Peeing the bed during pregnancy
Pregnancy & Bladder Control: Causes, Diagnosis & Treatment
What is incontinence?
Urinary incontinence is the inability to control the passage of urine. If you experience incontinence, you might feel an urgent need to urinate or leak urine between trips to the bathroom. You also might find that you have to make frequent trips to a toilet if you have incontinence. This can happen for many reasons, including pregnancy, childbirth and age.
How does the bladder work?
Your bladder is a round, muscular organ that’s located above the pelvic bone. It’s held in place by the pelvic muscles. A tube called the urethra allows urine to flow out of the bladder. The bladder muscle relaxes as your bladder fill with urine, while the sphincter muscles help to keep the bladder closed until you’re ready to urinate.
Other systems of your body also help to control the bladder. Nerves from the bladder send signals to the brain when the bladder is full and then nerves from the brain signal the bladder when it’s ready to be emptied. All of these nerves and muscles must work together so that your bladder can function normally.
How do pregnancy and childbirth affect bladder control?
During pregnancy, you might leak urine between trips to the bathroom. This is called incontinence. One type of incontinence that can affect pregnant women is stress incontinence. If you’re experiencing stress incontinence, you might leak urine when you:
- Cough.
- Laugh.
- Do physical activity.
Your bladder rests under the uterus. As your growing baby expands, the bladder gets compressed (flattened), making less space for urine. This extra pressure can make you feel the urge to urinate more often than normal. Usually, this is temporary and goes away within a few weeks of your baby’s birth.
However, the risk of experiencing incontinence after pregnancy often depends on your particular pregnancy, the type of delivery and the number of children you have. Women who have given birth — by vaginal delivery or C-section — are at a much higher risk of stress incontinence than women who have never had a baby.
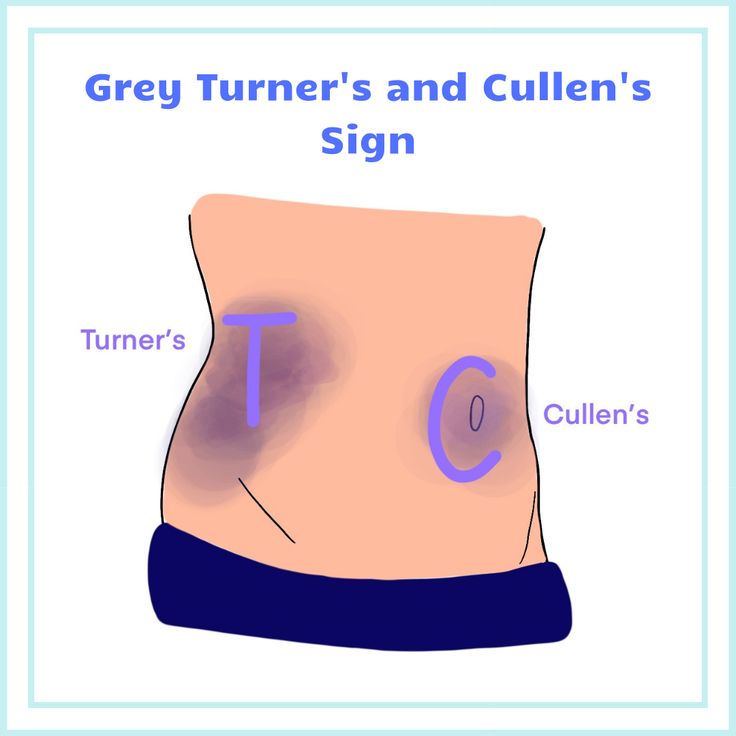
Loss of bladder control can be caused by pelvic organ prolapse (slipping down) that can sometimes happen after childbirth. Your pelvic muscles can stretch and become weaker during pregnancy or a vaginal delivery. If the pelvic muscles do not provide enough support, your bladder might sag or droop. This condition is called cystocele. When the bladder sags, it can cause the urethra’s opening to stretch.
What causes bladder control loss in women after pregnancy and childbirth?
There are several things that can cause you to experience a loss of bladder control after having a baby, including:
- Pelvic organ prolapse: If the muscles around your bladder become weak, the organ can actually slip out of position. This condition is called cystocele.
- Pelvic nerve damage: The pelvic nerves that control your bladder function can get injured during a long or difficult vaginal delivery.
- Injury during delivery: Sometimes, delivery with forceps can result in injuries to the pelvic floor muscles and anal sphincter muscles.

- Injury because of prolonged pushing: Prolonged pushing during a vaginal delivery can also increase the likelihood of injury to the pelvic nerves.
Is it common to leak urine during pregnancy?
For many women, urine leakage (incontinence) is a common during pregnancy or after giving birth. As your body changes throughout pregnancy to accommodate a growing baby, the bladder can be placed under pressure. This is normal for many women during pregnancy.
How are bladder control problems during or after pregnancy diagnosed?
Although most problems with bladder control during or after a pregnancy disappear over time, you should talk to your healthcare provider if the problem continues for six weeks or more after birth. It’s a good idea to keep a diary that records your trips to the bathroom. In this diary, you’ll want to make sure to keep track of how often your have urine leakage and when it occurs.
During an appointment, your healthcare provider will perform a physical examination to rule out various medical conditions and see how well your bladder is functioning. Your provider may also order various tests, including:
Your provider may also order various tests, including:
- Urinalysis: During this test, you will be asked to provide a urine sample. This sample will be analyzed for possible infections that could cause incontinence.
- Ultrasound: Images produced by ultrasound waves can make sure that your bladder is emptying completely.
- Bladder stress test: During this test, your provider will check for signs of urine leakage when you cough forcefully or bear down.
- Cystoscopy: This test involves a thin tube with a miniature camera at one end being inserted into your urethra. Your provider will be able to look inside your bladder and urethra during this test.
- Urodynamics: A thin tube is inserted into your bladder during this test. Water flows through this tube to fill the bladder, so that the pressure inside the bladder can be measured.
How are bladder control problems treated?
There are several techniques for treating bladder control problems. Kegel exercises may help to improve bladder control and reduce urine leakage. In addition, changing your diet, losing weight, and timing your trips to the bathroom may help.
Kegel exercises may help to improve bladder control and reduce urine leakage. In addition, changing your diet, losing weight, and timing your trips to the bathroom may help.
Some suggestions to help with bladder control problems include:
- Switching to decaffeinated beverages or water to help prevent urine leakage. Drinking beverages such as carbonated drinks, coffee and tea might make you feel like you need to urinate more often.
- Limiting the amount of fluids you drink after dinner to reduce the number of trips to the bathroom you need to make during the night.
- Eating foods that are high in fiber to avoid being constipated, since constipation can also cause urine leakage.
- Maintaining a healthy body weight. Extra body weight can put additional pressure on the bladder. Losing weight after your baby is born can help to relieve some of the pressure on your bladder.
- Keeping a record of when you experience urine leakage. It’s a good idea to keep track of what times during the day you have urine leakage.
 If you can see a pattern, you might be able to avoid leakage by planning trips to the bathroom ahead of time.
If you can see a pattern, you might be able to avoid leakage by planning trips to the bathroom ahead of time.
After you’ve established a regular pattern, you might be able to stretch out the time between trips to the bathroom. By making yourself hold on longer, you’ll strengthen your pelvic muscles and increase control over your bladder.
How can loss of bladder control due to pregnancy or childbirth be prevented?
Labor and vaginal delivery have an impact on the pelvic floor muscles and nerves that affect bladder control, so you should discuss your options with your healthcare provider.
Cesarean sections (C-sections) are associated with a lower risk of incontinence or pelvic prolapse than vaginal deliveries, but they may present other risks. Large babies who weigh more than 9 pounds at birth may increase the risk of nerve damage during delivery.
Exercising pelvic floor muscles with Kegel exercises can help prevent bladder control problems.
Bladder control problems might show up months to years after childbirth. Talk to your healthcare team if this happens to you.
Talk to your healthcare team if this happens to you.
How do I do Kegel exercises?
Kegel exercises, also called pelvic floor exercises, help strengthen the muscles that support the bladder, uterus and bowels. By strengthening these muscles during pregnancy, you can develop the ability to relax and control the muscles in preparation for labor and birth.
Kegel exercises are highly recommended during the postpartum period (after you give birth) to promote the healing of perineal tissues, increase the strength of the pelvic floor muscles and help these muscles return to a healthy state (including better urinary control).
To do Kegel exercises, imagine you are trying to stop the flow of urine or trying not to pass gas. When you do this, you are contracting (tightening) the muscles of the pelvic floor, and are practicing Kegel exercises. While doing these exercises, try not to move your leg, buttock or abdominal muscles. In fact, no one should be able to tell that you are doing Kegel exercises.
Kegel exercises should be done every day. Doing five sets of Kegel exercises a day is recommended. Each time you contract the muscles of the pelvic floor, hold for a slow count of 10 seconds and then relax. Repeat this 15 times for one set of Kegels.
How to Avoid Peeing The Bed When Pregnant – ONDR wear
Why does this keep happening?
You went to the bathroom right before bed, but like so many recent nights, you're waking up on soaking wet sheets.
Is there something wrong with you?
If you’re pregnant and struggling with wetting the bed, you’re not alone — We can help.
We’ll cover what you need to know about peeing the bed when pregnant.
Table of Contents- Is It Normal to Pee the Bed When Pregnant?
- 2 Reasons You May Be Peeing the Bed During Pregnancy
- 7 Tips to Help With Bed Wetting During Pregnancy
- ONDRwear Can Keep You Feeling Fresh and Dry During Pregnancy and Beyond
According to Urologist Jessica Lubahn, peeing the bed when pregnant is common and totally normal.
In fact, one survey revealed that 94% of pregnant women experienced an increase in peeing at night.
But good news! While bed-wetting may be common during pregnancy, the condition won’t necessarily persist after delivery.
2 Reasons You May Be Peeing the Bed During Pregnancy#1: Hormonal ChangesPregnancy hormones cause your ligaments and joints to loosen, giving your belly the ability to expand. Due to this, the changing levels of hormones throughout your pregnancy can weaken your pelvic floor.
While this is great preparation for your baby’s delivery, it also loosens the ligaments in your pelvis that help you hold your pee, making you more susceptible to bed-wetting.
#2: Pressure on Your BladderAny time you gain weight, you’re more susceptible to bladder leakage. And the bigger your baby grows, the less space there is for your bladder.
Especially in the third trimester, when the little guy has his elbow under your rib and is headbutting your bladder.
Your growing baby takes up lots of room and puts pressure on your bladder.
You’ll find this to be especially noticeable towards the end of the third trimester. As your baby is preparing to meet the world, his or her head drops straight into your pelvis, pressing squarely on your already over-taxed bladder. Oof.
7 Tips to Help With Peeing the Bed When Pregnant #1: Stay Well Hydrated Throughout The Day
What does drinking plenty of water throughout the day have to do with peeing the bed when you’re pregnant?
Turns out, a lot.
If you're not drinking enough throughout the day, chances are pretty high that you're going to be quite thirsty by the time evening rolls around.
Try to focus on drinking as much water as you can from the moment you wake in the morning until late in the afternoon. Then, start decreasing your fluid intake from early evening to dinner time, stopping completely two hours before bedtime.
How much water should you drink in a day?
There really are no specific guidelines regarding daily water intake, but the Centers for Disease Control and Prevention (CDC) recommend letting your thirst be your guide.
A good rule of thumb is to drink eight 8 oz. glasses of water each day, give or take.
#2: Stop Drinking 2 Hours Before BedtimeIf you like to down a couple of La Croix with your dinner, you might want to think again.
What goes in has got to come out. Unless you have a really long stretch between dinner and bedtime, you could be setting yourself up for disaster.
If you stop drinking around two hours before bedtime, you should notice an improvement in bed-wetting.
#3: Avoid Foods and Drinks That Irritate Your BladderDid you know that there are certain foods and drinks that can throw your bladder into a tizzy, and increase the chances of peeing in the bed while pregnant?
Here are just a few of the main culprits that you’ll want to try and stay away from:
- Tomatoes or tomato-based items
- Spicy foods
- Citrus fruits, including lemons, limes, and those fun little “cuties”
- Chocolate
- Carbonated drinks
- Alcohol, including wine and champagne
- Orange juice
- Apple juice
- Coffee, yup, even decaf
- Tea, including green, black, and decaf; and
- Caffeinated drinks
It can also be helpful to keep a journal of what you're eating and drinking throughout your pregnancy. If you happen to pee the bed, check back to see if anything that you ate or drank might have upset your bladder.
If you happen to pee the bed, check back to see if anything that you ate or drank might have upset your bladder.
Gaining too much weight can cause extra pressure on your bladder, which in turn can cause peeing in the bed while pregnant.
While pregnancy certainly isn't the time to be overly concerned about your weight, here are some recommended guidelines for weight gain throughout the course of your pregnancy:
- If you were underweight before becoming pregnant, you should gain 28 to 40 lb.
- If you were at a normal weight before becoming pregnant, you should gain 25 to 35 lb.
- If you were overweight before becoming pregnant, you should gain 15 to 25 lb.
- If you were obese before becoming pregnant, you should gain 11 to 20 lb.
These weight gain recommendations are for pregnant women carrying one baby.
#5: Avoid ConstipationNever underestimate the importance of being regular.
Not only is being unable to poop terribly uncomfortable, but it also can be a huge factor when it comes to peeing the bed when pregnant.
But what’s a soon-to-be mama to do?
You can start by eating foods that encourage your body to run smoothly. Here are a few ideas to get you started:
- Whole grains, such as
- Oats
- Brown rice
- Whole wheat
- Quinoa
- Barley; and
- Rye
- Fruits, like:
- Berries
- Peaches
- Apples
- Plums
- Apricots
- Raisins
- Melons
- Kiwi
- Plums; and
- Prunes
- Vegetables, like:
- Broccoli
- Kale
- Lettuce
- Cauliflower
- Squash; and
- Sweet potatoes
- Nuts and seeds, such as
- Walnuts
- Almonds
- Pecans
- Chia
- Ground flaxseeds; and
- Psyllium
- Legumes, including
- Lentils
- Kidney beans
- Navy beans; and
- Chickpeas
And you'll also want to be sure to stop eating foods that can make constipation worse, like:
- Fast food
- Cheese
- Sweetened cereal
- Ice cream
- Chips
- Processed meats, like hot dogs and lunch meat
- Fried foods; and
- Refined flours
Sticking with (or beginning) a regular exercise schedule during your pregnancy will also help keep your bowels moving regularly. Even a quick 10-minute walk each day can get things moving — and keep them going.
Even a quick 10-minute walk each day can get things moving — and keep them going.
#6: Sleep on Your Side
Are you a back sleeper? If so, take note that sleeping on your back during pregnancy can be problematic.
The American Pregnancy Association recommends SOS (sleep on side) during pregnancy.
Not only will this give you the best possible circulation, but it will also put the least amount of pressure on your pregnant bladder.
#7: Strengthen Your Pelvic FloorYour pelvic floor is made up of your …
- Bladder
- Small intestines
- Rectum; and
- Uterus
Some of the most common forms of urinary incontinence, including peeing the bed when pregnant, are because the muscles in the pelvic floor are weak.
Here are a few pelvic floor exercises you can do to help tone up your pelvic muscles and keep your bladder in tip-top shape.
You’ll want to be sure to empty your bladder before doing these exercises.
To do Kegels, follow these instructions:
- Relax the muscles in your stomach, abdomen, chest, thighs, and butt.
- Tighten the muscles in your pelvic floor and hold there for 5 to 10 seconds.
- Relax your muscles for 5 to 10 seconds.
Do 10 repetitions, 3 times each day.
#2: Standing KegelsTo do Standing Kegels follow these instructions:
- Stand up straight and focus on your pelvic muscles.
- Squeeze your pelvic muscles up and then in.
- Hold the squeeze for up to ten seconds, and then relax.
Do 10 repetitions, 3 times each day.
#3: Horizontal Kegel’sTo do Horizontal Kegals follow these instructions:
- Lie flat on the floor, bed, or sofa. If it is more comfortable, you can bend your knees, so your legs are at an angle. Put your hands on your stomach.
- Squeeze your pelvic muscles. Your stomach muscles should tighten under your hands.

- Hold the squeeze for up to ten seconds before releasing.
Do 10 repetitions, 3 times each day.
#4: Sitting Fast-TwitchFast-twitch muscles are muscles throughout your body that react quickly and are critical if you want to avoid peeing in the bed when pregnant.
To do the Sitting Fast Twitch exercise, follow these instructions:
- Sit in a chair and find your pelvic floor muscles.
- Quickly quench the muscles like you’re trying to squeeze something tightly.
- Quickly release.
Do 10 repetitions, 3 times each day.
#5: Sitting Slow-Twitch ExerciseSlow-twitch muscles are the ones that support your lower organs, including your bladder.
To do the Sitting Slow Twitch exercise, follow these instructions:
- Sit in a chair, focusing on your pelvic floor muscles.
- Tighten up your pelvic floor muscles (like you’re trying to keep from passing gas).

- Hold for up to ten seconds before relaxing.
Do 10 repetitions, 3 times each day.
ONDRwear Can Keep You Feeling Fresh and Dry During Pregnancy and BeyondAre you looking for a little extra protection at night to help keep your sheets nice and clean?
Look no further than ONDRwear.
Our incontinence underwear is perfect for pregnancy!
Created by a mom, who also happens to be a practicing Urologist, ONDRwear panties are:
- Machine washable
- Leakproof
- Naturally odor-free
- Lightweight; and
- Moisture-wicking
And just in case you're envisioning a pair of sagging granny panties, think again.
ONDRwear comes in:
- Thong
- Bikini
- Boy-shorts; and
- High-waisted briefs
And you know what’s really cool? Once your bundle of joy arrives, you can use your ONDRwear undies as period panties.
ONDRwear keeps you dry throughout your pregnancy and beyond.
What have you got to lose? Other than wet sheets, of course.
Frequent urination during pregnancy - Juno
Article content
When is considered frequent
Urges are frequent if they occur more than 9 times a day. Usually only a small amount of urine is passed at a time. Pregnant women may have about 20 visits to the toilet per day, while the daily amount of urine can also increase to 2 liters.
Is it an early sign of pregnancy?
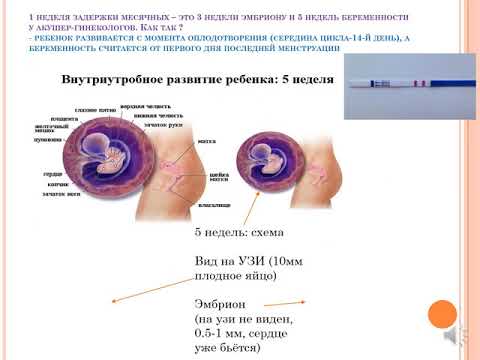
HCG slightly increases the volume of urine excreted, so frequent urination begins already in the first weeks of pregnancy. The symptom does not 100% indicate the onset of fertilization - it should be considered in conjunction with other manifestations - primarily with a positive test. nine0008
However, keep in mind that with an increase in the daily volume of urine at a very early date, a false negative result is possible. Also, the symptom is less pronounced in ectopic pregnancy due to lower hCG levels, so an examination is required in any case.
If you began to frequent the toilet and there is a delay, then pregnancy is very likely.
Physiological causes of frequent urination in pregnant women
In healthy women, this phenomenon is associated with the body getting used to carrying a baby, as well as with other physiological reasons. nine0008
In the first half of pregnancy
The main causes of frequent urination during early pregnancy:
- Increased progesterone production. This hormone relaxes muscle tissue, helping to maintain pregnancy. As a result, urine is retained worse, the urge to void becomes more frequent due to the reduced tone of the bladder.
- Increased blood supply in the pelvis. Due to the proximity of the bladder to the uterus, its increased sensitivity occurs - filling receptors react more strongly. nine0027
- Active work of the kidneys. During the bearing of a child, the renal blood flow increases 1.5 times for the constant renewal of amniotic fluid and the timely removal of metabolic products.
 Accordingly, more urine begins to be produced.
Accordingly, more urine begins to be produced.
Physiological increase in urination does not cause pain and discomfort, itching and burning. In the presence of negative symptoms, you need to consult a doctor to rule out pathologies.
Second half of pregnancy
The main reason for frequent urge to urinate in the second and third trimester is the increased pressure of the uterus on the bladder. However, diseases can also be the cause:
- Infections. Changes in the pelvis in pregnant women and a decrease in protective forces increase the risk of developing urethritis, cystitis, pyelonephritis. Such pathologies are accompanied not only by frequent urination, but also by pain, discomfort in the area of inflammation, and a burning sensation. The woman's health is deteriorating; nine0027
- Gestational diabetes. An increase in blood glucose in violation of carbohydrate metabolism. The amount of urine separated increases significantly.
Other pathologies include neoplasms in the small pelvis, endocrine and neurological disorders.
Soreness with frequent urination in pregnant women - is it normal or not?
Painful urination is not normal. Unpleasant sensations indicate the development of a pathological process. Pain and discomfort are a sign of urinary tract irritation. Cystitis is very likely if a woman has severely reduced immunity or has chronic diseases of the pelvic organs. Sometimes it can be accompanied by a temperature and requires a mandatory visit to the doctor. nine0008
Calls at night
Pregnant women often complain about how tired they are at night "hiking". The situation is explained by the fact that the work of the kidneys depends on the position of the body. In the later stages, the female body is prone to fluid retention and edema, especially when in an upright position. When the expectant mother lies down, the renal blood flow and the outflow of fluid from the tissues increase. As a result, the kidneys excrete more urine.
What is the duration of frequent urination during pregnancy? nine0003
The phenomenon begins already from the first days of pregnancy and is especially pronounced up to about 12 weeks. Later, the number of emptyings gradually decreases, because by 4-5 months the body adapts to new conditions. The diaphragm rises, creating more space for the growing uterus and "unloading" the pelvic organs.
Later, the number of emptyings gradually decreases, because by 4-5 months the body adapts to new conditions. The diaphragm rises, creating more space for the growing uterus and "unloading" the pelvic organs.
Frequent urination during pregnancy in the second trimester may indicate the addition of an infection or the development of inflammation, but it is also possible as a manifestation of the individual characteristics of the organism. You can find out more precisely this moment from your doctor, who is involved in pregnancy management. nine0008
In the third trimester, the opposite phenomenon is possible - fluid retention. However, the closer the birth, the more often the urge to urinate becomes. In the last month of gestation, the uterus descends and puts pressure on the organs of the urinary system.
How likely is miscarriage in the absence of frequent urination?
A woman does not always immediately find out about a missed pregnancy. Fetal movements are not felt in the early stages, so pregnant women "listen" to other signs. In the first weeks, the abrupt cessation of toxicosis and frequent urge to urinate are alarming. These symptoms can indeed indicate the death or developmental delay of the fetus, as well as an ectopic pregnancy, but not always. Toward the end of the first trimester, the kidneys excrete less urine, in some this has been observed since 9‒10 weeks.
In the first weeks, the abrupt cessation of toxicosis and frequent urge to urinate are alarming. These symptoms can indeed indicate the death or developmental delay of the fetus, as well as an ectopic pregnancy, but not always. Toward the end of the first trimester, the kidneys excrete less urine, in some this has been observed since 9‒10 weeks.
How to deal with frequent urination during pregnancy: tips
In the absence of pathologies, the discomfort caused by physiological frequent urination can be reduced as follows:
- Stay hydrated. Drink enough, but don't overdo it. Give preference to water over sugary drinks like coffee.
- Eat rationally. Eliminate diuretic foods (citrus fruits, spicy foods), as well as things that cause constipation. nine0027
- Exercise. Strengthen your pelvic muscles by training your vaginal and anus sphincters.
- Get more rest. Sleep during the day is very useful, especially in the later stages - after being in a horizontal position, the bladder empties faster, as a result, the load on the kidneys during night rest is reduced.

- Maintain immunity. Avoid hypothermia, take vitamin complexes as prescribed by the doctor.
- Empty your bladder as much as possible. Do not hold back the urge and try to make sure that all the urine comes out completely. In this regard, it is easier to urinate in the shower. nine0027
Control your condition. If other symptoms (pain, fever, burning sensation) appear in addition to frequent urination, tell your doctor immediately.
First part. "A large number of cases of enuresis resolve spontaneously"
Up to 15% of children over 5 years of age suffer from enuresis. What is this problem, how to treat it and what not to miss in the behavior and health of children? Galina Evgenievna Tishchenko, neurourologist at GMS Clinic, answers these and other questions of children's health. nine0008
It must be understood that by pronouncing the term "enuresis", we mean periodic urinary incontinence during night sleep in children over 5 years old. Everything that concerns the age of up to 5 years, urination during a night's sleep fits into the concept of the norm, and everything that concerns problems with urination, in addition to bedwetting, is no longer monosymptomatic enuresis. That is, there is a complex dysfunction of the lower urinary tract. If we are talking about monosymptomatic enuresis, when children have only incontinence at night, then it occurs in 15% of children at 5 years old, and then this percentage decreases with the age of the child. At 6 years -13%, at 7 years - 10%. And by the age of 15, there will be 1% of children who have this diagnosis. For a medical diagnosis, age 5 is the starting point. nine0008
Everything that concerns the age of up to 5 years, urination during a night's sleep fits into the concept of the norm, and everything that concerns problems with urination, in addition to bedwetting, is no longer monosymptomatic enuresis. That is, there is a complex dysfunction of the lower urinary tract. If we are talking about monosymptomatic enuresis, when children have only incontinence at night, then it occurs in 15% of children at 5 years old, and then this percentage decreases with the age of the child. At 6 years -13%, at 7 years - 10%. And by the age of 15, there will be 1% of children who have this diagnosis. For a medical diagnosis, age 5 is the starting point. nine0008
Why am I paying attention to this? Sometimes parents complain about enuresis, and the child has complex dysfunction of the pelvic organs, and the task of the specialist to whom the parents turned is to determine: does the child really have monosymptomatic enuresis or is there other dysfunction of the lower urinary tract, accompanied by urinary incontinence? In addition, there is also the concept of primary and secondary enuresis.
Primary enuresis is a situation when a child has not previously had a long period (more than 6 months) of dry nights. If there were dry nights for more than 6 months and then enuresis appeared again, then we are talking about secondary enuresis. nine0008
Who should pay attention to this?
Along with enuresis, there may be subtle disorders that should be identified by a pediatrician, neurologist, urologist, or a specialist who was initially contacted for help. It is important to ask parents if there are other components of pelvic dysfunction. Does the child have frequent urination (more than 8 times a day)? Or vice versa, too rare urge to urinate (less than 3 times a day)? Do you have urinary incontinence during the day? This is important when a child, by the age of 6-7, can already control urination during wakefulness. nine0008
Further. Is there a state of urgency? That is, when the urge to urinate occurs abruptly, without a preliminary slight urge, which the child can postpone. And immediately there is a strong unbearable urge that forces the child to urinate without delay. The doctor should ask how the child goes to the toilet during the day? Doesn't he have to strain, grunt, strain his stomach in order to start urinating? Does he have an intermittent stream of urine when the bladder is emptied in several portions. Is there a condition associated with discomfort, cutting, burning, pain, during or immediately after urination. Does the child have constipation or vice versa fecal incontinence? nine0008
And immediately there is a strong unbearable urge that forces the child to urinate without delay. The doctor should ask how the child goes to the toilet during the day? Doesn't he have to strain, grunt, strain his stomach in order to start urinating? Does he have an intermittent stream of urine when the bladder is emptied in several portions. Is there a condition associated with discomfort, cutting, burning, pain, during or immediately after urination. Does the child have constipation or vice versa fecal incontinence? nine0008
If signs of any additional dysfunction of the pelvic organs are revealed, this condition is no longer just enuresis, but dysfunction of the lower urinary tract, which is accompanied by a component of urinary incontinence at night.
What do doctors have to deal with more often?
In 80% of cases, we meet with primary enuresis, and in 20% with complex enuresis, when there are other symptoms. Among complex cases, in about 15% of children, the problem will be combined with impaired bowel function, that is, urinary incontinence will be associated with constipation. And we say that in general we are dealing with a violation of the functions of the pelvic organs. The doctor must understand this. nine0008
And we say that in general we are dealing with a violation of the functions of the pelvic organs. The doctor must understand this. nine0008
It is very important not to miss a congenital anomaly when we are dealing with an incorrect laying of the nervous system and spine, and not just with what lies on the surface.
Which of the children is more likely to have enuresis, and is there a genetic reason for this?
According to statistics, enuresis occurs 2 times more often in boys than in girls. As for the characteristics of children or genetics, there are no obvious causes and relationships. Some scientists have investigated sleep disturbances, suggesting that children with enuresis sleep more soundly than healthy ones. Some children were found to have deeper sleep, they tried to track the connection with the alternation of fast and slow phases of sleep. Some researchers have found that incontinence occurs during REM sleep, and then they got other results. The gene in the chromosomes responsible for the transmission of primary enuresis was examined in families, if there is a mutation of this gene, then the trait will be transmitted to children. In any case, even if there is no genetic predisposition, in 15% of cases, children after 5 years of age will have monosymptomatic enuresis. nine0008
The gene in the chromosomes responsible for the transmission of primary enuresis was examined in families, if there is a mutation of this gene, then the trait will be transmitted to children. In any case, even if there is no genetic predisposition, in 15% of cases, children after 5 years of age will have monosymptomatic enuresis. nine0008
There have been many studies on urodynamics during night sleep, they are amazing. Scientists installed sensors in the bladder cavity and on the muscles of the perineum, and also filmed brain activity. The wall of the bladder began to tense up, and if another sensor simultaneously recorded a response increase in the activity of the muscles of the perineum, the child remained dry, and if the tone of the perineum did not increase, then there was no signal from the nervous system to hold and urine leaked. Science still cannot find a connection with the posture in a dream. The main thing is that the urge does not awaken one child, but awakens another, all other things being equal. Why this happens, we do not know. Additional evidence is required. nine0008
Why this happens, we do not know. Additional evidence is required. nine0008
It turns out that urination in the body is very complicated?
Urination is one of the most complex organized acts. The muscles of the bladder, the urethra, and the muscles of the perineum must work very, very well together. During the accumulation of urine, the muscles of the bladder remain relaxed, and the sphincter and muscles of the perineum are in good shape, they are clamped, and we are dry all day without thinking about it in the norm. Then the reverse process takes place, but only under our volitional control. Thus, there is a regulation. When the brain decides to urinate, the accumulation phase changes to the urine output phase. This is a complex process in the body. The muscles of the perineum relax, and only after that a signal is given to contract the bladder wall. Urine is excreted. This is the so-called mature type of urination. When a child is unable to retain urine by force of will, it means that his nervous system is not yet mature. And up to 5 years, there is no point in expecting complete control over urination, including at night. The regulatory mechanisms of the body are not yet mature. When a child is already learning to control bowel function, and he does not have incidents with fecal excretion, then, often, in the interval from a month to a year, complete control over the function of urination will develop. And this means that a mature type of urination has been formed. The child will have longer intervals between urges, the capacity of the bladder will increase, the functions of the perineal muscles that hold urine will be coordinated. The pressure inside the bladder will remain low despite the newly arriving urine from the kidneys, and the child will control his urination completely. When the urge to urinate can awaken a child at night, it means that the child already has a mature type of urination. It is believed that enuresis is caused by the late maturation of all regulatory mechanisms of the nervous system.
And up to 5 years, there is no point in expecting complete control over urination, including at night. The regulatory mechanisms of the body are not yet mature. When a child is already learning to control bowel function, and he does not have incidents with fecal excretion, then, often, in the interval from a month to a year, complete control over the function of urination will develop. And this means that a mature type of urination has been formed. The child will have longer intervals between urges, the capacity of the bladder will increase, the functions of the perineal muscles that hold urine will be coordinated. The pressure inside the bladder will remain low despite the newly arriving urine from the kidneys, and the child will control his urination completely. When the urge to urinate can awaken a child at night, it means that the child already has a mature type of urination. It is believed that enuresis is caused by the late maturation of all regulatory mechanisms of the nervous system.