Tiny raised bumps on arm
Pictures, Types, Causes, and Treatment
Raised skin bumps are mostly harmless. They may present in various ways, from skin tags to keloids. Conditions like acne and chickenpox can also cause them. Seek medical help if your bumps resemble those caused by MRSA or skin cancer.
Raised skin bumps are very common, and in most cases, they’re harmless. They can result from a number of conditions, including:
- infections
- allergic reactions
- skin disorders
- skin cancer
Skin bumps can vary in appearance and number depending on the cause. They may be the same color as your skin or a different color. They may be itchy, large, or small. Some can be hard, while others can feel soft and movable.
Most skin bumps do not need treatment. However, you should speak with a doctor if your bumps are causing discomfort. You should also call a doctor if you’re concerned about any changes in your bumps or in the overall condition of your skin.
Many conditions can cause raised bumps to appear on the skin. Here’s a list of 25 possible causes.
Warning: Graphic images ahead.
Acne
- commonly located on the face, neck, shoulders, chest, and upper back
- breakouts on the skin composed of blackheads, whiteheads, pimples, or deep, painful cysts and nodules
- may leave scars or darken the skin if untreated
Read the full article on acne.
Cold sore
- red, painful, fluid-filled blister that appears near the mouth and lips
- affected area will often tingle or burn before the sore is visible
- may be accompanied by mild, flu-like symptoms, such as low fever, body aches, and swollen lymph nodes
Read the full article on cold sores.
Corns and calluses
- small, round circles of thickened skin with a painful, horn-like central area of hardened tissue
- commonly found on the tops and sides of the toes and on the soles of the feet
- caused by friction and pressure
Read the full article on corns and calluses.
Skin tags
- skin growths that can become up to half an inch long
- same color as your skin or slightly darker
- most likely caused by friction
- commonly found near the neck, armpits, breasts, groin, stomach, or eyelids
Read the full article on skin tags.
Nodule
- small to medium growth that may be filled with tissue, fluid, or both
- usually wider than a pimple and may look like a firm, smooth elevation under the skin
- usually harmless, but may cause discomfort if it presses on other structures
- nodules may also be located deep inside the body where you cannot see or feel them
Read the full article on nodules.
Impetigo
- common in babies and children
- irritating rash and fluid-filled blisters that pop easily and form a honey-colored crust
- rash is often located in the area around the mouth, chin, and nose
Read the full article on impetigo.
Molluscum contagiosum
- bumps that may appear in a patch of up to 20
- small, shiny, and smooth
- flesh-colored, white, or pink
- firm and dome-shaped with a dent or dimple in the middle
Read the full article on molluscum contagiosum.
Lipoma
- soft to the touch and moves easily if prodded with your finger
- small, just under the skin, and pale or colorless
- commonly located in the neck, back, or shoulders
- only painful if it presses on a nerve
Read the full article on lipoma.
Cyst
- slow-growing bump under the skin that has a smooth surface
- can be large or small and is usually painless
- typically not a problem unless it’s infected, very large, or growing in a sensitive area
- some grow deep inside your body where you can’t see or feel them
Read the full article on cysts.
Wart
- caused by many different types of a virus called human papillomavirus (HPV)
- may be found on the skin or mucous membranes
- may occur as one wart or in groups
- contagious and may be passed to others
Read the full article on warts.
Actinic keratosis
- typically less than 2 centimeters (cm), or about the size of a pencil eraser
- thick, scaly, or crusty skin patch
- appears on parts of the body that receive a lot of sun exposure (hands, arms, face, scalp, and neck)
- usually pink in color but can have a brown, tan, or gray base
Read the full article on actinic keratosis.
Basal cell carcinoma
- raised, firm, and pale areas that may resemble a scar
- dome-like, pink or red, shiny, and pearly areas that may have a sunk-in center, like a crater
- visible blood vessels on the growth
- easy bleeding or oozing wound that doesn’t seem to heal, or heals and then reappears
Read the full article on basal cell carcinoma.
Squamous cell carcinoma
- often occurs in areas exposed to ultraviolet (UV) radiation, such as the face, ears, and back of the hands
- scaly, reddish patch of skin that progresses to a raised bump and continues to grow
- growth that bleeds easily and doesn’t heal, or heals and then reappears
Read the full article on squamous cell carcinoma.
Melanoma
- the most serious form of skin cancer, more common in people with lighter skin tones
- mole anywhere on the body that has irregularly shaped edges, asymmetrical shape, and multiple colors
- mole that has changed color or gotten bigger over time
- usually larger than a pencil eraser
Read the full article on melanoma.
Boils
- bacterial or fungal infection of a hair follicle or oil gland
- can appear anywhere on the body but are most common on the face, neck, armpit, and buttock
- red, painful, raised bump with a yellow or white center
- may rupture and weep fluid
Read the full article on boils.
Bullae
- clear, watery, fluid-filled blister that is greater than 1 cm in size
- can be caused by friction, contact dermatitis, and other skin disorders
- if clear liquid turns milky, there might be an infection
Read the full article on bullae.
Contact dermatitis
- appears hours to days after contact with an allergen
- rash has visible borders and appears where your skin touched the irritating substance
- skin is itchy, red, scaly, or raw
- blisters that weep, ooze, or become crusty
Read the full article on contact dermatitis.
Cherry angioma
- common skin growth that can be found anywhere on the body but is most likely to be seen on the torso, arms, legs, and shoulders
- more common in people over age 30
- small, bright red circular or oval spots that may be raised or smooth and bleed if rubbed or scratched
- generally harmless but may require removal if they’re in problem areas
Read the full article on cherry angioma.
Keloids
- symptoms occur at the site of a previous injury
- lumpy or rigid area of skin that may be painful or itchy
- area is flesh-colored, pink, or red
Read the full article on keloids.
Keratosis pilaris
- common skin condition that’s most often seen on the arms and legs but might also occur on the face, buttocks, and torso
- often clears up on its own by age 30
- patches of skin that appear bumpy, slightly red, and feel rough
- may get worse in dry weather
Read the full article on keratosis pilaris.
Seborrheic keratoses
- common, harmless skin growth that is usually seen in older adults
- can be located anywhere on the body except for the palms of the hands and soles of the feet
- round, oval, dark-colored growth with a “stuck-on” appearance
- raised and bumpy with a waxy feel
Read the full article on seborrheic keratoses.
Chickenpox
- clusters of itchy, red, fluid-filled blisters in various stages of healing all over the body
- accompanied by fever, body aches, sore throat, and loss of appetite
- remains contagious until all blisters have crusted over
Read the full article on chickenpox.
MRSA (staph) infection
This condition is considered a medical emergency. Urgent care may be required.
- an infection caused by a type of Staphylococcus, or staph, bacteria that is resistant to many different antibiotics
- causes an infection when it enters through a cut or scrape on the skin
- skin infection that often looks like a spider bite, with a painful, raised, red pimple that may drain pus
- needs to be treated with powerful antibiotics and can lead to more dangerous conditions like cellulitis or blood infection
Read the full article on MRSA (staph) infection.
Scabies
- symptoms may take 4 to 6 weeks to appear
- extremely itchy rash that may be pimply, made up of tiny blisters, or scaly
- raised white or flesh-colored lines
Read the full article on scabies.
Strawberry nevus
- red or purplish raised mark, commonly located on the face, scalp, back, or chest
- appears at birth or in very young children
- gradually gets smaller or disappears as the child ages
Read the full article on strawberry nevus.
The most common causes of raised skin bumps are harmless and do not require medical treatment unless you have discomfort. Here are some of the possible reasons for raised skin bumps:
- Acne is the most common skin condition in the United States, according to the American Academy of Dermatology. It causes skin bumps that can range from very small and painless to large and painful. The bumps are usually accompanied by redness and swelling.
- Boils are infected hair follicles that look like red, raised bumps on the skin. They can be painful, but they eventually go away once they burst and release fluid.
- Bullae are raised, fluid-filled bumps that can result from friction, or conditions like contact dermatitis and chickenpox.
- Cherry angiomas are common skin growths that can form on most areas of the body. They develop when blood vessels clump together and create a raised, bright-red bump under or on the skin.

- Cold sores are red, fluid-filled bumps that form around the mouth or other areas of the face and can burst. They’re caused by a common virus called herpes simplex.
- Contact dermatitis is an allergic skin reaction that produces an itchy, red skin rash. The rash may consist of raised, red bumps that ooze, drain, or crust.
- Corns or calluses are rough, thickened areas of skin. They’re most often found on the feet and hands.
- Cysts are growths that contain fluid, air, or other substances. They develop under the skin in any part of the body. They feel like a small ball and can usually be moved around slightly.
- Keloids are smooth, raised growths that form around scars. They’re most commonly found on the chest, shoulders, and cheeks.
- Keratosis pilaris is a skin condition marked by an overgrowth of a protein called keratin. It causes small bumps around hair follicles on the body.

- Lipomas are collections of fatty tissue under the skin and are often painless. They usually form on the neck, back, or shoulders.
- Molluscum contagiosum are small, flesh-colored bumps with a dimple in the center that often form in all parts of the body. They can arise from skin-to-skin contact with someone affected with them.
- Nodules result from growth of abnormal tissue, and can appear on the skin in common areas like the armpits, groin, and head and neck region.
- Seborrheic keratoses are round, rough spots on the surface of the skin. They can affect many areas of the body, including the chest, shoulders, and back. They may be skin-colored, brown, or black.
- Skin tags are small, fleshy flaps of skin. They usually grow on the neck or in the armpits. They may be the same color as the skin or slightly darker.
- Strawberry nevus is a red birthmark also known as a hemangioma.
 They are most common in young children and usually disappear by age 10.
They are most common in young children and usually disappear by age 10. - Warts are raised, rough bumps caused by the human papillomavirus (HPV). They typically develop on the hands and feet. They may be skin-colored, pink, or slightly brown.
Less commonly, raised skin bumps are caused by more serious conditions that require treatment. Certain bacterial and viral infections cause bumps and will only get worse if they go undiagnosed and untreated. These serious conditions include:
- chickenpox, a common childhood virus characterized by red, itchy bumps that form all over the body
- impetigo, a bacterial skin infection common in young children that is highly contagious and results in reddish blisters that ooze and develop a honey-colored crust
- MRSA (staph) infection, an illness triggered by a staph bacteria that commonly lives on the skin, causing a swollen, painful bump with a white center
- scabies, a skin infestation caused by a tiny mite called Sarcoptes scabiei, producing an itchy, pimple-like rash
Other types of raised skin bumps can be caused by skin cancer. There are several types of skin cancer, all requiring medical management and treatment:
There are several types of skin cancer, all requiring medical management and treatment:
- Actinic keratosis is a precancerous skin condition characterized by scaly, crusty spots on areas of sun-exposed skin, such as hands, arms, or face. These spots are typically brown, gray, or pink. The affected area may itch or burn.
- Basal cell carcinoma is a form of cancer that affects the top layer of skin. It produces painful bumps that bleed in the early stages. The associated bumps appear on sun-exposed skin and may be discolored, shiny, or scar-like.
- Squamous cell carcinoma is a type of skin cancer that begins in the squamous cells. These cells make up the outermost layer of skin. The condition causes scaly, red patches and raised sores to develop on the skin. These abnormal growths often form in areas exposed to ultraviolet radiation.
- Melanoma is the least common but most serious form of skin cancer.
 It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
It begins as an atypical mole. Cancerous moles are often asymmetrical, multi-colored, and large, with irregular borders. They can appear anywhere on the body.
Most skin bumps are harmless and aren’t cause for concern. However, you should see your doctor if:
- skin bumps change or worsen in appearance, or last for a long time
- you are in pain or they cause discomfort
- you don’t know the cause of the bumps
- you suspect you have an infection or skin cancer
Your doctor will perform a physical examination and inspect the skin bumps. Expect to answer questions about your bumps, medical history, and lifestyle habits.
Your doctor may also perform a skin biopsy to test if the skin bump is cancerous. This procedure involves taking a small sample of skin tissue from the affected area for analysis. Depending on the results, your doctor may refer you to a dermatologist or other specialist for further evaluation.
The Healthline FindCare tool can provide options in your area if you don’t already have a doctor.
Removal
Treatment for raised skin bumps depends on the underlying cause. Most of the common causes of skin bumps are harmless, so you probably won’t need treatment. However, if your skin bumps are bothering you, you might be able to have them removed for cosmetic reasons.
For example, a dermatologist can remove skin tags or warts by freezing them off. A dermatologist can also surgically remove certain skin bumps, including cysts and lipomas. Other bumps that are itchy or irritated may be treated with topical ointments and creams.
If your doctor finds that your skin bumps are cancerous or precancerous, they will most likely remove the bumps completely. You will also need to attend regular follow-up appointments so your doctor can check the area and make sure the cancer doesn’t come back.
Medication
In cases where additional medical treatment is required, your doctor will prescribe medications that can help eliminate your skin bumps and the underlying cause.
For a bacterial infection, such as MRSA, you may need antibiotics. For a viral infection, such as chickenpox, your doctor may recommend over-the-counter medications and home treatments. Some viral infections, such as herpes, can’t be cured. However, your doctor can give you medications to ease symptoms.
For most skin bumps, the long-term outlook is excellent. The majority of bumps are caused by harmless, temporary conditions that don’t require treatment. If skin bumps are caused by an infection or long-term condition, timely medical treatment should either clear it up or effectively ease the symptoms. The outlook is also good when skin cancer is caught early. However, frequent follow-ups will be necessary to ensure the cancer doesn’t return or grow. The outlook for more advanced forms of skin cancer varies with each situation.
Keratosis Pilaris (Chicken Skin): Pictures, Causes, and Treatment
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission. Here’s our process.
Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.Keratosis pilaris happens when hair follicles become plugged up with dead skin cells, causing bumps.
Keratosis pilaris, sometimes called “chicken skin,” is a common skin condition that causes patches of rough-feeling bumps to appear on the skin. These tiny bumps or pimples are actually dead skin cells plugging hair follicles. They sometimes appear red or brown in color.
These tiny bumps or pimples are actually dead skin cells plugging hair follicles. They sometimes appear red or brown in color.
Keratosis pilaris is commonly found on the upper arms, thighs, cheeks, or buttocks. It isn’t contagious, and these bumps don’t usually cause any discomfort or itching.
This condition is known to worsen in the winter months when the skin tends to dry out and may also worsen during pregnancy.
There’s no cure for this harmless, genetic skin condition, but there are some ways to treat it or prevent it from getting worse. Keratosis pilaris will usually clear up naturally by the time you reach 30 years old.
Here’s everything you need to know about this skin condition.
The most notable symptom of keratosis pilaris is its appearance. The visible bumps appearing on the skin resemble that of goosebumps or the skin of a plucked chicken. For this reason, it’s commonly known as “chicken skin.”
The bumps can appear anywhere on the skin where hair follicles exist and, therefore, will never appear on the soles of your feet or palms of your hands. Keratosis pilaris is commonly found on the upper arms and thighs. In excess, it can extend to the forearms and lower legs.
Keratosis pilaris is commonly found on the upper arms and thighs. In excess, it can extend to the forearms and lower legs.
Other symptoms associated with it include:
- slight pinkness or redness around bumps
- itchy, irritable skin
- dry skin
- bumps that feel like sandpaper
- bumps that can appear in different colors depending on skin tone (flesh-colored, white, red, pink, brown, or black)
Not sure if you have keratosis or psoriasis? We break down the differences here.
This benign skin condition is the result of a buildup of keratin, a hair protein, in the pores.
If you have keratosis pilaris, the keratin of your body hair gets clogged in the pores, blocking the opening of growing hair follicles. As a result, a small bump forms over where a hair should be. If you were to pick at the bump, you may notice a small body hair emerge.
The exact cause of keratin buildup is unknown, but doctors think it may be associated with skin conditions such as atopic dermatitis and genetic diseases.
Who can develop keratosis pilaris?
Chicken skin is common in women, children or teenagers, and those of Celtic ancestry, as well as those with:
- dry skin
- eczema
- ichthyosis
- hay fever
- obesity
Anyone can be susceptible to this skin condition, but it’s most common in children and teenagers. Keratosis pilaris often begins in late infancy or during adolescence. It typically clears up in one’s mid-20s, with most cases completely gone by the age of 30.
Hormonal changes can cause flare-ups during pregnancy and during puberty. Keratosis pilaris is most common in people with fair skin.
Keratosis pilaris is diagnosed based on medical history and a physical exam. A skin doctor, known as a dermatologist, can typically confirm the diagnosis just by looking at the affected area. Factors that go into the diagnosis include:
- your age
- what it looks like
- which areas it affects
No formal testing exists to confirm the diagnosis.
There’s no known cure for keratosis pilaris. It usually clears up on its own with age. There are some treatments you can try to alleviate the look of it, but keratosis pilaris is typically treatment-resistant. Improvement may take months, if the condition improves at all.
Dermatological treatments
Your dermatologist may recommend a moisturizing treatment to soothe itchy, dry skin and improve the skin’s appearance from the keratosis rash. Many over-the-counter and prescription topical creams can remove dead skin cells or prevent hair follicles from being blocked. A doctor or healthcare professional can determine the best treatment for you.
If you don’t already have a dermatologist, our Healthline FindCare tool can help you connect to physicians in your area.
Two common ingredients within moisturizing treatments are urea and lactic acid. Together, these ingredients help to loosen and remove dead skin cells and soften dry skin. Other treatment methods a dermatologist may suggest include:
- microdermabrasion, an intense exfoliating treatment
- chemical peels
- retinol creams
Be wary of the ingredients in these creams, though, and talk with a doctor before using them. Some prescription topical creams include acids that may cause negative side effects, including:
Some prescription topical creams include acids that may cause negative side effects, including:
- redness
- stinging
- irritation
- dryness
There are also some experimental treatment options available, such as photopneumatic therapy and vascular laser treatment.
Keratosis pilaris isn’t preventable. But following a gentle skin care routine can help prevent flare-ups and minimize its appearance. For example, using an oil-free cream or ointment to moisturize your skin can help prevent the clogged pores that contribute to keratosis pilaris.
If you don’t like the look of your keratosis pilaris, there are some techniques you can try to treat it at home. Although the condition can’t be cured, self-care treatments can help minimize bumps, itching, and irritation.
- Take warm baths: Taking short, warm baths can help unclog and loosen pores. It’s important to limit your time in the bath, though, as longer wash times can remove the body’s natural oils.

- Exfoliate: Daily exfoliation can help improve the appearance of the skin. Dermatologists recommend gently removing dead skin with a loofah or pumice stone, which you can purchase online.
- Apply hydrating lotion: Lotions with alpha hydroxy acid such as lactic acids can hydrate dry skin and encourage cell turnover. Some dermatologists recommend products such as Eucerin Advanced Repair and AmLactin, which you can purchase online. Glycerin, found in most beauty supply stores, can also soften bumps, while rose water can soothe skin inflammation.
- Avoid tight clothes: Wearing tight clothes can cause friction that can irritate the skin.
- Use humidifiers: Humidifiers add moisture to the air in a room, which can maintain the moisture in your skin and prevent itchy flare-ups.
Keratosis pilaris, a skin condition often referred to as “chicken skin” due to its appearance, commonly affects people at a young age.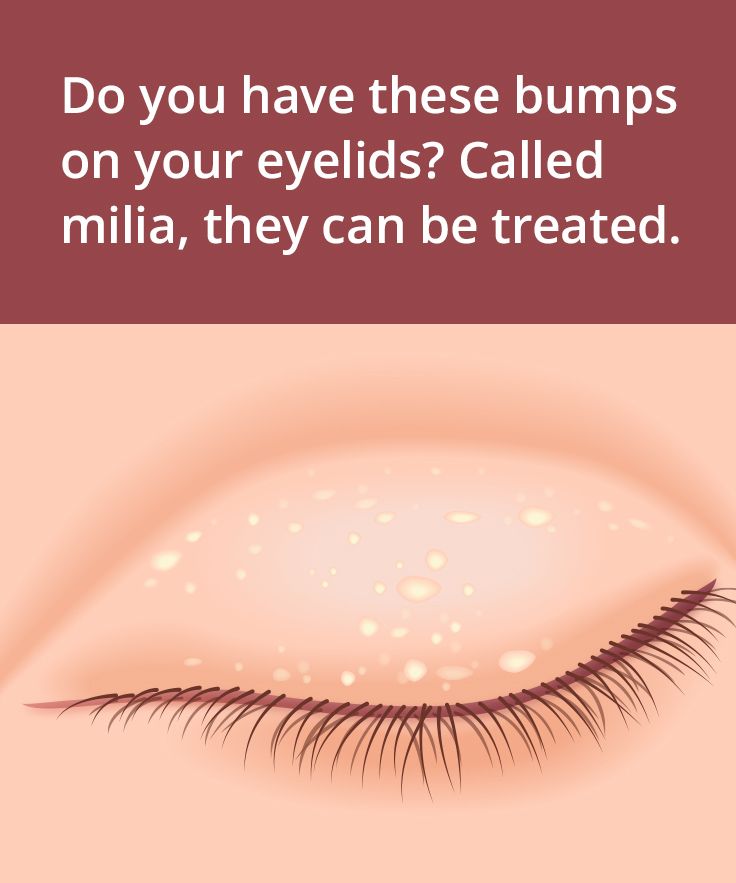 While there’s no cure, it tends to go away on its own by the time you reach 30 years old.
While there’s no cure, it tends to go away on its own by the time you reach 30 years old.
In the meantime, certain steps can help you manage it. Work with a dermatologist to discover the best ways to treat it.
Read this article in Spanish.
causes of development, diagnosis, treatment - Omega-Kyiv reference book
Synovial cyst of the wrist or hygroma is a benign formation with a gel-like or liquid content. It looks like a round-shaped lump ranging in size from 1-2 to 5-6 cm. At the initial stage, it does not hurt and does not interfere, causing only aesthetic discomfort. As the tumor grows, it can press on numerous nerve fibers in the tissues of the hand, causing pain. Soreness and ugly appearance encourages the patient to get rid of the annoying defect. Why hygroma appears, how to treat it, and in the future to avoid relapse - read about this in our article. nine0003
How does hygroma occur?
Synovial fluid, being in the capsule of the joint of the hand, flows from one area to another in case of excessive load. The capsule, stretching, forms a protrusion in the form of a bump. The flow of joint fluid is unidirectional - from the joint into the cavity of the neoplasm. Over time, if you continue to load the arm, the protrusion will grow and may detach from the joint capsule, forming a cyst - a closed cavity. Inside the cyst, the synthesis of synovial fluid continues, which contributes to the further growth of the neoplasm. nine0003
The capsule, stretching, forms a protrusion in the form of a bump. The flow of joint fluid is unidirectional - from the joint into the cavity of the neoplasm. Over time, if you continue to load the arm, the protrusion will grow and may detach from the joint capsule, forming a cyst - a closed cavity. Inside the cyst, the synthesis of synovial fluid continues, which contributes to the further growth of the neoplasm. nine0003
Synovial cyst occurrence factors
- Age, sex: young women from 20 to 40 years old are most often affected by the disease.
- Susceptibility to chronic traumatization of the hands (carrying a child in her arms, sports, professional activities).
- Increased elasticity of the connective tissue, excessive joint mobility.
- Heredity: hygromas in close relatives.
Diagnosis of hygroma
An orthopedic surgeon can diagnose hygroma by the appearance and complaints of the patient. Most often it is a hard and elastic formation, not fixed to the skin, single or multi-chamber, which is easily displaced by 1-3 cm in any direction.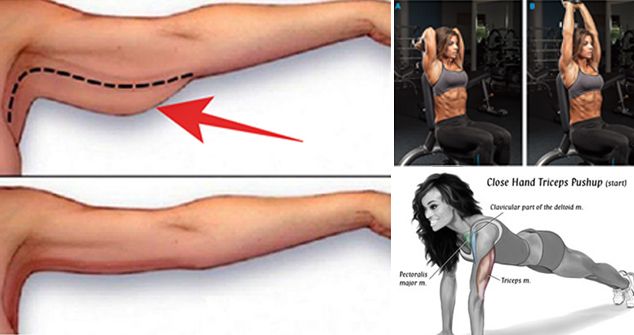 Sometimes the hygroma cannot be felt. The movement of the hand, especially in extreme positions, causes pain of a dull and aching nature. nine0003
Sometimes the hygroma cannot be felt. The movement of the hand, especially in extreme positions, causes pain of a dull and aching nature. nine0003
To confirm the diagnosis, instrumental methods are used:
- Ultrasound of the soft tissues of the hand is the most accessible and informative type of diagnosis. Well visualizes the cyst, allows you to determine the homogeneity of its structure, fullness of fluid, the presence of blood vessels in the walls of the tumor.
- Radiography - to exclude osteoarticular pathologies (arthrosis, exostosis).
- MRI - to detect very small hygromas, for differential diagnosis with Kienböck's disease and with suspicion of an oncological nature of the tumor. nine0012
- Puncture of a cyst with subsequent analysis of its contents.
Is hygroma dangerous?
Hygroma (if it really is) is not life-threatening, it is a completely benign formation without the risk of rebirth. Malignant tumors with localization on the hand are rare. They are more painful, quickly increase in size and fuse with the skin (the skin can neither be lifted nor moved over the tumor).
They are more painful, quickly increase in size and fuse with the skin (the skin can neither be lifted nor moved over the tumor).
Treatment of hygroma
In 40% of cases, the cyst ruptures with the outpouring of its contents into the joint cavity - and the hygroma disappears without any intervention (self-healing). True, cases of its repeated formation (relapse) are not uncommon. nine0003
If the bump itself does not resolve, there are three options for treating hygroma:
- Conservative, with the help of medicines (tablets, ointments - anti-inflammatory, analgesic, absorbable), physiotherapy. It is used for small tumors (up to 1-2 cm), not complicated by purulent processes. With the help of non-surgical treatment, you can slow down the growth of hygroma, reduce its size.
- Mechanical crushing (the method is used for small formations). The hygroma is pressed into the joint cavity, the cyst shell bursts, and the contents spread over the surrounding tissues.
 After the manipulation, anti-inflammatory drugs and wearing an orthosis are prescribed. Among the disadvantages: the procedure is accompanied by rather strong pain, besides, there is a high probability of recurrence - from 20 to 60%, as well as the development of complications in the form of traumatic inflammation, microbes entering tissues, and even sepsis. nine0012
After the manipulation, anti-inflammatory drugs and wearing an orthosis are prescribed. Among the disadvantages: the procedure is accompanied by rather strong pain, besides, there is a high probability of recurrence - from 20 to 60%, as well as the development of complications in the form of traumatic inflammation, microbes entering tissues, and even sepsis. nine0012 - Puncture: the contents of the lump under local anesthesia are pumped out with a syringe, followed by the introduction of medicines (hormonal agents, sclerosing drugs, antibiotic solutions). You can also make a simple aspiration of the hygroma, without the introduction of drugs. The recurrence rate is 15-50%.
- Surgical intervention (excision with a scalpel or laser beam) is the most effective way to get rid of the hygroma. During the operation, the hygroma capsule is completely removed along with the contents, and the excised tissues are sent for analysis for histology. Relapses happen, but only in 10-20% of cases.
 nine0012
nine0012
Prevention
- Exclusion of injury to the wrist and hand.
- Timely treatment of inflammatory processes in the joints (bursitis, tendovaginitis).
- When playing sports: to minimize stress on the hands and wrists, strengthen the muscles of the shoulder girdle and monitor posture during arm exercises. To avoid recurrence after removal of the hygroma, a bandage should be worn for training.
Although hygroma does not pose a threat to health, this defect can cause discomfort, affect the functionality of the hand and have an unaesthetic appearance. It is quite possible to get rid of it, while it is important to follow all the doctor's recommendations for treatment and prevention. nine0003
12 reasons why you have small bumps on your face - Kavun City
Rest assured that you are not alone if you notice a few small bumps on your face. The good news is that most of these buds, which come in many shapes, colors, and textures, are completely harmless. You can easily identify some of them as pimples, while others will require detective work and a doctor to figure out what they really are. In some cases, this may be a sign of a more serious concern. nine0072
You can easily identify some of them as pimples, while others will require detective work and a doctor to figure out what they really are. In some cases, this may be a sign of a more serious concern. nine0072
In general, as long as the bump on your face isn't bleeding, darkening, or changing, it probably doesn't need any medical attention, says Joel Schlessinger, MD, dermatologist and RealSelf consultant. Some bumps, like acne, can often be treated at home or by a dermatologist with a skincare regimen, he says.
But "if the bump changes color or shape, bleeds or grows in size rapidly, it's time to schedule an appointment with a board-certified dermatologist to check it out," says Dr. Schlessinger. These are signs that the bump may be related to an underlying health problem (more on that in a moment), so it's important to pay attention to it. nine0003
Of course, it may be inconvenient for you to make an appointment in person right now because of the pandemic. Many doctors, including dermatologists, can help with virtual sessions, depending on your specific concerns. (Here are some helpful tips on how to make an appointment with your doctor during a pandemic.) If you're worried about any abnormalities, call your dermatologist or your GP if possible to discuss the problem.
(Here are some helpful tips on how to make an appointment with your doctor during a pandemic.) If you're worried about any abnormalities, call your dermatologist or your GP if possible to discuss the problem.
But again, many small bumps are harmless. The following information can help you determine what type of bumps you have and whether they should be reported to your doctor. nine0003
1. Comedones
These common bumps can appear on the face and other parts of the body and are divided into two groups: closed comedones (better known as white dots) and open comedones (black dots).
"They look like pores clogged with excess oil and dead skin cells," says Dr. Schlessinger. The difference is that "blackheads have an open comedone, so fatty and dead cells are oxidized, turning brown or black," he explains. Whiteheads, on the other hand, are closed, causing the cocktail inside to appear white, pinkish, or flesh-colored. nine0003
How to treat and prevent comedones
While not harmful, these bumps can be annoying. To manage them (and prevent full blown breakouts), Dr. Schlessinger recommends always washing your face before bed with a cleanser containing at least 2% salicylic acid (available over the counter). It dissolves dead skin cells, clears clogged pores, and helps prevent future breakouts. Neutrogena Oil-Free Acne Wash is affordable and recommended by experts. Retinoids, benzoyl peroxide, azelaic acid, and oral antibiotics (which are required by prescription) may also be helpful. A dermatologist can help put together a skin care regimen that makes sense for you if over-the-counter products aren't working. Be patient and give the medication time to work - for example, using salicylic acid to reduce acne can take several weeks. nine0003
To manage them (and prevent full blown breakouts), Dr. Schlessinger recommends always washing your face before bed with a cleanser containing at least 2% salicylic acid (available over the counter). It dissolves dead skin cells, clears clogged pores, and helps prevent future breakouts. Neutrogena Oil-Free Acne Wash is affordable and recommended by experts. Retinoids, benzoyl peroxide, azelaic acid, and oral antibiotics (which are required by prescription) may also be helpful. A dermatologist can help put together a skin care regimen that makes sense for you if over-the-counter products aren't working. Be patient and give the medication time to work - for example, using salicylic acid to reduce acne can take several weeks. nine0003
It is also important not to use blackhead removal strips. "The glue used to stick them to the skin can damage the complexion," says Dr. Schlessinger. “In addition, they cleanse the skin of natural oils and usually only successfully remove the tops of blackheads, keeping pores clogged and leaving the problem unresolved. ”
”
2. Inflamed pimples
You know you have one of these when you notice a painful bump on your face, sometimes with a large white head and possibly a red circle around it. This happens when the bacteria in our pores start to mix with the excess buildup of dead skin cells and oil that causes acne. Inflamed pimples are often red, painful, swollen, and sometimes filled with pus. nine0003
If you have inflammatory pimples, whatever you do, do not pop them, as this can lead to more redness and inflammation. It can also increase the risk of scarring, says Jerome Garden, MD, a dermatologist and director of the Institute for Laser and Dermatology Medicine in Chicago.
How to Treat and Prevent Inflamed Pimples
To try and reduce these pimples, Dr. Garden recommends using a gentle cleanser containing benzoyl peroxide and oil-free skin care products. You can also add some anti-inflammatories: “Once a pimple has formed, a safe way to quickly reduce inflammation is to mix a 1% hydrocortisone cream and benzoyl peroxide cream and apply to the pimple twice a day until the inflammation has resolved,” he says. Cerave Hydrocortisone Cream 1% and La-Roche Posay Effaclar Duo Acne Treatment with Benzoyl Peroxide are two good options. nine0003
Cerave Hydrocortisone Cream 1% and La-Roche Posay Effaclar Duo Acne Treatment with Benzoyl Peroxide are two good options. nine0003
3. Milia
If you've ever noticed a few tiny white dot-like bumps on your face that didn't budge no matter how many times you tried to wash them off with an acne cleanser, they probably were harmless cysts known as milia.
These keratin-filled cysts “commonly appear around the eyes, cheeks, and nose, can occur in any skin type or color, and tend to be very common in newborns,” explains Dr. Schlessinger. “Milia often appear without any specific cause, although they are more common in people with skin conditions such as rosacea, as well as those with excessive sun damage, skin injuries such as burns, or those whose pores are chronically clogged with oil, cosmetics, and skin care products.” nine0003
How to Treat and Prevent Milia
Milia are basically dead skin cells stuck under the skin and are not harmful. But if you want to try and get rid of them, Dr. Schlessinger recommends choosing products with alpha hydroxy acids (AHAs) like glycolic or lactic acid to exfoliate your skin. A good option is L'Oréal Revitalift Derm Intensives 10% Pure Glycolic Acid Serum. In addition, a dermatologist can remove milia with a small incision. nine0003
But if you want to try and get rid of them, Dr. Schlessinger recommends choosing products with alpha hydroxy acids (AHAs) like glycolic or lactic acid to exfoliate your skin. A good option is L'Oréal Revitalift Derm Intensives 10% Pure Glycolic Acid Serum. In addition, a dermatologist can remove milia with a small incision. nine0003
4. Keratosis pilaris
These tiny, goosebump-like marks usually appear on the thighs and upper arms, says Dr. Schlessinger, but they can also appear on your face. Sometimes they can also be hereditary, and although they can appear at any age, they are usually more common in children.
"Keratosis pilaris bumps can be confused with goosebumps or even pimples, but they are actually caused by small plugs of dead cells that block the hair follicle," Dr. Schlessinger explains. "They don't pose a health risk and don't require treatment, but regular skin exfoliation can help reduce keratosis bumps." nine0003
How to treat and prevent keratosis pilaris
Doctors don't know why some people, such as people with eczema, are more likely to get keratosis pilaris, so according to the Cleveland Clinic, there is no real method of prevention. Many people find that this condition improves with age. In the meantime, Dr. Schlessinger recommends a face wash containing glycolic acid, which exfoliates the skin to visibly reduce blemishes. Dry skin can aggravate bumps, which is why the Cleveland Clinic recommends moisturizing your skin with a lotion that contains AHAs. nine0003
Many people find that this condition improves with age. In the meantime, Dr. Schlessinger recommends a face wash containing glycolic acid, which exfoliates the skin to visibly reduce blemishes. Dry skin can aggravate bumps, which is why the Cleveland Clinic recommends moisturizing your skin with a lotion that contains AHAs. nine0003
5. Moles
Whether you've had them forever or just notice that some moles appear on your skin as you age, they're completely normal and in most cases harmless. They often appear as brown, red, or flesh-colored spots or bumps on the face, as well as other parts of the body, and are quite common. In fact, according to the American Academy of Dermatological Association, almost everyone has at least one mole. nine0003
These types of bumps or spots form when melanocytes, the skin cells that produce melanin, stick together or grow in clusters rather than spreading. Experts aren't entirely sure what causes moles to form, but sun exposure is thought to increase the number of moles on your skin, AAD explains.
"Moles can be flat or raised and, if harmless, are usually round," says Dr. Schlessinger. AAD explains that it is normal for them to lighten or darken with age. A mole that does not pose a risk for cancer does not require treatment or removal. nine0003
How to treat and prevent moles
Ordinary moles do not usually require treatment. According to the AAD, dermatologists remove moles for cosmetic reasons if the mole rubs against your clothes and it bothers you, or if they suspect the mole may be skin cancer. Dr. Schlessinger warns that if a mole starts to change or grow in size, it could be a sign of something more serious, especially skin cancer. The Mayo Clinic also reports that the mole is asymmetrical, irregularly bordered, variable or uneven in color, and is over a quarter of an inch in diameter. (This is a good time to talk about the importance of using sunscreen. If you don't have one you like, this story will help you figure out what works best for your needs. Minimum SPF 30 every day.)
Minimum SPF 30 every day.)
6. Papular dermatosis black (PCHD)
These are not moles, but a different type of skin bump: papular dermatosis black (PKD), which are completely benign and harmless skin patches characteristic of darker skin tones that usually found in families. According to Dr. Garden, these spots are technically not moles and cannot become cancer. "Moles are deeper in the skin, but PSCs are a very superficial collection of epidermal cells and usually start to appear around the age of 20," he says. “These brown bumps can be very small and not grow more than a few millimeters; however, one person can have dozens of spots on their face.” nine0003
How to treat and prevent
If you think you may have PCD, you can call your dermatologist to confirm your suspicion. There is little you can do to prevent it from forming or becoming more visible other than using sunscreen and practicing sun protection. Sunscreen is an important part of any skin care routine to help prevent skin cancer, so it's important to choose the one you like.
If you already have bumps, you can try an over-the-counter face wash that contains salicylic acid or glycolic acid, which are "mild chemical exfoliators that can reduce or completely erase these bumps," adds Dr. Garden. "In addition, prescription retinoids also have the potential to reduce the appearance of PSHD, although they are unlikely to be removed." nine0003
You can also gently remove these spots by a certified dermatologist with a laser or moxibustion. However, people with dark skin can develop hyperpigmentation due to laser use, so you should talk to your doctor about the best treatment for you.
7. Skin tags
These are usually benign oval-shaped lesions that are connected to the skin of the body or face through a stalk. They are soft to the touch and typically appear on the neck, upper chest, eyelids, groin, and underarms, according to Dr. Schlessinger. Skin tags tend to develop in older adults, according to Mount Sinai Health, which experts say can form when skin rubs against each other. nine0003
nine0003
How to Treat and Prevent
Skin tags are completely harmless unless they grow quickly, change color, become infected, or cause pain. "It's very common for me to have patients who think they have some sort of 'skin marks' but it's actually skin cancer or some other, more dangerous condition," says Dr. Schlessinger. Therefore, if any dangerous changes are found on your skin tag (for example, moles), if possible, contact a dermatologist to have it checked. nine0003
However, if your skin tags don't bother you, there's no reason to remove them. "But for aesthetic purposes, a dermatologist can remove them by cutting them off or cauterizing them with heat," says Dr. Schlessinger.
8. Allergic reaction
Sometimes bumps on the face or other parts of the body can be the result of an allergic reaction to something you have eaten or worn, or to a product you have applied.
In some cases, the marks on your body may be hives, which are red, itchy, or welts that suddenly appear when exposed to an allergen. If the hives are mild, Dr. Schlessinger recommends simply treating it at home with a cool bath, over-the-counter allergy medication, or applying cool compresses to the site. If the hives are more severe, or you are also experiencing shortness of breath, swelling, or difficulty breathing, call your doctor or the emergency room if you do not have one. nine0003
If the hives are mild, Dr. Schlessinger recommends simply treating it at home with a cool bath, over-the-counter allergy medication, or applying cool compresses to the site. If the hives are more severe, or you are also experiencing shortness of breath, swelling, or difficulty breathing, call your doctor or the emergency room if you do not have one. nine0003
Another type of common allergic reaction or skin sensitivity that occurs on the skin is known as irritant contact dermatitis. It is markedly different from urticaria in that it is more of a general redness than individual welts. It is also the result of direct skin contact with things like poison ivy, jewelry, or ingredients in skincare or cosmetics.
How to treat and prevent allergic reactions
This is probably obvious, but you should definitely stop using or coming into contact with whatever is causing your reaction if you can pinpoint the source. To determine the cause of an allergy, it's helpful to think about any recent changes you've made, such as a new cleanser, shower gel, or deodorant. Then try not to scratch the area so that the damaged skin can begin to heal. You can take an oral antihistamine and use an over-the-counter hydrocortisone balm, according to Dr. Schlessinger. nine0003
Then try not to scratch the area so that the damaged skin can begin to heal. You can take an oral antihistamine and use an over-the-counter hydrocortisone balm, according to Dr. Schlessinger. nine0003
If this tactic doesn't work, talk to your dermatologist, who may prescribe a stronger anti-itch or a corticosteroid shot to calm the inflammation.
9. Bumps due to eczema
This common skin condition, also called atopic dermatitis, usually appears before the age of five, but technically can occur at any age. "Eczema often appears as oozing or crusted bumps, patches, or plaques, and when chronic, even as thick scales, and results from the interaction of both genes and the environment," said Jeremy A. Brower, MD, a dermatologist at New York. nine0003
There are several types of eczema, but it usually occurs when the top layer of skin cannot retain moisture and protect you from irritants, allergens, and environmental elements. And, as we just explained, this condition goes beyond dry skin and can cause severe discomfort to people suffering from this condition.![]()
How to treat and prevent eczema
You can't prevent this condition, but you can manage the flare-ups. You can talk to your doctor to confirm that you have eczema so that you can find the right treatment together. Several factors, including a patient's age and their symptoms, can affect treatment, which usually includes oral, topical, or injectable medications. "In many cases, changing environmental factors - avoiding known triggers, changing bathing habits - can relieve symptoms," says Dr. Brouwer. nine0003
He recommends that patients choose shorter, warm showers using gentle, unscented products followed by moisturizing. He also suggests washing your clothes with a cleanser for sensitive skin, as well as washing your hands less frequently or making sure to use a moisturizer afterwards. The Cleveland Clinic also recommends using a humidifier at night, applying a moisturizer (more effective than lotion) several times a day, and using a cortisone cream to help relieve symptoms. nine0003
nine0003
10. Rosacea bumps
Dr. Garden says that another chronic inflammatory condition, rosacea, usually appears on the face. "It tends to cause background redness of the cheeks, nose, chin and lower forehead, as well as pimples in some patients."
How to treat and prevent rosacea
Unfortunately, no one knows what causes rosacea, and there is no complete cure for it yet. However, there are ways to reduce the inflammation that causes redness and bumps. “People with rosacea tend to have more sensitive skin on the affected areas of the face, so it’s helpful to replace harsh soaps with gentle cleansers and light moisturizers,” says Dr. Garden. "Sun protection is also paramount for rosacea, as UV exposure exacerbates inflammation." nine0003
But everyone has their own set of triggers, which can include things like alcohol, exercise, and certain skincare or makeup ingredients. Therefore, it is important to control the impact of these triggers as much as possible.
There are some other treatment options such as topical azelaic acid, topical prescriptions, and oral antibiotics that your dermatologist can refer you to. Because there are many skin conditions that can mimic rosacea, such as acne, eczema, and lupus, it's important to consult with a board-certified dermatologist who can identify your bumps before embarking on self-treatment at home. nine0003
11. Bumps due to ingrown hairs
Most of us have had ingrown hairs on our body or face at some point as a result of hair removal. Usually, when the hair grows back, it grows up and over the skin. But if it starts to curl up instead, it can get stuck and form a small, raised, reddened bump that may or may not be filled with pus. People with thick curly hair have more ingrown hairs than people with thin hair, but no one is completely immune. nine0003
How to treat and prevent the bumps associated with ingrown hairs
The best way to prevent ingrown hairs is not to wax, shave or tweeze, but this is not always a practical option for some people who are committed to hair removal, explains Dr. Garden. Another way to reduce ingrown hairs is to always wash your skin with mild soap and rub in a lubricating cream gel before shaving.
Garden. Another way to reduce ingrown hairs is to always wash your skin with mild soap and rub in a lubricating cream gel before shaving.
"If your razor has been used a few times, replace it with a new one, as dull blades don't make clean, precise cuts and can increase the risk of ingrown hairs," says Dr. Garden. nine0003
Another long-term solution is laser hair removal, which completely removes hair at a deeper level, damaging the hair follicle. “Laser hair removal requires multiple treatments over several weeks and months, but the results are usually semi-permanent, although it is less effective on light or very light hair,” says Dr. Garden. "Because there are powerful lasers involved and risks including skin discoloration, burns, and even scarring, it's important to find a board-certified dermatologist experienced with lasers." African Americans, Native Americans, and/or people with dark skin tones should make sure their doctor is experienced in treating dark skin, as some lasers can only be used on fair skin, according to the Cleveland Clinic. But again, this option is not an easy decision and you may not be able to schedule electives during a pandemic. nine0003
But again, this option is not an easy decision and you may not be able to schedule electives during a pandemic. nine0003
- Lipoma
A lipoma is a growth of fatty tissue that can occur almost anywhere on the body (including the face), but is most common on the chest, back, shoulders, neck, and armpits. “While they tend to grow slowly, often over months or years, you will notice them as a rubbery bulge under the skin that is usually less than 2 inches across and seems to move,” explains Dr. Garden. "Sometimes larger lipomas occur, some reaching almost 8 inches in diameter, although this is rare." nine0003
The good news is that lipomas are almost always benign. However, there is a very rare form of cancer known as liposarcoma, which occurs in fatty tissue and can look like a deep lipoma, explains Dr. Garden. Therefore, if you notice something like a lipoma that is painful or growing rapidly, it should be checked out by a dermatologist who will determine if a biopsy is needed.