Pregnancy burping after eating
7 Safe Home Remedies for Gas During Pregnancy
Medically reviewed by Fernando Mariz, MD — By Juliann Schaeffer — Updated on February 12, 2021
Share on PinterestSDI Productions/Getty ImagesWe include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Got gas while pregnant? You’re not alone. Gas is a common (and potentially embarrassing) symptom of pregnancy.
You’re likely paying special attention to what you eat and the medications you ingest right now, which often means that typical gas remedies should be shelved for the time being.
Fortunately, there are several home remedies that can help ease any gas troubles you’re having, and some are as easy as reaching for a tall glass of water.
Your body goes through many changes during pregnancy, and unfortunately gas is an uncomfortable result of some very normal body processes, says Sheryl Ross, MD, an OB/GYN and women’s health expert at Providence Saint John’s Health Center in Santa Monica, California.
The hormone progesterone is one of the main causes of excess gas during pregnancy. As your body produces more progesterone to support your pregnancy, progesterone relaxes muscles in your body.
This includes the muscles of your intestine. Slower moving intestine muscles mean that your digestion slows down. This allows gas to build up, which in turn leads to bloating, burping, and flatulence.
Learn more about how your body changes during pregnancy.
Once you get further along in your pregnancy, the increased pressure from your growing uterus on your abdominal cavity can slow down digestion, leading to more gas.
Some foods can also contribute to gas, and your prenatal vitamins (especially the iron component) can cause constipation, leading, you guessed it, to even more gas.
This uncomfortable, and sometimes painful, gas is generally due to constipation, and it can get worse as your pregnancy progresses.
Thankfully, there are various things you can do to combat the gas. The more consistent you are with these lifestyle changes, the better results you’re likely to see.
The more consistent you are with these lifestyle changes, the better results you’re likely to see.
1. Drink plenty of fluids
Water is your best bet. Aim for eight to 10 (8-ounce) glasses every day, but other fluids count too.
If your gas is causing pain or extreme bloating, you may have irritable bowel syndrome (IBS), in which case make sure any juice you drink is low in certain types of gas and bloating-promoting sugars called FODMAPs.
Cranberry, grape, pineapple, and orange juice are all considered low-FODMAP juices.
Be sure to monitor sugar intake when drinking juices and sodas, especially if you’re at an increased risk for developing gestational diabetes.
Also, many varieties of carbonated drinks can lead to more gas.
2. Get moving
Physical activity and exercise should be a part of your daily routine. If you can’t make it to a gym, add a daily walk to your routine. Aim to walk or exercise for at least 30 minutes.
Not only can exercise help keep you physically and emotionally fit, but it can also help prevent constipation and speed up digestion.
Be sure to consult your obstetrician first before starting any exercise regimen during pregnancy.
Learn more about how to safely exercise in the third trimester of pregnancy.
3. Test out your diet
Try removing potential food triggers from your diet one at a time, until your gas symptoms improve, recommends Brett Worly, MD, an assistant professor in the OB/GYN department at the Ohio State University Wexner Medical Center.
It’s recommended that you continue to eat a balanced diet while doing any form of elimination diet.
Weight gain is necessary for most pregnancies, so it’s important to avoid restrictive diets.
That way, you’re only eliminating foods that are contributing to the problem. Brussels sprouts, cabbage, broccoli, wheat, and potatoes are common gas culprits, says Worly.
Some women experience IBS during pregnancy, but talk with your doctor and dietitian before starting a low-FODMAP diet.
This diet can be very restrictive and put you and your baby at risk for not getting adequate nutrition.
4. Fill up on fiber
Many foods that make gas worse in the short term can actually help manage constipation.
Why? “Fiber brings water into the intestines, softening the stool and allowing it [to pass more easily],” explains Ross.
Try including 25 to 30 grams of high fiber foods into your diet to help ease gas concerns.
Many fruits, such as prunes, figs, and bananas, and vegetables as well as whole grains like oats and flax meal are all good fiber boosters to consider.
5. Ask about fiber supplements
If you’re not a fan of high fiber foods, or you’re looking for a quick and easy alternative, ask your doctor about whether a fiber supplement, such as psyllium (Metamucil), methylcellulose (Citrucel), or polyethylene glycol 3350 (MiraLAX), might benefit you.
You can buy Metamucil, Citrucel, or MiraLAX online.
6. … And stool softeners
Docusate (Colace), a gentle stool softener, moistens the stool, allowing easier and regular passage. Only take docusate if you’re experiencing constipation or having too much gas.
Only take docusate if you’re experiencing constipation or having too much gas.
Ross encourages women to take 50 to 100 mg of docusate two times a day throughout the duration of their pregnancy.
It’s important to avoid any stimulant laxatives, such as sennosides (Ex-Lax, Senokot), as these can cause complications during pregnancy.
7. When in doubt, just breathe
Anxiety and stress can increase the amount of air you swallow, which may increase upper abdominal gas, bloating, and belching, says Michael R. Berman, MD, medical director of labor and delivery at Mount Sinai Beth Israel Medical Center.
Try to eliminate as much stress from your life as possible. Here are several recommendations:
- Assign chores to someone else, or allow yourself to accept that they may not get done at a specific time — or at all — and that’s OK.
- Find some quiet time during the day to take some deep breaths and relax, or look into a prenatal spa day.
- Do whatever you need to do to stay calm.

Gas isn’t always a laughing matter.
To ensure something more serious isn’t going on, seek immediate medical attention if you have severe pain without improvement for more than 30 minutes or constipation for more than 1 week.
Otherwise, choose the remedies that work best for your lifestyle. Then stick with them because consistency is key.
“Pregnancy is not a sprint; it’s a marathon,” says Ross. “So pace yourself and keep a healthy and positive attitude as it relates to your diet and exercise.”
Gas During Pregnancy: Causes and Prevention
Gas during pregnancy is a frequent occurrence, which also means that gas during pregnancy is a common concern. The typical person will pass gas approximately 18 times a day. The reason for this is that the average person produces up to 4 pints of gas daily.
For some, gas is the bloating feeling that is sometimes called indigestion. However, for most, it is the passing of gas. Gas is frequently referred to as “farting,” but professionally it is known as flatulence. Gas looks to escape the body; sometimes this is through flatulence, whereas other times it may be through belching or burping.
Gas is frequently referred to as “farting,” but professionally it is known as flatulence. Gas looks to escape the body; sometimes this is through flatulence, whereas other times it may be through belching or burping.
What causes gas during pregnancy?
The buildup of gas happens whether you are pregnant or not. However, you may discover more challenges with gas once you discover you are pregnant. One of the key contributing factors to experiencing more gas during pregnancy is the increased levels of progesterone. Progesterone is a hormone that causes the muscles throughout your body to relax.
Subsequently, your intestinal muscles relax more, which causes your digestion to slow down. The transient time through the intestine can increase by 30%. This allows gas to build up easier and creates bloating, burping and of course flatulence. Gas during pregnancy can also increase later in pregnancy when the enlarging uterus places pressure on your abdominal cavity.
This pressure can also slow digestion allowing gas to build up.
Unfortunately, the progesterone-induced muscle relaxation makes it harder to control the release of gas. Don’t be surprised if you ended up passing gas in an awkward situation creating a little embarrassment. Just laugh it off and blame it on the baby.
How can you prevent gas during pregnancy
It is pretty much impossible to prevent gas during pregnancy. However, there are steps you can take to manage the gas you experience. Your primary objective is making it happen less often. Certain foods can be triggers for experiencing gas during pregnancy.
If it is really bothering you, you may want to start a diary tracking the food you eat daily. This can help you identify the foods that cause more gas for you.
Suspicious foods that frequently create gas include beans, peas, and whole grains. Unfortunately, there are other healthy foods that can be the cause of your gas. These include broccoli, asparagus, cabbage, and Brussels sprouts. The best course of action is to track your diet and make any associations between increased gas and what you eat. Increased gas is triggered by different foods for different people.
The best course of action is to track your diet and make any associations between increased gas and what you eat. Increased gas is triggered by different foods for different people.
The American Pregnancy Association provides the following recommendations for managing, reducing and hopefully preventing extra gas during pregnancy:
- Avoid or reduce carbohydrate drinks
- Avoid fatty fried foods
- Drink from a glass without using a straw
- Focus on smaller meals throughout the day
- Exercise, which will help stimulate digestion
- Avoid tight clothing around your waist
- Limit or avoid artificial sweeteners
- Drink plenty of water, which will help prevent constipation
- Eat slowly and chew thoroughly
Chewing your food thoroughly is one of the best ways to reduce gas. Most gas is caused by bacteria in the large intestine working to break down food that was not digested thoroughly by enzymes in the stomach. Gas is also related to constipation, so it should prove helpful to learn more about preventing constipation.
Gas is also related to constipation, so it should prove helpful to learn more about preventing constipation.
Gas during pregnancy and safety precautions
It is important you don’t eliminate everything from your diet that may increase your gas. It is more essential to make sure that you are getting the nutrients you and your baby need for healthy development.
There are no concerns for your baby when it comes to gas during pregnancy. You may not like burping or passing gas, but your baby doesn’t care one bit. As noted above, the most important thing is to eat the foods necessary for providing your baby with the nutrients he/she needs as they grow. Learn more about foods to avoid during pregnancy.
Want to Know More?
- Abdominal Pain During Pregnancy
- Sharp Pain During Pregnancy
- Cesarean Birth After Care
Compiled using information from the following sources:
Netter’s Obstetrics and Gynecology, Second Ed. Smith, Roger, Ch. 24.
Smith, Roger, Ch. 24.
Mayo Clinic Guide to a Healthy Pregnancy– Ed. Harms, Roger M.D., et al, Section III.
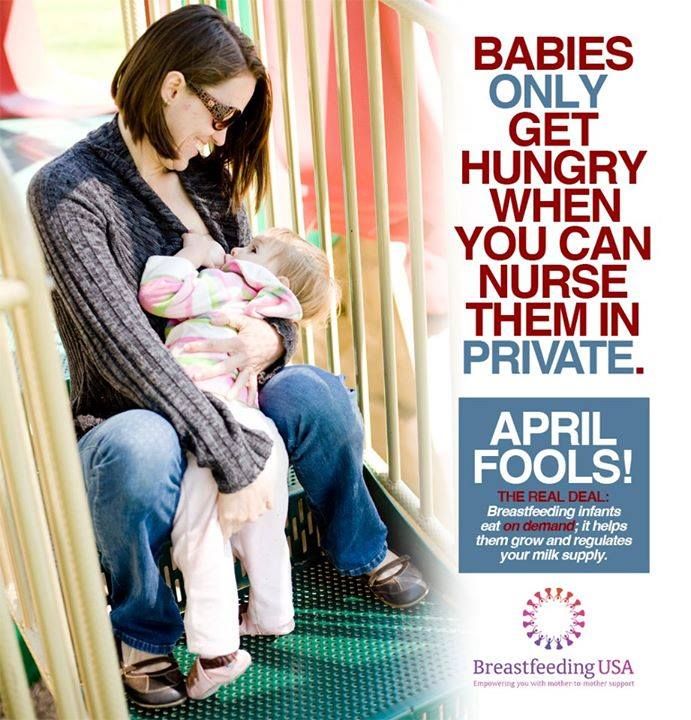
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile.
What explains physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled.
-
Swallowing air during feeding (aerophagia).
 A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation.
A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
Pathological regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
-
increased intracranial pressure.
Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case. It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air. Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again.
-
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency.

-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.
-
The surface in the bed on which the baby lies should rise 10 cm at the head.
-
In addition, it is possible to use special "thickeners" of milk or anti-reflux mixtures, which the doctor will help you choose.
In the event that regurgitation begins to become more frequent or becomes abundant, or first began after six months of the baby's life, or does not subside by one and a half to two years of life, the child should be consulted by a pediatrician. With a high probability, additional help from a gastroenterologist will be needed.
In our Family Medical Center you can always find highly professional help.
← Back to the list of articles
why baby spit up after feeding
If a child spits up after feeding, this is in most cases due to the anatomical immaturity of the upper digestive system. More often than others, premature babies, babies with congenital pathologies suffer from regurgitation. Sometimes the cause is the wrong breastfeeding technique.
Regurgitation in infants is perhaps the most common occurrence in modern pediatrics. More than half of children spit up at least once a day, which is almost always a physiological reaction.
As the baby grows older, spitting up less and less and by 6 months it practically stops doing it. However, sometimes the problem remains, and burping continues for up to a year. In such a situation, you need to make sure that the gastrointestinal tract is functioning normally and consult a doctor.
Why does the baby spit up after every feed
There is a very simple explanation for this. The esophagus of newborns is a funnel with a wide part at the top, and the sphincter at the transition to the stomach actually gapes and hardly retains food.
The esophagus of newborns is a funnel with a wide part at the top, and the sphincter at the transition to the stomach actually gapes and hardly retains food.
Normally, after food enters the stomach, the sphincter contracts and prevents it from “returning” into the esophagus. But in this case, when the stomach is full, part of the contents immediately comes out if the baby takes an inclined or horizontal position.
Babies have two more features: increased pressure over the lower esophageal sphincter, as well as a straight and sometimes obtuse angle of His, formed by the side walls of the esophagus and stomach. In adults, this angle is sharp, which also prevents the return of food eaten into the esophagus.
After feeding, do not put the baby on his stomach, it is better to hold him upright in your arms, trying not to put pressure on his chest. But if he still burps, you should not worry, this is a normal process. If in doubt, please contact our doctors. At a remote consultation, they will explain the causes of regurgitation, talk about pathologies. If necessary, they will tell you which specialists to go through.
At a remote consultation, they will explain the causes of regurgitation, talk about pathologies. If necessary, they will tell you which specialists to go through.
A few more reasons why a child often spit up
Physiological belching after feeding is due to two factors: swallowing air (aerophagia) and increased intra-abdominal pressure. The first is usually associated with fast and greedy suckling, improper attachment of the baby to the breast, or the wrong position of the bottle when it comes to artificial feeding. An air bubble forms in the stomach, pushing out a small amount of milk or formula.
The same results are obtained by a quick change in the position of the baby's body after feeding, which will easily burp if it is immediately started to swaddle, shake, bathe or massage. After all, his stomach resembles an open bottle: tilted / turned over - the contents spilled out.
As for the increase in intra-abdominal pressure, it increases with a too tight-fitting diaper or tight swaddling, as well as against the background of increased gas formation, intestinal colic or stool retention.
Regurgitation in newborns after feeding may be due to the lack of a feeding regimen and overeating.
Baby burps an hour after feeding: what does it mean
The most common cause is constipation, which increases intra-abdominal pressure. Food moves slowly through the gastrointestinal tract, so the child can burp an hour or two after feeding.
Attention! Delayed regurgitation combined with delayed defecation may be a sign of a lazy stomach. But such a diagnosis should be made by a doctor.
5 causes of regurgitation in newborns after formula feeding
The selection of artificial nutrition is a purely individual process with an unpredictable result. There is no 100% guarantee that the mixture will suit the child, even if the brand is very popular.
Poor digestion of the mixture may well cause not only frequent spitting up, but also other digestive problems, including colic, constipation and allergic reactions. In addition, store-bought baby food has a denser texture than breast milk and lasts longer in the stomach. Therefore, the likelihood of its reverse promotion to the esophagus after feeding is higher.
In addition, store-bought baby food has a denser texture than breast milk and lasts longer in the stomach. Therefore, the likelihood of its reverse promotion to the esophagus after feeding is higher.
Your baby may spit up after every feed because:
- the proportions of dilution of the mixture are violated;
- the feeding regime is not observed;
- the transition from breastfeeding to artificial feeding was too abrupt;
- the wrong bottle is selected;
- allergy.
Improper mixing ratio
Each manufacturer indicates on the packaging of the mixture how much water is required to dilute it, and what volume is suitable for the baby by weight and age. Sometimes mothers mistakenly or intentionally dilute food in a way that is not recommended, and the child eats more than normal. As a result, the surplus, of course, comes out.
Case study:
After 3 months, a breastfed child suddenly began to behave restlessly, sleep poorly, spit up after eating, weight gain became slightly below normal. From a conversation with the mother, the doctor learned that the baby was fed too often, the feeding regimen was not observed. After increasing the intervals between breastfeeding, the regurgitation stopped.
From a conversation with the mother, the doctor learned that the baby was fed too often, the feeding regimen was not observed. After increasing the intervals between breastfeeding, the regurgitation stopped.
Refusal of night feedings is also undesirable: the daily volume of food is distributed during the daytime, which leads to stomach overload and regurgitation.
Feeding schedule not followed
Unlike natural, artificial feeding involves eating by the hour.
Baby food takes longer to digest, so the recommended interval between feedings is at least 3 hours. If you feed the child more often, he will “give out” the excess back, since the previous portion has not yet been absorbed.
Abrupt transition from breastfeeding to artificial feeding
When changing the diet, the child's body must first get used to, adapt to the new food. This applies not only to the transition from breastfeeding to artificial feeding, but also from one type of mixture to another.
Wrong bottle selected
This refers to the too wide neck of the container, because of which the child swallows a lot of air along with food. Its discharge will provoke regurgitation after feedings.
Allergy
An allergic reaction to cow's milk protein causes inflammation of the intestinal wall, which in turn leads to malabsorption. Carbohydrate metabolism worsens, since secondary lactase deficiency occurs against the background of an inflammatory reaction - a decrease in the synthesis of the lactase enzyme.
As a result, sugar is broken down incorrectly, increased gas formation occurs, and the baby spits up a fountain. In addition, the baby may feel discomfort at the beginning of feeding and react with an increase in nervous excitability during the period of increased intestinal motility. This also often leads to belching.
What does curd regurgitation mean
Belching with curdled milk after feeding only indicates that the food was in the stomach for some time and managed to curdle - it was fermented. The reason may be in a change in body position or indicate pyloric stenosis with profuse vomiting with a fountain.
The reason may be in a change in body position or indicate pyloric stenosis with profuse vomiting with a fountain.
Attention! When spouting against the background of pyloric stenosis, the child spits up profusely, the jet scatters to a distance of half a meter.
What to do
First you need to make sure that you really need to do something. Pediatricians are advised to determine the intensity and frequency of regurgitation on a five-point scale.
| Points | Regurgitation frequency | Volume |
| one | No more than 5 per day | Not more than 3 ml |
| 2 | > 5 times a day | > 3 ml |
| 3 | > 5 times a day | > 0. |
| four | After every feeding | Small amount over 30 minutes or more |
| 5 | At least half of the meals are accompanied by regurgitation | > 0.5 volume of food eaten |
Now you can determine if there really is a problem. The criteria are:
- the baby is not yet a year old;
- he spits up 2 times a day for 3 weeks or longer;
- before burping there are no precursors, specific signs;
- during regurgitation, the tension of the anterior abdominal wall is not felt;
- there are no difficulties with swallowing, sucking, the child does not take any specific forced position;
- the baby does not begin to sweat a lot, turn pale after burping, and feels normal;
- he is active, has a good appetite, and is gaining weight appropriately for his age.

The above points indicate that everything is in order.
If the intensity and frequency of spitting up is 3 points or more, this is a reason to consult a doctor. Our doctors are ready to advise on all issues at any time of the day. At a remote consultation, possible causes will be identified, and a plan of further actions will be drawn up.
How parents determine the amount of rejected food
Normal regurgitation after feeding occurs in small volumes, within 1-2 tablespoons. You can determine how much food came out when you burp.
When the child burps into the diaper, you need to pour 1 tbsp nearby. l. water and compare the size of the spots. If they are almost the same, there is no reason to worry.
Alarm symptoms
Medical assistance is necessary if the child spits up a lot after feeding, while crying and acting up. A bad symptom is the requirement of supplementary feeding, that is, the baby remains hungry after he has eaten his portion.
Serious illnesses can present with symptoms such as:
- sudden weight loss, weight gain does not meet the standards;
- lack of stool;
- profuse vomiting with an admixture of bile;
- urination less than 8-10 times a day;
- continued spitting up after the child is one year old.
How to deal with regurgitation: a step-by-step guide
If the baby is spitting up after feeding breast milk or formula, you can start with a nutritional correction. When breastfeeding, it is important to ensure that the baby completely captures the nipple along with the areola. His lower lip is usually slightly twisted.
Step 1
It is better to feed the baby while sitting, holding the baby at an angle of 45-60 ° to the chest. In this position, the air freely leaves the stomach, due to which the likelihood of reflux of food into the esophagus is reduced. After eating, it is preferable to put it on its side in a crib: this way, when returning from the stomach, the masses will not enter the respiratory tract. If the child burped while lying on his back, you should lift him up and turn him face down.
If the child burped while lying on his back, you should lift him up and turn him face down.
Step 2
After the baby has eaten, it must be held upright (pose of a soldier) for at least 20 minutes.
Step 3
You can partially remove the air from the stomach before feeding, putting the baby on the stomach for 10-15 minutes. With a tendency to intestinal colic, a light massage of the abdomen, which is done in between meals, will help.
Step 4
Even if the child is constantly spitting up, this is not a reason to transfer him to artificial mixtures. But a clear feeding regimen is desirable after a more or less strict period of time. In addition, mom should follow a hypoallergenic diet and exclude foods that can provoke flatulence - cabbage, legumes, black bread.
Step 5
For artificial babies, it is preferable to use a special anti-colic bottle and a nipple with a special design. The bottle has a valve that prevents you from swallowing air while eating. It is also necessary to make sure that the milk does not flow like a river, but slowly drips, that is, the hole in the nipple must have the appropriate diameter.
It is also necessary to make sure that the milk does not flow like a river, but slowly drips, that is, the hole in the nipple must have the appropriate diameter.
Step 6
When buying a mixture for a spitting up baby, it is better to consult a pediatrician. He may recommend a hypoallergenic formula or a formula that does not contain bovine protein. For some children, the so-called anti-reflux mixture is suitable.
Step 7
Normally, complementary foods are introduced from the 4th month of a child's life, but in the presence of regurgitation, it is allowed to include food thickeners in the diet after the 1st month. It can be mixtures with rice flour, rice porridge without milk. But they are used in an amount of a maximum of 1 tsp. in one feeding.
Step 8
Do not swaddle too tightly, massage, and generally somehow disturb the child after eating. You can only lightly pat him on the back, putting him on his knees, to prevent spitting up.
Step 9
Is the child overeating? To check this, you just need to weigh it before feeding and after. And it does not matter what he eats - mother's or artificial milk.
FAQ
What symptoms should you call an ambulance for?
+
If, after spitting up, the child does not breathe or has lost consciousness; lips and face take on a bluish tint; reflux - gastric contents - has a green or brownish color, which may indicate intestinal obstruction, gastric bleeding.
Why does a baby spit up breast milk, but formula does not?
+
If everything is in order with the calculation of “doses”, and there is no overfeeding with breast milk, most likely it is lactose intolerance. To clarify the diagnosis, it is necessary to take tests.
Should I supplement my baby if he burps?
+
No, by no means.
 5 volume of food eaten
5 volume of food eaten