Do contractions cause dilation
Stages of labor and what to expect
During labor, the cervix changes from a tightly closed entrance to a fully open exit for the baby.
Looking at a cervix dilation chart can help people to understand what’s happening at each stage of labor.
Each woman experience labor differently. In this article, we discuss in detail how the cervix is likely to change throughout the stages of labor, and what to expect at each stage.
Most of the time, the cervix is a small, tightly closed hole. It prevents anything from getting into or out of the uterus, which helps to protect the baby.
During labor, intense contractions of the uterus help move the baby down and eventually out of the pelvis, and into the vagina. These contractions put pressure on the cervix and cause it to expand slowly. Contractions tend to get stronger, closer together, and more regular as labor progresses.
Most medical guides divide labor into three stages:
- Stage one: early, active, and transition labor.
Contractions begin, the cervix dilates, and the baby moves down in the pelvis. Stage one is complete when the cervix has dilated to 10 centimeters (cm).
- Stage two: The body begins pushing out the baby. During this stage, women often feel a strong urge to push. This stage ends with the birth of the baby.
- Stage three: Contractions push out the placenta. This stage ends with the delivery of the placenta, usually within a few minutes after the birth of the baby.
However, many women in labor may feel that they are experiencing many more stages than this.
Stage one: early labor
In the early stages of labor, the cervix dilates to the following sizes:
- 1 cm, about the size of a cheerio
- 2 cm, the size of a small to medium-sized grape
- 3 cm, the size of a quarter
Late in pregnancy, the cervix may have already dilated several centimeters before a woman experiences any symptoms of labor.
Some women, particularly those who are giving birth for the first time, have difficulty telling whether labor has begun. This is because contractions in early labor are often mild and irregular, growing steadily more intense as the labor progresses and the cervix dilates.
This increase in intensity may take just a few hours or can take many days. Knowing whether this is actual labor can help people to prepare.
During true labor, a person’s contractions:
- are not just on one side of the body
- begin at the top of the uterus, and feel like they are pushing down
- get more intense and regular with time
- do not stop with rest or taking a warm shower
Some women may benefit from resting or eating a snack at this stage to ensure they have enough energy for the more tiring stages ahead.
Stage one: active labor
During the active stage of labor, the cervix dilates to the following sizes:
- 4 cm, the size of a small cookie, such as an Oreo
- 5 cm, the size of a mandarin orange
- 6 cm, the size of a small avocado or the top of a soda can
- 7 cm, the size of a tomato
Labor contractions become more intense and regular during active labor.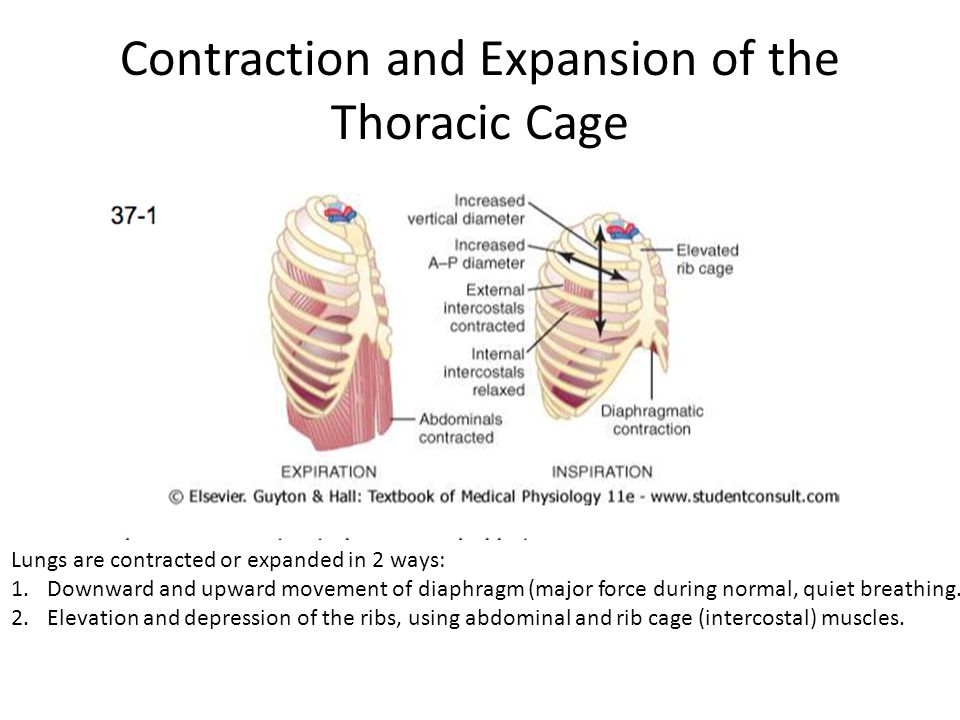 Many women find that the main characteristic of active labor is that the contractions are extremely painful rather than uncomfortable.
Many women find that the main characteristic of active labor is that the contractions are extremely painful rather than uncomfortable.
At this stage of labor, some women may choose medication, such as an epidural to cope with the pain. Others prefer to manage the pain naturally. Changing positions, moving, and remaining hydrated can help with the pain of active labor.
Stage one: transition phase
During the transition phase of labor, the cervix dilates to the following sizes:
- 8 cm, the size of an apple
- 9 cm, the size of a donut
- 10 cm, the size of a large bagel
For many women, transition is the most challenging stage. However, it is also the shortest. Some people begin feeling an urge to push during the transition stage. It is also common to feel overwhelmed, hopeless, or unable to cope with the pain. Some women vomit.
Some women find that the coping strategies that worked well in the earlier stages of labor are no longer useful. Transition tends to be short and is a sign that the baby will soon arrive. Moving, changing positions, and visualization exercises can help.
Transition tends to be short and is a sign that the baby will soon arrive. Moving, changing positions, and visualization exercises can help.
The cervix continues dilating during transition, and transition ends when the cervix has fully dilated.
Stage two: full dilation and pushing
Once the cervix has reached 10 cm, it is time to push the baby out. Contractions continue but also produce a strong urge to push. This urge might feel like an intense need to have a bowel movement.
This stage can last anywhere from a few minutes to a few hours. It is often longer for those giving birth for the first time.
Historically, doctors told women to push according to a schedule, to count to 10, and to remain on their backs. Today, the advice is very different, and research says it is safe for women to push according to their body’s cues and for as long as feels comfortable.
Pushing from a standing or squatting position may also help speed things along. Allowing people to push from a range of positions gives the medical staff better access to the woman and baby should they need to assist with the delivery for any reason.
As a woman delivers the baby, she may feel an intense burning and stretching as her vagina and perineum stretch to accommodate the baby. This sensation typically lasts just a few minutes, though some women tear during this process.
Stage three: after the birth
Share on PinterestAfter delivery, the cervix will start to contract to its previous size.
A few minutes after the birth, a woman may experience weaker contractions. After a contraction or two, the body should expel the placenta.
If the body does not entirely expel the placenta, a doctor or midwife may have to help deliver it. Sometimes, they will give a woman an injection of synthetic oxytocin to speed up delivery and prevent excessive bleeding.
Shortly after delivery, the cervix begins contracting back down to its previous size. This process can take several days to several weeks.
As the uterus and cervix shrink, many women will feel some contractions. Most women bleed for several weeks after giving birth.
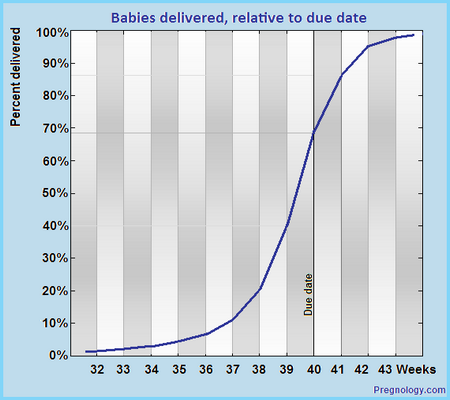
Labor is different for each woman. It typically lasts longer with a first birth, but the length and type of labor vary greatly between individuals.
Some people experience labor that consists of a weaker type of contraction for days or weeks before giving birth. Others give birth in a matter of minutes, while some labors take days. Most fall somewhere in the middle.
Labor often starts slowly, becoming progressively more intense. It may also start and stop, or slow during moments of stress or intrusion.
Visualizing the cervix expanding might help some people understand the source of labor pain, offering a sense of control and deeper insight into the processes of labor.
Signs, Progression & What To Expect
What to expect during labor and delivery.How does labor work?
As your pregnancy begins to wrap up, your body will prepare for labor and delivery.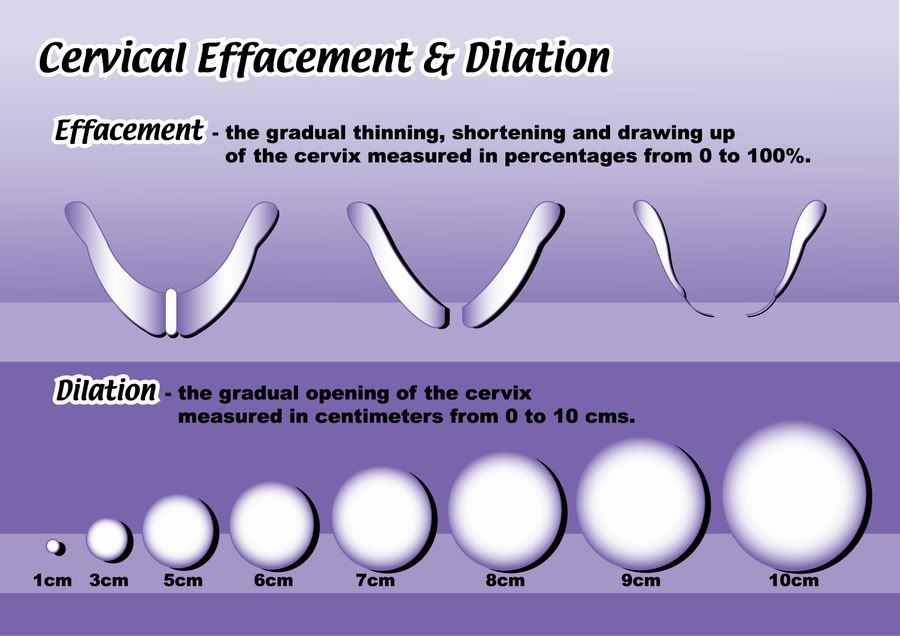 This is the process through which your baby will be born. Labor is often different for each person. Some have quick labors and some long, difficult labors. Other people may even experience labor that stalls or stops, leading to medical intervention.
This is the process through which your baby will be born. Labor is often different for each person. Some have quick labors and some long, difficult labors. Other people may even experience labor that stalls or stops, leading to medical intervention.
Early labor
The average labor lasts 12 to 24 hours for a first birth and is typically shorter (eight to 10 hours) for other births. Throughout this time, you’ll experience three stages of labor. The first stage of labor is usually the longest and it ranges from when you first go into labor until your cervix is open. The beginning of this stage is called early labor. Early labor is described as dilating from 0 to 6 centimeters.
Active labor
As you progress and your contractions become stronger, you’ll move into the second part of the first stage of labor called active labor. Active labor is dilating from 6 to 8 centimeters and then transitioning into the second stage as you dilate 8 to 10 centimeters. Your contractions will become even stronger during active labor and your cervix will open up quickly. The second stage of labor is when you push. This is the phase of your labor when you will actually give birth to your baby.
The second stage of labor is when you push. This is the phase of your labor when you will actually give birth to your baby.
Afterbirth
The third stage is the point when you deliver the placenta. This is also called afterbirth.
During these stages, your body prepares for childbirth by going through dilation and effacement.
- Dilation: This is a process where your cervix stretches and opens to make way for your baby’s birth. Dilation is measured from 1 to 10 centimeters. Your provider will do a vaginal exam to check how dilated you are throughout your labor. You’ll be 10 centimeters dilated in the second stage of labor for the delivery of your baby.
- Effacement: The cervix not only stretches during labor but it also becomes thinner. The shortening and thinning of your cervix are measured in percentages. You’ll progress from 0% to 100% effacement during your labor.
Think of your cervix as a round doorway that needs to stretch outward and get thinner before your baby can pass through it. This stretching and thinning are caused by contractions. Contractions can be described in a variety of ways ranging from uncomfortable, period-like cramps to a painful tightening of your abdomen. You might also feel a dull ache in your back and lower abdomen, as well as pressure in your pelvis.
This stretching and thinning are caused by contractions. Contractions can be described in a variety of ways ranging from uncomfortable, period-like cramps to a painful tightening of your abdomen. You might also feel a dull ache in your back and lower abdomen, as well as pressure in your pelvis.
When you have a contraction, it’s actually the muscles of your uterus tightening at regular intervals to dilate and efface (open and thin) your cervix. During contractions, your abdomen becomes hard. Between contractions, your uterus relaxes and your abdomen becomes soft. Even though they can be painful, each contraction helps move you forward through your labor.
How will I know I’m in labor?
It can be difficult to know when you’re in true labor. First-time parents, in particular, might mistake other symptoms or irregular practice contractions (called Braxton Hicks contractions) for true labor. True labor has a pattern and progresses steadily over time.
When you’re in true labor, you’ll notice a pattern in your contractions. Instead of the irregular Braxton Hicks contractions you might have felt during your pregnancy that showed up and then went away randomly, these contractions will keep coming for an extended period of time. There are three things you’ll want to look for when you are in true labor.
Instead of the irregular Braxton Hicks contractions you might have felt during your pregnancy that showed up and then went away randomly, these contractions will keep coming for an extended period of time. There are three things you’ll want to look for when you are in true labor.
- Frequency: How often are your contractions happening? Keep track of them with a journal or labor app on your phone to make sure they're coming at regular intervals.
- Duration: How long are each of your contractions? As your labor continues, your contractions will last longer and longer. Use a stopwatch, watch a clock or keep the timer on your phone handy so you can record the length of each contraction.
- Intensity: Are your contractions getting stronger? Contractions can get stronger and you might feel them more intensely as you move through the stages of labor. Keep track of how your contractions feel over time.
Are there any signs that I will go into labor soon?
Many women have several pre-labor signs that might hint that labor will start soon. These signs of labor include:
These signs of labor include:
- Backaches.
- Diarrhea.
- Weight loss.
- Nesting (cleaning and organizing your home).
No one knows for sure what causes labor to start, but several hormonal and physical changes may point to the beginning of labor.
What are Braxton Hicks contractions?
Often called practice contractions, Braxton Hicks are irregular contractions that don’t cause cervical change. Think of them as a test run for the real thing. They can start happening at the end of your pregnancy and can startle people into thinking they’re in labor. This is called false labor.
A Braxton Hicks contraction will feel like a sudden, sharp tightening of your abdominal muscles. Even though this is very similar to how a contraction feels, Braxton Hicks contractions don’t follow a pattern or progress over time. They may also stop when you lay down or relax. When you start to experience these practice contractions, keep track of them. Writing them down is the best way to tell the difference between true and false labor.
What is lightening?
Lightening is the process where your baby settles or lowers into your pelvis. This can happen a few weeks or a few hours before labor. When this happens, you may experience some increased lower pelvic pressure. Because your uterus rests on your bladder more after lightening, you might also feel the need to urinate more frequently. You might notice that you’re not as short of breath once your baby drops.
What’s the mucus plug and what does it mean when it falls out?
During pregnancy, a thick piece of mucus called a plug blocks the cervical opening. This plug keeps your uterus closed off from the birth canal and the outside of your body and prevents bacteria from traveling into your uterus. When your cervix begins to soften, thin, and open, the mucus is expelled into your vagina. Not every mucus plug will look the same. Possible colors of the mucus plug can include:
- Clear.
- Pink.
- Slightly bloody.
Labor could start shortly after you lose your mucus plug or it could begin several weeks later.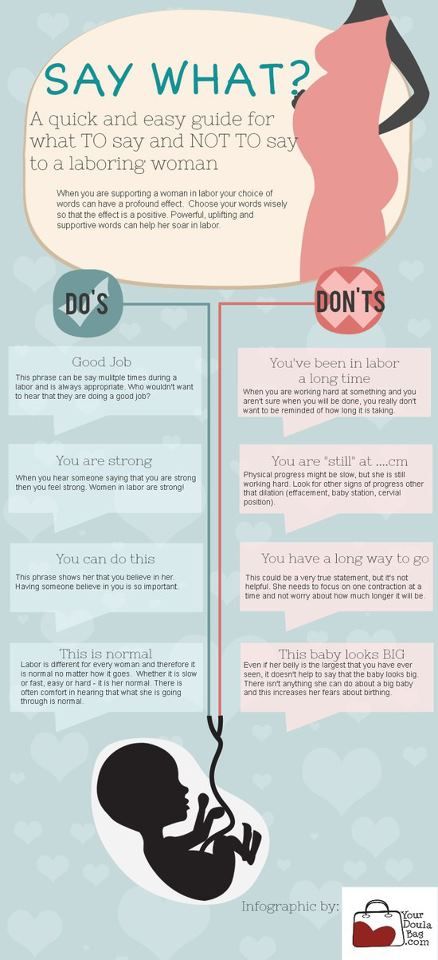
How do I time my contractions?
Once you’re in labor, it’s important to keep track of your contractions. Your healthcare provider will need to know how long your contractions are lasting (duration), how often they’re happening (frequency) and how intense they are. When you’re timing your contractions, you will want to have a way to record each one – pen and paper or through an app on your phone – and a timer or clock. Make sure you keep track of each contraction from start to end, as well as the time between each contraction. This second measurement will help your provider know the frequency of your contractions.
It can be difficult to record the intensity of your contractions. This can really vary from person to person. Often, an easy way to keep track of the intensity of your contractions is to record when you cannot walk, talk or laugh during contractions.
Is there anything I can do to cope with contractions?
As you approach the end of your pregnancy, it’s a good idea to talk to your healthcare provider about different ways to deal with pain and discomfort during labor. There are several options your provider will discuss with you to relieve pain.
There are several options your provider will discuss with you to relieve pain.
There are also ways to deal with the discomforts of labor at home or without medication, including:
- Distract yourself by taking a walk, going shopping or watching a movie.
- Soak in a warm tub or take a warm shower. Make sure to ask your healthcare provider if you should take a tub bath if your bag of water has broken.
- Sit on a birth ball.
- Listen to music.
- Dim the lights.
- Use aromatherapy.
- Get a massage.
- Stay in an upright position. This can help with the descent and rotation of your baby.
- Try to sleep if it’s evening. You’ll want to store up your energy before active labor and delivery.
How will I know when my water breaks?
You may be familiar with the common phrase “my water broke.” This is actually the rupturing of your amniotic membrane. During pregnancy, your baby is inside a fluid-filled sac, also called your bag of water. When this membrane breaks, you might feel a sudden gush or trickle of fluid. Like many parts of labor and childbirth, this experience can be different for each person. The fluid is usually odorless and may look clear or straw-colored.
When this membrane breaks, you might feel a sudden gush or trickle of fluid. Like many parts of labor and childbirth, this experience can be different for each person. The fluid is usually odorless and may look clear or straw-colored.
Unlike urine leakage that some pregnant women experience, this won’t stop. The amniotic fluid will often continue to leak.
If your water breaks, call your healthcare provider. Let your provider know what time your water broke, the amount (trickle or gush), the color of the fluid and the odor. Don't use tampons if your water has broken. Your labor might start right after your water breaks. Some women are already in labor when their water breaks while others don’t experience the first stage of labor for a while after their water breaks.
When should I call my healthcare provider or go to the hospital?
If you ever have any questions, it’s always a good idea to call your healthcare provider. Your provider can answer any questions you have about true labor versus false labor and discuss how you’re feeling. When you start to notice that you’re having regular contractions, call your provider to talk about when you should go to the hospital. Some women are able to stay home throughout early labor, while others may need to come in sooner.
When you start to notice that you’re having regular contractions, call your provider to talk about when you should go to the hospital. Some women are able to stay home throughout early labor, while others may need to come in sooner.
You should also call your healthcare provider if you:
- Think your water has broken. This could be a sudden gush of fluid or a trickle of fluid that leaks steadily.
- Are bleeding (more than spotting).
- Experience contractions that are very uncomfortable and have been coming every five minutes, lasting for one minute and have been like this for one hour.
What happens when I get to the hospital?
When you get to the hospital, you will check in at the labor and delivery desk. Most people will be seen in a triage room first. This is part of the admission process. It’s usually recommended that you only bring one person with you to the triage room.
From the triage room, you will be taken to the labor, delivery and recovery (LDR) room. You’ll be asked to wear a hospital gown. Your pulse, blood pressure and temperature will be checked. An external fetal monitor will be placed on your abdomen for a short time to check for uterine contractions and measure your baby’s heart rate. Your healthcare provider will also examine your cervix to see how far labor has progressed. An intravenous (IV) line might be placed into a vein in your arm to deliver fluids and medications.
You’ll be asked to wear a hospital gown. Your pulse, blood pressure and temperature will be checked. An external fetal monitor will be placed on your abdomen for a short time to check for uterine contractions and measure your baby’s heart rate. Your healthcare provider will also examine your cervix to see how far labor has progressed. An intravenous (IV) line might be placed into a vein in your arm to deliver fluids and medications.
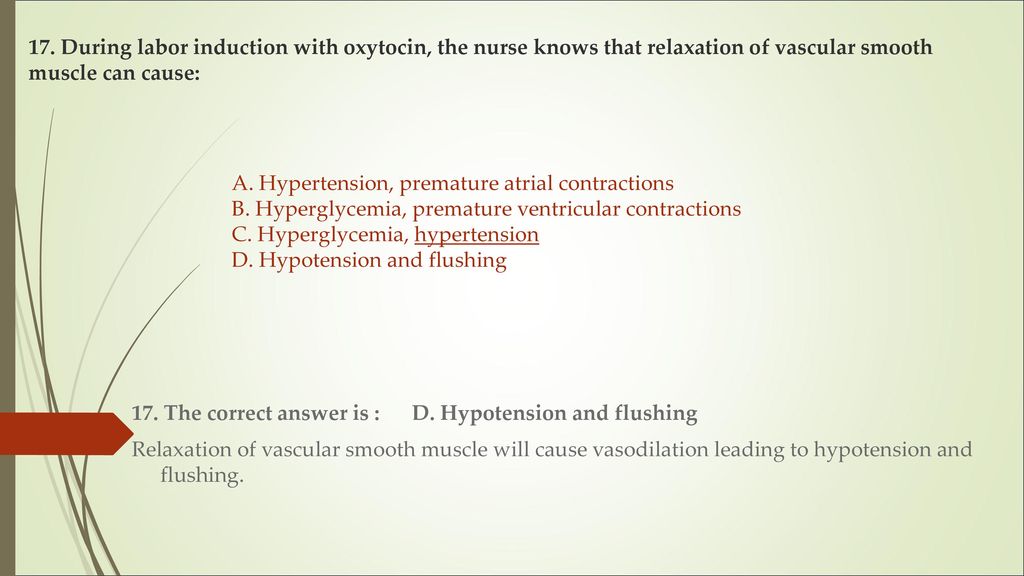
What does it mean to have labor induced?
Labor doesn’t always start naturally or progress as it should. In these cases, your provider might talk to you about inducing labor. This is a medical procedure where labor is started by your healthcare provider. This could happen if you:
- Are past your due date.
- Have health complications like high blood pressure, preeclampsia, infection or diabetes.
- Had your water break but labor didn’t start.
- Have low levels of amniotic fluid.
Your labor can be advanced or induced in several ways. Your provider will advise you about the best and safest option depending on your health. Inducing labor can be done by using:
Your provider will advise you about the best and safest option depending on your health. Inducing labor can be done by using:
- Medications (oxytocin) given through an IV (directly into your vein).
- Breaking your amniotic sac (water).
- Separating the amniotic membrane (the sac of fluid the baby is inside within your uterus) from your uterine wall. This is also called sweeping the membrane.
- Softening your cervix and encouraging it to open with a medication that can be placed directly in your vagina.
Labor induction can take longer than spontaneous labor because the cervical ripening process takes time.
What are the different types of delivery?
There are two main types of delivery: vaginal and cesarean section (C-section). During vaginal birth, your baby will pass naturally through the birth canal. A C-section is a surgical procedure where your provider makes an incision (cut) in your abdomen and delivers the baby in an operating room. Vaginal delivery is the most common type of birth. However, sometimes you might need a C-section for a variety of reasons, including:
Vaginal delivery is the most common type of birth. However, sometimes you might need a C-section for a variety of reasons, including:
- If your baby is not in the head-down position.
- If your baby is too large to naturally pass through your pelvis.
- If your baby is in distress.
- If the placenta blocks your cervix (a condition called placenta previa).
- If you have health issues or complications that make a C-section the safest option.
- If there’s an emergency situation that requires your baby to be delivered quickly.
In many cases, a cesarean delivery is not determined until after labor begins.
How long will I be in the hospital?
The length of your hospital stay can depend on the hospital where you deliver your baby and the type of delivery you have. Typically, you will stay in the hospital longer if you have a C-section delivery because it's a surgical procedure. You may also need to stay in the hospital for a longer period of time if you experience any complications or health issues during your delivery.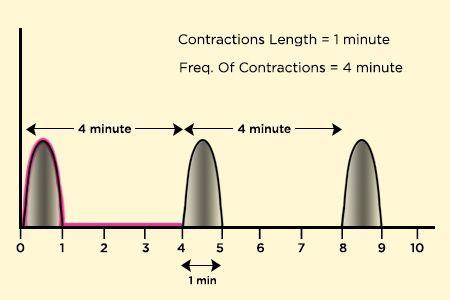
A note from Cleveland Clinic:
You're bound to a lot of feelings as you prepare to deliver your baby. It's normal to feel both excited and nervous. Discussing the signs and symptoms with your healthcare provider can help you know what to expect. Your partner and healthcare team are here to support you and will help you remain as comfortable as possible through the delivery process.
Thermal Actions on Structures - Part 2: Thermomechanics
See beginning: Thermal Actions on Structures - Part 1: Design Codes
Introduction
This part discusses the theoretical basis of thermal actions on structures from the point of view of classical mechanics of materials.
In the previous part 1, the features of taking into account temperature effects in the design of building structures according to the Russian code of rules SP 20.13330.2011 (SNiP 2.01.07-85) are considered. nine0003
Part 3 presents examples of temperature effects on simple structures - beams with different fastening conditions.
1. Theoretical foundations of temperature effects on materials
1.1. Thermal expansion-contraction
Changes in temperature cause structural materials to expand or contract, resulting in thermal deformations and thermal stresses. A simple illustration of thermal expansion is shown in Figure 2.1, where the block of material is not fixed and is therefore free to expand [1]. nine0003
Figure 2.1 - A bar of material under the influence of an increase in temperature [1]
When this bar is heated, each element of the material undergoes thermal deformations in all directions, and, accordingly, the dimensions of the bar also increase in all directions. If we take angle A as the reference point and give side AB the opportunity to maintain its original direction, then the bar will take the form shown by dashed lines.
For most construction materials thermal deformation 0028 T is a proportional temperature change ΔT , that is,
ε T = α · ΔT , 9003 9000 (1)
9000 9000 ( - a property of the material, which is called the coefficient of thermal expansion. According to the “sign agreement” adopted in the world, thermal expansion is considered positive, and thermal contraction is negative [1, 2]. nine0003
According to the “sign agreement” adopted in the world, thermal expansion is considered positive, and thermal contraction is negative [1, 2]. nine0003
1.2. Coefficient of Thermal Expansion of Structural Materials
Since strain is a dimensionless quantity, this coefficient of thermal expansion has the dimension inverse to temperature change. In the SI system, the dimension α T can be expressed as 1 / K (the reciprocal of the SI unit Kelvin ) or 1 / ºС (the reciprocal of Celsius). Value α T is the same in both cases, since the temperature change is numerically the same in both Kelvin and Celsius.
It is convenient to represent the value of the coefficient of thermal expansion in units of 10 -6 /ºС or µm/m·ºС. The latter view is especially convenient - it clearly shows how many micrometers one meter of material lengthens with an increase in temperature by one degree of temperature. nine0003
nine0003
Information on the thermal expansion coefficients of some structural materials is presented in Table 1.
Table 2.1 - Thermal expansion coefficient of structural materials [1]
1.3. Thermal expansion coefficient of aluminum alloys
Thermal expansion coefficients of the main aluminum alloys used in construction are shown in Table 2.
Table 2.2 - Thermal expansion coefficient of building aluminum alloys [3]
Table 2.2 shows that the coefficients of thermal expansion of various aluminum alloys differ slightly. Therefore, in the set of rules SP 128.13330.2012 (SNIP 2.03.06-85) for the calculation of aluminum structures in the temperature range from minus 70 ºС to 100 ºС, for all aluminum alloys used in construction, a thermal expansion coefficient of 0.23 10 -4 is used 1/ºС [4]. In the European standard EN 1991-1-5, the value of the calculated coefficient of thermal expansion is 24 10 -6 1/ºС [5].
1.4. Thermal stresses
To demonstrate the relative importance of thermal stresses, thermal stresses can be compared with the stresses that occur during force loading [1]. Suppose we have a beam that is loaded with forces in the axial direction with longitudinal deformations, which are given by the equation0027 E - modulus of elasticity. Further suppose we have an identical bar that is subject to a temperature change of ΔT . This means that this bar has temperature deformations according to equation (1). The equation of these two types of deformations gives the equation
Calculate axial stress σ, which gives the same deformations as the change in temperature ΔT in aluminum alloy rods and building (low carbon) steel with an increase in their temperature by 50 ºС.
for aluminum rod ( α = 23 · 10 6 , E = 70000 N/mm 2 ):
σ = 70000 · 23 · 10 -6 · 50 = 80. 5.5.5.5 N/mm 2
5.5.5.5 N/mm 2
For mild steel rod ( α = 12
Note the well-known fact that with the same change in temperature, the temperature stresses in an aluminum rod are only 2/3 of the temperature stresses in a steel rod. This happens because the magnitude of thermal stresses depends on the product of the modulus of elasticity and the coefficient of thermal expansion (see formula (3)). Therefore, although the coefficient of thermal expansion of aluminum is twice that of steel, but the modulus of elasticity of aluminum is three times less than that of steel. nine0003
As can be seen from the above calculations, thermal stresses can reach values comparable to stresses from mechanical loads. Therefore, thermal effects on building structures must be taken into account along with other loads, as required by regulatory documents [4, 5].
1.5. Temperature displacements
Let's return to the bar of material shown in Figure 1 [1]. We assume that the bar material is homogeneous and isotropic, that is, the mechanical properties of the bar material are the same throughout its entire volume.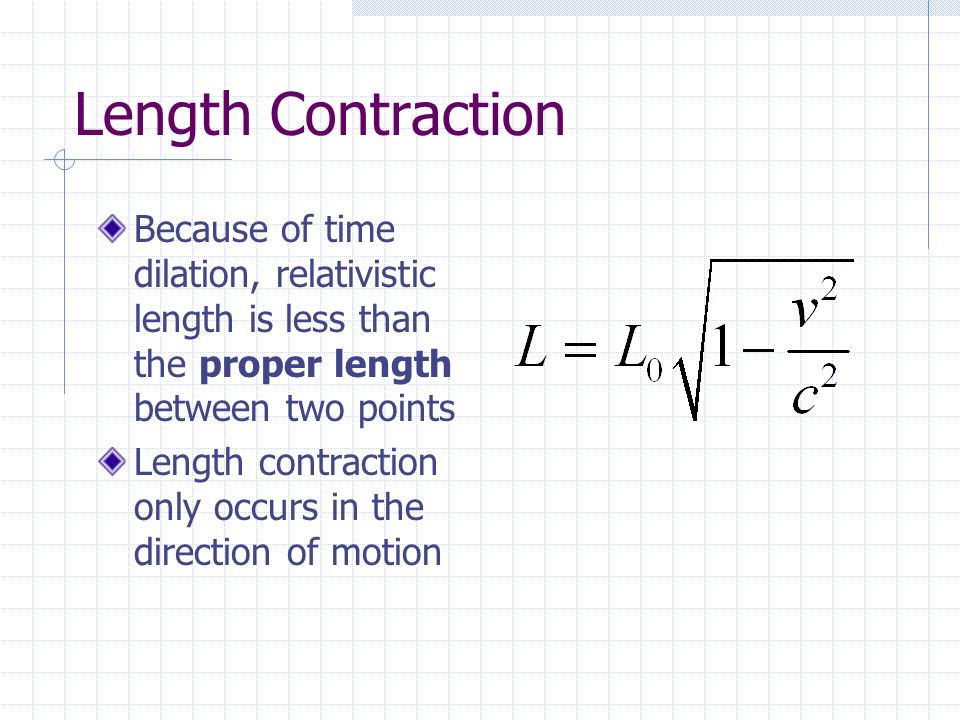 In addition, we assume that the change in temperature ΔT is homogeneous, i.e. the same, throughout the bar. Under these conditions, we can calculate the increase in any size of the bar by multiplying the original size by the thermal deformation. For example, if one of the size of the bar is L, then this size increases by
In addition, we assume that the change in temperature ΔT is homogeneous, i.e. the same, throughout the bar. Under these conditions, we can calculate the increase in any size of the bar by multiplying the original size by the thermal deformation. For example, if one of the size of the bar is L, then this size increases by
Δ T = ε T · L α · δT 27 · 0 · 0 L (4)
Equation (4) can be used to calculate changes in the lengths of structural members after uniform heating, such as the elongation of a prismatic bar in Figure 2.2. The transverse dimensions of the bar will also change, but these changes are not shown in figure 2.2, since they usually do not affect the axial forces that are transmitted by this bar.
Figure 2.2 - Increase in the length of the prismatic rod
as a result of a uniform increase in temperature (equation (4)) [1]
Example.
Let us estimate the elongation of loose aluminum and steel rods 3 m long with an increase in their temperature by 50 ºС.
for aluminum rod:
Δ T = α · ΔT · L = 23 · 10 -6 · 50 · 3000 · 3000 · 3000 · 3000 · 3000 · 3000 · 3000 · 3000
For mild steel rod:
δ T = α ΔT L = 12 10 -6 50 3000 = 1.8 mm
allowed it to expand or contract completely freely. Such conditions arise, for example, when an object lies on a smooth surface on which there is no friction [1]. In such cases, uniform heating of the entire object as a whole does not cause stresses, although non-uniform temperature changes can cause internal thermal stresses. However, many structures have supports that prevent free expansion and contraction of their dimensions. Therefore, thermal stresses develop in them even if the temperature change is uniform throughout the structure. nine0003
nine0003
1.6. Thermal deformations in statically determinate structures
Let's consider the ABC truss of two rods shown in Figure 2.3. Let us assume that the temperature of the rod AB has changed by ΔТ 1 , and that of the rod BC - by ΔТ 2 . Since this truss is statically determinate, both bars can freely lengthen or shorten, resulting in movement of connection B. However, in this case, there are no thermal stresses in the bars, as well as reactions in the supports. nine0003
Figure 2.3 - Statistically determined truss
with a uniform temperature change in each element
This conclusion is true in general for all statically determined structures, namely: temperature deformations (and corresponding changes in the lengths of elements) cause a uniform temperature change in structural elements without the occurrence of corresponding thermal stresses [1, 2].
1.7. Temperature deformations in statically indeterminate structures
Statically indeterminate structures are structures in which the number of reactions exceeds the number of static equilibrium equations. Unlike statically determinate structures, deflections are taken into account in the calculation of such structures [1, 2].
Unlike statically determinate structures, deflections are taken into account in the calculation of such structures [1, 2].
In a statically indeterminate design, thermal stresses may or may not occur, depending on the design features and the characteristics of temperature changes. To illustrate some of these possibilities, consider the statically indeterminate farm shown in Figure 2.4. nine0003
Figure 2.4 - Static indeterminate truss
under the influence of temperature changes
Supports of this design allow node D to move horizontally. Therefore, when the entire truss is uniformly heated, there is no thermal stress in it. All elements increase in length in proportion to their original lengths, and the entire truss as a whole becomes slightly larger in size.
However, if some of the rods are heated and others are not, then thermal stresses arise, since the statically indeterminate arrangement of the rods prevents their free expansion. nine0003
nine0003
Conclusion
1) A change in the temperature of structural elements causes thermal deformations in them. Thermal stresses occur only in statically indeterminate structures.
2) Homogeneous heating of an aluminum rod by 50 ºС is capable of causing significant thermal stresses when the ends of the rod are rigidly fixed. With this heating, the elongation of the rod with free ends is 3.5 mm.
See end:
Thermal effects on structures - Part 3: Theory and examples
Sources:
1. James M. Gere & Barry J. Goodno - Mechanics of Materials, 2009
3. Aluminum and Aluminum Alloys / ed. J.R. Davis, ASM International, 1993
4. SP 128.13330.2012 (SNIP 2.03.06-85) Aluminum structures
5. EN 1991-1-5 Eurocode 1: Actions on structures. Part 1-5. Main impacts. Temperature effects
Prepared by Aluk staff
What is varicose veins
08/13/2020
One of the most common diseases in phlebology is varicose veins.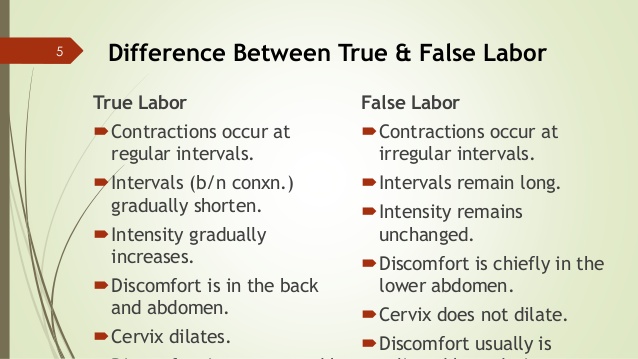
"Good" (saturated with oxygen and nutrients) blood from the heart comes to the legs through the arteries. Further, all cells of the skin, bones, muscles of the legs take all the useful substances from the arterial blood (this process occurs in the capillaries) and give it all the used (waste) waste, and it is this blood that then enters the veins. nine0003
Difference between arterial and venous blood
The veins contain used, waste blood containing, so to speak, “waste”. This blood must go through the veins from the legs upwards, for purification – to the kidneys, liver, lungs. That is, THE MAIN FUNCTION OF THE VEINS IS THE PUMPING OF THE USED BLOOD FROM THE LEGS TO THE TRUNK. But the problem is that when the patient is standing upright, the waste blood through the veins goes against gravity, and this is a very complicated process. Blood is pumped by the heart and lungs, which are located very high from, for example, the feet.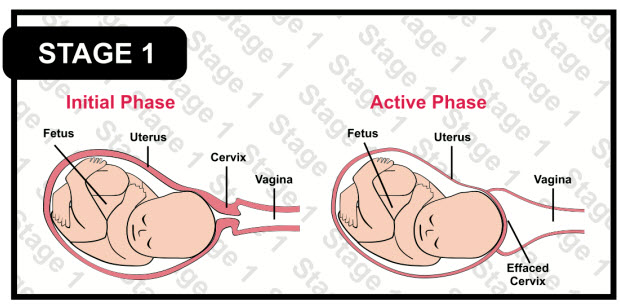 What other mechanisms help blood to rise? Firstly, these are the calf muscles, inside which there are deep popliteal veins with their tributaries. During the contraction of the muscles of the legs, the popliteal veins are compressed, providing additional "blowing" of blood, therefore, with varicose veins, walking and swimming are useful and, on the contrary, it is harmful to stand in one place for a long time. nine0003
What other mechanisms help blood to rise? Firstly, these are the calf muscles, inside which there are deep popliteal veins with their tributaries. During the contraction of the muscles of the legs, the popliteal veins are compressed, providing additional "blowing" of blood, therefore, with varicose veins, walking and swimming are useful and, on the contrary, it is harmful to stand in one place for a long time. nine0003
The work of the calf "venous pump" of the muscles of the legs
But, no matter how well the pump system works - the blood during pauses (or standing on the legs without movement) should have flowed back, but this does not happen. Why? Because here the following mechanism is activated. It turns out that all veins have valves that prevent the reverse flow of blood (flowing down). Here they are in the picture. On the left, normal valves are drawn, which close when the blood flows back. nine0003
And in the figure on the right - dilated (varicose) veins in which, due to overstretching or inflammation of the vein wall, the valves stopped working and as a result, the used blood containing harmful substances through such veins goes back down to the legs, creating an excessive concentration of harmful substances in tissues and muscles.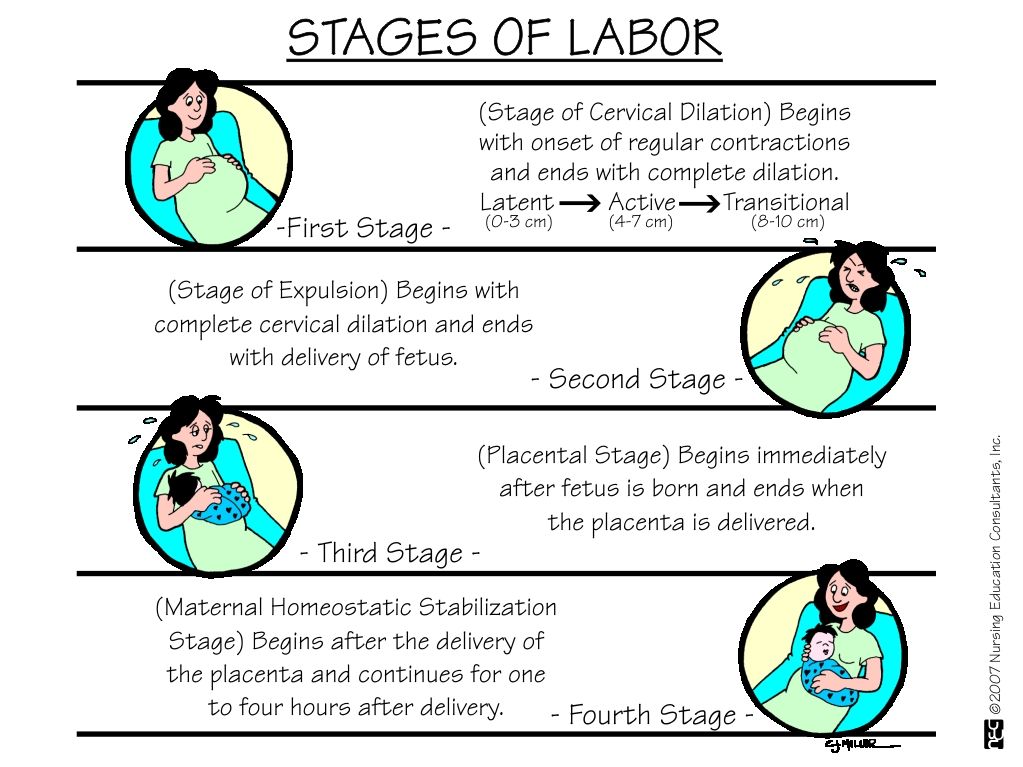 This leads to complaints typical of varicose veins - a feeling of fullness in the legs (impaired blood outflow and excess fluid in the leg), itching (irritation of skin receptors by cell waste), discomfort, a feeling of heaviness, venous pain, a feeling of "goosebumps", burning, cramps (muscle spasm), feeling of heaviness in the legs. Outwardly, this can be manifested by swelling of the legs, swelling of the veins, increased vascular pattern, cyanosis of the skin, etc. In the initial stages of varicose veins, symptoms appear only with prolonged exertion or in the evening. Then they begin to repeat themselves more and more often. Finally, they become almost constant or appear with a slight load. Puffiness does not go away in the morning. The color of the skin in the area of varicose veins becomes reddish at first, then dark, indicating the development of trophic eczema - skin damage that may become irreversible. Long-term edema and eczema can eventually lead to the development of a trophic ulcer.
This leads to complaints typical of varicose veins - a feeling of fullness in the legs (impaired blood outflow and excess fluid in the leg), itching (irritation of skin receptors by cell waste), discomfort, a feeling of heaviness, venous pain, a feeling of "goosebumps", burning, cramps (muscle spasm), feeling of heaviness in the legs. Outwardly, this can be manifested by swelling of the legs, swelling of the veins, increased vascular pattern, cyanosis of the skin, etc. In the initial stages of varicose veins, symptoms appear only with prolonged exertion or in the evening. Then they begin to repeat themselves more and more often. Finally, they become almost constant or appear with a slight load. Puffiness does not go away in the morning. The color of the skin in the area of varicose veins becomes reddish at first, then dark, indicating the development of trophic eczema - skin damage that may become irreversible. Long-term edema and eczema can eventually lead to the development of a trophic ulcer.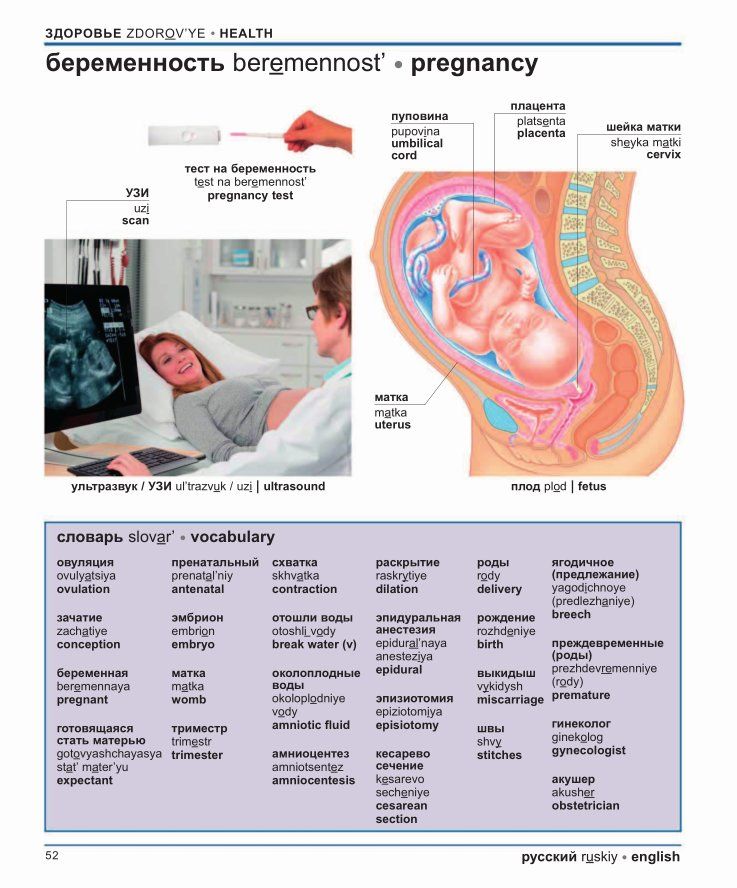 At this stage, the treatment of venous pathology is very difficult and in some cases may not lead to complete healing, but only to maintaining the situation in a relatively stable state. nine0003
At this stage, the treatment of venous pathology is very difficult and in some cases may not lead to complete healing, but only to maintaining the situation in a relatively stable state. nine0003
What is varicose veins
So, what is varicose veins - this is an excessive expansion (overstretching) of some veins with DISTURBANCE OF THEIR FUNCTION. That is, through the varicose vein, the used blood does not flow up to the torso for cleaning, but vice versa - down to the foot, causing a number of problems.
Why is it necessary to remove the diseased veins, through which the waste blood containing waste products of cellular metabolism flows not to be cleaned up, but back to the legs? There are several reasons for this. The first reason is that overstretched veins containing used blood are a common source of blood clots in the body. Blood is a complex biological fluid, practically a tissue containing, in addition to water, a large number of substances, cells, and protein structures.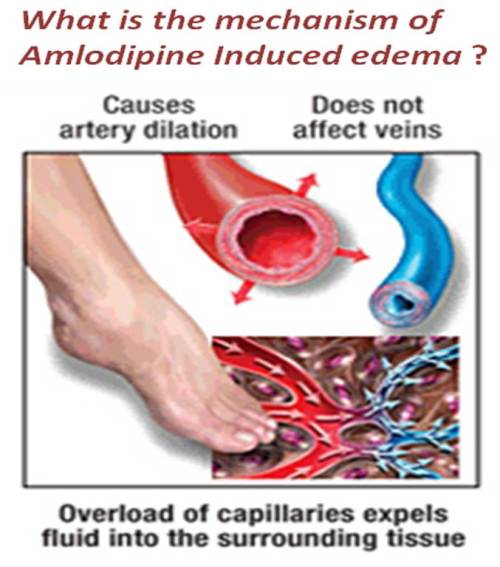 For normal functioning, it must flow all the time and not stagnate, as happens in varicose veins. Let's show you what we're talking about. In order to understand what happens during blood stasis, we collect blood in a test tube and see what happens. If the tube is not shaken, but left to stand on the table, in a few minutes a blood clot of coagulated plasma and blood cells will fall to the bottom of the tube - a thrombus. If such a thrombus forms inside a vein, it can “trip” through the vessels, causing blockage of those places that are smaller than its diameter, and the first target on its way is the vessels of the lungs. This phenomenon is called pulmonary embolism, abbreviated as PE. This is a very serious disease, the treatment of which is usually carried out in the intensive care units of large hospitals, which is associated with a sharp deterioration in blood flow in the lungs and a violation of gas exchange in vessels clogged with blood clots. Clinically, this is manifested by sudden severe shortness of breath, which is very difficult to stop even on a ventilator.
For normal functioning, it must flow all the time and not stagnate, as happens in varicose veins. Let's show you what we're talking about. In order to understand what happens during blood stasis, we collect blood in a test tube and see what happens. If the tube is not shaken, but left to stand on the table, in a few minutes a blood clot of coagulated plasma and blood cells will fall to the bottom of the tube - a thrombus. If such a thrombus forms inside a vein, it can “trip” through the vessels, causing blockage of those places that are smaller than its diameter, and the first target on its way is the vessels of the lungs. This phenomenon is called pulmonary embolism, abbreviated as PE. This is a very serious disease, the treatment of which is usually carried out in the intensive care units of large hospitals, which is associated with a sharp deterioration in blood flow in the lungs and a violation of gas exchange in vessels clogged with blood clots. Clinically, this is manifested by sudden severe shortness of breath, which is very difficult to stop even on a ventilator. If the separation of the thrombus from the veins of the legs and the occurrence of PE did not occur and the thrombus remained in the varicose vein, then with thrombosis, inflammation of the vein wall in the thrombus zone is almost always observed, manifested by redness, thickening of the varicose vein, as well as a feeling of a dense "strand" along the dilated nodes. In such a situation, surgical treatment of varicose veins or the appointment of drugs that thin the blood to prevent further growth and separation of a blood clot are indicated. If anticoagulant therapy is carried out as the first stage, then varicose veins should definitely be treated (diseased veins should be removed), since the risk of re-thrombosis of a varicose vein after anticoagulant withdrawal is about 5 times higher than before thrombosis. nine0003
If the separation of the thrombus from the veins of the legs and the occurrence of PE did not occur and the thrombus remained in the varicose vein, then with thrombosis, inflammation of the vein wall in the thrombus zone is almost always observed, manifested by redness, thickening of the varicose vein, as well as a feeling of a dense "strand" along the dilated nodes. In such a situation, surgical treatment of varicose veins or the appointment of drugs that thin the blood to prevent further growth and separation of a blood clot are indicated. If anticoagulant therapy is carried out as the first stage, then varicose veins should definitely be treated (diseased veins should be removed), since the risk of re-thrombosis of a varicose vein after anticoagulant withdrawal is about 5 times higher than before thrombosis. nine0003
Another reason why it is necessary to remove dilated non-functioning veins is that the presence of such veins, due to the reverse flow of waste blood, constantly creates an increased concentration of harmful used substances in the tissues of the legs, as well as an overfilling of the venous system with blood and poor removal of fluid in general from the leg. This leads to swelling, pain in the legs, a feeling of fullness, itching, cramps and other clinical symptoms of venous insufficiency. Gradually, these symptoms worsen, reducing the resistance of the affected leg to stress. A long-term increased concentration of waste substances in the skin, in the zone of which varicose inflow is located, leads to disruption of its nutrition (poisoning by the cells' own waste products), that is, trophic changes, such as venous eczema and ulcers, prolonged edema, damage to the microcapillary and lymphatic channels, and ultimately as a result, to irreversible changes in the skin and subcutaneous tissue of the legs. In this regard, the most important component of the treatment of varicose veins today is the planned removal of diseased dilated and non-functioning sections of the venous bed. And as maintenance therapy, drug and compression therapy can be used, but after the correction of the underlying problem. nine0003
This leads to swelling, pain in the legs, a feeling of fullness, itching, cramps and other clinical symptoms of venous insufficiency. Gradually, these symptoms worsen, reducing the resistance of the affected leg to stress. A long-term increased concentration of waste substances in the skin, in the zone of which varicose inflow is located, leads to disruption of its nutrition (poisoning by the cells' own waste products), that is, trophic changes, such as venous eczema and ulcers, prolonged edema, damage to the microcapillary and lymphatic channels, and ultimately as a result, to irreversible changes in the skin and subcutaneous tissue of the legs. In this regard, the most important component of the treatment of varicose veins today is the planned removal of diseased dilated and non-functioning sections of the venous bed. And as maintenance therapy, drug and compression therapy can be used, but after the correction of the underlying problem. nine0003
Causes of varicose veins
- Hereditary predisposition:
More than 25% of people with varicose veins have close relatives who also have some form of the disease.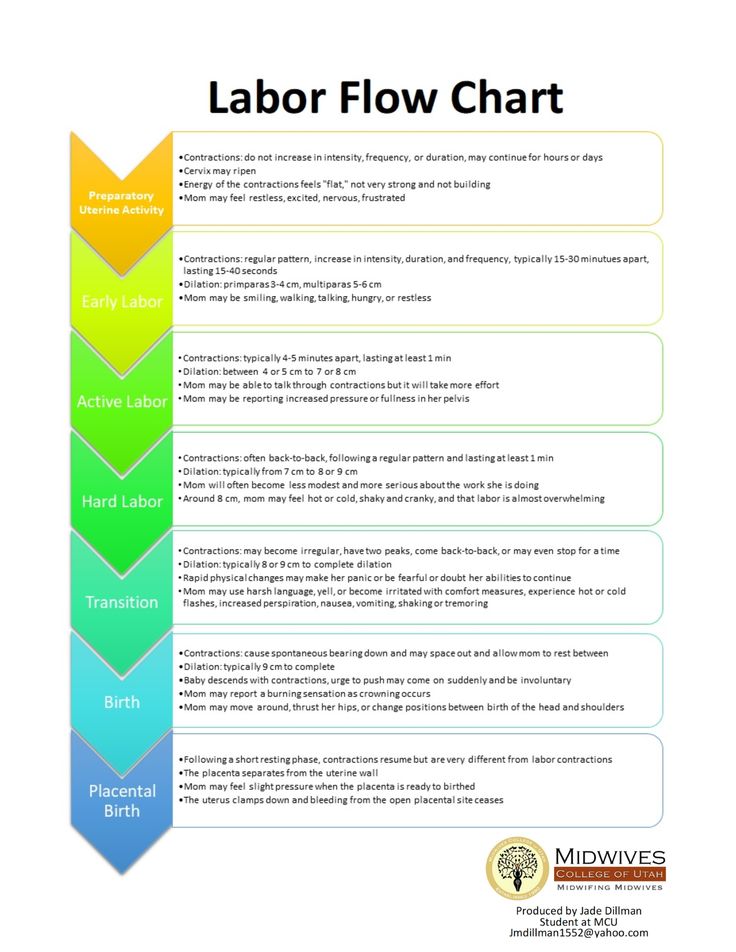 Most likely, a connective tissue defect is inherited, which later leads to the development of varicose veins. Connective tissue is the framework of all organs and tissues of the body, including the framework of blood vessels (arteries and veins).
Most likely, a connective tissue defect is inherited, which later leads to the development of varicose veins. Connective tissue is the framework of all organs and tissues of the body, including the framework of blood vessels (arteries and veins).
- Lifestyle:
- Prolonged, static loads (lifting weights, immobile standing or sitting) can become a trigger in the development of varicose veins. Surgeons, cooks, hairdressers, waiters, teachers and office workers fall into the risk category. If a person is forced to stand for most of the day, and there are no active muscle contractions, his venous system cannot resist gravity. As a result, physiological stasis develops - the lower limbs overflow with blood and edema develops. nine0404
- Insufficient physical activity.
- Smoking, which increases blood pressure and increases the risk of varicose veins.
- The lack of raw vegetables and fruits in the diet, as well as the high level of food processing, causes a lack of fiber, which is necessary for the normal functioning of the walls of the veins.
 In addition, such a diet can contribute to the development of chronic constipation, which, in turn, leads to an increase in intra-abdominal pressure. nine0404
In addition, such a diet can contribute to the development of chronic constipation, which, in turn, leads to an increase in intra-abdominal pressure. nine0404 - Tight underwear, corsets, especially at the level of the inguinal folds, increase intra-abdominal pressure, which can provoke the occurrence or development of varicose veins.
- Overweight is a scientifically proven risk factor for the occurrence and development of varicose veins for women of reproductive and post-reproductive age. For men, obesity is not a statistically confirmed risk factor for varicose veins. However, excess body weight increases the load on the legs and veins of the lower extremities. For the same reasons, height is a risk factor for varicose veins. nine0404
- Hormonal imbalance. The role of this factor has increased many times in recent years due to the wide popularity of hormonal contraceptives and substitution therapy in women of pre- and postmenopausal age. Progesterone, estrogen and their analogues help to reduce the tone of the venous walls due to the destruction of elastic and collagen fibers.
- Pregnancy, childbirth, physical stress. With such an excessive load, there is a sharp increase in pressure in the veins of the lower extremities and damage to the valvular apparatus, which triggers the mechanism of varicose expansion of the superficial veins. nine0404
Every third woman over the age of 30 has signs of varicose veins. The legs hurt, swell, so-called spider veins appear, which eventually turn into varicose veins. You have to give up high heels, and often hide your legs under long skirts. Varicose veins are not a purely cosmetic problem . Varicose veins are a disease caused by a malfunction of the valves responsible for the movement of blood through the veins from the bottom up. With varicose veins, pressure increases, blood stagnates, which leads to painful heaviness in the legs, edema, varicose veins (in Latin, “varixes”), and in a neglected state, to thrombophlebitis, thrombosis, lymphovenous insufficiency and trophic ulcers.