Post nasal drip pregnancy first trimester
Understanding Pregnancy and Post-Nasal Drip
Welcoming a tiny new family member into your family can be one of life’s most exciting experiences. At the same time, pregnancy can often take a toll on a woman’s health. One of the least discussed health challenges that accompany pregnancy is the increased risk of developing post-nasal drip. Post-nasal drip during pregnancy is actually quite common; 30% of women suffer from chronic sinus issues during their pregnancy.
Why does pregnancy cause sinus problems? What can you do relieve your symptoms? Get the facts that every mom-to-be needs to know!
Why Post-Nasal Drip and Pregnancy Happen Together
Have you ever experienced the uncomfortable sensation of being unable to clear the mucus that has collected at the back of your throat? This miserable state of affairs is a condition known as post-nasal drip. Unfortunately, pregnant women are extremely susceptible to developing post-nasal drip. In fact, the development of post-nasal drip during pregnancy is so common that it has its own name: pregnancy rhinitis.
There’s a strong link between pregnancy and post-nasal drip. During pregnancy, the body produces excessive amounts of mucus that the body expels through the nose. Unfortunately, the excess mucus can clog the sinuses and begin to drain down the throat, causing irritation. As if bothersome drainage wasn’t bad enough, post-nasal drip can cause chronic nasal congestion, a raspy cough, post-nasal drip headaches, and a sore throat.
Taking care of a “normal” sinus infection is hard enough, but doing so during pregnancy comes with its own set of challenges. The hormonal influx that occurs during pregnancy makes a woman’s immune system very sensitive, which in turn can cause worse-than-normal inflammation and congestion in pregnant women. Symptoms can be further exacerbated if the pregnant woman suffers from pre-existing seasonal allergies or chronic sinusitis.
Safe Sinus Treatments For Post-Nasal Drip During Pregnancy
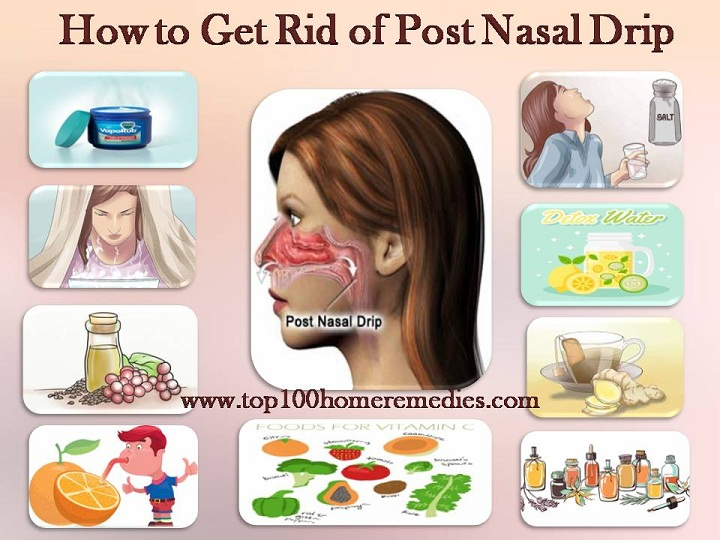
Common sinusitis and post-nasal drip treatments such as decongestants, allergy medications, and antibiotics, may be off-limits during a woman’s pregnancy. However, relief from sinus symptoms is still obtainable for pregnant women.
However, relief from sinus symptoms is still obtainable for pregnant women.
- Avoid Allergens: Taking allergy medications can be dangerous for pregnant women, but that doesn’t mean they don’t have options. Avoid indoor and outdoor allergies so as not to trigger the immune system. If possible, invest in a HEPA air filter to help keep indoor spaces clean and allergy-free.
- Stay Active: With a doctor’s approval, keep up a routine of light exercise. Exercise can help reduce the symptoms of pregnancy rhinitis.
- Adjust Your Diet: During pregnancy, a woman’s body is far more likely to experience symptoms of acid reflux, which can worsen post-nasal drip. Avoid acid reflux and the accompanying sinus pain by steering clear of very acidic foods, such as chocolate, fruit juices, or drinks that contain caffeine.
Achieve Healthy Sinuses Before and After Pregnancy at Kaplan Sinus Relief
If you or a loved one are planning to get pregnant in the near future, now is the time to address pre-existing sinus problems. Effective treatments like balloon sinuplasty can eliminate sinus issues for years at a time. Similarly, if your sinus issues do not clear up after your pregnancy, it may be time to seek long-term relief.
Effective treatments like balloon sinuplasty can eliminate sinus issues for years at a time. Similarly, if your sinus issues do not clear up after your pregnancy, it may be time to seek long-term relief.
Whether you are pre-pregnancy, post-pregnancy, or currently pregnant, Kaplan Sinus Relief can help you find true sinus relief right here in Houston. To discover a treatment that’s right for you, contact today us to schedule an appointment.
Baby (and tissues!) on board: Tips for managing pregnancy rhinitis | Your Pregnancy Matters
×
What can we help you find?Refine your search: Find a Doctor Search Conditions & Treatments Find a Location
Appointment New Patient Appointment
or Call214-645-8300
MedBlog
Your Pregnancy Matters
October 6, 2020
Your Pregnancy Matters
Robyn Horsager-Boehrer, M. D. Obstetrics and Gynecology
D. Obstetrics and Gynecology
When you think of side effects or symptoms brought on by pregnancy, nasal congestion and runny nose are not typically among the first to come to mind.
But maybe they should. Having a stuffy nose, difficulty breathing or sleeping, and snoring when pregnant can be alarming, especially amid the COVID-19 pandemic and the start of flu season.
Pregnancy rhinitis, also called gestational rhinitis, is a common ailment in the second and third trimesters, affecting approximately 20% of women. Characterized by inflammation and swelling of the mucous membranes in the nose, pregnancy rhinitis symptoms include congestion (nasal obstruction), sneezing, postnasal drip, and runny nose.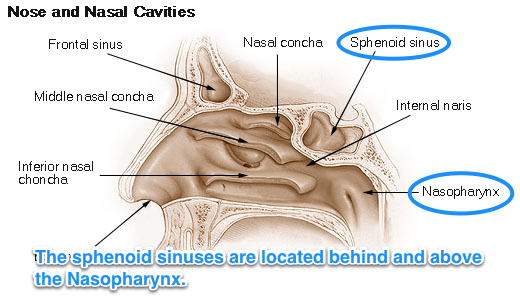 These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
These symptoms can also lead to poor sleep when your growing belly might already be making it difficult to rest.
All these issues can dramatically affect your mood and quality of life. The good news is that, for most patients, pregnancy rhinitis is temporary and there are safe, effective treatments available.
I've invited my colleague, Ashleigh Halderman, M.D., an ear, nose, and throat specialist at UT Southwestern to explain in more detail the causes of pregnancy rhinitis and how patients can manage their symptoms.
What causes pregnancy rhinitis?
Dr. Ashleigh HaldermanThe root cause of rhinitis can be allergic (affected by environmental irritants) or non-allergic (caused by infection). However, we are still learning how rhinitis is related to pregnancy.
We know that smoking, as well as having chronic rhinitis before pregnancy, predisposes patients to developing pregnancy rhinitis. Research suggests a few more potential causes:
Research suggests a few more potential causes:
- Having extra fluid in the body: During pregnancy, the body makes more blood and fluids, which can cause swelling, even in unexpected places such as the nasal passages. Blood vessels in the nose can swell with this additional volume, causing stuffiness.
- Higher levels of estrogen: Estrogen in older formulations of birth control pills has been associated with a side effect of nasal obstruction. However, in studies of the menstrual cycle, we don't see congestion with fluctuating estrogen levels. So, the connection remains unclear for now.
- Creation of human growth hormone: The placenta creates a variant of the human growth hormone (HGH), which has been associated with nasal symptoms in other conditions. For example, tumors that grow on the pituitary glands secrete growth hormones, which can cause severe nasal congestion.
Gestational rhinitis is under-researched. Data to date suggest no known association of rhinitis with pre-existing asthma, maternal age, duration of pregnancy, or the number of times a patient has been pregnant.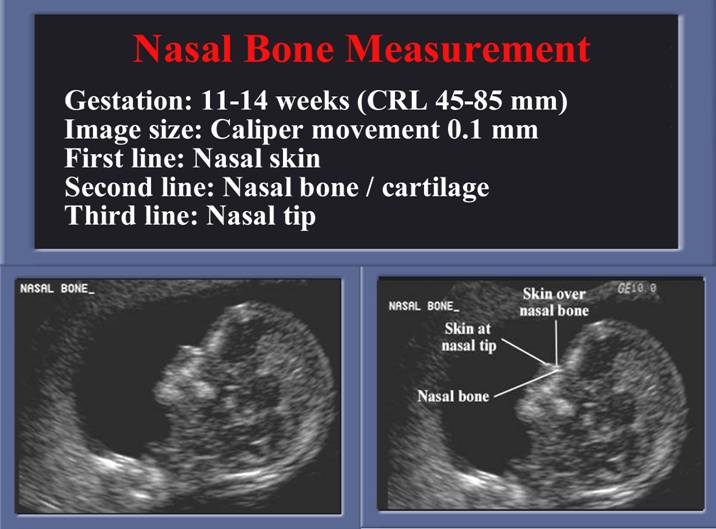 However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
However, a recent study found that patients carrying female babies were diagnosed significantly more often than patients carrying male babies.
Related reading: How to manage allergies and asthma during pregnancy
How long do symptoms last?
The annoying, uncomfortable symptoms of pregnancy rhinitis typically last six weeks or longer. For most patients, symptoms typically resolve two weeks after delivery.
Approximately a third of patients who had chronic rhinitis before pregnancy will have the same level of symptoms during, and a third will experience worsening of rhinitis symptoms. However, the remaining third will have less severe or no symptoms during pregnancy. I've had many women tell me they've felt the best, sinus-wise, when they were pregnant. However, there's no specific reason why this occurs.
Related reading: 5 weird pregnancy symptoms you might not know about
What treatments are available?
The first step toward relief is a visit with your doctor to rule out infection, such as COVID-19, influenza, or sinusitis.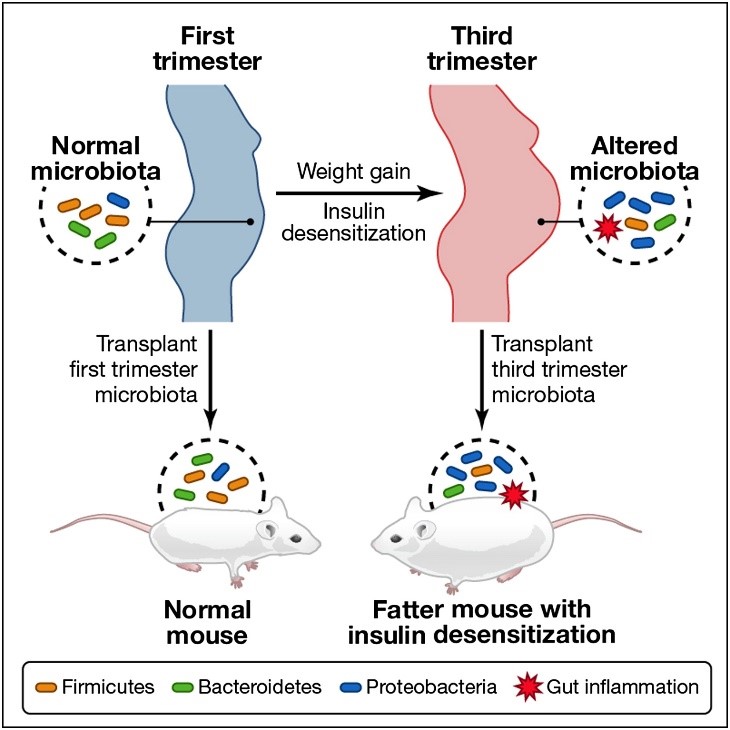 We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
We may also recommend testing for concerns such as sinusitis or pregnancy tumor (pyogenic granuloma) – a non-cancerous growth of blood vessels that may appear during pregnancy.
From there, your doctor and Ob/Gyn may suggest:
- Getting regular exercise: Working out has been shown to significantly help relieve nasal congestion and regulate the sleep cycle. All the more reason to bust a move during pregnancy!
- Elevating your mattress: Try positioning the mattress so your whole body is situated at a 45-degree angle. While not widely studied, patients have reported that this helps clear the nasal passages enough to sleep.
- Using a humidifier: Adding a little moisture to the air can help alleviate nasal irritation. Many patients use them at night to wake up feeling less stuffy.
- Trying a sinus wash: Nasal saline sprays or sinus irrigation systems such as a neti pot can help clear the sinuses. Make sure to use distilled or boiled (and cooled) water – using water straight from the tap is not recommended.
Topical decongestants such as Afrin can be incredibly and immediately effective, but there is a risk of dependency. If you use this type of treatment more than once or twice a week, your nose can become "addicted" to it, which can lead to rhinitis medicamentosa – the spray will stop working as well, and your symptoms may get worse. Also, unlike gestational rhinitis, rhinitis medicamentosa won’t resolve after you deliver. It will only resolve when you stop using topical decongestants.
In general, pregnant patients can take decongestants that include pseudoephedrine as directed. However, we always recommend talking with your Ob/Gyn first, especially if you have high blood pressure.
Your Ob/Gyn might also recommend a steroid nasal spray, such as Flonase or Rhinocort, for severe symptoms. If you were using a spray to manage chronic rhinitis prior to pregnancy, your Ob/Gyn might advise you to keep using it during pregnancy. It is generally considered safe to use these products while breastfeeding, under your Ob/Gyn's guidance.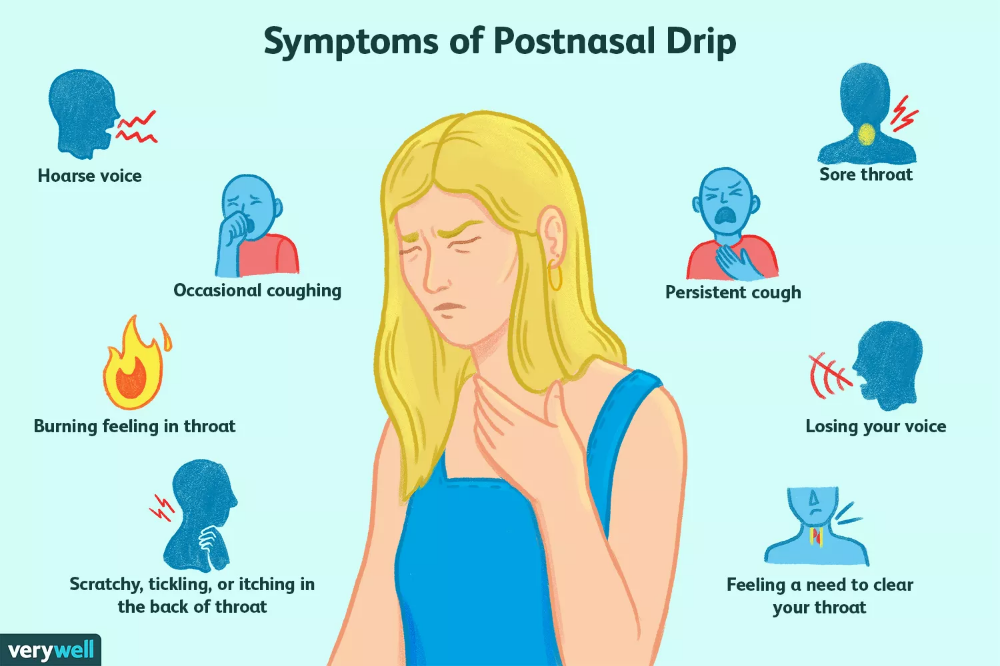
Your body will change in interesting ways during pregnancy. If you have new or unusual symptoms, call your doctor. We'll help you sort out what's normal from what could be a sinus infection or respiratory illness.
To talk with a doctor about nasal symptoms during pregnancy, call 214-645-8300 or request an appointment online.
More in: Your Pregnancy Matters
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
December 20, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
December 13, 2022
Pediatrics; Your Pregnancy Matters
- Jessica Morse, M.D.
December 6, 2022
Your Pregnancy Matters
- Shivani Patel, M.
 D.
D.
November 22, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 15, 2022
Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
November 7, 2022
Mental Health; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.
 D.
D.
October 11, 2022
Prevention; Your Pregnancy Matters
- Robyn Horsager-Boehrer, M.D.
October 4, 2022
Mental Health; Your Pregnancy Matters
- Meitra Doty, M.
 D.
D.
September 27, 2022
More Articles
Drug-induced vasomotor rhinitis when planning a pregnancy
01/06/2023
Dependence on vasoconstrictor drops is a serious disease, especially if you are planning a pregnancy. The condition in which addiction develops to the use of vasoconstrictor drugs in the nose is called medicamentous rhinitis.
Today, the pharmaceutical market is replete with a variety of vasoconstrictor drugs. They are available to any buyer, as they do not require a prescription. However, not everyone knows that the use of such drugs has a strictly limited period of use. Namely, no more than 7-10 days. Self-medication and misuse of such drugs lead to the development of drug-induced rhinitis. nine0003
What to do if addiction has already developed, life without drops from the common cold is no longer possible, and you decide to become a mother?
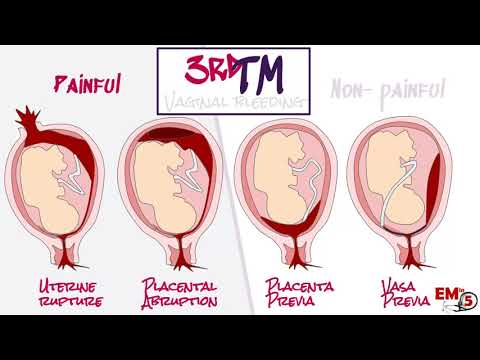
During pregnancy, the use of vasoconstrictor drugs is highly undesirable, as they have an adverse effect on the fetus. Vasoconstrictor drops have not only local, but also systemic effects. As a result, there is a chronic vasospasm of the forming placenta, which in the early stages can lead to spontaneous miscarriage. At a later date - to primary placental insufficiency, which is a formidable obstetric pathology leading to a syndrome of fetal growth retardation and intrauterine hypoxia. nine0003
Vasoconstrictor drops have not only local, but also systemic effects. As a result, there is a chronic vasospasm of the forming placenta, which in the early stages can lead to spontaneous miscarriage. At a later date - to primary placental insufficiency, which is a formidable obstetric pathology leading to a syndrome of fetal growth retardation and intrauterine hypoxia. nine0003
Therefore, if you have already developed drug-induced rhinitis, we strongly recommend that you consult an ENT doctor before planning a pregnancy. It will help you choose the correct treatment regimen and completely abandon the drops. After complex treatment and recovery, at least in a month, you will be able to plan a pregnancy.
Treatment of drug-induced rhinitis
For the treatment of drug-induced rhinitis of the ENT, the doctor prescribes complex conservative treatment, appropriate medications and, of course, the rejection of vasoconstrictor drops. If conservative methods do not help, the doctor prescribes surgery.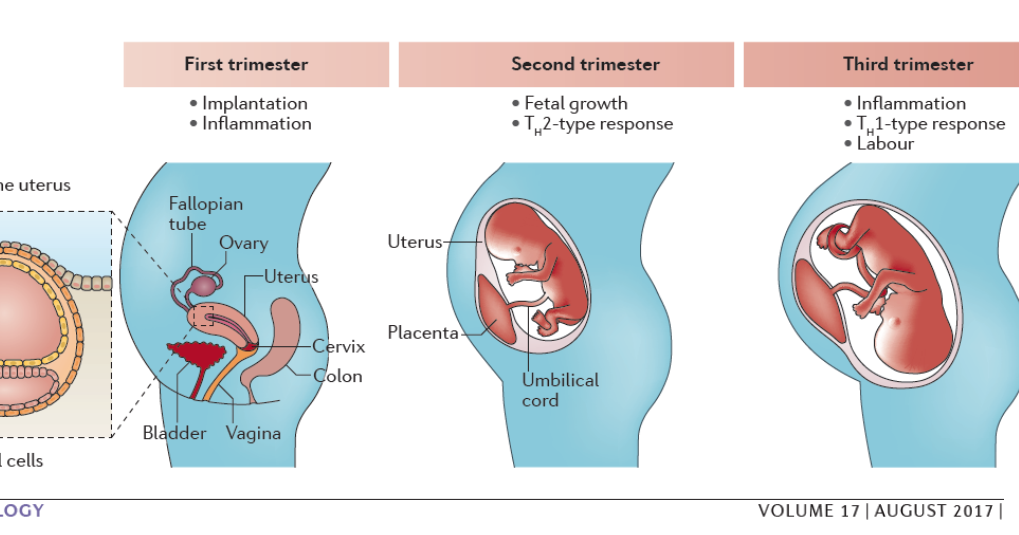 The most modern method is radiofrequency disintegration of the inferior turbinates. nine0003
The most modern method is radiofrequency disintegration of the inferior turbinates. nine0003
What if the dependence on the drops returns during pregnancy?
During pregnancy, many women experience swelling of the nasal mucosa and "rhinitis of pregnancy" occurs. This is a temporary phenomenon and has nothing to do with drug-induced rhinitis in the past. Since rhinitis of pregnancy is an exclusively physiological condition, the appointment of special preparations for the nose is not required. Independent attempts to facilitate breathing in this case are excluded.
For the treatment of drug-induced rhinitis, you can contact our clinic - our experienced ENT doctor will prescribe an effective treatment for you and help you get rid of the dependence on the use of vasoconstrictor drops. The clinic "Osnova" employs highly qualified specialists, including candidates of sciences, with extensive practical experience in the treatment of all forms of rhinitis. nine0003
Read us on Yandex Zen
Pregnancy rhinitis
Otorhinolaryngologist, surgeon at GMS Clinic Oleg Abramov talks in his article about rhinitis of pregnancy (hereinafter referred to as RH).
It was no coincidence that I chose this topic after a series of publications on the social network about allergic rhinitis (hereinafter referred to as AR), as recent studies note that although the cause of RB is not completely clear, the combination of AR, which is especially poorly controlled together with RB, can lead to severe nasal congestion, to insufficient oxygen supply, and, as a result, to increased fatigue, irritability, frequent SARS, sleep disturbance, which can certainly affect the development of the fetus. Moreover, the presence of AR is associated with snoring in women during pregnancy, and together they can provoke the development of sleep apnea syndrome (stopping breathing during sleep), which leads to arterial hypertension, preeclampsia, slowed fetal growth and low Apgar scores. Therefore, the relevance of this problem is only growing. nine0003
Definition and concept
Rhinitis of pregnancy is a disease accompanied by nasal congestion and discharge, periodic sneezing without signs of inflammation, allergies, or other causes.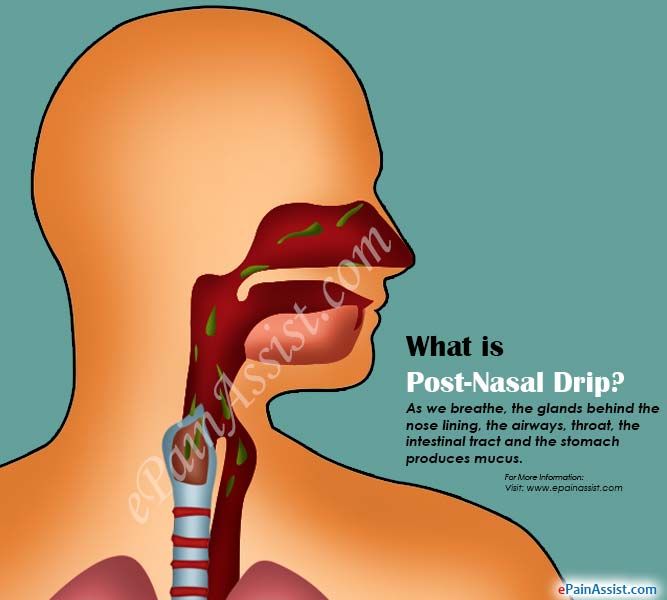 This condition can occur in any trimester of pregnancy and usually resolves within two weeks after delivery.
This condition can occur in any trimester of pregnancy and usually resolves within two weeks after delivery.
Occurrence
Nasal congestion is a very common problem during pregnancy (occurs in about 65% of cases), which can occur due to various reasons. RB, according to various sources, occurs in 9-40% of cases, and in one of the last observations there is an increasing incidence, that is, most of all RB is observed in the 3rd trimester - 38.9%, including those who did not have problems in the 1st and 2nd trimesters.
Causes and mechanism of occurrence
The mechanism of occurrence is not fully understood, and it is believed that RB occurs due to hormonal changes, in particular, under the influence of progesterone, estrogen, hCG and other hormones, the concentration of which gradually increases during pregnancy. Some authors believe that the occurrence of RB is associated with the worsening of concomitant AR. Some studies show that hormonal action leads to relaxation of the smooth muscles that make up the vessel wall of the nasal mucosa, resulting in nasal congestion. Such findings are supported by other studies that show that oral contraceptives cause similar effects in the nasal cavity (but not in everyone). Other studies show that elevated body mass index, overweight, multiple pregnancies provoke or aggravate RB. nine0003
Such findings are supported by other studies that show that oral contraceptives cause similar effects in the nasal cavity (but not in everyone). Other studies show that elevated body mass index, overweight, multiple pregnancies provoke or aggravate RB. nine0003
Progression and potential risks
RB, in the absence of adequate treatment, has an adverse effect on the course of pregnancy and can lead to the development of rhinosinusitis, which is especially difficult to tolerate in the 3rd trimester. On the other hand, pregnancy is a special period in a woman's life, during which a large number of drugs are prohibited, and ENT pathologies, these restrictions have not been spared either. Very often I hear at the reception: "Doctor, I'm pregnant and I've been suffering with my nose all this time, but the doctors tell me - there's nothing to be done, I need to endure it." On the other hand, the opposite situation is often observed: “Doctor, I am pregnant and I cannot live without vasoconstrictor drops. ” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all. nine0003
” These situations, of course, are not correct, since on the one hand there is a way out and optimal treatment, and on the other hand, constant exposure to vasoconstrictor drugs is not a way out of the situation at all. nine0003
Diagnostics
At the moment, there is no specific test to confirm or exclude RB. The diagnosis is made on the basis of the patient's complaints and the exclusion of other pathologies of the nasal cavity.
Choice of therapeutic tactics
Saline solutions
Before considering more serious medications, we should start with our favorite saline solutions. It should be noted that we are not talking about ordinary saline solutions, but hypertonic saline solutions (with an increased salt content, approximately 19-23 g/l). Such sprays are sold in all pharmacies, but they will not be sold to you right away (you need to ask). Several studies have noted significant efficacy in reducing congestion when used in AR, chronic rhinosinusitis.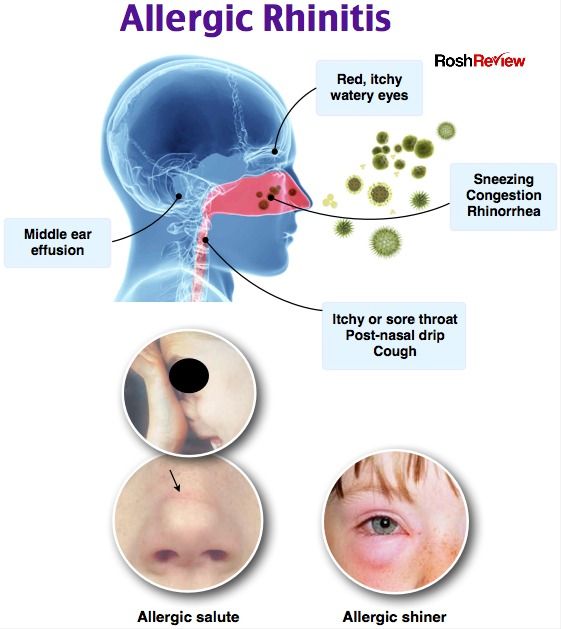 Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
Also, comparative studies show their greater effectiveness compared to conventional isotonic solutions. Examples: Physiomer - hypertonic solution (my favorite), Aqualor-congestion, or Aqualor-severe runny nose, Aquamaris Strong.
As is known from past publications, intranasal glucocorticosteroids (iGCS) are the most effective in the treatment of AR today. They have proven efficacy in reducing nasal congestion, as well as nasal itching and watery eyes, and allow adequate control of symptoms. But, given their hormonal effect and possible harmful effects on the fetus, there are certain risks in their use. It should also be noted that at the moment there are no studies that provide reliable data confirming the danger of their use. Modern ICS — mometasone (nasonex, desrinit) and fluticasone (avamys, flixonase) has a very low systemic bioavailability, less than 1% and proven efficacy, thus can be considered as initial therapy for RB. The studies did not reveal a statistically significant relationship between the development of fetal defects and the use of these drugs. nine0003
nine0003
Who are the US FDA and why is everyone listening to them?
Everything is very simple (it’s a pity that everything is not so simple with us). I copy the explanation from Wikipedia: “An agency of the US Department of Health and Human Services, one of the federal executive departments. The department is engaged in quality control of food products, medicines, cosmetics, tobacco products and some other categories of goods, and also monitors compliance with legislation and standards in this area. nine0003
Budesonide (Tafen Nasal) is classified as category B according to the FDA's classification for drug effects on the fetus, which means that there is evidence that the drug is safe to use during pregnancy. The bioavailability of budesonide is 33%. This drug has moved from group C to group B, thanks to several high-quality studies in Sweden since the beginning of the 21st century, proving its safety.
Also, according to the current recommendations of the American Academy of Allergology and Immunology (AAAAI), ICS are considered safe and effective in the treatment of rhinitis and rhinosinusitis during pregnancy.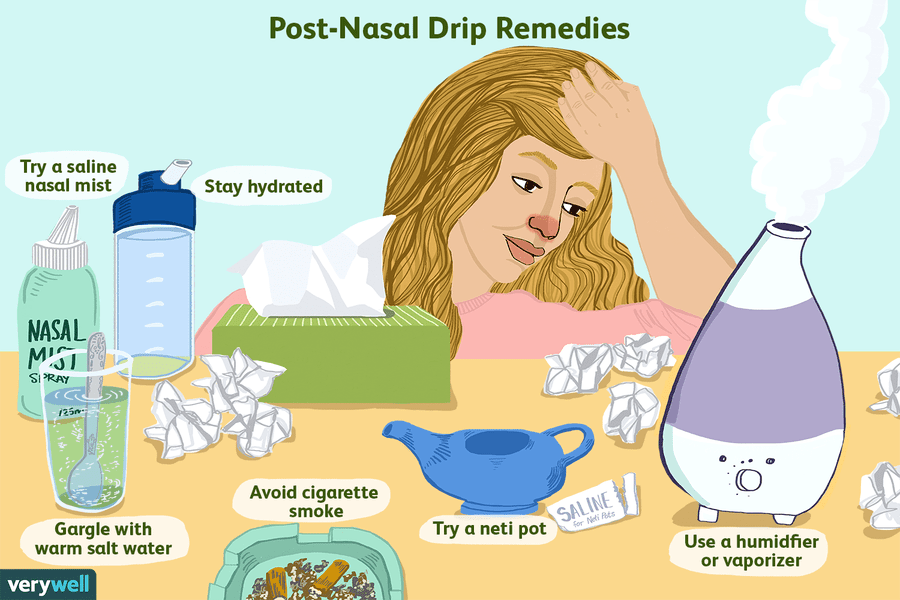 But at the same time, there is no indication of specific drugs. Other competent medical associations also do not give any recommendations in terms of choosing a drug. Therefore, summing up all of the above, and also according to the latest review, mometasone, fluticasone, budesonide can be considered as safe and effective agents in the treatment of RB. It should also be noted that an experienced ENT doctor should be involved in prescribing the drug and managing the patient, since these drugs are sold without a prescription in the Russian Federation; we strongly recommend not to self-medicate. nine0003
But at the same time, there is no indication of specific drugs. Other competent medical associations also do not give any recommendations in terms of choosing a drug. Therefore, summing up all of the above, and also according to the latest review, mometasone, fluticasone, budesonide can be considered as safe and effective agents in the treatment of RB. It should also be noted that an experienced ENT doctor should be involved in prescribing the drug and managing the patient, since these drugs are sold without a prescription in the Russian Federation; we strongly recommend not to self-medicate. nine0003
Yes, I will not take these hormones!
In some situations, acute respiratory viral infections during pregnancy may be accompanied (largely due to concomitant RB or AR, or their combination) with a prolonged runny nose, nasal congestion and heaviness in the face - classic symptoms of rhinosinusitis. This disease, if not adequately treated, can lead to serious complications, so the correct diagnosis of this disease is extremely important.