Milk sensitivity in infants
What should I do if I think my baby is allergic or intolerant to cows' milk?
If you think your baby is having a reaction to cows' milk, see your GP or health visitor to discuss your concerns.
They will be able to assess if your baby's symptoms may be caused by a cows' milk allergy or something else. Make sure you get medical advice before taking cows' milk out of your child's diet as it contains important nutrients.
Cows' milk allergy in babies
Cows' milk allergy (CMA), also called cows' milk protein allergy, is one of the most common childhood food allergies. It is estimated to affect around 7% of babies under 1, though most children grow out of it.
CMA typically develops when cows' milk is first introduced into your baby's diet either in formula or when your baby starts eating solids.
More rarely, it can affect babies who are exclusively breastfed because of cows' milk from the mother's diet passing to the baby through breast milk.
There are 2 main types of CMA:
- immediate CMA – where symptoms typically begin within minutes of having cows' milk
- delayed CMA – where symptoms typically begin several hours, or even days, after having cows' milk
Symptoms of cows' milk allergy
Cows' milk allergy can cause a wide range of symptoms, including:
- skin reactions – such as an itchy rash or swelling of the lips, face and around the eyes
- digestive problems – such as stomach ache, vomiting, colic, diarrhoea or constipation
- hay fever-like symptoms – such as a runny or blocked nose
- eczema that does not improve with treatment
Occasionally CMA can cause severe allergic symptoms that come on suddenly, such as swelling in the mouth or throat, wheezing, cough, shortness of breath, and difficult, noisy breathing.
A severe allergic reaction (anaphylaxis) is a medical emergency. Call 999 for an ambulance immediately if you think your child has anaphylaxis (even if they start to feel better).
Treatment for CMA
If your baby is diagnosed with CMA, you'll be offered advice by your GP or an allergy specialist on how to manage their allergy. You may also be referred to a dietitian.
Treatment involves removing all cows' milk from your child's diet for a period of time.
If your baby is formula-fed, your GP can prescribe special infant formula.
Do not give your child any other type of milk without first getting medical advice.
If your baby is exclusively breastfed, the mother will be advised to avoid all cows' milk products.
Your child should be assessed around every 6 to 18 months to see if they have grown out of their allergy.
Read more about cows' milk allergy in children on National Institute for Health and Care Excellence (NICE).
Could it be lactose intolerance?
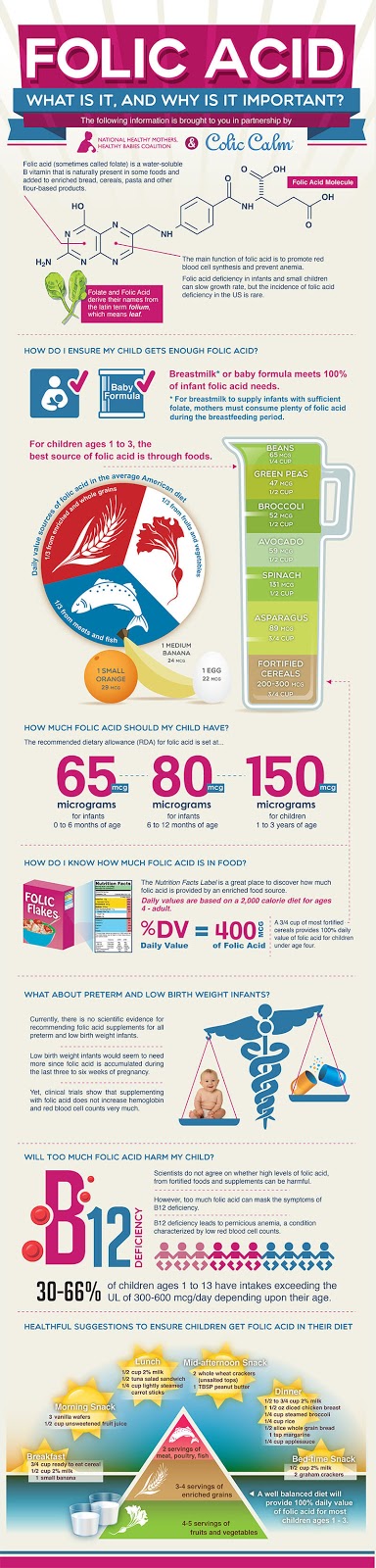
Lactose intolerance is another type of reaction to milk, when the body cannot digest lactose, a natural sugar found in milk. However, this is not an allergy.
Lactose intolerance can be temporary – for example, it can come on for a few days or weeks after a tummy bug.
Symptoms of lactose intolerance include:
- diarrhoea
- vomiting
- stomach rumbling and pains
- wind
Treatment for lactose intolerance
Treatment depends on the extent of your child's intolerance. Some children with lactose intolerance may be able to have small amounts of dairy products without having symptoms.
Your child may be referred to a dietitian for specialist advice.
Read more about treatment for lactose intolerance.
Further information:
- Colic
- Food allergies in babies and children
- Reflux in babies
- How can I tell if my baby is seriously ill?
- Your baby's first solid foods
- National Institute for Health and Care Excellence (NICE): food allergy in children
Page last reviewed: 28 November 2022
Next review due: 28 November 2025
Milk Allergy in Infants (for Parents)
What Is a Milk Allergy?
When a baby is allergic to milk, it means that his or her immune system, which normally fights infections, overreacts to proteins in cow's milk. Every time the child has milk, the body thinks these proteins are harmful invaders and works hard to fight them. This causes an allergic reaction in which the body releases chemicals like
This causes an allergic reaction in which the body releases chemicals like
histamine.
Cow's milk is in most baby formulas. Babies with a milk allergy often show their first symptoms days to weeks after they first get cow milk-based formula. Breastfed infants have a lower risk of having a milk allergy than formula-fed babies.
People of any age can have a milk allergy, but it's more common in young children. Many kids outgrow it, but some don't.
If your baby has a milk allergy, keep two epinephrine auto-injectors on hand in case of a severe reaction (called anaphylaxis). An epinephrine auto-injector is an easy-to-use prescription medicine that comes in a container about the size of a large pen. Your doctor will show you how to use it.
What Are the Signs & Symptoms of a Milk Allergy?
In children who show symptoms shortly after they have milk, an allergic reaction can cause:
- wheezing
- trouble breathing
- coughing
- hoarseness
- throat tightness
- stomach upset
- vomiting
- diarrhea
- itchy, watery, or swollen eyes
- hives
- swelling
- a drop in blood pressure causing lightheadedness or loss of consciousness
The severity of allergic reactions to milk can vary. The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
The same child can react differently with each exposure. This means that even though one reaction was mild, the next could be more severe and even life-threatening.
Children also can have:
- an intolerance to milk in which symptoms — such as loose stools, blood in the stool, refusal to eat, or irritability or colic — appear hours to days later
- lactose intolerance, which is when the body has trouble digesting milk
If you're not sure if your child has an intolerance versus an allergy, talk to your doctor.
If Your Child Has an Allergic Reaction
If your child has symptoms of an allergic reaction, follow the food allergy action plan your doctor gave you.
If your child has symptoms of a serious reaction (like swelling of the mouth or throat or difficulty breathing, or symptoms involving two different parts of the body, like hives with vomiting):
- Give the epinephrine auto-injector right away. Every second counts in an allergic reaction.

- Then, call 911 or take your child to the emergency room. Your child needs to be under medical supervision because, even if the worst seems to have passed, a second wave of serious symptoms can happen.
How Is a Milk Allergy Diagnosed?
If you think your infant is allergic to milk, call your baby's doctor. He or she will ask you questions and talk to you about what's going on. After the doctor examines your baby, some stool tests and blood tests might be ordered. The doctor may refer you to an allergist (a doctor who specializes in treating allergies).
The allergist might do skin testing. In skin testing, the doctor or nurse will place a tiny bit of milk protein on the skin, then make a small scratch on the skin. If your child reacts to the allergen, the skin will swell a little in that area like an insect bite.
If the allergist finds that your baby is at risk for a serious allergic reaction, epinephrine auto-injectors will be prescribed.
Avoiding a Milk Allergy Reaction
If You're Breastfeeding
If your breastfed infant has a milk allergy, talk to the allergist before changing your diet.
If You're Formula Feeding
If you're formula feeding, your doctor may advise you to switch to an extensively hydrolyzed formula or an amino acid-based formula in which the proteins are broken down into particles so that the formula is less likely to trigger an allergic reaction.
You also might see "partially hydrolyzed" formulas, but these aren't truly hypoallergenic and can lead to a significant allergic reaction.
If you're concerned about a milk allergy, it's always best to talk with your child's doctor and work together to choose a formula that's safe for your baby.
Do not try to make your own formula. Commercial formulas are approved by the U.S. Food and Drug Administration (FDA) and created through a very specialized process that cannot be duplicated at home. Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
Other types of milk that might be safe for an older child with a milk allergy are not safe for infants.
If you have any questions or concerns, talk with your child's doctor.
Allergy to cow's milk proteins (CMP)
- Nestlé Health Science
- health care
- The concept of "Allergy to cow's milk proteins (CMP)"
The concept of cow's milk protein allergy (CMP)
What is a food allergy?
Food allergies occur when the body's immune system (the body's own defense mechanism) reacts incorrectly to certain foods. Normally, the immune system helps the body fight harmful things, such as infectious agents. In a food allergy, the immune system misrecognizes certain food components as harmful, leading to unpleasant and sometimes life-threatening allergy-related signs and symptoms. nine0017 More than 120 foods are known to cause food allergies. Cow's milk protein allergy (CMP) is the most common type of food allergy in infants under one year of age.
nine0017 More than 120 foods are known to cause food allergies. Cow's milk protein allergy (CMP) is the most common type of food allergy in infants under one year of age.
Do not confuse CMPA with lactose intolerance
Sometimes CMPA is confused with lactose intolerance. Both diseases have some common signs and symptoms, but different causes and treatments.
CMPA usually develops at an early age, while lactose intolerance is extremely rare before the age of 5 years. nine0013
What is ABKM?
CMA is a type of food allergy in which the child's immune system reacts to proteins found in cow's milk. As a result, the child develops allergy symptoms: skin problems (rash, hives, dry, flaky or itchy skin), digestive system disorders (diarrhea, vomiting, constipation and reflux) and respiratory problems (noisy breathing, cough, runny nose). CMPA usually occurs before a child's first birthday. nine0013
What is lactose intolerance?
Unlike CMPA, lactose intolerance does not depend on the immune system. This is actually lactase deficiency, the inability to digest the lactose sugar found in cow's milk, and is very rare in children under 5 years of age. Lactose is one of the most important carbohydrates (sugars) in breast milk and is very beneficial for babies. Lactose promotes healthy intestinal flora and calcium absorption. nine0013
This is actually lactase deficiency, the inability to digest the lactose sugar found in cow's milk, and is very rare in children under 5 years of age. Lactose is one of the most important carbohydrates (sugars) in breast milk and is very beneficial for babies. Lactose promotes healthy intestinal flora and calcium absorption. nine0013
Cow's milk protein allergy and lactose intolerance are different diseases
learn more about cow's milk protein allergy
All about CMPA
How common is CMPA?
Is CMPA hereditary?
Why does my child have CMPA?
Can CMPA be cured?
What is the difference between the AAA line and hypoallergenic formulas?
Your steps towards the diagnosis of CMPA
Allergy symptoms can be frightening, but CMPA can be easily managed with the right diet, so it's important to get the right diagnosis from your doctor and get treatment on time. If you notice any symptoms in your child that could be associated with CMPA, first of all, don't worry. Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA. nine0013
Discuss the problems with the doctor, the doctor will take the necessary actions to make a final diagnosis. Follow the links below for information and guidance regarding the diagnosis of CMPA and the common signs and symptoms of CMPA. nine0013
SIGNS AND SYMPTOMS OF CMPA
CMPA is a food allergy, but symptoms can affect more than just the digestive system, they can also affect the respiratory system and skin.
Learn more about the signs and symptoms of CMPA
Symptom Analysis
Diagnosis
To make a diagnosis, the doctor will examine the child and ask about any symptoms you may notice. If an allergy to cow's milk proteins is suspected, a doctor may do certain tests. Once diagnosed, the symptoms of CMPA can be easily managed under the experienced guidance of a physician. nine0013
Find out more about the diagnosis of CMDD
Get ready for your doctor's visit
Would you like some help preparing for your doctor's visit? By printing and completing My Child's Symptom Diary, you can be sure that your doctor will have all the information you need to make an accurate diagnosis.
Symptom diary
IMPORTANT NOTE: Breastfeeding may continue if the infant is allergic to cow's milk protein. To do this, the mother needs a special diet with the exclusion of all sources of cow's milk protein. Only if these measures do not bring the desired effect, the doctor recommends the use of a special therapeutic mixture intended for children from 0 to 1 year old. It is important to follow the correct methods of preparing the mixture: using boiled water, sterilized bottles and following the rules for diluting the mixture. Medicinal mixtures intended for diet therapy of CMPA should be used under the supervision of a physician. nine0013
Gluten and lactose sensitivity
Gluten and lactose intolerance are the most common digestive disorders in which the human body cannot break down foods containing grains and milk. This can be expressed by many symptoms - from mild abdominal pain and flatulence to diarrhea, abdominal cramps and bloody stools. As a rule, intolerance does not appear unexpectedly, but due to frequent and long-term use of products. nine0013
Sensitivity to gluten and lactose occurs not only in case of intolerance, but also in a number of diseases that have similar symptoms and require a thorough diagnostic approach - analysis of anamnesis, clinical and laboratory data.
Therefore, we have developed test packages in which one-stage diagnostics of all major conditions associated with sensitivity to gluten and lactose is carried out: nine0004