Pregnant cold sore
Cold sores in pregnancy | Pregnancy Birth and Baby
Cold sores in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
What is HSV?
If you or your partner has the virus that causes cold sores or genital herpes, you might be worried about what could happen when you're pregnant or have a new baby. Here's what you need to know about herpes simplex virus (HSV), and how to protect your baby from infection.
The herpes simplex virus is a very common virus carried by most people. Sometimes it causes cold sores or genital herpes.
Cold sores are blisters that form on the lips, around the mouth and nose. Genital herpes is blisters or sores around the genitals or anus. The blisters may form a crust after about 3 days. The sores go away by themselves within 2 weeks.
There are two main types of HSV:
- HSV-1 causes mostly cold sores on the face and lips, and sometimes on the genitals
- HSV-2 causes mostly genital herpes
Both viruses are transferred though contact of the skin, saliva or genitals, and the viruses stay in the body for life. The viruses do not always cause symptoms, so you can carry the virus without knowing it.
HSV-1 is very common, with about 8 in 10 Australians carrying it in their bloodstream. But only 1 in 3 people with the virus has ever had a cold sore. HSV-2 is less common.
It is common for women who have had cold sores in the past to experience an outbreak while pregnant.
What happens if I get cold sores or genital herpes during pregnancy?
Having the HSV virus does not affect your chance of becoming pregnant.
It is quite common for women to have a cold sore during their pregnancy, even if they haven’t had one for a long time. Cold sores should not affect your unborn baby.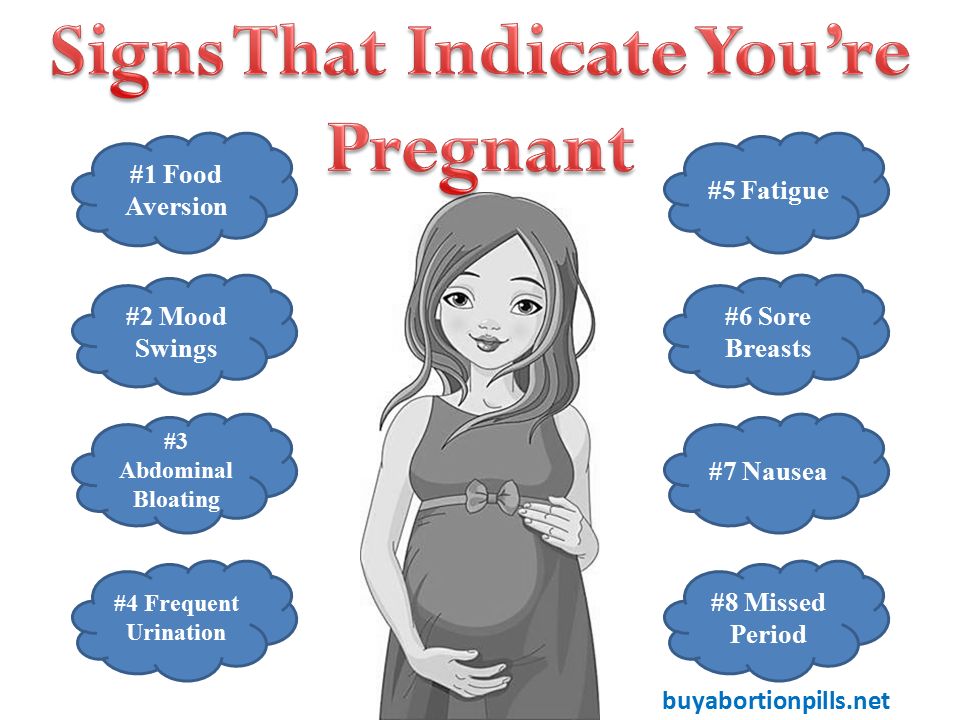 But they are infectious, so it’s a good idea to treat them.
But they are infectious, so it’s a good idea to treat them.
Genital herpes should not affect the baby if you have your first outbreak or it comes back in the first 34 weeks. But it can be transferred to your baby during the birth, especially if it’s your first outbreak.
If you've ever had a cold sore or genital herpes and you become pregnant, or you develop these conditions during pregnancy, it's important to tell your doctor or midwife about it. Together you can make a plan for managing herpes during pregnancy and birth.
How is HSV treated during pregnancy or breastfeeding?
You can treat cold sores and genital herpes with:
- aciclovir cream, available from a pharmacist without prescription
- aciclovir or valaciclovir tablets, for which you need a prescription
These 'antiviral' drugs are known to be safe for pregnant and breastfeeding women and are effective most of the time.
Famciclovir tablets are not recommended to take during pregnancy. Speak to your doctor if the cold sore is severe.
Speak to your doctor if the cold sore is severe.
How is genital herpes treated during pregnancy?
You should take acyclovir or valaciclovir tablets, as above.
If it's your first outbreak of genital herpes, your baby may be more at risk because you haven't had time to develop immune protection against the virus, which also helps protect the baby.
Some women experiencing an outbreak of genital herpes might be advised to have a caesarean. This would prevent the herpes virus passing from mother to baby during a vaginal birth. But most women in Australia with genital herpes do give birth safely to healthy babies vaginally.
It's often recommended that women who have ever had genital herpes take antiviral tablets prior to the birth, even if the herpes isn't active at the time.
Talk to your doctor or midwife about the best course of action for your situation.
How do I protect my baby from herpes?
Herpes can cause serious problems in a baby, such as infections to the eyes and throat, brain damage and even death.
A newborn baby can catch HSV-1 and HSV-2 from being kissed or touched by someone with cold sores, or during childbirth.
Fortunately, most babies born to women who carry the virus are not affected. But if you or your partner has a cold sore or genital herpes, talk to your doctor about keeping it under control during the pregnancy and after the birth. It is also important to treat these conditions aggressively while you are breastfeeding.
It's important to maintain strict hygiene habits when caring for a new baby if you, or anyone in close contact with the baby, have cold sores.
If you have cold sores, you should:
- cover cold sores when you're around the baby
- avoid kissing your baby until the sores are completely healed
- avoid touching the cold sores then touching your baby
- wash your hands thoroughly before touching your baby
What if I have a cold sore while breastfeeding?
If you have cold sores, it is safe to breastfeed your baby as long as the cold sores are not on the breast or nipple.
If they are, it may be wise to breastfeed from the unaffected nipple only until the lesions have cleared up. You would express and dispose of breastmilk from the affected nipple. Breastmilk itself doesn't contain the herpes virus but it can be contaminated through the skin lesions.
Talk to your doctor or midwife as soon as you notice any cold sores on your breast or nipple.
What happens if my baby gets herpes?
It is very important that herpes in a newborn is recognised and treated by a doctor in hospital immediately. Signs of herpes in a newborn include:
- blisters on the skin
- fever
- irritability
- tiredness
- lack of appetite
If you think your baby might have the herpes virus, don't wait to see if they get better — seek medical help. Tell medical staff if you or your partner carry the herpes virus.
Resource and Support
If you are worried about your baby, see a doctor or midwife, or take them to the hospital.
FIND A HEALTH SERVICE — The Service Finder can help you find doctors, pharmacies, hospitals and other health services.
If you're not sure what to do or want more information, you call Pregnancy Birth Baby on 1800 882 436 to speak with a maternal child nurse.
Sources:
Family Planning NSW (Genital herpes), The Royal Woman’s Hospital (Genital herpes), Mothersafe (Cold sores in pregnancy and breastfeeding), Queensland Government Health (Genital Herpes and Pregnancy), SA Health (Cold sores (herpes simplex type 1) - including symptoms, treatment and prevention), Safer Care Victoria (Herpes simplex virus in neonates)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: May 2021
Back To Top
Need more information?
Cold sores - Better Health Channel
Cold sores are blisters around the mouth and nose, caused by the herpes simplex virus.
Read more on Better Health Channel website
Cold sores overview - MyDr.com.au
A cold sore is a skin infection that is caused by the herpes simplex virus (HSV). Cold sores usually occur on or around the lips or nose and are very common. They have nothing to do with colds.
Read more on myDr website
Cold sores: self-care - MyDr.com.au
Cold sores are caused by the herpes simplex type 1 virus. Most people carry this virus in their bodies. Find out what products are available for cold sores.
Read more on myDr website
Cold sores | SA Health
Herpes simplex virus type 1 (HSV1) causes cold sores on the face or lips - it is spread by skin or mucous membrane contact with infected saliva
Read more on SA Health website
Cold sore infections - MyDr.
 com.au
com.au Find the answers to common questions about cold sores, irritating blisters which are caused by the herpes simplex type 1 virus and can be triggered by stress, fatigue or exposure to sunlight.
Read more on myDr website
Cold sores: children & teens | Raising Children Network
Cold sores are quite common in older children and teenagers. Cold sores usually clear up by themselves, but see your GP if you’re concerned.
Read more on raisingchildren.net.au website
Genital Herpes | Family Planning NSW
Genital herpes is a common sexually transmitted infection (STI) caused by the herpes simplex virus (HSV). There are two types of herpes simplex virus.
Read more on Family Planning NSW website
Genital Herpes and Pregnancy
If you are pregnant and you get genital herpes, it is important to tell your midwife or obstetrician.
Read more on Queensland Health website
Genital herpes
Genital herpes is a sexually transmitted infection (STI) which shows as blisters or sores on the genitals. This is caused by the herpes simplex virus (HSV).
Read more on WA Health website
Genital herpes: what is it? - MyDr.com.au
Genital herpes is a viral infection characterised by outbreaks of blisters and sores around your genital area.
Read more on myDr website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Affect on Baby and Safe Treatments
If you’ve ever had cold sores — those annoying, painful, tiny, fluid-filled blisters that usually form around your mouth and on your lips — you know how inconvenient they can be.
But also if you’ve ever had cold sores (and therefore already have the virus that causes them), did you know they can recur, especially when you’re under stress or are undergoing hormonal fluctuations?
Stress and hormonal changes. That sounds an awful lot like pregnancy.
That sounds an awful lot like pregnancy.
Cold sores in pregnancy aren’t unheard of, and they don’t usually have any impact on your growing baby. So first, let out a deep sigh of relief. Next, read on — because there are still important things to know about cold sores if you’re expecting.
Cold sores are caused by a virus — the herpes simplex virus (HSV). Of the two types of HSV, cold sores are generally caused by HSV-1, whereas genital herpes is usually a result of exposure to HSV-2. There have been a few instances where HSV-1 sores have been found in the genitals and vice versa.
Once you’ve had a cold sore (oral herpes), the virus remains in your system for life — it’s just not active unless you have a current outbreak.
But when we say that stress and hormones can cause the virus to reactivate, it’s important to know that stress and hormones don’t cause the virus in the first place.
If you’ve never had HSV, you can only get it through contact with someone who has. When it comes to a first-time cold sore infection, this can happen via activities like:
When it comes to a first-time cold sore infection, this can happen via activities like:
- kissing
- sharing food or utensils
- using someone else’s ChapStick or lip gloss
- oral sex
Here’s the really good news: If you already have the virus that causes cold sores, and you have an outbreak of oral herpes during pregnancy, it’s most likely not going to have any impact on your growing baby.
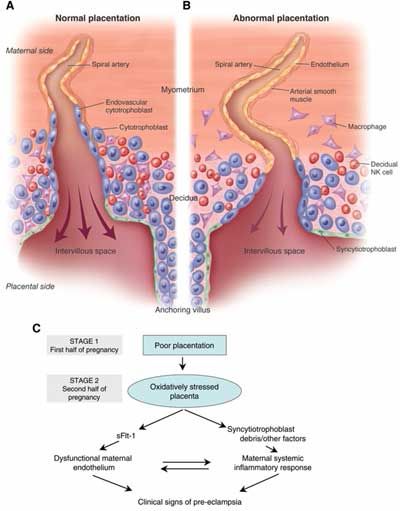
Cold sores are a localized infection, usually around the mouth area. They don’t typically cross the placenta and reach your baby.
The highest risk scenario is if you get HSV for the first time during your third trimester of pregnancy.
When you get the virus for the first time, your body hasn’t developed any protective antibodies to it yet. And while HSV-1 is usually associated with oral herpes, it can cause a genital herpes outbreak, which can be dangerous to your baby — especially as they pass through the birth canal.
Birth-acquired herpes is serious.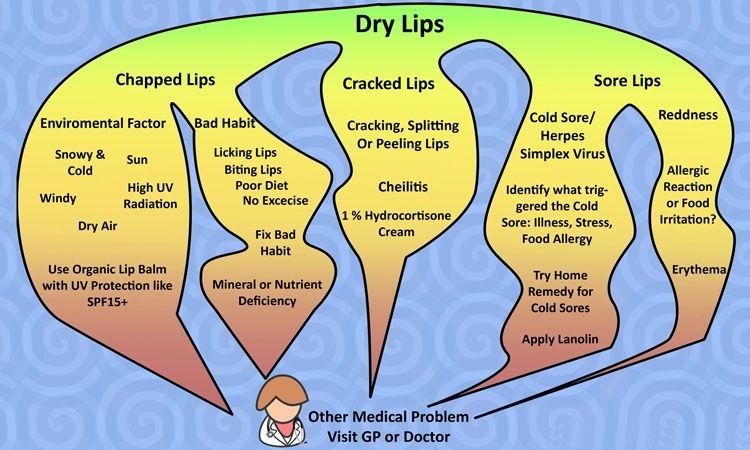 However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
However, it’s a concern with genital rather than oral herpes. That being said, because the same virus can cause both, it’s important to talk to your OB about any cold sores during pregnancy.
The most common treatment for cold sores is docosanol (Abreva), an over-the-counter topical cream. But the Food and Drug Administration hasn’t evaluated it for safety in pregnancy.
While some research has determined that it’s “likely safe” during pregnancy, at least one pharmaceutical company that manufactures the drug warns against using it unless it’s definitely needed — which really means you need to check with your doctor. There may be other treatments you should try first.
If you’ve had herpes in the past, your doctor may recommend antivirals — like acyclovir or valacyclovir — starting at week 36 and continuing until delivery of your baby, even if you don’t have a current outbreak of lesions around the genital area. This helps prevent reactivation and spread of the virus to the genital area.
This precaution is because you shouldn’t expose your baby to herpes in the vaginal area during delivery.
Alternatively, your doctor may suggest a cesarean delivery, which avoids the birth canal altogether — something that’s especially important if you have a current outbreak of genital herpes.
Cold sores are highly contagious, despite the fact that they won’t affect your baby in the womb. If you have them after your baby is born, avoid kissing those adorable little cheeks or touching any sores and then touching your newborn without first washing your hands with soap.
In the extremely rare event that you have cold sores on either breast, avoid breastfeeding from that breast while you’re still contagious.
Your cold sores are contagious until they crust over, at which point they’ll start to heal.
If you do pass a cold sore infection on to your newborn, it’s known as neonatal herpes. While not as serious as the birth-acquired version, it can still cause serious complications in a baby who hasn’t yet developed a robust immune system.
The cold sore on your mouth is likely to be more of an annoyance to you than a serious risk to your developing baby, particularly in your first two trimesters of pregnancy and especially if you’ve had one before. But you should still let your OB know about it.
The virus that causes cold sores — usually HSV-1 — can also cause genital herpes, which is more of a risk to your pregnancy and growing little one.
If you have an outbreak in your third trimester — or if you acquire the virus for the first time in your third trimester — your doctor may want you to follow certain treatment or precautionary guidelines, like antivirals or a cesarean delivery.
Colds during pregnancy: how to treat?
Any cold or respiratory disease in early pregnancy, during the primary formation of the fetus, can lead to unpredictable consequences and complications. The matter is complicated by the fact that most medications are absolutely contraindicated for use during gestation.
In this regard, the treatment and prevention of colds in pregnant women is an important issue, which should be approached especially responsibly! The main thesis is: be careful with medicines and apply mild preventive measures based on alternative medicine methods to avoid respiratory diseases and flu.
"One for two - immunity"
This is a very fragile system, it is not necessary to interfere in its work, but it is necessary to support and strengthen it. Pregnancy belongs to the category of special, albeit temporary, conditions during which a woman needs additional protection.
This issue will help simple recommendations that are available to everyone:
• During the period of frequent weather changes, it is necessary to dress warmer, paying special attention to footwear.
• During an epidemic, it is better for a pregnant woman to refrain from being in crowded places - transport, metro, shops and hospitals. If there is an urgent need, to prevent possible infection, a protective respiratory mask should be worn before leaving the house.
• Be especially careful about hygiene after visiting the street and public places. Upon returning home, the first thing to do is wash your hands thoroughly.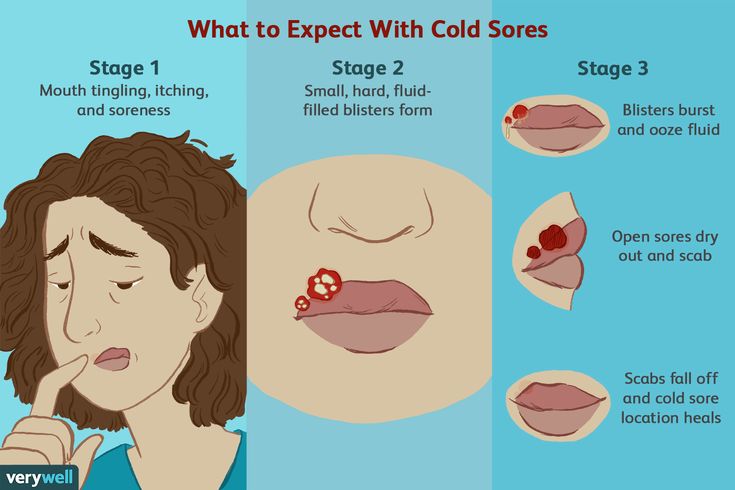
Interesting: More than 90% of all acute respiratory infections are caused by viruses, about 10% are bacteria and other pathogens. Accordingly, any soap can be used, not necessarily antibacterial.
• Before going outside, you can lubricate the nasal mucosa with oxolinic ointment. Upon returning home, flush the upper respiratory tract with soda solution.
• Rationalization of nutrition and intake of vitamins will strengthen the immune defense. It is especially useful to eat fruits and vegetables that are enriched with vitamins and have not undergone heat treatment.
Interesting: our grandmothers used to say: in order not to get sick, you need to drink chicken broth! Strange, but until recently, scientists did not attach much importance to this prophylactic. Pulmonologist Stefan Rennard decided to find out if this was true or not. The professor conducted a study and proved that the use of chicken broth affects the mobility of neutrophils, white blood cells that protect the body from infections and activate the immune system.
- Vitamins can be taken using ready-made pharmaceutical multivitamin complexes. Before choosing a drug, you should consult your doctor.
- Compliance with the regimen and duration of sleep - at least 9 hours a day. The possibility of psychotraumatic situations should be minimized.
- Maintaining cleanliness in the living quarters (ventilation, wet cleaning).
- Air humidification is an important aspect in the prevention of influenza and respiratory diseases. If air conditioners or heaters are used in the pregnant woman's house, it would be best to purchase a mechanical humidifier.
Medications for prevention
- Grippferon - a drug in the form of drops for the nose, which provides prevention and treatment of influenza, is not contraindicated for pregnant and lactating women. The medicine stimulates an increase in immunity, has a pronounced antiviral effect that can protect against colds, infections and influenza varieties.

- Ascorbic acid - can be used as a separate source of vitamin C in a synthetic version, with a reduced daily intake from food. Ascorbic acid not only prevents infection, but also fights viruses that have already entered the body of a woman.
- Viferon - nasal ointment, which is prescribed for the prevention of influenza and respiratory infections during an epidemic. The ointment has protective and immunomodulatory effects, and also allows you to deal with disorders that are already occurring in the body at the time of use. Viferon in the form of a nasal ointment has no contraindications for use in pregnant women at any time, including the first trimester.
- Aquamaris is a natural drug in the form of a nasal spray that allows you to moisturize the nasal mucosa, thereby reducing the risk of influenza viruses entering the nasal cavity.
I would like to say a few words about such a method of prevention as vaccination. Most often, the expectant mother may be at risk of infection due to the annual influenza epidemic. This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media. Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus.
This disease is dangerous for a pregnant woman precisely because of its complications: pneumonia, bronchitis, otitis media. Influenza in a pregnant woman can also affect the health of the fetus. Most of all, it is dangerous in the early stages of pregnancy, when the tissues and organs of the human embryo are laid and formed. Viral intoxication or drug exposure can lead to pathology of the child's organs. In later pregnancy, there is a risk of infection of the fetus.
The most dangerous consequence of influenza in a pregnant woman is threatened miscarriage or premature birth!
It is quite natural that expectant mothers often wonder whether or not to vaccinate.
Studies have concluded that the use of inactivated ("killed") influenza vaccines does not have a teratogenic effect on the fetus and does not harm the health of a pregnant woman. After consulting with your doctor about such an inoculation, you can come to an optimal solution. If an influenza epidemic is inevitable, and the pregnant woman has no contraindications, then the vaccine should be given. If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of mothers reduces the risk of influenza infection of a born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy.
If a pregnant woman has a negligible risk of infection, she does not come into contact with a large number of people, or is opposed to vaccination, then you can not do it. According to research, it is known that vaccination of mothers reduces the risk of influenza infection of a born child by 63%. Seasonal influenza prevention is carried out in September, October. Vaccinations for pregnant women are recommended from the second trimester of pregnancy.
In the period of a planned pregnancy, a flu shot is given 1 month before it: the formation of immunity occurs 2-4 weeks. Protection after vaccination lasts about a year.
If infection does occur, action should be taken immediately if at least one symptom of the disease is detected. The health of a pregnant woman and her unborn child depends entirely on her responsibility and respect for her own body.
Proven folk remedies will be used first. Since pregnant women cannot steam their legs, steam their hands, and this will facilitate nasal breathing. Bundle up, put on woolen socks and crawl under the covers: warmth, peace and sleep are good for colds. Do not forget to drink plenty of water - hot green tea with lemon and honey, lime blossom tea, cranberry juice, rosehip broth, dried fruit compote. Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning.
Bundle up, put on woolen socks and crawl under the covers: warmth, peace and sleep are good for colds. Do not forget to drink plenty of water - hot green tea with lemon and honey, lime blossom tea, cranberry juice, rosehip broth, dried fruit compote. Ginger in the form of tea also helps, not only with catarrhal symptoms, but with nausea in the morning.
Various hot milk drinks are also suitable. Honey can be added to milk, and it is best to boil it on onions. It must be emphasized right away that not all herbs for colds during pregnancy can be used. Here is a list of medicinal plants that are contraindicated: aloe, anise, barberry, elecampane (grass and root), sweet clover, oregano, St. John's wort, strawberries (leaves), viburnum (berries), raspberries (leaves), lemon balm, lovage, wormwood, licorice ( root), celandine, sage. Accordingly, preparations containing these plants should not be taken.
The use of medicines for colds during pregnancy must be treated with great care!
It is contraindicated to use the following drugs : Pertussin, Tussin plus, Joset, Glycodin, Ascoril, Travisil, Broncholitin, ACC, Grippeks, Codelac, Terpinkod. Do not use lozenges and lozenges for sore throat or cough are also undesirable due to the likelihood of allergic reactions.
Do not use lozenges and lozenges for sore throat or cough are also undesirable due to the likelihood of allergic reactions.
Spray Pinosol, judging by the components indicated in the instructions, is not dangerous during pregnancy. However, the essential oils contained in the preparation - pine, peppermint, eucalyptus, thymol, guaiazulene (wormwood oil) - can lead to an allergic reaction with swelling of the nasal mucosa.
Viferon suppositories are allowed to be used only after 14 weeks from the start of conception. This drug contains recombinant human interferon alpha-2, ascorbic acid and alpha-tocopherol acetate and has antiviral, immunomodulatory and antiproliferative effects. It is used in the treatment of various infectious and inflammatory diseases in adults and children (including newborns). In the form of an ointment, Viferon is used to treat herpetic lesions of the skin and mucous membranes. The ointment is applied in a thin layer to the affected areas of the skin 3-4 times a day for 5-7 days.
The homeopathic preparation Stodal, which includes predominantly herbal ingredients, acts on various types of cough and has an expectorant and bronchodilator effect.
Viburkol - homeopathic suppositories - have analgesic, anti-inflammatory, sedative, antispasmodic action. They are prescribed in the complex therapy of acute respiratory viral infections and other uncomplicated infections (including in newborns), as well as in inflammatory processes of the upper respiratory tract and inflammatory diseases of the genitourinary system.
So, you can try to eliminate a slight ailment on your own, but there are conditions under which you need to call a doctor at home:
- Prolonged fever;
- Myalgia, fatigue, fatigue, general malaise;
- Difficulty breathing, nasopharyngeal lumps and dry or wet barking cough;
- A pregnant woman is troubled by severe pressing headache.
In conclusion, I would like to emphasize the importance of treating chronic diseases before pregnancy, a healthy lifestyle during childbearing and following all doctor's orders.
I wish expectant mothers and their loved ones to try to maintain a good mood: optimists live longer and happier, they are more productive. Remember your victories and pleasant moments more often and everything will be fine!
Cold during pregnancy. What to do?
When you're expecting, your immune system works at a slower pace than usual, which is actually a good thing because it protects your growing baby and keeps your body from thinking the fetus is a foreign creature. However, the downside of this immune suppression is that your body does not defend itself against many of the viruses that cause colds, which can make you more vulnerable to symptoms such as nasal congestion, cough, and sore throat.
The good news about even the worst cold symptoms is that your child doesn't experience any of them. In fact, the environment of the womb keeps the baby completely protected from these hardships.
As far as you are concerned, a cold is basically an uncomfortable irritation that is best relieved by rest, drinking plenty of water, patience, and consultation with your doctor. The doctor must be aware of all your symptoms and ailments, including any cold. If necessary, he can also prescribe you the necessary medicines that are considered safe during pregnancy.
The doctor must be aware of all your symptoms and ailments, including any cold. If necessary, he can also prescribe you the necessary medicines that are considered safe during pregnancy.
Although many cold medicines are usually prohibited during pregnancy, you do not need to suffer from a runny nose and a violent cough when you are pregnant. Some of the most effective cold remedies are not available over the counter.
Here are some of them:
- Lying in bed doesn't necessarily shorten the duration of a cold, but if your body is asking for some rest, be sure to listen.
- If you do not have a fever or cough, do some light to moderate exercise that is safe for pregnant women. It can really help you feel better faster.
- Keep eating. Sure, you probably don't have much of an appetite, but eating as healthy a meal as possible can help you manage some of your cold symptoms.
- Vitamin C foods can help boost your immune system naturally.
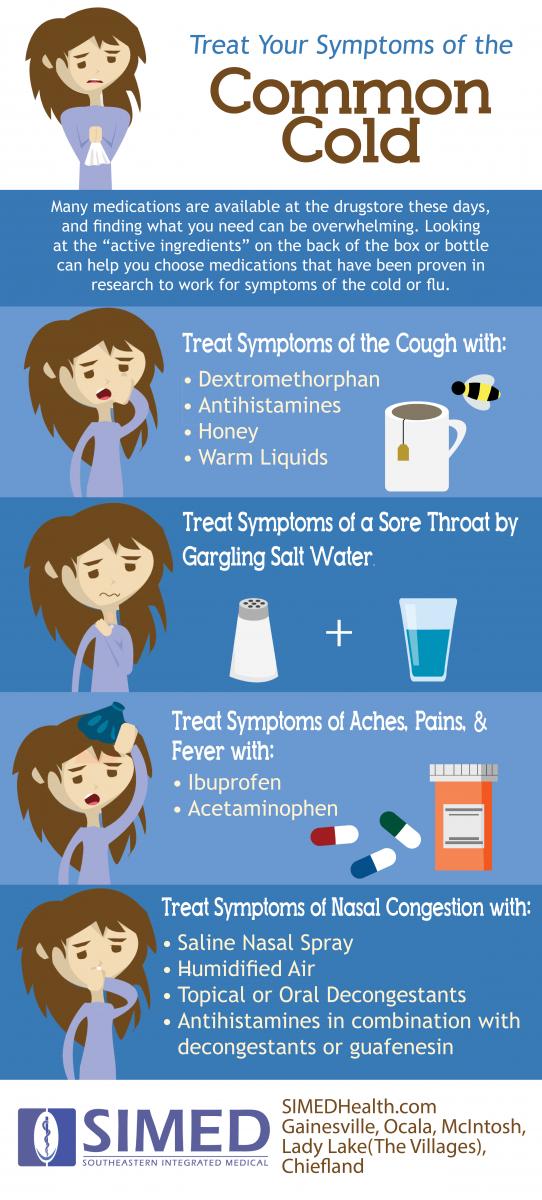 Try all kinds of citrus fruits (oranges, tangerines, grapefruits), strawberries, melon, kiwi, mangoes, tomatoes, bell peppers, papaya, broccoli, sauerkraut and spinach.
Try all kinds of citrus fruits (oranges, tangerines, grapefruits), strawberries, melon, kiwi, mangoes, tomatoes, bell peppers, papaya, broccoli, sauerkraut and spinach. - Zinc may also help strengthen the immune system. Pregnant women should aim to get 11-15 milligrams each day from all sources, including vitamins.
- Fever, sneezing and a runny nose help you lose fluids that you and your baby need. Warm drinks are soothing, so keep a thermos of hot beverages like ginger tea, hot soup, or chicken broth close at hand. Try to drink enough to stay "well hydrated" - your urine should be the color of pale straw. Water and juices also work great, but they don't have to be very cold.
- If you have a runny nose, elevate your head with a pair of pillows to help you breathe easier. Cold patches can also help. They gently open the nasal passages, making it easier to breathe, moreover, they are sold without a prescription and are completely safe.
- If the air in the house is dry, you can use a special humidifier.