Pregnancy thyroid hormone
Thyroid Disease & Pregnancy | NIDDK
On this page:
- What role do thyroid hormones play in pregnancy?
- Hyperthyroidism in Pregnancy
- Hypothyroidism in Pregnancy
- Postpartum Thyroiditis
- Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
- Thyroid Disease and Eating During Pregnancy
- Clinical Trials
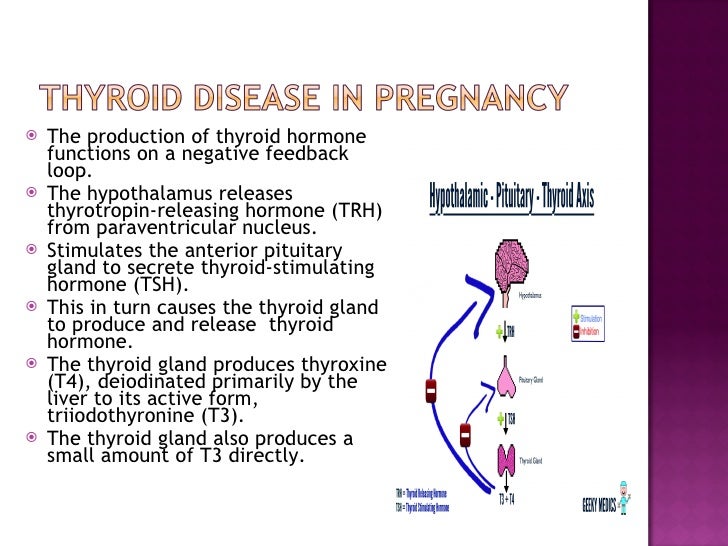
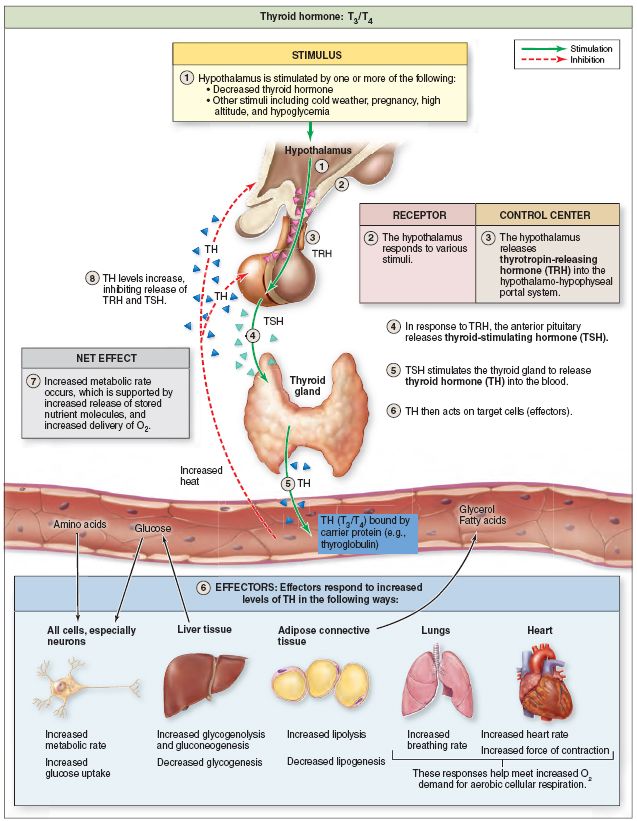
Thyroid disease is a group of disorders that affects the thyroid gland. The thyroid is a small, butterfly-shaped gland in the front of your neck that makes thyroid hormones. Thyroid hormones control how your body uses energy, so they affect the way nearly every organ in your body works—even the way your heart beats.
The thyroid is a small gland in your neck that makes thyroid hormones.Sometimes the thyroid makes too much or too little of these hormones. Too much thyroid hormone is called hyperthyroidism and can cause many of your body’s functions to speed up. “Hyper” means the thyroid is overactive. Learn more about hyperthyroidism in pregnancy. Too little thyroid hormone is called hypothyroidism and can cause many of your body’s functions to slow down. “Hypo” means the thyroid is underactive. Learn more about hypothyroidism in pregnancy.
If you have thyroid problems, you can still have a healthy pregnancy and protect your baby’s health by having regular thyroid function tests and taking any medicines that your doctor prescribes.
What role do thyroid hormones play in pregnancy?
Thyroid hormones are crucial for normal development of your baby’s brain and nervous system. During the first trimester—the first 3 months of pregnancy—your baby depends on your supply of thyroid hormone, which comes through the placenta. At around 12 weeks, your baby’s thyroid starts to work on its own, but it doesn’t make enough thyroid hormone until 18 to 20 weeks of pregnancy.
Two pregnancy-related hormones—human chorionic gonadotropin (hCG) and estrogen—cause higher measured thyroid hormone levels in your blood.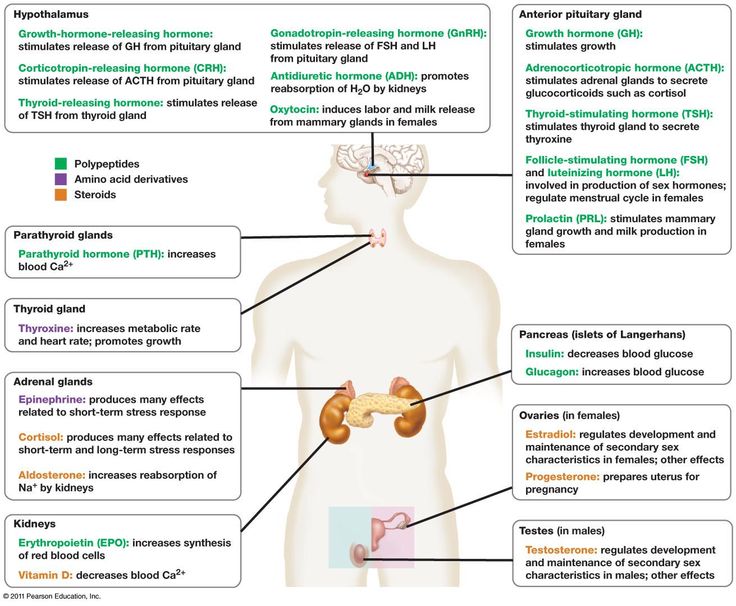 The thyroid enlarges slightly in healthy women during pregnancy, but usually not enough for a health care professional to feel during a physical exam.
The thyroid enlarges slightly in healthy women during pregnancy, but usually not enough for a health care professional to feel during a physical exam.
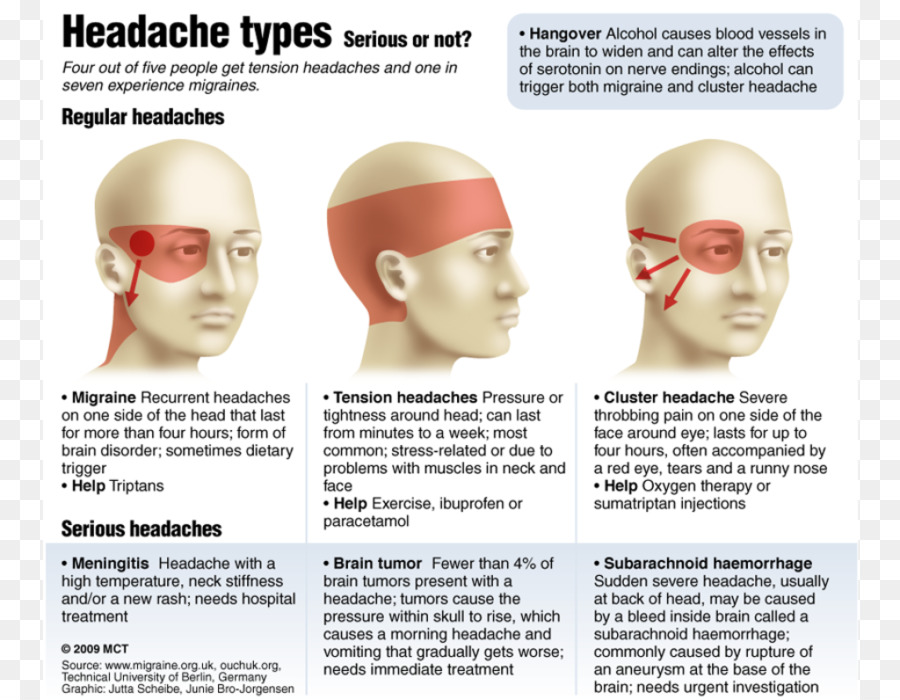
Thyroid problems can be hard to diagnose in pregnancy due to higher levels of thyroid hormones and other symptoms that occur in both pregnancy and thyroid disorders. Some symptoms of hyperthyroidism or hypothyroidism are easier to spot and may prompt your doctor to test you for these thyroid diseases.
Another type of thyroid disease, postpartum thyroiditis, can occur after your baby is born.
Hyperthyroidism in Pregnancy
What are the symptoms of hyperthyroidism in pregnancy?
Some signs and symptoms of hyperthyroidism often occur in normal pregnancies, including faster heart rate, trouble dealing with heat, and tiredness.
Other signs and symptoms can suggest hyperthyroidism:
- fast and irregular heartbeat
- shaky hands
- unexplained weight loss or failure to have normal pregnancy weight gain
What causes hyperthyroidism in pregnancy?
Hyperthyroidism in pregnancy is usually caused by Graves’ disease and occurs in 1 to 4 of every 1,000 pregnancies in the United States. 1 Graves’ disease is an autoimmune disorder. With this disease, your immune system makes antibodies that cause the thyroid to make too much thyroid hormone. This antibody is called thyroid stimulating immunoglobulin, or TSI.
1 Graves’ disease is an autoimmune disorder. With this disease, your immune system makes antibodies that cause the thyroid to make too much thyroid hormone. This antibody is called thyroid stimulating immunoglobulin, or TSI.
Graves’ disease may first appear during pregnancy. However, if you already have Graves’ disease, your symptoms could improve in your second and third trimesters. Some parts of your immune system are less active later in pregnancy so your immune system makes less TSI. This may be why symptoms improve. Graves’ disease often gets worse again in the first few months after your baby is born, when TSI levels go up again. If you have Graves’ disease, your doctor will most likely test your thyroid function monthly throughout your pregnancy and may need to treat your hyperthyroidism.1 Thyroid hormone levels that are too high can harm your health and your baby’s.
If you have Graves’ disease, your doctor will most likely test your thyroid function monthly during your pregnancy.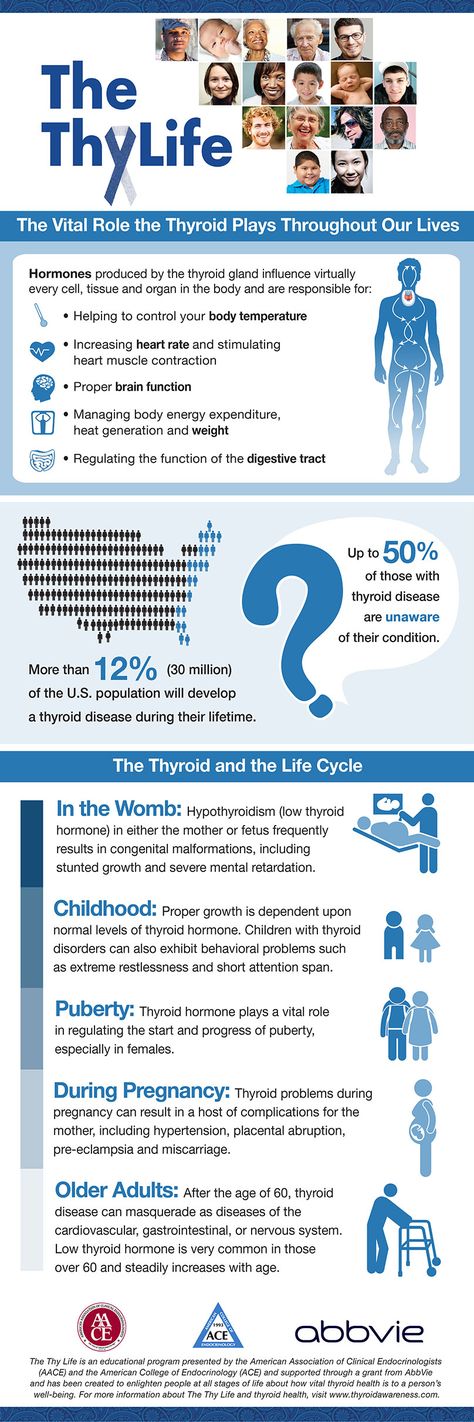
Rarely, hyperthyroidism in pregnancy is linked to hyperemesis gravidarum—severe nausea and vomiting that can lead to weight loss and dehydration. Experts believe this severe nausea and vomiting is caused by high levels of hCG early in pregnancy. High hCG levels can cause the thyroid to make too much thyroid hormone. This type of hyperthyroidism usually goes away during the second half of pregnancy.
Less often, one or more nodules, or lumps in your thyroid, make too much thyroid hormone.
How can hyperthyroidism affect me and my baby?
Untreated hyperthyroidism during pregnancy can lead to
- miscarriage
- premature birth
- low birthweight
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- thyroid storm—a sudden, severe worsening of symptoms
- congestive heart failure
Rarely, Graves’ disease may also affect a baby’s thyroid, causing it to make too much thyroid hormone. Even if your hyperthyroidism was cured by radioactive iodine treatment to destroy thyroid cells or surgery to remove your thyroid, your body still makes the TSI antibody.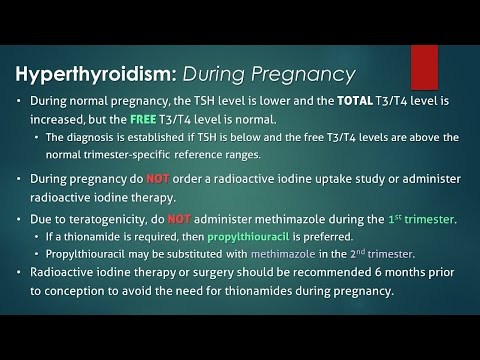 When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
When levels of this antibody are high, TSI may travel to your baby’s bloodstream. Just as TSI caused your own thyroid to make too much thyroid hormone, it can also cause your baby’s thyroid to make too much.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease so he or she can check your TSI levels. If they are very high, your doctor will monitor your baby for thyroid-related problems later in your pregnancy.
Tell your doctor if you’ve had surgery or radioactive iodine treatment for Graves’ disease.An overactive thyroid in a newborn can lead to
- a fast heart rate, which can lead to heart failure
- early closing of the soft spot in the baby’s skull
- poor weight gain
- irritability
Sometimes an enlarged thyroid can press against your baby’s windpipe and make it hard for your baby to breathe. If you have Graves’ disease, your health care team should closely monitor you and your newborn.
How do doctors diagnose hyperthyroidism in pregnancy?
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for antibodies in your blood to see if Graves’ disease is causing your hyperthyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hyperthyroidism during pregnancy?
If you have mild hyperthyroidism during pregnancy, you probably won’t need treatment. If your hyperthyroidism is linked to hyperemesis gravidarum, you only need treatment for vomiting and dehydration.
If your hyperthyroidism is more severe, your doctor may prescribe antithyroid medicines, which cause your thyroid to make less thyroid hormone. This treatment prevents too much of your thyroid hormone from getting into your baby’s bloodstream. You may want to see a specialist, such as an endocrinologist or expert in maternal-fetal medicine, who can carefully monitor your baby to make sure you’re getting the right dose.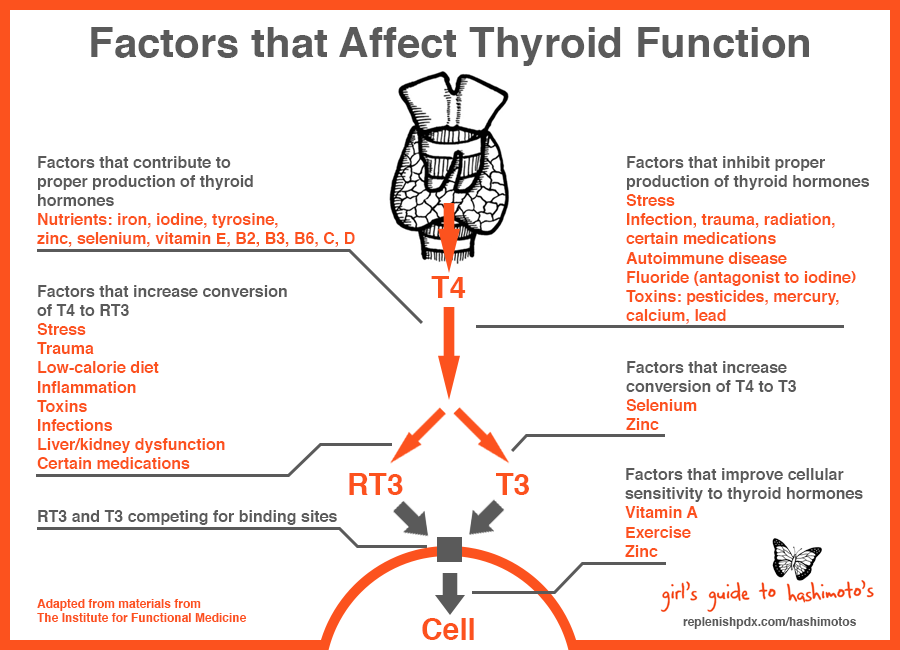
Doctors most often treat pregnant women with the antithyroid medicine propylthiouracil (PTU) during the first 3 months of pregnancy. Another type of antithyroid medicine, methimazole, is easier to take and has fewer side effects, but is slightly more likely to cause serious birth defects than PTU. Birth defects with either type of medicine are rare. Sometimes doctors switch to methimazole after the first trimester of pregnancy. Some women no longer need antithyroid medicine in the third trimester.
Small amounts of antithyroid medicine move into the baby’s bloodstream and lower the amount of thyroid hormone the baby makes. If you take antithyroid medicine, your doctor will prescribe the lowest possible dose to avoid hypothyroidism in your baby but enough to treat the high thyroid hormone levels that can also affect your baby.
Antithyroid medicines can cause side effects in some people, including
- allergic reactions such as rashes and itching
- rarely, a decrease in the number of white blood cells in the body, which can make it harder for your body to fight infection
- liver failure, in rare cases
Stop your antithyroid medicine and call your doctor right away if you develop any of these symptoms while taking antithyroid medicines:
- yellowing of your skin or the whites of your eyes, called jaundice
- dull pain in your abdomen
- constant sore throat
- fever
If you don’t hear back from your doctor the same day, you should go to the nearest emergency room.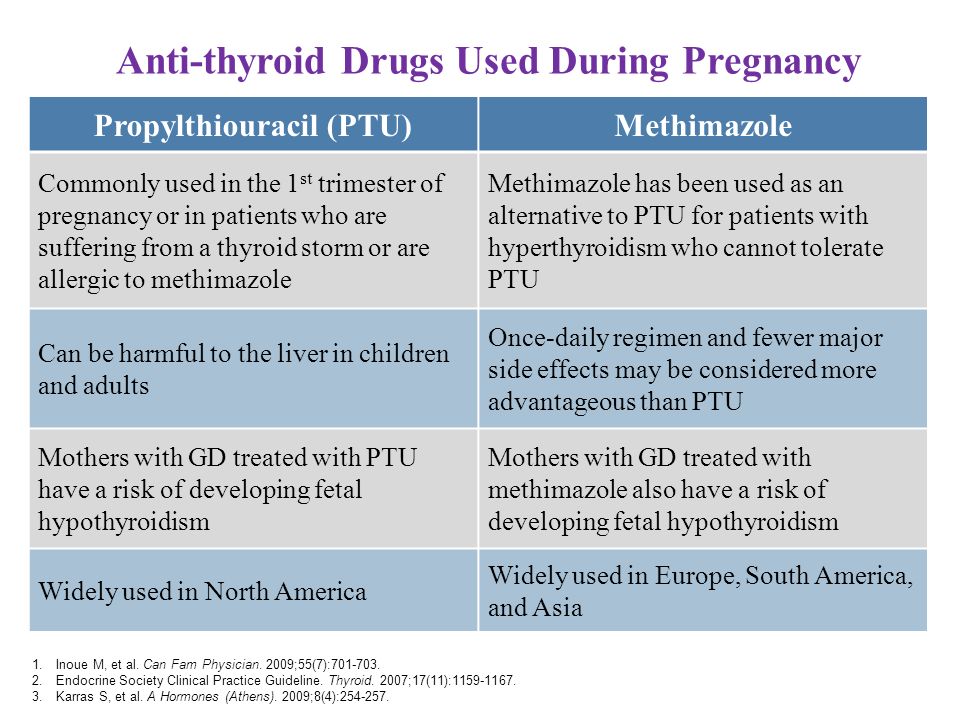
You should also contact your doctor if any of these symptoms develop for the first time while you’re taking antithyroid medicines:
- increased tiredness or weakness
- loss of appetite
- skin rash or itching
- easy bruising
If you are allergic to or have severe side effects from antithyroid medicines, your doctor may consider surgery to remove part or most of your thyroid gland. The best time for thyroid surgery during pregnancy is in the second trimester.
Radioactive iodine treatment is not an option for pregnant women because it can damage the baby’s thyroid gland.
Hypothyroidism in Pregnancy
What are the symptoms of hypothyroidism in pregnancy?
Symptoms of an underactive thyroid are often the same for pregnant women as for other people with hypothyroidism. Symptoms include
- extreme tiredness
- trouble dealing with cold
- muscle cramps
- severe constipation
- problems with memory or concentration
Most cases of hypothyroidism in pregnancy are mild and may not have symptoms.
What causes hypothyroidism in pregnancy?
Hypothyroidism in pregnancy is usually caused by Hashimoto’s disease and occurs in 2 to 3 out of every 100 pregnancies.1 Hashimoto’s disease is an autoimmune disorder. In Hashimoto’s disease, the immune system makes antibodies that attack the thyroid, causing inflammation and damage that make it less able to make thyroid hormones.
How can hypothyroidism affect me and my baby?
Untreated hypothyroidism during pregnancy can lead to
- preeclampsia—a dangerous rise in blood pressure in late pregnancy
- anemia
- miscarriage
- low birthweight
- stillbirth
- congestive heart failure, rarely
These problems occur most often with severe hypothyroidism.
Because thyroid hormones are so important to your baby’s brain and nervous system development, untreated hypothyroidism—especially during the first trimester—can cause low IQ and problems with normal development.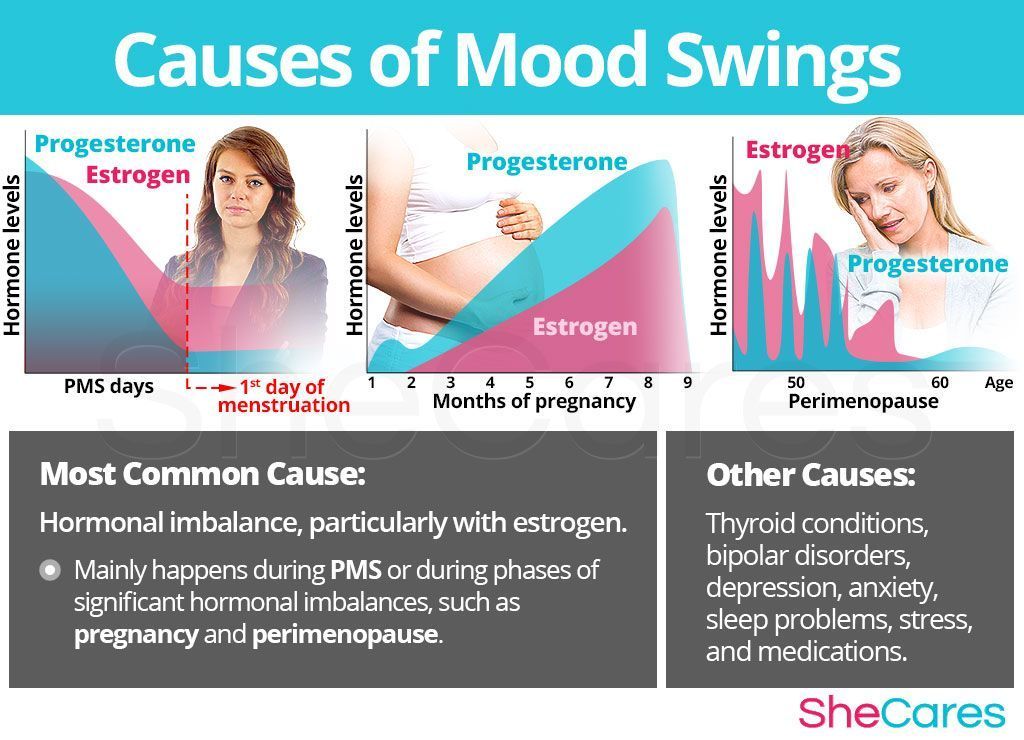
How do doctors diagnose hypothyroidism in pregnancy?
Your doctor will review your symptoms and do some blood tests to measure your thyroid hormone levels. Your doctor may also look for certain antibodies in your blood to see if Hashimoto’s disease is causing your hypothyroidism. Learn more about thyroid tests and what the results mean.
How do doctors treat hypothyroidism during pregnancy?
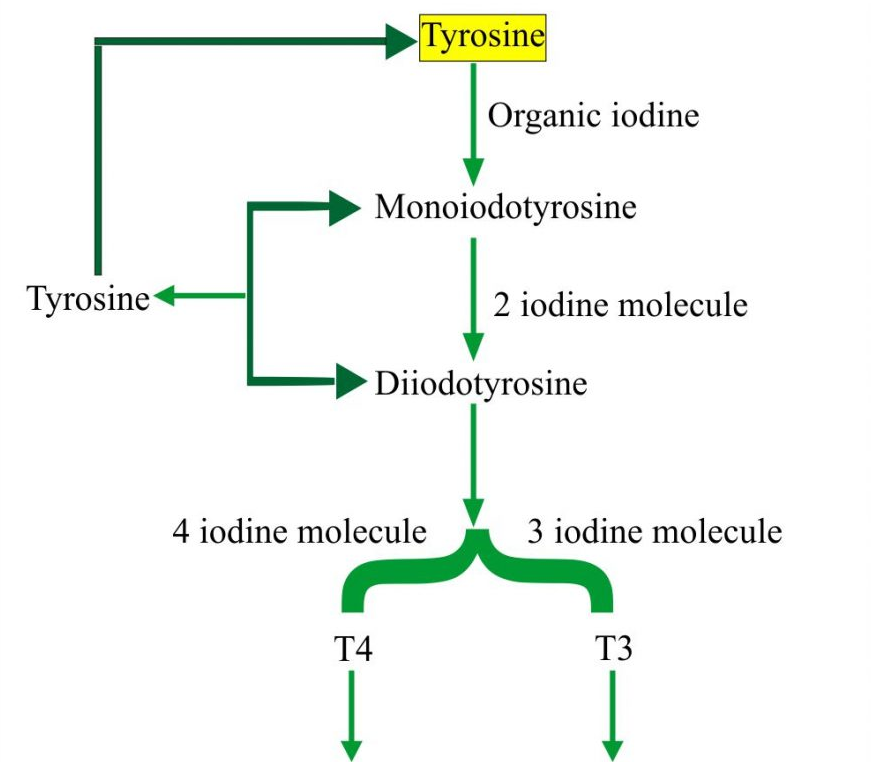
Treatment for hypothyroidism involves replacing the hormone that your own thyroid can no longer make. Your doctor will most likely prescribe levothyroxine, a thyroid hormone medicine that is the same as T4, one of the hormones the thyroid normally makes. Levothyroxine is safe for your baby and especially important until your baby can make his or her own thyroid hormone.
Your thyroid makes a second type of hormone, T3. Early in pregnancy, T3 can’t enter your baby’s brain like T4 can. Instead, any T3 that your baby’s brain needs is made from T4. T3 is included in a lot of thyroid medicines made with animal thyroid, such as Armour Thyroid, but is not useful for your baby’s brain development.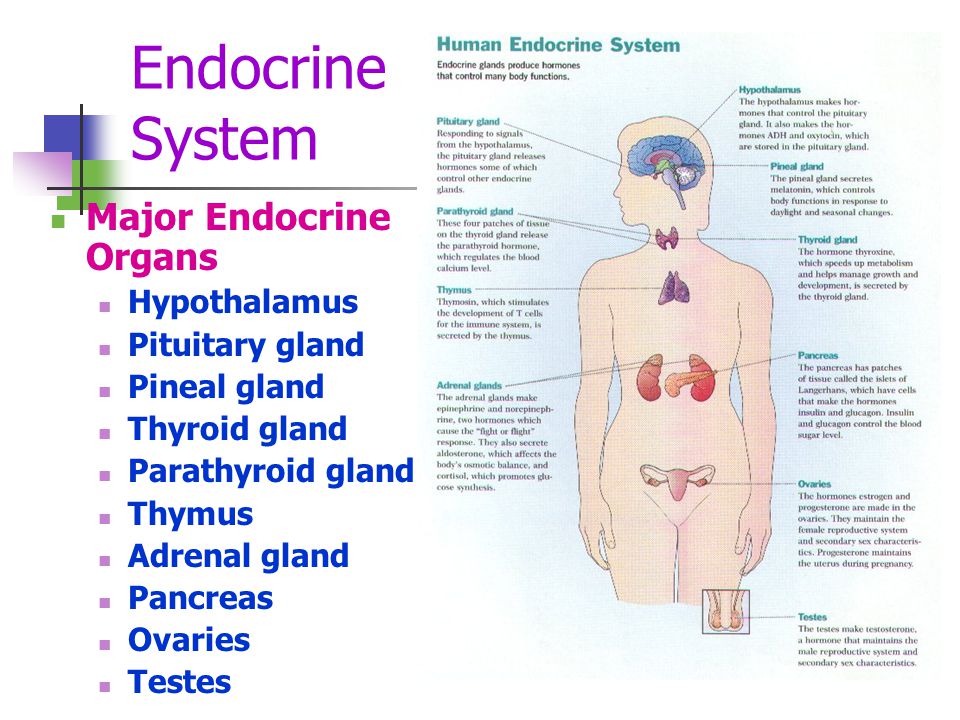 These medicines contain too much T3 and not enough T4, and should not be used during pregnancy. Experts recommend only using levothyroxine (T4) while you’re pregnant.
These medicines contain too much T3 and not enough T4, and should not be used during pregnancy. Experts recommend only using levothyroxine (T4) while you’re pregnant.
Some women with subclinical hypothyroidism—a mild form of the disease with no clear symptoms—may not need treatment.
Your doctor may prescribe levothyroxine to treat your hypothyroidism.If you had hypothyroidism before you became pregnant and are taking levothyroxine, you will probably need to increase your dose. Most thyroid specialists recommend taking two extra doses of thyroid medicine per week, starting right away. Contact your doctor as soon as you know you’re pregnant.
Your doctor will most likely test your thyroid hormone levels every 4 to 6 weeks for the first half of your pregnancy, and at least once after 30 weeks.1 You may need to adjust your dose a few times.
Postpartum Thyroiditis
What is postpartum thyroiditis?
Postpartum thyroiditis is an inflammation of the thyroid that affects about 1 in 20 women during the first year after giving birth1 and is more common in women with type 1 diabetes. The inflammation causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage raises the hormone levels in your blood, leading to hyperthyroidism. The hyperthyroidism may last up to 3 months. After that, some damage to your thyroid may cause it to become underactive. Your hypothyroidism may last up to a year after your baby is born. However, in some women, hypothyroidism doesn’t go away.
The inflammation causes stored thyroid hormone to leak out of your thyroid gland. At first, the leakage raises the hormone levels in your blood, leading to hyperthyroidism. The hyperthyroidism may last up to 3 months. After that, some damage to your thyroid may cause it to become underactive. Your hypothyroidism may last up to a year after your baby is born. However, in some women, hypothyroidism doesn’t go away.
Not all women who have postpartum thyroiditis go through both phases. Some only go through the hyperthyroid phase, and some only the hypothyroid phase.
What are the symptoms of postpartum thyroiditis?
The hyperthyroid phase often has no symptoms—or only mild ones. Symptoms may include irritability, trouble dealing with heat, tiredness, trouble sleeping, and fast heartbeat.
Symptoms of the hypothyroid phase may be mistaken for the “baby blues”—the tiredness and moodiness that sometimes occur after the baby is born. Symptoms of hypothyroidism may also include trouble dealing with cold; dry skin; trouble concentrating; and tingling in your hands, arms, feet, or legs. If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
If these symptoms occur in the first few months after your baby is born or you develop postpartum depression, talk with your doctor as soon as possible.
What causes postpartum thyroiditis?
Postpartum thyroiditis is an autoimmune condition similar to Hashimoto’s disease. If you have postpartum thyroiditis, you may have already had a mild form of autoimmune thyroiditis that flares up after you give birth.
Postpartum thyroiditis may last up to a year after your baby is born.How do doctors diagnose postpartum thyroiditis?
If you have symptoms of postpartum thyroiditis, your doctor will order blood tests to check your thyroid hormone levels.
How do doctors treat postpartum thyroiditis?
The hyperthyroid stage of postpartum thyroiditis rarely needs treatment. If your symptoms are bothering you, your doctor may prescribe a beta-blocker, a medicine that slows your heart rate. Antithyroid medicines are not useful in postpartum thyroiditis, but if you have Grave’s disease, it may worsen after your baby is born and you may need antithyroid medicines.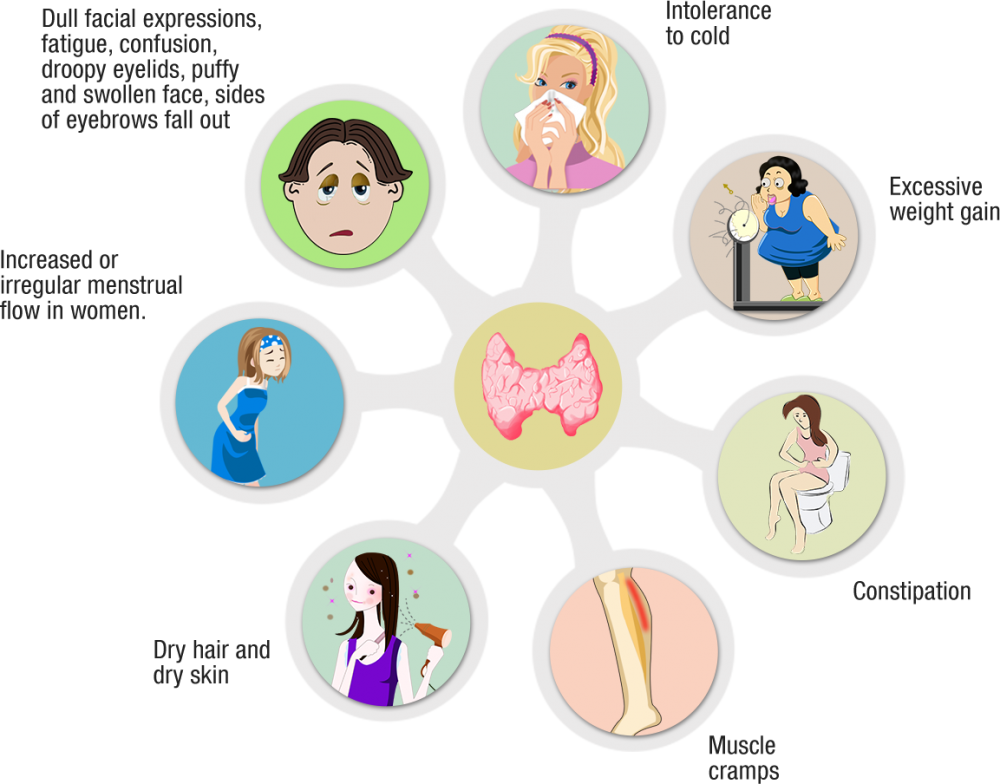
You’re more likely to have symptoms during the hypothyroid stage. Your doctor may prescribe thyroid hormone medicine to help with your symptoms. If your hypothyroidism doesn’t go away, you will need to take thyroid hormone medicine for the rest of your life.
Is it safe to breastfeed while I’m taking beta-blockers, thyroid hormone, or antithyroid medicines?
Certain beta-blockers are safe to use while you’re breastfeeding because only a small amount shows up in breast milk. The lowest possible dose to relieve your symptoms is best. Only a small amount of thyroid hormone medicine reaches your baby through breast milk, so it’s safe to take while you’re breastfeeding. However, in the case of antithyroid drugs, your doctor will most likely limit your dose to no more than 20 milligrams (mg) of methimazole or, less commonly, 400 mg of PTU.
Thyroid Disease and Eating During Pregnancy
What should I eat during pregnancy to help keep my thyroid and my baby’s thyroid working well?
Because the thyroid uses iodine to make thyroid hormone, iodine is an important mineral for you while you’re pregnant.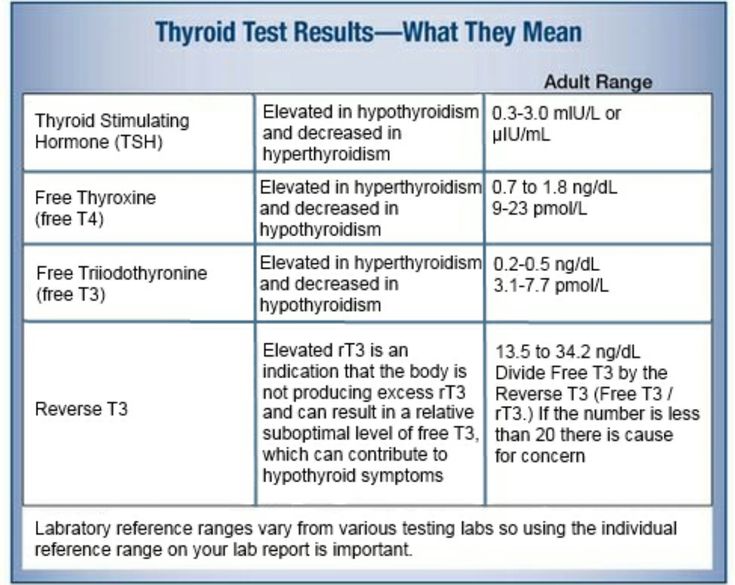 During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
During pregnancy, your baby gets iodine from your diet. You’ll need more iodine when you’re pregnant—about 250 micrograms a day.1 Good sources of iodine are dairy foods, seafood, eggs, meat, poultry, and iodized salt—salt with added iodine. Experts recommend taking a prenatal vitamin with 150 micrograms of iodine to make sure you’re getting enough, especially if you don’t use iodized salt.1 You also need more iodine while you’re breastfeeding since your baby gets iodine from breast milk. However, too much iodine from supplements such as seaweed can cause thyroid problems. Talk with your doctor about an eating plan that’s right for you and what supplements you should take. Learn more about a healthy diet and nutrition during pregnancy.
Clinical Trials
The National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and other components of the National Institutes of Health (NIH) conduct and support research into many diseases and conditions.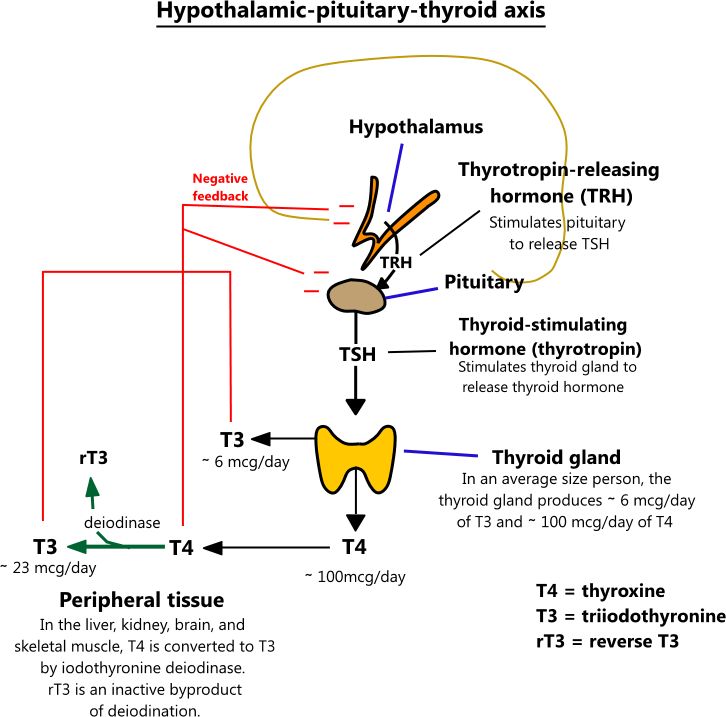
What are clinical trials, and are they right for you?
Clinical trials are part of clinical research and at the heart of all medical advances. Clinical trials look at new ways to prevent, detect, or treat disease. Researchers also use clinical trials to look at other aspects of care, such as improving the quality of life for people with chronic illnesses. Find out if clinical trials are right for you.
What clinical trials are open?
Clinical trials that are currently open and are recruiting can be viewed at www.ClinicalTrials.gov.
References
Thyroid function during pregnancy - PubMed
Review
. 1999 Dec;45(12):2250-8.
C R Fantz 1 , S Dagogo-Jack, J H Ladenson, A M Gronowski
Affiliations
Affiliation
- 1 Department of Pathology and Division of Endocrinology, Washington University School of Medicine, Saint Louis, MO 63110, USA.
- PMID: 10585360
Review
C R Fantz et al. Clin Chem. 1999 Dec.
. 1999 Dec;45(12):2250-8.
Authors
C R Fantz 1 , S Dagogo-Jack, J H Ladenson, A M Gronowski
Affiliation
- 1 Department of Pathology and Division of Endocrinology, Washington University School of Medicine, Saint Louis, MO 63110, USA.
- PMID: 10585360
Abstract
Background: This Case Conference reviews the normal changes in thyroid activity that occur during pregnancy and the proper use of laboratory tests for the diagnosis of thyroid dysfunction in the pregnant patient.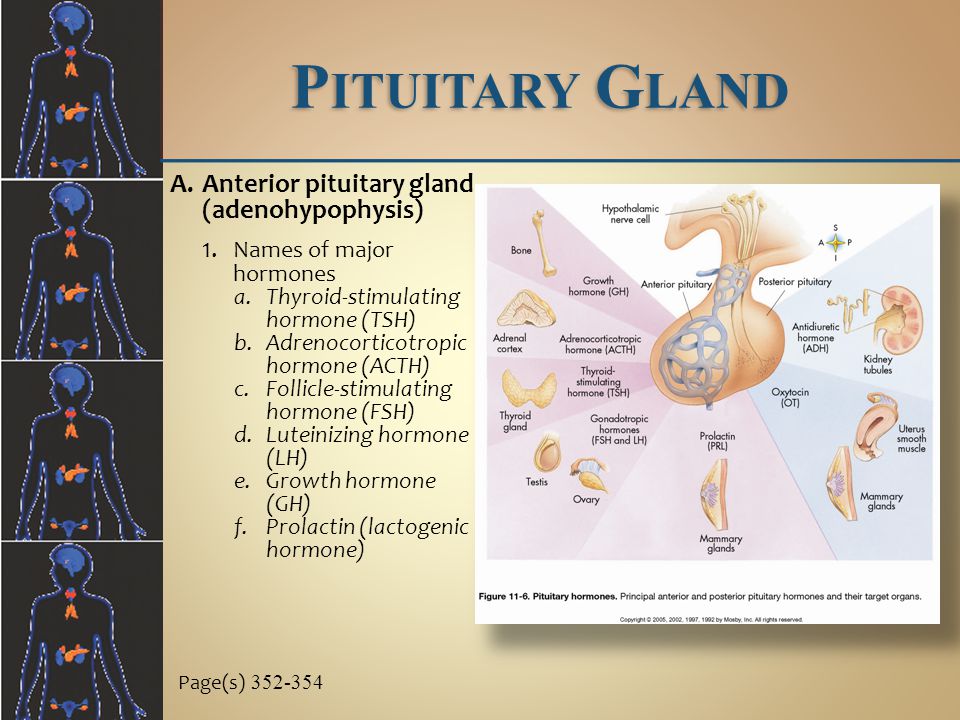
Case: A woman in the 18th week of pregnancy presented with tachycardia, increased blood pressure, severe vomiting, increased total and free thyroid hormone concentrations, a thyroid-stimulating hormone (TSH) concentration within the reference interval, and an increased human chorionic gonadotropin (hCG) beta-subunit concentration.
Issues: During pregnancy, normal thyroid activity undergoes significant changes, including a two- to threefold increase in thyroxine-binding globulin concentrations, a 30-100% increase in total triiodothyronine and thyroxine concentrations, increased serum thyroglobulin, and increased renal iodide clearance. Furthermore, hCG has mild thyroid stimulating activity. Pregnancy produces an overall increase in thyroid activity, which allows the healthy individual to remain in a net euthyroid state. However, both hyper- and hypothyroidism can occur in pregnant patients.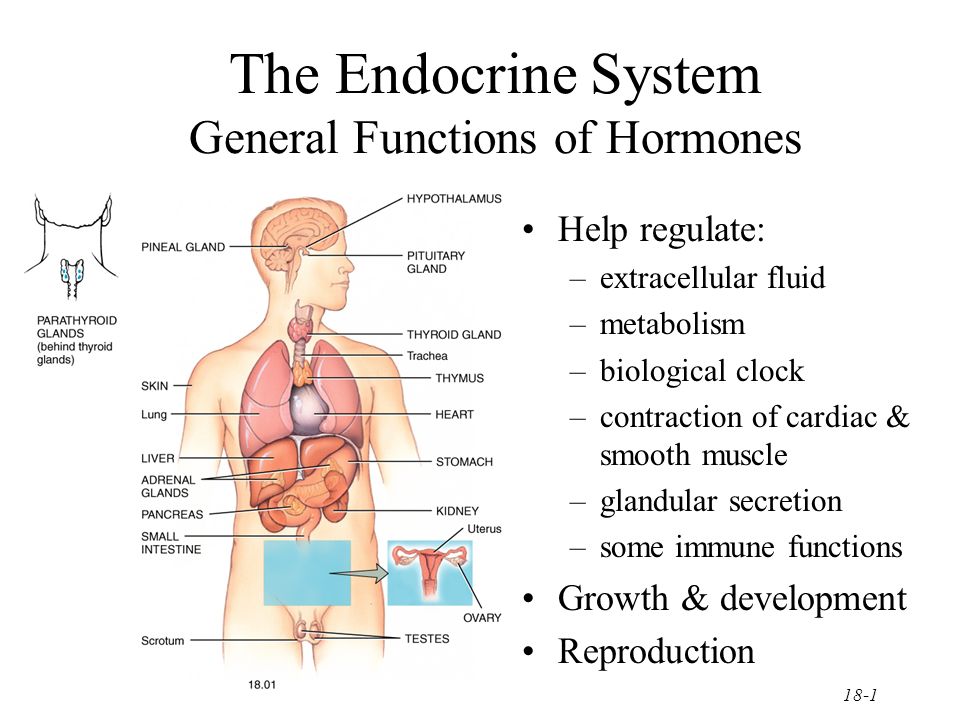 In addition, two pregnancy-specific conditions, hyperemesis gravidarum and gestational trophoblastic disease, can lead to clinical hyperthyroidism. The normal changes in thyroid activity and the association of pregnancy with conditions that can cause hyperthyroidism necessitates careful interpretation of thyroid function tests during pregnancy.
In addition, two pregnancy-specific conditions, hyperemesis gravidarum and gestational trophoblastic disease, can lead to clinical hyperthyroidism. The normal changes in thyroid activity and the association of pregnancy with conditions that can cause hyperthyroidism necessitates careful interpretation of thyroid function tests during pregnancy.
Conclusion: Assessment of thyroid function during pregnancy should be done with a careful clinical evaluation of the patient's symptoms as well as measurement of TSH and free, not total, thyroid hormones. Measurement of thyroid autoantibodies may also be useful in selected cases to detect maternal Graves disease or Hashimoto thyroiditis and to assess risk of fetal or neonatal consequences of maternal thyroid dysfunction.
Similar articles
-
Human chorionic gonadotropin and the thyroid: hyperemesis gravidarum and trophoblastic tumors.
Hershman JM. Hershman JM. Thyroid. 1999 Jul;9(7):653-7. doi: 10.1089/thy.1999.9.653. Thyroid. 1999. PMID: 10447009 Review.
-
Nausea, vomiting and thyroid function before and after induced abortion in normal pregnancy.
Appierto U, Subrizi DA, Minozzi M, Unfer V. Appierto U, et al. Clin Exp Obstet Gynecol. 1996;23(1):18-20. Clin Exp Obstet Gynecol. 1996. PMID: 8653928
-
Thyroid disorders associated with pregnancy: etiology, diagnosis, and management.
Lazarus JH. Lazarus JH. Treat Endocrinol. 2005;4(1):31-41. doi: 10.2165/00024677-200504010-00004. Treat Endocrinol. 2005. PMID: 15649099 Review.
-
Urinary iodine excretion and maternal thyroid function.
 During pregnancy and postpartum.
During pregnancy and postpartum. Ardawi MS, Nasrat HA, Mustafa BE. Ardawi MS, et al. Saudi Med J. 2002 Apr;23(4):413-22. Saudi Med J. 2002. PMID: 11953767
-
[Thyroid gland and pregnancy--physiology and pathology].
Łacka K, Łakoma H. Łacka K, et al. Wiad Lek. 2002;55(7-8):450-62. Wiad Lek. 2002. PMID: 12428574 Review. Polish.
See all similar articles
Cited by
-
Association between isolated maternal hypothyroxinemia during the first trimester and adverse pregnancy outcomes in Southern Chinese women: a retrospective study of 7051 cases.
Li P, Cui J, Li L, Chen X, Ouyang L, Fan J, Lin S. Li P, et al. BMC Pregnancy Childbirth.
 2022 Nov 23;22(1):866. doi: 10.1186/s12884-022-05194-w. BMC Pregnancy Childbirth. 2022. PMID: 36424562 Free PMC article.
2022 Nov 23;22(1):866. doi: 10.1186/s12884-022-05194-w. BMC Pregnancy Childbirth. 2022. PMID: 36424562 Free PMC article. -
Expression of mitochondrial protein genes encoded by nuclear and mitochondrial genomes correlate with energy metabolism in dairy cattle.
Dorji J, Vander Jagt CJ, Garner JB, Marett LC, Mason BA, Reich CM, Xiang R, Clark EL, Cocks BG, Chamberlain AJ, MacLeod IM, Daetwyler HD. Dorji J, et al. BMC Genomics. 2020 Oct 19;21(1):720. doi: 10.1186/s12864-020-07018-7. BMC Genomics. 2020. PMID: 33076826 Free PMC article.
-
Cell Type- and Sex-Specific Dysregulation of Thyroid Hormone Receptors in Placentas in Gestational Diabetes Mellitus.
Knabl J, de Maiziere L, Hüttenbrenner R, Hutter S, Jückstock J, Mahner S, Kainer F, Desoye G, Jeschke U.
 Knabl J, et al. Int J Mol Sci. 2020 Jun 5;21(11):4056. doi: 10.3390/ijms21114056. Int J Mol Sci. 2020. PMID: 32517091 Free PMC article.
Knabl J, et al. Int J Mol Sci. 2020 Jun 5;21(11):4056. doi: 10.3390/ijms21114056. Int J Mol Sci. 2020. PMID: 32517091 Free PMC article. -
Thyroid Screening During Early Pregnancy and the Need for Trimester Specific Reference Ranges: A Cross-Sectional Study in Lahore, Pakistan.
Talat A, Khan AA, Nasreen S, Wass JA. Talat A, et al. Cureus. 2019 Sep 15;11(9):e5661. doi: 10.7759/cureus.5661. Cureus. 2019. PMID: 31720137 Free PMC article.
-
Human chorionic gonadotropin promotes cell proliferation through the activation of c-Met in gastric cancer cells.
Zhao R, Zhang T, Xi W, Sun X, Zhou L, Guo Y, Zhao C, Bao Y. Zhao R, et al. Oncol Lett. 2018 Oct;16(4):4271-4278. doi: 10.3892/ol.2018.9215. Epub 2018 Jul 25.
 Oncol Lett. 2018. PMID: 30197669 Free PMC article.
Oncol Lett. 2018. PMID: 30197669 Free PMC article.
See all "Cited by" articles
Publication types
MeSH terms
Substances
Thyroid gland and pregnancy - GAUZ City Clinical Hospital No. 9
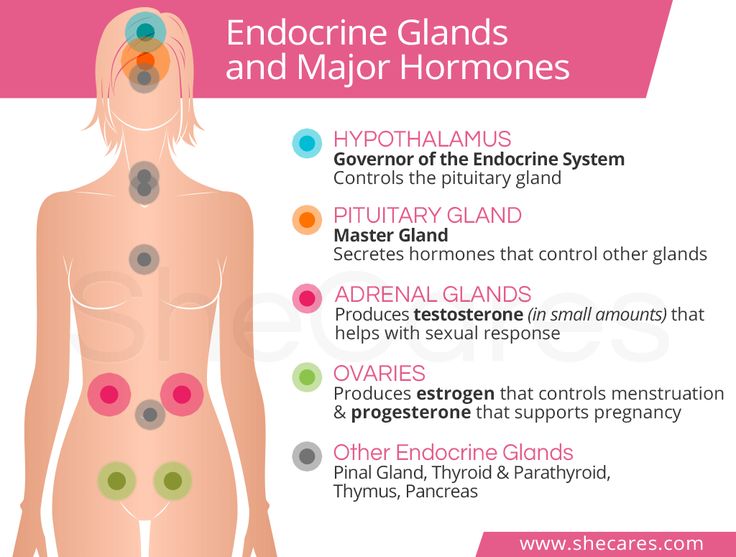
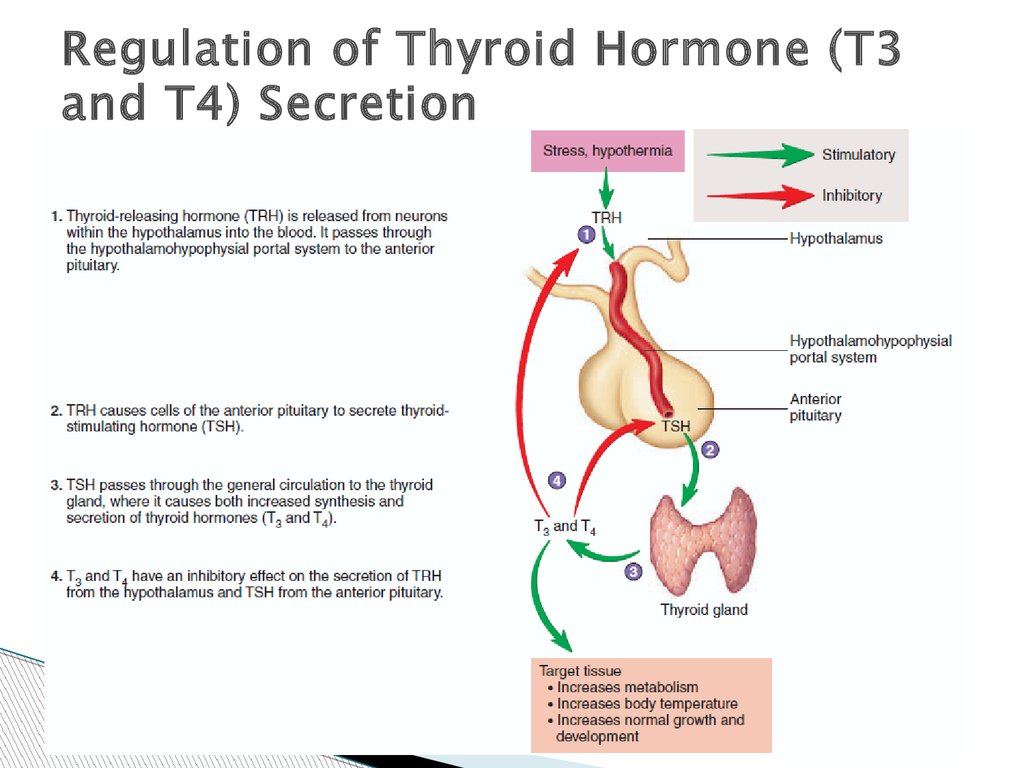
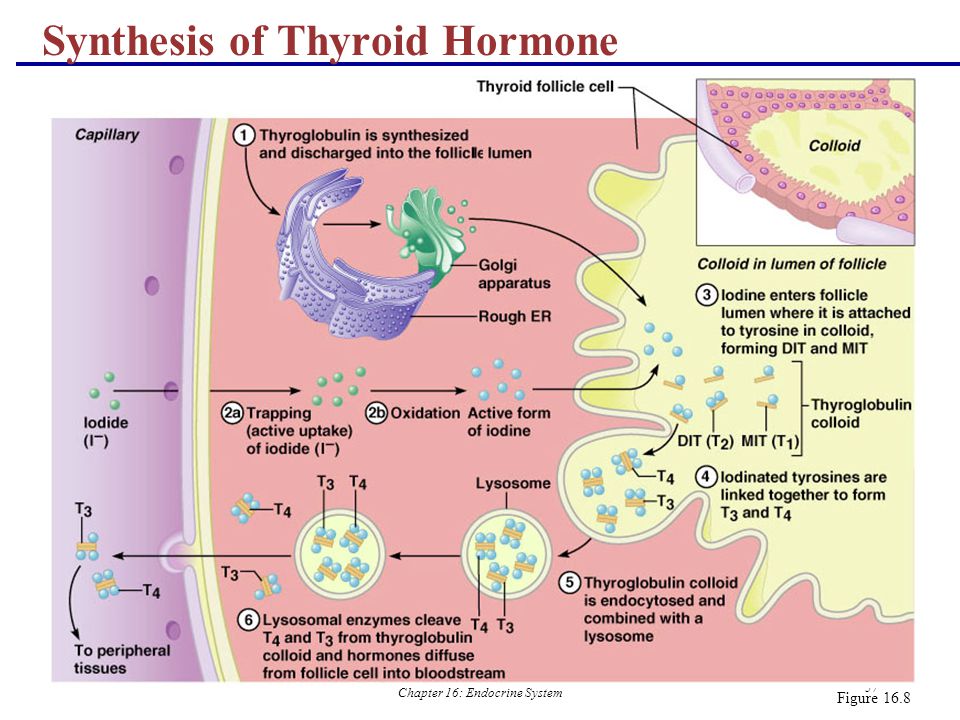
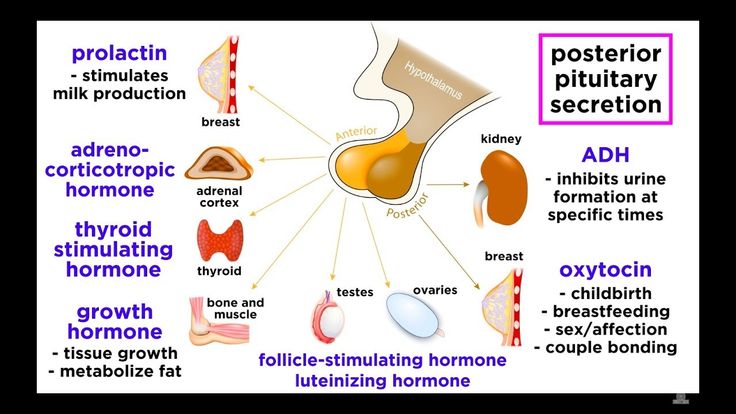
The thyroid gland is a small, butterfly-shaped organ located on the front of the neck. Its weight is on average 18-30 and depends on the region of residence. The thyroid gland produces the most important hormones for the body: thyroxine (or T4) and triiodothyronine (TK), the material for them is amino acid and iodine. The functions of the thyroid gland are monitored by the "superior" glands - the pituitary gland (which produces the thyroid-stimulating hormone TSH) and the hypothalamus. nine0005
nine0005
Thyroid hormones perform a number of important functions in the body. First of all, they regulate the basic metabolism, i.e. the production of energy necessary for the life of the whole organism. Also, thyroid hormones affect the laying and intrauterine development of such organs and systems of the child as the nervous, cardiovascular, reproductive systems, musculoskeletal system, etc. In the first three years of life, they are especially important for the normal functioning of the brain, in the future, for the development and maintenance of intelligence. nine0005
In order for the thyroid gland to be able to produce the hormones T3 and T4 in the amount necessary for the body, 150-200 micrograms of iodine with food should enter the human body per day. During pregnancy and lactation, this need increases to 250-300 mcg. A large territory of Russia, including the Ural region, is a zone of iodine deficiency, therefore, meat, fish, dairy and vegetable products eaten do not satisfy the body's daily need for iodine. Together with the deteriorating environmental situation, harmful, but common habits of young people (smoking, alcohol), this leads to the development of iodine deficiency conditions. nine0005
Together with the deteriorating environmental situation, harmful, but common habits of young people (smoking, alcohol), this leads to the development of iodine deficiency conditions. nine0005
An underactive thyroid (hypothyroidism) and an overactive thyroid (hyperthyroidism) cause certain problems. How do they threaten a pregnant woman and her offspring?
Iodine deficiency can lead to low levels of thyroid hormones even before pregnancy. Therefore, when planning a pregnancy, it is very important to consult an endocrinologist, especially if you notice any signs of hypothyroidism (weakness, weight gain, drowsiness, decreased memory and speed of thinking, dry skin, brittle nails, hair loss, menstrual irregularities). , decreased blood pressure, hoarseness). nine0005
The thyroid gland and pregnancy.
If you find that you have a decrease in thyroid function and find out the cause, most likely, the doctor will prescribe you replacement therapy, i.e. “Add” a certain amount of thyroxine to the body.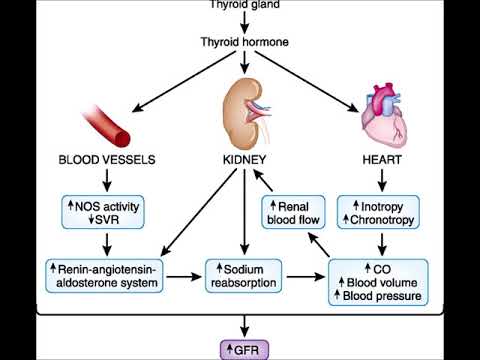 Thyroxine will also need to be taken during pregnancy and breastfeeding.
Thyroxine will also need to be taken during pregnancy and breastfeeding.
Hypothyroidism during pregnancy can lead to spontaneous abortion, fetal death, the birth of a child with malformations, mental retardation, psychomotor disorders. To avoid these complications, in addition to taking thyroxin, it is necessary to carry out iodine prophylaxis: daily take a drug containing potassium iodide at a dose of 250 mcg. Hormone doses are set only by an endocrinologist, so his consultations are necessary during pregnancy. In addition to adding tableted iodine, it is necessary to include seafood (shrimp, seaweed, squid), dairy products, and meat in the diet of a pregnant woman. It must be remembered that from the first weeks of pregnancy, the unborn child receives hormones and trace elements from the mother. The laying of the thyroid gland in the fetus occurs by 4-5 weeks of intrauterine development, from the 12th week this thyroid gland is able to synthesize hormones by itself, and by the 16th week it is fully formed and functioning.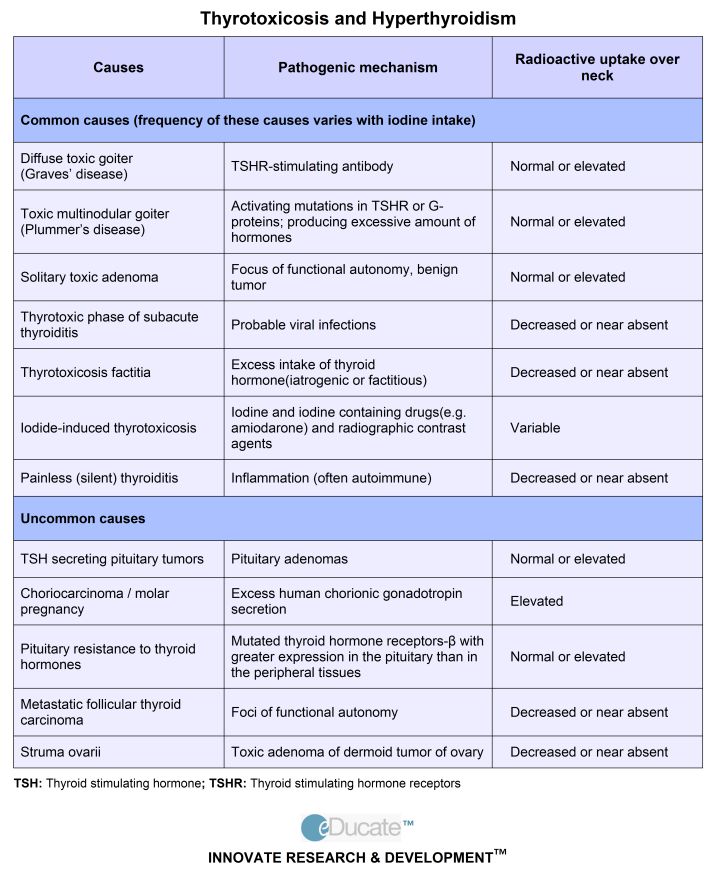 But the only source of iodine for her is the iodine circulating in the mother's blood. nine0005
But the only source of iodine for her is the iodine circulating in the mother's blood. nine0005
In the first trimester, the mother's thyroid gland works hard, "covering" the unformed thyroid gland of the fetus. This is manifested by temporary (transient) hyperthyroidism. Most often it does not require any treatment and goes away on its own. But diffuse toxic goiter (DTG) may develop, requiring timely treatment. Possible complaints in hyperthyroidism: weakness, weight loss, feeling hot, hot skin, irritability, nervousness, tearfulness, palpitations, rapid pulse, increased blood pressure, muscle weakness, trembling of the hands, body, loose stools, sweating, menstrual irregularities, shine eyes, widened palpebral fissures. nine0005
Having such complaints, a pregnant woman should report them to her gynecologist and be sure to consult an endocrinologist. After all, mood changes, sensations of heat, vomiting, some weight loss can be manifestations of early toxicosis or symptoms of diffuse toxic goiter.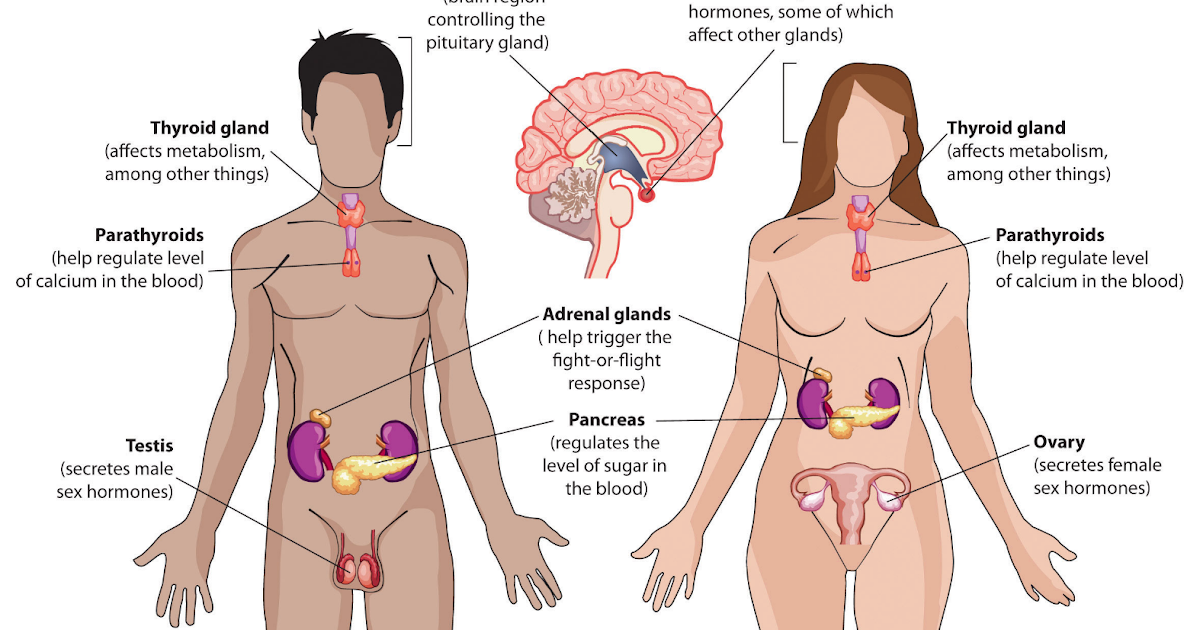 In addition, with diffuse toxic goiter, an increase in the thyroid gland, tachycardia (more than 100 beats per minute), the difference between systolic and diastolic pressure will attract attention. The main diagnostic role is played by the determination of the content of the level of thyroid hormones and thyroid-stimulating hormone of the pituitary gland. nine0005
In addition, with diffuse toxic goiter, an increase in the thyroid gland, tachycardia (more than 100 beats per minute), the difference between systolic and diastolic pressure will attract attention. The main diagnostic role is played by the determination of the content of the level of thyroid hormones and thyroid-stimulating hormone of the pituitary gland. nine0005
The prognosis for the mother and fetus depends on how much hyperthyroidism is compensated.
With hyperthyroidism, premature birth, malformations of the newborn, low fetal weight, severe gestosis, severe fetal hypothyroidism are possible.
In all cases, the treatment of thyrotoxicosis is carried out by a doctor !!!
Very low doses are used to suppress maternal thyroid function, and sometimes surgery is required.
After childbirth, the woman's immune system, which was suppressed during pregnancy, is restored. There is a surge in the activity of the immune system, antibodies are produced that destroy thyroid cells. In 3-5% of young mothers, postpartum thyroiditis develops 1-3 months after birth. Its peculiarity is the change of the phase of a moderate increase in the function of the thyroid gland by the phase of a moderate decrease in its function. As a rule, after 6-8 months, the immune system returns to normal and postpartum thyroiditis disappears. It must be remembered that postpartum thyroiditis increases the likelihood of developing persistent hypothyroidism in the future with all its clinical manifestations that interfere with normal life. nine0005
In 3-5% of young mothers, postpartum thyroiditis develops 1-3 months after birth. Its peculiarity is the change of the phase of a moderate increase in the function of the thyroid gland by the phase of a moderate decrease in its function. As a rule, after 6-8 months, the immune system returns to normal and postpartum thyroiditis disappears. It must be remembered that postpartum thyroiditis increases the likelihood of developing persistent hypothyroidism in the future with all its clinical manifestations that interfere with normal life. nine0005
In summary, it is recommended that all women planning pregnancy have their thyroid function tested before it occurs. Timely iodine prophylaxis will prevent the birth of children with low intellectual abilities. If a woman went to the doctor after pregnancy, the thyroid gland should be examined as early as possible and start taking iodine-containing drugs. It must be remembered that a high need for iodine persists in children immediately after birth and those who are both natural and artificially fed. A nursing mother should continue taking iodine supplements for the entire period of feeding. If the child is on artificial feeding, it is necessary to use milk mixtures with a high content of iodine. nine0005
A nursing mother should continue taking iodine supplements for the entire period of feeding. If the child is on artificial feeding, it is necessary to use milk mixtures with a high content of iodine. nine0005
Thus, you will provide your offspring with a good level of thyroid hormones, which means you will improve the formation of his cognitive abilities, improve intellectual development, in the future this will manifest itself in a high IQ of the child and reduce his morbidity.
Obstetrician-gynecologist, endocrinologist MBUZ City Clinical Hospital No. 9,
Chernysheva EV
Thyroid gland and pregnancy / Endocrinology / Articles about health / Articles and encyclopedia / madez.ru
The thyroid gland has a huge impact on the reproductive function of women. Thyroid hormones:
- regulate the processes of development, maturation, specialization and renewal of all fetal tissues;
- are of exceptional importance for the laying and development of the fetal brain;
- form the child's intelligence, learning ability, IQ;
- growth and maturation of the bone skeleton, the reproductive system of the child.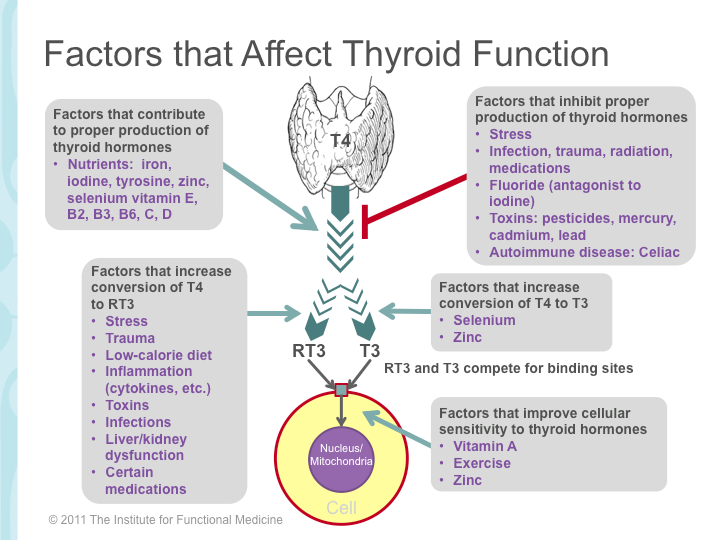
Thyroid hormones are made from dietary iodine. If before pregnancy the production of thyroid hormones is relatively stable, then from the first weeks of pregnancy there is already a change in the functioning of the thyroid gland. Changes in the hormonal system, metabolism in the first trimester of pregnancy directly or indirectly stimulate the thyroid gland of a woman. In the first trimester of pregnancy, the fetal thyroid gland does not yet function (until the 15th week of pregnancy) and the high need for thyroid hormones in the fetus, namely the correct and high-quality development of the fetus, the formation of its central nervous system, thyroid gland, other organs and systems, is provided only for due to the sufficient content of mother's hormones, especially in the first trimester of pregnancy, when the fetal organs are laid. In general, the production of thyroid hormones during pregnancy normally increases up to 50%. nine0005
Even after the beginning of the synthesis of hormones by the thyroid gland of the fetus in the 2nd half of pregnancy, maternal hormones do not lose their role.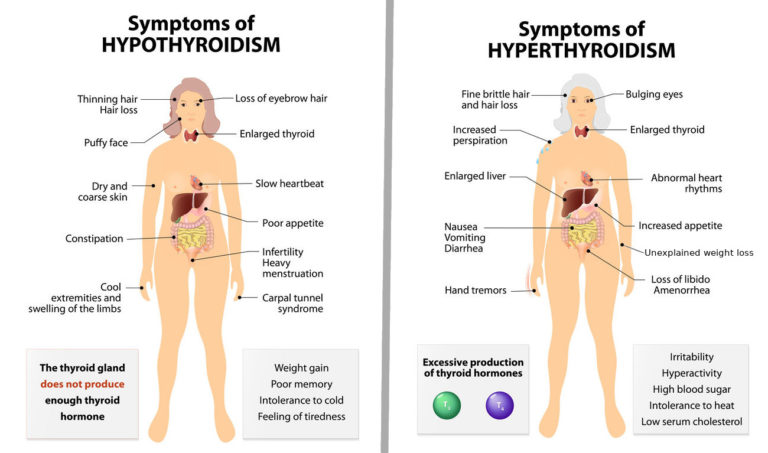
Diseases of the maternal thyroid gland can have a significant effect on the synthesis of thyroid hormones by the maternal gland and lead to insufficient or excessive amounts for the fetus.
So, according to modern ideas about the effect of thyroid pathology on reproduction, several postulates can be formulated:
1. During pregnancy there is a change in the functioning of the mother's thyroid gland.
2. Pregnancy is a powerful factor that stimulates the thyroid gland, which under certain conditions can acquire pathological significance.
3. For the normal development of the fetus, especially in the early stages, a normal level of maternal thyroid hormones is necessary
4. The principles of diagnosis and treatment of thyroid diseases in pregnant women differ significantly from standard diagnostic and treatment approaches
5. Both low and high thyroid function can cause a decrease in reproductive capacity in women and are a risk factor for fetal malformations.
6. Pregnancy can develop both against the background of hypothyroidism (decreased thyroid function) and against the background of thyrotoxicosis (increased thyroid function)
7. Indications for termination of pregnancy in women with impaired thyroid function are significantly limited.
8. Indications for surgical treatment of thyroid pathology during pregnancy are significantly limited. nine0005
9.During pregnancy, the impaired function of the thyroid gland is corrected with medications in accordance with the accepted principles of treatment of pregnant women.
Necessary examinations.
Currently, thyroid function testing in healthy women is not included in the mandatory recommendations for preparing for pregnancy. Nevertheless, there are clinical recommendations with a good degree of evidence, accepted all over the world, which say that the best conditions for conception, gestation, and fetal development exist precisely at certain intervals of thyroid hormones (TSH, T4f) both before conception and during pregnancy.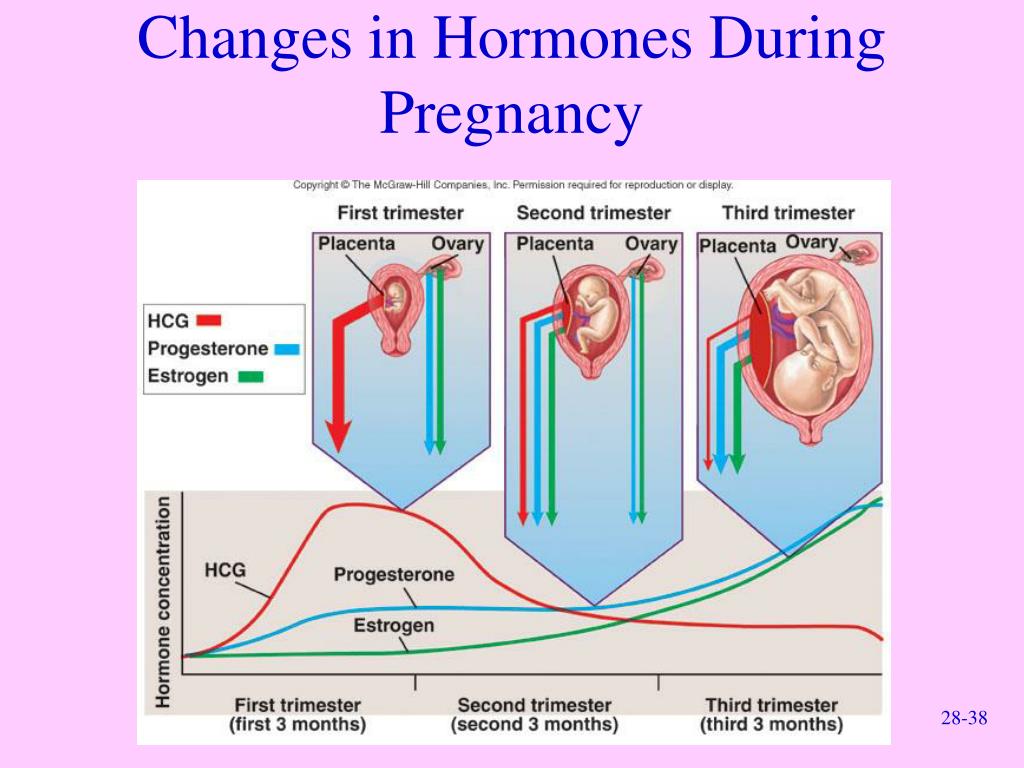 during pregnancy, especially in the 1st trimester. nine0005
during pregnancy, especially in the 1st trimester. nine0005
Thus, the best TSH interval for conception is in the range of 0.4-2.5 MED / l with normal T4 values. If TSH falls out of the required intervals, it is possible to correct the content of hormones.
According to the laws of physiology, TSH should decrease in the 1st half of pregnancy, sometimes quite strongly; T4 levels should rise, sometimes to the upper limit of normal. In the 2nd half of pregnancy, TSH levels out, increases compared to the low level in the 1st half; T4 may be normal or low normal. nine0005
Recently, the reference intervals (permissible content) of thyroid hormones in pregnant women in the 1st, 2nd, 3rd trimesters of pregnancy have changed, an endocrinologist's consultation is required.
Different approaches to women with thyroid disorders. You need constant monitoring and treatment by an endocrinologist, control of thyroid hormones with a certain regularity, which depends on the type of disease.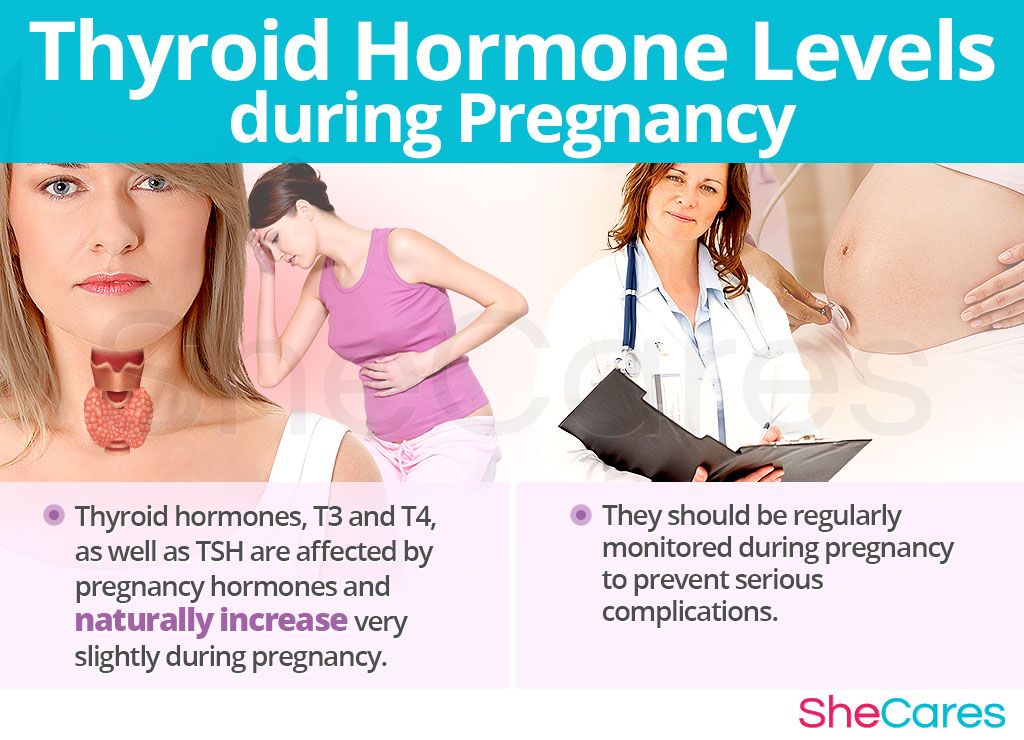
If you have been assigned to determine AT/TPO and their increase is revealed, you should not sound the alarm. The so-called "AT/TPO carriage" is a common phenomenon in the population, it is determined in healthy women and does not always have a prognostic value. Among pregnant women, AT/TPO are detected in at least 10% of cases and do not have a pathological effect on the fetus. nine0005
Nevertheless, an increase in AT/TPO can be a diagnostic criterion for xp. autoimmune thyroiditis, as well as to have a prognostic value in the development of postpartum thyroiditis and hypothyroidism (decreased thyroid function) in the future, consultation with an endocrinologist is required.
Ultrasound of the thyroid gland during pregnancy is not contraindicated.
Needle biopsy of thyroid nodules during pregnancy is not contraindicated at any stage of pregnancy. Nodes with a size greater than 1 cm and with progressive growth, especially during pregnancy, are subject to mandatory biopsy.