How to soothe a child sore throat
Sore Throat (Viral)
Nationwide Children’s Hospital
Two different germs cause sore throats – viruses and bacteria. They are both contagious and easily spread to others.
- The germs hang out in the nose and throat. When the infected person coughs, sneezes, or talks, the germs go into the air. They are then breathed in by others.
- The germs can also land on things and be picked up by touching them.
Most often, a sore throat is caused by a virus like the flu or common cold. The sore throat will go away on its own in a few days without any treatment.
When a sore throat comes on fast, it may be caused by the bacteria streptococci (strep-tuh-kaak-sai), or strep. Antibiotics will not help treat viruses.
Symptoms of a Virus
If your child has a sore throat with any of these symptoms, it is likely due to a virus.
- Sore throat, maybe red with yellow patches
- Decreased appetite
- Red, itchy, or watery eyes
- Sleeping more than normal
- Runny nose, stuffed nose, or sneezing
- Fussiness
- Cough
- Hoarseness
Diagnosis
It is important to know if your child’s sore throat is due to a virus or to strep bacteria.
- The doctor or health care provider will examine your child and ask about their symptoms.
- If they suspect strep, 1 or 2 soft swabs will be brushed over the back of your child’s throat to do 1, or both, of the tests on the next page. Your child may gag a little.
- A rapid strep test (rapid antigen test) – It takes up to 30 minutes to get the results of a rapid strep test. You will stay until you get the results.
- A throat culture – Sometimes only this test is done. If your child had a rapid strep test first, the same swab can be sent to the lab for testing.
 It takes 1 to 2 days to get the results. The lab will notify your child’s doctor or health care provider, who will then let you know the results.
It takes 1 to 2 days to get the results. The lab will notify your child’s doctor or health care provider, who will then let you know the results.
- A positive rapid strep test or positive throat culture means that your child has strep throat. They must start to take antibiotic medicine right away. Early treatment can prevent harm to the body.
- Let your child’s doctor know if they are a strep carrier. Strep carriers always test positive for strep even after taking antibiotics. Their sore throat will be treated like a virus.
How to Care For Your Child
There are things you can do to help your child feel better.
- Give them soft, easy-to-swallow foods, like applesauce, mashed potatoes, hot cereal, or eggs. Do not force them to eat. Your child may not want to eat much if it hurts to swallow.
- Give them lots of liquids, like water, Pedialyte®, diluted apple juice, or popsicles. Give small amounts of liquid often (Picture 1).

- To soothe a sore throat, for children:
- For children over age 1, give warm fluids like water, herbal tea with honey, or diluted apple juice. Do not give honey to children under age 1. For some children, cold fluids or popsicles can be soothing.
- For children over age 4, give throat or cough lozenges or use throat sprays. Read the label to know the right dose for your child. Do not use throat sprays that contain benzocaine, as this could cause a drug reaction.
- For children over age 6 who are able to gargle without swallowing, mix ½ teaspoon of table salt in 8 ounces of warm water. Have them swish and gargle the mixture 2 to 3 times a day for the next few days. Do not let your child swallow the salt water; have them spit it out.
- For a fever or throat pain, give acetaminophen (such as Tylenol®) or ibuprofen (Advil®, Motrin®) as directed.
 Read the label to know the right dose for your child. Do not give aspirin or products that contain aspirin.
Read the label to know the right dose for your child. Do not give aspirin or products that contain aspirin.
How to Protect Others
- Good hand washing is VERY important! Clean your hands and your child’s hands often with soap and water. Wash for 15 to 20 seconds, or the time it takes to sing the Happy Birthday song (Picture 2). If soap and water are not available, an alcohol-based hand sanitizer that contains at least 60% alcohol may be used. Rub hands until dry.
- Make sure to wash your child’s drinking glass and eating utensils in hot soapy water before others use them.
- Give your child a paper bag and have them put their used tissues in this bag. Moisture from the child’s nose and mouth is contagious.
When to Call the Doctor
Call your child's doctor of health care provider if they:
- Start pulling at their ears.
- Have a sore throat that lasts more than 3 days.
- Have trouble breathing.

- Start drooling, can't talk, or voice gets muffled.
- Can't eat or drink.
- Have a fever:
- Younger than 3 months of age - 100.4° Fahrenheit (F) or 38° Celsius (C) or above.
- Older than 3 months of age
- 104° F (40° C) or above.
- Above 102° F (38.9° C) for more than 2 days or it keeps coming back.
- Treated to bring their fever down, but it hasn’t worked.
- Any age - call with a fever and:
- Has an unusual rash.
- Looks ill, is fussy, or is drowsy.
- Has been in a very hot place, such as an overheated car.
- Is not eating or drinking and shows signs of dehydration - dry or sticky mouth, sunken eyes, dark urine, dry diapers, or not urinating.
- Has a stiff neck, a bad headache, a very sore throat, a painful stomach ache, vomiting, or diarrhea.
- Has immune system problems that make them more likely to get sick, such as sickle cell disease or cancer, or takes medicine that weakens the immune system.

Sore Throat (Viral) (PDF), Somali (PDF), Spanish (PDF)
HH-I-121 11/89, Revised 5/22 Copyright 1989, Nationwide Children’s Hospital
You Might Also Be Interested In
Blog
What You Need to Know about Strep Throat
Roseola
Blog
Sore Throat Spectrum: Runny Nose to Strep and Everything in Between
Home Remedies for Fevers, Sore Throats, and More
Medically Reviewed by Neha Pathak, MD on December 01, 2021
Rest helps you heal. And that’s a good reason to keep your child home when they are not feeling well. It’s even more important if they have a fever. You’ll help prevent spreading the germs to other people.
And that’s a good reason to keep your child home when they are not feeling well. It’s even more important if they have a fever. You’ll help prevent spreading the germs to other people.
If they are not sleepy, they can rest while looking at books, magazines, or their favorite movie. The key is to limit activity. Once the fever passes and they feel more like themselves again, it’s time to go back to school.
Give your young child water, milk, or formula to keep them hydrated. If they are older, you can also give them frozen fruit bars and ice pops. And don't forget about good ol' chicken soup.
It can be tough to tell the difference. In general, your child will feel worse with the flu, and they may go from fine to lousy fast. They may be exhausted and have chills, muscle aches, a headache, and a high fever. If you think it’s the flu, call your doctor right away. There’s medication that can help if it’s taken within a day or two of symptoms starting.
A fever is the body’s way of fighting an infection. But having one can make your child uncomfortable. If they have a fever, they’ll be more comfy in light clothing in a cool room. Put a cool washcloth on their forehead and neck, too.
But having one can make your child uncomfortable. If they have a fever, they’ll be more comfy in light clothing in a cool room. Put a cool washcloth on their forehead and neck, too.
They may not need medicine to bring down their fever, but they may be able to take acetaminophen or ibuprofen. Check with your doctor before you give any medicine to a child younger than 2, and follow instructions carefully. Don't give ibuprofen to infants less than 6 months old.
For children under 4 years old, home remedies are the way to go for treating colds. Most cold medicines aren’t good for kids that young. After age 4, you should get your doctor’s OK and read the directions carefully. Don’t give your child medicine made for adults, aspirin, or more than one medicine with the same ingredients.
If your baby’s congested, get rid of the mucus with a rubber suction bulb. Put three drops of warm water or saline in each nostril to soften the mucus, and wait a minute before you suction it out.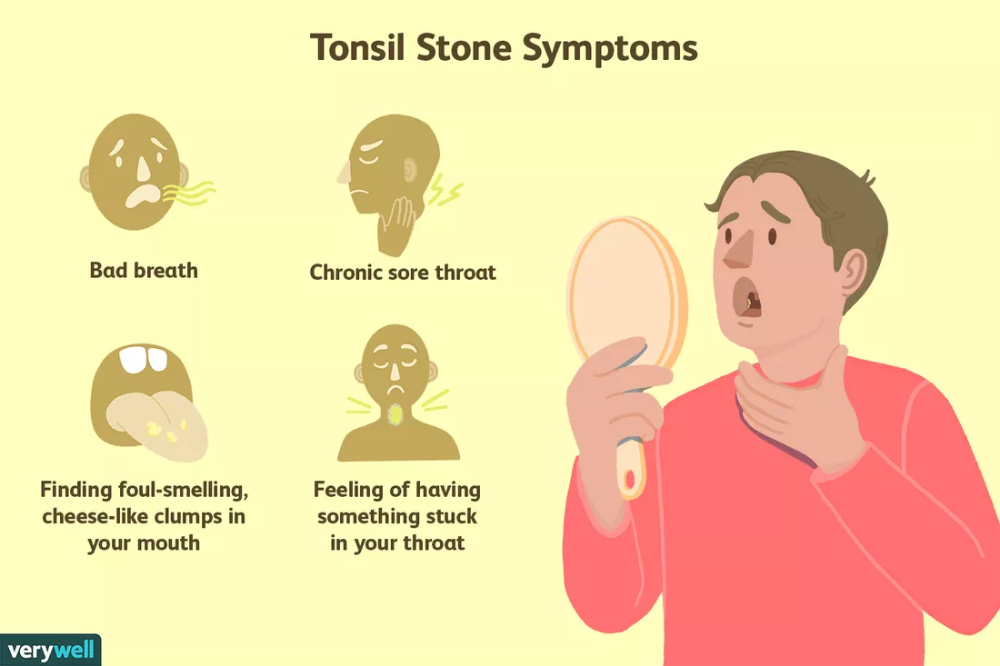 Raise the head of your child’s crib or bed 3 to 4 inches to make it easier for them to breathe.
Raise the head of your child’s crib or bed 3 to 4 inches to make it easier for them to breathe.
A cool-mist humidifier or vaporizer can also help clear the stuffiness. And if their nose is red from too much blowing, put a little petroleum jelly on the skin beneath it.
Think hot and cold. Milkshakes, cold drinks, and ice chips numb the throat. Warm broth, tea, or hot apple cider soothe it.
If your child is 8 or older, gargling with warm salt water twice a day may help them feel better. Over-the-counter medications such as acetaminophen or ibuprofen can ease pain, too.
Treat a cough or not? It depends on your child’s age and how much it’s bothering them. A hacking cough that’s uncomfortable and disrupts their sleep needs attention. For kids between 6 months and 1 year old, give warm, clear liquids like diluted apple juice, lemonade, or water. If your child is older than 1, honey can help fend off nighttime coughing fits. Children 6 years or older can suck on cough drops or hard candies, too.
What else can help? Have your child breathe in the steam from a warm shower, or put a humidifier or vaporizer in their room.
Don’t worry about "feeding a cold and starving a fever." Just make sure your child eats when they are hungry. Soft foods that are easy to swallow are more appealing to a child who isn’t feeling well. Try applesauce, oatmeal, mashed potatoes, and yogurt.
Kids who've got the flu sometimes have upset stomachs with vomiting or diarrhea. If this happens to your child, they are losing fluids. So have them drink small amounts of an electrolyte solution or water and suck on ice pops. Ginger ale and other sodas, juices, and sports drinks can make diarrhea worse. If your child is not drinking enough, peeing less, or looks sick, call your doctor.
A child with diarrhea who isn’t dehydrated or vomiting can keep eating. Just give them smaller portions and more liquids.
Talk to your doctor if you’re worried or if your child's symptoms are getting worse.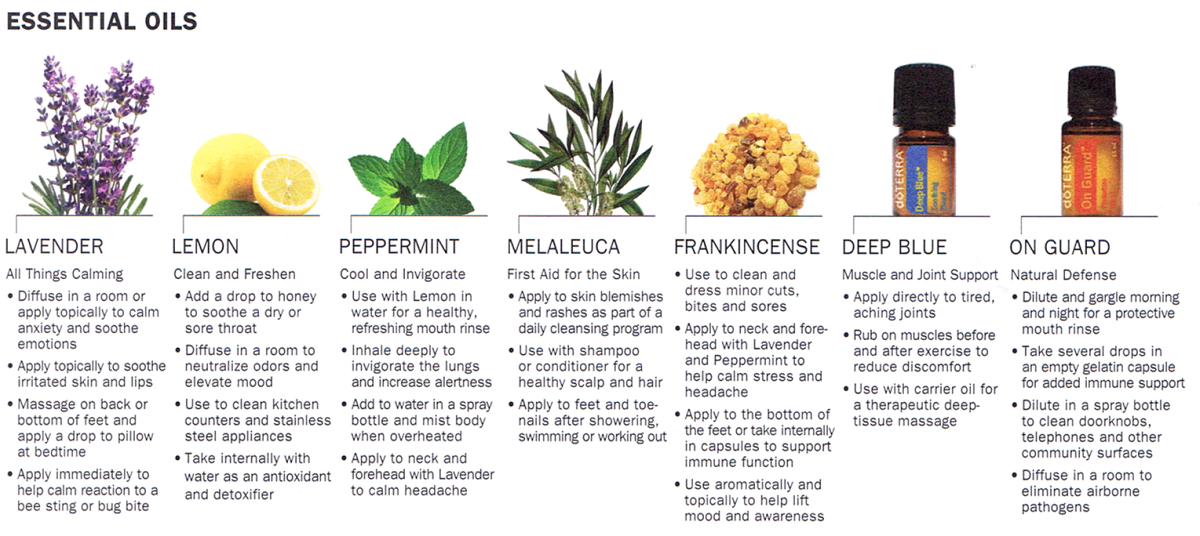 Watch for chest or stomach pain, shortness of breath, a headache, unusual fatigue, or face or throat pain that gets worse. Let your doctor know if your child has a fever of 103 F or higher, or has had a fever of 101 F or higher for more than 72 hours. If they are having trouble swallowing, is coughing up a lot of mucus, or has swollen glands or an earache, you should take them to see a doctor.
Watch for chest or stomach pain, shortness of breath, a headache, unusual fatigue, or face or throat pain that gets worse. Let your doctor know if your child has a fever of 103 F or higher, or has had a fever of 101 F or higher for more than 72 hours. If they are having trouble swallowing, is coughing up a lot of mucus, or has swollen glands or an earache, you should take them to see a doctor.
IMAGES PROVIDED BY:
1) VStock / Getty Images
2) Steven Pomberg
3) Robert Marmion / Getty Images
4) dragon_fang / Getty Images
5) BananaStock / Getty Images
6) yocamon / Getty Images
7) Steven Pomberg
8) Steven Pomberg
9) tycoon751 / Getty Images
10) Laikwunfai / Getty Images
11) spwidoff / Getty Images
SOURCES:
CDC: “The Flu: Caring for Someone Sick at Home.”
FamilyDoctor.org: “Colds and the Flu – Treatment.”
Healthychildren.org: “Caring for a Child with a Viral Infection,” “Children and colds,” “Flu: A Guide for Parents of Children or Adolescents with Chronic Health Conditions,” “Treating Vomiting. ”
”
Kaiser Permanente: “Self Care for Kids: A Guide for Parents and Caregivers.”
Kidshealth.org: “Common Cold,” “Diarrhea,” “Infections: Common Cold,” “Is it a cold or the flu?” “Tips for Treating the Flu.”
Rennard, B. American College of Chest Physicians, October 2000.
FDA: “Tamiflu (oseltamivir phosphate) Information.”
Seattle Children’s Hospital: “Should Your Child See a Doctor? Sore Throat.”
St. Louis Children’s Hospital: “Coughs and Colds: Medicines or Home Remedies?”
UpToDate: “Patient Information: Fever in Children, Beyond the Basics.”
If a child has a sore throat
A child has a sore throat: what and how should parents do in this case?
consultation of a pediatrician at the medical center "Onni"
Sore throat is one of the common causes of outpatient and emergency visits by parents of children to doctors for help. Upper respiratory tract infections are very common in both children and adults and have significant economic consequences due to the frequent prescription of antibiotics by physicians, even when the infection is not caused by bacteria.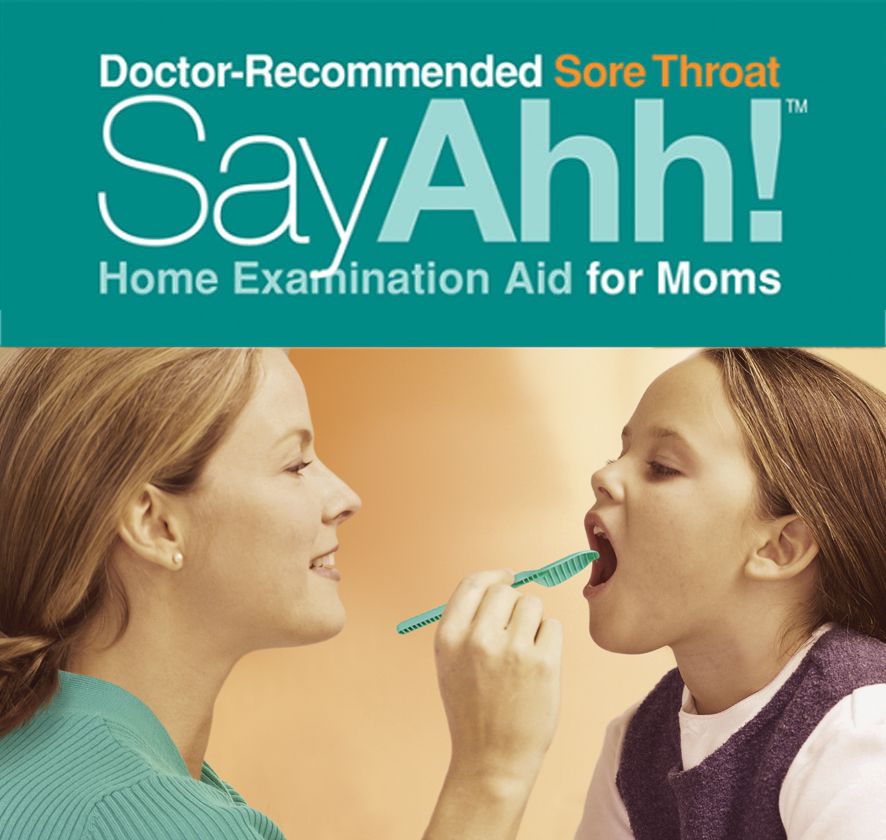 About a quarter of children suffering from tonsillitis also suffer from bacterial pharyngitis. Identification and adequate antibiotic treatment of group A streptococcal angina is important for the primary prevention of acute rheumatic fever, which occurs in 3% of cases. Therefore, in any case, with a sore throat, it is necessary to show the child to the doctor in order to exclude diseases that are dangerous to health and life. nine0005
About a quarter of children suffering from tonsillitis also suffer from bacterial pharyngitis. Identification and adequate antibiotic treatment of group A streptococcal angina is important for the primary prevention of acute rheumatic fever, which occurs in 3% of cases. Therefore, in any case, with a sore throat, it is necessary to show the child to the doctor in order to exclude diseases that are dangerous to health and life. nine0005
How does a sore throat manifest itself?
The main symptom of a sore throat is pain, both at rest and when swallowing or talking. Sore throat is the primary symptom of pharyngitis. The terms "tonsillitis" and "pharyngitis or pharyngotonsillitis" are often used interchangeably. Pharyngitis refers to the objective signs of inflammation of the pharynx: edema, exudate, ulceration, or overt erythema. Redness of the throat may occur as part of a general redness of all the mucous membranes of the upper respiratory tract in small patients with fever. The diagnosis of pharyngitis is justified only when the pharynx is objectively redder than the rest of the mucous membranes. nine0005
The diagnosis of pharyngitis is justified only when the pharynx is objectively redder than the rest of the mucous membranes. nine0005
What could be the causes of a sore throat?
Most often, sore throats are caused by viruses. Less commonly, sore throats occur due to bacterial infections. Viral pathogens such as coronovirus, rhinovirus, adenovirus, influenza and parainfluenza are the most common and usually present as the common cold. Other viral infections that can present with sore throats are the Epstein-Barr virus and HIV, which cause sore throats early in the course of the disease.
Recurrent angina may be due to cytomegalovirus or fungal infections in immunocompromised young patients.
Group A beta-hemolytic streptococcus (GABHS) is the most common cause of bacterial angina among bacterial infections. It accounts for 15–36% of cases of acute pharyngitis in children in developed industrial countries. Streptococcus types C and G may be other pathogens.
Streptococcus types C and G may be other pathogens.
More rare causes of sore throat include infection with Staphylococcus aureus, Mycoplasma, Chlamydia pneumoniae, Moraxella catarrhalis, and Yersinia. nine0005
Fusobacterium necrophorum infection is an uncommon infection that begins with fever and sore throat and can subsequently develop into Lemierre's syndrome, which is characterized by blood poisoning, internal jugular vein thrombosis, and at least one metastatic infection.
Another group of causes of sore throat in children are peritonsillar, pharyngeal and lateral pharyngeal abscesses, which occur due to the spread of infection from local sources, such as bacterial tonsillitis. Along with fever and sore throat, other symptoms may be present in these cases, such as painful swallowing, drooling, trismus, visible swelling under the lower jaw, and deviation of the uvula away from the inflammation. nine0005
Sore throats can also be caused by allergies, especially when complicated by nasal bleeding. Irritants such as dust, tobacco and stove smoke, and chemical air pollutants can lead to chronic sore throats.
Irritants such as dust, tobacco and stove smoke, and chemical air pollutants can lead to chronic sore throats.
Prolonged conversation in raised tones, shouting for a long time also lead to sore throat.
Sore throat can also occur due to damage to the larynx by gastric juice in gastroesophageal reflux disease (GERD). nine0005
What signs of the disease are assessed by the doctor?
When taking a history of examining a child, the doctor will pay attention to the following symptoms:
- Onset and duration of sore throat
- Severity of fever
- Associated cough, runny nose, conjunctivitis, headache, myalgia (muscle pain)
- Any difficulty in breathing, especially nighttime snoring or stridor
- History of rash, diarrhea or allergy nine0040 Regurgitation (reflux of gastric contents into the esophagus), pain in the epigastric or retrosternal region.
- Family history of sore throat in the last 2 weeks.
- Similar complaints in the past,
- Vaccination history

When examining the throat, a doctor may notice:
- White or gray deposits on the surface of the tonsils or pharynx that are easily rubbed off without bleeding.
- Ulcerations
- Film-like plaques characteristic of infectious mononucleosis, diphtheria, and sometimes streptococcal infections. Tularemia can also be a rare cause of such raids. nine0041
- Films of gray or black color, extending beyond the tonsils, with swallowing disorders and the absence of severe fever, are characteristic of diphtheria.
- Oral thrush, which is common in newborns and infants, may have a pseudomembrane (cheesy plaques), removal of which can cause mild pinpoint bleeding.
- Oropharyngeal bulge or uvula lateral displacement indicates a parapharyngeal or peritonsillar abscess. nine0041
- Herpetic sore throat is characterized by painful vesicular (bubbly) formations on the pharynx and tonsils.
 Herpes simplex develops painful blisters limited to the front of the mouth, which can sometimes spread to the front of the tonsils.
Herpes simplex develops painful blisters limited to the front of the mouth, which can sometimes spread to the front of the tonsils. - Lymphadenopathy (enlarged and painful anterior and posterior cervical lymph nodes are characteristic of bacterial tonsillitis or Epstein-Barr virus infection.
- Streptococcal pharyngitis is characterized by sore throat, fever ≥38.3°C, plaque on the tonsils and pharynx, and cervical lymphadenopathy. nine0041
- Cough, runny nose and diarrhea are more common in viral pharyngitis.
Still have questions?
Get an online consultation from leading pediatricians Petersburg!
A professional and experienced pediatrician will answer your questions.
Medical care for a child without leaving home at a convenient time.
book a consultation
A Skype consultation lasts 45 minutes.
Additional tests for sore throat
The main problem in diagnosing sore throat is not to miss the dangerous diagnoses of diphtheria and GABHS angina. For this, a throat swab is taken from the child for bacterial and culture, including Albert stain for diphtheria. A provisional diagnosis of diphtheria is suggested if typical tympanic bacillus organisms are found in the smear. However, definitive diagnosis requires confirmation of growth of C. diphtherium in culture.
For this, a throat swab is taken from the child for bacterial and culture, including Albert stain for diphtheria. A provisional diagnosis of diphtheria is suggested if typical tympanic bacillus organisms are found in the smear. However, definitive diagnosis requires confirmation of growth of C. diphtherium in culture.
For the diagnosis of GABHS angina, there are antigen rapid tests. Their action is based on the extraction of group A carbohydrate antigen from throat swab materials with nitrous acid. These rapid tests are very specific (> 95%) and give immediate results but have variable sensitivity. Confirmation of a positive result is not required, and if negative, culture is recommended to exclude an infection dangerous for the child. A streptococcal antibody titer is not useful in diagnosing strep pharyngitis and is not usually recommended.
Other tests:
- Complete blood count
- Peripheral blood smears - for the presence of atypical lymphocytes.

- Epstein-Barr virus serology (IgM antibodies)
- X-ray of the soft tissues of the neck (lateral view) in case of suspected retropharyngeal abscess.
- CT scan of the neck, including the base of the skull, for an abscess.
Treating a child with sore throat
Prescriptions must be made by a doctor based on the established diagnosis and identified or suspected pathogen. Self-administration of drugs by parents is unacceptable. This can lead to serious consequences for the health of the child.
GABHS farnigitis is a disease that resolves on its own. However, antibiotic treatment in this case provides rapid relief of symptoms, prevents purulent (otitis media, sinusitis, tonsillitis) and non-suppurative complications, and also reduces the possibility of infection transmission. Antibiotics reduce the incidence of rheumatic fever by more than two-thirds.
Clinical features, epidemiological criteria, and judgment by an experienced clinician, with or without additional evaluation, usually indicate the need for antibiotics. The currently used score for decision making in pharyngitis has been adapted by adding age to the four components of the original Centor score (no cough, swollen and painful anterior cervical nodes, temperature >38°C, tonsil plaque or swelling. Each component is given 1 point. For age 3 to 14 years is also given a score of 1. Children or adolescents with a score of 0 or 1 do not require antibiotic therapy. scores of 4 or higher are at high risk for streptococcal GABHS pharyngitis and should receive antibiotic therapy.
The currently used score for decision making in pharyngitis has been adapted by adding age to the four components of the original Centor score (no cough, swollen and painful anterior cervical nodes, temperature >38°C, tonsil plaque or swelling. Each component is given 1 point. For age 3 to 14 years is also given a score of 1. Children or adolescents with a score of 0 or 1 do not require antibiotic therapy. scores of 4 or higher are at high risk for streptococcal GABHS pharyngitis and should receive antibiotic therapy.
Due to cost, narrow spectrum, safety and efficacy, penicillin is the drug of choice. A shorter duration of treatment increases the risk of bacteriological recurrence of the disease. The unreasonable use of macrolides for the treatment of GABHS pharyngitis has become the main reason for the formation of resistant strains of pathogens.
What can parents do to relieve their child's sore throat?
Here are some simple ways children can help relieve sore throats:
- Drink warm liquids
- Have cold or frozen liquids (eg sorbet or ice cream)
- Gargle with salt water
- Suck throat lozenges (for children aged 4 and over)
- Give the child ibuprofen or acetaminophen as needed
When should I see a doctor urgently?
Seek immediate medical attention if the child:
- has trouble swallowing
- does not drink liquids
- drooling
- extremely lethargic
- Pus is visible in the back of the throat
- severe sore throat lasting longer than a few days
Do not self-medicate. Beautiful and saving from “everything in the world” medicines from advertisements in cute jars (with “bears and bunnies”) are not the best solution if the diagnosis is not clear. Medicines for the child should be prescribed by a doctor. Especially antibiotics.
Beautiful and saving from “everything in the world” medicines from advertisements in cute jars (with “bears and bunnies”) are not the best solution if the diagnosis is not clear. Medicines for the child should be prescribed by a doctor. Especially antibiotics.
Seeing a doctor about a sore throat in a child is not a whim, but a necessity. We are always happy to help. The sooner your child gets the right treatment, the less chance of complications.
Call a doctor at home To make an appointment with a doctor or call +7 (812) 331-17-74
Sore throat: top 5 ways to help yourself
Sore throat often comes on suddenly: you wake up in the morning and swallow with difficulty. We will figure out where to start treatment and how not to start the disease. nine0005
Symptoms and causes
We call everything with the same phrase “sore throat”, but in reality we experience different sensations. Symptoms of discomfort vary depending on the cause or pathogen. Doctors refer to the most common:
Doctors refer to the most common:
- feeling of "scratching" and "tingling" in the throat
- worsening pain when swallowing, talking
- swollen tonsils
- redness of the posterior wall of the larynx
- enlarged lymph nodes on palpation
Causes of discomfort are often:
- colds
- influenza
- viruses and bacteria
- allergy
- dry air
- smoking, including passive smoking
- loud talking and shouting, for example, at a concert of your favorite band
The good news is that most sore throats can resolve within 5-10 days [1]. Our body copes with the disease by producing antibody proteins. Simply provide yourself with home supportive care that will ease the onset of symptoms. nine0005
Helping ourselves at home
Method One: Drink plenty of fluids.
Cranberry juice, herbal tea, water, lemon tea.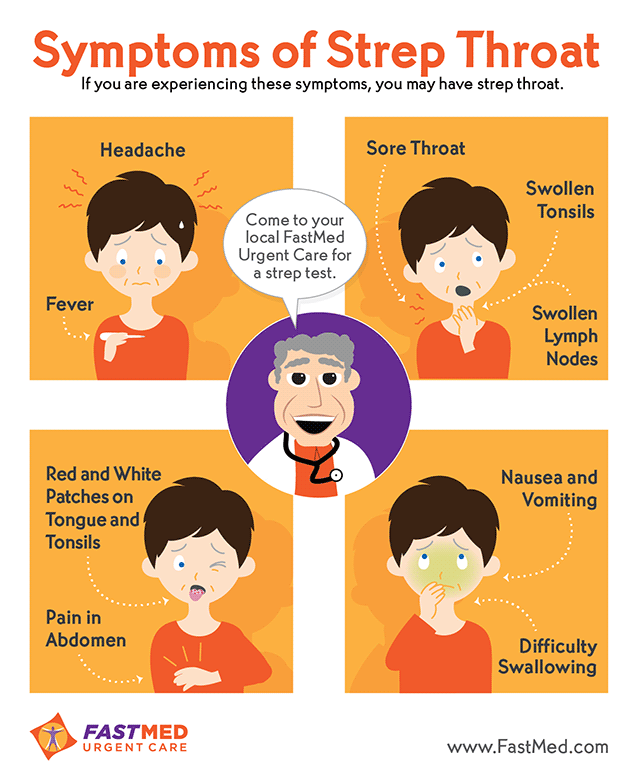 Drinks reduce the intoxication of the body and accelerate the elimination of viruses if they caused pain.
Drinks reduce the intoxication of the body and accelerate the elimination of viruses if they caused pain.
Second method: gargle.
Prepare yourself a sage decoction or add a teaspoon of propolis tincture to half a glass of warm water - the procedure will relieve swelling and inflammation. You will not see the effect immediately, but it is important to continue treatment for several days so that the sore throat goes away. nine0005
Method three: tie a scarf around your throat.
A very kind way to show your throat that you care about it. A scarf keeps warmth around your neck and can distract you from pain. But there is a small caveat - with angina, all warming procedures can be carried out only with the permission of a doctor.
Method four: increase the humidity in the room.
This can be done even without a humidifier. Hang a wet towel on the battery, place water containers around the apartment. nine0005
nine0005
Method five: take painkillers.
Topical non-steroidal anti-inflammatory drugs such as benzydamine reduce pain and inflammation in tonsillitis and pharyngitis. This restores the ability to talk and makes it easier to swallow food.
When to see a specialist
If you have a severe sore throat, you should still see a doctor. Medical treatment is needed if you experience any of the following symptoms:
- labored breathing
- difficulty opening the mouth
- temperature above 38.3 °C
- lump in throat
- blood present in saliva
- ear pain
Preparations with benzamidine are useful in the complex treatment of the disease. One of these is Angidak Forte from Solopharm. It combines three actions at once: analgesic, anti-inflammatory and antiseptic. It also helps relieve sore throat from the first minute [3,4]. More information about "Angidaka" and other forms of release can be found here.