin, are often used to treat children).
Slapped cheek syndrome
Slapped cheek syndrome – also known as fifth disease or parvovirus B19 – is a viral infection that's common in children aged six to 10.
It causes a distinctive bright red rash to develop on both cheeks. This can look alarming, but it usually clears up by itself in one to three weeks.
Unless your child is feeling unwell, they don't need to stay away from school. Once the rash appears, the infection is no longer contagious. However, it's a good idea to notify your child's school about the infection.
Urticaria (hives)
Urticaria – also known as hives, weals, welts or nettle rash – is a raised, itchy rash that can affect one part of the body or be spread across large areas. It's a common skin reaction that often affects children.
Urticaria occurs when a trigger causes high levels of histamine and other chemical messengers to be released in the skin. These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
These substances cause the blood vessels in the skin to open up, resulting in redness or pinkness, and swelling and itchiness.
There are many possible triggers of urticaria, including allergens, such as food or latex, irritants, such as nettles, medicines, and physical factors, such as heat or exercise. Sometimes, a cause can't be identified.
The rash is usually short-lived and mild, and can often be controlled with antihistamines.
Chickenpox (varicella) | NHS inform
See all parts of this guide Hide guide parts
- 1. About chickenpox
-
2.
 Symptoms of chickenpox
Symptoms of chickenpox
- 3. Causes of chickenpox
- 4. Diagnosing chickenpox
- 5. Treating chickenpox
- 6. Complications of chickenpox
-
7.
 Preventing the spread of chickenpox
Preventing the spread of chickenpox
About chickenpox
Chickenpox is a mild and common childhood illness that most children catch at some point.
It causes a rash of red, itchy spots that turn into fluid-filled blisters. They then crust over to form scabs, which eventually drop off.
Some children have only a few spots, but other children can have spots that cover their entire body. These are most likely to appear on the face, ears and scalp, under the arms, on the chest and belly, and on the arms and legs.
Read more about the symptoms of chickenpox.
Chickenpox (known medically as varicella) is caused by a virus called the varicella-zoster virus. It's spread quickly and easily from someone who is infected.
Read more about the causes of chickenpox.
Chickenpox is most common in children under the age of 10.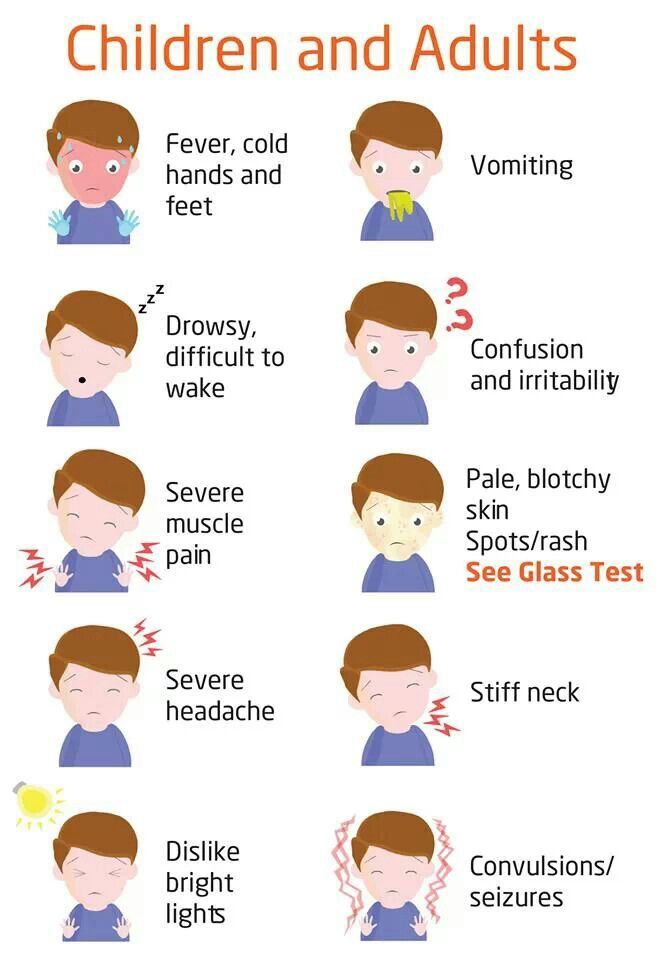 In fact, chickenpox is so common in childhood that over 90% of adults are immune to the condition because they've had it before.
In fact, chickenpox is so common in childhood that over 90% of adults are immune to the condition because they've had it before.
Children usually catch chickenpox in winter and spring, particularly between March and May.
What to do
To prevent spreading the infection, keep children off nursery or school until all their spots have crusted over.
Chickenpox is infectious from 1 to 2 days before the rash starts, until all the blisters have crusted over (usually 5 to 6 days after the start of the rash).
If your child has chickenpox, try to keep them away from public areas to avoid contact with people who may not have had it, especially people who are at risk of serious problems, such as newborn babies, pregnant women and anyone with a weakened immune system (for example, people having cancer treatment or taking steroid tablets).
Read more about what you need to do to stop chickenpox spreading.
Chickenpox treatment
Chickenpox in children is considered a mild illness, but your child will probably feel pretty miserable and irritable while they have it.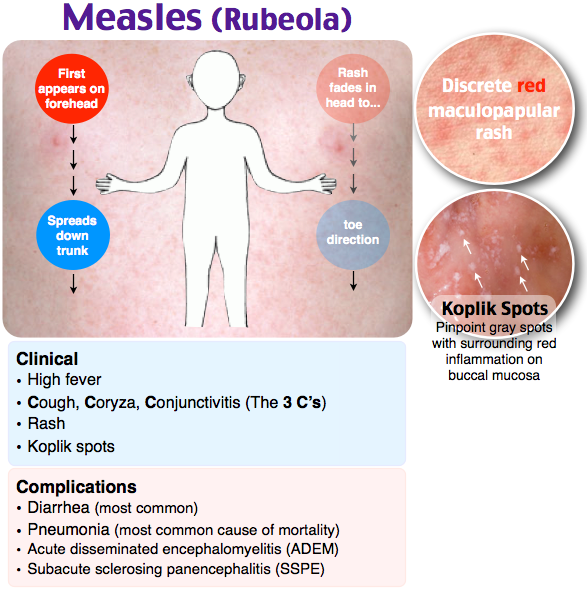
Your child may have a fever for the first few days of the illness. The spots can be incredibly itchy.
There is no specific treatment for chickenpox, but there are pharmacy remedies that can alleviate symptoms. These include paracetamol to relieve fever, and calamine lotion and cooling gels to ease itching.
In most children, the blisters crust up and fall off naturally within one to two weeks.
Read more about chickenpox treatments.
When to see a doctor
For most children, chickenpox is a mild illness that gets better on its own.
However, some children can become more seriously ill with chickenpox and need to see a doctor.
Contact your GP straight away if your child develops any abnormal symptoms, such as:
- if the blisters on their skin become infected
- if your child has a pain in their chest or has difficulty breathing
Chickenpox in adults
Chickenpox may be a childhood illness, but adults can get it too. Chickenpox tends to be more severe in adults than children, and adults have a higher risk of developing complications.
Chickenpox tends to be more severe in adults than children, and adults have a higher risk of developing complications.
Adults with chickenpox should stay off work until all the spots have crusted over. They should seek medical advice if they develop any abnormal symptoms, such as infected blisters.
Adults with chickenpox may benefit from taking antiviral medicine if treatment is started early in the course of the illness. Read more about antivirals in the treatment of chickenpox.
Who's at special risk?
Some children and adults are at special risk of serious problems if they catch chickenpox. They include:
- pregnant women
- newborn babies
- people with a weakened immune system
These people should seek medical advice as soon as they are exposed to the chickenpox virus or they develop chickenpox symptoms.
They may need a blood test to check if they are protected from (immune to) chickenpox.
Read more about immunity testing and the diagnosis of chickenpox in people at special risk.
Chickenpox in pregnancy
Chickenpox occurs in approximately 3 in every 1,000 pregnancies. It can cause serious complications for both the pregnant woman and her baby. See complications of chickenpox for further information on what to do if you are exposed to chickenpox during pregnancy.
Chickenpox and shingles
Once you have had chickenpox, you usually develop antibodies to the infection and become immune to catching it again. However, the virus that causes chickenpox, the varicella-zoster virus, remains inactive (dormant) in your body's nerve tissues and can return later in life as an illness called shingles.
It's possible to catch chickenpox from someone with shingles, but not the other way around.
Read more about shingles.
Is there a vaccine against chickenpox?
There is a chickenpox vaccine, but it is not part of the routine childhood vaccination schedule. The vaccine is only offered to children and adults who are particularly vulnerable to chickenpox complications.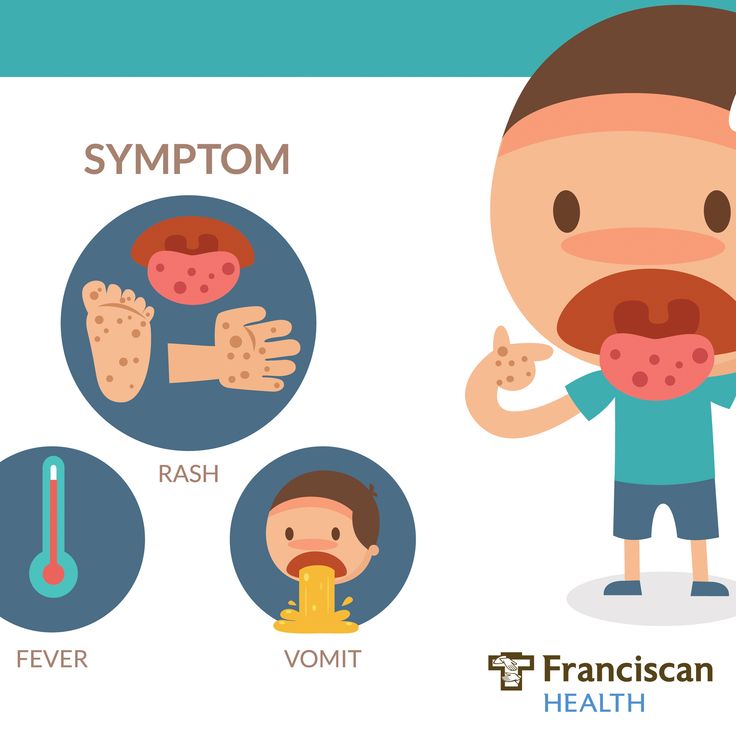
The recommended 2 doses of the vaccine is estimated to offer 98% protection from chickenpox in children and 75% protection in adolescents and adults.
So it may be possible to develop the infection after vaccination. Similarly, there is a chance that someone who has received the vaccine could develop chickenpox after coming in close contact with a person who has shingles.
Symptoms of chickenpox
The most commonly recognised chickenpox symptom is a spotty, blistering red rash that can cover the entire body.
Chickenpox spots
Chickenpox spots
The spots normally appear in clusters and tend to be:
- behind the ears
- on the face
- over the scalp
- on the chest and belly
- on the arms and legs
However, the spots can be anywhere on the body, even inside the ears and mouth, on the palms of the hands, soles of the feet and inside the nappy area.
Although the rash starts as small, itchy red spots, these develop a blister on top and become intensely itchy after about 12-14 hours.
After a day or two, the fluid in the blisters gets cloudy and they begin to dry out and crust over.
After 1 to 2 weeks, the crusting skin will fall off naturally.
New spots can keep appearing in waves for 3 to 5 days after the rash begins. Therefore, different clusters of spots may be at different stages of blistering or drying out.
Read more about how to ease the itchiness and other symptoms of chickenpox in our section on chickenpox treatments.
Find out what you can do to stop chickenpox spreading.
Feeling unwell
Before the rash appears, you or your child may have some mild flu-like symptoms, including:
- feeling sick
- a high temperature (fever) of 38C (100.4F) or over
- aching, painful muscles
- headache
- generally feeling unwell
- loss of appetite
These flu-like symptoms, especially the fever, tend to be more common and worse in adults than in children.
Unusual symptoms
Most healthy children (and adults) recover from chickenpox with no lasting ill-effects simply by resting, just as with a cold or the flu.
However, some children and adults are unlucky and have a more severe bout.
Contact your GP straight away if you or your child develop any abnormal symptoms, such as:
- the skin surrounding the blisters becoming red and painful
- pain in the chest or difficulty breathing
- signs of dehydration, such as fewer wet nappies, drowsiness and cold hands and feet
In cases such as this, prescription medicine or hospital treatment may be needed.
Read more about chickenpox complications.
Causes of chickenpox
Chickenpox is caused by the varicella-zoster virus. You catch it by coming into contact with someone who is infected.
Chickenpox is a very contagious infection. Around 90% of people who have not previously had chickenpox will become infected when they come into contact with the virus.
How you catch the virus
The chickenpox virus is spread most easily from someone who has the rash. The blisters are very itchy and break open easily, which can contaminate surfaces or objects. The virus may then be transferred by touching the surface or object, then touching your face.
The virus is also contained in the millions of tiny droplets that come out of the nose and mouth when an infected person coughs or sneezes. This can also contaminate surfaces or objects.
It normally takes 14 days for the symptoms of chickenpox to show after you have come into contact with the virus. However, this can vary from person to person – from as little as 7 days, up to 21 days. This is called the "incubation period".
Someone with chickenpox is most infectious from 1 to 2 days before the rash appears, until all the blisters have crusted over. This usually takes 5 to 6 days from the start of the rash.
Read more about the diagnosis of chickenpox and how to stop chickenpox spreading.
Shingles
If you have not had chickenpox before, you can also catch chickenpox from someone with shingles (an infection caused by the same virus). However, it's not possible to catch shingles from someone who has chickenpox.
Read more about shingles.
Diagnosing chickenpox
You or your child should not usually need any medical tests to diagnose chickenpox. You can be pretty sure that it is chickenpox if there are the key symptoms of a mild fever followed by an itchy rash, with blisters and scabs.
Chickenpox spots are usually distinctive enough to distinguish from other rashes, although they can be confused with other conditions that affect the skin, such as insect bites or scabies (another contagious skin condition that causes intense itching).
If you're uncertain about what is causing the symptoms, your GP can carry out a simple blood test to identify the virus.
Find your local GP surgery.
When to contact your GP
1. See your GP if you're not sure whether you or your child have chickenpox.
2. Contact your GP urgently if you have been in contact with someone who has chickenpox, or you have chickenpox symptoms and:
- you are pregnant
- you have a weakened immune system (the body’s defence system)
- your baby is less than 4 weeks old
Chickenpox in these instances can cause serious complications, if left untreated. It is essential to seek medical advice so that you can receive any necessary treatment.
3. Contact your GP if you have chickenpox and are breastfeeding. They can advise about whether you should continue breastfeeding your baby.
Having a blood test
Once you have contacted your GP, you may need a test to see if you're already immune from chickenpox.
If you have had chickenpox in the past, it is extremely unlikely that you will develop chickenpox for a second time. If you've never had chickenpox, or you're unsure whether you've had it, you may need an immunity test.
This is a blood test that checks whether you are producing the antibodies to the chickenpox virus.
If your blood test result shows that you have the antibodies, you'll be naturally protected from the virus. If you don't have the antibodies, you'll need to be monitored closely to see if you develop chickenpox symptoms. If you do, further treatment may be needed.
Read more about chickenpox treatment.
Treating chickenpox
There is no cure for chickenpox, and the virus usually clears up by itself without any treatment.
However, there are ways of easing the itch and discomfort, and there are important steps you can take to stop chickenpox spreading.
Painkillers
If your child is in pain or has a high temperature (fever), you can give them a mild painkiller, such as paracetamol (available over the counter in pharmacies). Always read the manufacturer's dosage instructions.
Paracetamol is the preferred painkiller for treating the associated symptoms of chickenpox. This is due to a very small risk of non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, causing adverse skin reactions during chickenpox.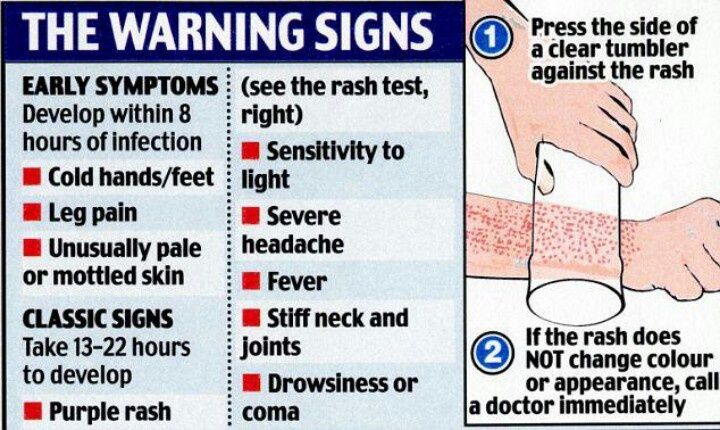
Avoid giving your child ibuprofen if they have asthma or a history of stomach problems. If you're not sure whether ibuprofen is suitable, check with your GP or pharmacist. If your child is younger than 3 months old, you should always speak to your GP before giving your child any kind of pain relief.
Never give your child aspirin if you suspect or know that they have chickenpox.
If you're pregnant and need to take painkillers, then paracetamol is the first choice. You can use it at any stage of pregnancy. Only take ibuprofen during the second trimester (weeks 14-27 of the pregnancy).
If you're pregnant and have chickenpox, you should visit your GP as soon as possible. You may need to have antiviral medicine or immunoglobulin treatment to prevent your symptoms from getting worse.
Keeping hydrated
It is important for children (and adults) with chickenpox to drink plenty of water to avoid dehydration. Sugar-free ice lollies are a good way of getting fluids into children.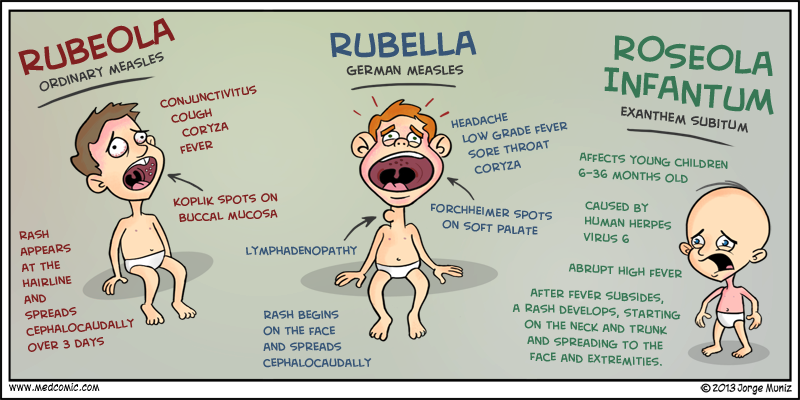 They also help to soothe a sore mouth that has chickenpox spots in it.
They also help to soothe a sore mouth that has chickenpox spots in it.
Avoid anything that may make the mouth sore, such as salty foods. Soup is easy to swallow as long as it is not too hot.
Stop the scratching
Chickenpox can be incredibly itchy, but it's important for children (and adults) to not scratch the spots, to avoid future scarring.
One way of stopping scratching is to keep fingernails clean and short. You can also put socks over your child's hands at night to stop them scratching the rash as they sleep.
If your child's skin is very itchy or sore, try using calamine lotion or cooling gels. These are available in pharmacies and are very safe to use. They have a soothing, cooling effect.
A stronger medicine called chlorphenamine can also help to relieve the itching. It's available from your pharmacist over the counter or it can be prescribed by your GP. Chlorphenamine is taken by mouth and is suitable for children over 1 year old.
Cool clothing
If your child has a fever, or if their skin is sore and aggravated, dress them appropriately so that they don't get too hot or too cold. Loose-fitting, smooth, cotton fabrics are best and will help stop the skin from becoming sore and irritated.
Loose-fitting, smooth, cotton fabrics are best and will help stop the skin from becoming sore and irritated.
If your child has chickenpox, avoid sponging them down with cool water. This can make your child too cold and may make them shiver.
Stronger treatments
Antiviral medicine
Aciclovir is an antiviral medicine that is sometimes given to people with chickenpox.
Aciclovir may be prescribed to:
- pregnant women
- adults, if they visit their GP within 24 hours of the rash appearing
- newborn babies
- people with a weakened immune system (the body’s defence system)
Ideally, aciclovir needs to be started within 24 hours of the rash appearing. It does not cure chickenpox, but it makes the symptoms less severe. You normally need to take the medicine as tablets 5 times a day for 7 days.
If you are taking aciclovir, make sure you drink plenty of fluids. Side effects are rare, but can include nausea and diarrhoea.
Immunoglobulin treatment
Immunoglobulin is a solution of antibodies that is taken from healthy donors. Varicella-zoster immunoglobulin (VZIG) contains antibodies to the chickenpox virus.
Immunoglobulin treatment is given by injection. It is not used to treat chickenpox, but to protect people who are at high risk of developing a severe chickenpox infection. This includes:
- pregnant women
- newborn babies
- people with weakened immune systems
In the case of pregnant women, immunoglobulin treatment also reduces the risk of the unborn baby becoming infected.
As the supply of VZIG is limited, it will only be considered if a high-risk person has:
- been significantly exposed to the virus – significant exposure could be face-to-face contact with someone who has chickenpox
- been in the same room for 15 minutes with someone who has chickenpox
- had a blood test to confirm that they've not had chickenpox before
In some cases, newborn babies may be given immunoglobulin treatment without having a blood test first.
Read more about the complications of chickenpox.
Complications of chickenpox
Complications of chickenpox are rare in healthy children. The most common complication is where the blisters become infected with bacteria.
A sign that the blisters have become infected is when the surrounding skin becomes red and sore.
If you think that your child's blisters have become infected, contact your GP as the child may need a course of antibiotics.
Other complications in children
Very rarely, chickenpox can lead to more serious complications involving the nervous system (brain and spinal cord) in children.
These include infections of the brain (encephalitis), the protective membranes around the brain (meningitis) or part of the brain called the cerebellum (cerebellitis).
Signs of these problems can include:
- a lack of energy
- drowsiness
- confusion
- seizures (fits)
- vomiting
- severe headaches
- a stiff neck
- behavioural changes
- problems with walking, balance or speech (ataxia)
Seek medical advice as soon as possible if your child develops any of these symptoms after having chickenpox.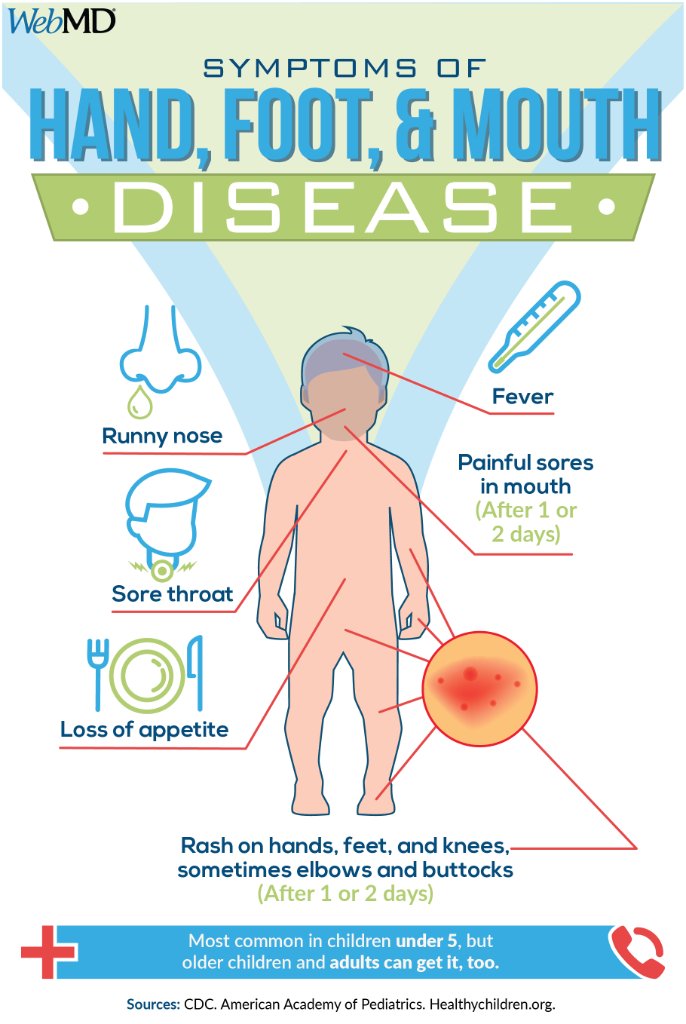
At-risk groups
The people who are most at risk of developing chickenpox complications are:
- adults
- pregnant women
- babies under four weeks old
- people with a weakened immune system
Adults
Chickenpox can be more serious in adults than in children. Adults with the virus are more likely to be admitted into hospital. Approximately 5-14% of adults with chickenpox develop lung problems, such as pneumonia. If you smoke, your risk of developing lung problems is much higher.
Although it is more serious in adults, most people will still make a full recovery from the chickenpox virus.
Pregnant women
If you're pregnant, chickenpox can occasionally cause complications.
For example, your risk of developing pneumonia is slightly higher if you're pregnant, especially if you smoke. The further you are into your pregnancy, the more serious the risk of pneumonia tends to be.
If you get chickenpox while you're pregnant, there is also a small but significant risk to your unborn baby.
If you are infected with chickenpox during the first 28 weeks of your pregnancy, there is a risk that your unborn baby could develop a condition known as foetal varicella syndrome (FVS).
This syndrome is rare. The risk of it occurring in the first 12 weeks of pregnancy is less than 1%. Between weeks 13 and 20, the risk is 2%.
There have only been a few reports of FVS due to an infection from weeks 20 to 28 of pregnancy, and the risk is thought to be much less than 1%.
FVS can cause serious complications, including:
- scarring
- eye defects, such as cataracts
- shortened limbs
- brain damage
There are also other risks from catching chickenpox after week 20 of pregnancy.
It's possible that your baby may be born prematurely (before week 37 of the pregnancy).
If you are infected with chickenpox 7 days before or 7 days after giving birth, your newborn baby may develop a more serious type of chickenpox. In a few severe cases, this type of chickenpox can be fatal.
See your GP urgently if you're pregnant or have given birth in the last 7 days and you think you may have chickenpox, or if you've been exposed to someone who has chickenpox.
People with a weakened immune system
Your immune system is your body's way of defending itself against disease, bacteria and viruses.
If your immune system is weak or does not work properly, you are more susceptible to developing infections such as chickenpox. This is because your body produces fewer antibodies to fight off the infection.
You may have a weakened immune system if you take immunosuppressive medication.
Immunosuppressive medication such as steroid tablets may be used if, for example, you have an inflammatory condition such as rheumatoid arthritis, lupus or certain blood conditions.
If you have a weakened immune system, you're also more at risk of developing complications from chickenpox. These complications include:
- pneumonia
- blood poisoning (septicaemia)
- meningitis
See your GP urgently if you have a weakened immune system and you've been exposed to the chickenpox virus.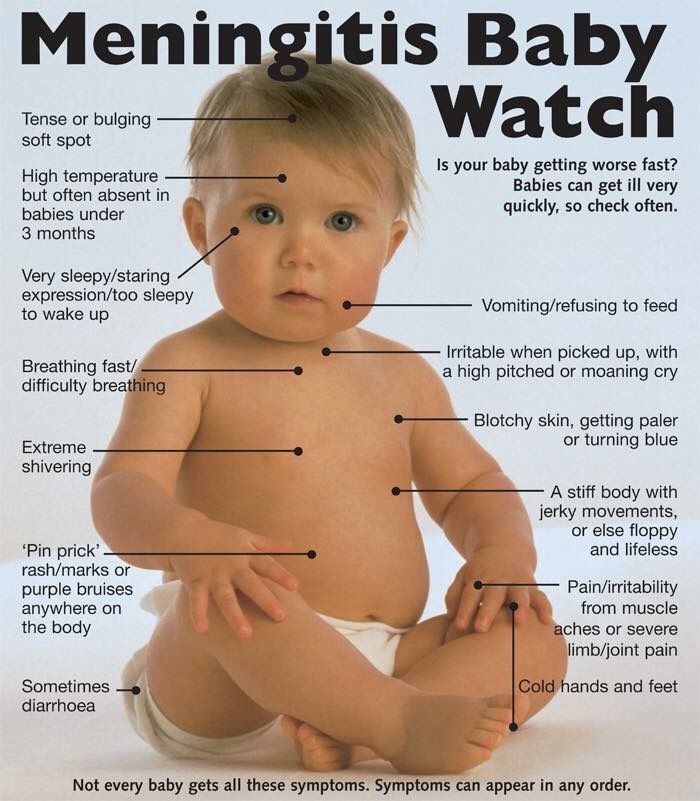
For more information, read about how to stop the spread of chickenpox.
Preventing the spread of chickenpox
If your child has chickenpox,it is recommended that you inform their school or nursery, and keep them at home for 5 days.
If you have chickenpox, stay off work and at home until you're no longer infectious, which is until the last blister has burst and crusted over. This usually happens five or six days after the rash begins.
It is a good idea for anyone who has chickenpox to avoid contact with:
- pregnant women
- newborn babies
- anyone who has a weak immune system, such as people who are having chemotherapy (a treatment for cancer) or taking steroid tablets
If you or your child have recently been exposed to the chickenpox virus, you may not be able to visit friends or relatives in hospital. Telephone the ward to check first.
Travelling on a plane
If you or your child have chickenpox, you may not be allowed to fly until 6 days after the last spot has appeared.
You and your child should be safe to fly once you're past the infectious stage and all of the blisters have crusted over. However, it's best to check the policy of your airline first. Inform the airline as soon as chickenpox is diagnosed.
It is also important to let your travel insurer know if you or your child has chickenpox. You need to make sure that you'll be covered if you have to delay or cancel your holiday, or if you need to extend your stay until your child is well enough to fly home.
Stop the virus spreading
Chickenpox can sometimes be spread through contact with objects that have been contaminated with the virus, such as children's toys, bedding or clothing.
If someone in your household has chickenpox, you can help stop the virus spreading by wiping any objects or surfaces with a sterilising solution and making sure that any infected clothing or bedding is washed regularly.
Vaccination
There is a chickenpox vaccine that is used to protect people who are most at risk of a serious chickenpox infection or of passing the infection on to someone who is at risk.
People who may be considered for chickenpox vaccination include:
- healthcare workers who are not already immune – for example, a nurse who has never had chickenpox and who may pass it to someone they are treating if they become infected
- people living with someone who has a weakened immune system – for example, the child of a parent receiving chemotherapy
The vaccine is not suitable for pregnant women. Avoid getting pregnant for 3 months after having the vaccine. The vaccine is also not suitable for people with weakened immune systems.
How effective is the vaccine?
The recommended 2 doses of the vaccine is estimated to offer 98% protection from chickenpox in children and 75% protection in adolescents and adults.
So it may be possible to develop the infection after vaccination.
Rash in a child on legs and arms
RASH IN A CHILD ON LEGS AND HANDS WITHOUT TEMPERATURE, WITH TEMPERATURE, ITCHING, NOT ITCHING
Children are the most beloved, defenseless people.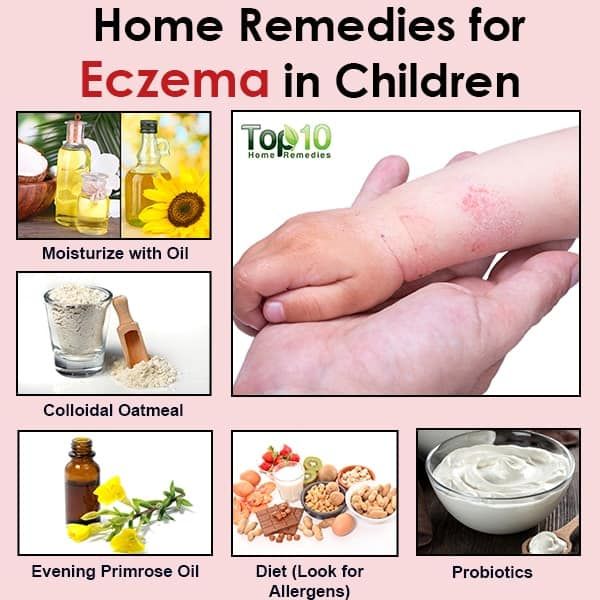 It is from adults that the health of the baby sometimes depends. They need our attention first and foremost. The skin of children is still imperfect and very susceptible to various infections. So, the appearance of a rash on the arms and legs can be an innocent manifestation, or it can be a signal of a dangerous disease. Below we will consider for what reason a rash may appear in a child and how to act in this situation. nine0003
It is from adults that the health of the baby sometimes depends. They need our attention first and foremost. The skin of children is still imperfect and very susceptible to various infections. So, the appearance of a rash on the arms and legs can be an innocent manifestation, or it can be a signal of a dangerous disease. Below we will consider for what reason a rash may appear in a child and how to act in this situation. nine0003
Rash - what is it?
What is such a phenomenon? A rash is a pathological change in the skin, mucous membranes, which differ from normal skin in appearance, structure, color. It can be primary and secondary, that is, appear at the site of previous rashes. The combination of primary and secondary elements determine the picture of the rash in the disease. This may be a reaction to some kind of allergen, or it may turn out that the rash is a sign of a disease. nine0003
Species
It turns out that rashes are of different nature and type. Allocate primary and secondary rashes. Such a rash occurs in a child on the legs and arms:
Allocate primary and secondary rashes. Such a rash occurs in a child on the legs and arms:
- Tubercles - do not have a cavity, are located deep in the dermis, up to 1 cm in diameter. At the same time, the color and texture of the skin is excellent. They can leave scars behind, develop into ulcers.
- Blisters - without a cavity, have a blurred outline and pink color. Appear due to swelling of the papillary dermis. Pass without a trace, itchy. nine0020
- Papules or nodules - no cavity. May or may not be inflamed, discolored. Pass without leaving traces
- Bubbles - have a bottom, a cover, a cavity. After they are opened, erosion can form.
- Pustules or pustules - have pus inside. May be superficial or deep.
- Roseola is irregularly shaped patches of pink. When the skin is stretched, the stain disappears. nine0020
If the rash appears a second time, it may form:
- Scars.
- Abrasions.
- Cracks.
- Scales.
- Erosions.
- Ulcers.
Diagnosis
If a child has a rash on his legs and arms, you should immediately seek help from a pediatrician and a dermatologist. First, the doctor must carefully examine:
- Appearance. nine0019 Form.
- Colour.
- Quantity.
- The nature of the rash.
- The location of the rash is also important.
Next, it turns out:
- Presence or absence of a feverish state.
- What infectious diseases have been transferred.
- What are the hereditary diseases.
- Tendency to allergies.
- Light sensitivity.
As a rule, a rash is not the main disease, but is a symptom of some disease. It acts as a sign that a failure has occurred in the body. To determine the cause of such a manifestation, the doctor prescribes tests. First of all - a blood and urine test. It is also possible to analyze the secretion of abscesses. After examination and analysis, the doctor prescribes treatment. What could be the reasons why a child has a rash on his legs and arms? nine0003
It is also possible to analyze the secretion of abscesses. After examination and analysis, the doctor prescribes treatment. What could be the reasons why a child has a rash on his legs and arms? nine0003
Sources of the problem
For a child's body, a rash is a very important symptom of some diseases, so it is important to consult a doctor. Its causes may be as follows:
- Allergic diseases.
- Infectious.
- Parasitic infections.
- Vascular and blood diseases.
- Violations of hygiene rules.
If the rash accompanies an infectious disease, the body temperature will certainly be elevated. There are other signs, these can be:
- Cough.
- Rhinitis.
- Sore throat.
Let's look at some diseases that are accompanied, in addition to a rash, also by fever.
Rash with fever
When an infection enters the body, its first reaction is fever.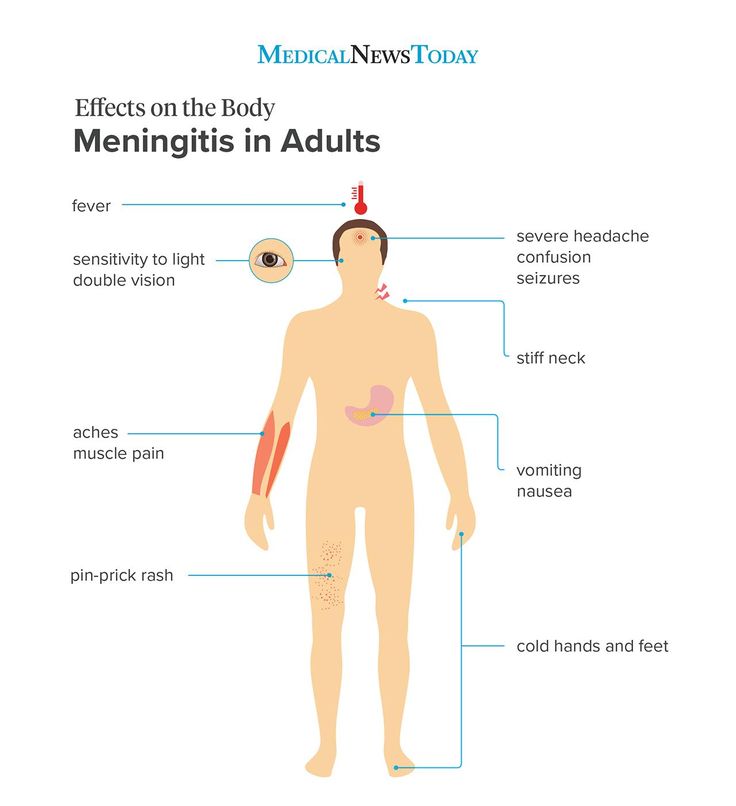 Skin rashes may appear with or without fever. There are several infectious diseases, a sign of which is a rash. nine0003
Skin rashes may appear with or without fever. There are several infectious diseases, a sign of which is a rash. nine0003
This group includes:
- Chicken pox.
- Rubella.
- Scarlet fever.
- Measles.
- Enteroviral infection.
- Meningococcemia.
Each disease is characterized by its own characteristics of the spread of rashes. This is especially true for childhood diseases. Consider which of them causes a rash in a child on the legs and arms, as well as on the body and face.
Windmill
This disease is most common in children. She is not vaccinated. The first sign of this disease is the appearance of red spots, which very quickly turn into blisters. In addition to blisters on the face, head, body, the child also has a rash on the legs and arms. The temperature is elevated, for some time the baby may experience weakness, headache.
If the blister is torn off, scars remain.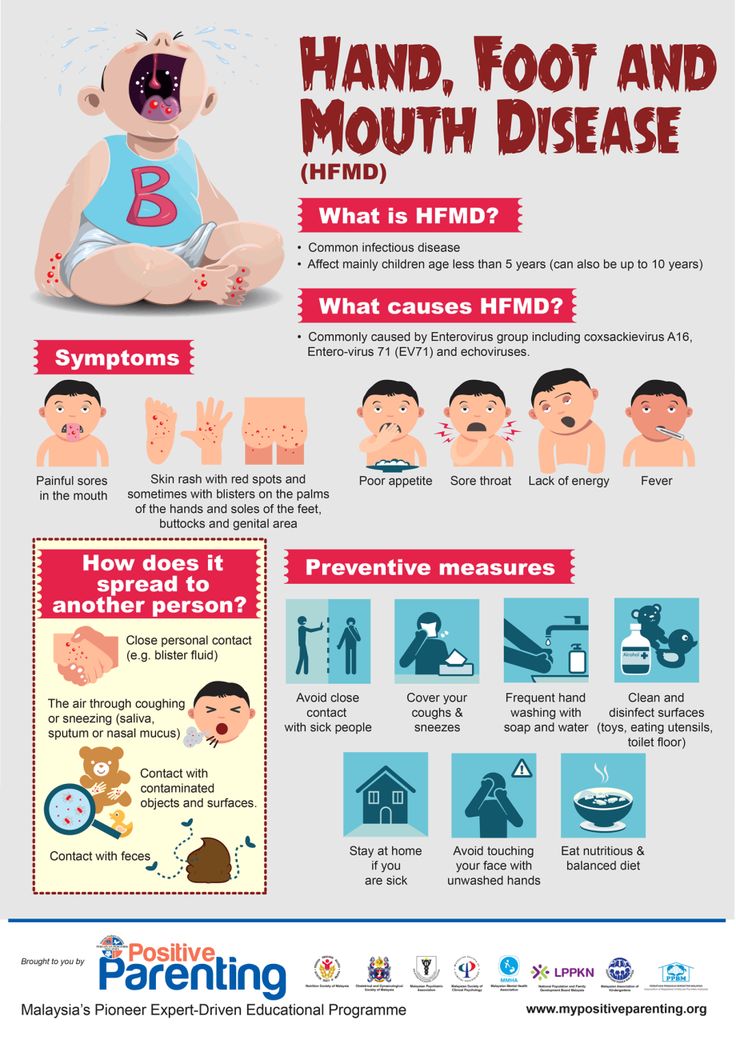 The main problem of this disease is that the rash on the child's arms and legs itches, there is a risk of infection. The doctor may prescribe medications to relieve itching. nine0003
The main problem of this disease is that the rash on the child's arms and legs itches, there is a risk of infection. The doctor may prescribe medications to relieve itching. nine0003
Rubella
This disease comes with fever. In older children, joint pains, general intoxication are possible. Rashes are shown on the 1st day or on the second day. First - on the face, neck, torso, then a small rash spreads in the child on the arms and legs, mainly on the folds. The younger the child, the easier this disease proceeds. However, in adolescents, complications are possible, such as encephalitis, meningoencephalitis. This disease is especially dangerous for pregnant women, fetal malformations are possible. Vaccination is also prohibited for immunocompromised patients. However, rubella is milder than scarlet fever. nine0003
Measles
A dangerous infectious disease, easily transmitted through the air with little contact with the carrier of the infection
There is a vaccination against measles. This disease is accompanied by intoxication of the body. There are symptoms characteristic of a cold - coughing, lacrimation, sneezing. The temperature rises to high values. Rashes begin with the buccal mucosa, then pass to the face, the entire body, to the extremities (in the form of papules that rise above the skin). Dangerous complications on the bronchi, can cause pneumonia. nine0003
This disease is accompanied by intoxication of the body. There are symptoms characteristic of a cold - coughing, lacrimation, sneezing. The temperature rises to high values. Rashes begin with the buccal mucosa, then pass to the face, the entire body, to the extremities (in the form of papules that rise above the skin). Dangerous complications on the bronchi, can cause pneumonia. nine0003
Scarlet fever
This is an infectious disease transmitted by airborne droplets through dirty hands and objects. It starts with a sore throat, chills. Then a small rash appears on the child's arms and legs with fever. Most often in places of bends of arms, legs. Then the rash spreads to the face, neck, torso. The source of the rash is streptococcus. The throat starts to hurt, which is very similar to a viral infection. Language is key to the definition. It will be crimson. As soon as the temperature begins to decrease, lamellar peeling of the skin of the hands and feet begins. With this disease, it is very important to observe bed rest and drinking. Antibiotics are required for treatment. Possible complications in the heart and kidneys. nine0003
With this disease, it is very important to observe bed rest and drinking. Antibiotics are required for treatment. Possible complications in the heart and kidneys. nine0003
Enterovirus infection
Preschool children are susceptible to these diseases. A rash appears on the child's legs and arms without fever. She usually doesn't itch
The child may be healthy, or there may be an increase in temperature to insignificant values within one or two days. This is due to the imperfection, susceptibility of children's skin.
Meningococcemia
This is a very dangerous disease. The temperature rises to high values in a short period of time. A rash appears on the child's legs and arms (does not itch) in the form of irregularly shaped hemorrhages, and is also on the buttocks. If such rashes are detected, an urgent need to call a doctor and determine the child in intensive care. nine0003
Hemorrhagic vasculitis
This disease is characterized by a rash in a child on the arms and legs with fever, mainly in the folds.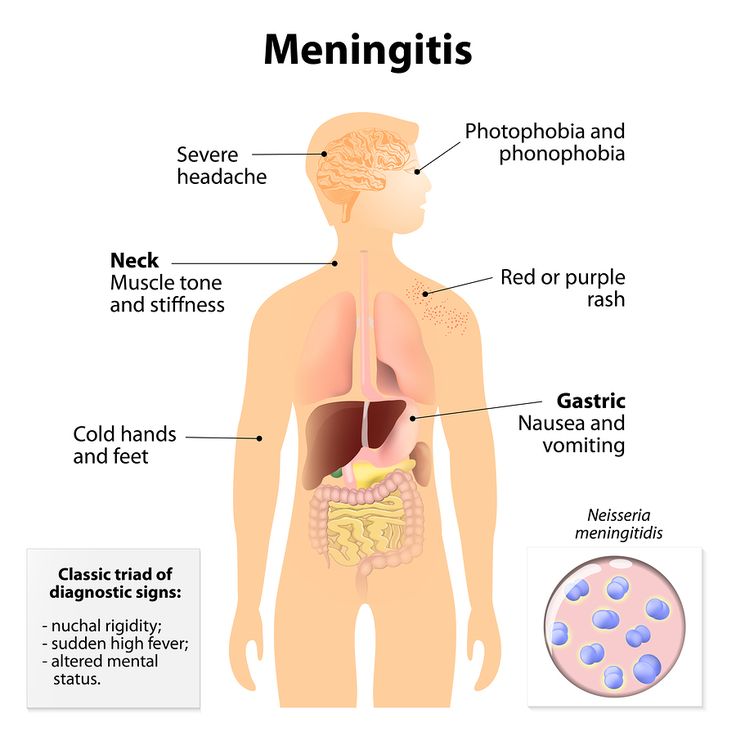 Initially, small blisters or lumps appear, then the rash turns red, takes on the color of rust and completely disappears. It is believed that the disease can be caused by allergies, trauma, and be the result of acute infectious diseases, such as tonsillitis, pharyngitis. Accompanied by fever, joint pain. With a lightning-fast course of this disease, a fatal outcome is possible. It is necessary to carefully consider the treatment. nine0003
Initially, small blisters or lumps appear, then the rash turns red, takes on the color of rust and completely disappears. It is believed that the disease can be caused by allergies, trauma, and be the result of acute infectious diseases, such as tonsillitis, pharyngitis. Accompanied by fever, joint pain. With a lightning-fast course of this disease, a fatal outcome is possible. It is necessary to carefully consider the treatment. nine0003
Rashes of non-infectious origin with itching
There are a number of diseases in which the rashes are very itchy. For example, with scabies, a child develops a rash on the legs and arms without fever, most often on the folds between the fingers. As a rule, it itches a lot, especially at night. Also, in case of helminthiases, rashes itch
The presence of a fungus on the skin in children is one of the causes of rashes in the form of blisters, erosions, red spots. Places of localization of the fungus, as a rule, on the legs, palms, feet, wrists. The rash spreads especially quickly on moist areas of the skin. It can be easily transmitted through contact with an infected object. Especially often infections occur in places where the environment is humid (shower, bathroom). The disease is accompanied by severe itching without fever. nine0003
The rash spreads especially quickly on moist areas of the skin. It can be easily transmitted through contact with an infected object. Especially often infections occur in places where the environment is humid (shower, bathroom). The disease is accompanied by severe itching without fever. nine0003
Small rash without itching
If a child has a small rash on the arms and legs, does not itch, it is possible that pseudotuberculosis is at the initial stage of development. This disease is transmitted by rodents - after contact with things to which they had access. This disease appears in children very rarely, but still it exists.
If a child was born with congenital syphilis, was infected in utero, the rash may appear from time to time without disturbing him. These are papules with a pustular core. Such rashes are not accompanied by itching and fever. Also, a small rash can be the result of a hereditary infectious disease, such as psoriasis. In children under 2 years of age, it is rare, but at an older age, the risk of development, having heredity, is quite possible. It begins with a small rash in the form of dry plaques of a round and oval shape of a red-pink color, peeling is noticeable on top. It spreads over vast areas of the skin, in the area of the knees, elbows, head - this is a characteristic sign of psoriasis. This rash does not itch. In infants, it may come and go, and in adulthood it may come back again. nine0003
It begins with a small rash in the form of dry plaques of a round and oval shape of a red-pink color, peeling is noticeable on top. It spreads over vast areas of the skin, in the area of the knees, elbows, head - this is a characteristic sign of psoriasis. This rash does not itch. In infants, it may come and go, and in adulthood it may come back again. nine0003
Allergic reaction
With allergic dermatitis, in addition to rashes on the face and trunk, a child may have a rash on the legs and arms. Photos clearly demonstrate the manifestation of an allergic reaction. Rashes can be present both on a small area of \u200b\u200bthe skin, and on an extensive one. As a rule, accompanying signs are peeling and severe itching. The body temperature remains within the normal range, intoxication of the body does not occur. Such a reaction is possible on food, household chemicals, drugs. If a child has allergies, you need to be extremely careful with allergens, exclude them from the diet if possible, as there is a risk of Quincke's edema.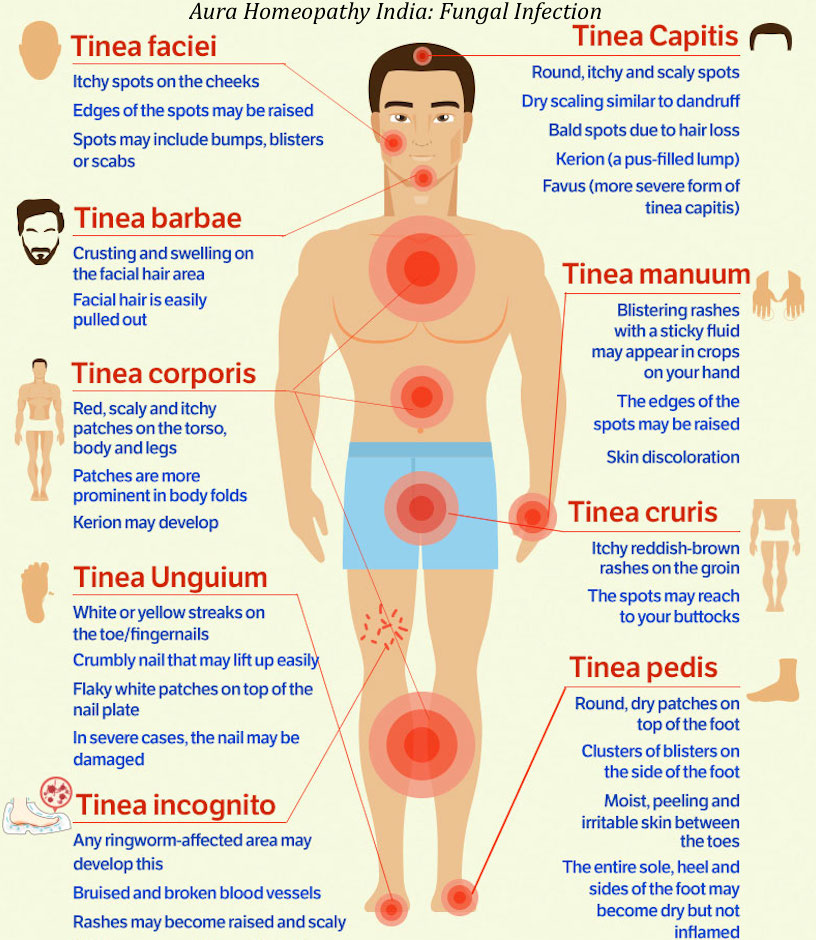 Possible respiratory arrest, swelling of the larynx. nine0003
Possible respiratory arrest, swelling of the larynx. nine0003
Urticaria - a small rash - may be a reaction to temperature factors, cold, sun.
What not to do if a child has a rash
First of all, it is strictly forbidden in situations when you see a rash on your baby's body:
- Squeeze out pustules.
- Break bubbles.
- Treat with brilliant green or other means until examined by a doctor.
- Self-medicate. nine0053
If the rash on the child's arms and legs is itchy, do not let him scratch it. If a rash is detected, it is necessary to limit contact with others, as the disease can be contagious. As we saw earlier, a rash can be an important symptom or result of a disease. An examination by a doctor is required to make the correct diagnosis and prescribe the appropriate treatment in order to exclude possible complications.
Therapy
The treatment of rashes is, first of all, the elimination of the disease that caused them. In infectious diseases, bed rest, antipyretic drugs, antihistamines, and treatment of rashes are recommended. If necessary, antibiotics are prescribed (to exclude the development of side effects). Allergy sufferers should definitely see an allergist. Eliminate allergens from your diet. And you should also follow the doctor's instructions, take antihistamines or glucocorticosteroids. In case of fungal diseases or scabies, observation by a dermatologist is necessary. nine0003
In infectious diseases, bed rest, antipyretic drugs, antihistamines, and treatment of rashes are recommended. If necessary, antibiotics are prescribed (to exclude the development of side effects). Allergy sufferers should definitely see an allergist. Eliminate allergens from your diet. And you should also follow the doctor's instructions, take antihistamines or glucocorticosteroids. In case of fungal diseases or scabies, observation by a dermatologist is necessary. nine0003
Prevention of rashes
Skin in childhood is not yet adapted to the manifestations of the external environment, so it requires special attention and care. First of all, you must follow the rules of hygiene. Parents should make sure that they have all the necessary vaccinations against dangerous diseases. If your baby suffers from allergies, be sure to see an allergist. Proper treatment, observation will help the child outgrow this difficult period. Eliminate allergens from your baby's diet. Strengthen the immune system of the child so that he can easily and without consequences fight diseases. nine0003
Strengthen the immune system of the child so that he can easily and without consequences fight diseases. nine0003
Do not leave a rash, no matter how small, unattended!
Rash in a child on the body, legs, back
We treat children according to the principles of evidence-based medicine: we choose only those diagnostic and treatment methods that have proven their effectiveness. We will never prescribe unnecessary examinations and medicines!
Make an appointment via WhatsApp
Prices Doctors nine0003
The first children's clinic of evidence-based medicine in Moscow
No unnecessary examinations and drugs! We will prescribe only what has proven effective and will help your child.
Treatment according to world standards
We treat children with the same quality as in the best medical centers in the world.
The best team of doctors in Fantasy!
Pediatricians and subspecialists Fantasy - highly experienced doctors, members of professional societies.