Placenta during pregnancy
What complications can affect the placenta?
Complications that can affect the placenta during pregnancy or childbirth include:
- low-lying placenta and placenta praevia
- retained placenta – when part of the placenta remains in the womb after giving birth
- placental abruption – when the placenta starts to come away from the wall of the womb
These complications aren't common.
Low-lying placenta and placenta praevia
As your pregnancy progresses, your womb expands and this affects the placenta's position. The area where the placenta is attached usually stretches upwards, away from your cervix.
If the placenta stays low in your womb, near to or covering your cervix, it may block the baby's way out.
This is called low-lying placenta if the placenta is less than 2cm from the cervix, or placenta praevia if the placenta is completely covering the cervix.
Placenta praevia, where the cervix is completely covered at the end of pregnancy, affects about 1 in every 200 births.
The position of your placenta will be recorded at your 18- to 21-week ultrasound scan.
If your placenta is significantly low, you'll be offered an extra ultrasound scan later in your pregnancy (usually at about 32 weeks) to check its position again.
For 9 in every 10 women, the placenta will have moved into the upper part of the womb by this point.
If the placenta is still low in your womb, there's a higher chance that you could bleed during your pregnancy or during your baby's birth. This bleeding can be very heavy and put you and your baby at risk.
You may be advised to come into hospital at the end of your pregnancy so emergency treatment (such as a blood transfusion) can be given very quickly if you bleed.
If the placenta is near or covering the cervix, your baby can't be delivered through the vagina, so a caesarean section will be recommended.
A low-lying placenta can be associated with painless, bright red bleeding from the vagina during the last 3 months of pregnancy. If this happens to you, contact your midwife or GP immediately.
Retained placenta
After your baby's born, part of the placenta or membranes can remain in the womb. This is known as retained placenta. If untreated, a retained placenta can cause life-threatening bleeding.
Breastfeeding your baby as soon as possible after the birth can help your womb contract and push the placenta out.
Your midwife may also ask you to change your position (for example, by moving to a sitting or squatting position). In some cases, you may be given an injection of a medicine to help your womb contract.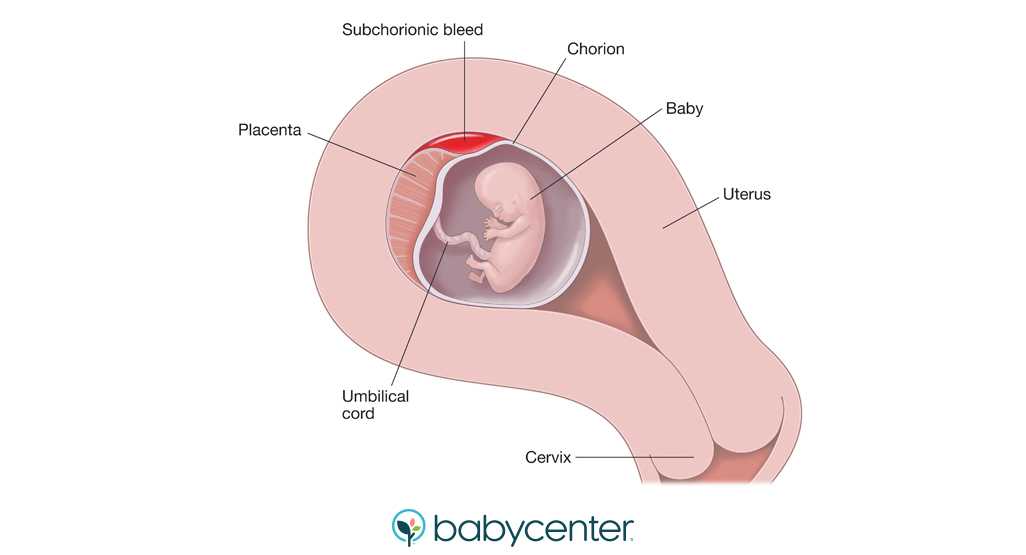
If these methods don't work, a doctor may need to remove the placenta by hand. This can be painful, so you'll be given an anaesthetic.
Placental abruption
Placental abruption is a serious condition in which the placenta starts to come away from the inside of the womb wall.
It can cause stomach pain, bleeding from the vagina and frequent contractions.
It can also affect the baby, increasing the risk of premature birth, growth problems and stillbirth.
It's not clear what causes placental abruption, but factors that increase the risk include injury to the abdominal area, smoking, cocaine use and high blood pressure.
If you're near your due date, the baby will need to be born straight away and a caesarean section may be recommended.
But if the baby's very premature and the abruption is minor, you may be kept in hospital for close observation.
Always speak to your midwife or GP if you're concerned about any aspect of your health when you're pregnant. You can also call NHS 111.
Further information
- Vaginal bleeding in pregnancy
- Antenatal care
Page last reviewed: 22 August 2022
Next review due: 22 August 2025
What does the placenta do? Learn about the placenta!: Garden OB/GYN: Obstetrics
What does the placenta do? Learn about the placenta!: Garden OB/GYN: ObstetricsSave time and Text Us!
What is the placenta exactly?
The placenta is frequently talked about during pregnancy, but do you know what it is?
It’s an organ! The placenta develops when you become pregnant as a way to protect and nurture your developing baby.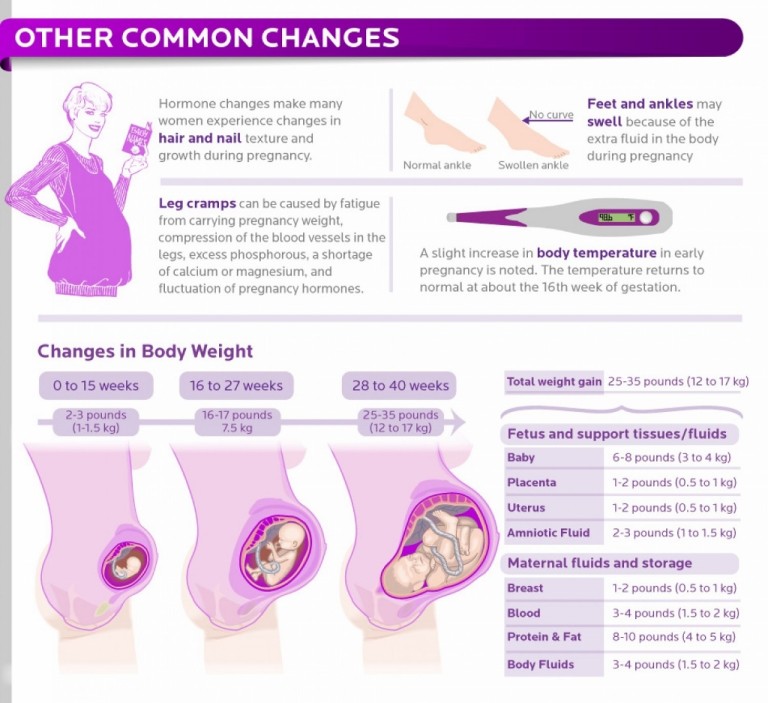 It then leaves your body through the birthing canal following the birth of your baby. It’s actually essential that the entire placenta leaves your body following birth, otherwise you may experience bleeding or an infection. So, if you were wondering if you always have a placenta your whole life, the answer is you don’t! It only exists during pregnancy.
It then leaves your body through the birthing canal following the birth of your baby. It’s actually essential that the entire placenta leaves your body following birth, otherwise you may experience bleeding or an infection. So, if you were wondering if you always have a placenta your whole life, the answer is you don’t! It only exists during pregnancy.
What is the purpose of the placenta?
Think of it as the organ of life. The mother’s placenta is connected to her baby through the umbilical cord. Through this connection, the placenta is able to filter and deliver important nutrients to the developing baby, including oxygen. The placenta also keeps your baby’s body safe and healthy by removing waste products from your baby’s blood. Amazingly, the placenta enables the support, nourishment, and protection of the baby, all without the mother’s and baby’s blood mixing, preventing infections in the baby.
Where is the placenta?
It is attached to your uterus’ wall at either the top, side, front or back.
Can there be issues with the placenta?
A condition known as placenta previa occurs if the placenta attaches to the bottom of the uterus. This condition usually resolves itself as the pregnancy progresses, but if the placenta is covering the cervix during labor, a caesarean section will be necessary.
Placenta accreta occurs if the placenta does not attach to the uterus or is improperly attached, which may result in heavy bleeding and can be life-threatening.
If you experience placental abruption, it means the placenta has become detached from the uterus prematurely, before labor. This condition will impact the delivery of nutrients to the baby and may require early delivery of the baby.
What can I do to keep my placenta healthy?
To keep your placenta and baby healthy, be sure to go to all your regular pregnancy check-ups with your obstetrician. This can ensure routine monitoring of your body and pregnancy so that any possible issues can be detected early.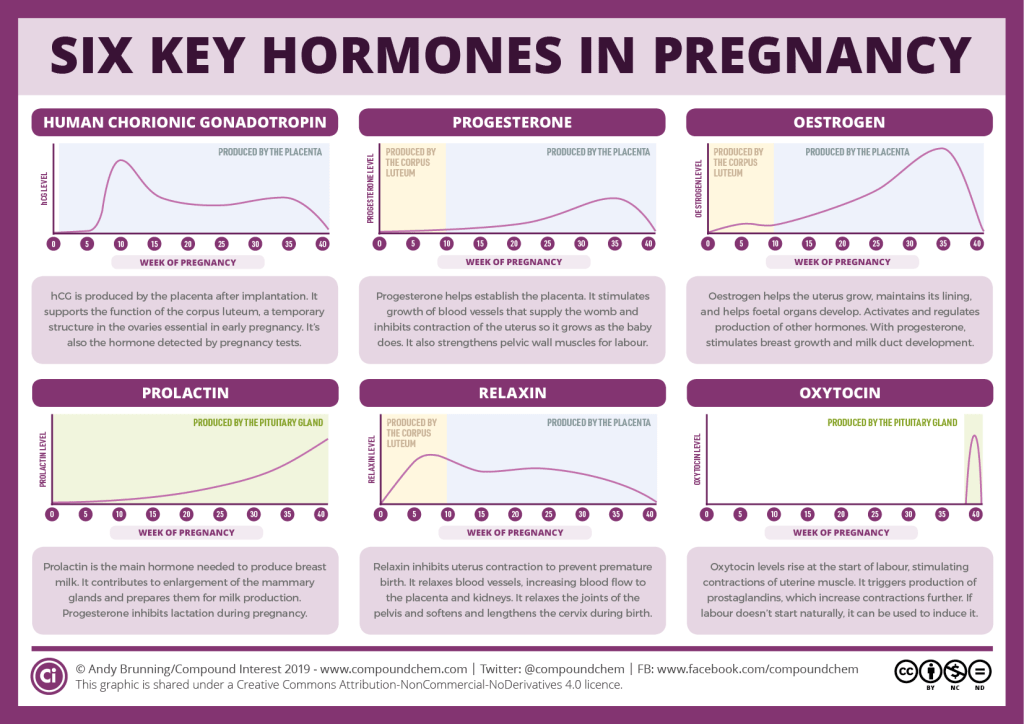
Abstain from alcohol and any drug use, including smoking cigarettes.
Notify your doctor of any medications or supplements you are taking and also be sure to inform them of any prior placenta issues you may have had with previous pregnancies.
If you have further questions about placentas and/or pregnancy, we encourage you to ask your healthcare provider or schedule a consult with one of our pregnancy expert Garden OB/GYN Obstetricians. Contact one of our office locations or book an appointment online to schedule your visit!
Sources:
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/placenta/art-20044425
https://www.pregnancybirthbaby.org.au/what-is-the-placenta
All About the Menstrual Cycle: Understanding Your Monthly Visitor
Are you tired of feeling confused about your menstrual cycle? Do you often wonder what is happening inside your body during this time of the month? Look no further! In this blog post, we will dive into the ins and outs of the menstrual cycle.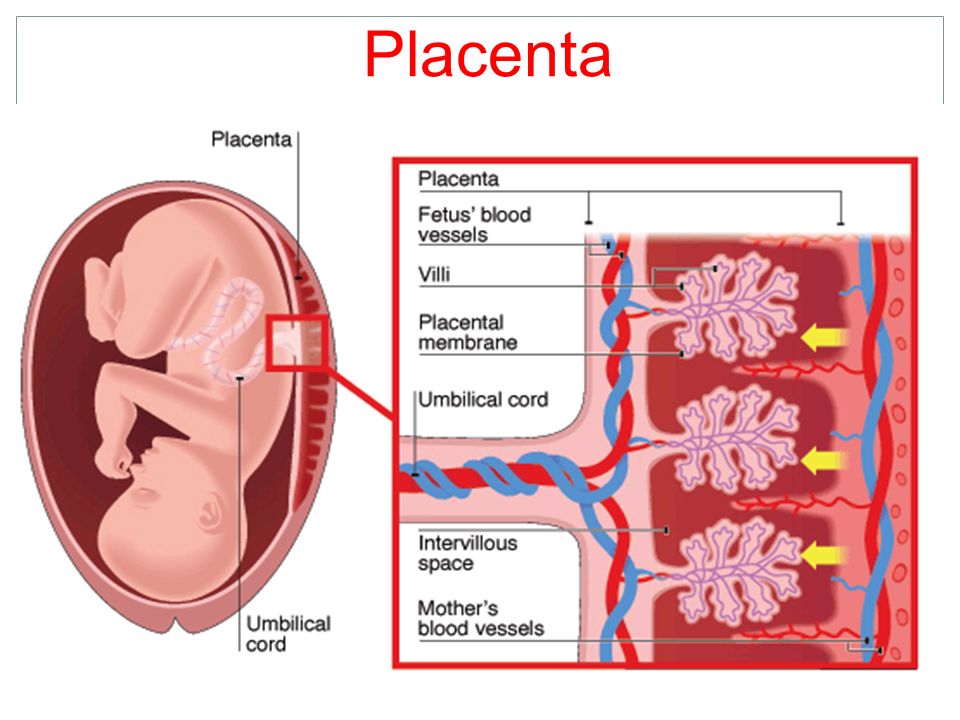
Why Do I Have Heartburn During My Pregnancy?
For many women heartburn can become quite the nuisance during pregnancy, even if they rarely experienced heartburn in the past. Many women experience frequent and/or very bothersome acid reflux.
High Blood Pressure in Pregnancies, Pre-Eclampsia and Eclampsia
If noted early in pregnancy then it is called chronic hypertension, if noted late in pregnancy it is called Pre-Eclampsia. Medicine should be started to keep the blood pressure below 140/90
New COVID-19 Protocol at Affiliated Hospitals
If you are planning to deliver a baby at Katz Women’s Hospital or a LIJ Hospital, you can visit our office to get a COVID-19 test or vaccine. To help our patients and communities stay safe, Garden OB/GYN is offering COVID-19 testing & vaccines.
Considering Sterilization or Tubal Ligation?
Considering Sterilization or Tubal Ligation? Having your partner receive a vasectomy is likely a safer, less risky, and more affordable permanent birth control option.
Maternity hospital №7, Novosibirsk - What is the placenta?
Anna Valentinovna Yakimova, obstetrician-gynecologist, MD talks about the placenta and placental insufficiency.
Picture from the site http://s7ya7.zdorovo-zivi.ru
Placenta. The name of the organ comes from lat. placenta - cake, cake, pancake. This is an extra-embryonic organ, consisting of villi, thanks to which the fetus is nourished, respired, and waste products are removed from its blood. There are free and fixing (anchor) villi. The placenta is formed in the place where the embryo was implanted, arises as a result of the connection of the chorion - extraembryonic tissue with a thickened uterine mucosa (decidual tissue).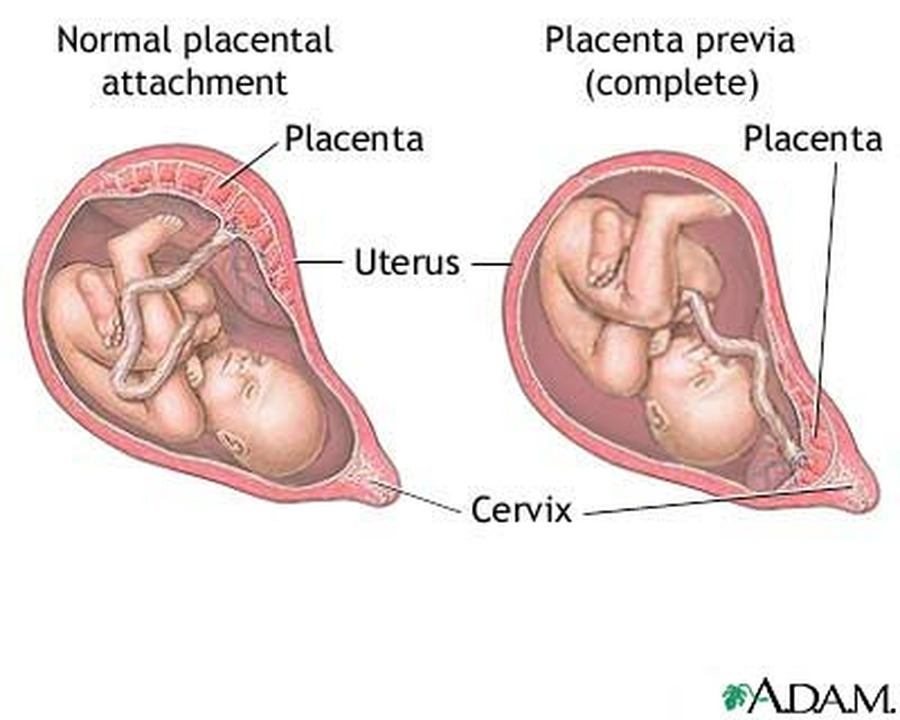 Despite the fact that the blood of the mother and fetus does not mix, as they are separated by the placental barrier, the fetus receives all the necessary nutrients and oxygen from the mother's blood. In addition, the placenta produces hormones that ensure the preservation of pregnancy. The placenta has two surfaces. The surface that faces the fetus is called the fetal. It is covered with a smooth shell - the amnion, through which large vessels shine through. The one that is attached to the wall of the uterus is called maternal.
Despite the fact that the blood of the mother and fetus does not mix, as they are separated by the placental barrier, the fetus receives all the necessary nutrients and oxygen from the mother's blood. In addition, the placenta produces hormones that ensure the preservation of pregnancy. The placenta has two surfaces. The surface that faces the fetus is called the fetal. It is covered with a smooth shell - the amnion, through which large vessels shine through. The one that is attached to the wall of the uterus is called maternal.
The main structural unit of the placenta is cotelidone. Cotyledon of the placenta is conditionally comparable to a tree. Each cotyledon is formed by a stem villus, from which, like branches of a tree, villi of the second and third order extend, containing vessels. The central part of the cotyledon forms a cavity, which is surrounded by many villi. Between the cotyledons there is a space - mejvirus, which on the maternal side is limited by partitions (septa) extending from the mucous membrane of the uterus.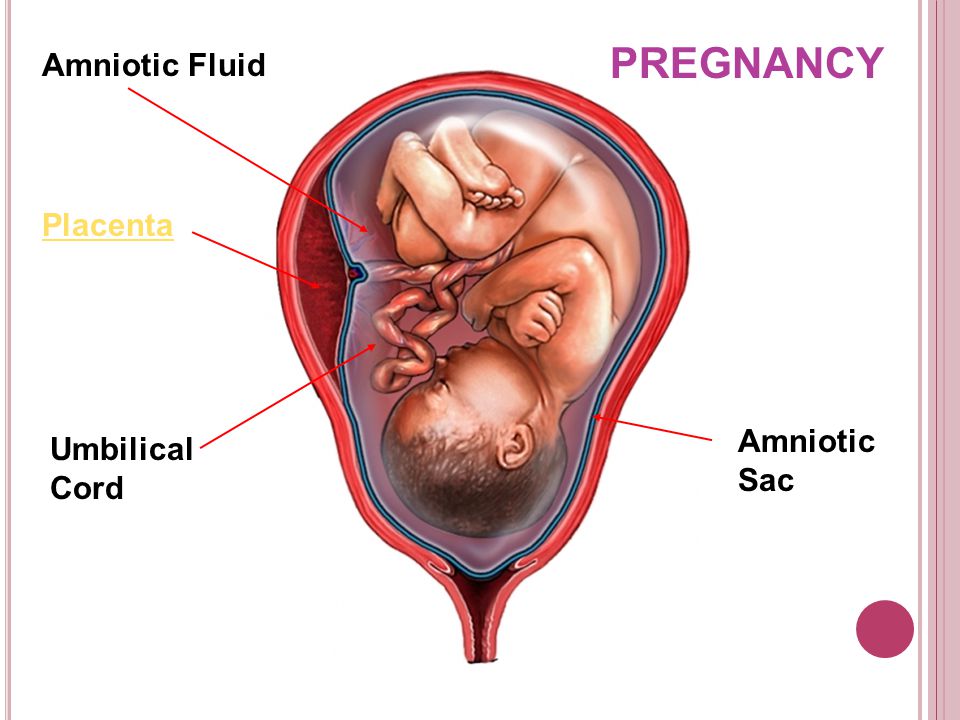 Most of the placental villi are freely immersed in the intervillous space (free villi) and are bathed in maternal blood. The spiral arteries, which are small branches of the arteries that supply the uterus, open into the intervillous space and supply oxygen-rich blood to the intervillous space. Due to the pressure difference, which is higher in the mother's arterial bed compared to the intervillous space, oxygenated blood from the mouths of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal circulation through the venous orifices through the separating septa. . In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates.
Most of the placental villi are freely immersed in the intervillous space (free villi) and are bathed in maternal blood. The spiral arteries, which are small branches of the arteries that supply the uterus, open into the intervillous space and supply oxygen-rich blood to the intervillous space. Due to the pressure difference, which is higher in the mother's arterial bed compared to the intervillous space, oxygenated blood from the mouths of the spiral arteries is directed through the center of the cotyledon to the villi, washes them, reaches the chorionic plate and returns to the maternal circulation through the venous orifices through the separating septa. . In this case, the blood flow of the mother and fetus are separated from each other. Those. maternal and fetal blood does not mix. Thus, the concept of the placental barrier appears: the blood of the mother of the fetus does not mix, because they are separated by the wall of the villus, loose connective tissue inside the villus and the wall of the vessel that is inside the villus, and in which the blood of the fetus circulates.
At the end of pregnancy, the placenta is a soft disk 15-18 cm in diameter, 2-4 cm thick in the central part, weighing about 500-600 g. their capillaries - 12 m2. The placenta, membranes, and umbilical cord together form the afterbirth, which is expelled from the uterus after the baby is born.
Normally, the placenta is attached to the uterine cavity on its anterior or posterior surface, sometimes in the fundus. If the placenta is attached in the lower part of the uterine cavity, close to the internal opening of the cervix - the internal pharynx, then its blood supply is often insufficient and the fetus may suffer from lack of oxygen and nutrients - a phenomenon called placental insufficiency occurs.
Placental insufficiency is a violation of all or some of the functions of the placenta, ultimately leading to oxygen starvation (hypoxia), fetal growth retardation or death and / or early termination of pregnancy.
Placental insufficiency may occur early in pregnancy due to impaired placental formation, for example, if the spiral arteries that supply blood to the villi do not lose the ability to narrow their lumen in response to exposure to vasoconstrictor substances.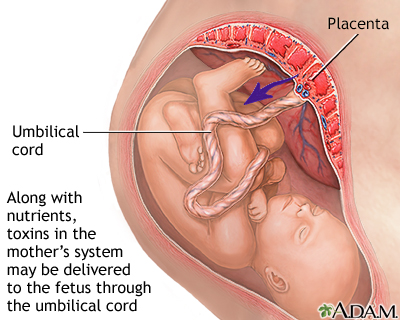 It is possible that there is a violation of the development of blood vessels inside the villi, the vessels can form in the central part of the villus, and not close to its wall, then the transfer of nutrients from the mother's blood to the fetal blood and the flow of metabolic products back will be difficult. The process of development of the placenta (in particular, vascular formation) occurs to a greater extent in the first and second trimesters of pregnancy, ending at about 30-32 weeks. After this period, involutive processes predominate ("aging", immuring the villi with fibrinoid). Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation.
It is possible that there is a violation of the development of blood vessels inside the villi, the vessels can form in the central part of the villus, and not close to its wall, then the transfer of nutrients from the mother's blood to the fetal blood and the flow of metabolic products back will be difficult. The process of development of the placenta (in particular, vascular formation) occurs to a greater extent in the first and second trimesters of pregnancy, ending at about 30-32 weeks. After this period, involutive processes predominate ("aging", immuring the villi with fibrinoid). Along with the processes of involution in the placenta during pregnancy, young villi develop, more often avascular, which, however, only partially compensate for the function of mature villi containing vessels that have “fallen out” of the circulation.
In another scenario, placental insufficiency occurs at a later date, as a result of damage to the placenta in inflammatory processes, diabetes in a pregnant woman, or high blood pressure, when blood flow to the uterus is disturbed, which can also occur with increased maternal blood clotting .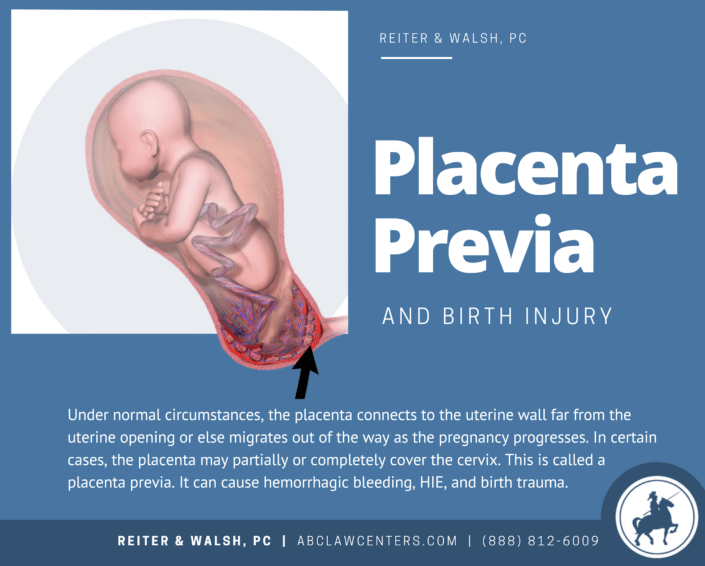 It is believed that it is the violation of the uteroplacental circulation that plays the main role in the formation of the intrauterine growth retardation syndrome. Before the advent of Doppler ultrasound research methods in obstetric practice, there were no non-invasive methods for studying blood flow in the mother-placenta-fetus system. To date, Doppler is the most preferred instrumental method that provides useful information in relation to the detection of blood flow disorders and the determination of pregnancy management tactics for placental insufficiency. If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography.
It is believed that it is the violation of the uteroplacental circulation that plays the main role in the formation of the intrauterine growth retardation syndrome. Before the advent of Doppler ultrasound research methods in obstetric practice, there were no non-invasive methods for studying blood flow in the mother-placenta-fetus system. To date, Doppler is the most preferred instrumental method that provides useful information in relation to the detection of blood flow disorders and the determination of pregnancy management tactics for placental insufficiency. If there are symptoms of placental insufficiency - a mismatch in the height of the uterine fundus, signs of a threat of early termination of pregnancy, rapid or slow fetal heart rate (normal: 120-160 beats per minute), an altered amount of amniotic fluid - it is necessary to conduct an ultrasound examination, Doppler blood flow in the vessels of the uterus, umbilical cord and fetus, and in the third trimester - cardiotocography.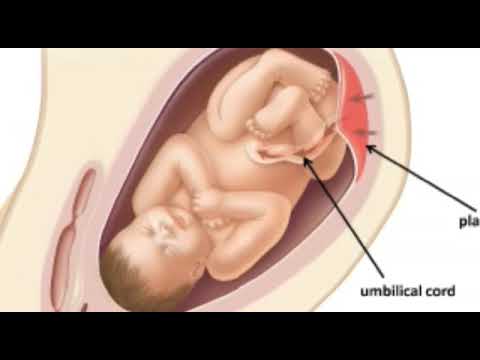 The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures.
The earliest sign of placental dysfunction is a decrease in its production of hormones and proteins, therefore, in pregnant women with a known risk of placental dysfunction (for example, if she has a chronic inflammatory process or often / constantly increased blood pressure, etc.), you can examine the level placental lactogen, progesterone, unconjugated estriol in the blood. And on the basis of the data obtained, predict the further development of pregnancy and take preventive measures.
Can placental insufficiency be treated? The answer to this question is ambiguous. It is possible to influence the development of the placenta when it is incomplete, improving the conditions for development - by eliminating, for example, the inflammatory process, normalizing blood pressure, lowering the tone of the uterus, and normalizing blood clotting. You can influence the metabolism in the cells of the placenta - by doing this, for example, by introducing drugs into the body of a pregnant woman that help improve the utilization of glucose by cells.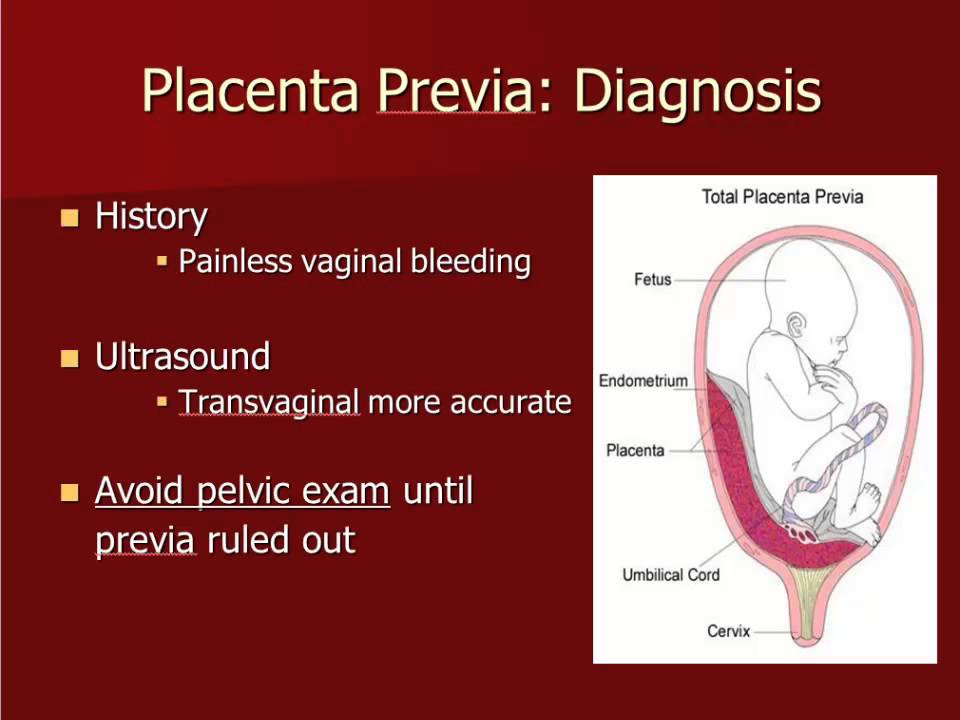 It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus.
It is possible to influence the tone of the vessels, reduce the permeability of the wall and, in this way, the swelling of the tissues decreases and the penetration of oxygen into them improves. But we must understand that we do not cure placental insufficiency, we are only trying to influence the compensatory mechanisms that exist in the placenta, if this succeeds, the manifestations of placental insufficiency disappear. But more often, treatment is aimed at prolonging the pregnancy to the term of a viable fetus.
But if the signs of placental insufficiency increase, and the gestation period is more than 32 weeks, when even in a normal placenta it undergoes involution, the placenta initially developed incorrectly, and now it performs its functions worse, the fetus suffers, then it is useless to treat placental insufficiency, it is better to carry out early delivery and to nurse the newborn without the risk of intrauterine death, which is possible if the placenta depletes its reserves. Sometimes it is necessary to make a decision on early delivery and at an earlier date, when the treatment of placental insufficiency is impossible and the delay threatens the life of the fetus.
Sometimes it is necessary to make a decision on early delivery and at an earlier date, when the treatment of placental insufficiency is impossible and the delay threatens the life of the fetus.
Save the future - articles from the specialists of the clinic "Mother and Child"
SAVE THE FUTURE
PREGNANCY COMPLICATIONS ARE NOT SO RARE. IF A WOMAN DOES NOT UNDERSTAND WHAT IS HAPPENING TO HER, THEN STARTS TO PANIC AND THEREFORE ONLY aggravates the SERIOUS SITUATION. WHEN THE FUTURE MOTHER HAS A CLEAR VIEW OF THE CURRENT SITUATION, AND SHE REALIZES WHAT AND WHY DOCTORS DO, AND STRICTLY FOLLOWS THEIR RECOMMENDATIONS, IT IS EASIER FOR DOCTORS TO ACHIEVE SUCCESS AND SAVE THE PREGNANCY.
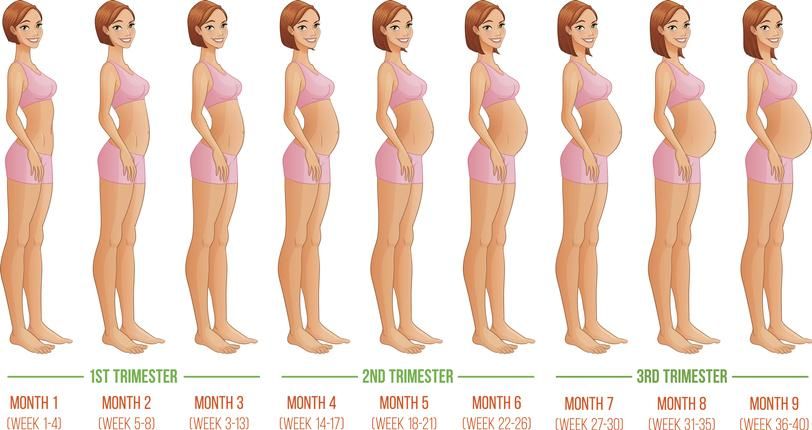
Pregnancy is a significant and very important period in the life of every woman. It can be divided into three trimesters, in each of which an “abnormal” situation may arise, that is, a complication of pregnancy. In such circumstances, the main thing is not to panic, but to immediately seek medical help. In order not to miss the moment and notice the first signs of trouble in time, the expectant mother should know what complications can occur in each of the trimesters and their symptoms.
In such circumstances, the main thing is not to panic, but to immediately seek medical help. In order not to miss the moment and notice the first signs of trouble in time, the expectant mother should know what complications can occur in each of the trimesters and their symptoms.
I TRIMESTER
ERROR EXISTED
For the first time, a woman is suspected of being pregnant when her period is delayed. To make sure that this is really the case, a blood test for human chorionic gonadotropin, a hormone whose level rises sharply during pregnancy, helps. And here it is necessary, without delay, to visit an obstetrician-gynecologist and do an ultrasound. It should confirm that the fetal egg is in the uterine cavity. Sometimes (recently, according to the literature, the percentage is growing), a fetal egg can also attach outside the uterine cavity.
In this case, one speaks of an ectopic pregnancy. Its most common form is tubal, when the fetal egg begins to develop in the fallopian tube. It happens that it is attached in the ovary, abdominal cavity or in the cervix. This condition is life-threatening and requires urgent surgical intervention. The risk is that no organ other than the uterus itself is fit for carrying a baby. A pipe, for example, has a very small volume and, under the “onslaught” of a growing embryo, it will burst sooner or later. The resulting bleeding poses a serious threat to a woman's life.
It happens that it is attached in the ovary, abdominal cavity or in the cervix. This condition is life-threatening and requires urgent surgical intervention. The risk is that no organ other than the uterus itself is fit for carrying a baby. A pipe, for example, has a very small volume and, under the “onslaught” of a growing embryo, it will burst sooner or later. The resulting bleeding poses a serious threat to a woman's life.
Against the background of a delay in menstruation, paroxysmal pains, often accompanied by weakness, dizziness, nausea, and bloody discharge from the genital tract, should cause anxiety. It is urgent to go to the doctor, since it is possible to accurately determine an ectopic pregnancy only with the help of ultrasound. When an ectopic pregnancy is detected, laparoscopic surgery is most often performed. After restorative treatment, a normal pregnancy often occurs.
EXPECTED COMPLICATION - TOXICOSIS
Everyone has heard about it, everyone is waiting with horror when it comes.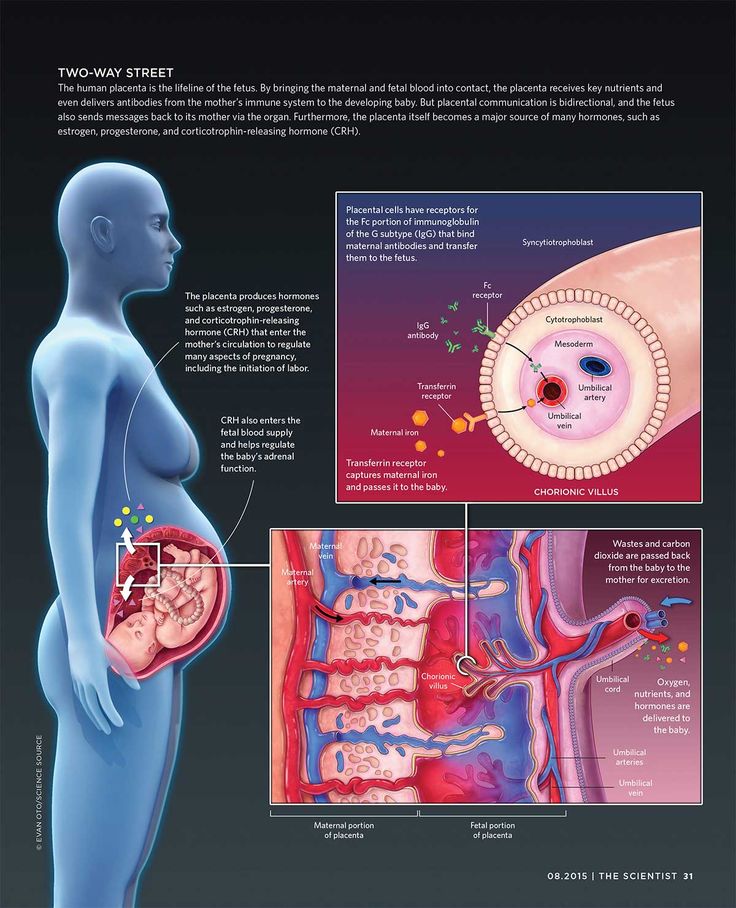 What is this? That's right - toxicosis. The most anticipated and most common complication of early pregnancy. Mild nausea, intolerance to certain odors, sometimes dizziness - these are the symptoms of early toxicosis, which, not without reason, are also considered indirect signs of pregnancy.
What is this? That's right - toxicosis. The most anticipated and most common complication of early pregnancy. Mild nausea, intolerance to certain odors, sometimes dizziness - these are the symptoms of early toxicosis, which, not without reason, are also considered indirect signs of pregnancy.
If vomiting is repeated no more than 3-5 times a day and the expectant mother generally feels fine, there is no need to change her usual lifestyle. But when nausea and vomiting occur 10 or even 20 times a day and any food and even a sip of water do not go for the future, a woman needs hospitalization. Lack of food and dehydration - that's what will worry doctors the most. After all, the expectant mother is losing weight, heart palpitations begin, blood pressure drops, but she needs strength to carry the baby. In the hospital, the fluid deficiency will be replenished with the help of droppers, vomiting will be eliminated with the help of special medications approved for pregnant women, and a full examination of the expectant mother will be carried out. Thanks to this, the unborn child and his expectant mother will feel much better and return to their normal lifestyle again.
I-II TRIMESTER
THREAT OF TERMINATION OF PREGNANCY
At the beginning of pregnancy, this condition is associated with a hormonal imbalance. For some reason, the hormones that support pregnancy begin to be produced in smaller quantities. Genetic malformations of the embryo can also provoke such a complication. This will seem strange to many, but in Western Europe, doctors do not seek to keep the pregnancy at any cost in the early stages. It is believed that in this way nature conducts natural selection.
No matter how you feel about this problem and whatever the causes of the complication, the expectant mother should be alerted by pulling pains in the lower abdomen and lower back, bloody discharge from the genital tract. Any of these symptoms may indicate a threatened miscarriage. Moreover, if there is a discharge, the doctors diagnose "a miscarriage that has begun", but this does not mean that the situation cannot be reversed and the situation normalized. So, when you see such a record in medical documents, do not be alarmed. Doctors will make every effort to still save the pregnancy.
And in order for the efforts of doctors to be successful, you should visit a doctor as soon as possible and have an ultrasound. With it, you can find out how the pregnancy develops, but if a woman is concerned about the discharge, then find out their cause: for example, malformations of the uterus or too low location of the placenta, as well as premature opening of the cervix caused by its shortening (isthmic-cervical insufficiency - ICI ). Another mandatory study is the level of hormones in the urine and blood.
In any case, bleeding, too much pain in the lower abdomen, increased uterine tension are a good reason for hospitalization. If hormonal deficiency is detected, hormonal therapy is prescribed to maintain the pregnancy. With a low location of the placenta, a woman will be advised to lead a calm lifestyle and take drugs that relieve tension in the uterus.
When signs of CCI are detected, the cervix is sutured. All these measures help to prolong the pregnancy to full term - 37 weeks. If the baby is still born earlier, modern equipment and advances in medicine make it possible to nurse babies even with low body weight (from 500 g).
III TRIMESTER
PLACENTA PRESENTATION
The placenta is formed during pregnancy and is excreted from the body after childbirth. Normally, it should be located in the upper and middle third of the uterus so that the child can be safely born at the time appointed by nature. If the placenta occupies a place near the exit from the uterus, is attached at least partially to the cervix, they speak of placenta previa. The reasons for this situation may be malformations of the internal genital organs, chronic inflammation of the uterus and others.
A characteristic symptom is bloody discharge from the genital tract, most often after 7 months of pregnancy. To determine this complication, it is enough to do an ultrasound. The woman is recommended hospitalization and bed rest, as well as drug therapy. If placenta previa persists at the time of delivery, the baby can only be born by caesarean section. The expectant mother is hospitalized at the 37-38th week of pregnancy (at this time the pregnancy is considered full-term) in order to prepare for the operation. But if a woman has heavy bleeding, a caesarean section will have to be done on an emergency basis.
PLACENTAL DETECTION
This complication occurs when the placenta separates from the uterine wall before the baby is born. Most often this occurs at the end of the third trimester or during childbirth. Women with high blood pressure are most at risk, which is why doctors strongly recommend expectant mothers to carefully monitor their blood pressure levels and strictly follow the doctor's recommendations when it rises.
Expectant mother should be alerted by prolonged pain in the abdomen, increased activity of the uterus, bleeding from the genital tract. This situation is risky both for the woman herself and for her unborn child. The woman is threatened with blood loss, and the baby is in danger of hypoxia: extensive placental abruption in the truest sense of the word cuts off oxygen to him. The actions of doctors depend on how strong the labor activity is and how great the woman's blood loss is. If the bleeding is weak, the contractions continue, the baby's heartbeat is normal, the baby feels good, the doctors allow the birth to go naturally, but closely monitor the well-being of the mother and baby. With heavy bleeding and the appearance of signs of hypoxia in crumbs, an emergency caesarean section is performed.
PREMATURE ROUTING OF WATER
This complication is said to occur when the amniotic fluid breaks before contractions begin. There can be many reasons for this development of events, but the main one is infection. That is why doctors carefully monitor expectant mothers and during pregnancy several times do bacteriological culture of flora from the cervical canal. According to modern international recommendations, it is also desirable to take a smear for group B streptococci before childbirth at about 36-37 weeks. If an infection is detected during childbirth, a woman is given antibiotic therapy.
If the amniotic fluid is shed, regardless of the gestational age, call an ambulance or go to the maternity hospital. Making sure that this is really amniotic fluid is quite simple. If the flow of urine can be stopped by tensing the muscles, then the amniotic fluid will continue to flow even if the muscles are tensed. In addition, you can use the amniotest (test for amniotic fluid). If amniotic fluid is expelled, the test strip will change color. There are also special pads that are much easier to use. The principle of their action is the same: if amniotic fluid gets on them, the pads change color.
You should also see a doctor if the amniotic fluid starts to leak only a little. Only a doctor can clarify the situation. Don't refuse hospitalization. If the leakage intensifies, medical attention is indispensable. In most cases, after the outflow of amniotic fluid, a woman and her unborn child begin to prepare for childbirth. If this happened before the 34th week of pregnancy, the baby is given medication to help his lungs open up. But when the waters have not completely poured out, it is possible to prolong the pregnancy. And the efforts of doctors will be directed precisely at this.
PRE-ECLAMPSIA
Another insidious complication in late pregnancy is preeclampsia, or, as it used to be called, preeclampsia. Another name for this complication is late toxicosis of pregnant women. Its main symptom is the presence of protein in the urine. It is for this reason that during pregnancy it is necessary to take this analysis so often. In addition, preeclampsia is manifested by an increase in blood pressure up to 130/90 mm Hg. and above, internal and external edema, due to which the expectant mother gains excess weight.