Pain in pelvis and lower back during pregnancy
Pelvic girdle pain in pregnancy
Pelvic girdle pain in pregnancy | Pregnancy Birth and Baby beginning of content6-minute read
Listen
Key facts
- Pelvic girdle pain refers to pain or discomfort in your lower back, pelvis, hips, or thighs during pregnancy.
- This pain can be mild or severe, and you may find you have difficulty sitting, standing and walking.
- • Pelvic pain is common in pregnancy, but you are more likely to have it if you had back or pelvic pain before you were pregnant, had an injury to the area, your work is physically demanding, you are overweight or you smoke.
- Your GP, obstetrician and physiotherapist can help you to manage your pelvic pain in pregnancy.
- Depending on your circumstances, your health team may recommend that you modify your daily activities, wear a pelvic support garment, or they may refer you to physiotherapy and exercise programs.
What is pelvic girdle pain?
Pelvic girdle pain (PGP) refers to pain or discomfort in the lower back or pelvis during pregnancy. The pain may also extend to your upper thighs and perineum. During pregnancy your pelvic ligaments relax, and other joints become more mobile. This can result in pain in the pelvic area. Pelvic girdle pain usually goes away without treatment after birth, though symptoms may return in future pregnancies.
What are the symptoms of pelvic girdle pain in pregnancy?
If you have PGP, you may only have mild discomfort in your pelvis or back. Alternatively, you may have severe pain making it difficult for you to sit, stand, walk and move around. Each person has a different levels of pain or discomfort.
Who gets pelvic pain in pregnancy?
Some people are more likely to have PGP than others. If you had back or pelvic pain before your pregnancy or had PGP in a previous pregnancy, you are more likely to have PGP in your current pregnancy.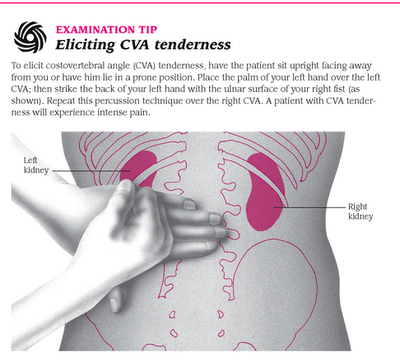 If you have had a back or pelvic injury, you are also more likely to develop PGP. Other risk factors for PGP include the number of times you’ve been pregnant, physically demanding work, being overweight, emotional distress, or smoking.
If you have had a back or pelvic injury, you are also more likely to develop PGP. Other risk factors for PGP include the number of times you’ve been pregnant, physically demanding work, being overweight, emotional distress, or smoking.
Who can help with pelvic pain?
If you are experiencing back, pelvic, or hip pain during pregnancy, you should see your doctor. Your doctor will ask you about your medical history and do a physical examination. It is important to see a doctor so you can be sure that your pain is because of PGP.
Your doctor may suggest that you see a physiotherapist. A physiotherapist can teach you exercises to help you to manage your pain.
If your pain is severe and you are not improving with standard care, you may be referred to a specialist pain service.
How is pelvic girdle pain treated?
There are several strategies that you can use to help you manage and control pelvic girdle pain. First, you can try and identify what daily activities cause you pain and try to adjust or avoid those activities. For example, you can avoid wearing high heeled shoes and standing on one leg. You can also reduce weight-bearing activities like climbing stairs or walking and standing for long periods of time. You can also try to avoid activities that involve straining your hip, like getting in and out of a car or bath, or squatting.
For example, you can avoid wearing high heeled shoes and standing on one leg. You can also reduce weight-bearing activities like climbing stairs or walking and standing for long periods of time. You can also try to avoid activities that involve straining your hip, like getting in and out of a car or bath, or squatting.
Wearing a pelvic support garment can also help to reduce pain. Pelvic support garments can help to stabilise your pelvic girdle and improve symptoms if the garment is fitted correctly and used for short periods of time. Ask your physiotherapist for more information about pelvic support garments.
You can also ask your doctor or pharmacist about medicines that can help you to manage your pain so you can continue with your daily activities. This may include taking medicines like paracetamol.
Physiotherapy and exercise programs can help to reduce pain too. They may also help to correct the problem causing the pain.
How can I relieve pelvic girdle pain at home?
Many of these pain-relieving techniques can be done at home. Ask your physiotherapist to suggest a home exercise program to help you when you first start to feel a pelvic-pain episode. If your pain stops you from doing essential daily activities, you can take a pain-relief medicine like paracetamol. Taking pain relief may mean that you’re better able to do the exercises that your physiotherapist has recommended. If you have a pelvic support garment, you can put that on.
Ask your physiotherapist to suggest a home exercise program to help you when you first start to feel a pelvic-pain episode. If your pain stops you from doing essential daily activities, you can take a pain-relief medicine like paracetamol. Taking pain relief may mean that you’re better able to do the exercises that your physiotherapist has recommended. If you have a pelvic support garment, you can put that on.
Applying heat to painful areas and sitting or lying down may help you control your pain. Extended bedrest without the guidance of a doctor is not recommended, so speak to your doctor if you feel you need to lie down for extended periods of time while you’re pregnant.
Will pelvic girdle pain affect labour and birth?
In most cases, people with PGP can have a normal vaginal labour and birth. Your doctor may recommend that during labour you position yourself in a way that puts less stress and strain on your pelvis and hips. For example, you might find it less painful to go through labour on your side or in the 'all fours' position.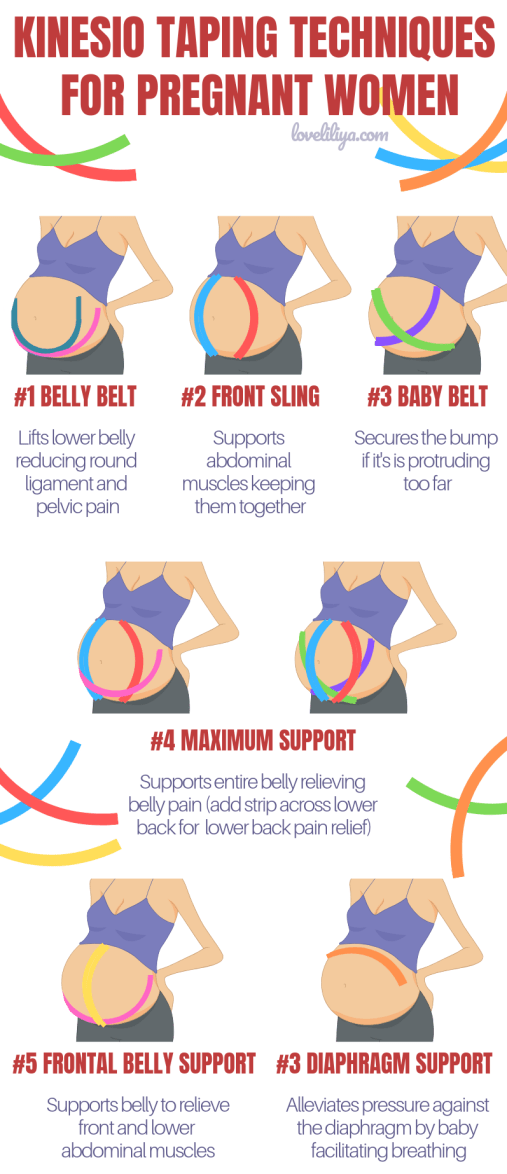 Usually inducing labour early or having a caesarean section are not recommended. These options may occasionally be suggested in severe cases.
Usually inducing labour early or having a caesarean section are not recommended. These options may occasionally be suggested in severe cases.
Will I have pelvic girdle pain in future pregnancies?
Not every person with PGP during pregnancy will have pelvic pain again in future pregnancies. However, recurrence is very common. Nearly 7 out of 10 people with PGP during pregnancy have it again in future pregnancies. Unfortunately, your pain may also be worse during future pregnancies.
If you’ve had PGP in a previous pregnancy, speak with your health team to develop a strategy to manage your pelvic pain early. Managing your pelvic girdle pain early can help to avoid pain from worsening as your pregnancy progresses.
Speak to a maternal child health nurse
Call Pregnancy, Birth and Baby to speak to a maternal child health nurse on 1800 882 436 or video call. Available 7am to midnight (AET), 7 days a week.
Sources:
Department of Health (Pelvic girdle pain), AJGP (Pelvic girdle pain in pregnancy), National Center for Biotechnology Information (Pregnancy-related pelvic girdle pain: an update), Royal Women's Hospital Victoria (Pregnancy related girdle pain fact sheet)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: October 2022
Back To Top
Related pages
- Pelvic floor exercises
- Exercising during pregnancy
- Yoga and Pilates during pregnancy
- Backache in pregnancy
Need more information?
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Pelvic pain in pregnancy - NHS
Some women may develop pelvic pain in pregnancy. This is sometimes called pregnancy-related pelvic girdle pain (PGP) or symphysis pubis dysfunction (SPD).
PGP is a collection of uncomfortable symptoms caused by a stiffness of your pelvic joints or the joints moving unevenly at either the back or front of your pelvis.
Symptoms of PGP
PGP is not harmful to your baby, but it can be painful and make it hard to get around.
Women with PGP may feel pain:
- over the pubic bone at the front in the centre, roughly level with your hips
- across 1 or both sides of your lower back
- in the area between your vagina and anus (perineum)
- spreading to your thighs
Some women may feel or hear a clicking or grinding in the pelvic area.
The pain can be worse when you're:
- walking
- going up or down stairs
- standing on 1 leg (for example, when you're getting dressed)
- turning over in bed
- moving your legs apart (for example, when you get out of a car)
Most women with PGP can have a vaginal birth.
Non-urgent advice: Call your midwife or GP if you have pelvic pain and:
- it's hard for you to move around
- it hurts to get out of a car or turn over in bed
- it's painful going up or down stairs
These can be signs of pregnancy-related pelvic girdle pain.
Treatments for PGP
Getting diagnosed as early as possible can help keep pain to a minimum and avoid long-term discomfort.
You can ask your midwife for a referral to a physiotherapist who specialises in obstetric pelvic joint problems.
Physiotherapy aims to relieve or ease pain, improve muscle function, and improve your pelvic joint position and stability.
This may include:
- manual therapy to make sure the joints of your pelvis, hip and spine move normally
- exercises to strengthen your pelvic floor, stomach, back and hip muscles
- exercises in water
- advice and suggestions, including positions for labour and birth, looking after your baby and positions for sex
- pain relief, such as TENS
- equipment, if necessary, such as crutches or pelvic support belts
These problems tend not to get completely better until the baby is born, but treatment from an experienced practitioner can improve the symptoms during pregnancy.
You can contact the Pelvic Partnership for information and support.
Coping with pelvic pain in pregnancy
Your physiotherapist may recommend a pelvic support belt to help ease your pain, or crutches to help you get around.
It can help to plan your day so you avoid activities that cause you pain. For example, do not go up or down stairs more often than you have to.
The Pelvic, Obstetric & Gynaecological Physiotherapy (POGP) network also offers this advice:
- be as active as possible within your pain limits, and avoid activities that make the pain worse
- rest when you can
- ask your family, friends or partner, if you have one, to help with everyday activities
- wear flat, supportive shoes
- sit down to get dressed – for example, do not stand on 1 leg when putting on jeans
- keep your knees together when getting in and out of the car – a plastic bag on the seat can help you swivel
- sleep in a comfortable position – for example, on your side with a pillow between your legs
- try different ways of turning over in bed – for example, turning over with your knees together and squeezing your buttocks
- take the stairs 1 at a time, or go upstairs backwards or on your bottom
- if you're using crutches, have a small backpack to carry things in
- if you want to have sex, consider different positions, such as kneeling on all fours
POGP suggests that you avoid:
- standing on 1 leg
- bending and twisting to lift, or carrying a baby on 1 hip
- crossing your legs
- sitting on the floor, or sitting twisted
- sitting or standing for long periods
- lifting heavy weights, such as shopping bags, wet washing or a toddler
- vacuuming
- pushing heavy objects, such as a supermarket trolley
- carrying anything in only 1 hand (try using a small backpack)
The physiotherapist should be able to provide advice on coping with the emotional impact of living with chronic pain, such as using relaxation techniques. If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
If your pain is causing you considerable distress, then you should let your GP or midwife know. You may require additional treatment.
Download the POGP leaflet Pregnancy-related pelvic girdle pain for mothers-to-be and new mothers.
You can get more information on managing everyday activities with PGP from the Pelvic Partnership.
Labour and birth with pelvic pain
Many women with pelvic pain in pregnancy can have a normal vaginal birth.
Plan ahead and talk about your birth plan with your birth partner and midwife.
Write in your birth plan that you have PGP, so the people supporting you during labour and birth will be aware of your condition.
Think about birth positions that are the most comfortable for you, and write them in your birth plan.
Being in water can take the weight off your joints and allow you to move more easily, so you might want to think about having a water birth.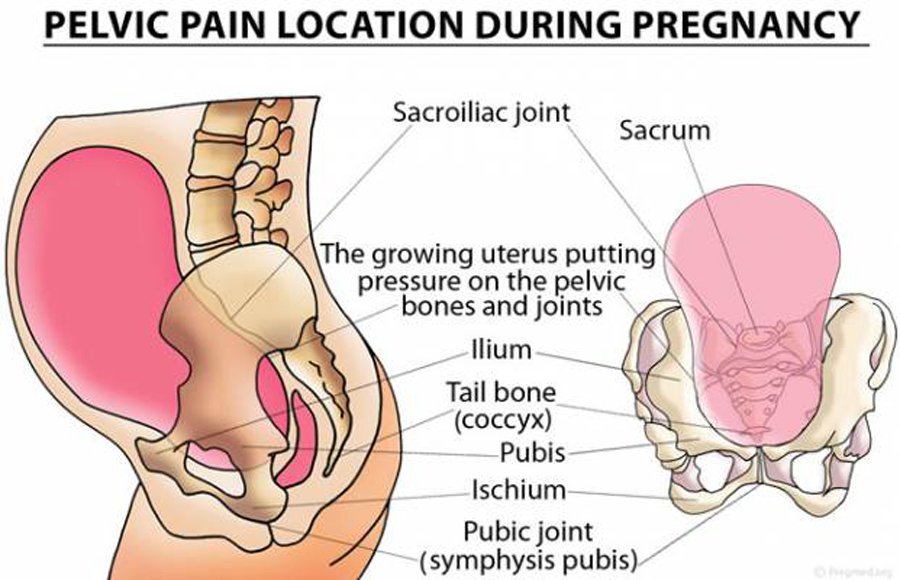 You can discuss this with your midwife.
You can discuss this with your midwife.
Your 'pain-free range of movement'
If you have pain when you open your legs, find out your pain-free range of movement.
To do this, lie on your back or sit on the edge of a chair and open your legs as far as you can without pain.
Your partner or midwife can measure the distance between your knees with a tape measure. This is your pain-free range.
To protect your joints, try not to open your legs wider than this during labour and birth.
This is particularly important if you have an epidural for pain relief in labour, as you won't be feeling the pain that warns you that you're separating your legs too far.
If you have an epidural, make sure your midwife and birth partner are aware of your pain-free range of movement of your legs.
When pushing in the second stage of labour, you may find it beneficial to lie on one side.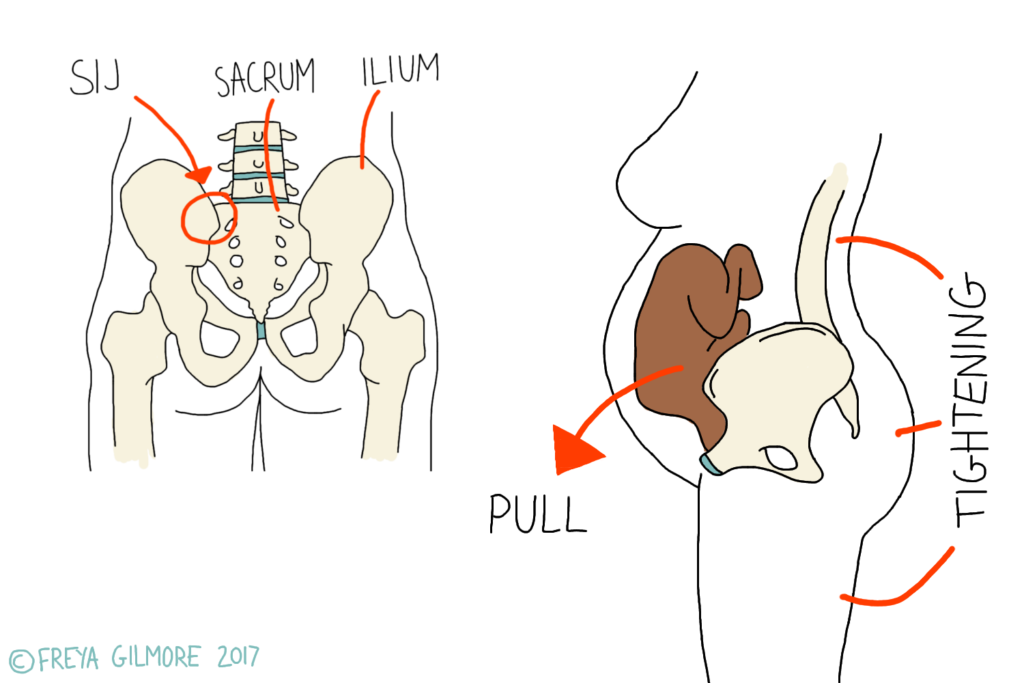
This prevents your legs from being separated too much. You can stay in this position for the birth of your baby, if you wish.
Sometimes it might be necessary to open your legs wider than your pain-free range to deliver your baby safely, particularly if you have an assisted delivery (for example, with the vacuum or ventouse).
Even in this case, it's possible to limit the separation of your legs. Make sure your midwife and doctor are aware that you have PGP.
If you go beyond your pain-free range, your physiotherapist should assess you after the birth.
Take extra care until they have assessed and advised you.
Who gets pelvic pain in pregnancy?
It's estimated that PGP affects up to 1 in 5 pregnant women to some degree.
It's not known exactly why pelvic pain affects some women, but it's thought to be linked to a number of issues, including previous damage to the pelvis, pelvic joints moving unevenly, and the weight or position of the baby.
Factors that may make a woman more likely to develop PGP include:
- a history of lower back or pelvic girdle pain
- previous injury to the pelvis (for example, from a fall or accident)
- having PGP in a previous pregnancy
- a physically demanding job
- being overweight
- having a multiple birth pregnancy
healthtalk.org has interviews with women talking about their experiences of pelvic pain in pregnancy.
Read more about coping with common pregnancy problems, including nausea, heartburn, tiredness and constipation.
Find maternity services or physiotherapy services near you.
Community content from HealthUnlockedMethods for the prevention and treatment of pain in the lumbar region and pelvic region during pregnancy
Review question
We were looking for evidence of the effect of any treatment used to prevent or treat low back pain, pelvic pain, or both during pregnancy.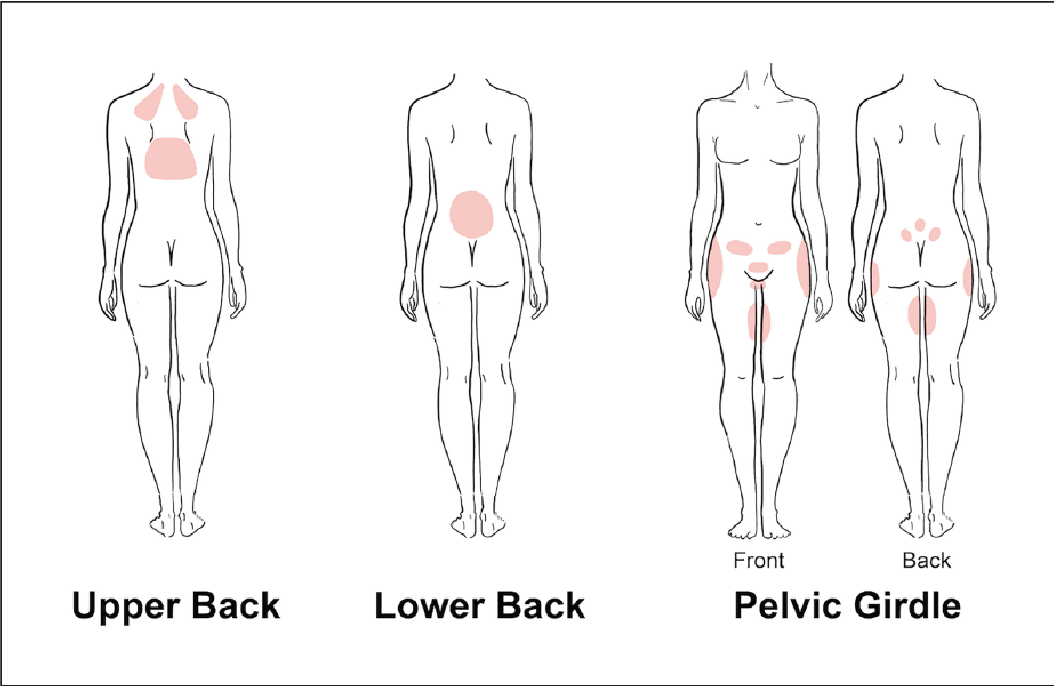 We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
We would also like to know if the treatment reduced disability or sick leave, and if the treatment caused any side effects for pregnant women.
Relevance
Pain in the lumbar region, pelvic region, or both is a common complaint during pregnancy, often progressing as the pregnancy progresses. This pain can interfere with the daily activities, work, and sleep of pregnant women. We wanted to find out which treatment or combination of treatment options would be better than conventional prenatal care for pregnant women with these complaints.
Study profile
This evidence is current to 19 January 2015. We included 34 randomized trials with 5,121 pregnant women aged 16 to 45 in this updated review. The women were between 12 and 38 weeks pregnant. Studies have looked at various treatments for pregnant women with low back pain, pelvic pain, or both types of pain. All treatments were added to routine antenatal care and only compared to routine antenatal care in 23 studies.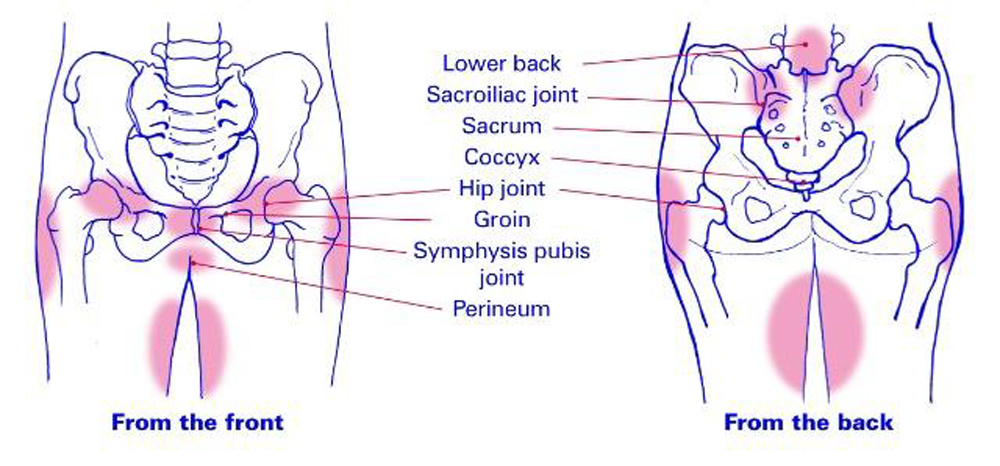 Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Symptoms in women in the studies were assessed in many ways, from self-reported pain to sick leave with the results of special tests.
Main results
Pain in the lumbar region
When we combined the results of seven studies (645 women) that compared any form of physical exercise with routine prenatal care, exercise (lasting five to 20 weeks), we found that women with low back pain improved and disability rates decreased .
Pelvic pain
Less evidence is available for the treatment of pelvic pain. Two studies showed that women who participated in group exercise and received training in pain management reported no difference in pelvic pain compared to women who received routine prenatal care.
Pain in the lumbar region and pelvis
Results from four studies (1,176 women) when combined showed that an 8 to 12 week exercise program reduced the number of women who complained of low back and pelvic pain. In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
In two studies (1,062 women), ground exercises of various formats also reduced sick leave-related low back and pelvic pain.
However, two other studies (374 women) found that group exercise and education was no better in preventing pain, both in the pelvic region and in the lumbar region, compared with conventional prenatal care.
There have been a number of separate studies that have evaluated different treatment options. These results confirm that craniosacral therapy, osteomanipulation therapy, or multimodal intervention (manual therapy, exercise, and education) may be beneficial.
When side effects were reported, there were no long-term side effects in any of the studies.
Quality of evidence and conclusions
There is low-quality evidence that exercise reduces pain and disability in women with low back pain, and moderate-quality evidence for the effect of exercise on reducing sick leave and reducing the number of women with both lower back and pelvic pain complaints. The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
The quality of the evidence depends on problems with study design, small numbers of women, and variable results. Ultimately, we believe that future research is likely to change our findings. There is not enough good quality evidence to make confident decisions about the treatment of these complaints.
Translation notes:
Translation: Kong Hong Han. Editing: Gamirova Rimma Gabdulbarovna, Ziganshina Lilia Evgenievna. Project coordination for translation into Russian: Cochrane Russia - Cochrane Russia (branch of the Northern Cochrane Center on the basis of Kazan Federal University). For questions related to this translation, please contact us at: [email protected]
Pelvic pain in early pregnancy | Symptoms
Ectopic pregnancy
Signs: Abdominal or pelvic pain that is often sudden and persistent (not crampy), localized, and may or may not be accompanied by vaginal bleeding. If an ectopic pregnancy is terminated, fainting, dizziness, or palpitations may occur.
Miscarriage (threatened miscarriage or ongoing spontaneous abortion)
Signs: Spasmodic pain in the pelvic area, often radiating to the abdominal cavity. Often vaginal bleeding, sometimes with the release of fragments of fetal tissue.
Septic abortion (infection of the contents of the uterus before, during or after a miscarriage)
Signs: Usually in women who have already had an abortion (usually performed by an inexperienced doctor or by the women themselves). Fever and chills, persistent abdominal or pelvic pain, and pus-filled vaginal discharge.
Normal changes during pregnancy (includes distension and growth of the uterus in early pregnancy)
Signs: Cramping or burning sensation in the lower abdomen, pelvis and/or lower back.
Uterine fibroma degeneration
Signs: Pelvic pain that starts suddenly and is usually accompanied by nausea, vomiting, and fever. Sometimes vaginal bleeding.
Torsion (twisting) of the ovarian appendages
Signs: Pain in the pelvic area that starts suddenly, may be with colic, which is often mild if the ovary uncoils on its own, often with nausea or vomiting.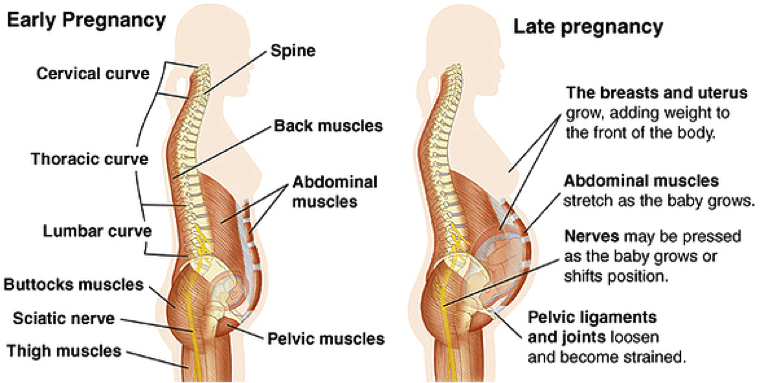
Rupture of a corpus luteum cyst (forms in the ovary from which the egg is released after ovulation)
Signs: Abdominal or pelvic pain that originates in a specific area, sometimes resembling pain due to ovarian torsion;
usually occurs suddenly. Vaginal bleeding.
Pelvic inflammatory disease
Signs: Pain in the pelvic area that lasts a long time, usually develops gradually, as a rule, is felt on both sides.
Vaginal discharge containing pus. Sometimes fever or chills. It is more common in women who have sex with new partners and do not use condoms or diaphragms.
Appendicitis
Signs: As a rule, continuous pain and tenderness in the lower abdomen on the right. There may be pain in a different place (higher in the abdomen) or a different nature of pain (weaker and more crampy) compared to non-pregnant women.
Urinary tract infections
Signs: Discomfort that is felt just above the pubic bone.