Pain cervix pregnancy
Why It Happens and What to Do About It
Causes of vaginal pain during pregnancy
A growing fetus, dilation of the cervix, increased blood flow to the vagina, and fungal infections can all contribute to vaginal pain during pregnancy.
Growing fetus
As your baby and your uterus grow, your pelvic ligaments stretch to accommodate the extra weight. When ligaments and vaginal muscles are overstretched, it can cause a sharp, shooting pain. If you’re already feeling vaginal pain in the first trimester, though, be sure to consult your doctor.
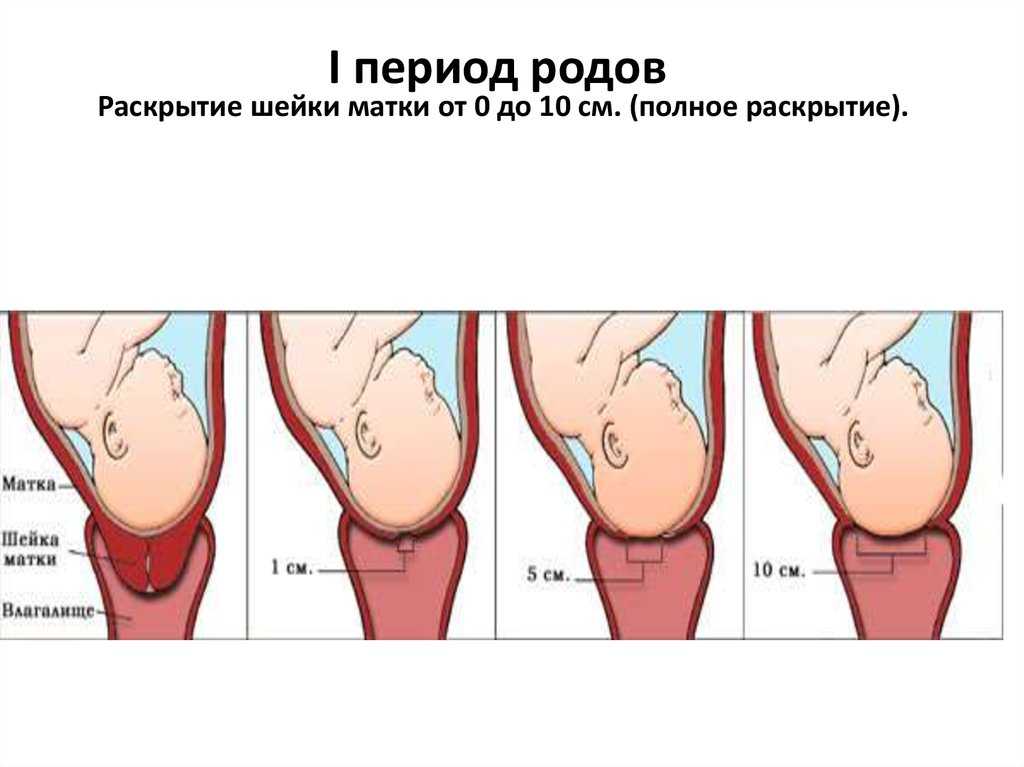
Dilation of the cervix
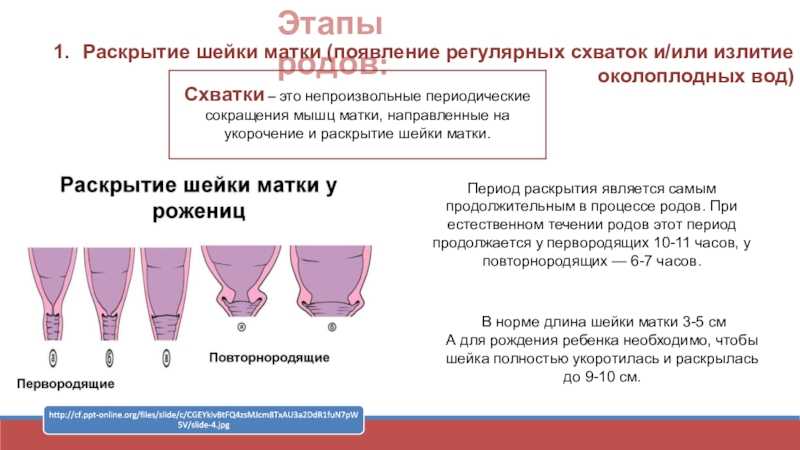
Dilation refers to the eventual opening of your cervix. Occasionally, cervical dilation is to blame for sharp, shooting vaginal pains in the final stages of pregnancy. This is a perfectly normal process that helps the body prepare for labor and delivery. But should the pain present in the lower abdomen, consult a doctor right away.
Take a quiz
Find out what you can do with our Health Assistant
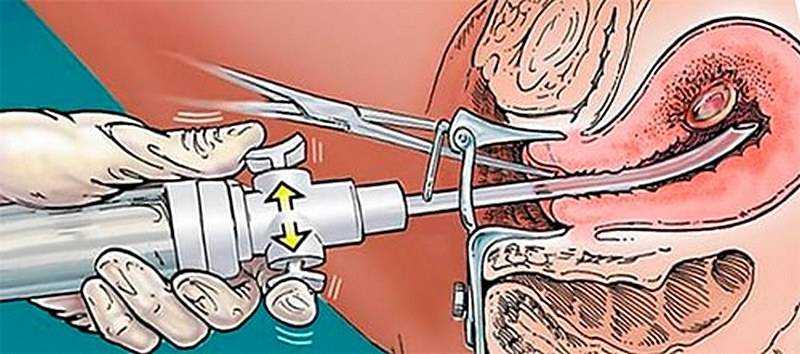
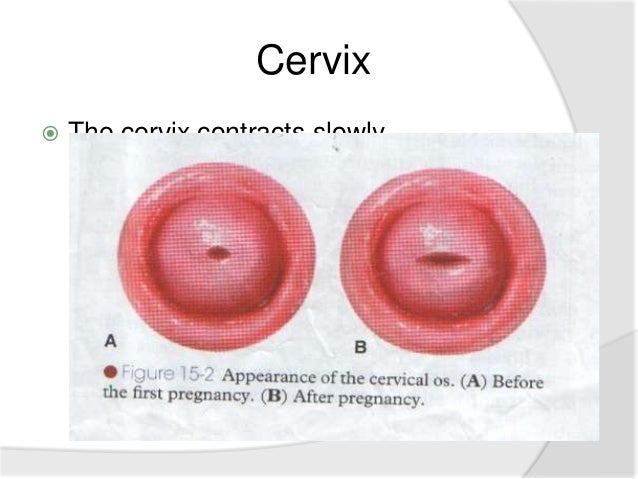
During labor, uterine contractions open the cervix while the baby moves into the proper position. Effacement (when the cervix stretches and thins) and dilation allow the baby to pass through the birthing canal. This happens near the end of the third trimester, but varies with each individual. Some people start to efface and dilate over several weeks, and others shortly before the baby is born. First-time moms might not dilate until they’re in actual labor. An OB-GYN may check the cervix manually to monitor progress as part of prenatal care.
Increased blood flow
Increased blood flow to the vagina, accompanied by heavy vaginal discharge, are normal during pregnancy. Higher levels of estrogen and progesterone produce these changes. The increased overall volume of blood can cause vaginal discomfort or pain.
Fungal infections
If you’re experiencing vaginal pain during pregnancy and suspect it’s the result of a fungal infection, talk to your physician. The most common infection is candida (yeast infection), which is common during pregnancy because of compromised immunity.
During pregnancy, recovering from candida might take longer than usual, as healthcare providers hesitate to prescribe cortisone medications. Consider treating it with an OTC antifungal cream or suppositories. Just remember to discuss this with your doctor first.
Lightning pain
Sometimes pain originating in the pelvic ligaments as they stretch to accommodate a baby can cause startling pain. It can be shocking enough to make some people think they’ve gone into labor. This is called lightning pain.
Some women naturally produce more relaxin and progesterone hormones, encouraging extra stretching and loosening of the ligaments. When round ligaments are stretched too quickly, it produces a sensation similar to that of lightning shooting through your crotch.
In certain cases, this does actually signal the start of labor. Constant back or lightning pain, contractions, or fluid leakage are all signs that the baby could be on their way. If you observe any of the above symptoms prior to 37 weeks, seek medical attention.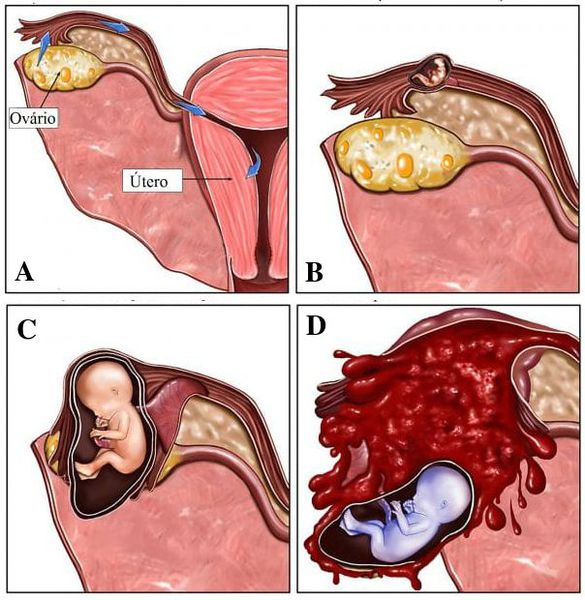
Ectopic pregnancy
Another potential cause of vaginal pain is ectopic pregnancy. This is when the fertilized egg implants anywhere other than the uterus. Most often, the fertilized egg will attach inside a uterine tube.
Ectopic pregnancies cannot be carried to term. The fertilized egg is unable to survive outside of the uterus. In certain cases, an ectopic pregnancy may cause the uterine tube to rupture, resulting in vaginal pain, bleeding, lightheadedness, and nausea. Seek medical help if you show any signs of ectopic pregnancy.
How to cope with vaginal pain during pregnancy
Vaginal pain occurs at some point during nearly every pregnancy. Besides pain medications (which should be approved by a doctor), there are a few different ways to find temporary relief:
- Lying on the left side to improve blood circulation and reduce vaginal pressure
- Sitting elevated feet, which could also decrease pressure levels and alleviate vaginal pain
- Elevating the hips to lessen cervical pain during pregnancy (which usually aggravates existing vaginal discomfort)
- Taking warm baths to soothe and relax achy muscles throughout the body
- Engaging in activities such as yoga or swimming to help boost blood circulation and strengthen muscles.
- Getting a doctor-approved pelvic massage that can simultaneously offer much needed pelvic support and a reprieve from vaginal pain during pregnancy.
When to see a doctor
Vaginal pain is a normal part of pregnancy for most people. Although a few minor lifestyle changes can help, a doctor is the best source of guidance, especially in later trimesters.
Additionally, there are various options available for treating vaginal pregnancy pain that you can research. Just remember that certain conditions, like infection or irregularities in the cervix, could potentially lead to miscarriage. That’s why it’s always a good idea to speak with a doctor about any questions, concerns, or possible treatments first.
Why It Happens, 5 Pain Remedies, and More
Lightning Crotch: Why It Happens, 5 Pain Remedies, and More- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Deborah Weatherspoon, Ph.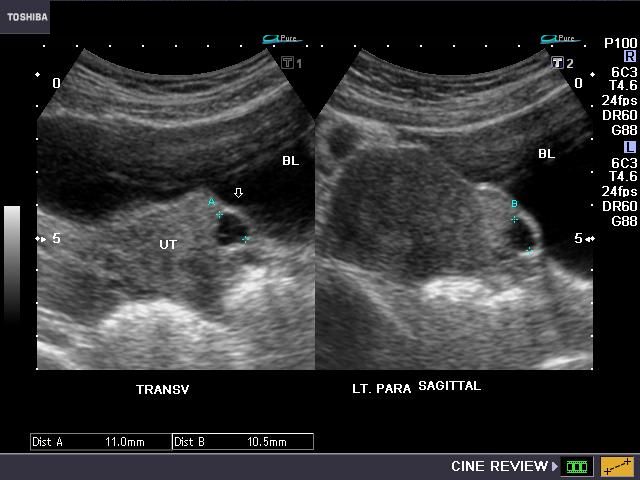 D., MSN — By Chaunie Brusie on December 12, 2018
D., MSN — By Chaunie Brusie on December 12, 2018
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
Healthline only shows you brands and products that we stand behind.
Our team thoroughly researches and evaluates the recommendations we make on our site. To establish that the product manufacturers addressed safety and efficacy standards, we:
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
We do the research so you can find trusted products for your health and wellness.
Read more about our vetting process.During the third trimester of pregnancy, the baby descends down the birth canal.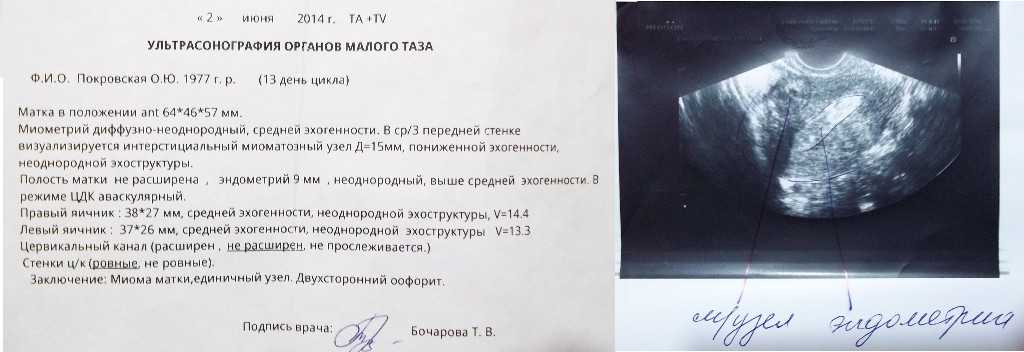 This may cause a pregnant person to experience shooting or lightning-like pain. This can mean labor is near, though not always.
This may cause a pregnant person to experience shooting or lightning-like pain. This can mean labor is near, though not always.
At a party I once attended, one of my pregnant friends suddenly stood up from the table and stretched her arms above her head.
“Ugh,” she said, rubbing her side. “This kid is killing me. It’s like these shooting pains down there. Do you know what I’m talking about?” Boy, did I know what she was talking about.
I’ve never been one to have a comfortable pregnancy. Grateful as I am to have experienced pregnancy and grow our family, I’ve always struggled with the physical demands of pregnancy.
One of those demands definitely is the aches and pains that come along with growing a human being in your body, so let’s take a look at pain “down there.” It’s actually not crotch pain due to lightning.
It’s important to learn what causes it, when you should be concerned, how to stay comfortable, and when it’s a sign that you should head to the hospital.
Symptoms of lightning pain
Like my friend, I experienced a lot of pain down there and it can be confusing to know what’s happening exactly.
Is it normal? Is the pain a sign that you should be worried? There are a lot of questions that go through a pregnant woman’s mind other than, “I wonder if there’s any ice cream left?”
Lightning pain might actually feel like what it sounds like: lightning shooting in your pelvic area.
It almost feels like a little “zing” of pain, especially when you move or shift or feel the baby move or shift. It can come and go and might actually be quite uncomfortable.
Causes of lightning pain
Lightning pain is caused by the pressure and position of the baby as they descend into the birth canal to get ready for delivery.
The good news is lightning pain means you are getting closer to delivery day. The bad news is that lightning can happen for weeks before you actually go into labor.
With my second daughter, I had so much pain and pressure I felt like I was constantly walking around with a bowling ball between my legs. At that point, I was a good month before delivery.
At that point, I was a good month before delivery.
Babies can change positions, but the lightning pain typically has two main causes:
- the actual pressure of the baby’s head on your cervix
- the baby putting pressure on nerve endings around your pelvis
Is lightning pain serious?
Most of the time, lightning pain isn’t serious, especially if it’s not interfering with your daily activities and isn’t accompanied by any other symptoms.
If you’re having pain or any other symptoms such as fever, increased or abnormal discharge, bleeding, or fluid leaking, schedule an appointment with your doctor. Be especially cautious if you’re under 37 weeks in your pregnancy.
5 tips for relieving the pain
There are a few ways you can help reduce your pain during pregnancy.
Stay active
It might sound counterproductive, but staying active will help a lot during your pregnancy.
Not only will it help ward off any excess pounds that might make you more uncomfortable, but it will help keep your joints open and flexible, which is important as they take on a heavier workload from your growing baby.
Focus on a mixture of cardio, weight training, and lots and lots of stretching, especially in the hip area. Get more tips on exercising in your third trimester.
Change up your workload
A large Norwegian study from 1995 found an increased prevalence of pelvic and lower back pain in pregnant women who performed physical jobs that involved a lot of twisting and bending or lifting.
A more recent study from Jordan in 2018 noted that long working hours were also associated with back pain in pregnant women.
If your job involves a lot of manual, hands-on labor or long hours, and you find yourself frequently in pain, consider talking to your boss.
See if you can take a reduced workload or do some temporary relocating to help you get through the rest of your pregnancy more comfortably.
Try a pregnancy massage
I had a lot of trouble with pain in my pregnancies. My massage therapist would apply counter-pressure to my back and sacral area, which helped ease some of those sore muscles that were pulling on the nerves around my hips.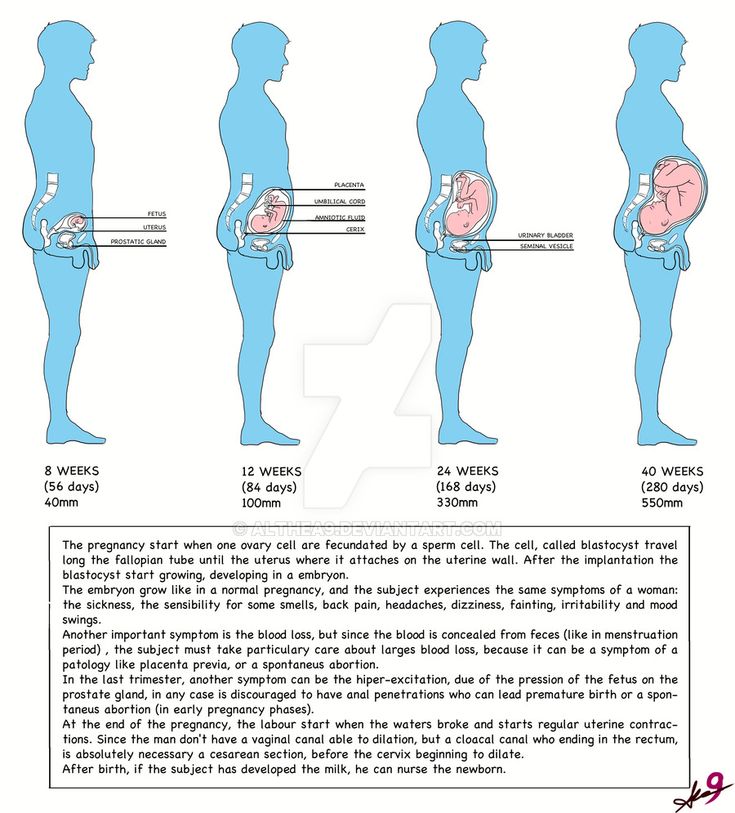 Relaxing those muscles really helped reduce the pain.
Relaxing those muscles really helped reduce the pain.
Just keep swimming
Sometimes, unfortunately, there really isn’t a lot you can do about the lightning pain. Your baby’s head and your cervix may be stuck together like glue.
I found that swimming a lot in the last weeks of pregnancy really made a difference, to just take some of the pressure off my poor body.
Wear a support brace
There are many different types of supportive garments and braces for pregnant women, but their function is usually the same. They help lift and support your belly to take some of that pressure off of your hips, joints, and yes, even cervix.
I used a BLANQI support tank top for my larger-than-life last pregnancy (I had polyhydramnios, so I was literally huge) and it made a big difference in my comfort and pain level.
Pain as a sign of labor
In some women, lightning pain is the first sign that they’re in labor. Some women can even feel their cervix as it dilates.
If you’re experiencing lightning pain and have any other symptoms like regular contractions, consistent backache, or any leaking of fluid, you might be in labor.
If you experience any of these symptoms and are under 37 weeks, be sure to seek medical treatment right away.
The takeaway
In general, lightning pain is a normal part of pregnancy and nothing to be too worried about.
If you’re concerned about your pain or it’s disrupting your day-to-day life, be sure to ask your doctor the following questions at your next checkup to rule out any other reasons for your pain.
- Will I need to be checked for dilation?
- Are there any signs of an infection?
- Can you tell if my baby is in the right position?
- Can you recommend some safe exercises I can do to help my baby get in the best position and help me be comfortable?
If everything checks out and you’re still experiencing lightning pain, you may actually want to congratulate yourself because your body is giving you a pretty clear sign that it’s getting ready to bring your baby into the world.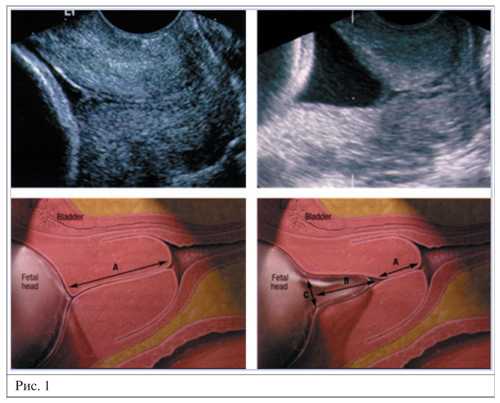
Share on Pinterest
Chaunie Brusie, BSN, is a registered nurse with experience in labor and delivery, critical care, and long-term care nursing. She lives in Michigan with her husband and four young children, and is the author of the book “Tiny Blue Lines.”
Last medically reviewed on December 12, 2018
- Parenthood
- Pregnancy
- Pregnancy Complications
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Endresen EH. (1995). Pelvic pain and low back pain in pregnant women--an epidemiological study. Scandinavian Journal of Rheumatology, 24(3), 135-41.
ncbi.nlm.nih.gov/pubmed/7777823 - Gharaibeh A, et al.
 (2018). Prevalence of low back pain in pregnant women and the associated risk factors.
(2018). Prevalence of low back pain in pregnant women and the associated risk factors.
medwinpublishers.com/JOBD/JOBD16000157.pdf - Mayo Clinic Staff. (2016). Signs of labor: Know what to expect.
mayoclinic.org/healthy-lifestyle/labor-and-delivery/in-depth/signs-of-labor/art-20046184 - Pregnancy: labor and birth. (2018).
womenshealth.gov/pregnancy/childbirth-and-beyond/labor-and-birth
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Dec 12, 2018
Written By
Chaunie Brusie
Medically Reviewed By
Deborah Weatherspoon, Ph.D., MSN
Share this article
Medically reviewed by Deborah Weatherspoon, Ph.D., MSN — By Chaunie Brusie on December 12, 2018
related stories
What Do Different Types of Labor Contractions Feel Like?
Cervix Dilation Chart: The Stages of Labor
Why Vaginal Pressure During Pregnancy Is Totally Normal
Do’s and Don’ts When a Loved One Is Experiencing a Stroke
How to Deal with Butt Pain During Pregnancy
Read this next
What Do Different Types of Labor Contractions Feel Like?
Medically reviewed by Michael Weber, MD
If you’re a first-time mom, you might be wondering what contractions feel like.
 Here’s a guide to contractions and how to tell if you’re in labor.
Here’s a guide to contractions and how to tell if you’re in labor.READ MORE
Cervix Dilation Chart: The Stages of Labor
Medically reviewed by Carolyn Kay, M.D.
Ready to deliver and welcome your little one? Here’s a look at the stages of labor.
READ MORE
Why Vaginal Pressure During Pregnancy Is Totally Normal
Medically reviewed by Nicole Galan, RN
Many pregnant women experience vaginal and/or pelvic pressure. Here's why it happens and how to find relief.
READ MORE
Do’s and Don’ts When a Loved One Is Experiencing a Stroke
Medically reviewed by Seunggu Han, M.D.
A stroke can be life-threatening, so it's important to act fast. If you think a loved one is having a stroke, here's what you should and shouldn't do.

READ MORE
How to Deal with Butt Pain During Pregnancy
Medically reviewed by Janine Kelbach, RNC-OB
Many pregnant women report butt pain as a symptom during the third trimester. These treatment options will help you stay comfortable until delivery.
READ MORE
How to Tell if You’re Having a Miscarriage Without Bleeding
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
A miscarriage is also known as a pregnancy loss. These are the symptoms, causes, and a look at how to move forward.
READ MORE
11 Foods and Beverages to Avoid During Pregnancy - What Not to Eat
By Adda Bjarnadottir, MS, RDN (Ice)
Certain foods can be very harmful for pregnant women and their babies. This is a list of 11 foods and drinks that pregnant women should avoid.

READ MORE
Pregnancy Complications
Medically reviewed by Michael Weber, MD
Sometimes a pregnant woman’s existing health conditions can contribute to problems, and other times new conditions arise because of body and hormonal…
READ MORE
The Best Pregnancy Apps of 2020
These are the best iPhone and Android apps to find information, answers, tools, and tracking during your pregnancy. From scheduling doctor’s visits…
READ MORE
Maintaining a Healthy Pregnancy
Medically reviewed by Stacy Sampson, D.O.
Pregnant people who eat well and exercise regularly along with regular prenatal care are less likely to have complications during pregnancy.
READ MORE
Changes in the cervix during pregnancy
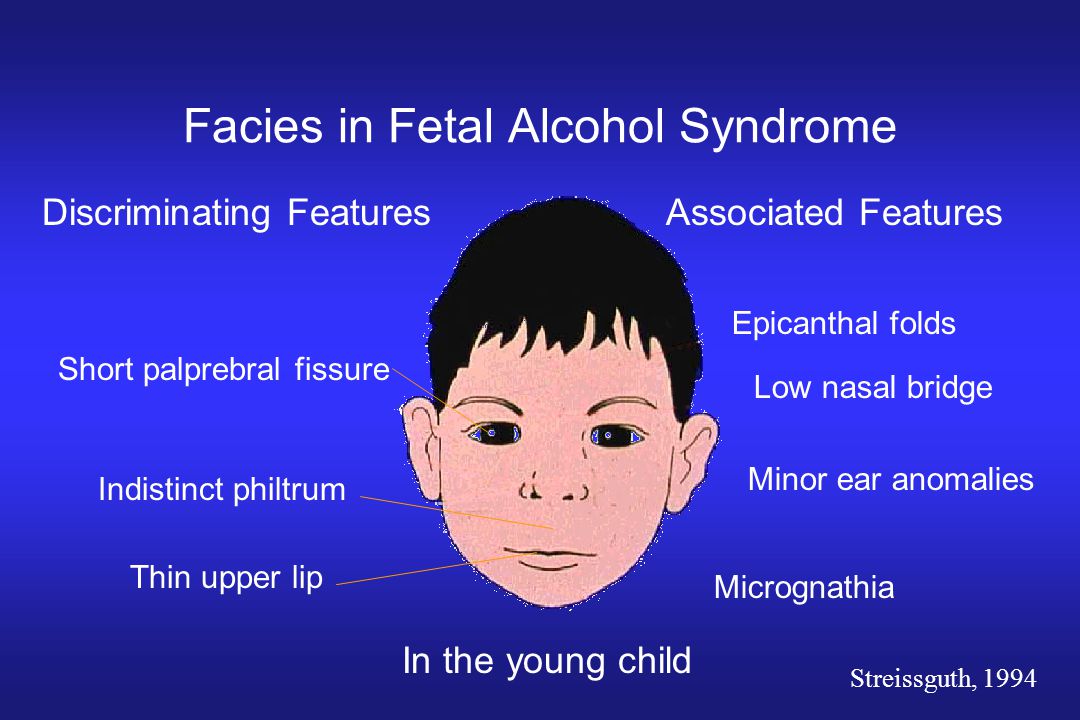
Pregnancy is always pleasant, but sometimes not planned. And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
And not all women have time to prepare for it, to be fully examined before its onset. And the detection of diseases of the cervix already during pregnancy can be an unpleasant discovery.
The cervix is the lower segment of the uterus in the form of a cylinder or cone. In the center is the cervical canal, one end of which opens into the uterine cavity, and the other into the vagina. On average, the length of the cervix is 3–4 cm, the diameter is about 2.5 cm, and the cervical canal is closed. The cervix has two parts: lower and upper. The lower part is called the vaginal, because it protrudes into the vaginal cavity, and the upper part is supravaginal, because it is located above the vagina. The cervix is connected to the vagina through the vaginal fornices. There is an anterior arch - short, posterior - deeper and two lateral ones. Inside the cervix passes the cervical canal, which opens into the uterine cavity with an internal pharynx, and is clogged with mucus from the side of the vagina. Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Mucus is normally impervious to infections and microbes, or to spermatozoa. But in the middle of the menstrual cycle, the mucus thins and becomes permeable to sperm.
Outside, the surface of the cervix has a pinkish tint, it is smooth and shiny, durable, and from the inside it is bright pink, velvety and loose.
The cervix during pregnancy is an important organ, both in anatomical and functional terms. It must be remembered that it promotes the process of fertilization, prevents infection from entering the uterine cavity and appendages, helps to "endure" the baby and participates in childbirth. That is why regular monitoring of the condition of the cervix during pregnancy is simply necessary.
During pregnancy, a number of physiological changes occur in this organ. For example, a short time after fertilization, its color changes: it becomes cyanotic. The reason for this is the extensive vascular network and its blood supply. Due to the action of estriol and progesterone, the tissue of the cervix becomes soft.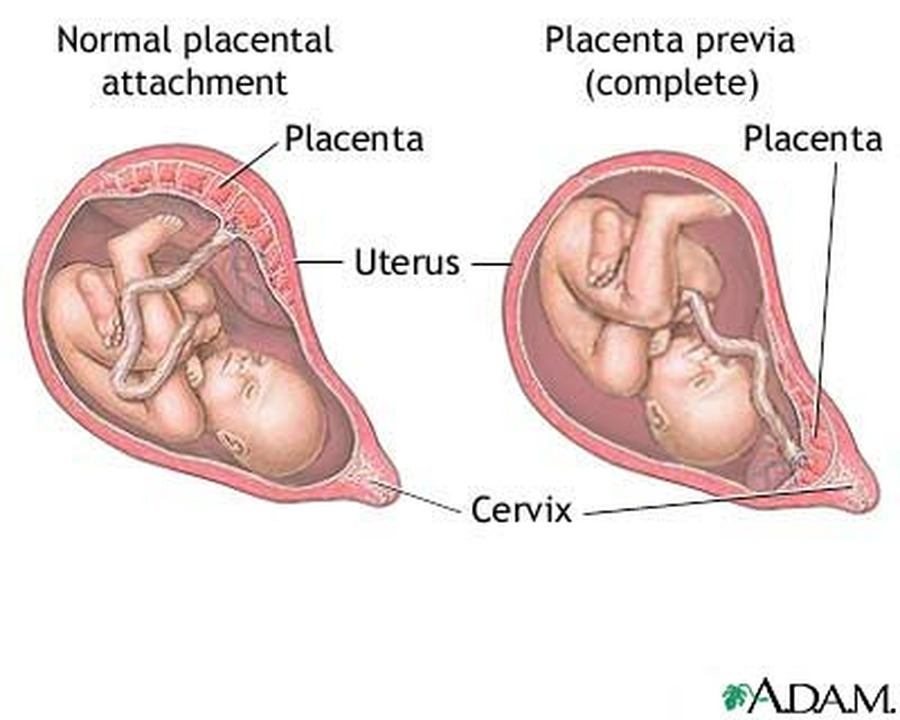 During pregnancy, the cervical glands expand and become more branched.
During pregnancy, the cervical glands expand and become more branched.
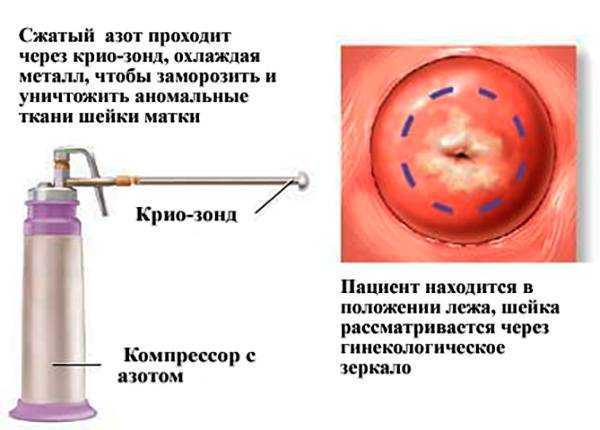
Screening examination of the cervix during pregnancy includes: cytological examination, smears for flora and detection of infections. Cytological examination is often the first key step in the examination of the cervix, since it allows to detect very early pathological changes that occur at the cellular level, including in the absence of visible changes in the cervical epithelium. The examination is carried out to identify the pathology of the cervix and the selection of pregnant women who need a more in-depth examination and appropriate treatment in the postpartum period. When conducting a screening examination, in addition to a doctor's examination, a colposcopy may be recommended. As you know, the cervix is covered with two types of epithelium: squamous stratified from the side of the vagina and single-layer cylindrical from the side of the cervical canal. Epithelial cells are constantly desquamated and end up in the lumen of the cervical canal and in the vagina. Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
Their structural characteristics make it possible, when examined under a microscope, to distinguish healthy cells from atypical ones, including cancerous ones.
During pregnancy, in addition to physiological changes in the cervix, some borderline and pathological processes may occur.
Under the influence of hormonal changes that occur in a woman's body during the menstrual cycle, cyclic changes also occur in the cells of the epithelium of the cervical canal. During the period of ovulation, the secretion of mucus by the glands of the cervical canal increases, and its qualitative characteristics change. With injuries or inflammatory lesions, sometimes the glands of the cervix can become clogged, a secret accumulates in them and cysts form - Naboth follicles or Naboth gland cysts that have been asymptomatic for many years. Small cysts do not require any treatment. And pregnancy, as a rule, is not affected. Only large cysts that strongly deform the cervix and continue to grow may require opening and evacuation of the contents. However, this is very rare and usually requires monitoring during pregnancy.
However, this is very rare and usually requires monitoring during pregnancy.
Quite often, in pregnant women, during a mirror examination of the vaginal part, polyps cervix. The occurrence of polyps is most often associated with a chronic inflammatory process. As a result, a focal proliferation of the mucosa is formed, sometimes with the involvement of muscle tissue and the formation of a pedicle. They are mostly asymptomatic. Sometimes they are a source of blood discharge from the genital tract, more often of contact origin (after sexual intercourse or defecation). The size of the polyp is different - from millet grain rarely to the size of a walnut, their shape also varies. Polyps are single and multiple, their stalk is located either at the edge of the external pharynx, or goes deep into the cervical canal. Sometimes during pregnancy there is an increase in the size of the polyp, in some cases quite fast. Rarely, polyps first appear during pregnancy. The presence of a polyp is always a potential threat of miscarriage, primarily because it creates favorable conditions for ascending infection.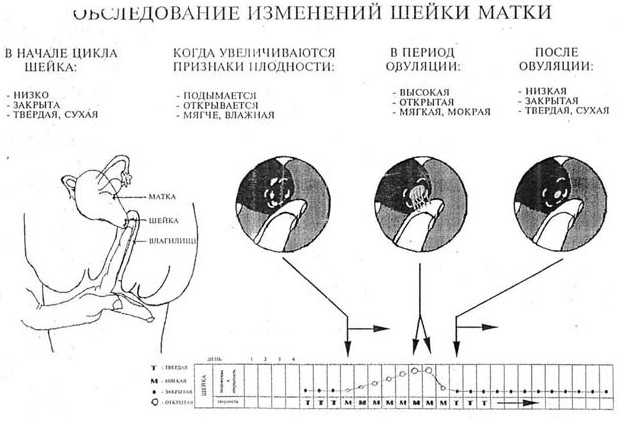 Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
Therefore, as a rule, more frequent monitoring of the cervix follows. The tendency to trauma, bleeding, the presence of signs of tissue necrosis and decay, as well as questionable secretions require special attention and control. Treatment of cervical polyps is only surgical and during pregnancy, in most cases, treatment is postponed until the postpartum period, since even large polyps do not interfere with childbirth.
The most common pathology of the cervix in women is erosion . Erosion is a defect in the mucous membrane. True erosion is not very common. The most common pseudo-erosion (ectopia) is a pathological lesion of the cervical mucosa, in which the usual flat stratified epithelium of the outer part of the cervix is replaced by cylindrical cells from the cervical canal. Often this happens as a result of mechanical action: with frequent and rough sexual intercourse, desquamation of the stratified squamous epithelium occurs. Erosion is a multifactorial disease. The reasons may be:
The reasons may be:
- genital infections, vaginal dysbacteriosis and inflammatory diseases of the female genital area;
- is an early onset of sexual activity and a frequent change of sexual partners. The mucous membrane of the female genital organs finally matures by the age of 20-23. If an infection interferes with this delicate process, erosion is practically unavoidable;
- is an injury to the cervix. The main cause of such injuries is, of course, childbirth and abortion;
- hormonal disorders;
- , cervical pathology may also occur with a decrease in the protective functions of immunity.
The presence of erosion does not affect pregnancy in any way, as well as pregnancy on erosion. Treatment during pregnancy consists in the use of general and local anti-inflammatory drugs for inflammatory diseases of the vagina and cervix. And in most cases, just dynamic observation is enough. Surgical treatment is not carried out throughout the entire pregnancy, since the excess of risks and benefits is significant, and after treatment during childbirth, there may be problems with opening the cervix.
Almost all women with various diseases of the cervix safely bear and happily give birth to beautiful babies!
Attention! Prices for services in different clinics may vary. To clarify the current cost, select the clinic
The administration of the clinic takes all measures to update the prices for programs in a timely manner, however, in order to avoid possible misunderstandings, we recommend that you check the cost of services by phone / with the managers of the clinic
Clinical Hospital IDKMother and Child Clinic Enthusiastov Samara
All directionsSpecialist consultations (adults)Specialist consultations (children)Molecular genetics laboratoryGeneral clinical examinationsProcedural roomOther gynecological operationsTelemedicine for adultsTherapeutic examinationsAdult ultrasound examinations
01.
Specialist consultations (adults)
02.
Consultations of specialists (children)
03.
Laboratory of molecular genetics
04.
General studies
05.
Procedure cabinet
06.
06.
other gynecological operations
07. 9000. 9000.
Adult Telemedicine
08.
Therapeutic Research
09.
Adult Ultrasound
Nothing found
The administration of the clinic takes all measures to timely update the price list posted on the website, however, in order to avoid possible misunderstandings, we advise you to clarify the cost of services and the timing of the tests by calling
Short cervix during pregnancy. What is a short cervix during pregnancy?
IMPORTANT
The information in this section should not be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For diagnosis and proper treatment, you should contact your doctor.
For diagnosis and proper treatment, you should contact your doctor.
A short cervix during pregnancy is a pathological condition in which the length of the organ is less than the minimum for a certain gestational age. In most cases, it is asymptomatic, detected by ultrasound screening. The appearance of clinical symptoms in the form of vaginal discharge and pain in the lower abdomen indicates a high risk of abortion. To make a diagnosis, the examination data on the chair are supplemented by the results of cervicometry and, if necessary, by the determination of the hormonal background. The treatment is combined with the use of tocolytics, hormone therapy, the installation of an obstetric pessary or suturing of the cervical canal.
- Causes of a short cervix during pregnancy
- Pathogenesis
- Symptoms of a short cervix during pregnancy
- Complications
- Diagnostics
- Treatment of a short cervix during pregnancy
- Prognosis and prevention
- Prices for treatment
General
A shortened cervix is one of the most common causes of miscarriage. According to experts in the field of obstetrics and gynecology, from 15 to 42% of late spontaneous abortions and premature births are provoked by this pathology. Signs of a short neck are detected in almost every 10th pregnant woman. The diagnosis is usually established at 15-20 weeks of gestation. An organ length of less than 3 cm at the 20th week of gestation is considered critical for continuing pregnancy. A direct indication for surgical correction of the disorder is the shortening of the neck to 2.0 cm or less by the end of the second trimester. Pathology is more often determined in multiparous women, which is associated with possible trauma in past births.
According to experts in the field of obstetrics and gynecology, from 15 to 42% of late spontaneous abortions and premature births are provoked by this pathology. Signs of a short neck are detected in almost every 10th pregnant woman. The diagnosis is usually established at 15-20 weeks of gestation. An organ length of less than 3 cm at the 20th week of gestation is considered critical for continuing pregnancy. A direct indication for surgical correction of the disorder is the shortening of the neck to 2.0 cm or less by the end of the second trimester. Pathology is more often determined in multiparous women, which is associated with possible trauma in past births.
Short cervix during pregnancy
Causes of a short cervix during pregnancy
A clinically significant shortening of the isthmic-cervical zone occurs in the presence of pathological changes in the tissues of the cervix, its hypersensitivity to the action of regulatory hormones or an increase in their concentration, pressure of the growing fetus and its membranes on the lower uterine segment. The immediate causes of the formation of a shortened neck are:
The immediate causes of the formation of a shortened neck are:
- Anatomical defects and mechanical damage. Initially, a short neck occurs with genital infantilism, congenital anomalies in the development of the uterus or cervical canal. Deformation with a decrease in the length of the organ is possible due to trauma received in previous births or during invasive manipulations (diagnostic curettage, abortion).
- Hormonal disorders. The condition of the cervix is affected by hormones produced by the ovaries and placenta during pregnancy. Most often, its shortening is observed with increased secretion of androgens. The occurrence of pathology is also facilitated by connective tissue dysplasia, caused by an increase in the level of relaxin as the birth approaches.
- Pressure on the isthmic-cervical region. The probability of stretching the lower uterine segment and the internal cervical os with its decrease increases from the 2nd trimester of pregnancy, when faster growth of the fetus begins.
 Risk factors are multiple pregnancies and polyhydramnios, in which the pressure on the cervix from inside the uterus is higher.
Risk factors are multiple pregnancies and polyhydramnios, in which the pressure on the cervix from inside the uterus is higher.
Pathogenesis
The mechanism of pathological disorders in the shortening of the cervix is associated with changes occurring in its tissues during pregnancy and an increase in pressure in the uterine cavity. Normally, after conception, the cervical canal closes, its mucosa becomes edematous and cyanotic due to accelerated blood supply, and the size of the cervix gradually increases, reaching a maximum value of 3.5-4.5 cm at 28 weeks. By the end of pregnancy, the cervix gradually shortens, opens and smoothes. In the presence of congenital or acquired anatomical defects, dyshormonal influences, the closing function of the cervical canal is impaired. As a result, under the pressure of the fetus, the internal and then the external uterine os are stretched, the neck becomes shorter. However, at the same time, it usually does not soften and does not reach the degree of maturity necessary for childbirth.
Symptoms of a short cervix during pregnancy
Pathology in more than 80% of cases is latent, diagnosed during routine ultrasound screening in the second trimester of pregnancy. The presence of a short neck may be indicated by the appearance of watery or bloody vaginal discharge, slight pulling pains in the lower abdomen, which become cramping as the disorder progresses. However, such disorders are typical for severe violations of the closure function of the cervix, occur with a high risk of premature termination of pregnancy, which increases the importance of routine examinations.
Complications
The most serious consequence of a short and deformed cervix is the increasing isthmic-cervical insufficiency. In the presence of such a pathology, the risk of spontaneous miscarriage and premature onset of labor increases. The failure of the cervical canal contributes to the upward spread of genital infections with the development of endometritis, chorioamnionitis, and other inflammatory processes. If a woman with a short neck carries a pregnancy, she may experience rapid labor with ruptures of the vagina and perineum, intranatal trauma to the child.
If a woman with a short neck carries a pregnancy, she may experience rapid labor with ruptures of the vagina and perineum, intranatal trauma to the child.
Diagnostics
In connection with the almost asymptomatic course of the disorder and the absence of its visible external signs, instrumental methods play a leading role in making the correct diagnosis, allowing you to accurately determine the size, condition and shape of the cervix. The most informative in the diagnostic plan are such studies of a pregnant woman as:
- Gynecological examination. The method is more indicative in multiparous patients with the expansion of the cervical canal along the entire length. An increase in the diameter of the external pharynx is clearly visible during examination of the neck in the mirrors. With a significant shortening, he passes the finger of an obstetrician-gynecologist, the fetal membranes can protrude through it. Palpation provides only indicative data on the possible size of the organ.
- Cervicometry. Transvaginal ultrasound determination of the length of the cervix, the diameter of its internal and external pharynx, the state of the cervical canal is the gold standard for diagnosing the disorder. As a screening method, the method is indicated for all pregnant women with a period of 18-22 weeks. With a burdened obstetric history, cervical ultrasound is performed in the 1st trimester. Unscheduled sonography is performed if organ shortening is suspected.
- Determination of the level of hormones. If the anatomical prerequisites for the development of pathology are not identified, laboratory tests are indicated to assess the concentration of hormones. With a functional shortening of the neck, an increase in the concentration of androgens, a decrease in the content of progesterone, may be noted. A small number of pregnant women with a short cervix have increased levels of relaxin, but data from this analysis are rarely used.
The short neck is differentiated from other pathological conditions that have characteristic signs of early termination of pregnancy - detachment of a normally located placenta, its presentation or infarction, leakage of amniotic fluid, etc.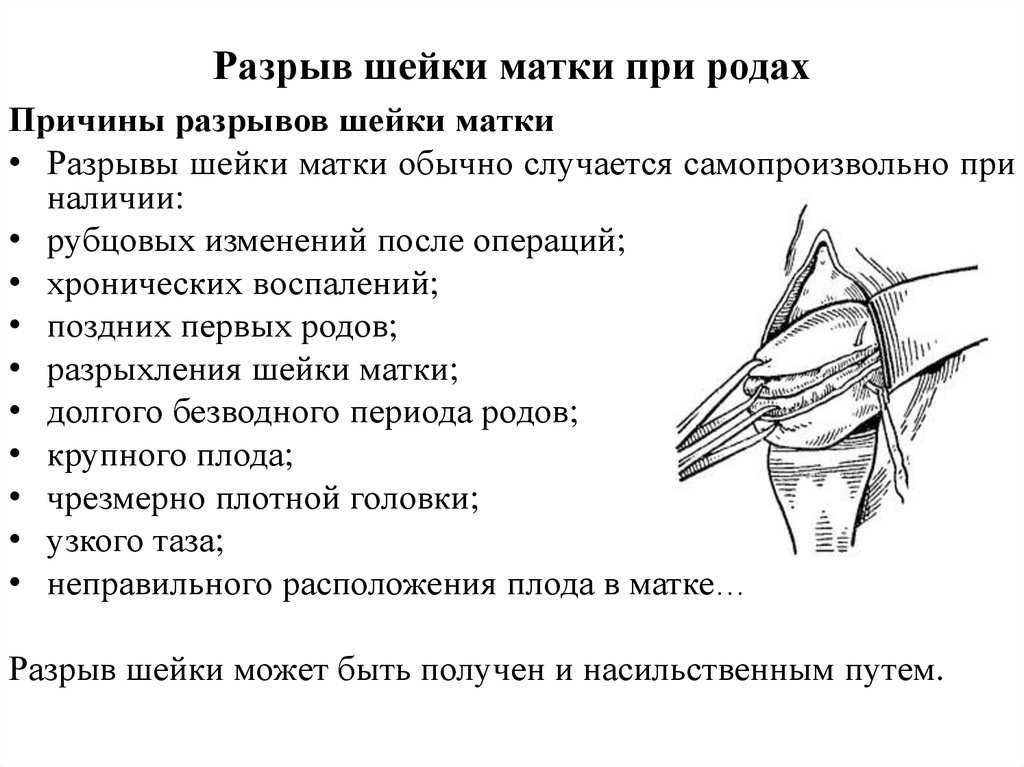 In doubtful cases, consultations of related specialists are prescribed - endocrinologist, infectious disease specialist, immunologist.
In doubtful cases, consultations of related specialists are prescribed - endocrinologist, infectious disease specialist, immunologist.
Treatment of short cervix during pregnancy
Medical tactics after the detection of pathology depends on the gestational age, the degree of shortening of the organ, the presence or absence of a threat of termination of pregnancy, the burden of the obstetric history with habitual miscarriages or premature births. All patients are recommended to limit physical and emotional stress, sufficient rest and night sleep. For best results, pharmaceuticals are usually combined with minor invasive techniques. Pregnant women with this disorder are shown:
- Medical therapy. To reduce pressure on the lower segment of the uterus, in addition to wearing a bandage, patients are prescribed antispasmodics and tocolytics that reduce the tone of the uterine muscles. In the presence of hormonal disorders, it is possible to use drugs that regulate the secretion of hormones.
 To correct emotional disorders, herbal remedies with a sedative effect are used.
To correct emotional disorders, herbal remedies with a sedative effect are used. - Installation of an obstetric ring (pessary). During the manipulation, a special device is put on the cervix, which keeps it closed. The method of non-surgical prophylaxis is effective with a slight shortening of the organ in 2-3 trimesters. The pessary allows you to compensate for the pressure of the fetus on the cervical region and prolong the pregnancy. The device is selected individually, taking into account the size of the body.
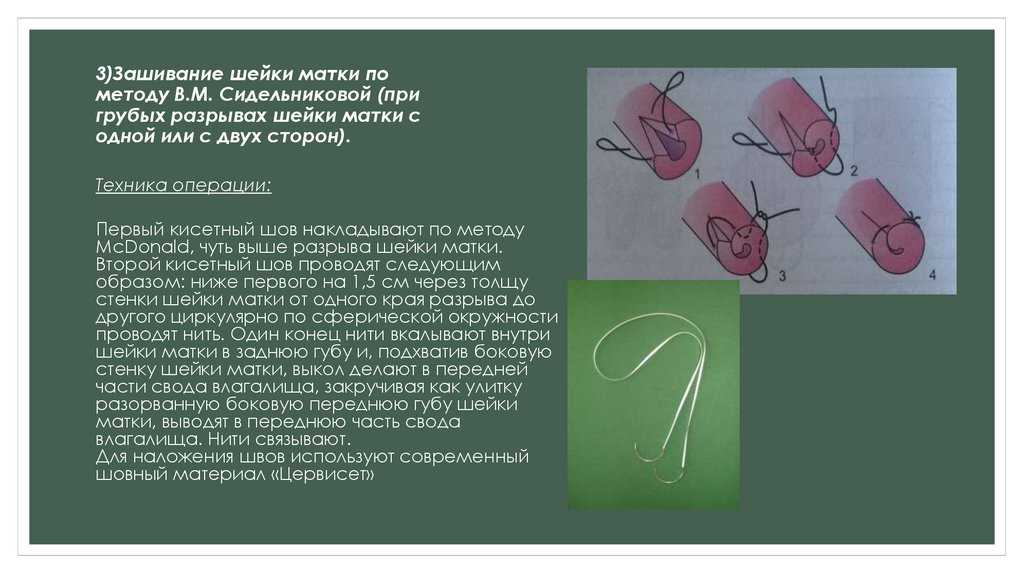
- Cervical cerclage. Surgical intervention for suturing the uterine neck is performed at 14-25 weeks of pregnancy. During the operation, circular purse-string or U-shaped sutures are placed around the cervical canal to prevent its expansion. Stitches are removed after the amniotic fluid breaks, the onset of labor, the onset of bleeding, or upon reaching the 38-week gestational age.
Prognosis and prevention
The prognosis of pregnancy with a shortened cervix depends on the time of detection of pathology and an adequate choice of pregnancy management tactics.