Pregnancy anal leakage
Symptoms & Types - Bowel Control
Bowel control disorders affect the normal pattern of emptying your bowels. There are many factors that contribute to normal bowel movements, including the consistency of your stools, diet, medical problems, surgical history, ability of the rectum to hold stool and the coordination of various pelvic muscles to allow emptying.
What is normal? That’s hard to say exactly. When it comes to bowels, we are all different. You don’t have to have a bowel movement every day. On average, normal stool frequency is at least 3 bowel movements a week, and no more than 3 stools per day. Stool consistency often varies based on what you’re eating, how much water you drink, and how much exercise you get. The first stop is to pay attention to your OWN normal.
You may want to keep a diary of your bowels to take with you to your doctor’s appointment – chart out the day, time, and consistency of the stools you pass, including any episodes of leakage.
Use this guide to help describe your stools:
Accidental Bowel Leakage
Accidental bowel leakage (ABL), also known as fecal incontinence, is the loss of normal control of the bowels, leading to leakage of solid or liquid stool or gas. About 8 out of every 100 women struggle with ABL. The number of women affected increases with age. And, researchers think that in reality, the total number of women is likely much higher, but many are too embarrassed to seek treatment.
Causes of Accidental Bowel Leakage
There are many causes of accidental bowel leakage, including injury caused during childbirth, damage to the anal sphincter or nerves, pelvic organ prolapse, fistula, medical problems and abnormal stool consistency.
Childbirth Injury
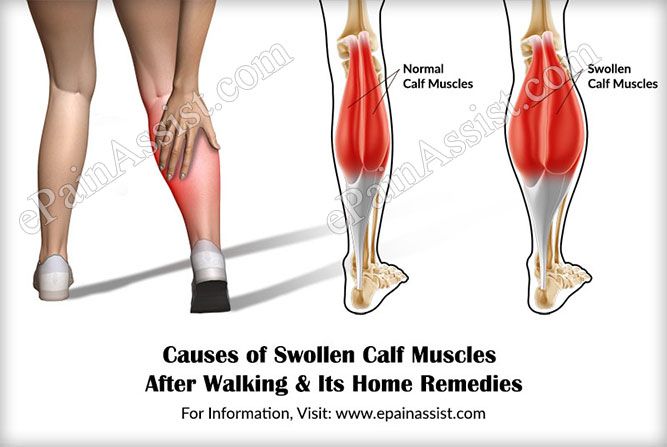
Pregnancy can increase the risk of accidental bowel leakage. It is more common in women who deliver vaginally than women who have a C-section. However, research also suggests that just carrying a pregnancy can increase your risk of these changes as well.
Delivering a large baby vaginally, especially if forceps are used, poses more risk than having a smaller baby. An episiotomy or significant tear of the tissues around the vagina and rectum can result in damage to the nerves, muscles, and tissues around the rectal canal. This can result in a tear of the anal sphincter muscles that help to hold in stool, but also some of the surrounding tissues that are important as well.
This can result in a tear of the anal sphincter muscles that help to hold in stool, but also some of the surrounding tissues that are important as well.
Anal Sphincter Injury
There are two main circular muscles, or sphincters, that help to hold in stool near the anal opening. During vaginal childbirth, the anal sphincter muscles can be damaged or torn. These muscles allow us to control bowel movements. It is estimated that as many as 40% of women experience muscle injuries in this area during childbirth. Some of these tears are recognized and repaired, but some are hidden. Injury is more common after episiotomy or forceps delivery.
The anal sphincter muscles can also become weakened for other reasons, such as diabetes or neurologic conditions. They can also be damaged during other surgeries, such as surgery to fix an anal fissure or hemorrhoids. This can cause decreased strength resulting in problems controlling passage of bowel movements.
Ultrasound can help to detect these injuries. Depending on the extent of the injury and the length of time from when it occurred (for example, how long ago you delivered your baby), surgery can repair the damage. If the damage occurred in the past, surgery may not be able to help.
Depending on the extent of the injury and the length of time from when it occurred (for example, how long ago you delivered your baby), surgery can repair the damage. If the damage occurred in the past, surgery may not be able to help.
Nerve Injury
Injury to the anal sphincter nerves can cause decreased sensation and muscle strength, both of which can contribute to ABL. Vaginal delivery, chronic constipation, or illnesses that affect the nerves such as diabetes and spinal cord injury can result in nerve damage. For some women, nerve damage that occurs during vaginal delivery improves on its own one or two years after childbirth.
Prolapse
Several types of prolapse can affect bowel control.
- Rectocele: A rectocele is a hernia of the bowel upward into the vaginal canal. It causes a vaginal bulge that can sometimes result in difficulty emptying the bowels.
- Rectal prolapse: Rectal prolapse is a condition where the rectum slides out through the anal opening.
 This causes a bulge coming from the anus, not from the vagina. Distortion of the anal opening can result in damage to the sphincter muscles and bowel leakage.
This causes a bulge coming from the anus, not from the vagina. Distortion of the anal opening can result in damage to the sphincter muscles and bowel leakage. - Hemorrhoids: Hemorrhoids are caused by enlarged blood vessels near the anal opening. Sometimes they can cause small bulges near the anal opening. These can make it difficult to clean near the anus, resulting in seepage of bowel contents. There are many treatments for hemorrhoids, ranging from medicines to surgery to remove them. However, if hemorrhoids are removed, one out of every 10 women will end up with fecal incontinence.
Fistula
Abnormal openings or connections (tracts or tunnels) known as “fistulas” can develop between the bowel and vagina, or the bowel and the skin. Fistulas can occur:
- After vaginal delivery or vaginal surgery. This is more likely if a large tear occurred during delivery but is still unusual.
- Spontaneously as a result of diverticulitis or other bowel conditions, including Crohn’s disease.

- In patients who have had radiation in the pelvis.
Abnormal Stool Consistency
Bowel movements with normal consistency are easiest to control. Ideally, stools should be like toothpaste. Abnormal stool consistency (either loose or hard stools) may contribute to ABL:
- Diarrhea or loose bowel movements are more difficult to control. This can also increase the sensation of needing to pass stool, called fecal urgency.
- Severe constipation. People who have significant problems passing stool can experience a hard lump of stool with diarrhea that develops around it.
Constipation
Everyone is different, but most women normally have bowel movements at least every other day and no more than twice daily. Having a bowel movement less than three times per week, along with straining to produce a hard bowel movement, is called constipation. Constipation is very common, affecting about 1 in 3 women.
Causes of Constipation
Constipation occurs for several reasons. It may be related to diet or changes in the nerves that control the pelvic floor muscle functioning that can affect the bowels. Lifestyle choices, medicines, or supplements, pelvic floor disorders, lack of exercise, and other health problems may also impact bowel movements.
It may be related to diet or changes in the nerves that control the pelvic floor muscle functioning that can affect the bowels. Lifestyle choices, medicines, or supplements, pelvic floor disorders, lack of exercise, and other health problems may also impact bowel movements.
Dietary Problems
The most common reason for constipation is not having enough fiber in your diet. This is very common in women who eat a typical American diet and getting enough fiber to fix this problem often requires planning and supplementation. The general recommendation is to aim for 25-35 gram/day of fiber between food and supplements.
Some foods, especially those high in starch such as white rice, pasta, or white bread, are more likely to lead to constipation.
Constipation may also be due to lack of fluids in your diet. Some women do not drink enough fluids to keep their stool soft. When there is not enough fiber or water in your diet, bowel movements are more likely to be hard or irregular. However, excessive fluid will not help constipation, especially if there is another underlying dietary problem. Discuss with your provider what the right amount of fluid is for you.
However, excessive fluid will not help constipation, especially if there is another underlying dietary problem. Discuss with your provider what the right amount of fluid is for you.
Medicines and Supplements
Talk with your doctor about the medicines and supplements you take, as many can cause constipation. Ask about alternative medicines without constipating effects. Medicines that treat bladder urgency, depression, blood pressure, and pain (especially narcotic medicines) commonly cause constipation. Iron and calcium supplements can do this also.
Pelvic Floor Disorders
Pelvic pain may prevent relaxation of pelvic floor muscles, leading to problems having bowel movements. Straining excessively with bowel movements may lead to pelvic floor disorders. Rectoceles do not cause constipation. Prolapse, including rectoceles and rectal prolapse, can make constipation worse.
Medical Conditions
Irritable bowel syndrome, chronic pain, kidney disease, colitis, thyroid disorders, neurological conditions (such as multiple sclerosis or spinal cord injuries), and cancer are other medical conditions that can impact the bowels. Talk with your doctor if you have these conditions or are concerned about them.
Talk with your doctor if you have these conditions or are concerned about them.
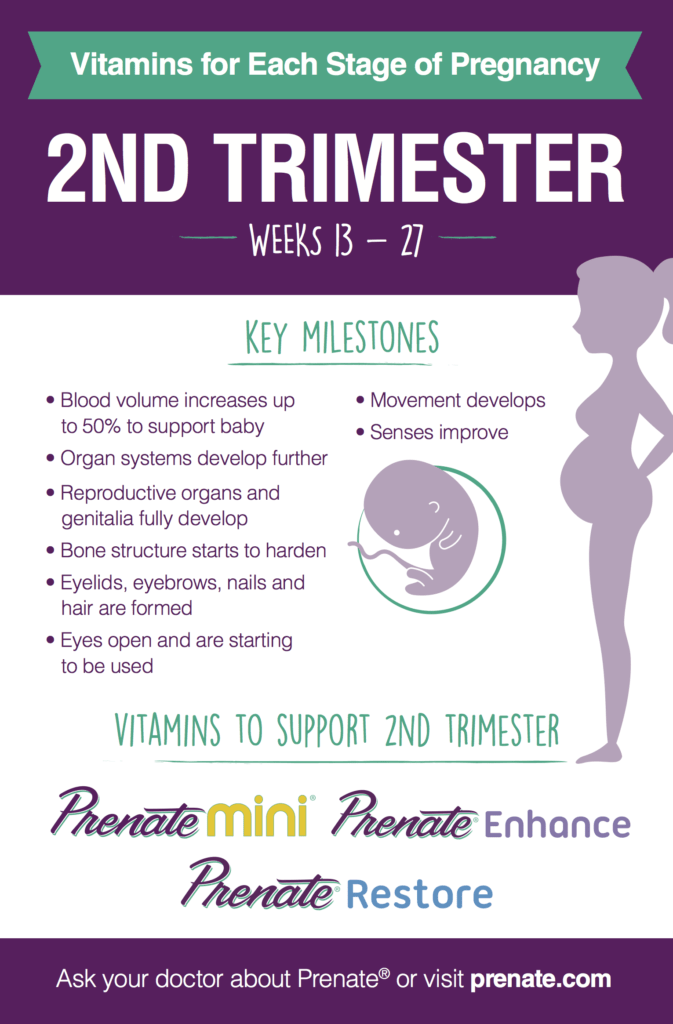
Incontinence During Pregnancy And Childbirth
You’ll find no mention of incontinence in prenatal classes or in parenting guides. But ask a soccer mom or baby boomer about ‘leaking, pads, and diapers’ in private, and you’ll likely hear a personal story or be shown a surgical scar. Among mothers of all ages, incontinence and other pelvic problems are common.
-
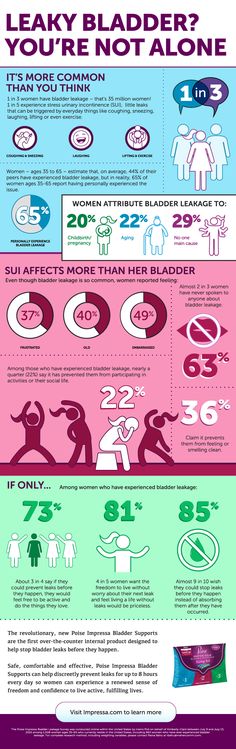
Urinary Incontinence. The most common type of incontinence to affect mothers, UI affects 30-50% of childbearing women by age 40. Up to 63% of stress-incontinent women report their problem began during or after pregnancy.
-
Fecal Incontinence. Defined as loss of control over gas or stool, fecal incontinence (also known as accidental bowel leakage or ABL) affects up to 25% of childbearing women, often resulting from injury during birth.
-
Pelvic Organ Prolapse.
 This refers to weakening around the vagina, uterus, and pelvic floor—common types include cystocele (dropped bladder), rectocele (bulging rectum), and uterine prolapse (dropped uterus).
This refers to weakening around the vagina, uterus, and pelvic floor—common types include cystocele (dropped bladder), rectocele (bulging rectum), and uterine prolapse (dropped uterus).
For too long, these problems have been regarded as inevitable costs of motherhood—but attitudes are changing. Life after childbirth does not need to include a routine of pads and liners. A woman should not have to constantly struggle with symptoms at home, work, the gym, or even in the bedroom.
Whether childbirth was easy or difficult, long or short, one fact holds constant: your body will never be exactly the same after pregnancy and delivery as it was before. And while learning ‘what to expect while you’re expecting’ is important, knowing what to expect afterwards is the key to prevention. Indeed, decisions made during pregnancy and childbirth may impact your bladder and pelvic function for years to come. A few areas of your body are particularly important:
-
The perineum lies between the vaginal and anal openings, it is the area cut with an episiotomy.
 Injuries may create vaginal ‘looseness’ or bowel problems.
Injuries may create vaginal ‘looseness’ or bowel problems. -
Levator muscles provide key support for the pelvic organs—helping to maintain control over bladder and bowels. After childbirth, muscle strength is usually compromised.
-
Pelvic nerves maintain strong and healthy levator muscles. Nerve injuries, especially common after a long or difficult delivery, are associated with incontinence.
-
Connective tissues help to secure the pelvic organs in place. During childbirth they routinely stretch, tear, and weaken.
-
Your pelvic bones have a unique size and shape, which may influence the physical ease or difficulty you might encounter with childbirth, and the extent of pelvic injury.
BIRTHING STRATEGIES
If you are pregnant, or even thinking about becoming pregnant, it is never too early to get your body in shape to minimize the physical effects of carrying a child.
Kegel exercises, also known as pelvic floor muscle exercises, can decrease incontinence, and your first pregnancy is one of the best times to learn about them. Not only because the need is so great—up to 70% of women have some leakage during or after pregnancy—but the muscles have not suffered the trauma of birth.
Not only because the need is so great—up to 70% of women have some leakage during or after pregnancy—but the muscles have not suffered the trauma of birth.
Another helpful activity is called the Perineal massage. It involves gentle stretching of the vaginal opening, and may decrease the risk of birth injury and pain afterwards.
Several aspects of childbirth that may seem inevitable are, in fact, choices to be considered. While easy to say but hard to enact, staying as relaxed as possible for as long as possible can greatly reduce pain of delivery. When stress hormones kick in and pelvic floor tension rises, pain or anxiety increases. The results can directly impact incontinence in the coming days and even for years to come.
Along with a relaxation strategy, there are other things you can explore to make childbirth less stressful on you and your child. There is no avoiding the fact that labor pushing introduces tremendous strain on the pelvic floor.
While there is no one ‘best’ method of pushing, you should know your options.
-
Which position? Although lying down on your back (lithotomy) is most common, alternatives include squatting, sitting, sidelying, and standing. Certain positions might influence the risk of pelvic or perineal injury, such as back lying with legs strapped in stirrups.
-
When to begin? Recent studies indicate by allowing the fetus to ‘passively’ descend through the birth canal with gentle pushing reduces the risk of difficult deliveries, forceps, and perineal injury.
-
For how long? Prolonged pushing may sometimes increase the risk of pelvic nerve injury, fecal incontinence, and bladder dysfunction. You may wish to discuss reasonable limits for pushing ahead of time with your doctor or nurse midwife.
Other childbirth issues include surgical techniques such as episiotomy. This refers to the intentional cutting of the perineum during childbirth. Today it’s known that episiotomies are rarely of benefit in terms of preventing injuries to the pelvic area. However, ‘selective’ episiotomy remains an important tool and can benefit the immediate health of mother and child.
However, ‘selective’ episiotomy remains an important tool and can benefit the immediate health of mother and child.
Obviously, big babies are associated with more severe perineal, rectal and pudendal nerve injuries, and incontinence. If you are carrying a macrosomic (9 pounds or more) baby, be sure to understand these issues.
While the use of a vacuum may be associated with less pelvic floor trauma, forceps delivery carries an increased risk for urinary incontinence and injuries to the anal sphincter and pelvic floor compared with spontaneous vaginal birth.
The ‘Cesarean by Choice’ debate is surrounded by complex medical, economic, and social questions. In parts of South America, cesarean rates exceed 90%, whereas trends in Europe have favored vaginal birth whenever possible, even if it entails a long or difficult labor.
Determining the right policy will require more research. In the meantime, know the facts.
-
Consider the risks.
 Although a c-section is safer today than at any time in the past, it still carries potentially serious risks for mother and baby.
Although a c-section is safer today than at any time in the past, it still carries potentially serious risks for mother and baby. -
Consider the benefits. Urinary incontinence, anal injuries, and pelvic prolapse are less common after cesarean. C-sections with the lowest incidence of injury appear to be those performed in the first pregnancy, before labor begins.
-
Individualize your choice. Most obstetricians and midwives share the goal of a vaginal birth whenever the benefits outweigh the risks. In some cases, a difficult vaginal delivery may be more physically traumatic than a cesarean. For others, the exact opposite will be true.
Breaking Her Silence: Some Things Are Too Important To Hold In
Childbirth can bring about lots of amazing changes, but many women don’t count on incontinence being one of them. Click the image below to watch our short film about dealing with incontinence after childbirth, and why it’s so important to speak up about your condition, not only for yourself, but for the ones closest to you.
AFTER DELIVERY
What can be done after delivery to prevent problems?
Physical recuperation after childbirth is substantial—and too often overlooked. Alongside the diaper changes, you should take steps to rehabilitate your pelvic floor. As noted above, Kegels are vital to strengthening pelvic floor muscles and reducing risk of incontinence issues.
Pelvic floor muscle exercises will help to restore muscle function before it is permanently lost and lessen the symptoms of incontinence. Women who have difficulty performing pelvic floor muscle exercises on their own may find that biofeedback therapy with the help of a nurse specialist or physical therapist enables them to witness significant improvement in pelvic floor strength. Incontinence and pelvic floor symptoms almost always have solutions and shouldn’t be shrugged off as normal.
Immediately following childbirth, preventing perineal swelling helps restore your body to health. Ice packs and proper hygiene are employed to avert infection. Also, avoiding constipation reduces strain against the pelvic floor.
Signs, symptoms and causes of hemorrhoids in pregnant women - NEARMEDIC network of clinics
The main causes of hemorrhoids in pregnant women can be as follows:
- Chronic constipation. In this case, the stretching and tension of the walls of the rectum increases during defecation, which leads to the formation of hemorrhoids. In pregnant women, constipation occurs much more often due to a decrease in intestinal tone.
- Inactive lifestyle. With hypodynamia, blood stagnation occurs in the venous plexus of the rectum, which eventually leads to vein thrombosis and the formation of hemorrhoids. Features of the condition do not always allow pregnant women to be mobile, therefore they have a high risk of developing this disease.
 nine0006
nine0006 - Disturbance of blood circulation in the lower half of the body. During pregnancy, the uterus grows and compresses the inferior vena cava. This leads to stagnation of blood in the veins of the legs and rectum. During childbirth, a woman's intra-abdominal pressure rises greatly - this can cause hemorrhoids after pregnancy.
Signs of hemorrhoids in pregnant women
The longer the period, the higher the likelihood of developing the disease. Most often, hemorrhoids appear in the 3rd trimester or after childbirth. nine0003
The blood vessels of the hemorrhoidal plexus of the rectum gradually dilate. Over longer periods, the stretching of the veins becomes even stronger. With the expansion of the walls of the veins of the rectum, they lose their elasticity. This provokes protrusion of the veins under the mucous membrane.
If hemorrhoids protrude only into the lumen of the rectum and do not come out of the anus, then we are talking about the treatment of hemorrhoids of the 1st stage. The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back. nine0003
The farther, the larger the knots become and the more they sag from the anus. In the second stage of hemorrhoids, the nodes sag from the anus, but are easily set back on their own. The third stage occurs when the nodes can no longer cope back. nine0003
The symptoms of the disease depend on its stage.
- Internal hemorrhoids. Symptoms are mild, there is no sagging of hemorrhoids from the anus. At this stage, women may experience pain during bowel movements, slight bleeding or fresh blood on the stool, and itching and discomfort in the anus.
- External hemorrhoids. The main symptom is the sagging of one or more purple-red nodes from the anus. This manifestation is the main sign of what is required, and not of another disease, such as anal fissure. Walking, sitting and defecation in this case become extremely painful. nine0006
Urgent medical attention is required in case of infringement of the hemorrhoid - a pregnant woman experiences very severe pain in the anus with fever.
Treatment of hemorrhoids during pregnancy
If a woman already has any symptoms of hemorrhoids - itching, pain in the anus, bleeding from the anus, etc. - professional treatment is required.
At NEARMEDIC, the first stage of treatment is the preventive measures described above, which stop the progression of the disease. Then the woman is prescribed drugs, both local and systemic. But due to pregnancy, local therapy is preferable, as this reduces the risk of side effects, increases the effectiveness of treatment and reduces the negative effects of drugs on the child. In any case, the medicine is prescribed only by the attending physician who observes the woman during pregnancy. nine0003
In the case when a woman already has prolapsed nodes that cannot be set, an operation is prescribed. Other indications for surgical intervention are infringement or necrosis of the hemorrhoid, as well as acute inflammation. Most often, in NEARMEDIC surgery is postponed until the postpartum period, and during pregnancy they are limited to conservative treatment.
Prevention of hemorrhoids during pregnancy
Due to the fact that all pregnant women are at high risk of developing hemorrhoids, NEARMEDIC clinic doctors strongly recommend that preventive measures be taken throughout pregnancy, without waiting for symptoms to appear. nine0003
- Relief of constipation. To do this, you need to adjust your diet: eat more foods that contain coarse vegetable fiber - vegetables, fruits, cereals, cereals, prunes. Dairy products also have a beneficial effect on digestion. On the contrary, it is better to refuse meat and other foods rich in protein. As well as from an excess of fat, coffee and hot spices.
- Hygiene. It is recommended to wash the perineum and anus after each act of defecation. In addition, once a day you can take sitz baths with antiseptics: chamomile infusion, a weak solution of potassium permanganate, etc. nine0006
Doctors
Who treat hemorrhoids during pregnancy
More doctorsClinics in Moscow
For all questions, you can contact the single contact center: +7 (495) 6-171-171
Anal fissure during pregnancy and after childbirth | CM Global Clinic
Contents
- 1 Causes of anal fissure during pregnancy
- 2 Anal fissure after childbirth
- 3 Why you need to see a doctor
An anal fissure during pregnancy and after childbirth is a problem that can ruin the life of even the most persistent woman. Do not hope that after childbirth, the anal fissure will pass. It should be treated both during pregnancy and after childbirth.
Do not hope that after childbirth, the anal fissure will pass. It should be treated both during pregnancy and after childbirth.
Anal fissure - a nuisance that can befall any person - woman or man; young guy or old man; a perfectly healthy strong man or a constantly ill weakling; a woman who has never given birth or is pregnant. nine0060 It is especially unpleasant when an anal fissure (AT) appears during pregnancy and after childbirth, as women during this period are quite vulnerable and weak. But it happens and, unfortunately, not so rare.
About ten to fifteen percent of women, during pregnancy and after childbirth, suffer from pain and rectal bleeding, and it is the anal fissure that causes these torments.
Causes of anal fissure during pregnancy
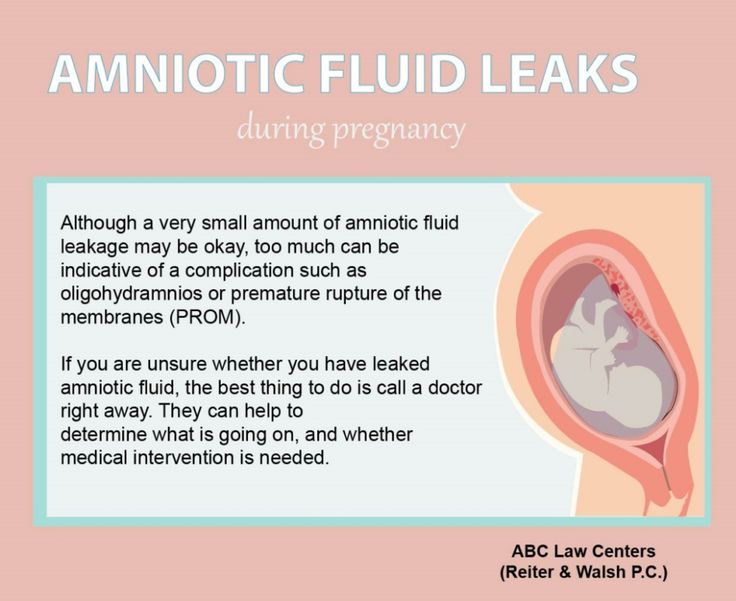
With the growth of the fetus, the uterus increases, and this causes compression of the pelvic veins. The outflow of blood from the pelvic organs is disturbed, and it stagnates in the veins of the rectum, creating conditions for the occurrence of AT. nine0060 Against the background of hormonal changes, tissue edema occurs, including rectal tissues. Intestinal tone decreases, peristalsis becomes sluggish, and this contributes to the formation of antibodies.
nine0060 Against the background of hormonal changes, tissue edema occurs, including rectal tissues. Intestinal tone decreases, peristalsis becomes sluggish, and this contributes to the formation of antibodies.
Many pregnant women constantly eat sweets, this also leads to digestive disorders and the appearance of AT.
For obvious reasons, a pregnant woman cannot be as active as she was before pregnancy. Low mobility causes constipation, due to which she strains in the toilet, and this, in turn, contributes to the development of AT. nine0003
Anal fissure after childbirth
Some doctors believe that anal fissure, diagnosed in a woman in the postpartum period, is formed during childbirth, when the fetus "goes". Since the passage of the fetus, and especially its head, through the pelvic floor, causes tension in the tissues of the rectum, creating favorable conditions for the occurrence of AT, and if the fetus is large, then the tension becomes even greater and therefore anal fissure is more often formed in such mothers.
However, often, after childbirth, a woman does not have any damage to the anus, but AT appears within the first two months. It is most often caused by constipation and the fact that dense stool passes through the vulnerable, postpartum, tissues in the rectum and causes sores, bleeding and pain. nine0060 Since many women know that during and after pregnancy there are painless rectal bleeding caused by an anal fissure, and that there are most often no swelling or nodes on the outside, they are in no hurry to go to the doctor and treat themselves. This is a big mistake.
Why you should go to the doctor
First . It happens that a woman confuses gynecological bleeding with rectal bleeding, and these are completely different problems. They cause completely disparate complications and require different methods of treatment. nine0060 Second . Even if bleeding does occur due to an anal fissure during pregnancy or after childbirth, it is necessary to determine exactly what stage the disease is at and treat the woman accordingly.