Pregnancy and headaches everyday
Pregnancy and Headaches: When Should I Worry?
Pregnancy is a beautiful thing to be celebrated, but few people fill you in on the not-so-great symptoms that may occur during the journey. Namely, heartburn, gas, constipation and, for some pregnant mamas, headaches.
While headaches can be just another normal symptom of pregnancy, should they ever be a cause for concern?
“Headaches are common in women both in and outside of pregnancy,” said Kelley Saunders, MD, an OBGYN with Banner – University Medicine Women’s Institute. “But whether they are normal or not should always be discussed with your doctor."
Here is some insight into what causes headaches during pregnancy, some remedies to treat them and why your doctor should be kept in the loop.
Is it a headache or something else?
It isn’t always easy to tell what kind of headache you’re having, but the most common types of headaches during pregnancy are tension-type headaches, migraines and cluster headaches.
Tension headaches are the most common kind of headache in pregnant women. It can feel like someone is trying to squish your head like a watermelon. If you carry your stress in your shoulders and neck, you may be more susceptible to this kind of headache.
Migraines are a particular type of headache that occur on one side of the head. For some women, migraine headaches can get worse the first few months and then improve in later stages of pregnancy. For others, they may experience no change, decrease or difference in their migraines.
Cluster headaches are less common but can occur during pregnancy. You’ll suddenly have severe pain around your eyes or temples usually about the same time every day.
The good news is that there are plenty of pregnancy-safe things you can do to prevent and relieve the most common pregnancy headaches.
Tips for relieving mild headaches
- Get plenty of rest. Sleep is especially hard later in your pregnancy but is so important to physical and mental health.
 Find yourself a comfy prenatal pillow and snuggle away.
Find yourself a comfy prenatal pillow and snuggle away. - Drink plenty of water. Pregnant moms require more water than the average person. While you may want to avoid extra trips to the bathroom, adequate fluid intake is important for you and baby.
- Eat regular, well-balanced meals. To prevent low blood sugar, eat small meals throughout the day. Avoid sugar, like soda and candy.
- Get a prenatal massage. A full-body massage can release tension in the muscles of your neck, shoulders and back.
- Use warm or cool compresses on head, neck and shoulders.
- Avoid triggers. Keep a journal to help identify specific triggers so you can learn what to avoid. Some common headache triggers include strong odors and nitrites or nitrates.
- Try exercise and relaxation techniques. There’s evidence that regular exercise can reduce stress and boost overall mood.
 Check with your doctor first before starting any new fitness routines.
Check with your doctor first before starting any new fitness routines. - Take acetaminophen to relieve symptoms (as approved by doctor).
- Take caffeine in doses less than 200mg in a day (as approved by doctor).
If you have a history of migraines, however, your doctor may treat them differently during pregnancy. Discuss with your doctor what medications are safe to take during pregnancy.
Is my headache a cause for concern?
Sometimes. Headaches tend to be more common in the first and third trimesters, but they can occur in the second trimester as well. While there are common causes for headaches during pregnancy, it’s important to note that headaches during the second and third trimester can also be due to high blood pressure, called preeclampsia.
“Preeclampsia is a pregnancy-related condition that requires prompt evaluation and management with an obstetrician or maternal fetal medicine specialist,” Dr.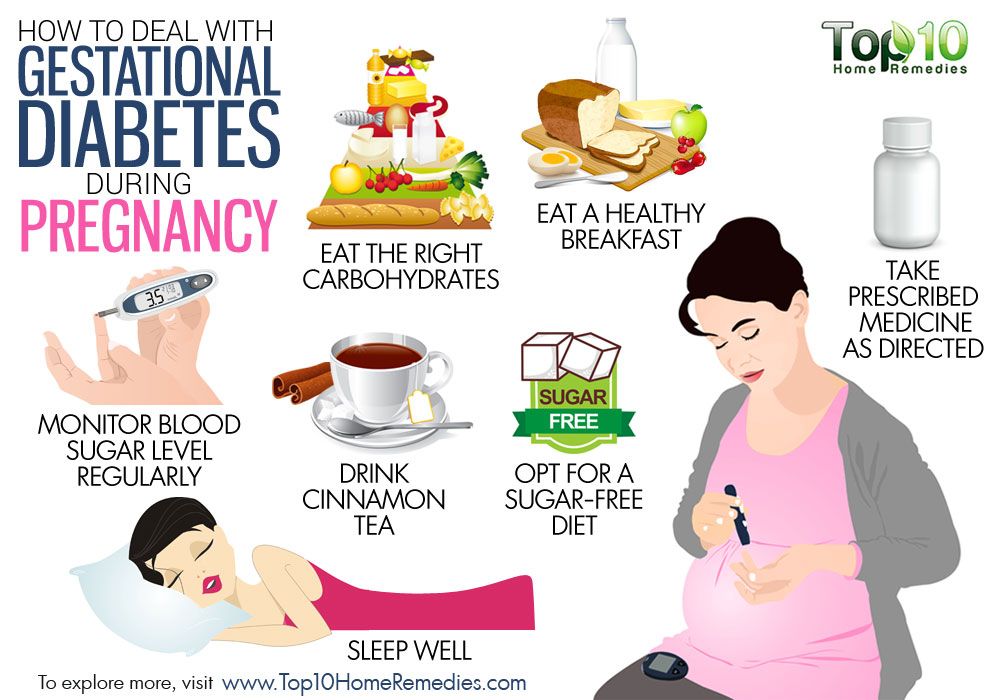 Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
Saunders said. “Elevated blood pressure prior to pregnancy puts a woman at increased risk for preeclampsia.”
When should I call my doctor?
Whether you experience headaches or not, it’s always important to discuss your pre-pregnancy history, obstetrical history and concerns with your doctor for an individualized assessment and management plan. However, if none of the above treatments resolve your mild headache or your headaches become more frequent and severe, talk to your doctor to determine the cause.
“This includes new headaches that present after 20 weeks, a sudden onset of severe headaches, headaches associated with a fever, mental health changes, elevated blood pressure and vision changes,” Dr. Saunders said. “It’s important to keep an open line of communication with your physician and let them know about any changes in your health so they can rule out anything serious."
Got questions? We can help!
If a headache is keeping you up at night and your doctor isn’t available, call the Banner Nurse Now line, a free health care service that offers advice 24-hours a day, seven days a week. Call 844-259-9494.
Call 844-259-9494.
Check out other pregnancy articles on our Banner Health blog
Pregnancy is an exciting, but also a bit scary time (especially if this is your first baby). Here are some other reads to help guide you through the trimesters and welcoming baby:
- 5 Tips for Having a Happy, Healthy Pregnancy
- Expect the Unexpected: How Your Body Changes During Pregnancy
- What To Expect In The Second Trimester
- Understanding Pulmonary Embolism Risk During Pregnancy
Women's Health Pregnancy
Join the Conversation
Headaches during pregnancy | Pregnancy Birth and Baby
Headaches during pregnancy | Pregnancy Birth and Baby beginning of content9-minute read
Listen
If you have a severe headache during pregnancy that is not usual for you, seek medical help immediately.
Key facts
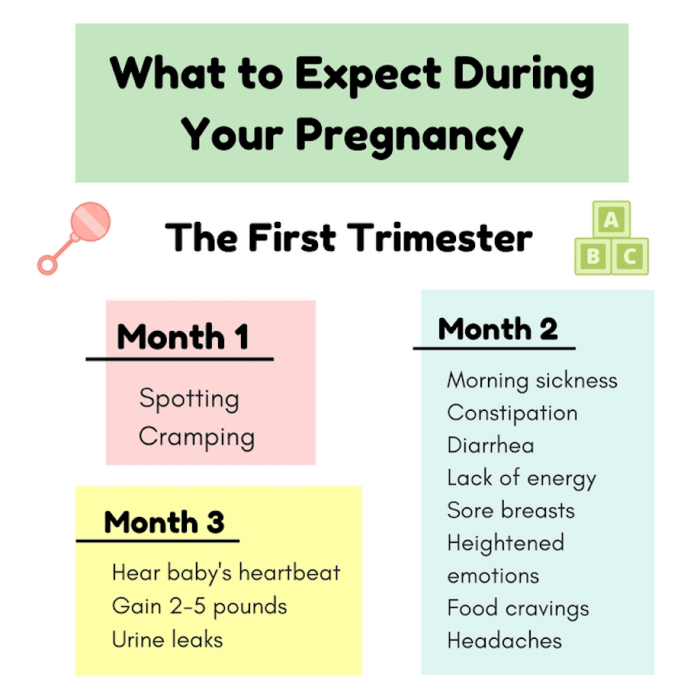
- It’s common to get mild headaches in the first few months of pregnancy because of hormonal changes.
- If you usually suffer from migraines, they may get better, worse, change or stay the same when you’re pregnant.
- Headaches during pregnancy may be triggered by poor sleep, stress, dehydration, low blood sugar or eye strain.
- If your headache doesn’t settle with simple measures (for example, rest and rehydration), you can take paracetamol.
- A headache after 20 weeks can be a sign of pre-eclampsia, which is a serious pregnancy condition that needs medical attention – see your doctor or midwife.
Does pregnancy cause headaches?
Many people get mild headaches when they are pregnant. Headaches can often be triggered by a change in hormones. They are more common in the first few months of pregnancy.
If you usually suffer from migraines, you might notice a change when you’re pregnant. There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
There’s a good chance that your migraines will improve after the first trimester. This may be because your oestrogen level starts to stabilise. However, some people don’t notice a change, or may get worse migraines during pregnancy. You also might notice different changes from one pregnancy to the next.
Headaches can develop for many different reasons — it’s not always because of pregnancy hormones.
Why else might I get headaches during pregnancy?
Besides hormonal changes, there are many triggers that cause headaches in general, but might occur more often when you’re pregnant, such as:
- not getting enough sleep
- withdrawal from caffeine — such as in coffee, tea or cola drinks
- low blood sugar from not eating regularly
- dehydration
- feeling stressed, anxious or depressed
- eye strain — especially as your eye muscles relax during pregnancy
Many of these triggers can cause tension headaches, which are very common.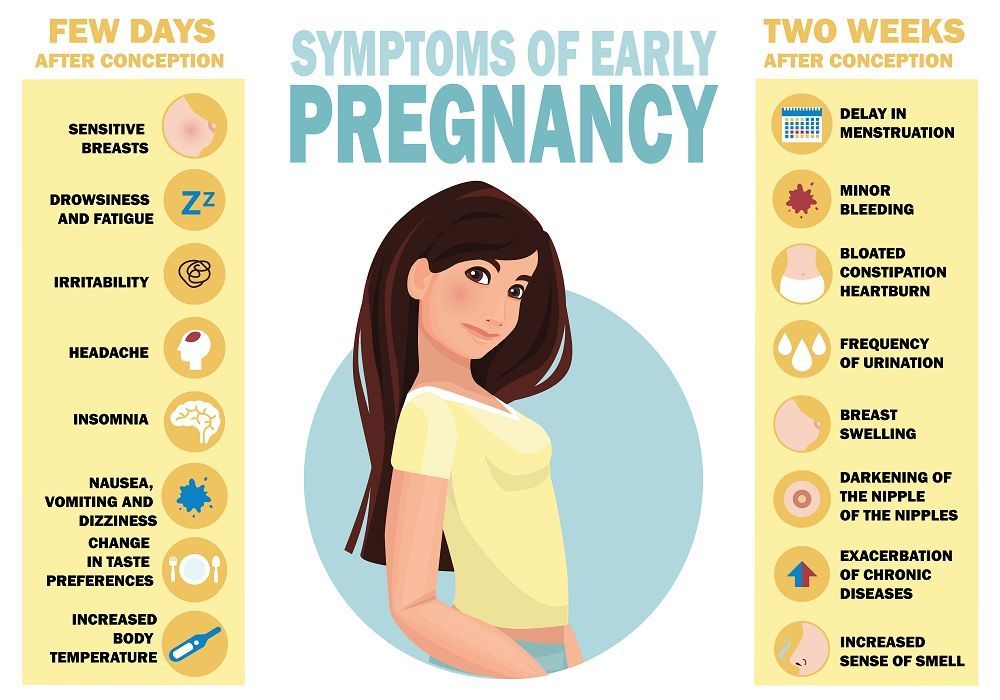 The pain is usually mild and on both sides of your head.
The pain is usually mild and on both sides of your head.
Some of these triggers can cause migraines, which are more severe and mostly occur on one side of your head. If you have migraines, you might also feel sick or vomit and be sensitive to light or sound.
Pre-eclampsia
If you start getting frequent headaches after 20 weeks of pregnancy, this could be a sign of a more serious pregnancy condition called pre-eclampsia. Pre-eclampsia is when you have high blood pressure that affects your kidneys and sometimes other parts of your body. If you have a pre-eclampsia headache, you may find that simple pain-relieving medicines like paracetamol don’t help.
It’s very important to tell your doctor or midwife if you are getting headaches in the second half of pregnancy, or if your headaches are very severe.
If you have a severe headache during pregnancy, call your doctor or midwife. It could be something more serious.
Health conditions
Just like when you’re not pregnant, a headache can sometimes be a sign of other health conditions, including:
- infections, such as an ear infection or flu
- sinusitis
- problems with your teeth
- an aneurysm or stroke
What can I do to treat a headache when I’m pregnant?
If you have a headache, you could try:
- having a nap, or resting with your eyes closed
- drinking water
- having something to eat
- putting a cold or heat pack on your forehead or the back of your neck
- asking someone to give you a gentle neck massage
If you need to take medicine for pain relief, paracetamol is safe during pregnancy. Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
Pain-relieving medicines can actually cause headaches if you take them too often, so don’t take paracetamol more than 3 times a week.
When you’re pregnant, avoid anti-inflammatories such as ibuprofen or aspirin and medicines that contain caffeine.
What can I do to prevent headaches during pregnancy?
If you find you are getting mild headaches often, it’s a good idea to:
- getting more sleep
- drink at least 8 cups of water a day
- go to pregnancy yoga classes or do some other type of exercise
- learn relaxation or stress management techniques
- don't go more than 4 hours without eating
- avoid processed foods
- see an optometrist for an eye check
What can I do if I suffer from migraines during pregnancy?
If you suffer from migraines, try to avoid things that may trigger migraines for you. People have different triggers for migraines, so it’s important to learn what your personal triggers are. Keep a headache diary, and see if your triggers include:
Keep a headache diary, and see if your triggers include:
- specific foods such as chocolate, or food additives such as caffeine or MSG
- bright or flickering lights, strong smells and loud sounds
- not enough sleep, or too much sleep
- skipping meals
- computer or movie screens
- strenuous exercise
- emotional triggers such as arguments or stress
Check with your doctor, pharmacist or midwife before you take a medicine for your migraine, to make sure it’s safe during pregnancy.
Paracetamol is the safest option for pain relief. If paracetamol doesn’t help and you need something stronger, ask your doctor about if you can take codeine. Try not to take codeine often, as you could become dependent on it and your baby could have withdrawal symptoms after they are born.
Most triptans (migraine medicines) are not considered safe in pregnancy. If you don’t get relief from paracetamol and codeine, you may be able to take sumatriptan occasionally. This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
This medicine is available from a pharmacist and requires a prescription. Speak with your doctor or pharmacist before using it to help you understand the risks and the benefits of this medicine during pregnancy.
You can take metoclopramide if you suffer from nausea or vomiting with migraines.
Acupuncture can help treat migraines. Talk to your doctor or midwife first to check it’s safe for you. Make sure to tell your acupuncturist that you’re pregnant, so they can avoid certain points that shouldn’t be used in pregnancy.
When should I see a doctor?
See your doctor or midwife if you have symptoms of pre-eclampsia, including:
- a headache that doesn’t get better with paracetamol
- severe pain below your ribs
- heartburn that doesn’t disappear after taking antacids
- sudden swelling in your face, hands or feet
- blurred vision
Headaches can sometimes be a sign of other serious health conditions. Contact your doctor straightaway if you have:
- a sudden severe headache
- a change in your usual headaches
- your first-ever migraine
- a headache together with fever, neck stiffness, sensitivity of your eyes to light, drowsiness or weakness of your arm or leg
- a recent head injury
CHECK YOUR SYMPTOMS — If you are feeling unwell and not sure what to do next, check your symptoms using the healthdirect Symptom Checker tool.
- Speak with your doctor or midwife, particularly if you have any concerns about pre-eclampsia.
- For more information about headaches, visit Migraine and Headache Australia.
- For more information about medicines you can take during pregnancy, talk to your doctor or pharmacist.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Tommy’s (Headaches in pregnancy – should I be worried?), NSW Government (Having a baby), Migraine & Headache Australia (Adults and headache), Migraine & Headache Australia (Migraine), Migraine & Headache Australia (Headache triggers), Migraine & Headache Australia (Headache treatment – no absolute cure), Migraine & Headache Australia (What is headache?), Migraine & Headache Australia (Tension headache), RANZCOG (Pre-eclampsia and high blood pressure in pregnancy), Royal Women's Hospital (Medicines in pregnancy), NSW Health (Migraine in pregnancy and breastfeeding), RANZCOG (Q&A: severe headache in the third trimester), Migraine & Headache Australia (Self-Care & Trigger Management)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Common discomforts during pregnancy
Need more information?
Treatment of Headache - Migraine & Headache Australia
There is no absolute cure for headache, but many effective treatments exist which can prevent and treat different headache types.
Read more on Migraine and Headache Australia website
Common discomforts during pregnancy
Your body has a great deal to do during pregnancy. Sometimes the changes taking place will cause irritation or discomfort, and on occasions they may seem quite alarming.
Read more on Pregnancy, Birth & Baby website
Adults and Headache - Headache Australia
Studies confirm that tension-type headache and migraine are more common in women while cluster headache, a rare form of headache, is more common in men.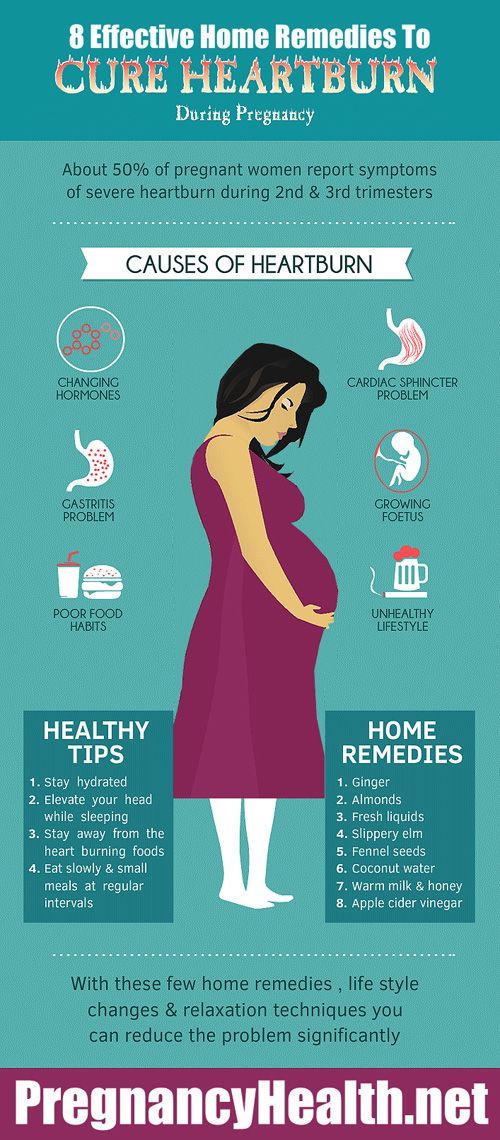
Read more on Migraine and Headache Australia website
Tension-type Headache - Migraine & Headache Australia
Tension-type headache is one of the most common everyday headaches. It causes a dull, non-throbbing pain and can be caused by stress.
Read more on Migraine and Headache Australia website
Migraine Management Tips - Headache Australia
It’s important to be organized and informed about your migraine attacks and how they impact your life. Here are some migraine management tips to assist.
Read more on Migraine and Headache Australia website
Six ways to manage migraine without drugs | The George Institute for Global Health
We’ve all heard of the crushing headache pain that comes with migraine but did you know that one in every seven people experience them, three in every four people with migraine are females, and migraine is the number one cause of disability in young people? With so many people affected worldwide, you’d think modern medicine would have developed a solution by now but unfortunately there’s still no definite cure for migraine.
Read more on The George Institute for Global Health website
Stress and pregnancy
Stress is a normal response to major life changes but you can reduce pregnancy-related stress. Learn more about causes and strategies to help.
Read more on Pregnancy, Birth & Baby website
Mumps and pregnancy
Find out about mumps and its symptoms, how it spreads, how to manage it at home, and how to avoid mumps if you’re planning a pregnancy.
Read more on Pregnancy, Birth & Baby website
Toxaemia of pregnancy (pre-eclampsia) - MyDr.com.au
Pre-eclampsia, also known as pre-eclamptic toxaemia, or just toxaemia, occurs in pregnancy, causing problems for the baby and mother.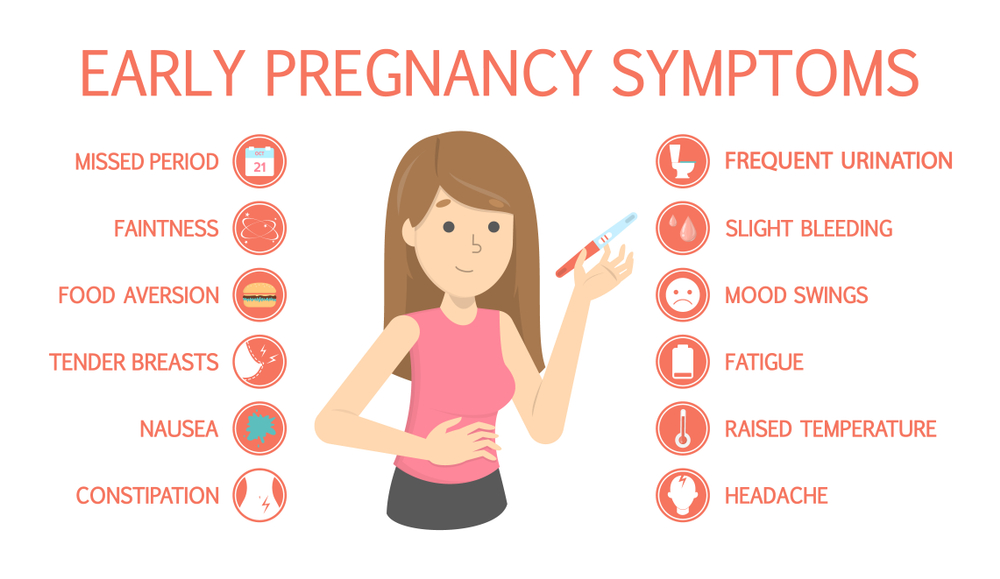
Read more on myDr website
Experiences of pregnancy - Healthtalk Australia
The parents we spoke with found pregnancy life-changing and exciting, and described at length its physical and emotional dimensions.
Read more on Healthtalk Australia website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Subscribe to newsletters
- Sign in
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Headache during pregnancy: where does it come from and how to get rid of it
November 14, 2020 Likbez Health
Sometimes you just need to get some sleep, and sometimes you need to call an ambulance immediately.
When to call an ambulance
Call 103 or 112 urgently if you experience any of the following symptoms:
- sudden and severe headache;
- consciousness becomes confused or completely lost;
- pain worsens over 5 minutes;
- flies, spots flash in the eyes;
- throbbing and noisy in the ears;
- speech has become slurred, words are drawn out;
- arms and legs weaken, convulsions set in;
- the muscles of the neck are very stiff, it is impossible to reach the chest with the chin;
- fever of 39 °C or more;
- increased heart rate at rest;
- severe shortness of breath;
- the child pushes without stopping or stops abruptly;
- leaking water or blood;
- lower abdomen hurts, as if contractions had started.
Why pregnant women can get headaches
Pregnancy headaches are not always life threatening. But the doctor needs to be told about it in any case. If the symptom appeared for the first time and does not hurt much, postpone the conversation until a scheduled visit. If your headache is recurring or gets worse, it's best to make an appointment as soon as possible. The gynecologist will decide what needs to be done or refer you to another doctor.
There are many causes of headaches. Scientists have found that in pregnant women in 57% of cases it is primary, that is, not associated with other diseases. The most common are migraines and tension headaches.
Everything else is a secondary headache caused by various pathologies. Usually it is high blood pressure and infections. But there are also more dangerous reasons.
1. Stress and fatigue
A pregnant woman's body experiences increased stress, because it has to work for two. If at the same time the expectant mother is exposed to stress, strong feelings or sleeps little, she develops a tension headache.
Discomfort lasts from 30 minutes to several days. The head hurts in the forehead, occiput, both temples. But there is no feeling that they put on a tight hoop or helmet. The pain does not get worse when bending over, walking, or climbing stairs, bright lights, or sounds.
What to do
Tension headache can go away on its own: just get some fresh air or sleep. Sometimes pleasant emotions help, which distract from experiences.
If the pain persists for 2-3 consecutive days, see a doctor. He will select painkillers that are safe for the child.
2. Medications
Any medicine that enters the stomach or bloodstream can cause headaches even if the dosage is correct. In pregnant women, this often occurs due to drugs for high blood pressure, heart disease, antibiotics, anticonvulsants.
Long-term use of non-steroidal anti-inflammatory drugs for headaches may cause the opposite effect: the pills do not remove, but provoke symptoms.
What to do
If your head hurts a few hours after taking the medicine, you need to see a doctor to change the medicine. Do not drink non-steroidal anti-inflammatory drugs for more than 3-5 days. If they do not help, you need to tell the doctor about it.
3. Love for coffee or rejection of it
Coffee can cause headaches during pregnancy. Unpleasant symptoms occur if you drink more than 3-4 cups a day.
Abrupt refusal of coffee is also harmful. It is worth finding out about pregnancy and stopping brewing a fragrant drink, and after 1-2 days, aching pain will appear in the temples and the back of the head.
What to do
Coffee is best avoided during pregnancy. If a headache occurs a day after this, you can drink a small cup of the drink and wait a day again. Gradually, the dependence on coffee will pass.
Coffee drinkers can reduce their drink intake to 1-2 cups per day.
4. Infection with fever
Acute viral (usually ARVI) or bacterial (eg, streptococcal tonsillitis) infections cause fever and headache. This is a normal reaction to foreign microorganisms.
But any infection is dangerous for pregnant women. It can cause fetal defects, growth retardation and even miscarriage. And with meningitis, especially listeriosis, there is a threat to the life of the mother.
What to do
If you have a headache with fever, call your doctor. He will prescribe safe medications or give you a referral to the hospital if a severe infection is suspected. In this case, you need strong antibiotics, droppers to maintain the body and sometimes hormones.
5. Preeclampsia and preeclampsia
After 20 weeks, preeclampsia may develop in pregnant women. This is a disease in which one of three symptoms or a combination of them may appear: high blood pressure, edema, and protein in the urine.
Without proper treatment, preeclampsia turns into preeclampsia. The pressure rises sharply, the head and lower abdomen hurt unbearably, the baby pushes unusually hard or, on the contrary, suddenly calms down. Preeclampsia can lead to placental abruption, damage to the liver and other organs, bleeding, and even seizures. Without urgent medical care, the fetus and mother die.
What to do
When the first signs of preeclampsia appear, the pregnant woman is hospitalized to find treatment. After that, she is discharged home under the supervision of her gynecologist.
But if her health worsens, the doctor again sends the woman to the hospital, where she is prescribed medication to reduce pressure, special drips to keep her body functioning. If improvement does not occur within a day, a caesarean section is performed.
6. Migraine
One of the causes of migraine is a change in estrogen levels. But the disease very rarely appears due to pregnancy. On the contrary, in 70% of women, the symptoms subside dramatically after conception. Nevertheless, migraines torment many.
It may begin with an aura: flashes of light, spots before the eyes, tingling in the hands or numbness of half of the face, sometimes tinnitus. Each symptom can last from 20 minutes to an hour.
A migraine attack develops after the aura. In this case, one side of the head hurts and throbs, nausea or vomiting appears. A woman is irritated by bright lights, loud noises, smells. They make the pain worse.
Seizures last from a few hours to a week or more. After a migraine, there is a feeling of severe fatigue, exhaustion, and an awkward turn of the head can return the pain.
What to do
Any medication for migraine during pregnancy must be prescribed by a doctor. In some cases, drugs from the group of beta-blockers are used.
Studies have shown that frequent migraine in pregnancy is associated with a lack of magnesium. The doctor will help you choose the appropriate type of vitamin and mineral complex and its dosage.
7. Cerebral vascular disease
Hormone problems in some pregnant women increase blood clotting, which increases the risk of thrombosis, stroke or bleeding in the meninges. These conditions are very dangerous: a woman can die within a few minutes or remain disabled.
Vascular involvement is always accompanied by several symptoms:
- severe headache on one side;
- nausea and vomiting;
- blurred vision;
- loss of consciousness;
- convulsions.
What to do
Urgently call an ambulance. The pregnant woman must be laid or seated so that she does not hit when she falls. You can't give medicine! You can only open the window so that there is more air in the room.
Which treatment the doctor prescribes depends on the specific disease. These can be drugs that reduce blood clotting and dissolve blood clots. In some cases, urgent surgery is needed.
8. Brain tumors
Studies show that progesterone and estrogens during pregnancy can trigger or accelerate the growth of tumors in the brain. Symptoms of the disease appear slowly, over several months, and depend on the size and location of the tumor.
The headache may gradually increase, then vision, speech, hearing deteriorate, limbs go numb and convulsions appear. Sometimes it is difficult for a woman to keep her balance.
What to do
If a pregnant woman often has a headache or she forgets what she wanted to buy in the store and how to cook her favorite borscht, confuses her way home, you need to go to a neurologist. First, he will prescribe standard treatment, simple and safe medicines, rest, good sleep.
If this does not help, the symptoms persist or worsen, a deep examination is needed. The pregnant woman will be sent for an MRI of the brain. This procedure is safe for the fetus. If the diagnosis is confirmed, surgery may be required.
What to do if the doctor cannot find the cause of the pain
If you have been examined and the doctor cannot tell you why your head hurts and diagnoses you with vascular dystonia, this is cause for concern. There is no such disease.
Seek another doctor. Perhaps he uses new diagnostic methods that will help to deal with the problem and choose a treatment.
How to avoid pregnancy headaches
Experts recommend:
- Avoid triggers.
For example, if you notice that certain foods, smells, or situations cause headaches, try not to encounter them.
- Protect yourself from stress, do not worry about trifles.
- Move more. During pregnancy, walk every day in the fresh air and do special exercises for expectant mothers.
- Eat right. Try to eat a lot of vegetables and fruits, dairy products, drink at least 2.4 liters of liquid. Every day, the menu should include fish, poultry or lean meat. And it is better not to buy sweet, fast food and other junk food.
- Follow the daily routine. You need to sleep at least 8 hours a day and go to bed no later than 22-23 hours in order for melatonin to be produced normally.
- Learn to relax. Learn simple meditation techniques or breathing exercises.
Read also 🧐
- How pregnancy develops by week
- How to calculate the duration of pregnancy
- What rights does a pregnant woman have at work
- 7 best sex positions for pregnant women
- How to recognize a miscarriage and what to do next
Migraine during pregnancy: what to do
Migraine is a benign disease, it does not affect the course of pregnancy and fetal development. However, migraine and pregnancy is a combination that requires a responsible attitude. Especially with frequent migraines (more than 2 times a week) and migraines with aura, since:
-
medicines approved for use, few,
-
and the approach to the treatment and prevention of migraine during this period is extremely individual: it depends on the frequency, severity and duration of headache, the degree of impact on life.
Our neurologist Daria Korobkova conducted a live broadcast on the clinic's Instagram account, where she told how migraine and pregnancy are connected, why attacks become more frequent or disappear, and answered subscribers' questions. The ether was saved, see “Air recording: migraine during pregnancy and GV.
We will tell about migraine during breastfeeding separately.
The statistics of clinical observations of migraine during pregnancy looks like this:
In 60-70% of pregnant women with migraine, headache attacks become less frequent, milder, or even completely disappear in the second and third trimesters. This is due to the stabilization of estrogen levels. By the beginning of the second trimester, it rises 6 times and its fluctuations stop.
In other women, migraine during pregnancy either remains unchanged or worsens. But as the duration of pregnancy increases, the proportion of such women gradually decreases:
If at the end of the first trimester the frequency and intensity of attacks persist, then it is most likely that migraine will disturb the woman during the entire period of pregnancy and after childbirth too.
How to manage migraine during pregnancy?
The main thing here is to learn how to control seizures and, if necessary, seek medical help.
-
Follow lifestyle advice:
-
get enough sleep;
-
drink plenty of fluids;
-
eat fractionally and without long breaks;
-
rest;
-
avoid stressful situations.
This is one of the main provocateurs of migraine. Psychotherapy, relaxation and stress management are here to help you.
-
Keep a headache diary. This will help you take control of migraine triggers.
Yes, yes, following these simple recommendations is sometimes enough to make seizures less frequent! Pregnancy is a special state of a woman. If in other periods of life we do not take such recommendations so seriously, then in this situation it is worth trying to change the philosophy of life and attitude towards ourselves =)
How to relieve an attack?
-
Favor non-drug methods. Sometimes, in order to relieve an attack, it is enough to eliminate an unfavorable factor:
-
dry biscuits, ginger, or applesauce may help with nausea;
-
for dehydration - diluted juice or other liquid;
-
sleep, walking or breathing exercises can also help to cope;
-
If the attacks are severe, interfere with your life, then under the supervision of a specialist, you can resort to drug therapy.
PARACETAMOL is considered the safest and can be taken throughout pregnancy.
All other drugs have nuances. For example:
-
ibuprofen can be taken in the second trimester, and in the first trimester it is better to limit, in the third trimester the drug is contraindicated for use;
-
aspirin is prohibited in the 3rd trimester and is undesirable for taking in the first two, as it can cause extremely undesirable consequences;
-
It is strictly forbidden to use ergotamine and opioid analgesics;
-
triptans are not officially approved for use during pregnancy as no controlled studies have been conducted. However, clinical observations of women around the world who took them on their own showed no adverse effects on the fetus. We discussed this issue in more detail on the air.
!Other than paracetamol, we do not recommend the use of any drug without a doctor's prescription.