How to intubate a child
Intubation & Mechanical Ventilation | Riley Children's Health
- Find A Doctor
- On This Page:
- What to Expect
- Key Points to Remember
- Related Conditions & Departments
Mechanical ventilation uses a breathing machine called a ventilator to help move air into and out of the lungs. In order to connect a child’s lungs to a ventilator, a doctor may insert a narrow plastic tube through the mouth and into the windpipe through a process called intubation.
Intubation and mechanical ventilation may be used for babies or children who are experiencing severe respiratory problems and need emergency treatment. Intubation and mechanical ventilation may also be used to help a child breathe while sedated during surgery.
Older children may need intubation and mechanical ventilation when being treated for a severe asthma attack, after a serious injury or near drowning or during a severe viral illness. In many cases, older children can receive oxygen through a face mask or nasal tube as long as the airway is clear. If the child is unconscious, or if he or she is conscious but has injuries that make it impossible to breathe deeply and get enough oxygen, intubation may be necessary.
What to Expect
What to Expect
You can expect the following if your child requires intubation and mechanical ventilation at Riley at IU Health:
- The care team may give your child medicines to prevent any discomfort during the treatment.
- The care provider will intubate your child by inserting a special plastic tube into the mouth and gently guiding it into the windpipe.
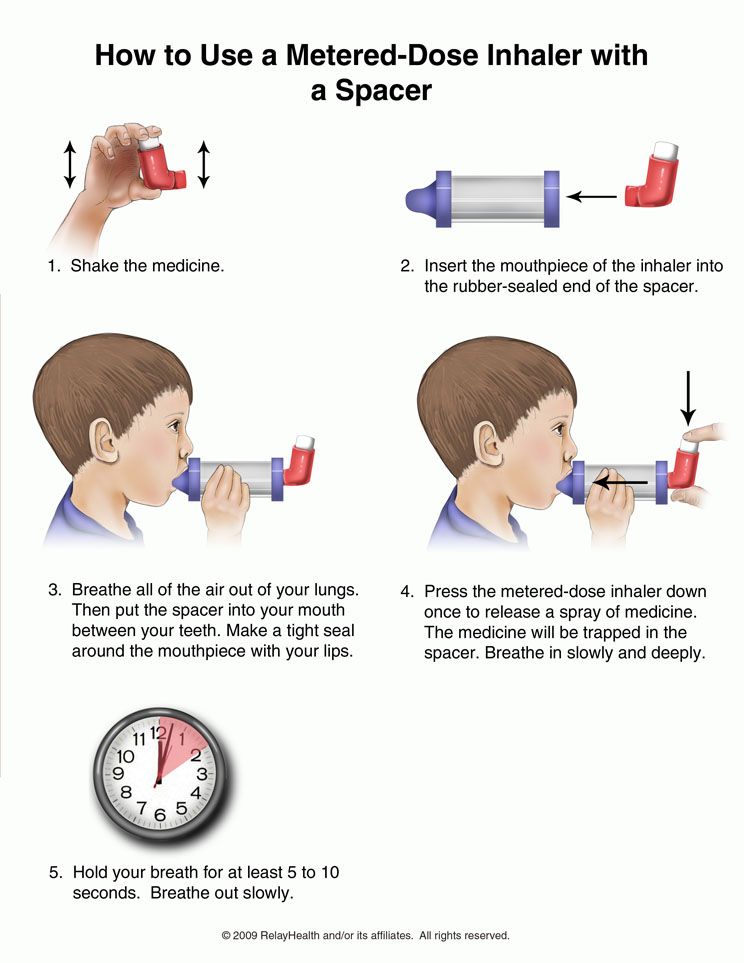 This tube connects to the ventilator.
This tube connects to the ventilator. - Once your child is intubated, a trained specialist will program the ventilator to move air in and out of the lungs at the right volume and speed. These settings may change during treatment.
- As your child’s lungs or ability to breathe improve, the settings will adjust to wean him or her off the ventilator slowly so that he or she can safely learn to breathe normally without it.
Babies and children may need to use a ventilator for a few hours, a few days or even a few months depending on their specific health needs and overall condition.
Key Points to Remember
Key Points to Remember
- Intubation and mechanical ventilation may be used for babies or children who are experiencing severe respiratory problems and need emergency treatment.
- Mechanical ventilation uses a breathing machine called a ventilator to help move air into and out of the lungs.

- In order to connect a child’s lungs to a ventilator, a doctor may insert a narrow plastic tube through the mouth and into the windpipe through a process called intubation.
- Ventilators are adjusted over the course of treatment to match your child’s condition.
Intubating An Infant or Toddler, discussion of intubation technique by age
This article discussion some of the key anatomy, physiology, and technical points to intubating an infant or small child safely. I’ve been hard at work on writing and illustrating my upcoming book on pediatric airway management so I thought I would spend some time talking about care of our littlest patients.
Providers who infrequently care for children less than two years of age are often rightfully anxious when faced with a sick child, especially if airway management is required. This is especially true if the child is less than one. Healthy respect is certainly indicated because airway complications are one of the leading causes of pediatric cardiac arrest.
Children are not small adults. From infants to toddlers to teenagers, the anatomy and physiology of the child is continuously morphing until finally reaching the adult form and function. We all know this instinctively. When we look at a child we can often tell how old he or she is simply by looking at head size, characteristics of the face, length of neck, shape of the body, and how long the arms and legs are related to the trunk. It should not be surprising that the inside of the child is changing as well.
Even placing an oral airway and using a mask in an infant can seem more challenging because of the size and fragility of the patient.
Infants and young children are small. The head of a newborn infant can fit on the palm of my hand. The palm of a premature infant’s hand may be the same size as my thumbnail. It’s challenging to open the airway of such a small infant when adult fingers dwarf the size of the baby’s mouth and all of the instruments are smaller. And babies are fragile, with little reserve.
Like adults, children can be small or tall, lean or overweight. But unlike adults, their airway anatomy is changing shape and structural relationships as they grow. A particular 2 year old may be as tall as a particular 6 year old, or as heavy as a particular 8 year old, but all have very different airways.
Intubating an infant or small child is more of a challenge than an older child or adult both because of their anatomical differences as well as their physiologic predisposition for hypoxia. One can certainly argue that faced with elective care, that only experienced providers should manage the airways of infants and children less than two. However, medical care is not always elective.
Faced with a sick child, especially in more urgent settings, anyone who can ventilate and intubate an adult can also ventilate or intubate an infant or toddler safely —if they take the differences in anatomy and physiology into account, and are gentle and methodical in their approach. Illustrations and photos from Anyone Can Intubate: a Step by Step Guide, and Pediatric Airway Management: a Step by Step Guide.
Illustrations and photos from Anyone Can Intubate: a Step by Step Guide, and Pediatric Airway Management: a Step by Step Guide.
Premature baby boy in intensive care, one day old but with a gestational age about 31 weeks.
It’s very common to be intimidated when treating an infant because infants are very small compared to the size of your adult hands. Premature infants are especially challenging. Infants are fragile and have little physiological reserve. However, if you prepare what you need ahead of time and use your natural anxiety to make you alert, methodical and gentle, then you will not hurt the baby.
Remember, the most important thing is oxygenation and ventilation. Even if you don’t feel you can intubate, don’t fail to open the airway or assist ventilation until someone who can arrives.
Let’s quickly review why infants and toddlers are more at risk of hypoxia.
Infants are at much higher risk of developing hypoxia for a many reasons. Some of the major ones include:
- Metabolic Rate
- approximately double the adult metabolic rate: hypoxia develops more quickly
- Lungs
- Lung volumes, especially, functional residual capacity (FRC) are smaller.
 Smaller oxygen tank means less tolerance for apnea
Smaller oxygen tank means less tolerance for apnea - Fewer alveoli means less gas exchange surface
- Minute ventilation is dependent on more rapid rate due to limited ability to increase tidal volume
- Deadspace is higher in the infant (3 ml/kg vs adult’s 2 mg/kg)
- Lung volumes, especially, functional residual capacity (FRC) are smaller.
- Chest wall/Diaphragm
- ribs more horizontal, with less ability to expand chest
- chest wall more complaint and easily collapses inward with either upper or lower airway obstruction or increased resistance to breathing
- muscles of respiration tire easily
- Nervous system
- hypoxia causes bradycardia as first response, not tachycardia
- brain is easily sedated
- Cardiac
- Cardiac output is primarily rate dependent
- bradycardia produces hypotension and worsens hypoxia
- hypovolemia easily produces shock, decreased perfusion, and hypoxia
- Cardiac output is primarily rate dependent
It is easy to lose track of time during an intubation when the baby is apneic. Paying close attention to how well a baby is ventilated and oxygenating is imperative. Stop and ventilate if the intubation attempt is taking longer than 30 seconds to a minute. You want to stop a prolonged intubation attempt and start ventilating before the baby starts to desaturate if you can.
Paying close attention to how well a baby is ventilated and oxygenating is imperative. Stop and ventilate if the intubation attempt is taking longer than 30 seconds to a minute. You want to stop a prolonged intubation attempt and start ventilating before the baby starts to desaturate if you can.
Not only is the size of the airway different, the shapes and locations of the structures also vary between the infant and the adult.
The table and illustration summarize the major anatomical differences in the infant and toddler airway compared to the older child and adult. The younger the child, the more different the airway.
The infant airway is quite different than an adult airway and you must take these difference into account when you intubate.
In addition, the appearance of the larynx itself is quite different. Over an above the anatomical variation, the color of the vocal cords in an infant is usually pink, rather than white, making identification more challenging.
Curved blades depend on displacing the tongue and soft tissue forward to lift the epiglottis. If you can’t displace the tongue forward, you won’t be able to see the larynx.
Straight blades are very helpful in situations where there is little room to displace the tongue and attached tissues forward. Examples include:
- larynxes higher in the neck (babies are a good example)
- short chins
- short necks
- large tongues
- obesity, especially with double chins
- larynxes fixed from scar, trauma, or mass effect.
We often use straight blades in young children for multiple reasons. The pediatric larynx is located higher in the neck than an adult, and their tongues are larger relative to the size of their mouths. Babies in particular have short necks. The smaller separation between the hyoid and the thyroid cartilage also makes displacing the tongue and associated tissues forward more difficult. A straight blade lifts the epiglottis, allowing a clear view of the cords.
Laryngoscope blades come in different sizes and you should choose the optimal size if you can.
Choose the optimal size blade for the size the child. You can estimate size by holding the blade up against the outside of the child’s jaw and see if it is long enough to reach the larynx. As you see in the illustration, an adult blade would be way too long. However, in an emergency if you only had an adult blade, you could insert just the very tip.
A MAC blade in a child younger than 2-3 years can fold the epiglottis downward. Use it like a Miller straight blade to lift the epiglottis.
In a baby or toddler, the curved MAC will often fold the child’s epiglottis down over the larynx, blocking your view of the cords.
This happens for two reasons related to the fact that the larynx is higher in the neck:
- the tissue folds in the vallecula pull the trap door of the epiglottis closed when pressed
- there is less room to displace the tongue and soft tissue under the tongue forward
If you must use a curved blade you can, if needed, use it to pick up the epiglottis.
However, to be able to see the larynx with a straight blade you have to be able to extend the head backward. If your patient can’t tilt his head back, a straight blade will be more difficult and a curved blade might be better. For a baby, this often means raising the shoulders to get the head and larynx into a good position.
When preparing for intubation, head and neck positioning can be key. For an infant, placing a small rolled towel under the shoulders lifts the body and compensates for the large round occiput, bringing the ear canal into alignment with the sternal notch.Older children may need a towel under their head. C. Whitten
When positioning the head, avoid raising it too high off the intubating surface. For easier visualization, the ear canal should be roughly level with the sternal notch, regardless of age. The baby’s occiput is larger and rounder than an adult’s. Placing a small folded towel or similar thickness object under an infant’s shoulders raises the rest of the body and straightens the airway path. Toddlers have a built in sniff position due to the occiput and may not need a towel. For an older child placing the towel under the head works best.
Toddlers have a built in sniff position due to the occiput and may not need a towel. For an older child placing the towel under the head works best.
The height of the occiput in an unconscious infant can also flex the baby’s head forward when the child lies flat in the bed. This can obstruct the airway.
The infant head tends to roll and stabilizing it make intubation faster and easier.
The infant occiput tends to roll, making the act of balancing the baby’s head on your blade a challenge. There are several ways to deal with this tendency:
- place a rolled towel on either side of the head
- have an assistant steady the head for you
- hold the head steady with your own right hand while placing your blade. Once you see the larynx let g, lift your ETT, then intubate
- use a small, flat gel “donut” designed for this task
- practice
Sometimes tipping the infant’s head backwards with your right hand will allow the mouth to fall open. If it doesn’t, then open the mouth with your right index finger and thumb as far to the right side of the mouth as possible. The infant’s mouth is very small compared to the size of your hand. Failure to place your fingers far to the right can block your view and prevent insertion of the blade. .
If it doesn’t, then open the mouth with your right index finger and thumb as far to the right side of the mouth as possible. The infant’s mouth is very small compared to the size of your hand. Failure to place your fingers far to the right can block your view and prevent insertion of the blade. .
Slowly lift the mandible upward as you advance the blade. Don’t pinch the lower lip between the gums/teeth and the blade as you lift. Avoid using the upper gum line or teeth as a fulcrum.
The infant tongue is much larger relative to the mouth and jaw than the adult. Failure to sweep the tongue to the left with your laryngoscope blade will leave you no room for visualization or for tube passage.
Continue to lift the jaw upward until you see the larynx.
Not only is the larynx smaller in an infant, it’s shaped differently, The epiglottis is shorter and more omega shaped. It’s softer and harder to pick up. The vocal cords tend to be pink rather than white and therefore may be harder to spot.
Comparison adult vs. infant larynx. Note the differences not just in size, but in shape and color.
It’s very easy in a child to insert the laryngoscope blade too deep, as in the right picture. If too deep you will not see recognizable anatomy because you are looking down the esophagus and hiding the larynx.
It’s very easy to insert the blade too deeply and into the esophagus of such a tiny patient. If you can’t identify anatomy, then pull the blade back slowly while you watch. Often the larynx will drop into view.
Picking up the epiglottis with the blade tip in a child less than two years old can be hard due to its short, stiff, “U” shaped form. Meticulous placement of the tip of the blade is necessary.
The arytenoids and vocal cords in the infant and young child incline anteriorly. This slant can cause the tip of the pediatric tube to hang up on the anterior commissure during insertion. Rotating the tube to the right or left usually allows the tip to slip off the anterior commissure and pass. While there may be a blind spot at the moment of intubation, you can often see the arytenoids behind the tube. Be gentle. Pediatric airways are small, delicate and prone to edema.
While there may be a blind spot at the moment of intubation, you can often see the arytenoids behind the tube. Be gentle. Pediatric airways are small, delicate and prone to edema.
Remember, the cricoid ring is smaller than the opening between the vocal cords. You can sometimes insert an ETT through the cords but not beyond the cricoid. Forcing a tube can cause traumatic swelling. If the tube won’t pass, use a smaller one.
Head position and movement of surrounding tissues shifts cartilages and may affect your ability to see the vocal cords. Sometimes the larynx lies anterior to your field of view during laryngoscopy. This view is often described as an “anterior larynx” and it commonly occurs with poor head positioning, as well as in patients with obesity, larynxes located higher in the neck than average, and in patients with poorly developed mandibles or weak chins. Ask your assistant to provide cricoid pressure when you can’t see the larynx during intubation.
Providing cricoid in an infant or young child may mean using just one finger to press on the larynx rather than two.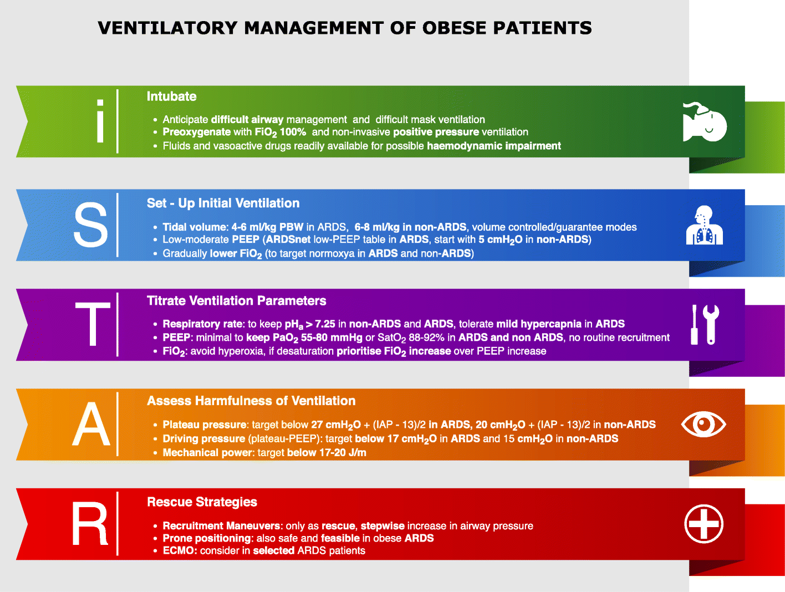 Use light pressure as the soft cartilage is easily distorted and the larynx compressed. Heavy cricoid pressure in an infant can distort the airway and make intubation more difficult.
Use light pressure as the soft cartilage is easily distorted and the larynx compressed. Heavy cricoid pressure in an infant can distort the airway and make intubation more difficult.
Infants and young children can’t hold their breaths as long as an adult before the onset of hypoxia. If you have trouble intubating, stop and ventilate before trying again. During awake intubations let the patient rest and breathe oxygen. Lack of ventilation hurts patients, not the lack of an endotracheal tube. The baby will get hypoxic quickly when apneic.
Remember, if mask ventilation is difficult that you can always place an LMA or other subpraglottic device to allow easier ventilation while you get extra help, prepare for a different approach, or if the intubation is elective even wake the patient up.
Minimal swelling can cause tracheal obstruction because the larynx and trachea are so small. One mm circumferential swelling in an adult with a 10 mm trachea causes only a 44% decrease in cross-sectional area.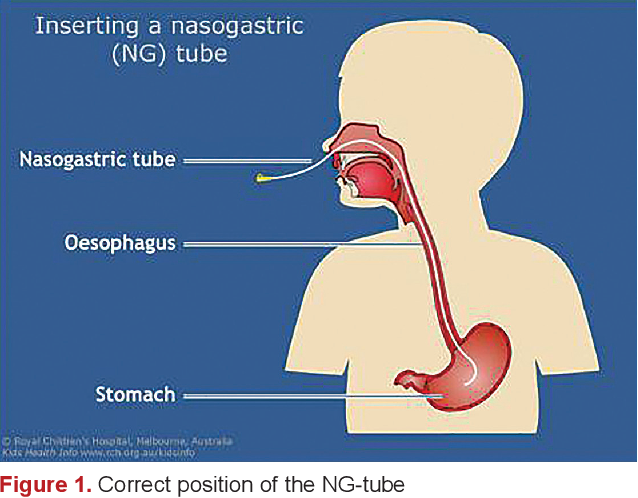 If an infant with a 4 mm trachea develops 1 mm circumferential edema from coup, or any other cause, there is a 75% decrease in area. Thus swelling from infections or trauma can have a much more devastating effect.
If an infant with a 4 mm trachea develops 1 mm circumferential edema from coup, or any other cause, there is a 75% decrease in area. Thus swelling from infections or trauma can have a much more devastating effect.
A little edema in a pediatric airway causes a lot of potential obstruction.
In addition, a little change in airway width causes a big change in resistance to breathing. A normal infant’s 4 mm diameter larynx has 16 X the resistance to flow of a normal adult larynx of 8 mm. The infant has less ability to compensate for increased resistance to airflow. So infections like croup and epiglottitis, or an asthma attack narrowing terminal bronchi, or an aspirated peanut stuck in the esophagus but compressing the soft trachea can all place serious limits on the infant or toddler’s ability to breathe.
A little edema in a child’s airway increases resistance to breathing significantly.
Always verify ETT placement carefully. Sound over an infant’s chest and abdomen transmit easily and esophageal intubation can be missed if you are not cautious.
If you fail to recognize esophageal intubation, your first sign may be hypoxia, bradycardia and potentially cardiac arrest.
The tip of the tube should be midway between the larynx and the carina. Securing the tube at the correct depth in an infant is especially critical. Too deep and it will easily block a mainstem bronchus. Too shallow and extubation is likely when the baby moves. In addition, when using a cuffed tube, the cuff must be below the cords and below the cricoid cartilage. since the infant trachea is so short, margin for error is also limited.
Endotracheal tubes have depth markings in centimeters. You should insert an uncuffed tube until the lowest most prominent mark is level with the vocal cords. Insert cuffed tubes until the cuff just passes through the cords, and is below the cricoid ring.
Size of endotracheal tube and depth of insertion is important to ensuring success and avoiding injury.
The depth of insertion can be estimated as:
(age in years divided by 2) plus 12
The most familiar formula for calculating endotracheal tube depth applies to children greater than 2 years of age. Note: Depth ATL (at the lip) calculations are in centimeters.
Note: Depth ATL (at the lip) calculations are in centimeters.
Depth ATL (at the lip) = (age in years/2) + 12
For infants and children younger than 2 years of age, calculate endotracheal tube depth by using the formula: [Hazinski, M.F., (Ed.) (2002) Textbook of Advanced Pediatric Life Support. American Heart Association.]:
Depth ATL (at the lip) = Calculated uncuffed ETT ID x 3
Endotracheal tube depth of insertion formulas have been clinically validated for the neonatal patient population, for patients weighing more than 750 grams up to 4 kilograms [Peterson, J., et al. (2006) Accuracy of the 7-8-9 Rule for Endotracheal Tube placement in the neonate. Journal of Perinatology 26; 333-336].
Depth ATL (at the lip) = weight (Kg) + 6
The chart in Figure 7-1 has suggested sizes. Although these formulas are reasonably accurate, you still must verify bilateral breath sounds as individual variability in height, and therefore pulmonary anatomy, is common in children of the same age.
Extension of the neck causes the endotracheal tube to rise within the trachea. Inadvertent extubation can occur of the tube is too high. Flexion of the head causes it to descend, possibly causing mainstem intubation (Fig. 7-58 a,b,c). “The hose follows the nose” is a useful memory aide. This means that you must be constantly alert to potential misplacement of an endotracheal tube.
Since airway tissue is friable and edema so devastating in such a small airway, it’s important to check for a leak after intubation to make sure you have not inserted too large a tube. The chart above has some suggested sizes for age but all children are different.
Listen at the child’s mouth for a leak when using an uncuffed tube. You want to hear an air leak around the tube at about 15-20 cm of water pressure after the child’s lungs are fairly well inflated. A leak at this pressure allows adequate lung inflation but avoids excessive pressure on the tracheal wall.
The absence of such a leak means that the tube may be pressing excessively on the inside the cricoid ring, which can damage the mucosa. Excessive pressure can also potentially injure the recurrent laryngeal nerves, causing transient or permanent vocal cord paralysis.
Excessive pressure can also potentially injure the recurrent laryngeal nerves, causing transient or permanent vocal cord paralysis.
A leak is too large if it prevents effective inflation of the lungs. Upsize the uncuffed endotracheal tube one half size if the leak occurs at less than 10 cm h3O.
Downsize by one half size if there is no leak at 20 cm h3O or if there is resistance to passing the ETT into the trachea.
Remember that because the cricoid is more elliptical than round in the small child, you may still have a small leak despite the fact that the tube may be causing mucosal pressure. If the tube was somewhat tight going in and the leak is small, consider whether changing it to a smaller size is prudent.
A problem with uncuffed tubes is that if too small a tube is inserted, then you may not be able to provide adequate tidal volumes because of too large an air leak around the tube. Too large a leak forces the need to repeat the laryngoscopy and replace the tube, actions that increase the risk of trauma and edema.
Use of cuffed tubes avoid this problem. We talked about cuffed tubes in pediatric patients earlier. When using a cuffed tube, you can seal the leak with the cuff, avoiding repeat laryngoscopies and tube changes. When sealing the leak, always inflate the cuff until the leak just stops. (follow this link)
However, occasionally you will insert a cuffed tube and then find that there isn’t a leak — even though the cuff is still deflated.
In this case you should not automatically inflate the cuff, since this might result in overinflation, which can also damage mucosa and potentially injure the recurrent laryngeal nerve as it travels through the cricoid ring.
On the other hand, when the cuff remains deflated, the folds from the deflated cuff can potentially cause mucosal injury because pressure against the mucosa is now uneven.
In this situation you should consider downsizing a cuffed ETT that does not have a leak with the cuff still deflated, to a smaller one that requires some inflation. This is especially true if the tube will be in place for a longer period of time. To make the decision to change the tube you must balance:
This is especially true if the tube will be in place for a longer period of time. To make the decision to change the tube you must balance:
- the risk of edema and trauma from the repeat laryngosopy and tube exchange
- the length of time the tube will be in place (a 30 minute OR case offers a different risk profile than days in the ICU)
- how difficult it was to place the tube
When intubating, don’t hesitate to ask for help. Also, if you are inexperienced in infant airway management, unless time is critical, you should have a more experienced provider with you before you start in case of problems. Once hypoxia develops in an infant or small child during an airway emergency, the time before cardiovascular collapse is short.
Open the laryngoscope blade of the appropriate size for the child. Straight blades are better for infants and small children. Note that you should optimally wear gloves.
Balancing the head of an infant can be harder due to the small size of the laryngeal structures. The relatively round and large occiput tends to roll. Here the incubator is stabilizing the head with his right hand as he starts to place the laryngoscope blade.
The relatively round and large occiput tends to roll. Here the incubator is stabilizing the head with his right hand as he starts to place the laryngoscope blade.
Sweep the tongue to the left and visualize the larynx. Be gentle, your patient is fragile.
Insert the endotracheal tube. Never force a tube. If it won’t slide in easily choose a smaller size. A helper is giving cricoid pressure. In an infant, pressing too hard on the cricoid ring can distort the airway and compress the trachea. Note cricoid pressure is being given with just one finger.
Once intubated, carefully remove the blade while securely holding the tube. Extubation is easy when your patient is so small. Be careful when you start to ventilate to use small and appropriately sized tidal volumes with the least amount of pressure needed.
Complications from intubation can occur in any patient at any time but infants and small children are at higher risk because their airways are smaller, they lack cardiorespiratory reserve, and in many ways they are predisposed to respiratory distress and failure.
Potential complications that can more easily happen in an infant are:
- Mainstem intubation and accidental extubation
- trachea is short and movement of head can shift ETT up or down 1-2 cm, which can be enough to malposition the tube, especially in premature infants
- kinking of the endotracheal tube: because it’s tiny, thin and very flexible
- pneumothorax
- because too large a tidal volume or too high inflation pressure can cause barotrauma easily. A tidal volume of 7 ml/kg in a 3 kg baby is 21 ml, less than two tablespoons.
Monitor your intubated child carefully and be prepared for emergencies.
May The Force Be With You
Christine Whitten MD,
author Anyone Can Intubate: A Step By Step Guide, 5th Edition &Pediatric Airway Management: A Step-by-Step Guide
Illustrations copyright C. Whitten MD 2016
Please click on the covers to see inside my books at amazon.
 com
com
Like this:
Like Loading...
20 complications of tracheal intubation in anesthesiology / Anest-Rean
Predisposing factors:
- Patients with difficult airways
- Insufficient knowledge and technical skills of the anesthetist
- Emergency intubation (without airway assessment)
- Faulty equipment (laryngoscope, anesthesia machine)
1. Failed intubation
Difficult airways include difficult mask ventilation, difficult laryngoscopy, and difficult intubation.
Intubation failed - neither ventilated nor intubated
Death or brain damage occurs in 85% of cases in this catastrophe. At the same time, the main problems are insufficient ventilation, poor quality care, esophageal intubation and failure to identify the problem . The approach to difficult airways and the standards for managing difficult airways are outlined in the ASA (American Society of Anesthesiologists) algorithm, more here. Emergency ventilation methods in situation “cannot be ventilated or intubated” include use of a laryngeal mask and transtracheal jet ventilation.
The approach to difficult airways and the standards for managing difficult airways are outlined in the ASA (American Society of Anesthesiologists) algorithm, more here. Emergency ventilation methods in situation “cannot be ventilated or intubated” include use of a laryngeal mask and transtracheal jet ventilation.
Conicotomy (not tracheostomy) is the preferred method of surgical access to the airway in an emergency such as the "cannot be ventilated or intubated" problem. Main problem with jet ventilation - risk of barotrauma due to the high pressure of the oxygen mixture. Respiratory rate should be limited to the minimum necessary to prevent life-threatening hypoxia ( 4-6 per minute ) and conicotomy or tracheostomy should be undertaken immediately.
2. Injury of the spinal cord and spine
Injury of the spinal cord and spine — severe complication of tracheal intubation . Extension of the cervical spine during laryngoscopy can lead to spinal cord injury and tetraplegia. This complication of tracheal intubation is most likely in patients with fractures or malformations of the cervical spine, tumors or osteoporosis. In patients with suspected cervical instability the head should always be in a neutral position during laryngoscopy and intubation; hyperextensions are strictly avoided . Alternative methods of tracheal intubation that avoid manipulation of the cervical spine, such as fiber optic intubation, may be considered.
Extension of the cervical spine during laryngoscopy can lead to spinal cord injury and tetraplegia. This complication of tracheal intubation is most likely in patients with fractures or malformations of the cervical spine, tumors or osteoporosis. In patients with suspected cervical instability the head should always be in a neutral position during laryngoscopy and intubation; hyperextensions are strictly avoided . Alternative methods of tracheal intubation that avoid manipulation of the cervical spine, such as fiber optic intubation, may be considered.
3. Acute traumatic complications of intubation
Acute traumatic complications of intubation - damage to the lips, teeth, tongue, nose, pharynx, larynx, trachea and broncho in which may occur during laryngoscopy and intubation. Most traumatic complications do not lead to serious morbidity or mortality. However, some of them require immediate elimination. The most frequent traumatic complications : damage to the larynx, pharynx and esophagus. Most often, injuries of the trachea and esophagus are accompanied by difficult intubation.
Most traumatic complications do not lead to serious morbidity or mortality. However, some of them require immediate elimination. The most frequent traumatic complications : damage to the larynx, pharynx and esophagus. Most often, injuries of the trachea and esophagus are accompanied by difficult intubation.
4. Dangerous autonomic reflexes
Arterial hypertension, tachycardia, arrhythmias, increased intracranial and intraocular pressure are the result of vegetative reflexes. Laryngoscopy and tracheal intubation cause reflex sympathetic stimulation and are associated with elevated plasma catecholamines , hypertension, tachycardia, myocardial ischemia and decreased contractility, ventricular arrhythmias, and intracranial hypertension. Hypoxia and hypercapnia enhance the autonomic response.
The magnitude of autonomic reactions is related to the duration of laryngoscopy and can be quite severe during complex intubation with multiple, prolonged attempts at tracheal intubation.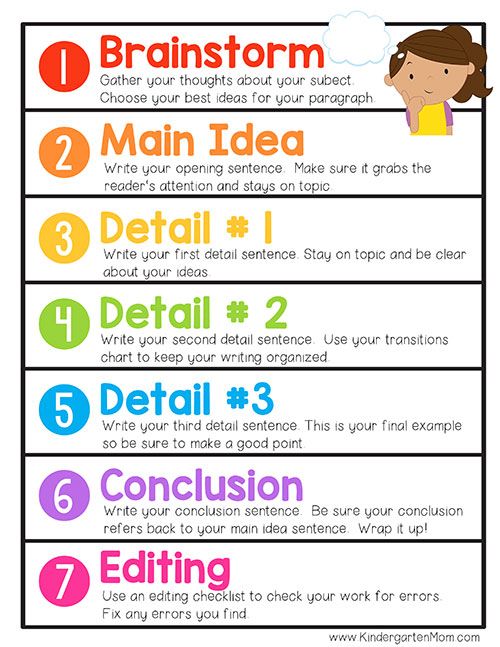 These reactions may be particularly harmful in patients with hypertension, CAD, myocardial dysfunction, and elevated intraocular and intracranial pressure. In patients with limited coronary reserve, this may cause ischemia or heart failure. Patients with cerebral vascular disease may experience intracranial hypertension or hemorrhage.
These reactions may be particularly harmful in patients with hypertension, CAD, myocardial dysfunction, and elevated intraocular and intracranial pressure. In patients with limited coronary reserve, this may cause ischemia or heart failure. Patients with cerebral vascular disease may experience intracranial hypertension or hemorrhage.
These reactions can be minimized by rapid and smooth tracheal intubation under adequate general anesthesia. Narcotic analgesics block autonomic reactions during tracheal intubation, and are used in premedication, for example, fentanyl at a dose of 3–5 µg/kg.
5. Laryngospasm
Laryngospasm is a complication of tracheal intubation. This may be the result of an attempted tracheal intubation under surface anesthesia. Lack of adequate lung ventilation leads to hypoventilation and, consequently, to hypoxia. To relieve laryngospasm, it is necessary to deepen anesthesia (with intravenous anesthetics and narcotic analgesics) and / or introduce muscle relaxants.
6. Bronchospasm
The presence of an endotracheal tube in the trachea causes reflex bronchoconstriction. Bronchospasm may be particularly severe in patients with superficial anesthesia and reactive airways. Bronchospasm can be prevented by prior use of anticholinergics, steroids, inhaled b2 agonists, and narcotic analgesics. After tracheal intubation, deepening of anesthesia with intravenous or inhaled anesthetics, as well as the introduction of inhaled or intravenous b-agonists, is useful. It is important to ensure that audible rales on lung auscultation are not due to mechanical obstruction of the endotracheal tube or other causes such as pneumothorax or heart failure.
7. Esophageal intubation
Rapid recognition of esophageal intubation is essential to prevent hypoxia in patients with sleep apnea. Hypoxemia occurring shortly after esophageal intubation may not be immediately visible. Clinically manifest absence of breath sounds over the chest during auscultation, gurgling sounds over the epigastrium and bloating. However, all clinical signs may be erroneous , and precious minutes of life may be lost if these signs of esophageal intubation are relied upon. The only way to confirm correct placement of the endotracheal tube is to visualize its passage through the vocal cords. But, unfortunately, this is not possible during the difficult intubation that often occurs with esophageal intubation.
Hypoxemia occurring shortly after esophageal intubation may not be immediately visible. Clinically manifest absence of breath sounds over the chest during auscultation, gurgling sounds over the epigastrium and bloating. However, all clinical signs may be erroneous , and precious minutes of life may be lost if these signs of esophageal intubation are relied upon. The only way to confirm correct placement of the endotracheal tube is to visualize its passage through the vocal cords. But, unfortunately, this is not possible during the difficult intubation that often occurs with esophageal intubation.
IMPORTANT! End-tidal CO monitoring only 2 confirms placement of the endotracheal tube in the trachea. Passing the bronchoscope through the endotracheal tube and visualizing the tracheal rings also confirms tube placement in the trachea, but this is not always available.
8. Endobronchial intubation
Endobronchial intubation is a complication of tracheal intubation that occurs when the endotracheal tube enters one of the bronchi, usually in the right main bronchus . This is the most common complication of intubation if the patient has a minimal distance between the carina and the vocal cords, as in small children. This results in a significant right-to-left shunt, resulting in hypoxia. In addition, absorption of the inhalation anesthetic may be impaired and lead to changes in the depth of anesthesia.
If endobronchial intubation is detected , the endotracheal tube should be pulled up a few centimeters. Fiberoptic bronchoscopy is the optimal diagnostic tool. The anesthetist should be extremely careful when pulling on the tube, especially if the airway is difficult. Please note that a properly positioned endotracheal tube must be well fixed so as not to change its position during head movement or changes in the position of the patient's body.
Please note that a properly positioned endotracheal tube must be well fixed so as not to change its position during head movement or changes in the position of the patient's body.
9. Airway perforation
Airway perforation, tracheal rupture - serious complications of tracheal intubation.
Esophageal perforation may occur with multiple intubation attempts, especially in patients with difficult airways. Subcutaneous emphysema occurs shortly after intubation. Later, there may be pain and swelling in the neck, difficulty swallowing. Mediastinitis leading to sepsis can be fatal.
Tracheal rupture can occur due to excessive pressure in the cuff of the endotracheal tube, multiple attempts at intubation, the use of rigid stylets, improper position of the tip of the tube, repositioning the tube without deflating the cuff, severe coughing. It is important to know that the risk of intubation complications is higher in patients with tracheal deformity caused by neoplasm or large lymph nodes, chronic obstructive pulmonary disease, and in patients receiving long-term corticosteroid therapy. More often there is a rupture of the membranous part of the trachea.
It is important to know that the risk of intubation complications is higher in patients with tracheal deformity caused by neoplasm or large lymph nodes, chronic obstructive pulmonary disease, and in patients receiving long-term corticosteroid therapy. More often there is a rupture of the membranous part of the trachea.
Airway perforation can occur anywhere from the nose to the trachea. Clinical manifestations: subcutaneous emphysema, pneumomediastinum or pneumothorax . Awake patients may experience cough, hemoptysis, and cyanosis. When this occurs, the perforation must be found, including by bronchoscopy.
10. Acute traumatic complications of tracheal intubation
Dental trauma
Incidence of dental trauma rare (1:9000 anesthesias). The upper incisors are usually damaged. Risk factors : poor teething, difficult laryngoscopy and difficult intubation. If a tooth injury occurs, bleeding should be stopped to prevent blood aspiration. The fractured tooth must be placed in saline for possible reimplantation. The details of the injury should be recorded in detail on the anesthesia chart and the patient should be informed of the injury.
If a tooth injury occurs, bleeding should be stopped to prevent blood aspiration. The fractured tooth must be placed in saline for possible reimplantation. The details of the injury should be recorded in detail on the anesthesia chart and the patient should be informed of the injury.
Trauma to the nose
Nasotracheal intubation is often used in head and neck surgery. In patients with skull base fractures or severe facial trauma, transnasal tracheal intubation should not be performed because there is a risk of inadvertent skull intubation.
Nosebleeds are a common problem. More common in patients with coagulopathy. Nasotracheal intubation is relatively contraindicated in these patients.
Prolonged intubation may lead to tissue necrosis in the area of the nasal septum. This can lead to the formation of an abscess. Paranasal sinusitis occurs when the sinus is damaged, followed by swelling, obstruction and infection. It may present as unexplained fever and purulent discharge; often refractory to antibiotic therapy and can lead to intracranial infection and sepsis.
It may present as unexplained fever and purulent discharge; often refractory to antibiotic therapy and can lead to intracranial infection and sepsis.
Trauma of the pharynx
Necrosis and perforation of the pharynx may occur in the immediate postoperative period. Clinically manifested by subcutaneous emphysema and crepitus, fever, tachycardia and pain when swallowing. Most oropharyngeal tears can be treated conservatively. If a hematoma occurs, drainage should be considered. The patient must avoid oral feeding for 48 hours.
Temporomandibular joint injury
Joint displacement is usually detected during tracheal intubation. It is necessary to immediately reduce the dislocation of the temporomandibular joint, which can be easily achieved.
Tongue injury
Macroglossia occurs due to prolonged pressure of the endotracheal tube on the tongue, leading to ischemia and venous congestion. Obstruction of the submandibular lymphatic duct can lead to tongue enlargement. Compression injury to the lingual nerve during difficult intubation leads to loss of sensation on the tongue.
Obstruction of the submandibular lymphatic duct can lead to tongue enlargement. Compression injury to the lingual nerve during difficult intubation leads to loss of sensation on the tongue.
Trauma of the larynx
The anterior branch of the recurrent nerve innervates the internal muscles of the larynx. An overinflated endotracheal tube cuff can compress a nerve, causing injury. Bilateral injuries pose a much greater risk and often require emergency reintubation or tracheostomy . Unilateral damage to the recurrent nerve can cause hoarseness.
11. Tension pneumothorax
Tension pneumothorax during anesthesia rare . This complication should be suspected if there is unexplained hypoxia and hypotension or if there is any evidence of airway perforation. Tension pneumothorax can also occur due to barotrauma during mechanical ventilation . At the same time, the pressure in the airways increases, ventilation of the lungs is difficult, there are no respiratory sounds on the affected side during auscultation. Percussion has a boxy sound. An emergency chest x-ray will confirm the diagnosis. Required urgently perform a puncture of the pleural space in the 2nd intercostal space.
At the same time, the pressure in the airways increases, ventilation of the lungs is difficult, there are no respiratory sounds on the affected side during auscultation. Percussion has a boxy sound. An emergency chest x-ray will confirm the diagnosis. Required urgently perform a puncture of the pleural space in the 2nd intercostal space.
12. Aspiration of gastric contents (regurgitation)
Regurgitation - potentially fatal complication intubation. Although the cuffed endotracheal tube protects the lungs from aspiration, regurgitation can occur . The presence of spontaneous ventilation, fluid accumulation above the cuff, Trendelenburg position, and/or a poorly inflated cuff increase the likelihood of aspiration.
If aspiration occurs - urgently perform bronchoscopy to sanitize the trachea.
13. Endotracheal tube obstruction
Causes:
- Dental compression of endotracheal tube
- Endotracheal tube kink
- Sputum, blood clots, foreign body
- Herniated endotracheal tube cuff
Endotracheal tube obstruction manifested by high airway pressure and a characteristic wheezing sound. This complication can cause intraoperative bronchospasm. When an obstruction of the endotracheal tube is diagnosed, the first step is to find the cause and promptly correct it (eg, perform tracheal debridement).
This complication can cause intraoperative bronchospasm. When an obstruction of the endotracheal tube is diagnosed, the first step is to find the cause and promptly correct it (eg, perform tracheal debridement).
14. Displacement of the endotracheal tube
Accidental displacement of the endotracheal tube during anesthesia is a potentially lethal complication . bad or Poor fixation of the tube, excessive head movement during surgery, poor access to the tube during head and neck surgery, and heavy connectors connecting the breathing circuit to the endotracheal tube can lead to displacement of the latter.
15. Leakage of the breathing circuit
Leakage of the breathing circuit is a common complication of tracheal intubation. Detection of this complication is possible subject to continuous capnography and monitoring of airway pressure. In the intensive care unit with multi-day mechanical ventilation, the risk of contour kinking and unplanned extubation increases. Inadequate sedation, psychomotor agitation, lack of continuous respiratory monitoring, and poor endotracheal tube fixation predispose to accidental extubations in intensive care units.
In the intensive care unit with multi-day mechanical ventilation, the risk of contour kinking and unplanned extubation increases. Inadequate sedation, psychomotor agitation, lack of continuous respiratory monitoring, and poor endotracheal tube fixation predispose to accidental extubations in intensive care units.
16. Inflammation of the endotracheal tube
Inflammation of the endotracheal tube - an extremely rare complication of tracheal intubation. Laser respiratory and oral surgery is a fire hazard. Here are a few steps to prevent an emergency:
- Use of special endotracheal tubes, which can be made of transparent plastic (no radiopaque band)
- Wrap the exposed parts of the tube with aluminum tape
- Inflate the ETT cuff with saline instead of air
- Cover the outside of the ETT with wet sheets
- Use of helium-oxygen mixtures, which are less flammable than pure oxygen or oxygen-air mixtures
Important! In case of fire in the respiratory tract, switch off the oxygen flow immediately! Perform emergency extubation of the trachea. Stop surgery. The airway should be examined for burn injury and missing endotracheal tube fragments.
Stop surgery. The airway should be examined for burn injury and missing endotracheal tube fragments.
17. Cuff problems
Serious complications of extubation include: airway obstruction, laryngospasm and aspiration. The anesthetist should have a predetermined strategy for tracheal extubation. Reasons for difficult extubation:
- Endotracheal tube cuff may not deflate
- An unusual cause of difficult extubation: fixation of the endotracheal tube with a Kirschner wire used in head and neck surgery. The nature of the surgical procedure must always be considered to avoid injury from vigorous extubation attempts. Sometimes a bronchoscopy may be needed.
Tracheal extubation algorithm for difficult airways (ASA recommendations) more here
18. Sore throat
Sore throat and hoarseness are minor side effects that should resolve within 72 hours.
Angina is a complication of anesthesia that can occur when the throat, larynx or trachea becomes infected. Factors that can influence the incidence of angina: lack of sterility of the endotracheal tube, improper use of lubricants, traumatic tracheal intubation.
19. Laryngeal edema
Laryngeal edema manifested by stridor . It can be uvular, supraglottic and at the level of the vocal cords. Factors contributing to laryngeal edema include large diameter endotracheal tubes, trauma during laryngoscopy and/or intubation, excessive manipulation of the neck during intubation and surgery, excessive coughing, and upper respiratory infections. Treatment: humidified oxygen, epinephrine inhalation, intravenous dexamethasone. If airway obstruction is a serious problem, reintubation should be considered .
20.
 Tracheal stenosis
Tracheal stenosis Tracheal stenosis - rare complication of tracheal intubation . Ischemia and necrosis of the trachea can occur with increased pressure on its wall. Necrosis of the tracheal mucosa leads to its exfoliation and ulceration of the mucosal membrane, exposing the cartilage of the trachea. Continued ischemia is accompanied by partial or complete destruction of cartilage rings and loss of structural integrity of the affected segment, leading to tracheal dilatation. Healing of an injured tracheal segment can lead to fibrous stricture and tracheal stenosis.
Source
- Latto IP, Rosen M. Difficulties in tracheal intubation. M.: Medicine, 1989. - 304 p.
- Divatia J.V., Bhowmick K. Complications of endotracheal intubation and other airway management procedures. Indian J. Anaesth. 2005; 49(4): 308–318
Intubation Training Simulators - Realistic Manikins and Simulators
Home/Skills/CPR and EMS/Tracheal intubation
Sort by: alphabetically ↓ new ↓ default ↓
Filters
Intubation Trainer with Mobile Objective Assessment
P/N: BT-CSIE
Truman Trauma X - Tracheal Intubation and Comprehensive Chest Trauma Care Trainer
Part Number: TTR2000X
ALS Childbirth - Advanced Life Care Training Patient Simulator
P/N: BT-ACTB
Newborn Resuscitation Manikin
Code: LC.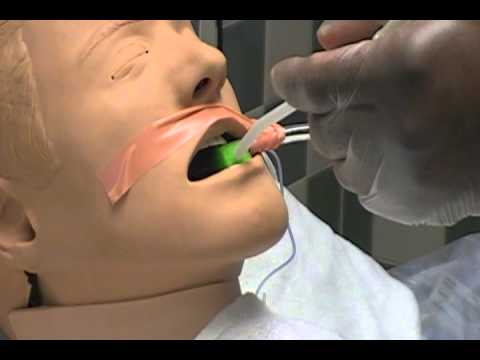 ALSB-001
ALSB-001
Resuscitation manikin 7-10 years old
Code: LC.ALSC-001
Young Woman Resuscitation Manikin
Code: LC.ALSF-001
Extended Resuscitation Premature Baby Manikin
Code: LC.ALSP-001
NenaSim Xcel - baby manikin with CPR
Code: NENASim Xcel
NenaSim Extra - Monitored CPR Infant Simulator
Code: NENASim Xtra
NenaSim Expert - baby robot for team training
Code: NENASim Xpert
Charlie - neonatology resuscitation simulator
P/N: NS.LF01420
CPR manikin 3-6 months
Article: LC. ALSB-001-3/6M
ALSB-001-3/6M
Hip dysplasia newborn manikin for examination and resuscitation
Code: LC.ALSB-001-HD
Resuscitation manikin 1-3 years old
Code: LC.ALST-001
Adult Male CPR Manikin
Code: LC.ALSM-001
Elderly Woman Resuscitation Manikin
Code: LC.ALSEF-001
Resuscitation Manikin Elderly Man
Code: LC.ALSEM-001
Lucy - Full Height OB Manikin, Advanced
P/N: NS.LF00040
CPR and Newborn Care Simulator
Code: KKMW32.11400-100
ADAM-X EXTREME - patient simulator with the ability to simulate clinical cases and scenarios
Code: ADAM-X Xtreme
ADAM-X EXPERT - patient simulator for practicing advanced resuscitation, with the ability to simulate clinical cases
Code: ADAM-X Xpert
Noel - OB Simulator with OB Controller
Code: NS.