Pregnancy week 35 cramps
Pregnancy at week 35 | Pregnancy Birth and Baby
Pregnancy at week 35 | Pregnancy Birth and Baby beginning of content4-minute read
Listen
Your baby
Your baby now weighs more than 2.3kg and measures about 32cm from head to bottom. They are quite cramped and their legs are bent up into their chest, but they can still change position and kick you. They can swallow about a litre of amniotic fluid every day, which is passed as urine.
Don’t worry if your baby is still in the breech position (head up, feet down) – most babies will gradually turn into the head-down position during the last month. If your baby is still in the breech position during the next week or two, your doctor or midwife may try to turn them using a procedure known as External Cephalic Version (ECV).
Your baby at 35 weeks
| Length: | 32cm (head to bottom) |
| Weight: | 2.3kg |
Your body
You may be having a lot of Braxton Hicks contractions by now. They feel like a tightening or cramping in your tummy, and they can happen as often as every 10 to 20 minutes in late pregnancy. They are your body’s way of preparing for the birth and are nothing to be worried about. You can tell if they’re Braxton Hicks and not real contractions because they normally go away if you move position.
They may be real contractions if:
- they get stronger or closer together
- they last longer as time goes by
- they are stronger when you walk
- you feel pain or pressure in your pelvis, abdomen or lower back
If you went into labour now it would be considered premature labour and you would need medical attention straight away. If you’re in doubt, contact your doctor or midwife.
If you’re in doubt, contact your doctor or midwife.
Things to remember
If your pregnancy is high risk, your doctor or midwife will probably want to see you more often from now on.
One serious complication that can develop in late pregnancy is pre-eclampsia. This is usually diagnosed if your doctor notices you have high blood pressure or protein in your urine.
See your doctor straight away if you develop:
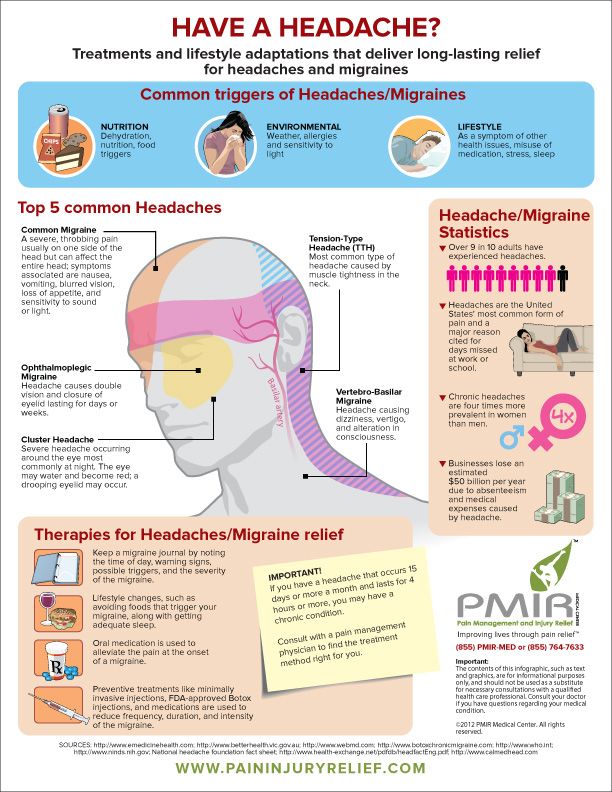
- a bad headache
- pain in the tummy
- blurry vision
- sudden swelling of your hands or feet
Read next
Your pregnancy at 36 weeks
Learn about your pregnancy journey and what is happening to you and your baby.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Raising Children Network (Pregnancy week-by-week), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Breech Presentation at the End of your Pregnancy), NHS (You and your baby at 35 weeks pregnant), Royal Australian and New Zealand College of Obstetricians and Gynaecologists (Labour and birth)Learn more here about the development and quality assurance of healthdirect content.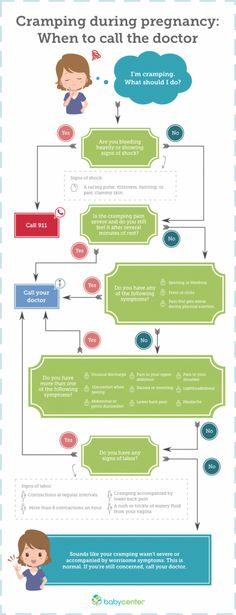
Last reviewed: August 2020
Back To Top
Need more information?
Pregnancy at week 34
As at the start of your pregnancy, you’re probably feeling tired and emotional. The baby doesn't have much room to move, but you might feel them kick and roll.
Read more on Pregnancy, Birth & Baby website
Pregnancy at week 39
Your baby's weight gain should slow down since they are now ready to be born. You might soon start to notice the early signs of labour.
Read more on Pregnancy, Birth & Baby website
Pregnancy and travel - Better Health Channel
Travelling to developing nations is not encouraged during pregnancy, due to the risk of disease and the standard of medical facilities.
Read more on Better Health Channel website
Multiple birth - triplets or more
If you are pregnant with triplets or more, the birth will need careful planning. The main risk is that your babies will be born prematurely. Find out more here.
Read more on Pregnancy, Birth & Baby website
Episiotomy
An episiotomy is a procedure performed during labour to assist with the delivery of your baby.
Read more on Pregnancy, Birth & Baby website
The role of exercise in improving fertility, quality of life and emotional wellbeing
Being in the healthy weight range reduces the risk of infertility and improves the chance of conceiving spontaneously and with assisted reproductive technology (ART).
Read more on Your Fertility website
Undescended testicles - Better Health Channel
Undescended testicles means that one or both testicles are missing from the scrotum.
Read more on Better Health Channel website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
35 Weeks Pregnant | Pregnancy
Many choose to begin their maternity leave around now, and then use the next few weeks to prepare for the baby's arrival. Others prefer to work until the birth. You can do what feels right for you.
What’s happening in my body?
If you've spotted any yellow stains in your bra, then that's probably colostrum, which is an early milk that is rich in antibodies. Some pregnant women start to make it weeks or even months before the birth. When you breastfeed, this helps to protect your baby from stomach bugs and other infections.
Some pregnant women start to make it weeks or even months before the birth. When you breastfeed, this helps to protect your baby from stomach bugs and other infections.
Around 3 to 5 days after the birth, your milk will come in, and your breasts will look even bigger. You may wish to get ready for this by getting measured for a feeding bra that will allow a bit of growth. You could also stock up on breast pads to soak up any extra milk, so that you don't stain your clothes.
Not everyone can breastfeed, and it takes a bit of practice, but if you can, then it gives your baby a good start in life. Read the Start for Life page about breastfeeding.
Talk to your midwife about group B strep
Group B strep is a common bacteria and up to 2 in 5 people have it living in their body. If you carry group B strep while you're pregnant, there's a small risk it could make your baby seriously ill. Most group B strep infections in newborn babies are preventable.
For more information talk to your midwife, or visit the Group B Strep Support website.
Your pain management options for labour
There are lots of effective ways for managing pain during childbirth. You do not need to pick just one of them. You could start with one, and then move on to another.
Self-help
This is the use of relaxation techniques, moving around, and feeling empowered through knowing what is likely to happen during labour. Self help relaxation techniques mean that you are in control and there are no side effects. They may not work for everyone
Gas and air (Entonox)
This involves breathing in a mixture of oxygen and nitrous oxide gas through a face mask or mouthpiece. Gas and air:
- works quickly
- may make you feel sick
- may not take the pain away completely
Pethidine (or sometimes Diamorphine)
This is an injection of a drug into your thigh or bottom. Pethidine:
- can help you relax for around 2 to 4 hours
- takes about 20 minutes to work
- may make you feel sick
- is not suitable for late stages of labour as the drugs can interfere with the baby's feeding and breathing
Epidural
This is a local anaesthetic that numbs the nerves that tell your brain you're in pain. You are given an injection into the space outside your spine. Your baby's heart will be monitored throughout. An epidural:
You are given an injection into the space outside your spine. Your baby's heart will be monitored throughout. An epidural:
- can work well during a difficult labour
- is unlikely to make you feel sick
- needs to be given by an anaesthetist, so is not available everywhere
- could slow down your labour and you may need further intervention, such as a forceps delivery
- does not always work – around 1 in 8 women who have an epidural also need other types of pain relief
Water birth
This is where you give birth in a special pool kept at a comfortable temperature. The warm water feels soothing and it's easier to move around. Many hospitals and birth centres have birthing pools, you can also hire them for home births. If you choose to have a water birth:
- try not to get into the pool too early, as it can slow down labour
- you will need to leave the pool and get medical help if there are complications
TENS machine
A TENS machine delivers small amounts of electrical currents through pads on your back. It's believed to encourage the body to produce more of its own natural painkillers (endorphins). If you use a TENS machine:
It's believed to encourage the body to produce more of its own natural painkillers (endorphins). If you use a TENS machine:
- you may need to hire or buy your own machine
- it might help with early labour, but not for the later stages
- there are no side effects – it's drug-free and you're in control
Alternative methods
Some women choose complementary treatments such as acupuncture, aromatherapy and homeopathy. Talk to your doctor or midwife if you're planning to give birth at a hospital or midwifery unit, and would like a therapist to be with you in labour.
Things to bear in mind with alternative methods:
- there are no side effects for most of them
- there is no strong evidence that they work
Have a look at where to give birth and your options on the NHS website.
Discuss your ideas with your midwife, doctor and partner. Then write your preferences in your birth plan. Remember – you can change your mind on the day.
Read more about pain relief on the NHS website.
3rd trimester pregnancy symptoms (at 35 weeks)
You may be getting sore ribs now. That could be because your baby is head down, and kicking away. If the pain is really bad, or under your ribs, then talk to your midwife or doctor, just in case it's a sign of a condition called pre-eclampsia. However, it's more likely that your little one is just very active.
Your signs of pregnancy could also include:
- painless contractions around your bump, known as Braxton Hicks contractions
- sleeping problems (week 19 has information about feeling tired)
- stretch marks (read about stretch marks on week 17's page)
- swollen and bleeding gums (week 13 has information about gum health during pregnancy)
- pains on the side of your baby bump, caused by your expanding womb ("round ligament pains")
- piles (read about piles on week 22's page)
- headaches
- backache
- indigestion and heartburn (week 25 talks about digestive problems)
- bloating and constipation (read about bloating on week 16's page)
- leg cramps (week 20 explains how to deal with cramp)
- feeling hot
- dizziness
- swollen hands and feet
- urine infections
- vaginal infections (see week 15 for vaginal health)
- darkened skin on your face or brown patches – this is known as chloasma or the "mask of pregnancy"
- greasier, spotty skin
- thicker and shinier hair
You may also experience symptoms from earlier weeks, such as:
- mood swings (week 8's page has information on mood swings)
- morning sickness (read about dealing with morning sickness on week 6's page)
- weird pregnancy cravings (read about pregnancy cravings on week 5's page)
- a heightened sense of smell
- sore or leaky breasts (read about breast pain on week 14's page)
- a white milky pregnancy discharge from your vagina and light spotting (seek medical advice for any bleeding)
Read Tommy's guide to common pregnancy symptoms.
What does my baby look like?
Your baby is around 46.2cm long from head to heel, and weighs about 2.4kg. That's approximately the height of 2 bananas and the weight of a honeydew melon.
Your baby is getting chubbier, which will help them to stay at the right temperature when they're born.
It's getting rather cramped in your womb now, but your baby should still be moving around, and you should feel movements as strongly and regularly as you have done in previous weeks.
If the movements change or stop, then talk to your doctor, midwife or call NHS 111.
Action stations
Have you had the whooping cough jab yet? It's usually offered to pregnant women between 16 and 32 weeks – but it's not too late to have it now. This vaccine will protect your tiny baby from this dangerous disease for the first few weeks of their life. Talk to your midwife or doctor about the jab, if you haven't already.
This week you could also...
You have maternity rights. You can ask for a risk assessment of your work place to ensure that you're working in a safe environment. You should not be lifting heavy things and you may need extra breaks and somewhere to sit. You can also attend antenatal appointments during paid work time.
You can ask for a risk assessment of your work place to ensure that you're working in a safe environment. You should not be lifting heavy things and you may need extra breaks and somewhere to sit. You can also attend antenatal appointments during paid work time.
It's a good time to tone up your pelvic floor muscles. Gentle exercises can help to prevent leakage when you laugh, sneeze or cough. Get the muscles going by pretending that you're having a wee and then stopping midflow. Visit Tommy’s.org for more ideas about pelvic floor exercises.
Tommy's has lots of useful information on antenatal classes and preparing you for birth.
Even if you've had children before, antenatal classes are still worth going to as you can meet other parents-to-be. The NCT offers online antenatal classes with small groups of people that live locally to you.
To keep bones and muscles healthy, we need vitamin D. From late March/early April to the end of September, most people make enough vitamin D from sunlight on their skin.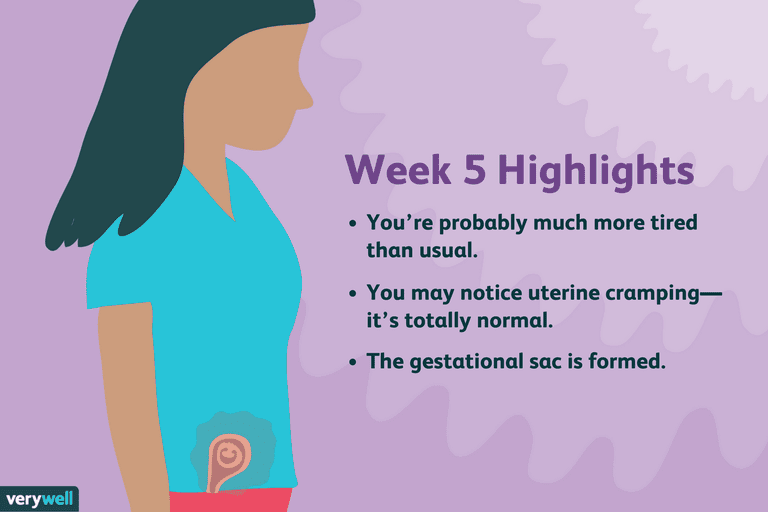 However, between October and early March, you should consider taking a daily vitamin D supplement because we cannot make enough from sunlight.
However, between October and early March, you should consider taking a daily vitamin D supplement because we cannot make enough from sunlight.
Some people should take a vitamin D supplement all year round, find out if this applies to you on the NHS website. You just need 10 micrograms (it's the same for grown-ups and kids). Check if you're entitled to free vitamins.
It's recommended that you do 150 minutes of exercise while pregnant. You could start off with just 10 minutes of daily exercise - perhaps take a brisk walk outside. Check out Sport England's #StayInWorkOut online exercises (scroll to the pregnancy section). Listen to your body and do what feels right for you.
There's no need to eat for 2. Now you're in the third trimester, you may need an extra 200 calories a day, but that's not much. It's about the same as 2 slices of wholemeal toast and margarine.
Try to eat healthily, with plenty of fresh fruit and veg, and avoid processed, fatty and salty foods. You may be able to get free milk, fruit and veg through the Healthy Start scheme.
You may be able to get free milk, fruit and veg through the Healthy Start scheme.
How are you today? If you're feeling anxious or low, then talk to your midwife or doctor who can point you in the right direction to get all the support that you need. You could also discuss your worries with your partner, friends and family.
You may be worried about your relationship, or money, or having somewhere permanent to live. Don't keep it to yourself. It's important that you ask for help if you need it.
Having another baby is probably the last thing on your mind. However now is a good time to start planning what type of contraception you would like to use after your baby is born. Getting pregnant again could happen sooner than you realise and too short a gap between babies is known to cause problems. Talk to your GP or midwife to help you decide.
You and your family should follow the government and NHS guidance on coronavirus (COVID-19):
To find out about about COVID-19 and pregnancy, childbirth and breastfeeding, have a look at advice on the:
Interventions for leg cramps during pregnancy
What is the problem?
Leg cramps manifest themselves as sudden, intense involuntary contractions of the leg muscles.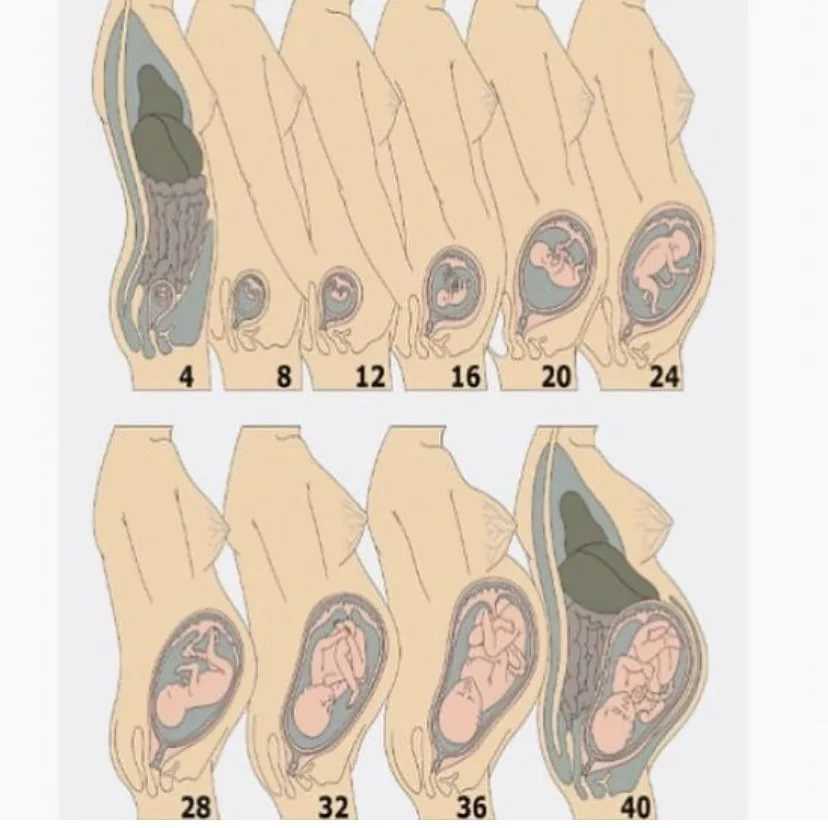 This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching. nine0005
This is a common problem during pregnancy, especially in the third trimester. They are painful and can interfere with daily activities, disrupt sleep, and reduce quality of life. Various types of interventions are used to treat leg cramps during pregnancy, including medications, electrolytes (magnesium, calcium, sodium) and vitamins, as well as non-drug therapies such as muscle stretching. nine0005
Why is this important?
The aim of this review was to find out which treatment for leg cramps during pregnancy is effective and safe.
What evidence did we find?
In September 2019, we searched for evidence and identified eight randomized controlled trials in 576 women 14 to 36 weeks pregnant comparing magnesium, calcium, calcium with vitamin D or B vitamins versus placebo or no treatment, and compared vitamin C with calcium. All drugs were given as tablets to chew or swallow. nine0005
All drugs were given as tablets to chew or swallow. nine0005
Magnesium supplements may reduce the incidence of leg cramps in women compared with placebo or no treatment, although studies have not been consistent. Different studies have assessed the effect of magnesium supplementation differently. Some studies have shown magnesium to help reduce the incidence of leg cramps, while others have shown little or no effect. Data on the effect of magnesium on pain reduction was also inconclusive, with only one study showing a reduction in pain intensity, while others showed no difference. Differences in the occurrence of side effects such as nausea and diarrhea were negligible or non-existent. nine0005
Calcium did not always reduce the incidence of leg cramps in women after treatment compared to those who did not receive any treatment. It also found that the evidence was of very low quality, so we cannot be sure of the results.
More women who received B-vitamin supplements made a full recovery compared to those who received no treatment; however, these results were based on a small sample size and the study had design limitations. nine0005
nine0005
Frequency of leg cramps did not differ between women receiving calcium and women receiving vitamin C. with placebo.
What does this mean?
The quality of the evidence was low to very low. This was mainly due to small study sample sizes and study design weaknesses. Four studies were well-conducted and presented their reports. The remaining four had flaws in their design: in several studies, women were not best assigned to different treatment groups, and in two studies, women knew whether they were receiving treatment or not. Adverse effects, such as the effect of treatment on complications of pregnancy, childbirth and child, were not reported. Several studies have focused primarily on serum calcium and magnesium levels. The frequency and intensity of seizures and duration of pain were not uniformly reported, and there was often no information on whether they were assessed during treatment, at the end of treatment, or after treatment was discontinued. nine0005
nine0005
It is not clear from the evidence reviewed whether any oral interventions (magnesium, calcium, calcium with vitamin D, B vitamins, vitamin D, or vitamin C) are an effective and safe treatment for leg cramps during pregnancy. Supplements can have different effects depending on how women usually take them. None of the trials looked at forms of treatment such as muscle stretching, massage, relaxation, or heat therapy.
Translation notes:
Translation: Luzan Maria Alexandrovna. Editing: Yudina Ekaterina Viktorovna. Russian translation project coordination: Cochrane Russia - Cochrane Russia, Cochrane Geographic Group Associated to Cochrane Nordic. For questions related to this transfer, please contact us at: [email protected]
Reduces legs during pregnancy: what to do?
Pregnancy is a time of waiting and doubts. Probably, women never have so many questions. Why does it bring her legs together so often? What to do if you wake up with cramps at night? How to deal with this scourge and avoid bouts of pain in the legs? We are looking for answers to these and other questions. nine0005
nine0005
What are seizures?
Legs cramps not only during pregnancy, from time to time every person faces unpleasant painful cramps. A cramp is a sudden, uncontrollable muscle contraction that a person cannot relax. This condition can be caused by neurological disorders (for example, seizures are characteristic of epilepsy), a number of diseases (such as diabetes mellitus, osteochondrosis, and others), and can also be associated with physiological conditions. After all, convulsions occur, for example, after a strong overload, dehydration, hypothermia, etc. Sometimes cramps cause severe sharp pain. Sometimes it seems that the legs are pulling. During pregnancy, this condition, unfortunately, is noted quite regularly. nine0005
Why do pregnant women cramp their legs?
The mechanism of muscle contraction is quite complex, it involves different ions (charged particles): potassium, calcium, sodium and magnesium. If we are talking about a cramp, that is, a condition when we cannot relax a muscle, then magnesium ions play a leading role here. It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
It is their lack that leads to the fact that women cramp their calves during pregnancy at night.
The lack of minerals in the body of the expectant mother is simply explained: such consequences are the restructuring of metabolism and functioning in the "double load" mode. In particular, the expectant mother needs one and a half times more magnesium than usual. nine0005
In addition to helping muscles relax, magnesium is also involved in a number of important physiological processes. In particular, magnesium is needed to regulate the processes of formation and expenditure of energy, it is involved in several hundred enzymatic reactions, and if there is little magnesium, then disturbances can occur in the work of almost any body system. Therefore, if magnesium preparations are prescribed during pregnancy, this recommendation should not be ignored. nine0005
Why do pregnant women cramp their legs at night?
The answer to this question is very simple. The fact is that during the day the body of the expectant mother bears an increased load. And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
And the longer the gestation period, the greater this load. Violation of blood circulation, increased stress on the muscles - all this can cause night cramps.
What should I do if my legs cramp during pregnancy?
To begin with, tell the doctor you are seeing about this. The magnesium preparations already mentioned, which he most likely recommends to you, can help solve the problem. nine0005
However, the reason that the expectant mother cramps her legs during pregnancy may be not only a metabolic disorder. Often muscle spasms begin as a result of varicose veins - the "faithful" companion of pregnancy. The veins of a woman carrying a baby are subject to increased stress. In addition, hormonal changes in the body seriously affect the state of blood vessels. All this contributes to the development of varicose veins. And a violation of the blood supply to the muscles of the legs, in turn, leads to convulsions.
If the expectant mother is faced with varicose veins, then the best prevention of its progression is to wear compression stockings selected by the doctor in accordance with the gestational age.