Post miscarriage bleeding
Treating miscarriage | The Royal Women's Hospital
If a miscarriage has begun, there is nothing that can be done to stop it. Any treatment you have will be aimed at avoiding heavy bleeding and infection.
A discussion with the doctor or nurse will help you to work out which treatment options are best and safest for you.
On this page:
- No treatment (expectant management)
- Treatment with medicine
- Surgical treatment (curette)
- Waiting for treatment
- After a miscarriage
No treatment (expectant management)
You can choose to wait and see what will happen. This is called 'expectant management'. If nothing is done, sooner or later the pregnancy tissue will pass naturally. If it is an incomplete miscarriage (where some but not all pregnancy tissue has passed) it will often happen within days, but for a missed miscarriage (where the fetus or embryo has stopped growing but no tissue has passed) it might take as long as three to four weeks.
While you are waiting you may have some spotting or bleeding, much like a period. When the pregnancy tissue passes, you are likely to have heavier bleeding with crampy, period-like pains. You can use sanitary pads and take pain relieving tablets, such as paracetamol.
If your miscarriage is incomplete, with just a small amount of pregnancy tissue remaining, it’s probably best to take a wait and see approach. But if there is heavy bleeding or signs of infection you will need treatment.
If the tissue does not pass naturally or you have signs of infection, the doctor will recommend a dilatation and curettage (D&C). You and the doctor can discuss and decide the preferred option for you.
Things to know
- There are many reasons why some women prefer to wait and see. It may feel more natural, it may help with the grieving process or it may give you more of a sense of control.
- Some women become worried or frightened when the bleeding gets heavier, especially if blood clots, tissue or even a recognisable embryo is passed.
- Usually, the wait and see approach takes longer than any other approaches such as surgery or medication. Sometimes bleeding can last for up to four weeks.
- Although excessive bleeding and blood transfusion are very rare, they are slightly more common with expectant management than with surgery.
- A few women still need to have surgery – sometimes urgently – if they develop infection, bleed heavily or if the tissue does not pass naturally.
- The waiting time can be emotionally draining for some women.
Treatment with medicine
Medicine is available that can speed up the process of passing the pregnancy tissue. For an incomplete miscarriage, the medicine will usually encourage the pregnancy tissue to pass within a few hours. At most it will happen within a day or two. For a missed miscarriage, it may happen quickly, but it can take up to two weeks and, occasionally, longer.
- Medication is not suitable if there is very heavy bleeding or signs of infection.
 It is usually not recommended for pregnancies that are older than about nine weeks.
It is usually not recommended for pregnancies that are older than about nine weeks. - If the tissue does not pass naturally, eventually your doctor will recommend a dilatation and curettage (D&C).
Things to know
- The pregnancy tissue will pass between four to six hours after taking the medicine, during which time you may be in hospital. After a few hours, if the pregnancy hasn’t passed, you may be sent home to wait. This will depend on where you are and which hospital you are in.
- The medicine has side effects which usually pass in a few hours but can be unpleasant, such as nausea, vomiting, diarrhoea, fever and chills. The tablets can be swallowed or dissolved under the tongue, or inserted in the vagina.
- After receiving the medication there may be some spotting or bleeding like a period. When the pregnancy tissue passes, you are likely to notice heavier bleeding and clots with strong cramping, period-like pains. You can use sanitary pads and take pain relieving tablets such as paracetamol.

- Some women may need stronger pain killers or a pain relieving injection.
- A few women still need to have surgery, sometimes urgently, if they develop infection, bleed heavily or if the tissue does not pass.
Surgical treatment (curette)
A D&C (or ‘curette’) is a minor operation. The full name is dilatation and curettage. It is done in an operating theatre, usually under general anaesthetic. There is no cutting involved because the surgery happens through the vagina. The cervix (neck of the uterus) is gently opened and the remaining pregnancy tissue is removed so that the uterus is empty. Usually the doctor is not able to see a recognisable embryo.
The actual procedure usually only takes five to ten minutes, but you will usually need to be in the hospital for around four to five hours. Most of this time will be spent waiting and recovering.
You may have to wait a day or two to have a curette and sometimes, while you are waiting, the pregnancy tissue will pass on its own.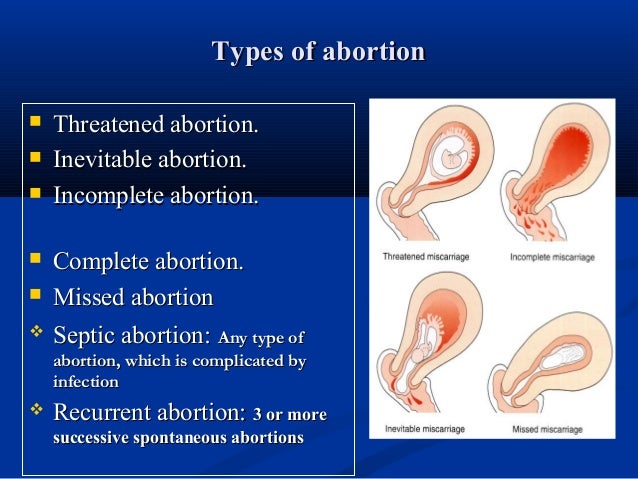 If this happens and all of the tissue is passed you may not need to have a curette.
If this happens and all of the tissue is passed you may not need to have a curette.
A curette is done in the following circumstances:
- You have heavy or persistent bleeding and/or pain.
- The medical staff advise that this is a better option for you; this may be because of the amount of tissue present, especially with a missed miscarriage.
- This is an option you prefer.
Things to know
The risks of a D&C are very low, but include:
- some pregnancy tissue remains in uterus. This can cause prolonged or heavy bleeding and the operation may need to be repeated
- infection needing antibiotics
- damage to the cervix or uterus. This is very rare (around 1 in 1000) and, when it does happen, it is usually a small hole or tear which will heal itself
- excessive bleeding (very rare)
- anaesthetic risks. These are very low for healthy women, but no anaesthetic or operation is without risk.
Waiting for treatment
If you have heavy bleeding with clots and crampy pain, it is likely that you are passing the pregnancy tissue. The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
The bleeding, clots and pain will usually settle when most of the pregnancy tissue has been passed. Sometimes the bleeding will continue to be heavy and you may need further treatment.
You should go to your nearest emergency department if you have:
- increased bleeding, for instance soaking two pads per hour and/or passing golf ball sized clots
- severe abdominal pain or shoulder pain
- fever or chills
- dizziness or fainting
- vaginal discharge that smells unpleasant
- diarrhoea or pain when you open your bowels.
What to do while you are waiting
- You can try to rest and relax at home.
- Usual activity that is not too strenuous will not be harmful. You can go to work if you feel up to it.
- If you have pain you can take paracetamol.
- If there is bleeding, use sanitary pads rather than tampons.
After a miscarriage
- It is usual to have pain and bleeding after a miscarriage.
 It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage.
It will feel similar to a period and will usually stop within two weeks. You can take ordinary painkillers for the pain. Your next period will usually come in four to six weeks after a miscarriage. - See a doctor or attend a hospital emergency department if you have strong pain and bleeding (stronger than period pain), abnormal discharge, (especially if it is smelly), or fever. These symptoms may mean that you have an infection or that tissue has been left behind.
- Try and avoid vaginal sex until the bleeding stops and you feel comfortable.
- Use sanitary pads until the bleeding stops (do not use tampons).
- All contraceptive methods are safe after a miscarriage
- See a GP (local doctor) in four to six weeks for a check-up.
Anti-D injection after a miscarriage
It is important to have your blood group checked. If you’re RhD negative and the fetus is RhD positive this can cause problems for future pregnancies. This is because the fetus’s blood cells have RhD antigen attached to them, whereas yours do not. If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
If small amounts of the fetus’s blood mixes with your blood, your immune system may perceive this difference in blood cells as a threat and produce antibodies to fight against the fetus’s blood. Once your body has made these antibodies they can’t be removed. This is unlikely to have caused your miscarriage and is more likely to affect future pregnancies. Women with a negative blood type usually need an Anti-D injection, which will stop the antibodies forming.
Future pregnancies after a miscarriage
One of the most common concerns following a miscarriage is that it might happen again. However, if you have had one miscarriage the next pregnancy will usually be normal.
If you do try for another pregnancy, try and avoid smoking, alcohol and excess caffeine as they increase the risk of miscarriage. It is recommended that all women take folic acid while trying to conceive, and continue until three months of pregnancy. In your next pregnancy you are encouraged to see your GP and have an ultrasound at about seven weeks. If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
If ultrasound is done too early in pregnancy the findings are often uncertain and cause unnecessary worry.
Feelings and reactions
There is no ‘right’ way to feel following a miscarriage. Some degree of grief is very common, even if the pregnancy wasn’t planned. Partners may react quite differently, just as people can respond differently to a continuing pregnancy. Feelings of loss may persist for some time and you may have mixed feelings about becoming pregnant again. Some friends and family may not understand the depth of emotion that can be attached to a pregnancy and may unreasonably expect for you to move on before you are ready.
Some couples decide that they want to try for a pregnancy straight away, while others need time to adjust to their loss. If you feel anxious about a possible loss in future pregnancies, you may find it helpful to talk to someone about this. If it’s difficult to speak with your friends and family about these issues, your doctor, community support group and counsellors can provide information and assistance.
Related Health Topics
-
- Treatment for miscarriage
Treatment for miscarriage is aimed at avoiding heavy bleeding and infection. It is also aimed at looking after you, physically and emotionally.
-
- (English) PDF (302 KB)
- Treatment for miscarriage
The Women’s does not accept any liability to any person for the information or advice (or use of such information or advice) which is provided on the Website or incorporated into it by reference. The Women’s provide this information on the understanding that all persons accessing it take responsibility for assessing its relevance and accuracy. Women are encouraged to discuss their health needs with a health practitioner.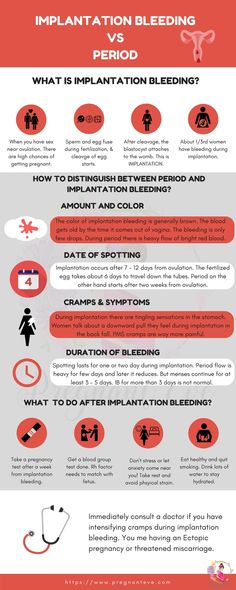 If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
If you have concerns about your health, you should seek advice from your health care provider or if you require urgent care you should go to the nearest Emergency Dept.
What happens after miscarriage | Pregnancy Birth and Baby
What happens after miscarriage | Pregnancy Birth and Baby beginning of content7-minute read
Listen
It can be very distressing to have a miscarriage. But aside from the emotional sides of things, there are practical things to decide on and your health to consider.
What should I do if I’ve miscarried at home?
If you wish to, you may decide to collect your baby in a container to show your doctor. Depending on your circumstances, your doctor may send the baby to a laboratory for testing to try to find out why it happened.
What will happen if I miscarry in hospital?
If you miscarry in hospital, you may decide that you wish to see your baby. Whether or not this is possible depends on:
- the stage of your pregnancy
- when the baby died
- whether you had a dilatation and curettage (also called a D&C or curette)
Sometimes your baby may no longer be recognisable, and the staff may advise you not to view the remains.
If you think you would like to see your baby, discuss your wishes with the hospital staff.
Are there any legal obligations?
Legal obligations following your miscarriage may vary according to your state or territory. Your hospital should inform you of any requirements.
Generally, if you lose your baby in the first 20 weeks of pregnancy (defined as a miscarriage), the birth and death of your baby cannot be formally registered. This means that you will not receive a birth or a death certificate.
Some state governments, such as NSW and Queensland, offer optional certificates recognising early pregnancy loss to support parents grieving a miscarriage. If this interests you, please contact the Births, Deaths and Marriage Registry in your state or territory to find out if similar certificates are available.
If this interests you, please contact the Births, Deaths and Marriage Registry in your state or territory to find out if similar certificates are available.
You are not legally required to have a funeral, burial or cremation, although you may choose to do so.
What services will the hospital offer?
The services offered for miscarriage vary between different hospitals.
Some hospitals offer services such as:
- saving the pregnancy tissue from a D&C where possible (provided you have explicitly requested this)
- arranging to have pregnancy tissue cremated at your request
- giving you back the pregnancy tissue for your own private burial or cremation
If you do not make any specific requests, the pregnancy tissue is commonly examined in a laboratory and then cremated according to the hospital protocol.
Some hospitals raise these issues with you. If they do not, it is important to raise these issues yourself.
Can I have a memorial service?
Some hospitals offer shared memorial services to commemorate the loss of all babies.
Your hospital may also offer bereavement support.
Can I have a funeral?
While there is no legal obligation to have a funeral, burial or cremation after a miscarriage, you may choose to make your own arrangements to mark the loss of your baby.
You may choose to engage a private funeral director or approach your religious leader for advice about having a funeral, burial or cremation. Alternatively, you may decide to bury your baby at home.
How long will it take to physically recover from a miscarriage?
How long recovery takes depends on how far along you were in your pregnancy, the treatment you needed and whether or not you had any complications.
Bleeding and discomfort
You may have discomfort and bleeding for up to 2 weeks.
Things to consider:
- use pads for the bleeding, not tampons
- use medication such as paracetamol for the discomfort
- avoid sex and swimming until the bleeding stops
See your doctor or go to your nearest emergency department if:
- the bleeding becomes heavy (soaking 1 to 2 pads in an hour) or goes on for longer than 2 weeks
- you pass large blood clots
- you have severe pain
- you have a temperature
- you have signs of infection, such as a temperature or a smelly vaginal discharge
Other changes
You may find the nausea gets better, and your breasts decrease in size and become less tender.
If you have had a miscarriage near 20 weeks, your breasts may produce milk. Please talk to your doctor or midwife if you have any questions or concerns.
When should I follow up with my doctor or midwife?
You should have a check-up with your doctor or midwife no later than 6 weeks after you miscarry. Your doctor or midwife can provide support, answer questions and advise about contraception.
Your doctor may want to order further tests, including:
- your blood group — if you have a negative blood group, your doctor may recommend an anti-D injection
- your haemoglobin level — if you have anaemia (low blood haemoglobin), your doctor may recommend a diet to follow and iron tablets
What does this mean for future pregnancies?
If you have had a miscarriage, the next pregnancy will usually be normal. After a miscarriage, the chance of you miscarrying again is low (1 in 5 women). If you have had 3 or more miscarriages, your doctor may recommend you that you see a fertility specialist.
How soon can I fall pregnant again?
Fertility can return immediately after a miscarriage, so consider using contraception until you are ready to start trying again.
If you fall pregnant straight after having a miscarriage, the risk that you will miscarry again is slightly higher. For this reason, doctors recommend that you wait until you have had at least one period before trying to get pregnant again.
How do I plan for another pregnancy?
Planning for pregnancy after a miscarriage can be confronting. It is important that both you and your partner are physically and emotionally ready for another pregnancy. Your doctor or midwife can provide advice about emotional support, falling pregnant again and lifestyle changes that may help you have a successful pregnancy.
Who can I talk to for advice and support?
Talk to your doctor or midwife for information and advice on what do and how to look after yourself if you experience a miscarriage.
Your hospital should be able to provide details of available support services, such as bereavement support.
SANDS is an independent organisation that provides support for miscarriage, stillbirth and newborn death. You can call them on 1300 072 637 or visit www.sands.org.au.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
NSW Registry of Birth Deaths & Marriages (Recognition of early pregnancy loss), Miscarriage Association (Management of miscarriage: your options), Queensland Government (Early pregnancy loss recognition certificate), The Royal Women's Hospital (After a miscarriage), The Royal Women's Hospital (Miscarriage), NSW Health (Early pregnancy - when things go wrong), SANDS (Miscarriage), SANDS (Early pregnancy loss brochure), Raising Children Network (Miscarriage: what it is and what to expect), Women's and Children's Health Network (Miscarriage), Red Nose (Women's physical health after a miscarriage)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: March 2022
Back To Top
Related pages
- Fathers and miscarriage
- Emotional support after miscarriage
- Miscarriage
- What really happens during a miscarriage
- Experiencing a pregnancy loss
Need more information?
Miscarriage
Miscarriage Despite being common and widespread, miscarriage can be a heartbreaking experience – with up to one in five pregnancies ending before week 20
Read more on Gidget Foundation Australia website
Miscarriage
A miscarriage is the loss of a baby, usually during the first three months or first trimester of pregnancy.
Read more on Pregnancy, Birth & Baby website
Fathers and miscarriage
A miscarriage can be a time of great sadness for the father as well as the mother.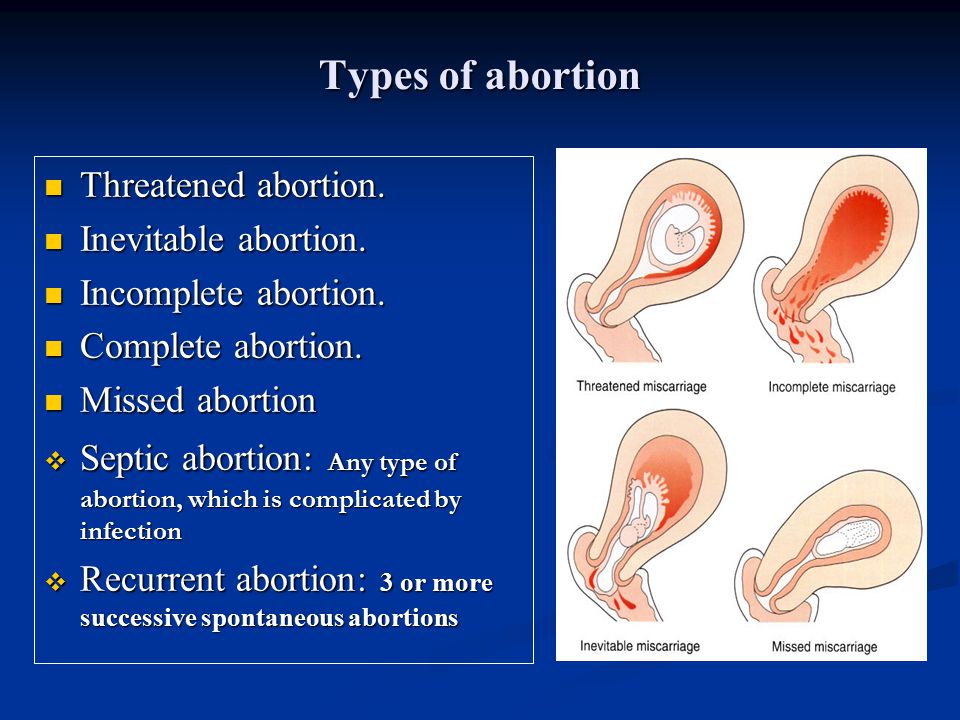
Read more on Pregnancy, Birth & Baby website
Emotional support after miscarriage
It is important to know that there is no right or wrong way to feel after experiencing a miscarriage.
Read more on Pregnancy, Birth & Baby website
Miscarriage | SANDS - MISCARRIAGE STILLBIRTH NEWBORN DEATH SUPPORT
Helping you understand the complex range of emotions you may experience during fertility treatment or after miscarriage or early pregnancy loss
Read more on Sands Australia website
Miscarriage: a guide for men | Raising Children Network
This Dads Guide to Pregnancy covers miscarriage, the grief men might experience after miscarriage, and how to support partners after pregnancy loss.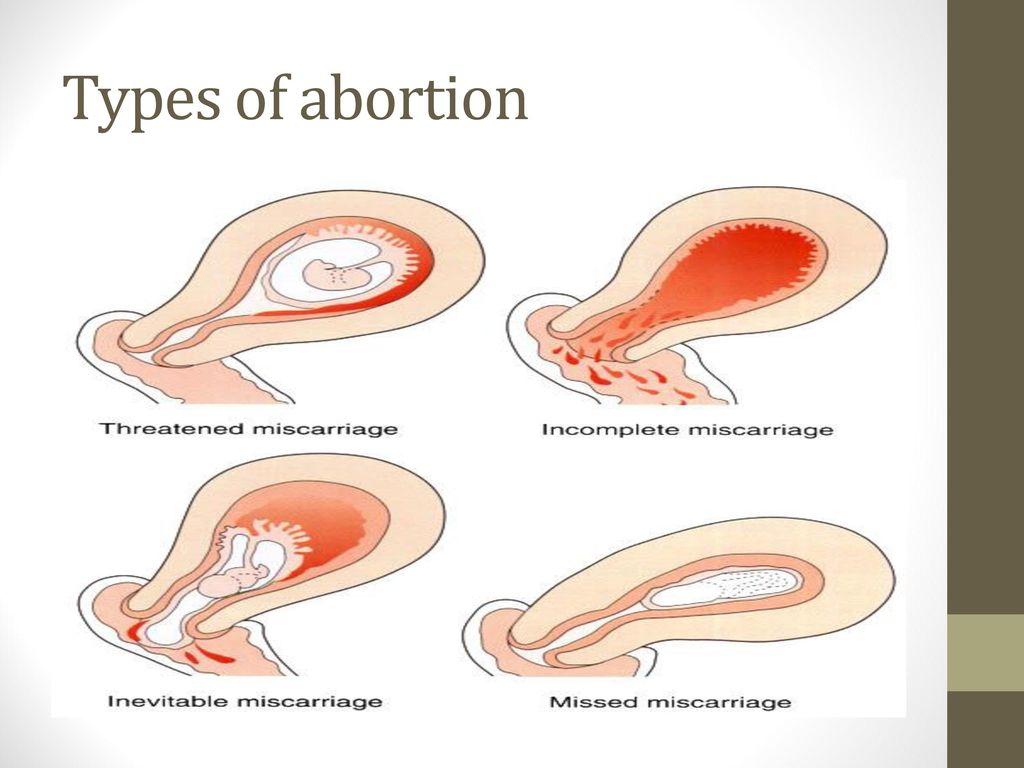
Read more on raisingchildren.net.au website
The Pink Elephants Support Network - Medical Options for Recurrent Miscarriage
In some cases, a medical reason for miscarriage or recurrent miscarriage can be found through testing
Read more on Pink Elephants Support Network website
What really happens during a miscarriage
Understand what actually happens during a miscarriage and what you might see and feel. Please be warned that this article contains some graphic descriptions.
Read more on Pregnancy, Birth & Baby website
New research on vitamin B3 and miscarriages
Pregnant women are being warned not to start taking vitamin B3 supplements, despite a recent study that suggests it might reduce the risk of miscarriages and birth defects.
Read more on Pregnancy, Birth & Baby website
Pregnancy: miscarriage & stillbirth | Raising Children Network
Have you experienced a miscarriage or stillbirth? Find articles and videos about coping with the grief of losing a pregnancy or having a stillbirth.
Read more on raisingchildren.net.au website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
norm or cause for panic
- Home
- Useful articles
Bleeding after abortion: normal or cause for alarm
Uterine bleeding after termination of pregnancy is a common phenomenon in obstetric practice that occurs on the first day after the operation. The intensity and duration of blood loss are individual and depend not only on the characteristics of the female body, but also on the type of abortion.
 nine0017
nine0017 Features of bleeding after abortion
Bleeding may be completely absent during the first two days after surgical termination of pregnancy, but later increases to menstrual bleeding and continues in some clinical pictures up to 6 weeks. This pathology indicates a hormonal imbalance, that is, there is insufficient "support" of endometrial tissues, which supports the development of pregnancy. As a result of this bleeding after termination of pregnancy can only intensify, and continue intermittently for several weeks. It is important to understand that here we are talking about pathology.
Most women of reproductive age are concerned about the main question, how long will bleeding after an abortion last? The question is individual, but if it does not pass more than two weeks after getting rid of the fetus, it is important to urgently contact the local gynecologist. The duration of the hemorrhage also depends on the gestational age: the earlier an abortion is performed, the more likely it is to solve such a piquant problem in a gentle “mode” and without serious consequences.
:max_bytes(150000):strip_icc()/hemorrhage-in-miscarriage-meaning-2371523-FINAL-f2ab04cab1cc491e964a45e682f93da5.png) nine0017
nine0017 Cause of abnormal bleeding after an abortion
The occurrence of bleeding after an abortion should not confuse the patient, but its duration should be a cause for concern. Among the pathological causes of this symptom, the following should be singled out:
- Perforation of the uterus;
- Injury of the cervix;
- Presence of residual fetal tissue;
- Blood clotting disorder;
- The reaction of the female body to individual anesthetics. nine0004
With such diagnoses, along with hemorrhage, there is an obvious violation of the temperature regime, convulsions, general weakness, fainting, hypotension, increased heart rate. It is important not to ignore such signs of shock, but to visit a medical center and a qualified specialist in a timely manner.
How to deal with bleeding after a miscarriage
It is important to understand that to stop prolonged bleeding after a miscarriage at home is impossible, only a competent gynecologist can determine an accurate and effective treatment regimen.
 Delay in this matter can cost the patient her life.
Delay in this matter can cost the patient her life. If the appeal to the doctor is timely, then the first thing the patient is referred for is an ultrasound scan. This accurate clinical examination allows to determine the etiology of the pathological process and the future treatment regimen. If it became known that there is residual fetal tissue in the uterus, additional surgical intervention is necessary to properly clean its cavity. In case of mechanical damage to the uterus or its cervix after interruption, the gynecologist prescribes the repair of the injured area of the uterus, bladder or intestines. nine0017
Possible complications
Bleeding after an abortion is dangerous for women's health and causes serious damage to the woman's reproductive system. Among the potential complications, doctors distinguish infertility, malignant tumors and even death of the patient. Therefore, the problem needs to be addressed in a timely manner, and early termination of pregnancy in order to avoid heavy bleeding.
Return to list
Spontaneous abortion (miscarriage)
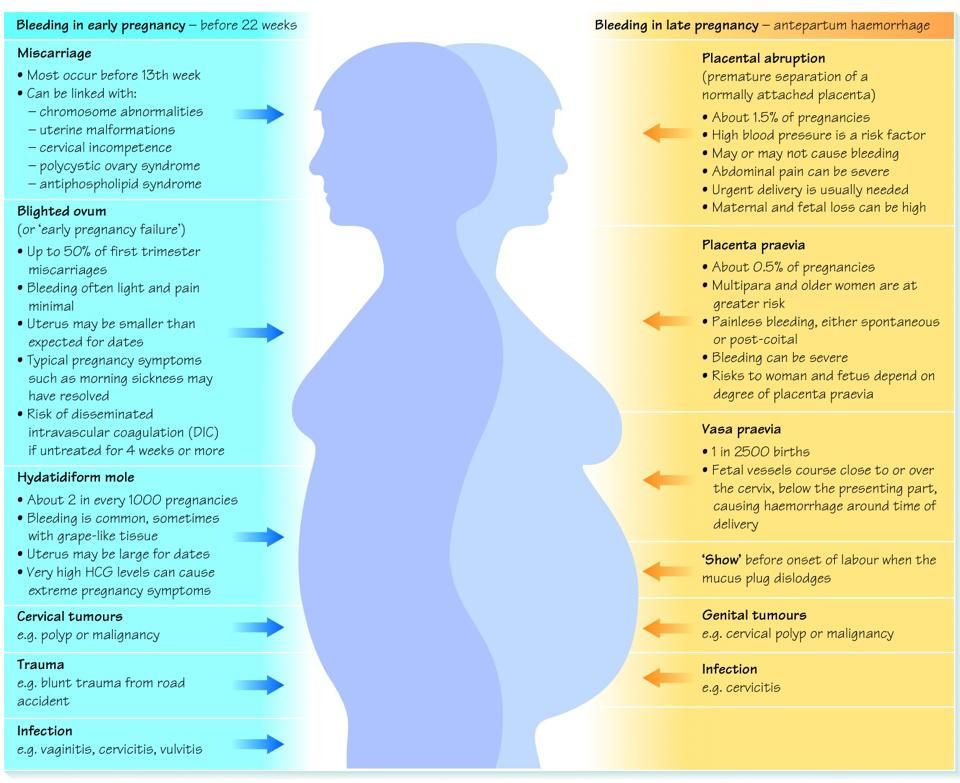
If the pregnancy ends naturally before the fetus reaches gestational age, this is called a miscarriage or miscarriage. More than half of miscarriages occur no later than 12 weeks of gestation due to fetal abnormalities. The rest falls on the period up to 20 weeks and is associated with pathologies of pregnancy. If the pregnancy is terminated in the second half, it is called preterm labor.
Spontaneous abortion, otherwise known as miscarriage, is one of the most common complications during pregnancy, accounting for 10-20% of diagnosed pregnancies, and is the rejection of a fetus weighing no more than 500 grams. and less than 22 weeks. Unfortunately, with such indicators, the fetus is not viable. Usually 80% of the total number of spontaneous abortions occurs before the 12th week of pregnancy. nine0017
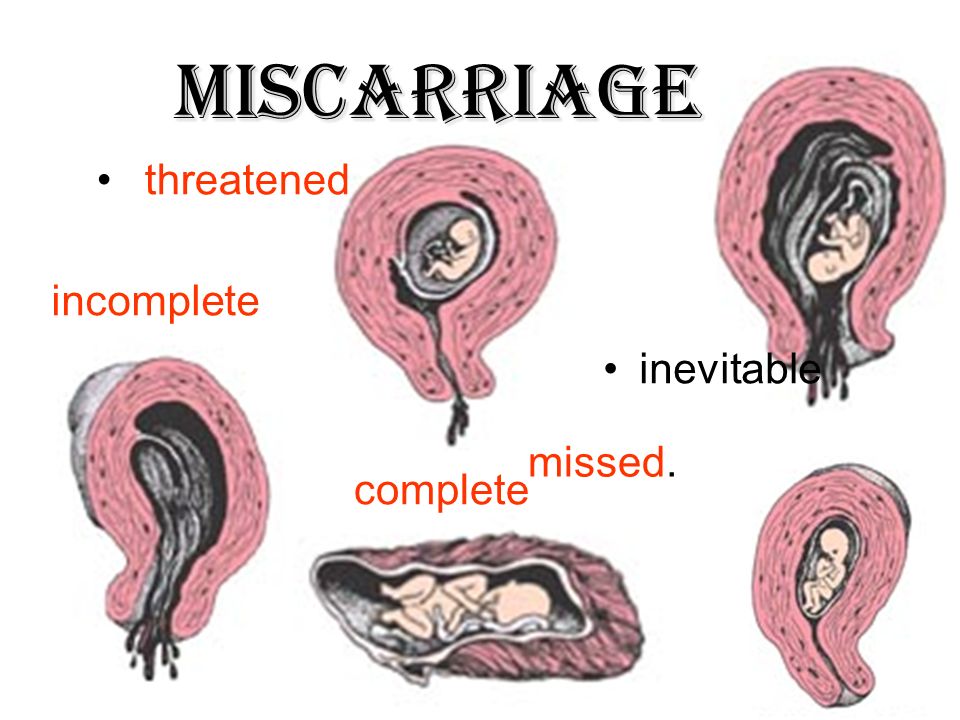
Types of spontaneous abortion
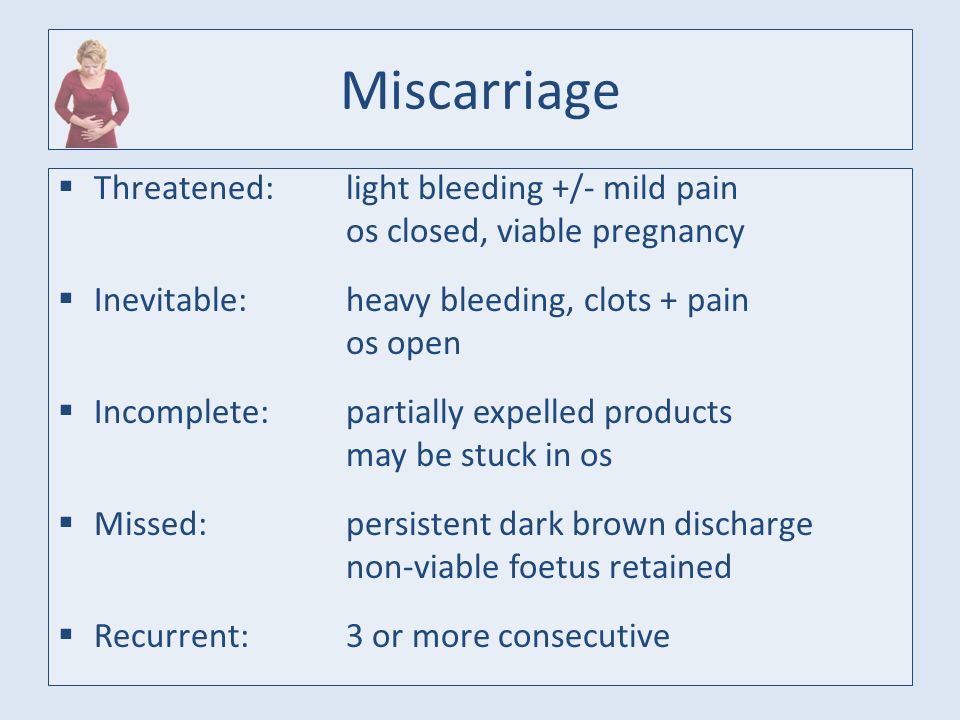
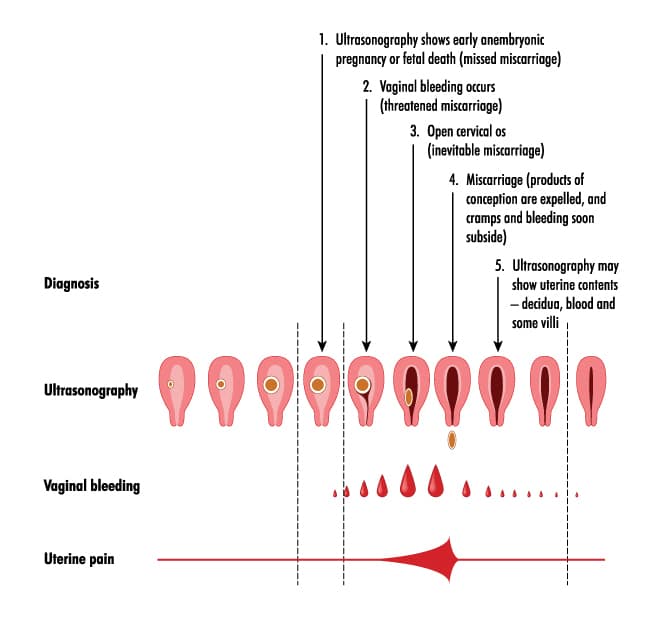
1. Threat of miscarriage - characterized by mild uterine cramps, pulling pain in the lower abdomen and sometimes mild bloody discharge from the vagina.

2. A miscarriage that has begun - is characterized by more severe pain and profuse bleeding. At the same time, the tone of the uterus is slightly increased, and the internal os is closed.
3. Inevitable miscarriage - accompanied by dilatation of the cervix - a fetal egg can be distinguished - with profuse bleeding and severe cramps in the lower abdomen. nine0017
4. Incomplete miscarriage - part of the fetus comes out. The bleeding is so profuse that it can lead to the death of a woman.
5. Completed miscarriage - the fetal egg and the fetus itself are completely out. After that, the bleeding and spasms stop.
The etiology of miscarriage is due to many factors. Among them:
- genetic disorders;
- previous induced abortions;
- too little time has passed since the previous pregnancy; nine0017
- inflammatory infections in the mother, endocrine disorders;
- blood conflict between mother and fetus;
- taking hormonal contraceptives and certain medications;
- smoking during pregnancy and drinking alcohol;
- unknown causes.

To prevent miscarriage, it is necessary to give up bad habits, not to have abortions and to be regularly examined by a doctor.
Spontaneous abortion begins with the appearance of cramping, pulling pains, similar to pain during menstruation. Then bleeding from the uterus begins. At first, the discharge is slight or moderate, and then, after detachment of the fetal egg, abundant discharge with bloody clots begins. The appearance of these symptoms requires urgent hospitalization. nine0017
After examining a woman in a hospital, having determined the degree of detachment of the embryo, one of the following diagnoses will be made:
- the threat of pregnancy - detachment is only outlined or is completely insignificant. In this case, the pregnancy can be saved;
- a miscarriage that has begun - detachment is already quite decent with a pronounced pain syndrome. And in this case, the fetus can be saved;
- abortion in progress - detachment with displacement progresses, labor-like contractions begin.
 Pregnancy cannot be saved, cleaning is required; nine0017
Pregnancy cannot be saved, cleaning is required; nine0017 - incomplete miscarriage - independent exit of a part of the fetus and membranes, curettage is necessary for the final curettage of the uterus;
- late abortion - premature delivery of an unviable baby.
After a miscarriage, a short break in planning and taking preventive measures is recommended to avoid recurrence.
In case of repeated miscarriage, a thorough comprehensive examination is necessary to determine the causes of miscarriage and eliminate them. nine0017
A miscarriage is a severe psychological trauma, especially during the first pregnancy. But do not give up, with a competent approach to planning and bearing, the next pregnancy will certainly end with the appearance of a long-awaited baby.
Causes of spontaneous abortion
1. Doctors call various chromosomal pathologies one of the main reasons: monosomy, autosomal trisomies, polyploidy. They account for 82-88% of spontaneous miscarriages.