How to get rid of breast engorgement
Breast Engorgement: Causes, Complications & Treatment
Overview
What is breast engorgement?
Breast engorgement is when your breasts are painful, swollen and tender because they’re overly full of milk. It occurs most often in the days and weeks after giving birth due to milk production and increased blood supply to your breasts (chest). The increase in blood supply helps your body make breast milk for your baby, but it can cause severe engorgement. Engorged breasts are a temporary problem but can happen as long as you produce milk.
The most common reasons for breast engorgement are:
- You’ve given birth and your milk is “coming in.”
- You’re breastfeeding (chestfeeding) and skip nursing sessions.
- Your baby changes their feeding schedule. For example, they start sleeping through the night.
- You skip pumping sessions or forget to pump when you’re away from your baby.
- You have an oversupply or make more milk than your baby needs.
- You’re weaning your child from breastmilk to another form of milk.
It can be tricky to balance managing your milk supply and preventing engorgement. However, there are ways you can relieve the discomfort and minimize complications from engorged breasts.
When do you start making breastmilk?
The first milk your breasts produce is called colostrum. It’s a highly nutritious first milk that your body begins making in pregnancy. Colostrum transitions to breast milk after three to five days. Engorgement tends to occur during this time because your milk production is ramping up. Your breasts will be fuller, firmer, swollen and tender to the touch. After several days, the pain and discomfort should gradually subside.
When does engorgement start?
The exact timing varies, but the most common time is between three and five days after you give birth. It may start later if you’ve had a cesarean birth (C-section). The degree of swelling and pain you feel can also vary. Some people are severely engorged, while others feel minor side effects of breast engorgement.
Some people are severely engorged, while others feel minor side effects of breast engorgement.
How long does it take for engorgement to go away?
There’s no set time for engorgement to subside. The engorgement you feel after giving birth is usually the most severe. Most people stop feeling engorged within 10 days; however, feeling “full” can last several weeks. Breast engorgement can come back as long as you breastfeed, chestfeed or pump breast milk.
Possible Causes
What causes breast engorgement?
Your breasts become engorged anytime they’re overly full of milk. It happens the first time within a few days of giving birth and can last several weeks. You can get engorged breasts for as long as you’re making milk.
Reasons your breasts may become overly full are:
- Your milk is transitioning from colostrum to mature breast milk.
- You miss or skip feedings or pumping sessions.
- Your baby sleeps through the night or starts eating solid food.
- You supplement feedings with formula.
- Your baby doesn’t eat as much due to illness.
- Your baby isn’t latching correctly and fully emptying the breast.
What are symptoms of breast engorgement?
No two people will have the same symptoms. People describe their engorged breasts as being:
- Fuller and larger than usual (up to a few cup sizes).
- Swollen.
- Painful.
- Hard and firm.
- Tender and sensitive to touch.
- Lopsided or rocky (hard lumps).
The swelling can also extend up into your armpit and across to your sternum (breast bone). This is because breast tissue extends to these areas. Your nipples may change from being soft and flexible to flat and firm.
Some people also experience a low fever (called milk fever) when they’re engorged. This is typically OK. Call your healthcare provider if your fever increases or lasts several days as it could be a sign of infection.
What does breast engorgement feel like?
Engorged breasts feel like they’re ready to burst.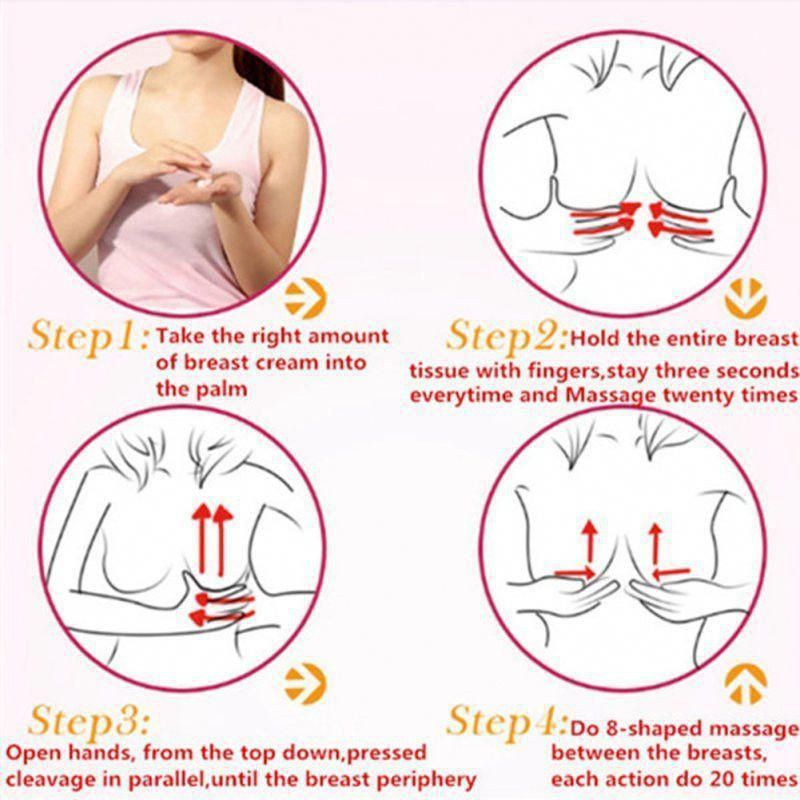 They may feel hard like rocks and so tender that it hurts to walk or change your clothes. Your breasts will feel heavier, and simple things like snuggling your baby may be extremely painful.
They may feel hard like rocks and so tender that it hurts to walk or change your clothes. Your breasts will feel heavier, and simple things like snuggling your baby may be extremely painful.
What do engorged breasts look like?
Engorged breasts look several sizes bigger than their normal size. Most people will see their veins protruding visibly under the skin of their breasts. The skin of your breasts may appear shiny from being stretched. Your breasts will likely have an uneven shape, and you may see visible lumps or hard spots.
Care and Treatment
How do you relieve breast engorgement?
Most people can relieve breast engorgement at home within a few days. Some common treatments for engorged breasts are:
- Using a warm compress or taking a hot shower before feedings to soften your breasts and encourage milk flow.
- Massaging your breasts while nursing or pumping.
- Hand expressing or pumping a small amount of milk between feedings to relieve pressure.
- Applying a cold compress or ice pack to your breasts between feedings to help with swelling.
- Taking ibuprofen or acetaminophen for pain.
- Feeding your baby or expressing milk every two to three hours.
- Letting your baby completely drain your breasts.
Should I pump to relieve engorgement?
Yes, you can pump a little bit of milk to relieve engorgement. Try to pump just enough to feel relief —around 1 to 2 ounces. Remember, producing milk is a supply and demand process. If you pump too much milk, your body will just produce more to make up for it.
How do I stop getting engorged at night?
It’s normal for your breasts to become engorged once your baby starts sleeping longer at night. It may take your milk supply a few days to adapt to your baby’s new pattern. If your breasts are overly filled, it’s OK to remove some milk. You should only remove a little milk – enough to provide some relief so you can get back to sleep.
This can happen anytime your baby goes longer without feedings. If you experience pain or fullness because your baby is going longer stretches between meals, pumping or hand-expressing a little bit of milk is fine.
If you experience pain or fullness because your baby is going longer stretches between meals, pumping or hand-expressing a little bit of milk is fine.
What do I do for engorgement if I don’t want to breastfeed or chestfeed?
You’ll have engorged breasts even if you choose not to breastfeed or chestfeed. However, milk production will eventually stop. Your body will recognize that you don’t need milk, and your supply will dry up. Don’t pump for relief. This will only prolong the process of ending your milk production. Instead, try some of the following treatments until your pain subsides:
- Take an over-the-counter (OTC) pain reliever for pain and swelling.
- Wear a tight-fitting and supportive bra.
- Apply cold compresses to your breasts several times a day.
When to Call the Doctor
What can happen if my breasts get too engorged?
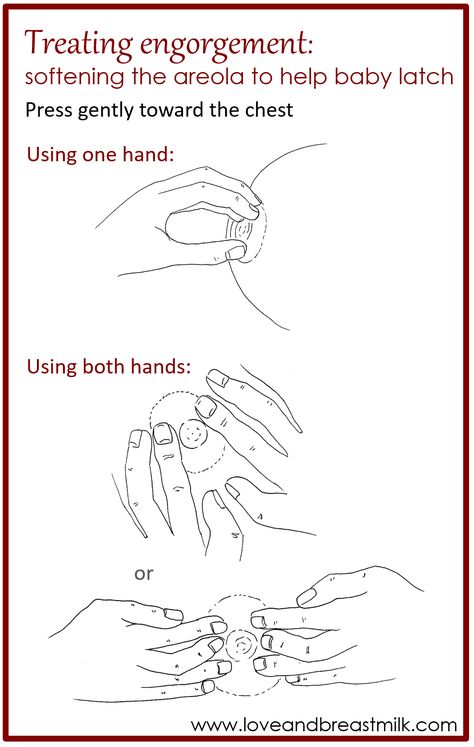
Engorged breasts can make it hard for your baby to feed. Relieving engorgement and softening your breasts and nipples can help with your baby’s latch (the way your baby attaches to your nipple).
Some of the most common feeding issues caused by engorged breasts are:
- Your baby can’t latch to your nipple because it’s too flat and stretched.
- Your nipples become sore and cracked because your baby isn’t latching correctly.
- You feed your baby less because it’s too painful. This can lower your milk supply.
- Overactive let-down or fast milk flow. This can lead to your baby gagging or choking on milk.
- Your baby is unable to empty your breast fully. This can cause clogged milk ducts.
Breast engorgement can also lead to complications like clogged milk ducts and mastitis.
What’s a clogged milk duct?
Milk ducts are a part of breast anatomy that carry milk to the nipples. When one of these ducts gets clogged with milk, you may feel a lump in your breast. Removing the clog as soon as possible can prevent it from becoming infected. To unclog a milk duct, apply heat to the area and gently massage the lump toward your nipple while nursing or pumping.
What’s mastitis?
Mastitis is an infection in your breast tissue. It happens when milk gets trapped in the breast. Bacteria grow in the trapped milk, leading to infection. Your healthcare provider will treat mastitis with antibiotics. You will also be encouraged to gently massage your breast, nurse or pump, and use medication to bring down any fever you may have.
When do I call my doctor?
Contact your healthcare provider, pediatrician or lactation consultant if:
- Your breasts are engorged longer than a few weeks.
- You develop symptoms of mastitis. Signs include a red spot on your breast, a fever, a painful spot on your breast or chills.
- Your baby has a poor latch or issues with breastfeeding/chesfeeding.
- You think you have low milk supply or your baby isn’t eating enough.
Don’t be ashamed to ask for help. Struggling with breastfeeding, chestfeeding or feeding your baby pumped milk is a common struggle. Healthcare providers can help you.
Frequently Asked Questions
Can you prevent breast engorgement?
No, you can’t prevent breast engorgement. It’s a natural part of childbirth. However, you can manage your symptoms so you’re more comfortable. Remember, it will subside once your milk supply is under control. When your milk comes in and your supply is regulated, you can prevent future breast engorgement by:
- Not skipping feeding or pumping sessions.
- Making sure your baby maintains a good latch on your breast.
- Weaning your baby from breast milk slowly.
- Emptying your breasts at each feeding.
A note from Cleveland Clinic
Engorged breasts are hard, swollen and extremely painful. Some engorgement is unavoidable – like when your milk comes in after giving birth. It’s good to learn how to manage breast engorgement and treat it quickly. Remember, engorged breasts are only temporary, and you can take steps to ease the discomfort by removing some milk, softening your breasts before nursing or using ice packs. Call your healthcare provider if your engorgement lasts longer than a few weeks or if you develop signs of mastitis.
Call your healthcare provider if your engorgement lasts longer than a few weeks or if you develop signs of mastitis.
Causes and Tips for Relief
What is breast engorgement?
Breast engorgement is breast swelling that results in painful, tender breasts. It’s caused by an increase in blood flow and milk supply in your breasts, and it occurs in the first days after childbirth.
If you’ve decided not to breastfeed, you may still experience breast engorgement. It can happen in the first few days after delivery. Your body will make milk, but if you don’t express it or nurse, the milk production will eventually stop.
Breast engorgement is the result of increased blood flow in your breasts in the days after the delivery of a baby. The increased blood flow helps your breasts make ample milk, but it can also cause pain and discomfort.
Milk production may not occur until three to five days postpartum. Engorgement may occur for the first time in the first week or two after delivery. It can also reoccur at any point if you continue to breastfeed.
It can also reoccur at any point if you continue to breastfeed.
Not producing enough milk? Here are 5 tips to increase breast milk production.
Certain conditions or events may make you more likely to experience the swollen fullness that’s commonly associated with breast engorgement. These causes include:
- missing a feeding
- skipping a pumping session
- creating an overabundance of milk for the baby’s appetite
- supplementing with formula between nursing sessions, which may reduce nursing later
- weaning too quickly
- nursing a baby that’s ill
- difficulty with latching and sucking
- not expressing breast milk when it first comes in because you don’t plan to breastfeed
The symptoms of breast engorgement will be different for each person. However, breasts that are engorged may feel:
- hard or tight
- tender or warm to touch
- heavy or full
- lumpy
- swollen
The swelling may be contained to one breast, or it may occur in both. Swelling can also extend up the breast and into the nearby armpit.
Swelling can also extend up the breast and into the nearby armpit.
The veins running under the breast’s skin may become more noticeable. This is a result of the increased blood flow, as well as the tightness of the skin over the veins.
Some with breast engorgement may experience a low-grade fever and fatigue in the first days of milk production. This is sometimes called a “milk fever.” You can continue to nurse if you have this fever.
However, it’s a good idea to alert your doctor to your increased temperature. That’s because some infections in the breast can cause fever, too, and these infections need to be treated before they become bigger issues.
Mastitis, for example, is an infection that causes inflammation of the breast tissue. It’s most commonly caused by milk trapped in the breast. Untreated mastitis can lead to complications such as a collection of pus in the clogged milk ducts.
Report your fever and any other symptoms you’ve recently experience to your doctor.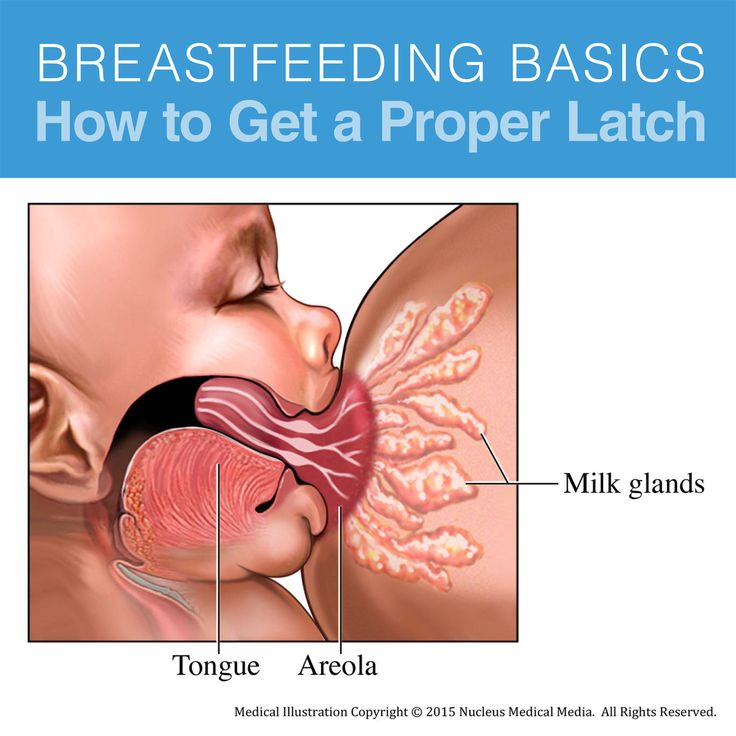 They will want you to monitor for signs of an illness or infection so you can seek immediate treatment.
They will want you to monitor for signs of an illness or infection so you can seek immediate treatment.
The treatments for breast engorgement will depend on whether you’re breastfeeding or not.
For those who are breastfeeding, treatments for breast engorgement include:
- using a warm compress, or taking a warm shower to encourage milk let down
- feeding more regularly, or at least every one to three hours
- nursing for as long as the baby is hungry
- massaging your breasts while nursing
- applying a cold compress or ice pack to relieve pain and swelling
- alternating feeding positions to drain milk from all areas of the breast
- alternating breasts at feedings so your baby empties your supply
- hand expressing or using a pump when you can’t nurse
- taking doctor-approved pain medication
For those who don’t breastfeed, painful engorgement typically lasts about one day. After that period, your breasts may still feel full and heavy, but the discomfort and pain should subside. You can wait out this period, or you can use one of the following treatments:
You can wait out this period, or you can use one of the following treatments:
- using a cold compress or ice packs to ease swelling and inflammation
- taking pain medication approved by your doctor
- wearing a supportive bra that prevents your breasts from moving significantly
You can’t prevent breast engorgement in the first days after giving birth. Until your body knows how to regulate your milk production, you may overproduce.
However, you can prevent later episodes of breast engorgement with these tips and techniques:
- Feed or pump regularly. Your body makes milk regularly, regardless of nursing schedule. Nurse your baby at least every one to three hours. Pump if your baby isn’t hungry or you’re away.
- Use ice packs to decrease supply. In addition to cooling and calming inflamed breast tissue, ice packs and cold compresses may help decrease milk supply. That’s because the cool packs turn off the “let down” signal in your breasts that tells your body to make more milk.

- Remove small amounts of breast milk. If you need to relieve the pressure, you can hand express some breast milk or pump a bit. Don’t pump or express too much, however. It could backfire on you, and your body may end up trying to produce more milk to make up for what you just removed.
- Wean slowly. If you’re too quick to stop nursing, your weaning plan may backfire. You could end up with too much milk. Slowly wean your child so your body can adjust to the decreased need.
If you don’t breastfeed, you can wait out breast milk production. In a matter of days, your body will understand it doesn’t need to produce milk and the supply will dry up. This will stop the engorgement.
Don’t be tempted to express or pump milk. You’ll signal to your body that it needs to produce milk, and you may prolong discomfort.
Breast engorgement is swelling and inflammation that occurs in your breasts because of increased blood flow and milk supply. In the days and weeks after giving birth, your body will begin to produce milk.
In the days and weeks after giving birth, your body will begin to produce milk.
Until your body knows how much you need, it may produce too much. This can lead to breast engorgement. Symptoms include hard, tight breasts that are swollen and tender. Regular nursing or pumping can help prevent breast engorgement.
If you continue to experience the painful swelling of breast engorgement, reach out to a lactation consultant or a lactation support group at your local hospital. Both of these resources can help you with your questions and provide support.
Also, call your doctor if the engorgement doesn’t subside in three to four days or if you develop a fever. They’ll ask you to monitor for other signs that may indicate a more serious problem, such as a breast infection.
Breast engorgement symptoms and first aid
search support iconSearch Keywords
Home ›› How to relieve the unpleasant symptoms of breast engorgement
Home ›› How to relieve the unpleasant symptoms of breast engorgement
↑ 0 Top Let's look at all the important issues, including prevention, symptoms, and help with engorgement. Breast engorgement occurs for various reasons. The most common: - Skipping a feeding or pumping session. - Making more milk than the baby eats. nine0003 - Insufficient outflow of milk (improper latching on to the breast by the baby). - Inflammation. Although engorgement and mastitis may appear similar, they are actually completely different conditions. 3. Make sure the baby is latching on correctly. To learn how to properly breastfeed a baby, a mother can seek advice from a breastfeeding specialist. Proper gripping of the breast during feeding is important for complete emptying of the breast. It also helps prevent other problems such as sore, irritated or cracked nipples. 4. Wean the baby gradually. Philips Avent 2-in-1 thermal pads can both warm and cool your breasts to both stimulate and soothe your breasts after feeding. Mom only needs to place them in a bra for 15-30 minutes before or after feeding (depending on the desired result).
One of the most common breastfeeding problems faced by mothers is breast engorgement. While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it. nine0003
While occasional engorgement while breastfeeding is normal, it can be uncomfortable and lead to other problems if not addressed and dealt with. It is important for mothers to understand what breast engorgement is and how to alleviate it. nine0003
What is breast engorgement?
Engorgement is an increase in the size of the mammary glands, in which the breast becomes painful and sensitive. This condition is associated with increased blood flow and increased milk production, so it very often occurs during the first few days after childbirth. In addition, engorgement may develop within one to two weeks after childbirth or at any time during breastfeeding. Although this is quite normal during breastfeeding, it can be uncomfortable and sometimes lead to other complications. Therefore, the main thing is to deal with engorgement of the mammary glands immediately when it occurs. nine0003
nine0003
How long does engorgement last?
All women are different, and, accordingly, the duration of this condition may vary. Some experience mild symptoms for only one day, while others may experience this condition for up to two weeks.
Breast engorgement symptoms
Breast engorgement symptoms vary, but the most common are:
 How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement. nine0003
How can a mother determine what exactly she has: engorgement or mastitis? Mastitis is an inflammation of the breast that typically results in fever (>38.5°C) and reddening of the breast, while engorgement is the result of excessive milk production and incomplete emptying of the breast. Engorgement can lead to problems such as blockage of the milk ducts or infection of the mammary glands, so it is important to start treating engorgement at the first sign of engorgement. nine0003
Prevention of engorgement
There are several ways to prevent this condition. Prevention of breast engorgement in the first days after childbirth can be difficult as the mother's body adapts to the changes. But you can try to avoid it as follows:
 nine0061
nine0061
Electronic breast pump will help you to comfortably and efficiently express the right amount of milk between feedings, if necessary, or instead of feeding when the mother is away from the baby. nine0061  When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement. nine0003
When it's time to stop breastfeeding, moms shouldn't do it abruptly. It is best to wean the baby gradually, gradually reducing the number of daily feedings. This will gradually slow down milk production and prevent breast engorgement. nine0003
Helping with breast engorgement
Breastfeeding with engorgement is not only safe, but necessary to prevent symptoms from getting worse and provide relief. While the body is learning how to produce the right amount of milk, moms can use the Philips Avent bra pads to absorb excess milk and prevent stains on clothes all day long. Philips Avent
Philips Avent
Multifunction thermal pads
SCF258/02
Overall rating / 5
- review review reviews Reviews
-
-{discount-value}
- Pictures It is important to achieve optimal outflow of milk during feedings.
 To stimulate the outflow of milk, during feeding, you can gently massage the breast.
To stimulate the outflow of milk, during feeding, you can gently massage the breast. - Express milk. There are situations when a nursing mother cannot be with the baby during feeding. It is important to empty your breasts by expressing milk to prevent engorgement and other problems. nine0061
- When feeding, change positions and alternate breasts. Changing your position while breastfeeding can be beneficial, as it improves the outflow of milk from different parts of the mammary glands. In addition, mothers can change their breasts during one feeding so that the baby can empty both of them.
Remember that minor pain and discomfort is completely natural during breastfeeding, but if these symptoms persist or worsen, the mother should consult a doctor. nine0003
Philips Avent Articles & Tips
Baby+ App
Download the app and track your baby's development and growth with trackers and keep those special moments forever.
Download app:
Pregnancy+ app
Download one of the world's best pregnancy tracking apps for weekly helpful information, articles and tips about pregnancy and baby development. nine0003
nine0003
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Treatment of breast engorgement (full, hard, painful breasts) in breastfeeding women
This translation is out of date. Please click here for the latest English version of this review.
Survey question
What is the best treatment for breast engorgement in breastfeeding women?
Relevance
Breast engorgement is the overflowing of milk, resulting in swelling, hardness and tenderness of the mammary glands. Many women experience this in the first days after giving birth, although it can also happen later. It most often occurs when feeding times are limited, or the baby has difficulty suckling, or the mother is separated from her newborn. This leads to the fact that the mammary glands are not completely emptied. Breast engorgement can make it difficult for women to breastfeed. This can lead to complications such as breast inflammation, infection, and ulcerated or cracked nipples. There is still a lack of solid evidence for effective forms of treatment. nine0003
Many women experience this in the first days after giving birth, although it can also happen later. It most often occurs when feeding times are limited, or the baby has difficulty suckling, or the mother is separated from her newborn. This leads to the fact that the mammary glands are not completely emptied. Breast engorgement can make it difficult for women to breastfeed. This can lead to complications such as breast inflammation, infection, and ulcerated or cracked nipples. There is still a lack of solid evidence for effective forms of treatment. nine0003
Study profile
We searched for trials evaluating any treatment for breast engorgement in breastfeeding women. We found 13 trials including 919 lactating women with breast engorgement. These trials looked at treatment options including acupuncture, acupressure, cabbage leaves, cold compresses, medication, massage, and ultrasound. Four studies were sponsored by organizations with a commercial interest in the results, two received philanthropic funding, and two were supported by government organizations. The remaining five did not name the source of funding. nine0003
The remaining five did not name the source of funding. nine0003
Results
One study comparing acupuncture with conventional care (advice and oxytocin spray) found no difference in stopping breastfeeding. However, women in the acupuncture group were less likely to develop an abscess, have less severe symptoms by day five, and have a lower incidence of fever compared to women in the conventional care group. Three trials looking at cabbage leaves showed no difference between room temperature and chilled cabbage leaves, between chilled cabbage leaves and gel packs, and between cabbage cream and inactive cream; however, all treatments provided some relief. Hot/cold compresses were found to be more effective than acupressure. nine0244 Gua Sha scraping therapy was found to be more effective than hot compresses and massage in reducing the symptoms of breast engorgement, although both forms of treatment reduced breast temperature, engorgement, pain and discomfort at five and 30 minutes after treatment. A study of ultrasound therapy showed the same minimal effect as sham ultrasound, while injections of oxytocin in another study did not bring relief at all. When the breast-shaped cold gel packs were compared to conventional care, women using the packs seemed to experience less pain; however, the study was of very low quality and the results are unreliable. nine0003
A study of ultrasound therapy showed the same minimal effect as sham ultrasound, while injections of oxytocin in another study did not bring relief at all. When the breast-shaped cold gel packs were compared to conventional care, women using the packs seemed to experience less pain; however, the study was of very low quality and the results are unreliable. nine0003
Quality of evidence
The quality of the evidence was low due to the small number of participants in the included studies and the limited number of studies looking at the same outcomes. More reliable research on the treatment of breast engorgement is urgently needed.
Translation notes:
Translation: Ekaterina Zmievskaya. Editing: Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: cochrane.