Placenta stuck after birth
What You Should Know About a Retained Placenta
Written by WebMD Editorial Contributors
In this Article
- Causes of a Retained Placenta
- Symptoms of a Retained Placenta
- Risks of a Retained Placenta
- Treatment for Retained Placenta
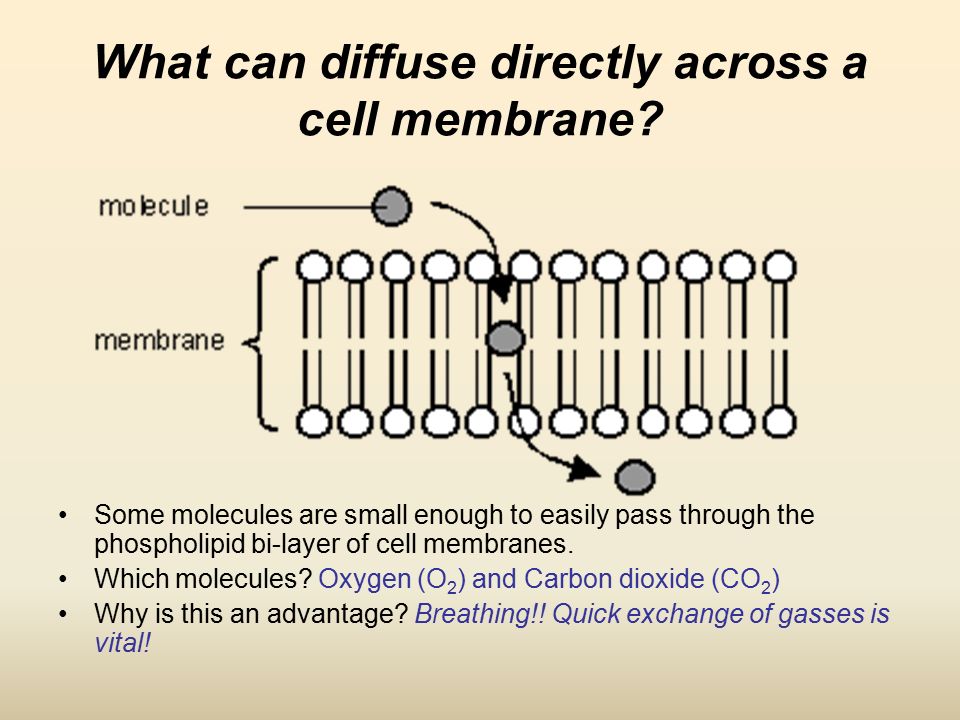
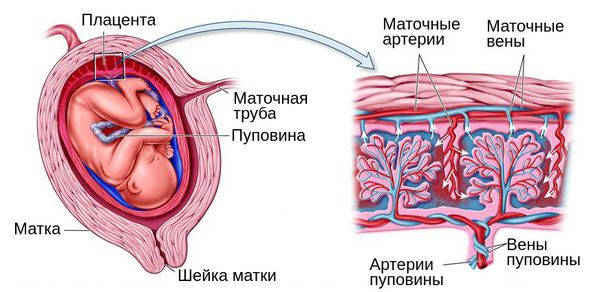
The placenta is a temporary organ that grows during pregnancy to filter oxygen, blood, and nutrients to your baby. After you give birth, you will also deliver your placenta shortly after.
Sometimes all or part of the placenta stays in the womb. This is called a retained placenta and it can have serious side effects.
Causes of a Retained Placenta
After your baby is born, you will usually deliver your placenta within 18 to 60 minutes. Your uterus contracts, which pulls the placenta away from the wall of your uterus and pushes it out. Sometimes this doesn’t happen and can be caused by different things, including:
- Not enough contractions
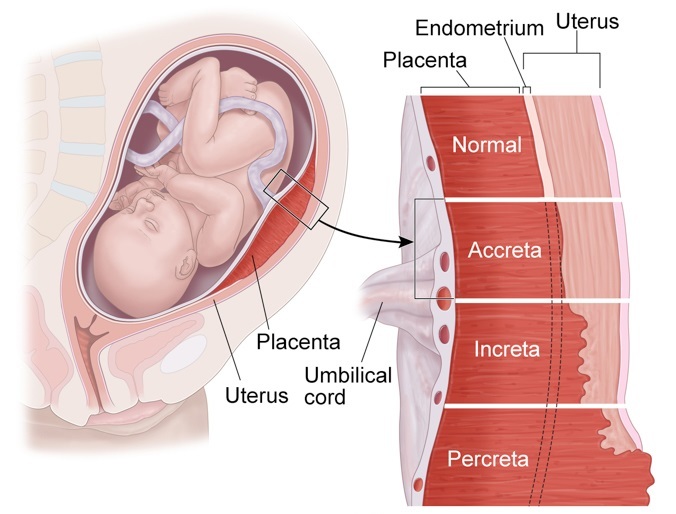
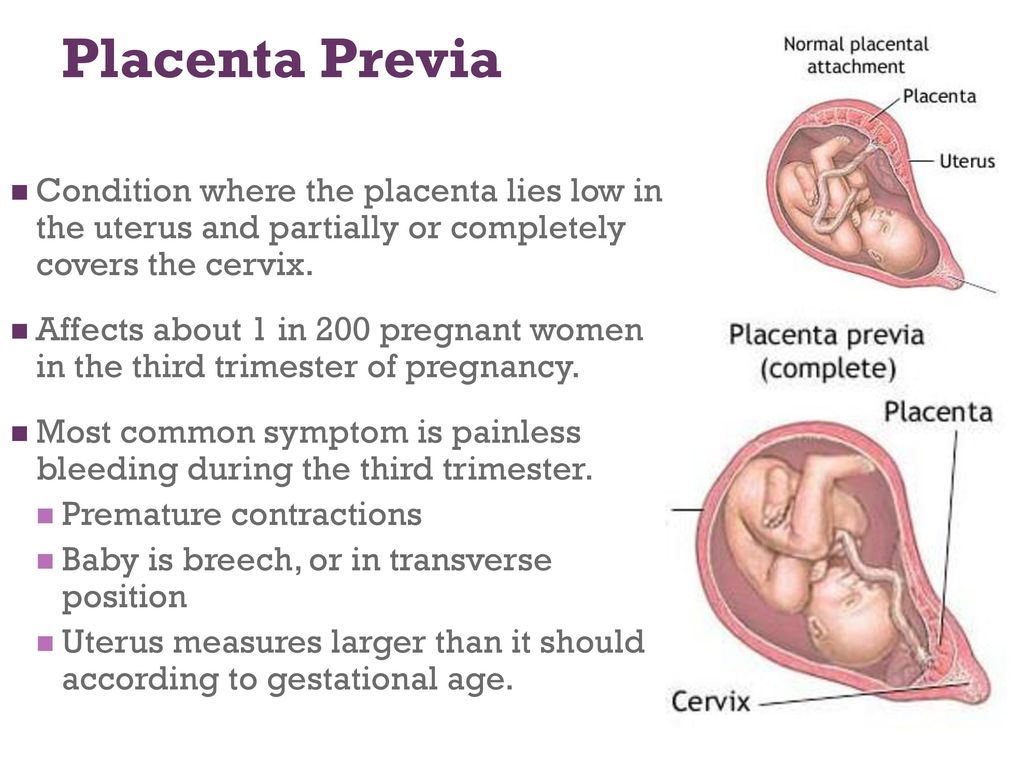
- The placenta grows into the uterus wall
- The cervix closes
- Early delivery
- Giving birth many times
- Previous surgery in the uterus
- Conceiving by in vitro fertilization
- Having a retained placenta in another pregnancy
- Being born with uterus deformities
- Having oxytocin medication for too long
The most common reason for a retained placenta is not enough contractions in the uterus. Contractions can slow down or the uterus can have trouble contracting for different reasons. These include:
- Having large babies
- Giving birth many times
- Too much oxytocin medication
- A long labor
- A fast labor
- Fibroids
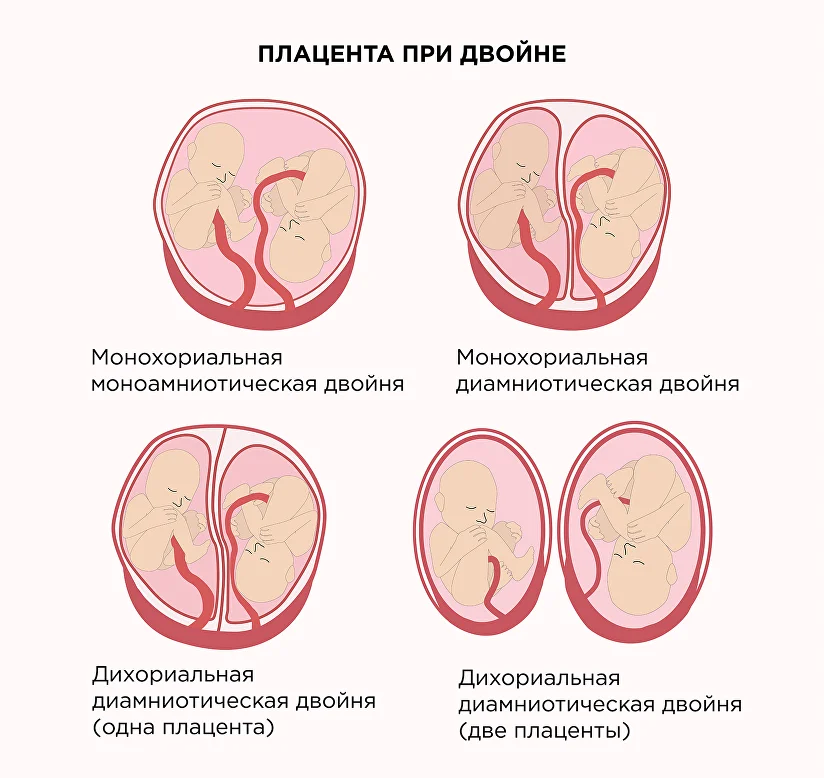
- Having twins or multiples
- Magnesium sulfate infusions
Symptoms of a Retained Placenta
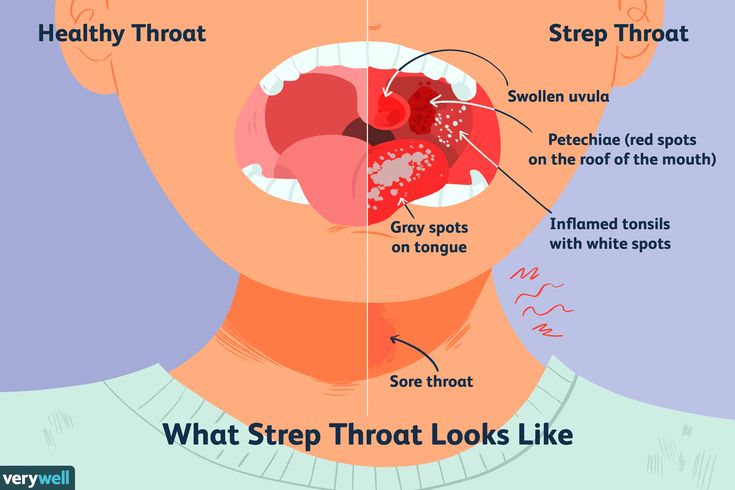
The most obvious sign of a retained placenta is that you don’t deliver it. The most common symptom of a retained placenta after birth is sudden blood loss and life-threatening bleeding.
At times you might push out most of it, however, some pieces of the placenta can be stuck inside. This can cause symptoms that take a while to show up such as:
- Delayed and heavy bleeding
- Blood clots
- Fever
- Chills
- Feeling sick or flu-like
- Foul-smelling vaginal discharge
If you have heavy bleeding and blood clots at home, make sure to keep your pads and show them to your doctor right away. They may want to check for placenta tissue.
They may want to check for placenta tissue.
Risks of a Retained Placenta
Most women safely deliver the placenta after having a baby, but sometimes it can stay inside the womb. This can cause serious side effects.
Life-threatening bleeding. If your placenta is not delivered, it can cause life-threatening bleeding called hemorrhaging.
Infection. If the placenta, or pieces of the placenta, stay inside your uterus, you can develop an infection.
A retained placenta or membrane has to be removed and you will need to see your doctor right away. If you have major bleeding, this is a medical emergency and you should go to your nearest hospital immediately.
Treatment for Retained Placenta
Some conditions can make it more likely that your uterus won’t contract properly. This can lead to a retained placenta. Your doctor will carefully check your medical history and consider how many births you’ve had and what kind of births.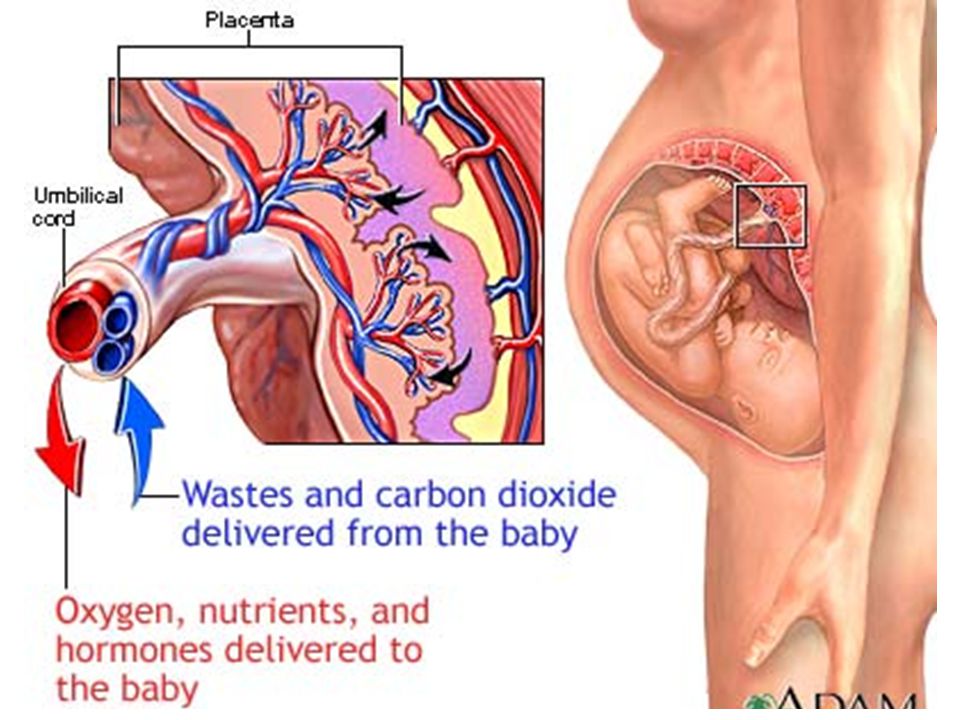 They might make plans during your pregnancy that can help ensure you won't have a retained placenta or prepare for retained placenta treatment.
They might make plans during your pregnancy that can help ensure you won't have a retained placenta or prepare for retained placenta treatment.
Your doctor or midwife will also usually ask you to do a few things right after giving birth that can help prevent a retained placenta.
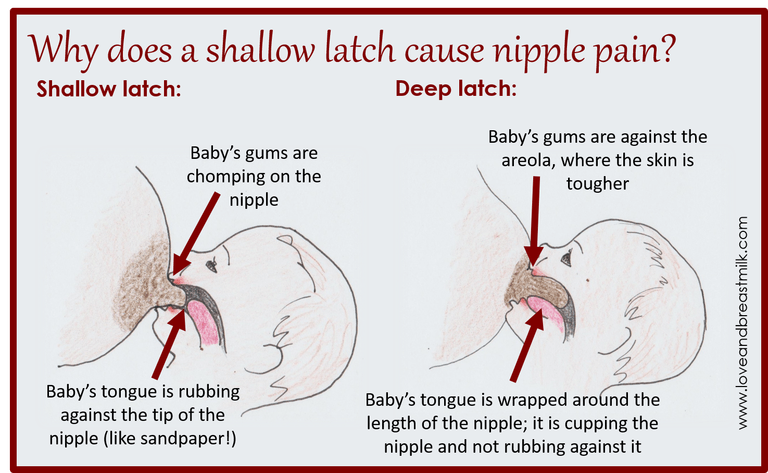
Breastfeeding. Your doctor, midwife, or nurse will likely ask you to start breastfeeding your baby as soon as possible after you give birth. This is because breastfeeding makes your uterus contract and is a natural process that will help prevent a retained placenta.
Changing positions. Your doctor might ask you to roll to the side or to squat. Changing positions can help your uterus contract and push out your placenta.
Massage. After delivery, your doctor might massage your abdomen to help it contract. This can feel uncomfortable but can be helpful. Abdominal massage is often used after your second birth. This is because your uterus might not contract very well if you’ve had several births.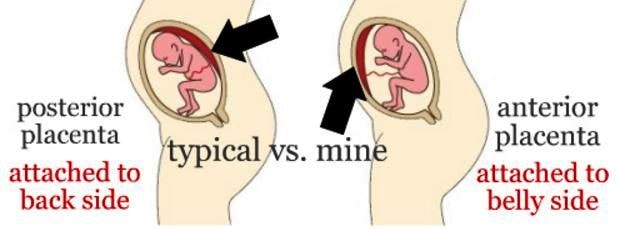
Medication. If these methods don’t work, your doctor might give you a shot of medicine that will make the uterus contract and help you deliver your placenta.
Manual removal. If your doctor diagnoses you with a retained placenta, they may want to remove the placenta by hand. They will often try another method first. Your doctor will give you an epidural or anesthetic medicine and manually separate the placenta inside the uterus.
Surgery. If massage, medication, or other options don’t work, your doctor might decide to do surgery. You will have an operation to safely remove the placenta. If the placenta has grown into the uterus wall and invaded other tissues, you may need to have your uterus removed.
Having surgery or a manual placenta removal can have risks, including infection and life-threatening bleeding. It can also cause endometritis, which is inflammation in the uterine lining. Your doctor may give you antibiotics to help stop infection and endometritis.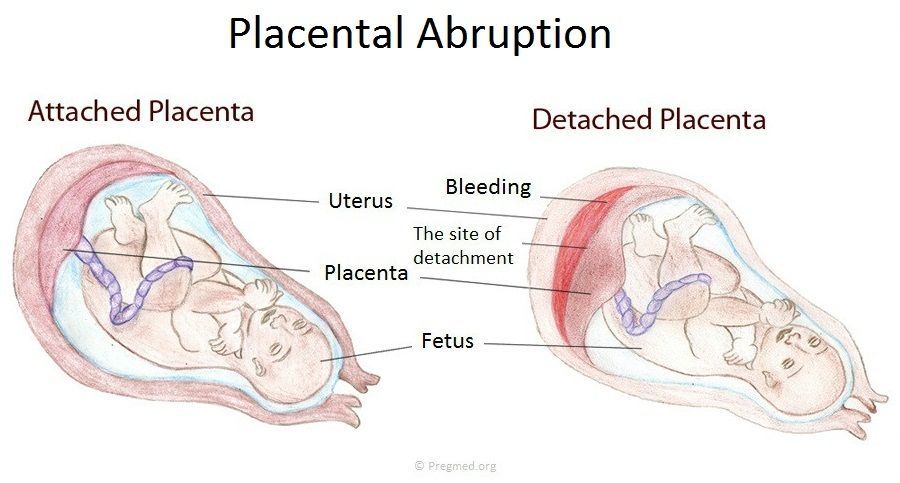
A retained placenta is not very common, but it can happen. Part of giving birth to a baby is also pushing out your placenta and your doctor will closely watch for it to come.
Retained placenta | Pregnancy Birth and Baby
Retained placenta | Pregnancy Birth and Baby beginning of content6-minute read
Listen
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
What is retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.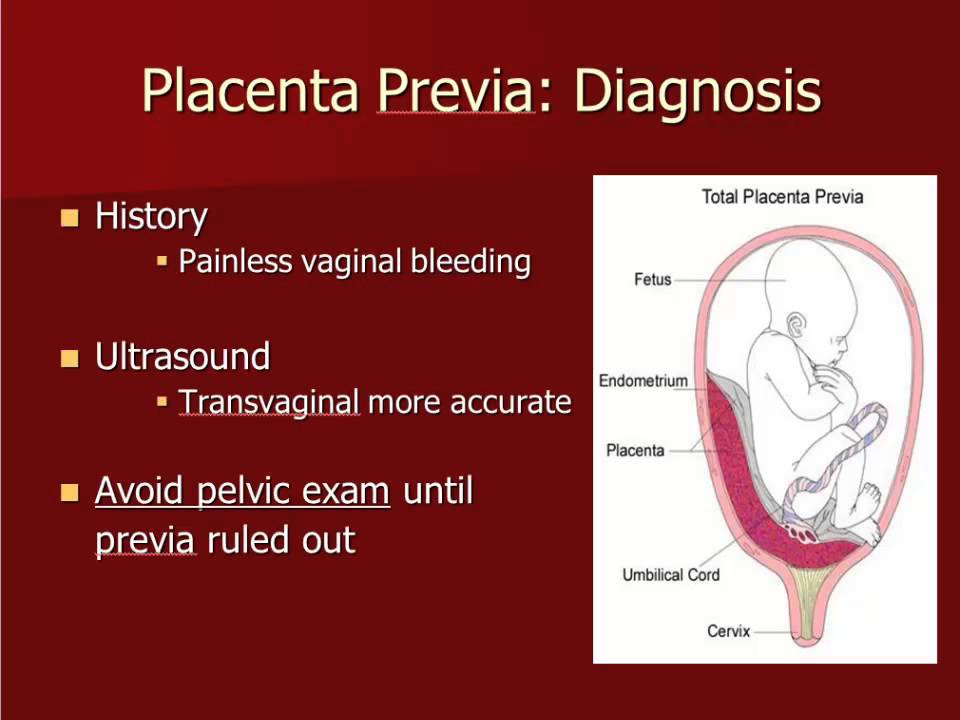
Sometimes, a piece of the placenta is left behind in the uterus (womb). It’s not common, but it can be serious. It can cause problems days or weeks after the birth.
Retained placenta can lead to severe infection or life-threatening blood loss for the mother.
How is the placenta delivered after birth?
After your baby is born, the placenta also needs to be delivered. This is called the third stage of labour.
You may choose to ‘actively manage’ this stage of labour. Meaning that you will receive an injection of Syntocinon (a synthetic version of the hormone oxytocin) to help your uterus contact and birth the placenta. Actively managing your 3rd stage of labour can take up to 30 minutes. This also helps reduce the risk of heavy bleeding from the vagina (called postpartum haemorrhage).
Some women choose not to have the oxytocin injection. This is called ‘expectant management’ or ‘physiological management of the third stage’. It means waiting for the placenta to be born naturally, usually with gravity and some contractions.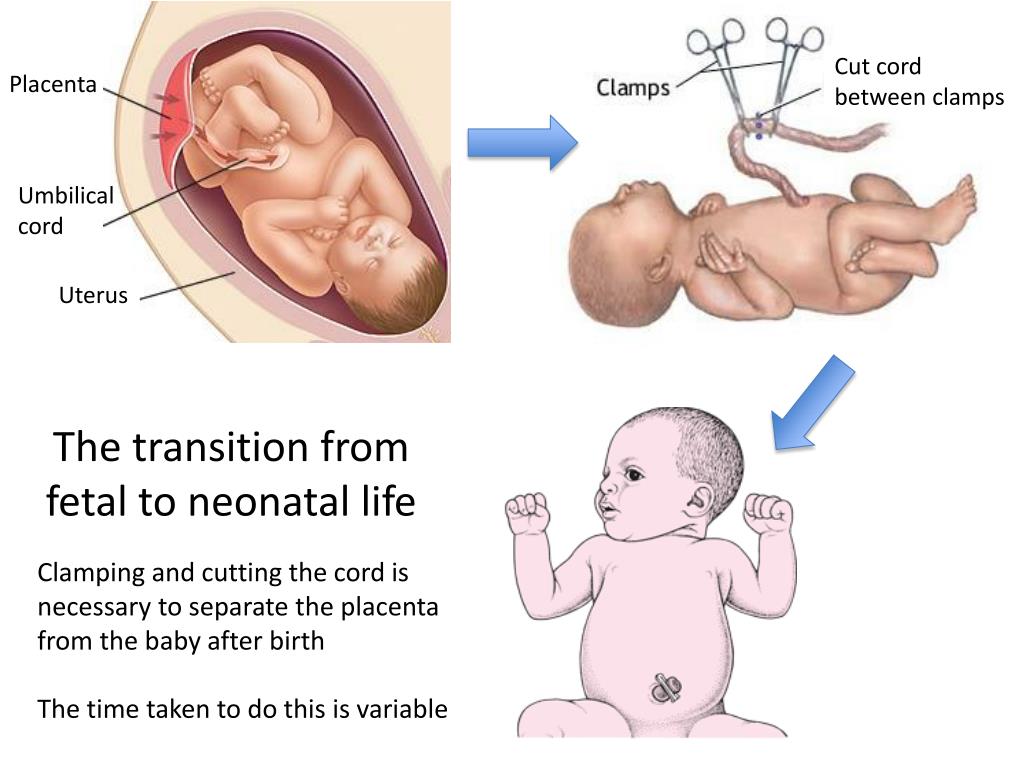 This may take up to one hour.
This may take up to one hour.
It’s important to make an informed decision by discussing the options with your midwife or doctor. You may choose to write your preferences in a birth plan.
What causes retained placenta?
Sometimes the placenta takes longer than expected to be delivered. The placenta can be retained after your baby is born if:
- your contractions aren’t strong enough to expel it
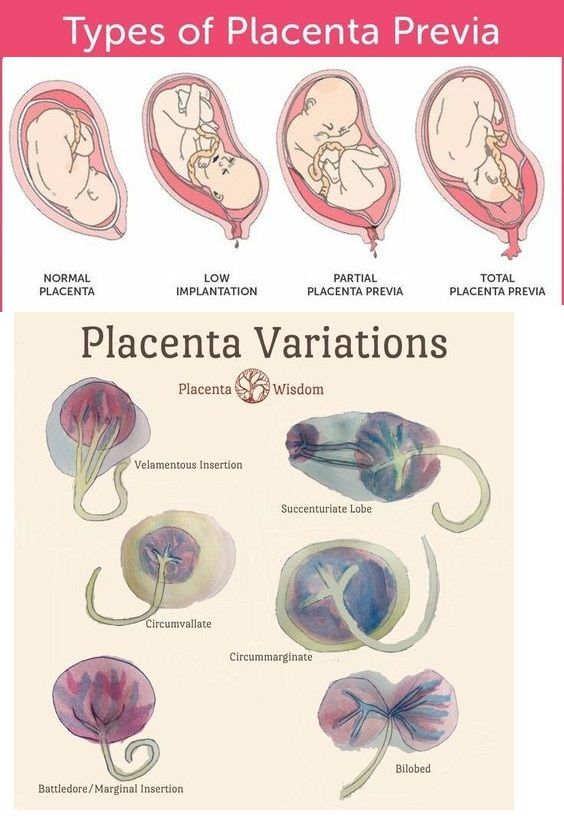
- the placenta is unusually strongly attached to the wall of the uterus
- you have placenta accreta (when the placenta implants too deeply into the wall of the uterus)
- the cervix closes and traps the placenta inside your uterus
What are the signs and symptoms of retained placenta?
Retained placenta is when the placenta doesn’t completely come out of the uterus after the baby is born.
Sometimes a piece of placenta is left behind in the uterus. If this happens, you may develop symptoms days or weeks after the birth.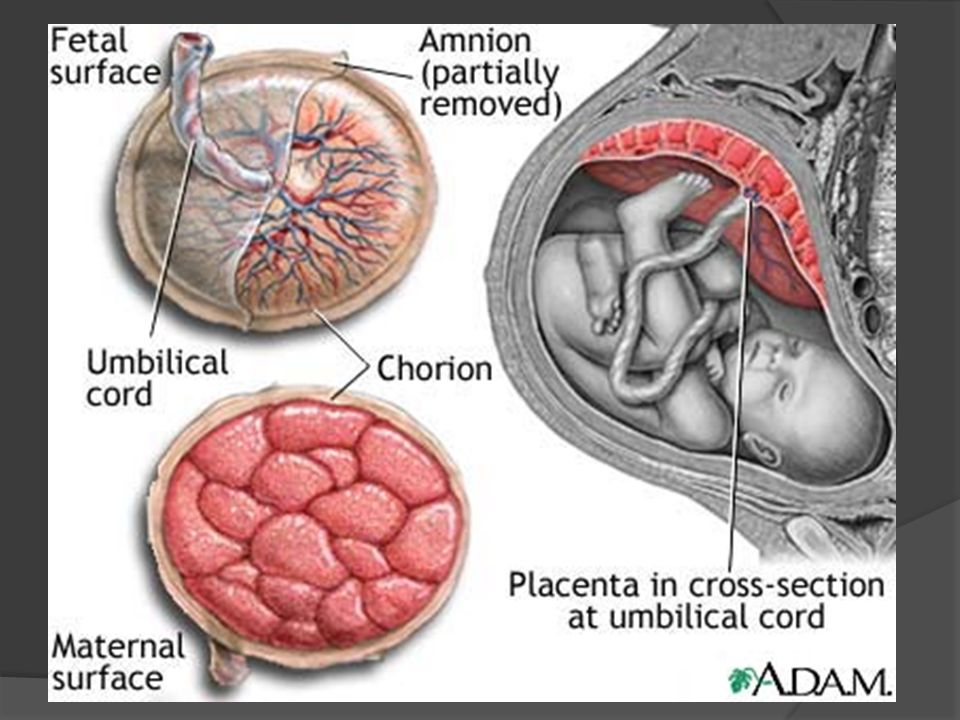 These may include:
These may include:
- fever
- a bad smelling discharge from the vagina
- heavy bleeding
- large pieces of tissue coming out of the vagina
- pain
It’s important to contact your doctor or medical team as soon as possible if you have any heavy bleeding from your vagina and/or pain in the days or weeks following birth.
If the bleeding and/or pain become significantly worse, call an ambulance on triple zero (000). Or go to your nearest hospital emergency department.
How is retained placenta diagnosed?
Your doctor or midwife will diagnose retained placenta if the placenta hasn’t completely come out of the uterus within 30 minutes - if you are actively manage or 1 hour - if you choose physiological management, after a vaginal birth.
At every birth, the midwife or doctor checks the placenta once it’s delivered. This is to check that none has been left in the uterus. But it is not always obvious if a small amount of tissue has been left behind.
If you have symptoms of retained placenta in the days or weeks after birth, your doctor may suspect that a piece of the placenta has been left behind. They may recommend an ultrasound scan. This is to check whether you have any retained placenta.
What is the treatment for retained placenta?
If you have just given birth, retained placenta might be treated by:
- emptying your bladder
- your doctor or midwife gently pulling on the umbilical cord.
If that doesn’t work, you will need a procedure to remove the placenta. You will be taken into surgery after the birth and given an epidural or anaesthetic so you don’t feel anything.
While you’re waiting for surgery, the medical team will keep a close eye on you to check you're not bleeding heavily (postpartum haemorrhage). The procedure itself is quick, but you will need to be monitored for several hours afterwards to make sure you are not bleeding.
It’s not always obvious after the placenta has been delivered that some placenta tissue may have been left behind.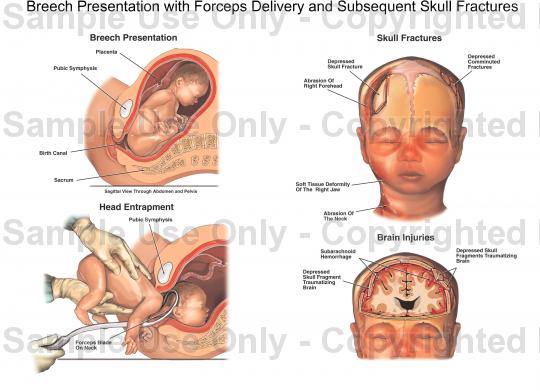 If you are bleeding heavily in the days or weeks after birth, you may need imaging tests or surgery to investigate the cause.
If you are bleeding heavily in the days or weeks after birth, you may need imaging tests or surgery to investigate the cause.
If you have an infection, you will need treatment with antibiotics.
What are the complications of a retained placenta?
Retained placenta can be serious. In rare cases, it can lead to life-threatening infection or blood loss (postpartum haemorrhage).
While there is usually some normal blood loss with birth, blood loss associated with retained placenta can be very severe. This is because the area in the uterus where the placenta is still attached can continue to bleed.
Postpartum haemorrhage can be divided into:
- primary postpartum haemorrhage – this happens within the first 24 hours after delivery
- secondary postpartum haemorrhage – this happens in the days and weeks following birth (between 24 hrs and 6 weeks after birth)
Diagnosing and managing retained placenta early helps prevent complications such as severe blood loss and infection.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
The Royal Women’s Hospital (Postpartum Haemorrhage), Government of Western Australia NMHS Health (Labour: Third Stage), International Journal of Women's Health (Retained placenta after vaginal delivery: risk factors and management), Cochrane Database of Systematic Reviews (Active versus expectant management for women in the third stage of labour), RANZCOG (Management of Postpartum Haemorrhage PPH)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: July 2022
Back To Top
Related pages
- Placenta complications in pregnancy
- About the placenta
Need more information?
Labour complications
Even if you’re healthy and well prepared for childbirth, there’s always a chance of unexpected problems.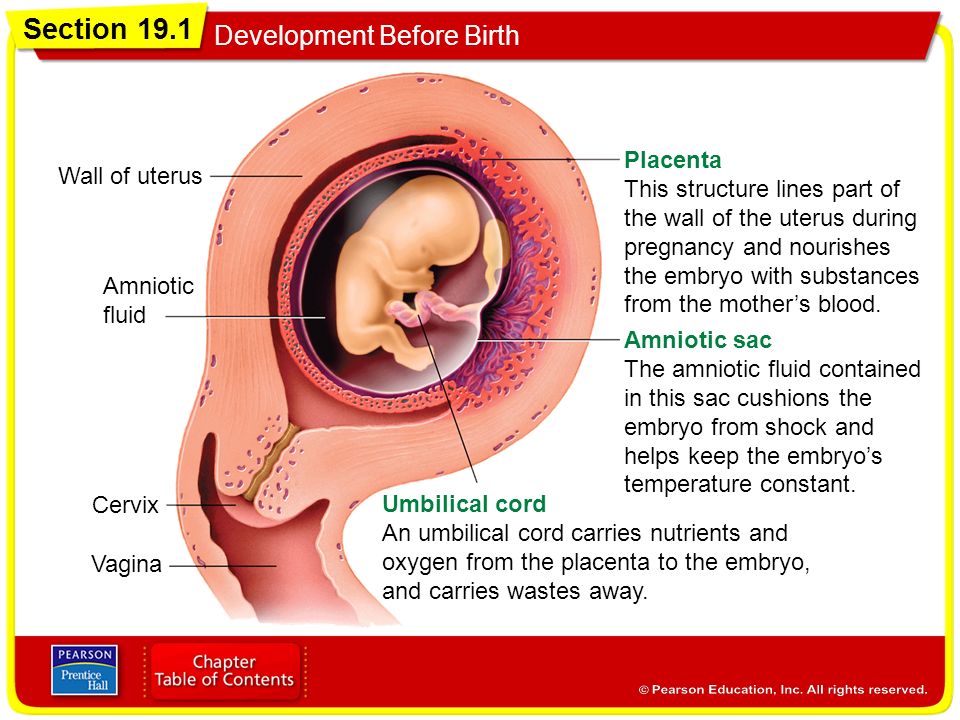 Learn more about labour complications.
Learn more about labour complications.
Read more on Pregnancy, Birth & Baby website
Asherman Syndrome
Read more on RANZCOG - Royal Australian and New Zealand College of Obstetricians and Gynaecologists website
Why do some mums stop breastfeeding before 6 months?
Most new parents know 'breast is best', but while more than 9 out of 10 babies are breastfed at birth, few mums are breastfeeding exclusively 5 months later.
Read more on Pregnancy, Birth & Baby website
What is freebirth?
Freebirth is when a woman chooses to birth her baby without medical or midwifery assistance, but this greater independence comes with some risks.
Read more on Pregnancy, Birth & Baby website
About the placenta
The placenta develops inside the uterus (womb) during pregnancy. It gives your baby nutrients and oxygen. Find out more about the placenta here.
Read more on Pregnancy, Birth & Baby website
Postpartum haemorrhage
Postpartum haemorrhage is when you bleed more than normal after giving birth. It can be very serious and requires medical attention right away.
Read more on Pregnancy, Birth & Baby website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
Need further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.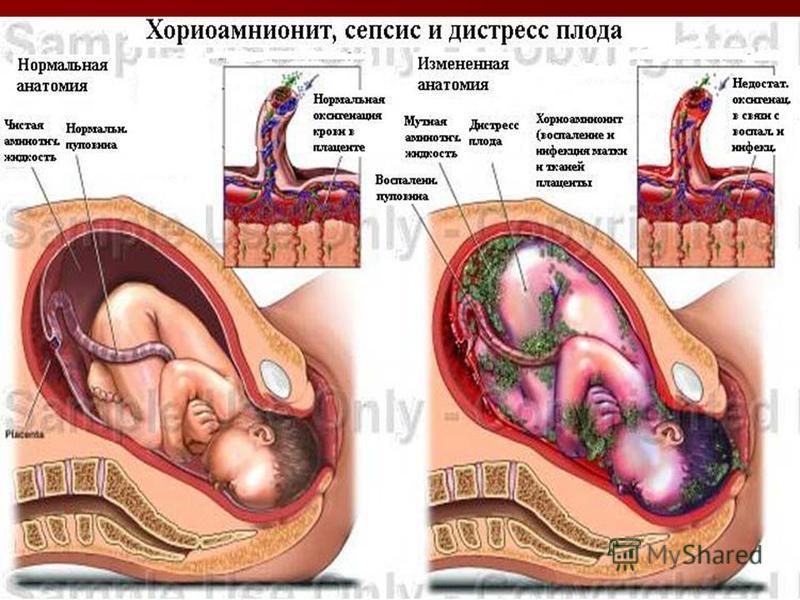
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari.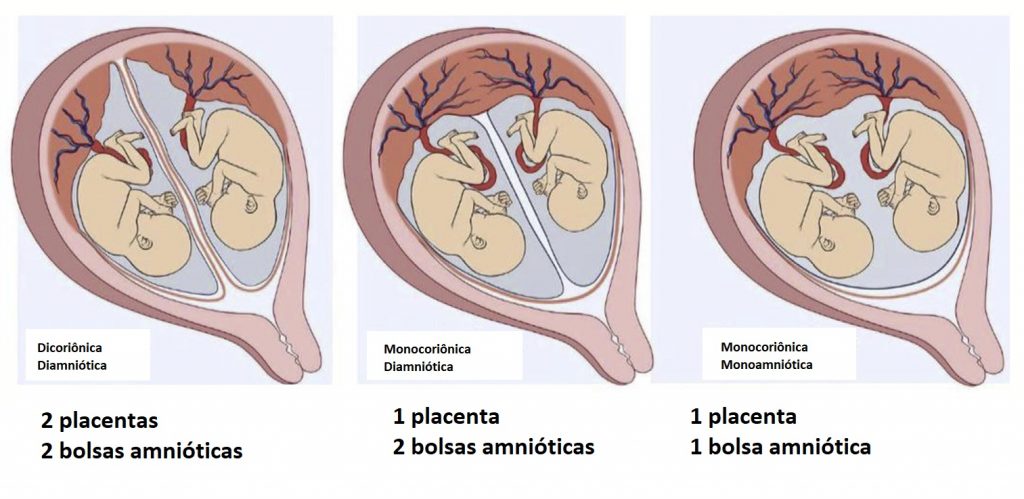 For more information, please visit the links below:
For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
what complications occur during and after childbirth - Forbes Kazakhstan
Photo: pixabay.com
Perhaps nothing in a person's life causes so many expectations, worries and joy as the birth of a child. The miracle of birth has been sung by poets and painters for centuries. Every mother remembers the first minutes of the birth of her baby as the most striking event of her life, and the overflowing feeling of fatherhood is unsurpassed in emotional richness and a sense of eternity.
Secrets of the origin of life
Conception, pregnancy and childbirth is the most ancient trivial process, which, it would seem, has been studied in detail and is quite predictable. At the same time, pregnancy and childbirth carry a colossal physiological burden, affecting almost all aspects of the life of the female body and the developing fetus. Because of this, the risks that arise almost from the moment of conception. In order to better understand these risks, as well as take steps to minimize them, it is important to understand what happens to the body of a woman and fetus during pregnancy and childbirth. nine0003
At the same time, pregnancy and childbirth carry a colossal physiological burden, affecting almost all aspects of the life of the female body and the developing fetus. Because of this, the risks that arise almost from the moment of conception. In order to better understand these risks, as well as take steps to minimize them, it is important to understand what happens to the body of a woman and fetus during pregnancy and childbirth. nine0003
Our "Pregnancy Calculator" allows you to see in detail and illustrations what happens in each week of the development of the unborn child. It also provides evidence-based advice on how to eat right at each stage of pregnancy to ensure the health of the expectant mother and the developing fetus.
In principle, in terms of how pregnancy and childbirth proceed, human individuals are not much different from other mammals. The history of this physiological phenomenon goes back millions of years, and labor pains were described in ancient legends and epics.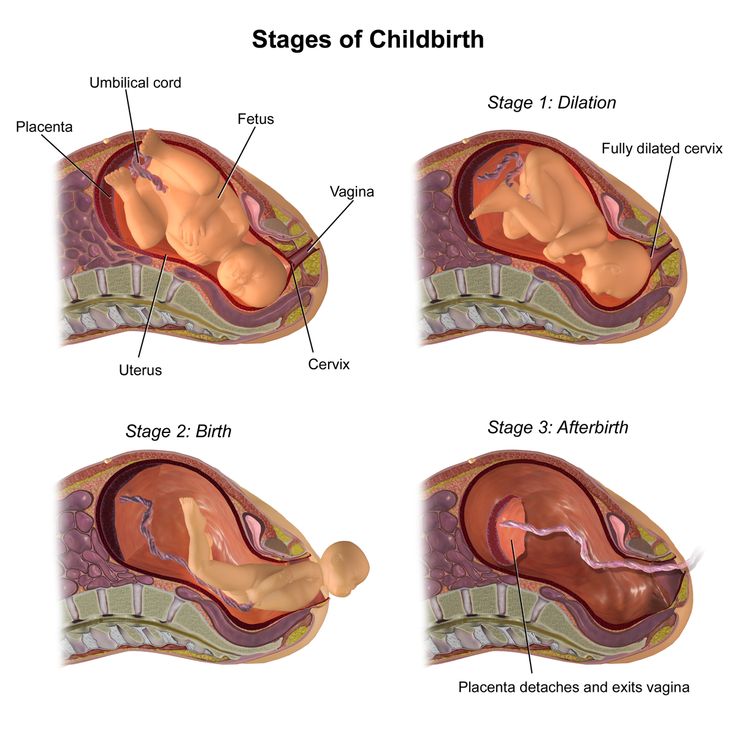 Ever since homo sapiens had a feeling of compassion for the woman in labor, the concept of obstetric care has arisen, the experience of which mankind has been accumulating for tens of thousands of years. nine0003
Ever since homo sapiens had a feeling of compassion for the woman in labor, the concept of obstetric care has arisen, the experience of which mankind has been accumulating for tens of thousands of years. nine0003
The meaning of most changes in the body of a future mother is preparation for childbirth. The uterus undergoes especially great changes, which, closer to childbirth, takes the form of a funnel. With each labor contraction, it contracts to “push” the fetus out. Moreover, this happens by itself, without requiring any effort on the part of the woman.
During childbirth, due to pressure from the fetal head, the walls of the uterus gradually stretch and thin. The neck starts to open. At first, a small hole appears, which expands with each contraction. It looks like a tight shirt is pulled over the child's head. The baby cannot "get out" of the mother's womb until the cervix dilates about ten centimeters, corresponding to the diameter of the baby's head. nine0003
Uterine contractions "squeeze" the fetal head into the narrowest part of the pelvis: the top of the head appears, then the head, shoulders, and suddenly - inhalation and crying, announcing the birth of a child. The umbilical cord is cut. The placenta separates, you can now gently pull on the umbilical cord while the mother pushes to expel the placenta. The uterus spontaneously contracts and turns into a muscle ball, blocking all bleeding cavities. At this time, colostrum, the first mother's milk, appears in the mammary glands of a woman, and the newborn can be applied to the breast. nine0003
The umbilical cord is cut. The placenta separates, you can now gently pull on the umbilical cord while the mother pushes to expel the placenta. The uterus spontaneously contracts and turns into a muscle ball, blocking all bleeding cavities. At this time, colostrum, the first mother's milk, appears in the mammary glands of a woman, and the newborn can be applied to the breast. nine0003
Birth: Miracle or Stress
Now let's imagine what happens to the body of a fetus during birth, which has been in warm conditions for 9 months, immersed in amniotic fluid. With the birth, all this suddenly disappears, as the fetal bladder bursts and warm amniotic fluid flows out. After a while, the baby enters a completely new environment. At this moment, all his organs - stomach, intestines, liver, kidneys - should immediately work. The blood flow must change its course, entering the lungs to supply the body with oxygen from the outside air. The nervous system begins to respond to a huge flow of information coming from outside, especially through vision.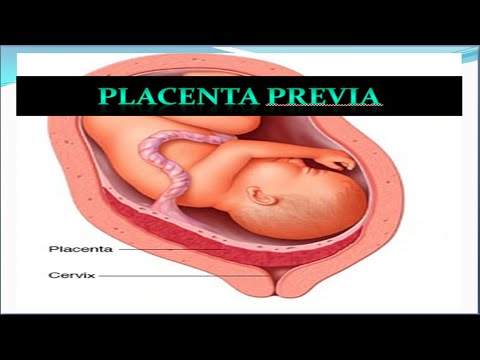 Air enters the lungs for the first time, and the newborn cries out - a new life begins. nine0003
Air enters the lungs for the first time, and the newborn cries out - a new life begins. nine0003
At the moment of birth, the fetus is pushed out of the heavenly water environment of the mother's womb into a hostile airy and cold environment with alien sounds, smells and numerous stresses. As Hugo Langerganz, a pediatric scientist at Karolinska University in Sweden, told , the process of birth in the fetus is accompanied by a massive release of the stress hormone norepinephrine, and such a power that in adults would be comparable to the first minutes of a parachute jump. Added to this is the disconnection from natural anesthetics and sedatives produced by the maternal placenta. nine0003 Responsibility for hospitality in the new world is initially assumed by doctors - most often neonatologists. Before the eyes of a stunned woman in labor, they take up the revival of a lifeless body, and after that they transfer a new living being to the family bosom. Then teamwork begins, when parents, in alliance with doctors, like an alien, introduce the baby to earthly existence. All of the above occurs under normal circumstances, when there are no complications. However, the unexpected can happen at any stage of labor. Bleeding or rupture of the placenta may occur, and part of the placenta may remain in the uterus after childbirth, which can lead to profuse bleeding. It is possible that the uterus does not contract after childbirth, while the internal wound surfaces continue to bleed, and the woman may die from blood loss. Although rare, uterine rupture can occur during contractions. nine0003 Approximately 5% of women develop so-called pre-eclampsia in late pregnancy, which poses a threat to the life of both mother and child. This mystical state still does not find a full explanation. In addition, infectious complications can seriously threaten the life of the woman in labor and the fetus. After the outpouring of amniotic fluid, the likelihood of bacteria entering the uterus increases every hour. In the 19th century, people began to realize that doctors themselves often spread the infection by examining the uterus without washing their hands. Bacteria penetrated into the body of pregnant women and caused blood poisoning (sepsis), threatening the life of both the fetus and the mother. Before the era of antibiotics, puerperal sepsis was the leading cause of maternal death. Even today, if delivery does not occur within 24 hours after amniotic fluid discharge, the probability of infection is about 40% . Serious problems can be associated with so-called pathological births. For example, a large fetus with a post-term (more than 40 weeks) pregnancy can pose a great threat, especially against the background of the small size of the mother's pelvis. In some cases, the fetus may be located across the birth canal, which is why its handles fall out first. nine0003 There may be a breech presentation, in which the child enters the birth canal not with the head, but with the pelvis, while pressing the legs to the chest. This situation creates an obstacle to the further progress of the child through the birth canal. There is a so-called foot presentation, in which the feet come out first, and the fetus is wedged in the canal at chest level with handles above the head. A situation is possible when the fetal head appears, but further progress is blocked due to the incorrect position of the head. Sometimes the head is completely born, and the shoulders are wedged by the pubic bone of the mother's pelvis. Labor pains sometimes last so long that women become weak and die without giving birth. Prolonged labor itself comes with many risks. Even today, if labor continues more than 24 hours after the release of amniotic fluid, there is a 40% risk of infectious complications. Princess Charlotte - the only adored daughter of the British King George IV died during a prolonged (more than 50 hours) childbirth as a result of bleeding. The royal throne was transferred to his brother, and in the subsequent niece - this is how the legendary queen came to power in England by the will of fate Victoria. By the beginning of the 20th century, many methods and means had been invented to ensure a favorable outcome of childbirth. However, despite all this, there was no significant reduction in mortality from childbirth at that time. Doctors often missed obvious signs of bleeding, violated the norms of antiseptics, allowed uterine ruptures and bacterial infections with improper application of forceps. In this case, we are talking about saving two lives: a mother and a child. The name "caesarean" was given to this type of operation on the basis of the legend, according to which it was in this way that Aurelia gave birth to the Roman king Caesar (Caesar). However, historians regard this story as more of a myth, since Aurelia lived long after Caesar's birth. Ancient Roman laws of the 7th century BC forbidden to bury pregnant women. They demanded that the child be removed from the mother's womb in the hope that he would survive. In 1614 Pope Paul IV issued a decree requiring the baptism of any child born alive. However, a caesarean section performed on a living woman was considered a criminal offence. This was due to the fact that in almost all cases, caesarean section ended in an unfavorable outcome due to bleeding and infectious complications. This is how a modern physician would describe the entire process of a caesarean section surgery. With a scalpel blade, a transverse incision is made in the lower abdomen of the woman in whose womb the fetus is located. First, a golden-colored fatty layer opens, which can be separated from the skin with a few precise movements of the scalpel. In this case, slight bleeding may occur, which is stopped with a gauze swab. Next, the so-called "fascia" opens - a fibrous membrane of the abdominal wall, similar to a wrapper. After its dissection, two vertical stripes of the rectus abdominis muscle of red color are opened. With the help of tools called "retractors", they are pulled apart like curtains. Then the peritoneum opens - a thin, almost transparent shell that covers the internal organs. What follows is seen as a surreal picture. You run your hand inside and feel for the moving fingers, heel, knee, and then the entire leg of the fetus. And suddenly you realize that a new human life is beating in your hands. In doing so, you almost forget about the mother lying on the table. If the fetal head is deep in the birth canal, then you need to confidently take the baby by the waist and pull. Sometimes it is required that the assistant from the bottom pushes the head. The baby is then released from the mother's womb and the umbilical cord is cut by an assistant. nine0003 After the next uterine contraction, you remove the placenta (afterbirth) and pull it out. Use a sterile gauze swab to clear the uterus of blood clots and other debris. Once a rarity, this procedure has now become quite routine. Many obstetricians are able to perform a caesarean section without any problems. Today, the caesarean section is fairly standardized and performed with remarkable uniformity. Gone are the days when obstetricians often had to use manual techniques for various cases: with prolapse of the legs, breech presentation, clamping the head in the pelvis, and more. Each of these techniques has its own difficulties and is accompanied by risks. Today, for all these problems, one solution is a caesarean section. nine0003 "Primum non nocere" (first of all, do no harm) - says the main principle of the doctor, formulated by the father of medicine Hippocrates in the collection of postulates named after him ("Hippocratic Corpus", 430-330 BC. If, after a caesarean section of the next child, a woman tries to give birth through the birth canal, the probability of rupture of the scar on the uterus is approximately 1 in 200 cases. In addition, the placenta can attach itself to the scar, which can lead to severe bleeding when it is separated. Nevertheless, it must be borne in mind that a caesarean section is a surgical operation with associated risks and possible complications. But you can't do without a caesarean section. We have reached the point where, in any doubt, doctors resort to cesarean section simply because it is faster, more reliable and less troublesome. If a woman is carrying a child weighing more than 4.5 kg or she has twins, triplets, usually go for a caesarean section. Caesarean section is recommended for transverse fetal position, breech presentation, and a range of situations that indicate a high risk of adverse outcome. Doctors are becoming increasingly reluctant to accept the risks associated with natural childbirth, even if they are insignificant - it is easier to do a caesarean section. Today in many clinics about 30% of babies are born by caesarean section. In most cases, this approach is fully justified. At the same time, it is important to note that elective caesarean sections are less risky than emergency ones, when the operation must be carried out quickly, in critical conditions. Still, there is something unsettling about this fact. With a cesarean section, the connection with another natural process of life, which has a thousand-year tradition, is lost. Scientists believe that at birth, a child must ingest a lot of beneficial bacteria contained in the birth canal. These bacteria create the very basis for the formation of a healthy microbiome. This is the advantage of natural childbirth compared to caesarean section, in which the child does not pass through the natural birth canal. Physicians recognize that the sterile environment, which was previously sought as a condition for the healthy development of the child, is not justified. We begin to realize that we are too carried away by the fight against microbes and, as they say, we throw out the baby with the water, in this case, beneficial bacteria. We are witnessing the decline of the art of traditional childbirth. Over the centuries, the skill of midwifery needed to help the baby to be born through the natural birth canal has been developed. It seems that soon this art will be carried away into oblivion by modern medicine. Today it is clear to everyone that it is not enough just to have knowledge and apply technology. Midwifery needs a different kind of ingenuity. It is important to standardize the delivery process. At 19In the 1930s, the medical "class" resorted to a strategy that was based on the standardization of medical practice. Standards have been developed for the training of birth attendants; hospitals have established strict regulations and requirements for birth attendants. In particular, professional requirements for obstetricians have been developed, taking into account their experience, ability to use obstetric forceps and other unsafe interventions. Standardization proved to be a turning point in obstetrics. Midwifery has come to be seen as both an art and a craft. As an art, midwifery provides for the improvement of the methods and techniques used in obstetric care. Special devices have been developed that allow you to control the fetal heartbeat. Epidural anesthesia has revolutionized many aspects of childbirth, greatly reducing the pain of childbirth. New synthetic drugs (pitocin instead of ergot) were invented that more effectively controlled uterine contractions during childbirth. nine0003 According to the World Health Organization, over the past 25 years, maternal mortality in the world has decreased by 44%. Nevertheless, despite the successful development of technology, about 1400 women die every day from various pathological conditions in the world before and during childbirth. There are many factors that lead to complications of pregnancy and childbirth, such as women's health problems, unfavorable environmental conditions, and sometimes insufficient medical qualifications. In developed countries, among the causes of maternal death, the most common are disorders of the heart and cerebral circulation, bleeding and embolism (blockage of blood vessels) with amniotic fluid. In the postpartum period, women are more likely to die from cardiomyopathy - insufficiency of the heart muscle. nine0003 Today, it is essential to focus on training obstetricians in the skills and abilities to apply traditional and new methods of childbirth. Last year, several cases of maternal deaths in the capital of Kazakhstan caused a great resonance. Then the invited foreign experts did not reveal unskilled actions on the part of doctors. Childbirth safety does not always depend on medical experience; much is determined by how the expectant mother prepares for the difficult process of having a baby. The body of a woman, exhausted by disease, malnutrition and exposure to bad habits, is ill-prepared to accept the hardships of pregnancy and childbirth. To this should be added the undesirability of short internatal intervals: a woman's body must rest and recover after childbirth and breastfeeding for at least one and a half to two years. In addition, it must be taken into account that with age, the compensatory capabilities necessary for physiological pregnancy and safe childbirth naturally fade in a woman's body. nine0003 Therefore, it is extremely important that the expectant mother deeply realizes the great responsibility for her own safety and the health of the expected baby. Pregnancy and childbirth in terms of physical sensations and experiences is perhaps the most amazing, emotionally intense period in a woman's life. It is important to make sure that you are ready for these most important events and phenomena so that the miracle of the birth of a baby is not overshadowed by the bitterness of ailments and losses. nine0003 Stars love to talk about how happy they are to become mothers, but few people talk about the other side of pregnancy and childbirth. Vomiting leading to a hospital bed, diabetes, the inability to stand up after a caesarean section - what difficulties the stars faced during pregnancy and childbirth and why they arise, Gazeta.Ru understood. Infertility, IVF and surrogacy, intractable vomiting and diabetes, manual removal of the placenta and caesarean section - many women go through this when they decide to have children, and celebrities are no exception. Famous women often talk about how happy they were to become mothers, but only a few share the details of pregnancy and childbirth. Meanwhile, this information allows expectant mothers to prepare for possible difficulties and survive them without too much panic. American actress Anne Hathaway at the end of July 2019 told subscribers in social networks that she was expecting her second child. Both during the first and during the second pregnancy, Hathaway had difficulty conceiving, but the actress prefers to keep their details a secret. However, she hopes that her victory over infertility will give hope to those of her fans who are unsuccessfully trying to get pregnant. nine0003 See this post on Instagram It's not for a movie... #2 All kidding aside, for everyone going through infertility and conception hell, please know it was not a straight line to either of my pregnancies. Posted by Anne Hathaway (@annehathaway) “Pregnancy is usually presented as an unconditional happiness, and all negative aspects are left in the shade. But it's different for everyone. And for many women, everything happens not at all so easily and simply. I'm tired of this state of affairs, because it's not true, and I love the truth, ”said Hathaway in an interview with Daily Mail . A couple is considered infertile if the woman does not become pregnant within a year of regular intercourse - at least two intercourse per week without the use of contraceptives. According to the WHO, about 8% of married couples face the problem of infertility during the reproductive period of their lives. Its causes are both developmental defects and traumas, as well as the consequences of infectious diseases or endocrine disorders. In men, infertility is often related to the quality of sperm. Fighting infertility means eliminating the causes that led to it. Sometimes you have to resort to assisted reproductive technologies. So, the singer Mariah Carey became pregnant for the first time with twins at the age of 39 with the help of IVF. The pregnancy was difficult, so after giving birth, the singer said that she no longer plans to have children. "I had gestational diabetes, life-threatening high blood pressure, and all the things you don't even want to know about," she said. nine0003 During IVF, a woman, as a rule, first undergoes a course of hormonal injections to stimulate superovulation - the maturation of several eggs at once during one menstrual cycle. Then the ovarian follicles are punctured and the eggs are removed from the body. The male usually collects the sperm for fertilization on his own. The embryologist then adds the suspension containing the spermatozoa to the oocytes in the culture medium, or injects the sperm into the oocyte manually using microsurgical instruments. Pregnancy diabetes goes away after childbirth, but doctors see it as a precursor to type 2 diabetes—women who experience it have an increased risk of developing diabetes in the future. Comedian Amy Schumer also faced the "charms" of pregnancy - she had to endure severe toxicosis. Because of him, she ended up in the hospital, all performances had to be canceled. Kate Middleton also complained about toxicosis - in all her three pregnancies in the initial stages, she had to miss some events that the royal protocol requires to attend. nine0003 See this post on Instagram Texas I am so deeply sorry. I have been really looking forward to these shows. Posted by @ amyschumer Toxicosis in pregnant women in mild form is manifested by nausea and vomiting up to five times a day, in moderate form - up to 12 times. This is accompanied by weakness, tachycardia, irritability. This is due, in particular, to a change in the hormonal background so that the embryo can gain a foothold in the uterus. Also, toxicosis is considered as a reaction of a woman's immune system to an "invasion" into her body. Hyperemesis, intractable vomiting of pregnancy, is a condition in which vomiting occurs up to 25 times a day. nine0003 Hyperemesis occurs in every 100 pregnant women. Frequent vomiting leads to dehydration and a sharp loss of body weight, lack of potassium and magnesium, anemia. In these cases, the woman is transferred to intravenous nutrition, given antiemetics. In the event of a threat to her life and health, the question of abortion is raised. Reality TV star Kim Kardashian, having survived two difficult pregnancies and childbirth, hired a surrogate mother to carry her third child - doctors forbade her to get pregnant. Shortly before the second birth, Kardashian admitted that pregnancy is the worst stage in her life. nine0003 “New mothers usually don't talk about the unpleasant side of pregnancy. But do you know, for example, that we have to wear a diaper for two months after giving birth?” she said. “After the baby is born, the placenta must come out. Factors that increase the risk of uterine growth - a history of inflammation of the uterus, curettage, scars after cesarean section, chronic infections, toxicosis. However, their absence does not protect against uterine growth by 100%. Placental accreta is divided into true, when the vessels of the placenta grow into the uterine tissue, and dense attachment, when it fuses only with the spongy layer located between the placental and muscular tissue of the uterus. In this case, if after childbirth the placenta did not come out by itself within about an hour, the doctor separates it manually by inserting a hand into the uterine cavity. nine0003 True augmentation often requires hysterectomy. Singer Madonna gave birth to her second child at the age of 41. The birth began prematurely: Madonna's placenta was torn and bleeding began. In the hospital, the actress had an emergency caesarean section. Tennis player Serena Williams also had to go through the operation - her daughter's heartbeat suddenly slowed down. The caesarean section itself was easy for Williams, but the postoperative period was hell for her. “I didn't even expect it to be so terrible - I couldn't walk. I couldn't even roll over in bed. I couldn't even go to the toilet on my own. My husband literally carried me in his arms. I didn’t expect that from one of the strongest athletes in the world I would turn into a person who can’t get out of bed without help.” — shared later in an interview with Harper's Bazaar. Caesarean section was used even before our era, although until the 19th century it was deadly. After they began to remove during the operation, and after a few years - simply sew up the uterus, a quarter of women died as a result of caesarean section.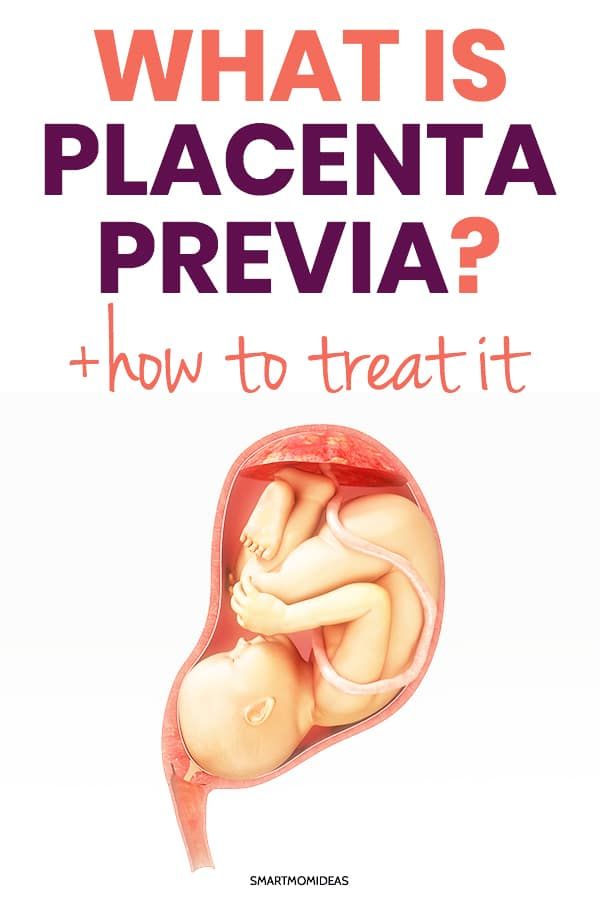 In the beginning, this is called newborn patronage. Then pediatricians are connected, and later other doctors. Man is perhaps the only mammal that is born helpless and needs constant care for a long time. And some believe that this should continue throughout life. nine0003
In the beginning, this is called newborn patronage. Then pediatricians are connected, and later other doctors. Man is perhaps the only mammal that is born helpless and needs constant care for a long time. And some believe that this should continue throughout life. nine0003 The thorns of motherhood
 Pre-eclampsia is manifested by the swelling and headaches often seen in normal pregnancies, making it easy to miss the true symptoms of this formidable condition. In a word, for physicians, some women in labor seem to be "powder kegs", with which one must always be on the alert. nine0003
Pre-eclampsia is manifested by the swelling and headaches often seen in normal pregnancies, making it easy to miss the true symptoms of this formidable condition. In a word, for physicians, some women in labor seem to be "powder kegs", with which one must always be on the alert. nine0003 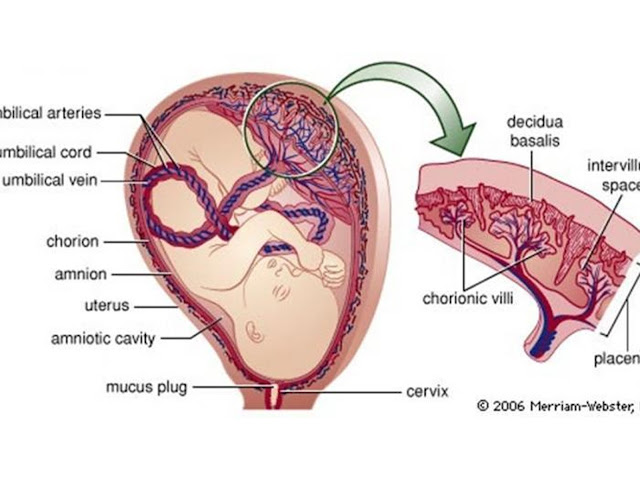
 When a baby gets stuck in the birth canal, the umbilical cord gets pinched or pinched over time. This can lead to suffocation (asphyxia) of the newborn. nine0003
When a baby gets stuck in the birth canal, the umbilical cord gets pinched or pinched over time. This can lead to suffocation (asphyxia) of the newborn. nine0003 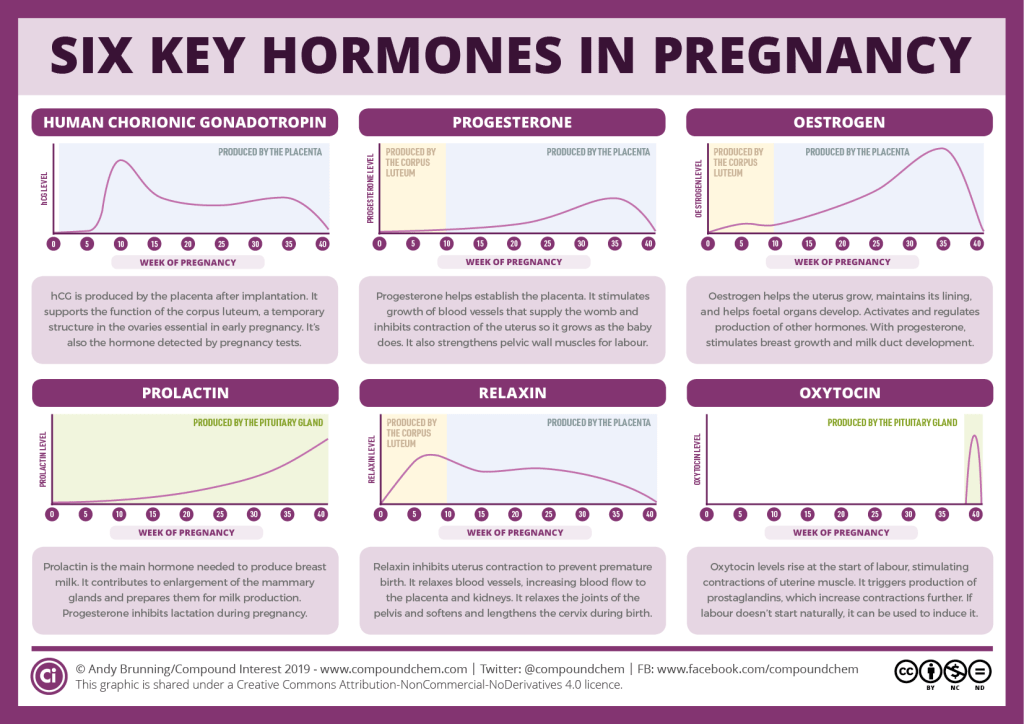 It seemed that the main risks associated with childbirth were quite surmountable. For example, antiseptics and obstetric forceps were invented. Netflix's historical television series The Crown shows how obstetrical forceps were relatively recently used during childbirth by the current British Queen Elizabeth. Blood transfusion has been introduced into medical practice. A drug (ergot) was created to stimulate labor and contract the uterus after childbirth to stop bleeding. They began to create special maternity wards of hospitals, entire maternity hospitals, and home births became a rarity. nine0003
It seemed that the main risks associated with childbirth were quite surmountable. For example, antiseptics and obstetric forceps were invented. Netflix's historical television series The Crown shows how obstetrical forceps were relatively recently used during childbirth by the current British Queen Elizabeth. Blood transfusion has been introduced into medical practice. A drug (ergot) was created to stimulate labor and contract the uterus after childbirth to stop bleeding. They began to create special maternity wards of hospitals, entire maternity hospitals, and home births became a rarity. nine0003 To Caesar is Caesar's, but to the doctor - saving a life
 That is a huge responsibility. One of the ways for a relatively safe delivery is a caesarean section. It is a surgical operation that allows a child to be born by removing it from the abdomen of a mother who cannot give birth in the usual way. nine0003
That is a huge responsibility. One of the ways for a relatively safe delivery is a caesarean section. It is a surgical operation that allows a child to be born by removing it from the abdomen of a mother who cannot give birth in the usual way. nine0003 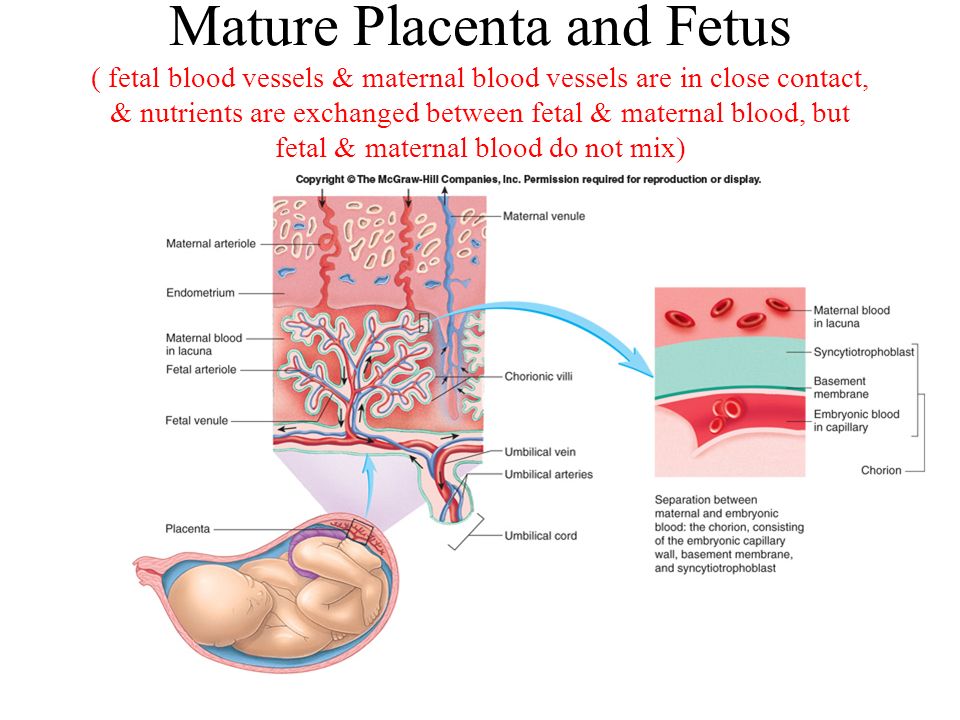 Only in the 19th - early 20th century, after the invention of anesthesia and antiseptics, as well as due to the introduction of the double-layer suture technique that prevents bleeding, did it become possible in medical practice to perform a relatively safe caesarean section. nine0003
Only in the 19th - early 20th century, after the invention of anesthesia and antiseptics, as well as due to the introduction of the double-layer suture technique that prevents bleeding, did it become possible in medical practice to perform a relatively safe caesarean section. nine0003 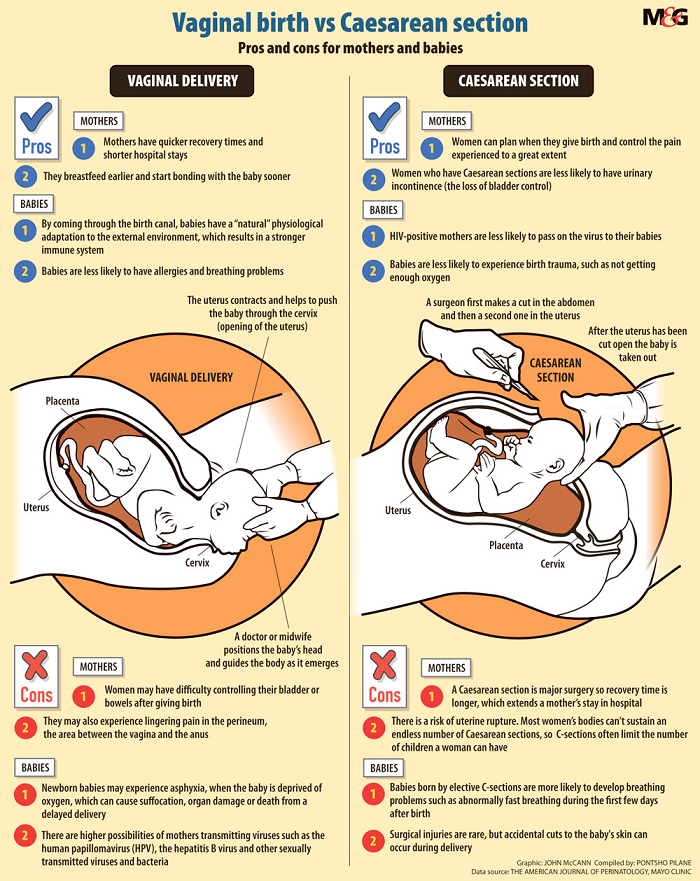 The peritoneum is excised, and the uterus appears - a large plum-colored muscular organ. With a scalpel, a small initial incision is made, and then, to speed up the process, they resort to scissors. It feels like cutting through a thick, leathery fruit. nine0003
The peritoneum is excised, and the uterus appears - a large plum-colored muscular organ. With a scalpel, a small initial incision is made, and then, to speed up the process, they resort to scissors. It feels like cutting through a thick, leathery fruit. nine0003  The uterus is sutured with two layers of dense threads, which subsequently dissolve on their own. With another thread, sew up the fascia, and then the skin. That's all.
The uterus is sutured with two layers of dense threads, which subsequently dissolve on their own. With another thread, sew up the fascia, and then the skin. That's all. First of all, do no harm
 e.). The principle prescribes not to cause more harm to the patient by treatment than the disease itself. Doctors are guided by this to some extent when they undertake a caesarean section. However, no matter how simple the operations, they are still associated with certain risks. In some women, caesarean section is complicated by pneumonia, and the recovery process is generally more protracted than with conventional childbirth. During the operation, the intestines may be damaged. Sometimes there is severe bleeding or a blood clot breaks off. The stitches may open or become infected. nine0003
e.). The principle prescribes not to cause more harm to the patient by treatment than the disease itself. Doctors are guided by this to some extent when they undertake a caesarean section. However, no matter how simple the operations, they are still associated with certain risks. In some women, caesarean section is complicated by pneumonia, and the recovery process is generally more protracted than with conventional childbirth. During the operation, the intestines may be damaged. Sometimes there is severe bleeding or a blood clot breaks off. The stitches may open or become infected. nine0003 
 A recent American study questioned the safety of elective caesarean sections. However, two other European studies have actually shown that maternal mortality is lower for caesarean sections than for vaginal delivery. nine0003
A recent American study questioned the safety of elective caesarean sections. However, two other European studies have actually shown that maternal mortality is lower for caesarean sections than for vaginal delivery. nine0003 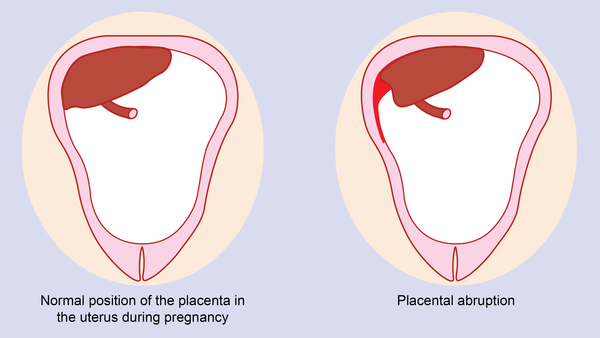 nine0003
nine0003 Childbirth is an art and craft
 By the early 1950s, thanks to the introduction of standards and, in part, the discovery of penicillin and other antibiotics, maternal mortality had declined to 90%.
By the early 1950s, thanks to the introduction of standards and, in part, the discovery of penicillin and other antibiotics, maternal mortality had declined to 90%. 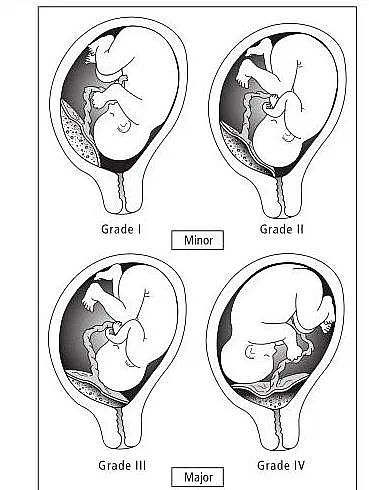 And this happens not only in developing countries, but also in developed countries, such as the United States of America. Approximately one third of maternal deaths occur during the last weeks of pregnancy, another third during childbirth and within a week after childbirth, and another third during the year after childbirth. nine0003
And this happens not only in developing countries, but also in developed countries, such as the United States of America. Approximately one third of maternal deaths occur during the last weeks of pregnancy, another third during childbirth and within a week after childbirth, and another third during the year after childbirth. nine0003 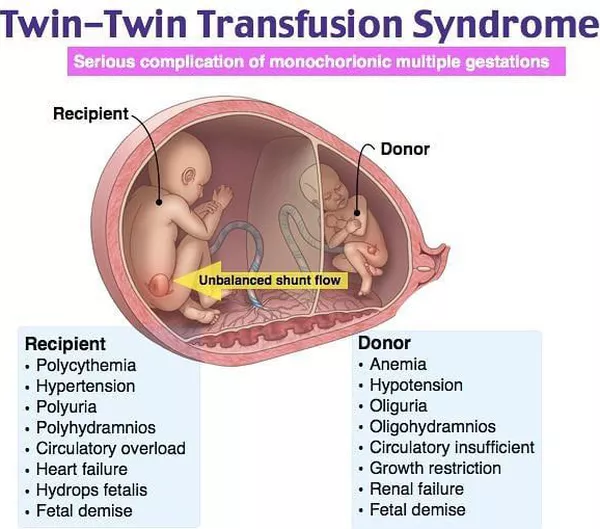 The craft provides for the constancy and continuous improvement of the acquired skills.
The craft provides for the constancy and continuous improvement of the acquired skills. 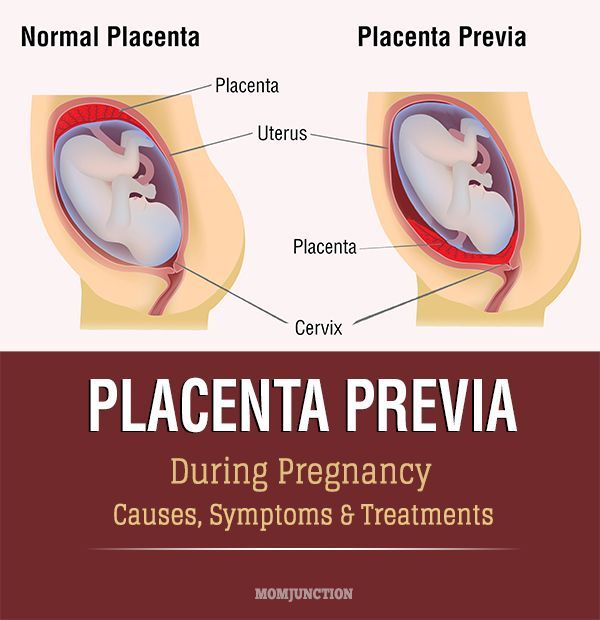 To do this, it is necessary to eat rationally, give up bad habits and a sedentary lifestyle, prevent and treat diseases in a timely manner, and regularly see a doctor in order to prevent potential health threats in time.
To do this, it is necessary to eat rationally, give up bad habits and a sedentary lifestyle, prevent and treat diseases in a timely manner, and regularly see a doctor in order to prevent potential health threats in time. What the stars faced during pregnancy and childbirth
 Gazeta.Ru found out what difficulties the stars faced during pregnancy and childbirth. nine0003
Gazeta.Ru found out what difficulties the stars faced during pregnancy and childbirth. nine0003
 Sending you extra love
Sending you extra love  nine0003
nine0003  The probability of successful fertilization is 60-70%. After 2-5 days, the embryos are transferred into the uterine cavity of the patient or a surrogate mother. Usually two embryos are transferred. nine0003
The probability of successful fertilization is 60-70%. After 2-5 days, the embryos are transferred into the uterine cavity of the patient or a surrogate mother. Usually two embryos are transferred. nine0003
 I have to reschedule. I am in the hospital. I'm fine. Baby's fine but everyone who says the 2nd trimester is better is not telling the full story. I've been even more ill this trimester. I have hyperemesis and it blows. Very lucky to be pregnant but this is some bullshit! Sending so much love to the doctors and nurses taking great care of me and Tati! They are cool as hell! And Texas I am really really sorry and I'll be out there as soon as I'm better. nine0003
I have to reschedule. I am in the hospital. I'm fine. Baby's fine but everyone who says the 2nd trimester is better is not telling the full story. I've been even more ill this trimester. I have hyperemesis and it blows. Very lucky to be pregnant but this is some bullshit! Sending so much love to the doctors and nurses taking great care of me and Tati! They are cool as hell! And Texas I am really really sorry and I'll be out there as soon as I'm better. nine0003 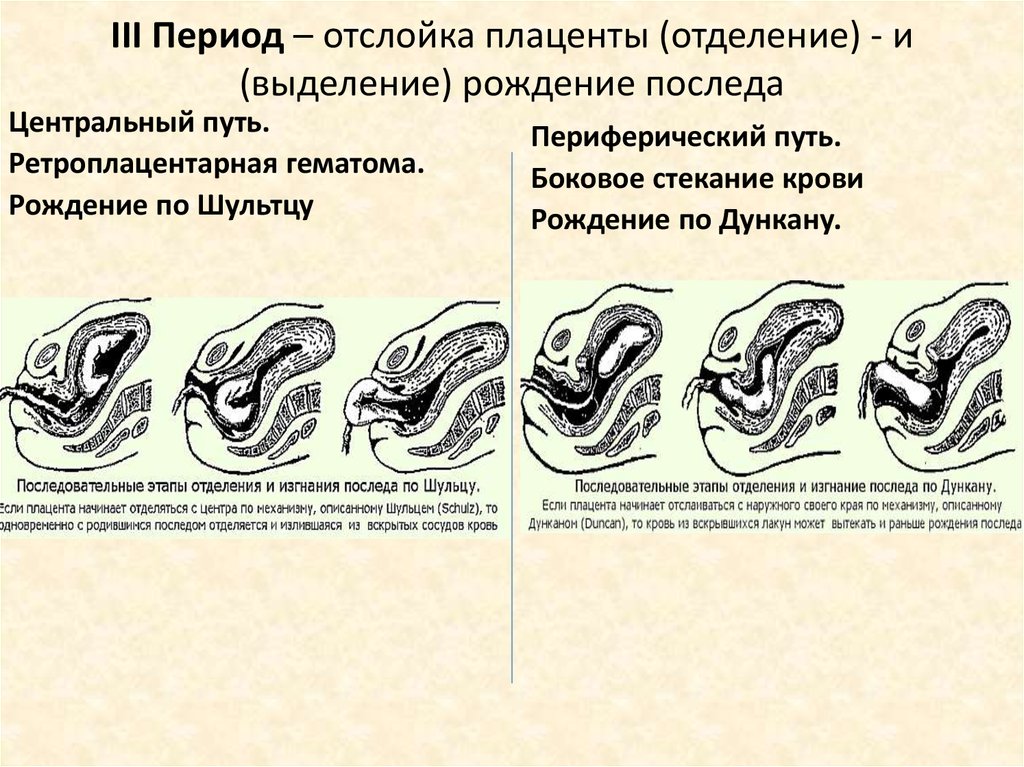
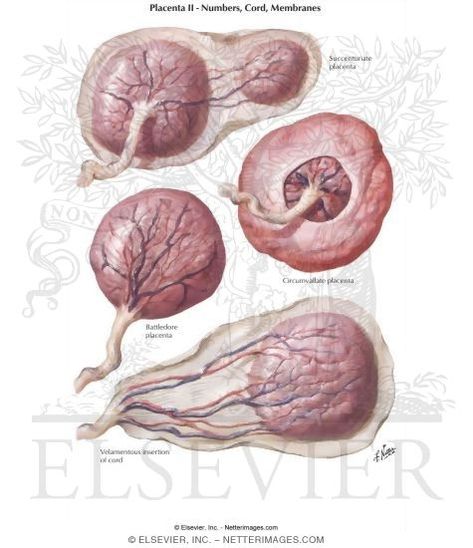 But mine is stuck. This causes severe bleeding and often leads to the death of a woman. In my case it was disgusting! - Remembered Kardashian after giving birth. - To get the placenta, the doctor had to stick his hand into me almost to the elbow and scrape it all out. It was unbearably painful." nine0003
But mine is stuck. This causes severe bleeding and often leads to the death of a woman. In my case it was disgusting! - Remembered Kardashian after giving birth. - To get the placenta, the doctor had to stick his hand into me almost to the elbow and scrape it all out. It was unbearably painful." nine0003