Partial molar pregnancy pictures
Symptoms, Causes, Treatment, Pictures, and More
Pregnancy happens after an egg is fertilized and burrows into the womb. Sometimes, though, these delicate beginning stages can get mixed up. When this happens, a pregnancy may not go the way it should — and this can be heartbreaking, even though it’s no one’s fault.
A molar pregnancy occurs when the placenta doesn’t develop normally. Instead, a tumor forms in the uterus and causes the placenta to become a mass of fluid-filled sacs, also called cysts. About 1 in every 1,000 pregnancies (0.1 percent) is a molar pregnancy.
This kind of pregnancy doesn’t last because the placenta typically can’t nourish or grow a baby at all. In rare cases, it may also lead to health risks for mom.
A molar pregnancy is also called a mole, a hydatidiform mole, or gestational trophoblastic disease. You can have this pregnancy complication even if you have had a typical pregnancy before. And, the good news — you can have a completely normal, successful pregnancy after having a molar pregnancy.
There are two kinds of molar pregnancy. Both have the same result, so one isn’t better or worse than the other. Both kinds are usually benign — they don’t cause cancer.
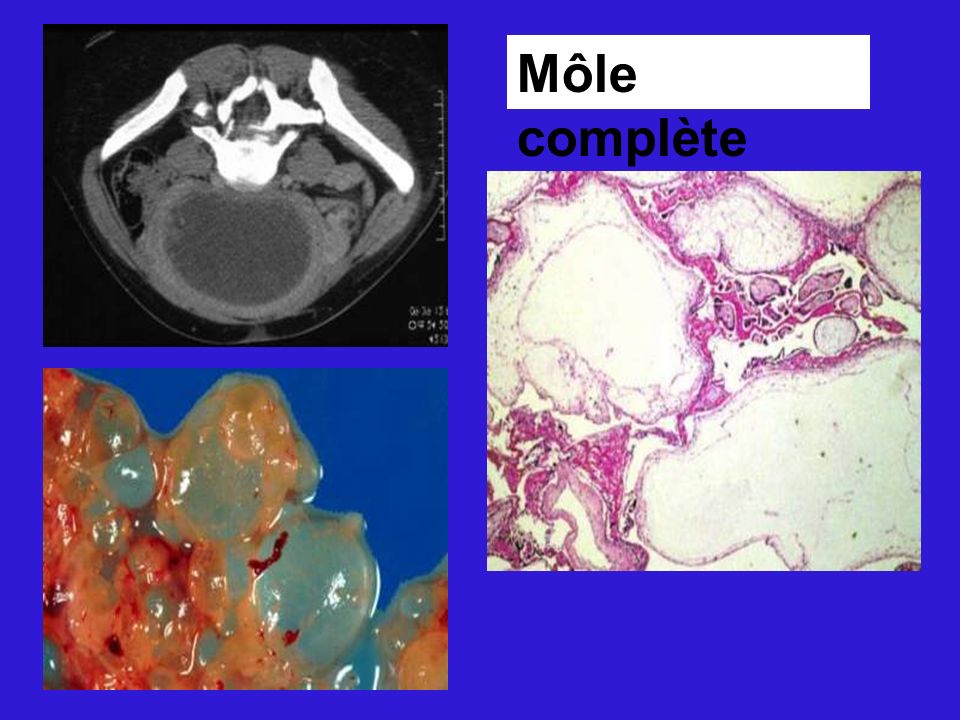
A complete mole happens when there’s only placenta tissue growing in the womb. There’s no sign of a fetus at all.
In a partial mole, there is placenta tissue and some fetal tissue. But the fetal tissue is incomplete and could never develop into a baby.
You can’t control whether or not you have a molar pregnancy. It’s not caused by anything you did. A molar pregnancy can happen to women of all ethnicities, ages, and backgrounds.
It sometimes happens because of a mix-up at the genetic — DNA — level. Most women carry hundreds of thousands of eggs. Some of these might not form correctly. They’re usually absorbed by the body and put out of commission.
But once in a while an imperfect (empty) egg happens to get fertilized by a sperm. It ends up with genes from the father, but none from the mother. This can lead to a molar pregnancy.
This can lead to a molar pregnancy.
In the same way, an imperfect sperm — or more than one sperm — may fertilize a good egg. This can also cause a mole.
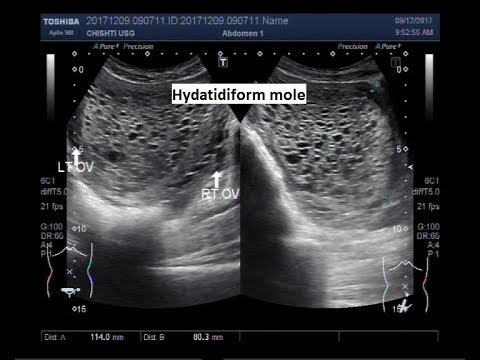
Share on PinterestA molar pregnancy is also known as a hydatidiform mole. Surgical removal is the mainstay of treatment for this condition. Image source: Wikimedia
Risk factors
There are some risk factors for a molar pregnancy. These include:
- Age. Although it can happen to anyone, you may be more like to have a molar pregnancy if you’re younger than 20 or older than 35 years.
- History. If you’ve had a molar pregnancy in the past, you’re more likely to have another one. (But again — you can also go on to have a successful pregnancy.)
A molar pregnancy may feel just like a typical pregnancy at first. However, you’ll likely have certain signs and symptoms that something is different.
- Bleeding. You may have bright red to dark brown bleeding in the first trimester (up to 13 weeks).
 This is more likely if you have a complete molar pregnancy. The bleeding might have grape-like cysts (tissue clots).
This is more likely if you have a complete molar pregnancy. The bleeding might have grape-like cysts (tissue clots). - High hCG with severe nausea and vomiting. The hormone hCG is made by the placenta. It’s responsible for giving many pregnant women a certain amount of nausea and vomiting. In a molar pregnancy, there may be more placenta tissue than normal. The higher levels of hCG might lead to severe nausea and vomiting.
- Pelvic pain and pressure. Tissues in a molar pregnancy grow faster than they should, especially in the second trimester. Your stomach may look too large for that early stage in pregnancy. The fast growth can also cause pressure and pain.
Your doctor may also find other signs like:
- high blood pressure
- anemia (low iron)
- pre-eclampsia
- ovarian cysts
- hyperthyroidism
Sometimes a molar pregnancy is diagnosed when you go for your usual pregnancy ultrasound scan. Other times, your doctor will prescribe blood tests and scans if you have symptoms that might be caused by a molar pregnancy.
Other times, your doctor will prescribe blood tests and scans if you have symptoms that might be caused by a molar pregnancy.
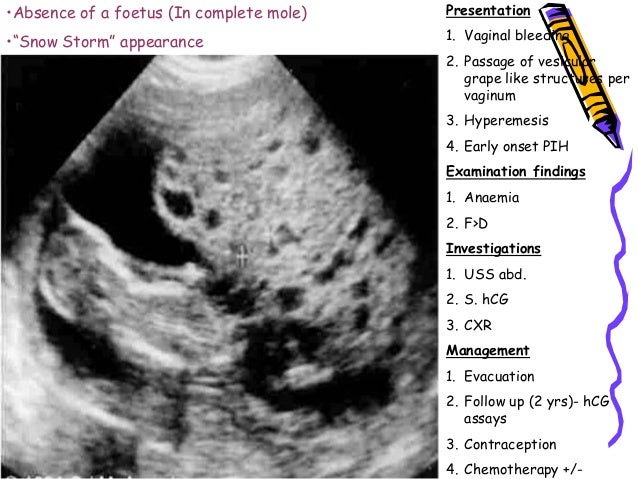
A pelvis ultrasound of a molar pregnancy will typically show a grape-like cluster of blood vessels and tissue. Your doctor may also recommend other imaging — like MRI and CT scans — to confirm the diagnosis.
Share on PinterestA molar pregnancy, although not dangerous by itself, has the potential to become a cancer. Image source: Wikimedia
High levels of hCG in the blood might also be a sign of a molar pregnancy. But some molar pregnancies may not raise hCG levels — and high hCG is also caused by other standard kinds of pregnancies, like carrying twins. In other words, your doctor won’t diagnose a molar pregnancy based on hCG levels alone.
A molar pregnancy can’t grow into a normal, healthy pregnancy. You must have treatment to prevent complications. This can be really, really hard news to swallow after the initial joys of that positive pregnancy result.
With the right treatment, you can go on to have a successful pregnancy and healthy baby.
Your treatment may involve one or more of the following:
Dilation and curettage (D&C)
With a D&C, your doctor will remove the molar pregnancy by dilating the opening to your womb (cervix) and using a medical vacuum to remove the harmful tissue.
You’ll be asleep or get local numbing before you have this procedure. Although a D&C is sometimes done as an outpatient procedure at a doctor’s office for other conditions, for a molar pregnancy it’s typically done at a hospital as an inpatient surgery.
Chemotherapy drugs
If your molar pregnancy falls into a higher risk category — due to cancer potential or because you have had difficulty getting proper care for whatever reason — you may receive some chemotherapy treatment after your D&C. This is more likely if your hCG levels don’t go down over time.
Hysterectomy
A hysterectomy is surgery that removes the entire womb. If you don’t wish to get pregnant again, you might choose this option.
If you don’t wish to get pregnant again, you might choose this option.
You’ll be fully asleep for this procedure. A hysterectomy is not a common treatment for a molar pregnancy.
RhoGAM
If you have Rh-negative blood, you’ll receive a drug called RhoGAM as part of your treatment. This prevents some complications related to developing antibodies. Be sure and let your doctor know if you have A-, O-, B-, or AB- blood type.
After-care
After your molar pregnancy is removed, you’ll need more blood tests and monitoring. It’s very important to make sure that no molar tissue was left behind in your womb.
In rare cases, molar tissue can regrow and cause some types of cancers. Your doctor will check your hCG levels and give you scans for up to a year after treatment.
Later-stage treatment
Again, cancers from a molar pregnancy are rare. Most are also very treatable and have a survival rate of up to 90 percent. You may need chemotherapy and radiation treatment for some cancers.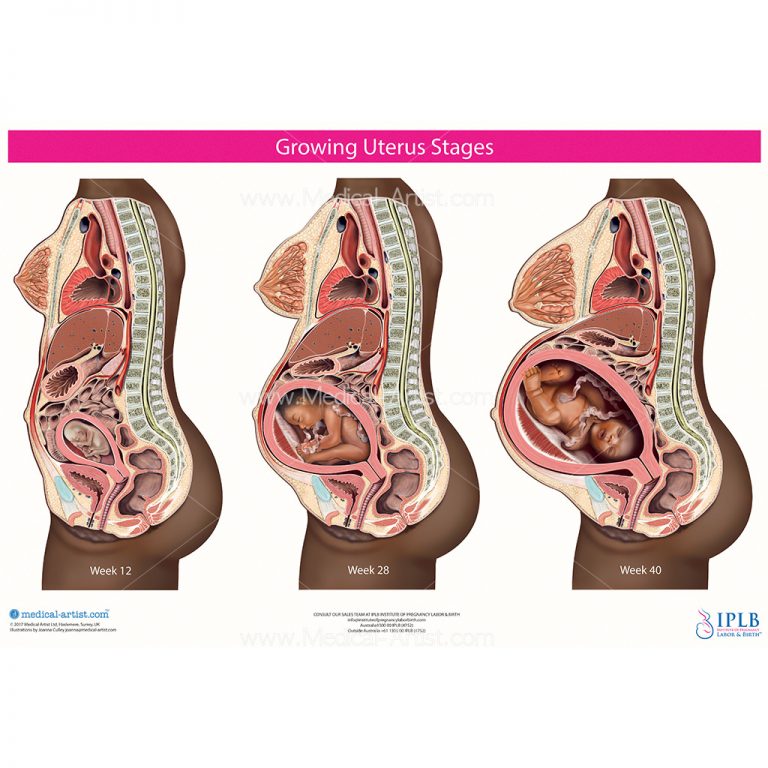
If you think you’re pregnant, see your doctor right away. As with many things, the best way to prevent complications from a molar pregnancy is to get diagnosed and treated as early as possible.
After treatment, see your doctor for all follow-up appointments.
It’s best to wait to get pregnant again for up to a year after treatment. This is because pregnancy can mask any rare, but possible complications after a molar pregnancy. But talk to your doctor — your situation is unique, just like you are.
Once you’re completely in the clear, it’ll likely be safe for you to get pregnant again and have a baby.
Also know that cancers and complications from molar pregnancies are very rare. In fact, the University of Pennsylvania Medical School advises that prior molar pregnancies or other risk factors for developing the related cancerous tumors shouldn’t factor into family planning.
Molar pregnancies aren’t common, but they can happen to women of all ages and backgrounds.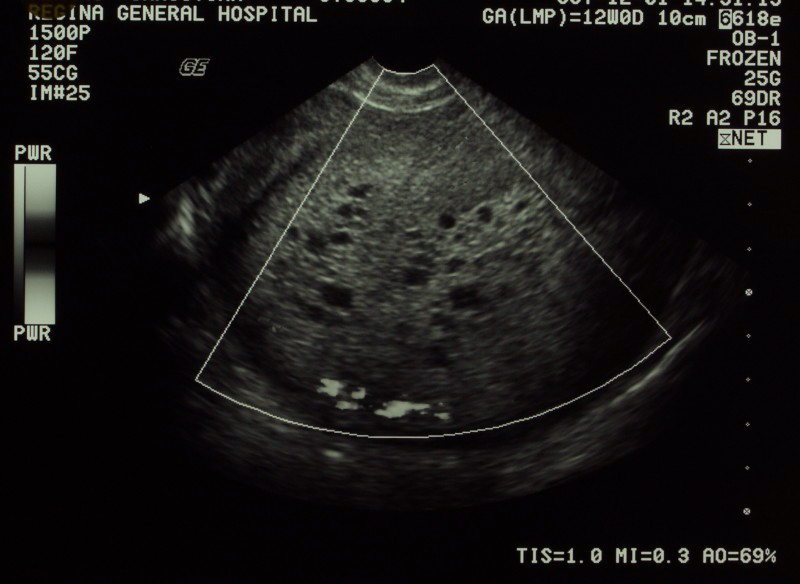 A molar pregnancy can be a long and emotionally draining experience.
A molar pregnancy can be a long and emotionally draining experience.
The treatment and waiting period can also take a toll on your emotional, mental, and physical health. It’s important to take the time to grieve for any kind of pregnancy loss in a healthy way.
Ask your doctor about support groups. Reach out to other women who have gone through a molar pregnancy. Therapy and counseling can help you look forward to a healthy pregnancy and baby in the not-so-distant future.
Symptoms, Causes, Treatment, Pictures, and More
Pregnancy happens after an egg is fertilized and burrows into the womb. Sometimes, though, these delicate beginning stages can get mixed up. When this happens, a pregnancy may not go the way it should — and this can be heartbreaking, even though it’s no one’s fault.
A molar pregnancy occurs when the placenta doesn’t develop normally. Instead, a tumor forms in the uterus and causes the placenta to become a mass of fluid-filled sacs, also called cysts.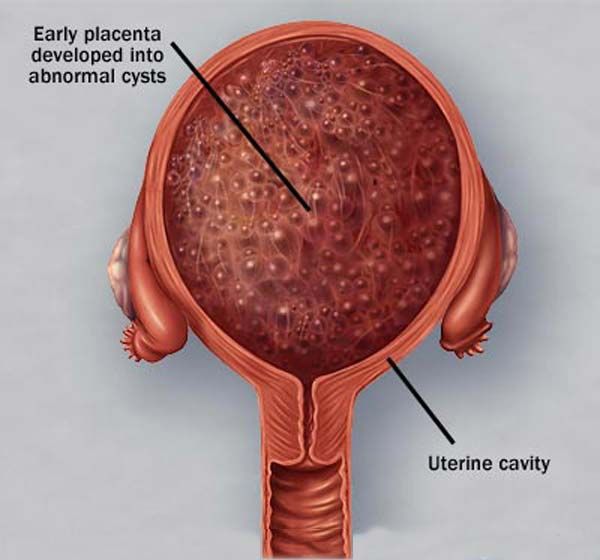 About 1 in every 1,000 pregnancies (0.1 percent) is a molar pregnancy.
About 1 in every 1,000 pregnancies (0.1 percent) is a molar pregnancy.
This kind of pregnancy doesn’t last because the placenta typically can’t nourish or grow a baby at all. In rare cases, it may also lead to health risks for mom.
A molar pregnancy is also called a mole, a hydatidiform mole, or gestational trophoblastic disease. You can have this pregnancy complication even if you have had a typical pregnancy before. And, the good news — you can have a completely normal, successful pregnancy after having a molar pregnancy.
There are two kinds of molar pregnancy. Both have the same result, so one isn’t better or worse than the other. Both kinds are usually benign — they don’t cause cancer.
A complete mole happens when there’s only placenta tissue growing in the womb. There’s no sign of a fetus at all.
In a partial mole, there is placenta tissue and some fetal tissue. But the fetal tissue is incomplete and could never develop into a baby.
You can’t control whether or not you have a molar pregnancy. It’s not caused by anything you did. A molar pregnancy can happen to women of all ethnicities, ages, and backgrounds.
It’s not caused by anything you did. A molar pregnancy can happen to women of all ethnicities, ages, and backgrounds.
It sometimes happens because of a mix-up at the genetic — DNA — level. Most women carry hundreds of thousands of eggs. Some of these might not form correctly. They’re usually absorbed by the body and put out of commission.
But once in a while an imperfect (empty) egg happens to get fertilized by a sperm. It ends up with genes from the father, but none from the mother. This can lead to a molar pregnancy.
In the same way, an imperfect sperm — or more than one sperm — may fertilize a good egg. This can also cause a mole.
Share on PinterestA molar pregnancy is also known as a hydatidiform mole. Surgical removal is the mainstay of treatment for this condition. Image source: Wikimedia
Risk factors
There are some risk factors for a molar pregnancy. These include:
- Age. Although it can happen to anyone, you may be more like to have a molar pregnancy if you’re younger than 20 or older than 35 years.

- History. If you’ve had a molar pregnancy in the past, you’re more likely to have another one. (But again — you can also go on to have a successful pregnancy.)
A molar pregnancy may feel just like a typical pregnancy at first. However, you’ll likely have certain signs and symptoms that something is different.
- Bleeding. You may have bright red to dark brown bleeding in the first trimester (up to 13 weeks). This is more likely if you have a complete molar pregnancy. The bleeding might have grape-like cysts (tissue clots).
- High hCG with severe nausea and vomiting. The hormone hCG is made by the placenta. It’s responsible for giving many pregnant women a certain amount of nausea and vomiting. In a molar pregnancy, there may be more placenta tissue than normal. The higher levels of hCG might lead to severe nausea and vomiting.
- Pelvic pain and pressure. Tissues in a molar pregnancy grow faster than they should, especially in the second trimester.
 Your stomach may look too large for that early stage in pregnancy. The fast growth can also cause pressure and pain.
Your stomach may look too large for that early stage in pregnancy. The fast growth can also cause pressure and pain.
Your doctor may also find other signs like:
- high blood pressure
- anemia (low iron)
- pre-eclampsia
- ovarian cysts
- hyperthyroidism
Sometimes a molar pregnancy is diagnosed when you go for your usual pregnancy ultrasound scan. Other times, your doctor will prescribe blood tests and scans if you have symptoms that might be caused by a molar pregnancy.
A pelvis ultrasound of a molar pregnancy will typically show a grape-like cluster of blood vessels and tissue. Your doctor may also recommend other imaging — like MRI and CT scans — to confirm the diagnosis.
Share on PinterestA molar pregnancy, although not dangerous by itself, has the potential to become a cancer. Image source: Wikimedia
High levels of hCG in the blood might also be a sign of a molar pregnancy. But some molar pregnancies may not raise hCG levels — and high hCG is also caused by other standard kinds of pregnancies, like carrying twins. In other words, your doctor won’t diagnose a molar pregnancy based on hCG levels alone.
In other words, your doctor won’t diagnose a molar pregnancy based on hCG levels alone.
A molar pregnancy can’t grow into a normal, healthy pregnancy. You must have treatment to prevent complications. This can be really, really hard news to swallow after the initial joys of that positive pregnancy result.
With the right treatment, you can go on to have a successful pregnancy and healthy baby.
Your treatment may involve one or more of the following:
Dilation and curettage (D&C)
With a D&C, your doctor will remove the molar pregnancy by dilating the opening to your womb (cervix) and using a medical vacuum to remove the harmful tissue.
You’ll be asleep or get local numbing before you have this procedure. Although a D&C is sometimes done as an outpatient procedure at a doctor’s office for other conditions, for a molar pregnancy it’s typically done at a hospital as an inpatient surgery.
Chemotherapy drugs
If your molar pregnancy falls into a higher risk category — due to cancer potential or because you have had difficulty getting proper care for whatever reason — you may receive some chemotherapy treatment after your D&C. This is more likely if your hCG levels don’t go down over time.
This is more likely if your hCG levels don’t go down over time.
Hysterectomy
A hysterectomy is surgery that removes the entire womb. If you don’t wish to get pregnant again, you might choose this option.
You’ll be fully asleep for this procedure. A hysterectomy is not a common treatment for a molar pregnancy.
RhoGAM
If you have Rh-negative blood, you’ll receive a drug called RhoGAM as part of your treatment. This prevents some complications related to developing antibodies. Be sure and let your doctor know if you have A-, O-, B-, or AB- blood type.
After-care
After your molar pregnancy is removed, you’ll need more blood tests and monitoring. It’s very important to make sure that no molar tissue was left behind in your womb.
In rare cases, molar tissue can regrow and cause some types of cancers. Your doctor will check your hCG levels and give you scans for up to a year after treatment.
Later-stage treatment
Again, cancers from a molar pregnancy are rare. Most are also very treatable and have a survival rate of up to 90 percent. You may need chemotherapy and radiation treatment for some cancers.
Most are also very treatable and have a survival rate of up to 90 percent. You may need chemotherapy and radiation treatment for some cancers.
If you think you’re pregnant, see your doctor right away. As with many things, the best way to prevent complications from a molar pregnancy is to get diagnosed and treated as early as possible.
After treatment, see your doctor for all follow-up appointments.
It’s best to wait to get pregnant again for up to a year after treatment. This is because pregnancy can mask any rare, but possible complications after a molar pregnancy. But talk to your doctor — your situation is unique, just like you are.
Once you’re completely in the clear, it’ll likely be safe for you to get pregnant again and have a baby.
Also know that cancers and complications from molar pregnancies are very rare. In fact, the University of Pennsylvania Medical School advises that prior molar pregnancies or other risk factors for developing the related cancerous tumors shouldn’t factor into family planning.
Molar pregnancies aren’t common, but they can happen to women of all ages and backgrounds. A molar pregnancy can be a long and emotionally draining experience.
The treatment and waiting period can also take a toll on your emotional, mental, and physical health. It’s important to take the time to grieve for any kind of pregnancy loss in a healthy way.
Ask your doctor about support groups. Reach out to other women who have gone through a molar pregnancy. Therapy and counseling can help you look forward to a healthy pregnancy and baby in the not-so-distant future.
How to diagnose a molar pregnancy - advice from an obstetrician
Quick navigation
Molar mole (molar pregnancy) is a rare complication of pregnancy and a type of gestational trophoblastic disease, when the fertilization of the egg, the sperm cells are filled with water abnormally or sacomanomal cells occurs inside the uterus. This pathology is rare, and according to statistics, for every 590 pregnancies, there is about 1 case of a molar pregnancy.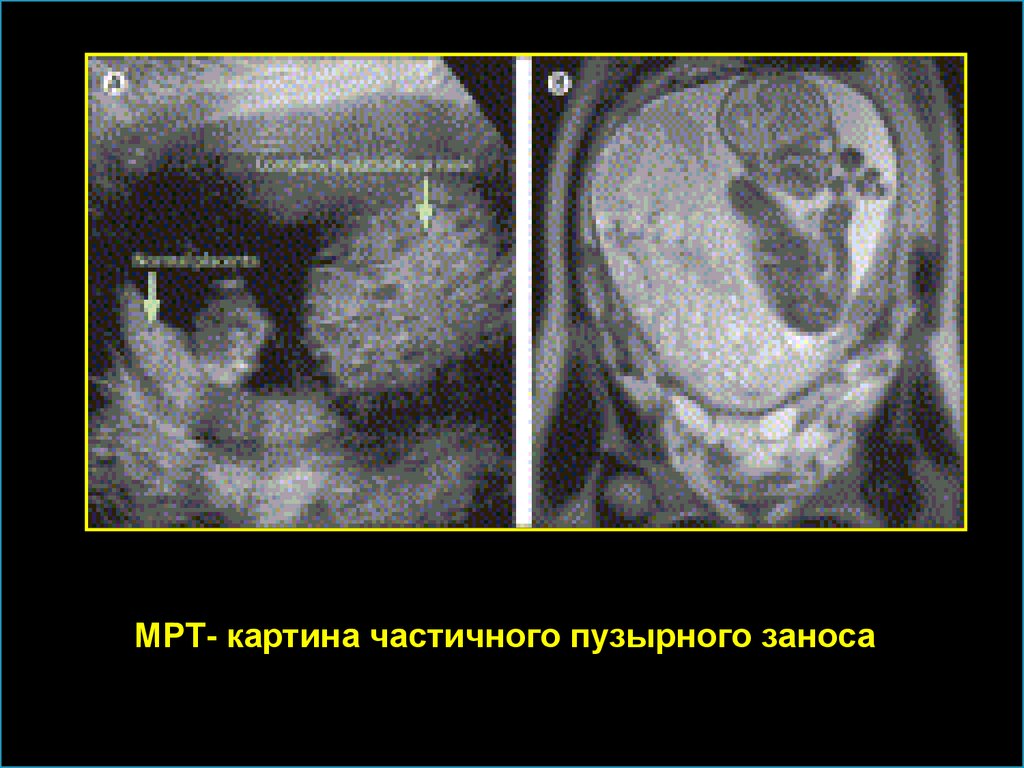 Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist. nine0003
Diagnosis and treatment of molar pregnancy of hydatidiform mole is carried out by an obstetrician-gynecologist. nine0003
Causes
Molar pregnancy is caused by an imbalance in the genetic material (chromosomes) during pregnancy. This usually occurs when an egg that contains no genetic information is fertilized by a sperm (complete molar pregnancy) or when a normal egg is fertilized by two sperm (partial molar pregnancy).
Mole risk factors
All pregnant women have a risk of developing a molar pregnancy, but this risk is very small. nine0003
Age. Researchers have found that certain types of molar pregnancies are more common in certain age groups. Complete molar pregnancies are more common in mothers over 45 years of age. The risk is moderately increased in young adolescents. Age does not affect the risk of partial molar pregnancies.
Previous molar pregnancy. If a woman has already had one molar pregnancy, she has a 1 in 100 chance of having a recurrence. If a woman has had two or more molar pregnancies, the risk of another pregnancy with this condition is higher, about 15 to 20 out of 100.
If a woman has had two or more molar pregnancies, the risk of another pregnancy with this condition is higher, about 15 to 20 out of 100.
Symptoms of molar pregnancy
Vaginal bleeding
Vaginal bleeding is the most common symptom of molar pregnancy. Bleeding can occur during normal pregnancy and is not always serious, but the woman should immediately inform the gynecologist or midwife about it. Women with a mole are more likely to develop blood clots or a watery brown vaginal discharge. In some pregnant women, pieces of molar tissue come out, which can look a bit like small bunches of grapes. Bleeding caused by a mole usually starts between 6 and 12 weeks of gestation. nine0003
The following symptoms are rare. This is because most hydatidiform moles are detected and corrected during routine ultrasound examinations performed in early pregnancy. In some women with a complete hydatidiform mole, the abdomen may expand faster than in a normal pregnancy. In women with partial hydatidiform mole, the uterus and abdomen may be smaller than expected for this stage of pregnancy.
In women with partial hydatidiform mole, the uterus and abdomen may be smaller than expected for this stage of pregnancy.
Nausea is common in normal pregnancies, but may be more severe and more frequent with mole. This is called hyperemesis. nine0003
Anemia means that the patient has few red blood cells in her body. If a woman is losing blood due to vaginal bleeding, her red blood cell count may decrease. Due to anemia, the patient may feel constant fatigue and shortness of breath.
Pre-eclampsia is a complication that can occasionally occur during the last 3 months of a normal pregnancy. The main symptoms are high blood pressure and protein in the urine. In rare cases, with a hydatidiform mole, preeclampsia can be obtained much earlier. nine0003
An overactive thyroid is a rare symptom of molar pregnancy. The medical term for this is hyperthyroidism.
Molar pregnancy stages
staging is a system doctors use to describe the size of a tumor and whether it has spread. Gynecologists usually remove abnormal molar tissue during pregnancy from the uterus. If the levels of a hormone called hCG return to normal shortly after the mole is removed, then the doctor does not need to stage the mole. In most women, the hCG level practically disappears within 4-6 weeks after the removal of the hydatidiform mole. Once the molar tissue has left the uterus, it cannot produce hCG. Thus, in addition to subsequent blood and urine tests to check for molar tissue return, the woman will not need additional tests. nine0003
Gynecologists usually remove abnormal molar tissue during pregnancy from the uterus. If the levels of a hormone called hCG return to normal shortly after the mole is removed, then the doctor does not need to stage the mole. In most women, the hCG level practically disappears within 4-6 weeks after the removal of the hydatidiform mole. Once the molar tissue has left the uterus, it cannot produce hCG. Thus, in addition to subsequent blood and urine tests to check for molar tissue return, the woman will not need additional tests. nine0003
If the hCG level remains high or rises, this may be a sign that abnormal cells are still present in the uterus. The cells may spread to deeper layers of the uterus or other parts of the body. Gynecologists call this persistent trophoblastic disease. In this case, the woman will need additional tests to determine the stage of the tumor.
Survival of hydatidiform mole
Almost all women with hydatidiform mole recover. Doctors remove all of the abnormal molar tissue with surgery, and most women don't need further treatment. In a small number of patients, some abnormal cells remain and may spread to deeper layers of the uterus or other parts of the body. This is called persistent trophoblastic disease. Chemotherapy can usually completely rid a woman of all abnormal cells. nine0003
In a small number of patients, some abnormal cells remain and may spread to deeper layers of the uterus or other parts of the body. This is called persistent trophoblastic disease. Chemotherapy can usually completely rid a woman of all abnormal cells. nine0003
Molar Pregnancy Diagnosis
When a woman is pregnant, the placenta produces the hormone human chorionic gonadotropin (hCG) to help the baby develop. The placenta releases hCG into the bloodstream, and the body gets rid of the rest in the urine. HCG is produced during molar pregnancy, but is at a much higher level than normal. Thus, routine blood tests during pregnancy may reveal a mole.
Women usually have a routine ultrasound at 12 weeks pregnant. Molar pregnancies may show a characteristic "blizzard appearance" on scans. An ultrasound scan is a good way to diagnose complete molar pregnancies, but it is not as good at detecting partial molar pregnancies. A partial molar pregnancy can still be detected by a blood test. nine0003
nine0003
Diagnosis after a miscarriage or abortion
A doctor will usually examine the tissues of the placenta and fetus if a woman has had a miscarriage in the hospital or an abortion. These checks may reveal abnormal mole cells. If positive, the woman will need treatment to remove molar tissue from the uterus.
Treatments for hydatidiform mole
There are various surgical options for removing a molar pregnancy.
Mole surgery
Most women have a minor operation under general anesthesia to remove molar tissue from the uterus. The operation is called dilation and suction evacuation. The surgeon uses a thin tube to gently suck out the molar tissue. Sometimes they may also use a sharp instrument to cut tissue from the uterine lining. This is called expansion and scraping. This treatment removes all of the molar tissue for most women.
Removal of the uterus (hysterectomy)
The surgeon may suggest removal of the uterus (hysterectomy) instead of removing just the molar tissue.
Drug treatment to remove molar tissue
Some women with partial mole are given drug treatment to make the uterus contract and get rid of the abnormal cells.
Author: Belyakov Nikolai Grigorievich
Specialization: Pediatrician
Where does the reception: Clinic General Medical Center (GMC), St. Petersburg
Share:
The best specialists in St. Petersburg with a rating of 4.5+
Veromei Dominika Tadeushevna
Specialization: Therapist, Gynecologist, Obstetrician-gynecologist
Medical experience: since 20104
Where does the appointment: Dr. Pel's ClinicAndreeva Oksana Sergeevna
Specialization: Ultrasound doctor, Gynecologist, Obstetrician-gynecologist
Medical experience: since 1998
Where does the appointment: Dr. Pel's Clinic nine0003
Kaminskaya Evgenia Grigorievna
Specialization: Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 1994
Where he meets: Clinic of Dr. Pel, IEM Medical Center, Medical College
Pel, IEM Medical Center, Medical College
Golotina Maria Vladimirovna
Specialization: Ultrasound doctor, Gynecologist, Endocrinologist, Obstetrician-gynecologist
Medical experience: since 2008
Where does the appointment: Dr. Pel's Clinic
Literature:
- Beskova T.K., Kalinin A.V. Study of the immune status in patients with hydatidiform mole // Journal "A and G" 1981. No. 9.
- Davydova M.A., Kalelyushnik N.L., Osipov R.A. Progressive form of hydatidiform drift//Kazan medical journal 1979 (1).
- Kalinin A.V. Clinical and morphological features of hydatidiform mole and its prognosis // Abstract of the discussion for the degree of candidate of medical sciences. 1982.
- I.Persianinov L.S., Demidov V.N. Ultrasonic diagnostics in obstetrics. — M.: Medicine. - nineteen80. —- 335 S.
- Kosenko IA, Bakinovskaya IE Ultrasound diagnosis of trophoblastic tumors of the uterus.
 Minsk: Medicine, 2005.-75p.
Minsk: Medicine, 2005.-75p.
Latest diagnostic articles
Radiation therapy
Radiation therapy is a treatment that uses radiation to kill cancer cells. This therapy is most often prescribed by oncologists for the treatment of oncological diseases.
Read more
Is MRI harmful to health
When making an MRI appointment, the patient sometimes has questions about the safety of the examination: “Is there any harm from MRI for the body, what is the danger of magnetic resonance imaging, and how often can MRI be done. Let's figure it out.
Read more
Principles of operation of MRI, ultrasound, CT, X-ray and PET
In modern medicine, thanks to advances in technology, there is a wide range of diagnostic equipment that helps doctors in the early detection of diseases and pathological disorders. In this article we will talk about the principles of operation of MRI, ultrasound, CT, nine0003
Read more
MRI during pregnancy
Since every day MRI technology provides doctors of St. Petersburg medical centers with an increasing range of diagnostic capabilities, it is being actively used in pediatrics, prenatal diagnostics in pregnant women and oncology. As soon as a woman finds out that she will become a mother, she immediately has the question of what procedures she can do and which are contraindicated. Almost all pregnant women know that they are strictly forbidden to take x-rays and can undergo ultrasound. nine0003
Petersburg medical centers with an increasing range of diagnostic capabilities, it is being actively used in pediatrics, prenatal diagnostics in pregnant women and oncology. As soon as a woman finds out that she will become a mother, she immediately has the question of what procedures she can do and which are contraindicated. Almost all pregnant women know that they are strictly forbidden to take x-rays and can undergo ultrasound. nine0003
Read more
Full and partial mole
Bubble drift is a pathological condition of the fetal egg, in which the normal development of the embryo does not occur. Chorionic villi are transformed into fluid-containing vesicles, and the chorionic epithelium begins to grow actively.
In order to avoid dangerous complications, it is very important to diagnose the pathology in a timely manner and undergo a course of treatment. You can make an appointment with a doctor by calling the phone number listed on the website, or by using the appointment button.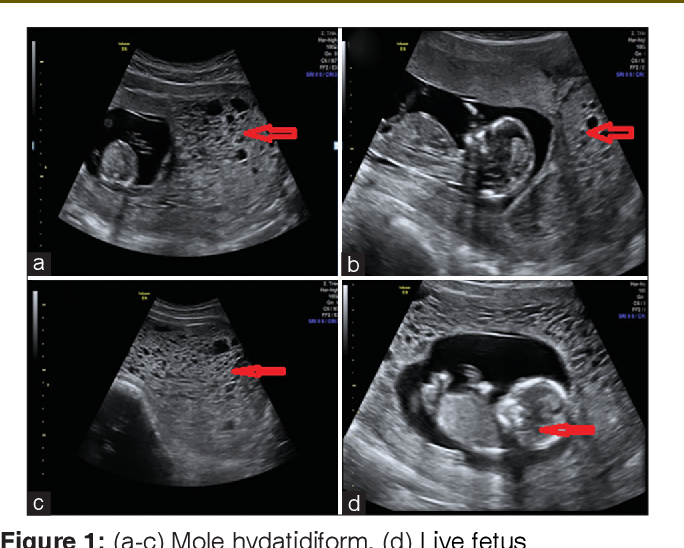 nine0003
nine0003
The size of the bubbles gradually increase, reaching 2.5 cm. Outwardly, such cysts filled with yellowish contents resemble grapes. In most cases, the vessels in them atrophy, although in rare cases capillaries are found in small quantities. Syncytium, the tissue that is the membrane of the vesicles, begins to grow and, with the help of enzymes, gradually melt the decidual membrane (this is the name of the functional layer of the endometrium that has undergone certain changes due to pregnancy). nine0003
Mole classification
There are several classifications of hydatidiform mole. One of them is based on the degree of hyperplasia (growth) and anaplasia (the cells lose their properties and return to undifferentiated forms, which is a harbinger of their malignant degeneration) of the chorionic epithelium. According to this classification, the following types of cystic drifts are distinguished:
- Benign - in this case there is slight hyperplasia, no anaplasia
- Potentially malignant - moderate hyperplasia and anaplasia
- Malignant - hyperplasia and anaplasia are severe
Also allocate full and partial hydatidiform skid.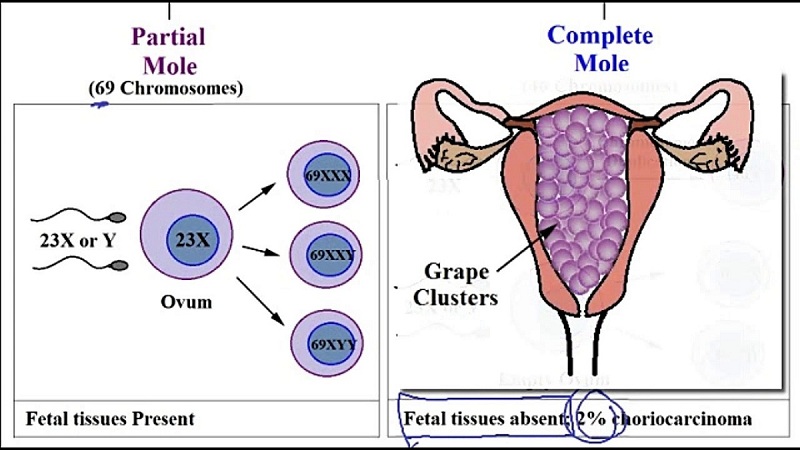
Complete mole
Complete hydatidiform drift is characterized by the fact that all chorionic villi are transformed into vesicles. This pathology develops in the 1st trimester of pregnancy, when the entire chorion is covered with villi. The death of the embryo occurs, which then resolves. nine0003
In the study of complete hydatidiform mole, in most cases, the 46XX karyotype is detected, while both X chromosomes are paternal. This situation is possible if the oocyte contains a damaged nucleus or does not have a nucleus at all. After fertilization, the paternal set of chromosomes is doubled. Much less often (on average, up to 10% of cases), complete hydatidiform mole contains the 46XY chromosome set, all chromosomes are also paternal.
With complete mole, the uterus enlarges to a greater extent than it should be normal in the early juices of pregnancy. nine0003
Partial hydatidiform mole
With this variant of cystic drift, in rare cases, pregnancy is possible.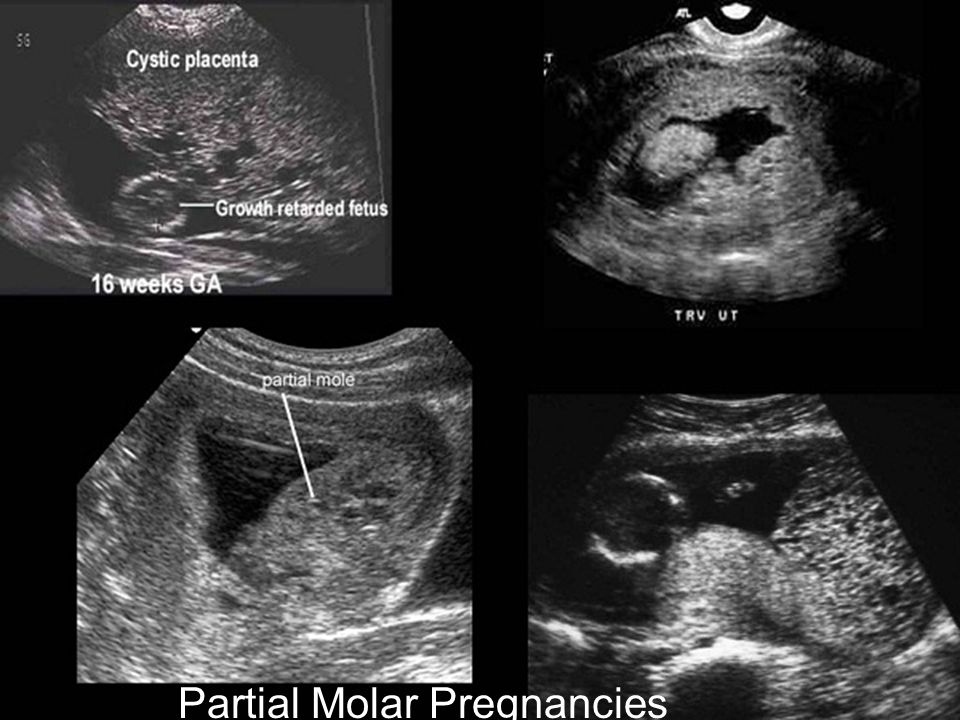 More often the fetus dies, and in the study of cystic drift, its elements are detected. If there is a multiple pregnancy, then the hydatidiform mole can spread to only one placenta.
More often the fetus dies, and in the study of cystic drift, its elements are detected. If there is a multiple pregnancy, then the hydatidiform mole can spread to only one placenta.
With partial hydatidiform mole, a triploid set of chromosomes (69.XXY, 69.XXX, 69.XYY) is most often detected, where there is a diploid set of father's chromosomes and a haploid set of mother's chromosomes. nine0003
The size of the uterus is usually smaller or corresponds to the gestational age.
If you have any questions related to complete and partial hydatidiform mole, you can ask Nova Clinic doctors. You can make an appointment with a doctor by calling the phone number listed on the website, or by using the appointment button.
Causes
To date, scientists have not yet been able to determine the causes of the pathology, but a number of risk factors can be identified. So, the probability of molar pregnancy is higher if: nine0003
- have been diagnosed with a mole in the past;
- pregnant age less than 15 or more than 40 years;
- in history there are cases of spontaneous or artificial termination of pregnancy.
In addition, it should be noted that hydatidiform drift is most often detected in Latin America and Asia.
Symptoms
Since the cystic skid entails dangerous consequences, a woman needs to pay close attention to symptoms such as: nine0003
- bleeding from the genital tract. Uterine bleeding occurs in 9 out of 10 molar pregnancies;
- a significant increase in the size of the abdomen, not corresponding to the gestational age;
- pain in the lower abdomen;
- nausea and episodes of vomiting;
- increased salivation;
- edema;
- weakness.
If you have noted these signs in yourself, immediately make an appointment with your obstetrician-gynecologist so that the doctor can conduct an examination and take the necessary measures in a timely manner. nine0003
Diagnostics
To identify a cystic drift, the doctor prescribes:
- blood test to determine the level of β-hCG (the beta subunit of human chorionic gonadotropin).
 With molar pregnancy, the results markedly exceed the norm for a certain period. In addition, in dynamics there is a significant daily increase in the concentration of the hormone. Since a similar situation is typical for multiple pregnancies, an ultrasound examination is prescribed; nine0134
With molar pregnancy, the results markedly exceed the norm for a certain period. In addition, in dynamics there is a significant daily increase in the concentration of the hormone. Since a similar situation is typical for multiple pregnancies, an ultrasound examination is prescribed; nine0134 - Ultrasound of the pelvic organs. On the monitor screen, the doctor sees significantly overgrown chorionic villi, which visually resemble grapes. With partial hydatidiform drift, separate foci of swollen chorionic villi are visualized.
In some cases, hysteroscopy, laparoscopy, CT or MRI may be additionally prescribed.
Treatment and possible complications
Pregnancy is terminated in any case. nine0003
It is very important to correctly carry out the complete evacuation of the mole. Usually, for this purpose, vacuum aspiration of the contents of the uterine cavity is performed, followed by control curettage.
The final diagnosis, indicating the type of hydatidiform mole, is made only on the basis of a histological examination of the material.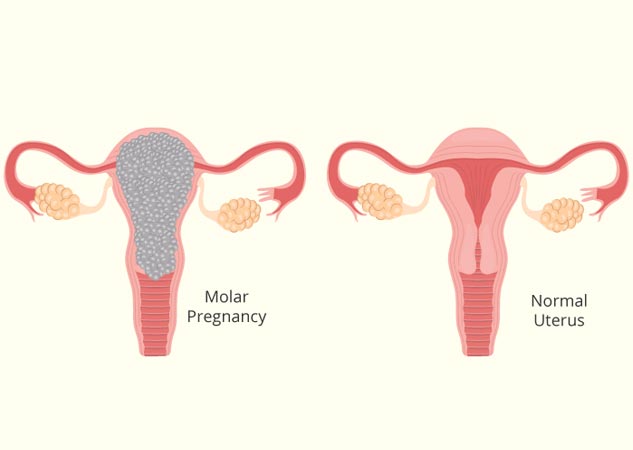
After surgery, a woman will need to take a blood test to determine the level of β-hCG several times before receiving three negative results in a row. If the cystic drift is not completely removed, then the villi remaining in the uterine cavity continue to produce the hormone. In this case, in the dynamics of the study will demonstrate an increased level and a further increase in the concentration of human chorionic gonadotropin. nine0003
In addition, a woman:
- immediately after surgery, and also after 1 and 2 months, makes an x-ray of the lungs;
- for six months continues to take tests for hCG and do ultrasound of the pelvic organs every month.
Complications that can develop as a result of hydatidiform mole include:
- formation of a malignant trophoblast tumor; nine0134
- complete cessation of menses;
- infertility;
- infectious and inflammatory processes in the uterine cavity.