Pregnancy and cf
Planning for a Safe Pregnancy
With proper management, careful monitoring, and working closely with your care team and obstetric team, many women with cystic fibrosis are able to carry a child without significantly impacting their long-term health. At the same time, however, the unique demands that pregnancy places on the body can have serious implications for women with CF.
The progressive decline in lung function and impaired nutrition associated with CF can pose several challenges, including a higher risk for health complications and an increased treatment burden. For this reason, women with CF who plan their pregnancies for a time when they are in the best health possible tend to have the most successful outcomes.
Am I Healthy Enough for Pregnancy?
Generally, there are four main factors that help determine how well a woman with CF will handle pregnancy. These factors are:
- Lung function: Ideally, a woman with CF should have a forced expiratory volume (FEV1) of 50 percent or more before becoming pregnant.
Women with lower FEV1 values can also get pregnant, but their risk for problems and other complications may be higher. According to many experts, your lung function is the most important factor that affects both your health and the baby's after delivery. Research has shown that the outcomes for you and your baby will likely be better if your FEV1 is over 50 percent before you get pregnant.
- B. cepacia: Some studies have shown that infection with Burkholderia cepacia can lead to more problems during pregnancy. If you have B. cepacia and are interested in becoming pregnant, talk to your CF care team to learn more about the possible implications for both your and your baby's health.
- Nutrition: Before getting pregnant, it is important that your nutrition status is good enough to support both you and your baby throughout your pregnancy, including potential morning sickness or changes in appetite. This means having a body mass index (BMI) of at least 22 kilograms per square meter (kg/m2).
 If your BMI is below this, improving your nutritional status before you get pregnant would benefit you and your baby, as low BMI in pregnancy is associated with problems including poor fetal growth and premature delivery.
If your BMI is below this, improving your nutritional status before you get pregnant would benefit you and your baby, as low BMI in pregnancy is associated with problems including poor fetal growth and premature delivery. - Cystic fibrosis-related diabetes: For women with CF who have cystic fibrosis-related diabetes (CFRD), monitoring and controlling your blood glucose prior to getting pregnant will be key. Diabetes has been shown to increase your risk of experiencing problems during pregnancy, so it is important to discuss your CFRD with your care team. If you are taking insulin to control your diabetes, your insulin requirements may change once you are pregnant.
- Cirrhosis (liver disease): CF can be associated with severe liver disease, such as cirrhosis. Liver disease is also a potential complication of pregnancy with CF. For this reason, women with CF who have liver disease should discuss the implications of getting pregnant with their CF care team.
Talk to your CF care team about important considerations if you are taking a CFTR modulator and are planning to get pregnant.
Potential Complications of Pregnancy With CF
According to several studies, the majority of CF pregnancies result in live births and there is no clear increased risk of fetal death or birth defects. However, this is not to say that getting pregnant with CF comes without risks.
The most common complication of pregnancy with CF is preterm or premature delivery, which, in one study, was associated with low pre-pregnancy lung function.1 Diabetes was also reported to be more common in women who delivered prematurely.
Overall, adequate nutrition, well-controlled blood sugars, and a reasonable pre-pregnancy FEV1 are associated with better outcomes.
In addition to premature delivery, some of the most common complications associated with pregnancy and CF include:
- Gestational diabetes: Pregnant women with CF have been found to have a higher risk of gestational diabetes than those in the general population.
 Many women with CF already have impaired glucose tolerance. Because the hormonal changes that accompany normal pregnancy often cause a degree of impaired glucose tolerance as well, women with CF are more likely to develop gestational diabetes than the average pregnant woman. For this reason, your care team should consistently screen for diabetes throughout your pregnancy.
Many women with CF already have impaired glucose tolerance. Because the hormonal changes that accompany normal pregnancy often cause a degree of impaired glucose tolerance as well, women with CF are more likely to develop gestational diabetes than the average pregnant woman. For this reason, your care team should consistently screen for diabetes throughout your pregnancy. - Nutritional deficiency: Because your nutritional demands will change during pregnancy and put you at risk for inadequate weight gain or weight loss, most women with CF will need to increase their caloric intake, drink supplements, and focus on maintaining and gaining weight while pregnant. Many women with CF need to take nutritional supplements during pregnancy, so it is important to pay close attention to your nutritional status and work closely with your CF dietitian or another member of your care team.
- Constipation: Although it is common for all women to experience constipation issues during pregnancy, having CF puts you at a higher risk.
 To prevent constipation, pregnant women with CF can try taking steps such as drinking more water, adding fiber to their diet, and eating more fruits and vegetables. In addition, your care team may recommend the use of stool softeners or laxatives while you are pregnant. Contact your CF care team if you notice a decrease in the number or amount of normal stools.
To prevent constipation, pregnant women with CF can try taking steps such as drinking more water, adding fiber to their diet, and eating more fruits and vegetables. In addition, your care team may recommend the use of stool softeners or laxatives while you are pregnant. Contact your CF care team if you notice a decrease in the number or amount of normal stools. - Exacerbations: Pregnant women with CF may experience more exacerbations, so it is important that you continue your CF respiratory therapies throughout pregnancy to stay as healthy as possible. Your CF care team and obstetrician will want to discuss whether any of your treatments should be stopped or changed during pregnancy — especially if you require antibiotics.
- Vitamin A (retinol) toxicity: Because high levels of vitamin A — especially within the first three months — can be associated with developmental issues for your baby, it is important that your care team carefully monitors your vitamin A levels when managing your pregnancy.
 If you are taking vitamin A supplements, your obstetrician will likely have you stop taking them during your pregnancy. However, it is important that you do not stop taking your other CF-related vitamins without discussing it with your care team and obstetrician first.
If you are taking vitamin A supplements, your obstetrician will likely have you stop taking them during your pregnancy. However, it is important that you do not stop taking your other CF-related vitamins without discussing it with your care team and obstetrician first. - Hypertension: According to some studies, pregnant women with CF have a higher risk of hypertension than pregnant women without CF. For this reason, your care team and obstetrician should closely monitor your blood pressure both before and during your pregnancy.
Dealing With the Unexpected
Although planning your pregnancy as a woman with CF is ideal, life does not always go according to plan. If you are a woman with CF experiencing an unexpected pregnancy, your first step should be to contact your CF care team. Your care team will work with you to assess the possible impact that being pregnant could have on your health, and ultimately help you weigh the risks and benefits.
The decision about how to proceed in the face of an unplanned pregnancy will depend on the trimester, as well as many other factors. For example, some people with CF may feel it would be difficult to care for both themselves and a child with CF, so getting your partner genetically tested could play a major role in your decision process.
For example, some people with CF may feel it would be difficult to care for both themselves and a child with CF, so getting your partner genetically tested could play a major role in your decision process.
In addition, women with severe lung disease may need to consider terminating the pregnancy to preserve their own health. Only you can decide what is right for you, but discussing both the physical and emotional implications of your pregnancy with your CF care team can help you make an informed decision.
1 Gilljam M, Antoniou M, Shin J, Dupuis A, Corey M, Tullis DE. Pregnancy in cystic fibrosis. Fetal and maternal outcome. Chest. Jul 2000;118(1):85-91.
Cystic fibrosis and pregnancy
What is cystic fibrosis?
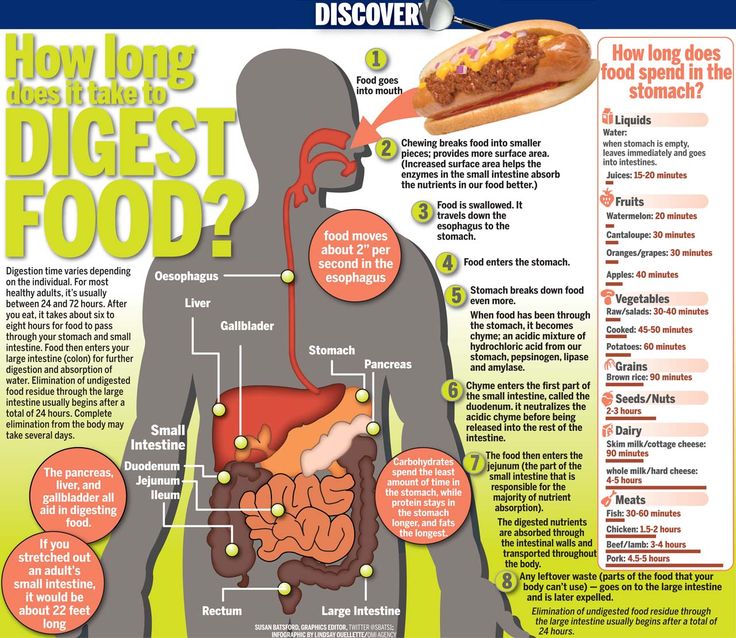
Cystic fibrosis (also called CF) is a chronic health condition in which very thick mucus builds up in the body. This causes problems with breathing and digestion. Digestion is the way your body processes the food you eat.
Mucus is a fluid that normally coats and protects parts of the body. It’s usually slippery and watery. But in people who have CF, the mucus is thicker and sticky. It builds up in the lungs and digestive system and can cause problems with how you breathe and digest food. The buildup of mucus in the body makes it easy for harmful bacteria to grow. This can lead to infections.
It’s usually slippery and watery. But in people who have CF, the mucus is thicker and sticky. It builds up in the lungs and digestive system and can cause problems with how you breathe and digest food. The buildup of mucus in the body makes it easy for harmful bacteria to grow. This can lead to infections.
CF is diagnosed in about 1,000 babies each year in the United States. Most people with CF are diagnosed by age 2.
Most people who have CF can have a healthy pregnancy. But CF can cause complications before and during pregnancy.
Can CF cause problems during pregnancy?
Yes. To best manage CF during pregnancy, you need a team of health care providers who work together to give you the best care. The team includes:
- Your prenatal care provider. This is often a doctor who specializes in high-risk pregnancies.
- Your CF doctor. This most often is a pulmonologist: a doctor who specializes in lung conditions.
Your team also may include:
- A nurse who helps you manage your overall care
- A dietitian who helps you with meal plans and nutrition and helps you manage your weight
- A social worker who helps you manage CF as part of your daily life
- A psychologist or other mental health professional who helps you deal with emotional aspects, like stress, that can come with CF
- A respiratory therapist who helps you with breathing therapy and inhaled medicines to help keep your airways clear
- A physical therapist to help you with a fitness plan
You may get your CF care at an accredited CF care center. These centers have expert providers who specialize in treating people who have CF.
These centers have expert providers who specialize in treating people who have CF.
If you have CF, make sure each provider knows about your pregnancy plans before you get pregnant. Your providers work together to help you get ready for pregnancy and stay healthy during pregnancy. Your provider team monitors you closely throughout pregnancy to manage your CF and make sure you and your baby are doing well.
If you have CF, you have a higher risk for diabetes, and you can have problems with breathing, nutrition and liver function. Symptoms of CF can get worse during pregnancy. For example, you’re more likely to have pulmonary exacerbations during pregnancy. This is when your breathing gets worse. You’re also more likely to have constipation during pregnancy. This is when you don’t have bowel movements or they don’t happen often, or your stools (poop) are hard to pass.
Some pregnancy complications are more common in people who have CF, including:
- Infertility.
 This means you have trouble getting pregnant.
This means you have trouble getting pregnant. - Premature birth. This is when your baby is born early, before 37 weeks of pregnancy. Babies born early are more likely to have health problems at birth and later in life than babies who are born on or close to their due date.
- Gestational diabetes. This is a kind of diabetes that some people get during pregnancy. Diabetes is a medical condition in which there’s too much sugar (also called glucose) in the blood. This can damage organs, including blood vessels, nerves, eyes and kidneys. If you have CF and don’t have diabetes before you became pregnant, you’re at increased risk to develop gestational diabetes.
- Not gaining enough weight during pregnancy. Your nutrition needs change during pregnancy. This can cause you to lose weight or not gain enough weight during pregnancy. Gaining the right amount of weight during pregnancy helps support your baby’s growth and development.

- Vitamin A toxicity. This means you have too much vitamin A in your body. Vitamin A helps your body fight infections and helps you have healthy skin, vision and intestines. If you have CF, you may not absorb as much vitamin A as you should, so you may need to take a vitamin A supplement to help you get the right amount. But during pregnancy, you can have too much vitamin A, and that can affect your baby’s development.
- High blood pressure (also called hypertension). This is when the force of blood against the walls of the blood vessels is too high. It can stress your heart and cause problems during pregnancy.
What causes CF?
CF is a genetic condition. This means it’s passed from parents to children through genes. A gene is a part of your body’s cells that stores instructions for the way your body grows and works. Genes come in pairs — you get one of each pair from each parent. CF is one of the most common genetic conditions in the United States.
Sometimes the instructions in genes change. The gene change in CF affects a protein that controls the balance of salt and water in the body. This causes the body to make thick, sticky mucus and salty sweat.
Parents can pass gene changes to their children. Sometimes a gene change can cause a gene to not work correctly. Sometimes it can cause birth defects or other health conditions.
You have to inherit the gene change for CF from both parents to have CF. If you inherit the gene change from just one parent, you have the gene change for CF, but you don’t have the condition. When this happens, you’re called a CF carrier.
If you and your partner are both CF carriers, your baby may get two CF gene changes (one from each of you) and have CF. About 1 in every 20 people is a CF carrier. If you and your partner are both CF carriers, there is a:
- 3-in-4 chance (75 percent) that your baby won’t have CF
- 1-in-2 chance (50 percent) that your child won’t have CF but will be a CF carrier
- 1-in-4 chance (25 percent) that your child will have CF
- 1-in-4 chance (25 percent) that your child will not have CF and not be a carrier
If you and your partner both have CF, your baby will have CF. However, CF affects the sperm count in semen, making it almost impossible for a parent with CF to fertilize an egg with their sperm. Genetic counseling can help you understand your chances of passing CF to your baby. A genetic counselor is a person who can help you understand about how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby's health. Ask your health care provider if you need help finding a genetic counselor, or contact the National Society of Genetic Counselors.
However, CF affects the sperm count in semen, making it almost impossible for a parent with CF to fertilize an egg with their sperm. Genetic counseling can help you understand your chances of passing CF to your baby. A genetic counselor is a person who can help you understand about how genes, birth defects and other medical conditions run in families, and how they can affect your health and your baby's health. Ask your health care provider if you need help finding a genetic counselor, or contact the National Society of Genetic Counselors.
How can you find out if you’re a CF carrier?
You can get carrier screening before or during pregnancy to find out if you’re a CF carrier. There are two kinds of carrier screening tests:
- A blood test
- A saliva test. Saliva is the clear liquid inside your mouth.
Your provider sends the blood or saliva sample to a lab for testing. Both tests are safe to take during pregnancy.
Carrier screening is your choice. You don’t have to have it if you don’t want it, even if your provider recommends it. All pregnant people or those who are thinking about getting pregnant can get screened for CF. If screening shows that you’re a CF carrier, your partner can get screening, too.
You don’t have to have it if you don’t want it, even if your provider recommends it. All pregnant people or those who are thinking about getting pregnant can get screened for CF. If screening shows that you’re a CF carrier, your partner can get screening, too.
About one in 31 people in the United States is a CF carrier. You and your partner may want to have CF carrier testing if:
- CF runs in either of your families.
- You are:
- White. About 1 in 29 White Americans is a CF carrier. It’s most common in those whose families come from Northern Europe.
- Latinx. One in 46 Latinx people in the United States is a CF carrier.
- Black. One in 65 Black people in the United States is a CF carrier.
- Asian. One in 90 Asian peoplein the United States is a CF carrier.
Can you find out during pregnancy if your baby has CF or is a CF carrier?
Yes. If you or your partner has CF or is a CF carrier, you can have a prenatal test to find out if your baby has the condition or is a carrier. You can have either of these tests:
You can have either of these tests:
- Chorionic villus sampling
- Amniocentesis
If you think your baby may have CF or be a carrier, talk with your provider or genetic counselor about these tests.
How is CF treated during pregnancy?
All of your providers work together to make sure your CF treatment is safe for you and your baby during pregnancy. Treatment can include:
- Medicine, like antibiotics to treat infections
- Inhalers to open the airways to the lungs and thin mucus
- Chest therapy to help clear the airways to the lungs
- A fitness plan
- Supplements to help your body get nutrients that it may not be able to get from food
Most likely you can continue your regular CF treatment throughout pregnancy, but you may need to make some changes. For example, certain antibiotics that you take to treat infections may not be safe for your baby during pregnancy. You may need to switch to a safer medicine. Or you may need to change the timing of certain treatments. Your provider team can help you make decisions about treatment that are best for both you and your baby.
Or you may need to change the timing of certain treatments. Your provider team can help you make decisions about treatment that are best for both you and your baby.
If you have CF, here’s what you can do to help you have a healthy pregnancy:
- Get early and regular prenatal care and go to all of your prenatal checkups, even if you’re feeling fine. At each visit, talk to your provider about your CF, your treatment plan and keeping your other providers informed about your prenatal care.
- Tell your prenatal care provider about any medicine you take, even if it’s prescribed by another provider. Be sure any provider who prescribes you medicine knows that you’re pregnant. Don’t start or stop taking any prescription medicine during pregnancy without talking to your providers first. Stopping your medicine suddenly may cause severe problems for you and your baby.
- Get regular treatment for CF. Don’t stop getting CF treatment because you’re going to your prenatal care checkups.
 You need to see both your prenatal provider and your CF providers throughout pregnancy.
You need to see both your prenatal provider and your CF providers throughout pregnancy.
Can you breastfeed or chestfeed if you have CF?
Yes. Even if you have CF, human milk is good for your baby, but it takes a lot of energy for a body to make milk. This may make it hard for you to get all the calories you need for both you and your baby. Work with your dietitian on a meal plan to make sure you get enough calories each day.
Medicines you take sometimes pass to your baby through your milk, and some may be harmful to your baby. Make sure your prenatal provider, your CF provider and your baby’s provider know about any medicine you take.
More information
Cystic Fibrosis Foundation
See also: Cystic fibrosis and your baby, Newborn screening, Your family health history
Last reviewed: May, 2021
Early pregnancy | Shchelkovsky perinatal center
Pregnancy is a wonderful period! However, the changes taking place in the body at this time can greatly frighten you. The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
The phenomena characteristic of pregnancy are different for all women, and will not necessarily be repeated during each subsequent gestation. Let's analyze the most common symptoms, their causes and possible methods of correction.
1. Frequent urination.
Frequent, painless (!) urge to urinate is one of the signs of pregnancy. This is due to increased secretion of progesterone (pregnancy hormone), changes in metabolism and pressure from the growing uterus on the bladder.
Be sure to see a doctor if:
- painful urination (this may be a sign of an infection)
- urine of strange color (stained with blood, brown)
- the amount of urine excreted per day is much less than the liquid drunk per day
Life hack! Under no circumstances should fluid intake be restricted! To alleviate the condition and reduce the frequent urge to urinate, it is necessary to exclude products that have a diuretic effect: tea, coffee, zucchini, watermelon; as well as salty, spicy and fried foods. It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
It is better to drink water or juice. Wear comfortable cotton underwear that does not squeeze the lower abdomen.
2. Nausea, vomiting, heartburn, increased susceptibility to smells.
Nausea is one of the common symptoms of early pregnancy. The range of issues related to nausea and vomiting during pregnancy is quite wide. From "it's good, I don't even feel sick" (with relief), "I don't feel sick, what's wrong with me?" (with anxiety) to "when will this nausea pass" (with hope). Indeed, these symptoms are not at all a mandatory accompaniment of gestation, they can manifest at 7-8 weeks and last up to 12-14 weeks. The duration of this condition can sometimes be delayed, but rarely persists throughout pregnancy.
Life hack! For nausea, eat before feeling hungry. Solid, non-hot food and drinks at a cool temperature are best. With heartburn, you should eat small portions of food and often, and most importantly, sit, stand or walk for at least 30 minutes after eating, but do not lie down.
You should definitely consult a doctor if:
- vomiting occurs even after drinking water
- vomiting is exhausting, accompanied by dizziness, weakness
- dryness, jaundice and flaking of the skin appear
- Nausea and vomiting interfere with proper nutrition, accompanied by weight loss
To reduce nausea and vomiting in the morning, try eating something before you get out of bed. It can be a cracker, a cookie, a piece of hard cheese. And salty food is preferable to sweet. You can have a snack in the same way at night when you get up to go to the toilet. Do not lie down immediately after eating, this will only increase nausea. Vitamins for pregnant women with nausea should be taken in the evening after meals. Cool water with lemon, ginger, mint tea, or ginger or mint candies can alleviate the condition. It is necessary to exclude those foods, drinks and smells that are unpleasant to you. Brushing your teeth and rinsing your mouth often can also reduce nausea.
3. Pain or cramps in the lower abdomen, constipation, pain in the lumbar region.
The simplest and most easily controlled cause of pain is delayed and incomplete bowel movements. An increase in the concentration of progesterone relaxes the smooth muscles, which are located not only in the uterus, but also in other hollow organs. In this case, the correction of the diet and the restoration of the passage of feces will help. If the measures are ineffective, the doctor may prescribe safe drugs for you. A special type of pain that occurs during exclusivity in pregnant women is pain in the round ligament of the uterus. This acute, rather intense pain occurs, as a rule, on the one hand with a sharp change in body position (for example, when getting up from a chair or leaving a car). This pain occurs due to stretching, and then a sharp contraction, like a spring, of the round uterine ligaments. The pain quickly passes if you immediately take a comfortable position and does not require special treatment.
You should definitely consult a doctor if:
- pain is accompanied by spotting bloody discharge from the external genitalia
- increasing duration and intensity of pain
- abdominal pain accompanied by dizziness, fever, loss of consciousness
Life hack! To normalize bowel movements, eat more vegetables and fruits, drink water and move more during the day. Try to eat often and in small portions.
4. Enlargement and soreness of the mammary glands.
Hormonal restructuring of the body during gestation is accompanied, among other things, by an increase in the size of the mammary glands and an increase in their sensitivity. By the end of the first trimester, the soreness usually disappears, no additional methods of treatment are needed.
Life hack! Choose comfortable supportive underwear (it should not leave marks on the skin at the end of the day). You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You may need a larger size or a sports bra. Pain in the mammary glands is relieved by a warm shower at the end of the day.
You should definitely see a doctor if:
- the pain is intense
- mammary glands are very dense with redness and body temperature is increased
- discharge from the nipples appears (purulent, bloody)
5. Increased body temperature.
In early pregnancy, an increase in body temperature to 37.5 ° C is not necessary, but is possible due to the peculiarities of the action of progesterone. Because of this, it is difficult for pregnant women to endure stuffy, hot rooms. Self-medication is dangerous: an attempt to bring down the temperature even with a seemingly harmless folk method - tea with raspberries - can mask the true cause of hyperthermia and delay the diagnosis. Due to the increased body temperature, pregnant women should dress in layers and avoid stuffy and hot rooms and spaces so that they can always “adjust” their temperature on their own.
- temperature above 37.5 °C
- along with fever, any pain occurs
- runny nose, cough, body aches appear
6. Nasal congestion, difficulty breathing, nosebleeds.
These symptoms can be explained by the individual reaction of the vascular system to the increase in blood volume that occurs during pregnancy. Another possible reason is dry air in the room, the operation of central heating batteries.
Life hack! The easiest way to deal with nasal congestion is to use a humidifier. If you don't have one, you can put a damp towel on the battery - less effective, but better than nothing. It is possible to use sprays with sea salt, but you need to carefully read the instructions and especially the "Indications" section, it should contain information about the safety of the product during pregnancy.
You should definitely see a doctor if:
- symptoms of a cold occur
- nasal congestion accompanied by ear congestion
- These symptoms appeared after exposure to the allergen known to you
7. Blood pressure fluctuations.
Blood pressure fluctuations.
An ideal option for the course of any pregnancy is the stability of the blood pressure throughout the gestation. However, this is extremely rare. A small (up to 10 units) increase in pressure from the usual reference may be due to an increase in the load on the cardiovascular system as a result of changes in body weight, hormonal changes, and uterine pressure on the vessels. Normal pressure: systolic below 130 mm Hg, diastolic no more than 85 mm Hg. Blood pressure in the range of 130–139/ 85–89 mm Hg considered high to be normal. High numbers are often observed in patients of older reproductive age, suffering from diabetes mellitus and kidney disease, obesity, etc. However, it is imperative to tell the doctor about all these concomitant pathological conditions at the first appointment and, if necessary, consult a neurologist, cardiologist, endocrinologist and other related specialists . Reasonable physical activity, adherence to sleep and wakefulness, a balanced diet, and the rejection of coffee and strong tea allow you to keep pressure within limits. Of the completely exotic for our days, but no less significant - the prevention of stress.
Of the completely exotic for our days, but no less significant - the prevention of stress.
Life hack! If you first discovered that you have high normal pressure, repeat the measurement after 15 minutes. If the pressure remains elevated, see a doctor.
Be sure to see a doctor if:
- your blood pressure is above 140/90 mmHg.
- pressure increased by more than 10 mm Hg. relative to your regular
- an increase in the pressure indicator is accompanied by edema, the appearance of "flies" before the eyes
NB! You should also pay attention to lowering blood pressure. Numbers less than 90/60 mmHg - an excuse to see a doctor.
Life hack! Keep a blood pressure diary, especially if you are prone to hypertension. Show your diary to your doctor at every appointment.
8. Heaviness and pain in the legs.
Heaviness and pain in the legs, especially in the evening, are frequent companions of pregnancy. There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
There is an explanation for the occurrence of symptoms: an increase in load due to growing weight and a shift in the center of gravity of the body.
Life hack! Ask your partner/husband to give you a foot massage, relax with your limbs elevated (not too much!) A therapeutic pedicure, dousing the legs with cool water, a contrast shower, a cream or gel for legs with cooling components (menthol, essential oils), as well as compression stockings or stockings of the lightest degree of compression will help.
You should always see a doctor if:
- one or both legs are very swollen or discolored
- previously diagnosed varicose veins, family history of thrombosis
9. Skin changes.
During pregnancy, you may notice dark spots on your skin. Especially often such darkening (hyperpigmentation) is observed in the nipple area, along the white line of the abdomen. Stretch marks (stretch marks) may appear on the skin of the abdomen and thighs. These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
These are normal signs and do not require any treatment. In most cases, skin color will return to normal after breastfeeding ends, and stretch marks will shrink and fade. Itching can be associated with stretching of the skin, especially in the abdomen and mammary glands. This symptom occurs infrequently and is usually successfully stopped by the use of special products to moisturize and soften the skin. By the way, these same remedies usually help in the fight against stretch marks.
Life hack! Oils and moisturizing creams to increase skin elasticity, contrast showers, massage with a hard brush will help reduce the likelihood of skin changes.
You should definitely consult a doctor if:
- along with itching there are areas of redness, spots, peeling
- itching increases
10. Bleeding gums.
Changes in the characteristics of blood circulation in the body of a pregnant woman can cause bleeding gums. The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
The appearance of minor blood impurities during brushing your teeth, when eating solid foods (for example, an apple) is acceptable. However, the key provision is "insignificant". If you find it difficult to assess your own condition, consult a specialist.
You should definitely consult a doctor if:
- you have loose teeth, sore gums, bad breath
- bleeding in the gum area increases
11. Fatigue, mood instability.
Tearfulness, lack of strength, forgetfulness, distraction, the whole palette of feelings "here and now"... The list can be continued, and there is only one explanation for this - pregnancy. The most common early symptom is severe fatigue. There is no universal recipe, just as there is no single picture of these states. The main recommendation for all pregnant women is to rest often, relax and even sleep during the day. Most importantly, you need to remember: pregnancy is not a disease, but a great time to prepare for motherhood.
Fears of pregnant women are overcome - nine useful tips :: Clinician
25 10.2017
-
Unfounded fears
-
Unnecessary alarms
-
Worries unsupported by arguments
-
Natural doubts
The time of pregnancy is nine months of happy expectation of a miracle, but sometimes the same number of months of fears and worries about the unborn child. In order to find joy and avoid unnecessary worries, to enjoy the gestation period, the necessary task is to get rid of the complexes, having determined the cause of the anxieties, to “quench” them. Mothers, husbands, relatives, of course, will help you (psychologically and physically), but the main mission to overcome your own anxieties lies with the pregnant woman.
The cause of anxiety is most often the physiological restructuring of the body, which leads to overwork, a weakened physical condition. This means that the expectant mother from the very beginning is predisposed to anxiety precisely in terms of physiological indicators. But understanding this phenomenon does not make it easier. The attending physician prescribes vitamins, trace elements, and in some cases hormones. It seems to be competent and according to plan, but ... it's still scary!
This means that the expectant mother from the very beginning is predisposed to anxiety precisely in terms of physiological indicators. But understanding this phenomenon does not make it easier. The attending physician prescribes vitamins, trace elements, and in some cases hormones. It seems to be competent and according to plan, but ... it's still scary!
But what are these very fears and how to overcome them? How many pregnant women, so many fears. Not all have a logical background, some are based on myths and superstitions, and some are based on elementary ignorance.
Unfounded fears
A woman does not always plan pregnancy while leading a normal life. And when she finds out about an accidental pregnancy, she begins to count with horror the number of glasses of wine drunk, cigarettes smoked, what harmful food she ate during conception. Of course, the correctness of the recommendations indicating the need for timely planning of pregnancy sounds reasonable. But if everything has already happened, a decision has been made to give birth, then it is important to clearly understand that the wisest thing is to bring your psychological state into harmony and create favorable conditions for the development of the fetus.
But if everything has already happened, a decision has been made to give birth, then it is important to clearly understand that the wisest thing is to bring your psychological state into harmony and create favorable conditions for the development of the fetus.
Fear of miscarriage is an understandable concern. To identify the problem as early as possible, take tests every other day. The best arguments for well-being in this matter are indicators and numbers.
Unnecessary worries
To drink coffee or not to drink - fans of aromatic grain drink exhaust themselves with this question, who cannot live a day without this drink. But every morning to tremble at this thought is definitely harmful to the unborn child. Let's look for an alternative. Is it better to spend the whole day at work sluggish and sleepy than to still dare to drink a cup of coffee with milk to cheer up?
Recent scientific studies have shown that a cup of coffee a day does not harm the child. Pregnant women are allowed to drink, but it is recommended to use it less often, in addition, use sparing options: instant coffee or no caffeine at all.
Pregnant women are allowed to drink, but it is recommended to use it less often, in addition, use sparing options: instant coffee or no caffeine at all.
Taking medicine or suffering pain (discomfort)? Pregnant women are usually extremely distrustful when even doctors prescribe pills to them. Even after the time spent at the consultation with a specialist, some “pregnant women” discuss the medicines prescribed by the doctor on women's forums for greater reliability. In order not to panic and not look on the Internet for advice from pregnant alarmists whose competence you are not sure, it is wiser to find a doctor who you can trust 100%! The field of gynecology in our clinic is one of the most developed and intensive areas of work.
Anxiety unsupported by arguments
Does it seem to you that your belly is growing slowly or, conversely, is it too big? This is not a serious cause for concern. The main thing is that the ultrasound confirmed that the fetus develops according to the deadline. Also, pregnant women worry that they are gaining weight rapidly or are malnourished. Eat a balanced diet and get enough (again, with the permission of your doctor) to move, then the weight will be within the normal range.
Also, pregnant women worry that they are gaining weight rapidly or are malnourished. Eat a balanced diet and get enough (again, with the permission of your doctor) to move, then the weight will be within the normal range.
When the baby pushes hard, it is scary at first, and if the pushes are weak, perhaps even more scary. Indeed, both may indicate hypoxia. Share your concerns with your doctor, a toned uterus is a solvable problem. Just in case, study the so-called "method 10", based on the calculation of the fetal heart rate. So you will participate in the process not passively, but meaningfully. By the way, it is in your power to actively help the cub: walk daily in the fresh air, sign up for an oxygen cocktail course. Most likely, this is how the child simply shows temperament. But if the reason is more complicated, remember that medicine can cope with such problems. Hypoxia (if it is not chronic) is amenable to medical adjustment, as a result of which the tension of the walls of the uterus decreases, and blood circulation improves.
Childbirth is delayed, and this is fraught with the fact that a woman is daily absorbed in listening to herself and looking for harbingers in fear of missing the start of the long-awaited process. On the one hand, vigilance does not seem to interfere, but one thing is clear - it is impossible to miss childbirth, there is no turning back. Perhaps the day of birth is simply incorrectly determined, because pregnant women do not always know the day of conception exactly.
Natural doubts
Are you afraid of natural childbirth, scary and surgical intervention? Remember that most panic plans (not related to pregnancy) are implemented in a completely different way than your imagination draws, so fantasizing, winding yourself up is not a good idea. Even if the child is born as a result of a caesarean section, this sometimes happens. The main thing is that the birth is safe for the baby and the mother. To give confidence in this matter, it is useful to attend childbirth preparation groups with your husband.