Overactive bladder and pregnancy
What is the effect of overactive bladder symptoms on woman's quality of life during and after first pregnancy?
. 2006 Feb;97(2):296-300.
doi: 10.1111/j.1464-410X.2006.05936.x.
Henriette Jorien Van Brummen 1 , Hein W Bruinse, Geerte Van de Pol, A Peter M Heintz, C Huub Van der Vaart
Affiliations
Affiliation
- 1 Department of Perinatology and Gynaecology, University Medical Centre Utrecht, the Netherlands. [email protected]
- PMID: 16430633
- DOI: 10.1111/j.1464-410X.2006.05936.x
Henriette Jorien Van Brummen et al. BJU Int. 2006 Feb.
. 2006 Feb;97(2):296-300.
doi: 10.1111/j.1464-410X.2006.05936.x.
Authors
Henriette Jorien Van Brummen 1 , Hein W Bruinse, Geerte Van de Pol, A Peter M Heintz, C Huub Van der Vaart
Affiliation
- 1 Department of Perinatology and Gynaecology, University Medical Centre Utrecht, the Netherlands. [email protected]
- PMID: 16430633
- DOI: 10.1111/j.1464-410X.2006.05936.x
Abstract
Objective: To evaluate the effect of overactive bladder symptoms (OAB) on women's quality of life (QoL) during and after the first pregnancy, using self-reported symptom-based QoL questionnaires.
Patients and methods: In a prospective cohort study, 474 women were asked to complete four self-reported questionnaires. Urogenital symptoms were assessed with the Urogenital Distress Inventory (UDI) and the Incontinence Impact Questionnaire (IIQ). A women was considered to experience 'dry' OAB if she replied positively to the following two questions: 'do you experience a strong feeling of urgency to empty your bladder?'; and 'do you experience frequent urination?'. A women was considered to experience 'wet' OAB if she replied positively to all of the following questions: 'do you experience a strong feeling of urgency to empty your bladder?'; 'do you experience frequent urination?'; and 'do you experience urine leakage related to the feeling of urgency?'.
Results: In all, 344 (72.6%) women who returned all four questionnaires were included in the analysis. After first childbirth there was a rapid decline in the prevalence of dry OAB (45.2% to 7.9%, P < 0.001). In pregnancy the prevalence of wet OAB increased significantly, but a year after childbirth the prevalence of wet OAB decreased and was similar to that at 12 weeks of gestation (P = 0.289). Women with wet OAB had higher scores on all IIQ domains than those with no OAB symptoms at 36 weeks of gestation. Women with dry or wet OAB all had higher scores on the mobility domain than those with no OAB. The scores on the physical, social and emotional functioning domains were low, suggesting a minimal restriction of lifestyle.
After first childbirth there was a rapid decline in the prevalence of dry OAB (45.2% to 7.9%, P < 0.001). In pregnancy the prevalence of wet OAB increased significantly, but a year after childbirth the prevalence of wet OAB decreased and was similar to that at 12 weeks of gestation (P = 0.289). Women with wet OAB had higher scores on all IIQ domains than those with no OAB symptoms at 36 weeks of gestation. Women with dry or wet OAB all had higher scores on the mobility domain than those with no OAB. The scores on the physical, social and emotional functioning domains were low, suggesting a minimal restriction of lifestyle.
Conclusion: OAB symptoms are common during pregnancy; dry OAB had no negative effect on QoL, whereas wet OAB compromised QoL both during and after pregnancy, mainly in the 'mobility' and 'embarrassment' domains. The urge urinary incontinence symptom in wet OAB seems to profoundly compromise QoL. Apparently, in young mothers with wet OAB, limitations in mobility are especially stressful and these symptoms can be embarrassing.
Apparently, in young mothers with wet OAB, limitations in mobility are especially stressful and these symptoms can be embarrassing.
Similar articles
-
Bothersome lower urinary tract symptoms 1 year after first delivery: prevalence and the effect of childbirth.
van Brummen HJ, Bruinse HW, van de Pol G, Heintz AP, van der Vaart CH. van Brummen HJ, et al. BJU Int. 2006 Jul;98(1):89-95. doi: 10.1111/j.1464-410X.2006.06211.x. BJU Int. 2006. PMID: 16831150
-
A longitudinal population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in women.
Wennberg AL, Molander U, Fall M, Edlund C, Peeker R, Milsom I. Wennberg AL, et al. Eur Urol. 2009 Apr;55(4):783-91. doi: 10.
 1016/j.eururo.2009.01.007. Epub 2009 Jan 13. Eur Urol. 2009. PMID: 19157689
1016/j.eururo.2009.01.007. Epub 2009 Jan 13. Eur Urol. 2009. PMID: 19157689 -
Impact of stress urinary incontinence and overactive bladder on quality of life in Thai women attending the urogynecology clinic.
Wattanayingcharoenchai R, Manonai J, Vannatim N, Saritapirak S, Imsomboon C, Chittacharoen A. Wattanayingcharoenchai R, et al. J Med Assoc Thai. 2007 Jan;90(1):26-31. J Med Assoc Thai. 2007. PMID: 17621729
-
Defining overactive bladder: epidemiology and burden of disease.
Tubaro A. Tubaro A. Urology. 2004 Dec;64(6 Suppl 1):2-6. doi: 10.1016/j.urology.2004.10.047. Urology. 2004. PMID: 15621220 Review.
-
Redefining response in overactive bladder syndrome.

Payne CK, Kelleher C. Payne CK, et al. BJU Int. 2007 Jan;99(1):101-6. doi: 10.1111/j.1464-410X.2007.06517.x. BJU Int. 2007. PMID: 17227496 Review.
See all similar articles
Cited by
-
Overactive Bladder during Pregnancy: A Prospective Longitudinal Study.
Chen HJ, Hsiao SM, Yang CF, Lee CN, Wang YW, Guo DW, Chang SR. Chen HJ, et al. Medicina (Kaunas). 2022 Feb 6;58(2):243. doi: 10.3390/medicina58020243. Medicina (Kaunas). 2022. PMID: 35208567 Free PMC article.
-
Long-term micturition problems of asymptomatic postpartum urinary retention: a prospective case-control study.
Mulder FEM, Hakvoort RA, de Bruin JP, Janszen EW, van der Post JAM, Roovers JWR.
 Mulder FEM, et al. Int Urogynecol J. 2018 Apr;29(4):481-488. doi: 10.1007/s00192-017-3457-6. Epub 2017 Sep 4. Int Urogynecol J. 2018. PMID: 28871388 Free PMC article.
Mulder FEM, et al. Int Urogynecol J. 2018 Apr;29(4):481-488. doi: 10.1007/s00192-017-3457-6. Epub 2017 Sep 4. Int Urogynecol J. 2018. PMID: 28871388 Free PMC article. -
Evaluation of the prevalence, type, severity, and risk factors of urinary incontinence and its impact on quality of life among women in Turkey.
Akkus Y, Pinar G. Akkus Y, et al. Int Urogynecol J. 2016 Jun;27(6):887-93. doi: 10.1007/s00192-015-2904-5. Epub 2015 Dec 5. Int Urogynecol J. 2016. PMID: 26638154
-
The evaluation of the psychometric properties of a specific quality of life questionnaire for physiological pregnancy.
Vachkova E, Jezek S, Mares J, Moravcova M. Vachkova E, et al. Health Qual Life Outcomes. 2013 Dec 23;11:214.
 doi: 10.1186/1477-7525-11-214. Health Qual Life Outcomes. 2013. PMID: 24365336 Free PMC article.
doi: 10.1186/1477-7525-11-214. Health Qual Life Outcomes. 2013. PMID: 24365336 Free PMC article. -
Overactive bladder after female genital mutilation/cutting (FGM/C) type III.
Abdulcadir J, Dällenbach P. Abdulcadir J, et al. BMJ Case Rep. 2013 Oct 4;2013:bcr2012008155. doi: 10.1136/bcr-2012-008155. BMJ Case Rep. 2013. PMID: 24096069 Free PMC article.
See all "Cited by" articles
MeSH terms
Incontinence During Pregnancy and After Childbirth
Written by WebMD Editorial Contributors
Medically Reviewed by Traci C. Johnson, MD on July 20, 2021
In this Article
- What Types of Incontinence Are Experienced During and After Pregnancy?
- How Is Urinary Incontinence During Pregnancy Treated?
- What Are Kegel Exercises?
- When Should You See a Health Care Professional About Incontinence?
During pregnancy, many women experience at least some degree of urinary incontinence, which is the involuntary loss of urine. The incontinence may be mild and infrequent for some pregnant women. But it can be more severe for others. Age and body mass index are risk factors for pregnancy incontinence, according to one study.
The incontinence may be mild and infrequent for some pregnant women. But it can be more severe for others. Age and body mass index are risk factors for pregnancy incontinence, according to one study.
Incontinence can continue after pregnancy and may not be present right after childbirth. Some women do not have bladder problems until they reach their 40s.
What Types of Incontinence Are Experienced During and After Pregnancy?
The kind of incontinence experienced during pregnancy is usually stress incontinence (SI). Stress incontinence is the loss of urine caused by increased pressure on the bladder. In stress incontinence, the bladder sphincter does not function well enough to hold in urine.
Urinary incontinence during pregnancy can also be the result of an overactive bladder. Women who have an overactive bladder (OAB) need to urinate more than usual because their bladders have uncontrollable spasms. In addition, the muscles surrounding the urethra -- the tube through which urine passes from the bladder -- can be affected. These muscles are meant to prevent urine from leaving the body, but they may be "overridden" if the bladder has a strong contraction.
These muscles are meant to prevent urine from leaving the body, but they may be "overridden" if the bladder has a strong contraction.
The bladder sphincter is a muscular valve that lies at the bottom of the bladder. It works to control the flow of urine. In pregnancy, the expanding uterus puts pressure on the bladder. The muscles in the bladder sphincter and in the pelvic floor can be overwhelmed by the extra stress or pressure on the bladder. Urine may leak out of the bladder when there is additional pressure exerted -- for example, when a pregnant woman coughs or sneezes.
After pregnancy, incontinence problems may continue, because childbirth weakens the pelvic floor muscles, which can cause an overactive bladder. Pregnancy and childbirth also may contribute to bladder control problems because of the following conditions:
- Damage to the nerves that control the bladder
- The fact that the urethra and bladder have moved during pregnancy
- An episiotomy, a cut made in the pelvic floor muscle during delivery of a baby to allow the fetus to come out more easily
How Is Urinary Incontinence During Pregnancy Treated?
Behavioral methods such as timed voiding and bladder training can be helpful in treating urinary incontinence during and after pregnancy. These techniques are often used first and can be done at home. The changes in habits that behavioral methods involve do not have serious side effects.
These techniques are often used first and can be done at home. The changes in habits that behavioral methods involve do not have serious side effects.
To practice timed voiding, you use a chart or diary to record the times that you urinate and when you leak urine. This will give you an idea of your leakage "patterns" so that you can avoid leaking in the future by going to the bathroom at those times.
In bladder training, you "stretch out" the intervals at which you go to the bathroom by waiting a little longer before you go. For instance, to start, you can plan to go to the bathroom once an hour. You follow this pattern for a period of time. Then you change the schedule to going to the bathroom every 90 minutes. Eventually you change it to every two hours and continue to lengthen the time until you are up to three or four hours between bathroom visits.
Another method is to try to postpone a visit to the bathroom for 15 minutes with the first urge. Do this for two weeks and then increase the amount of time to 30 minutes and so on.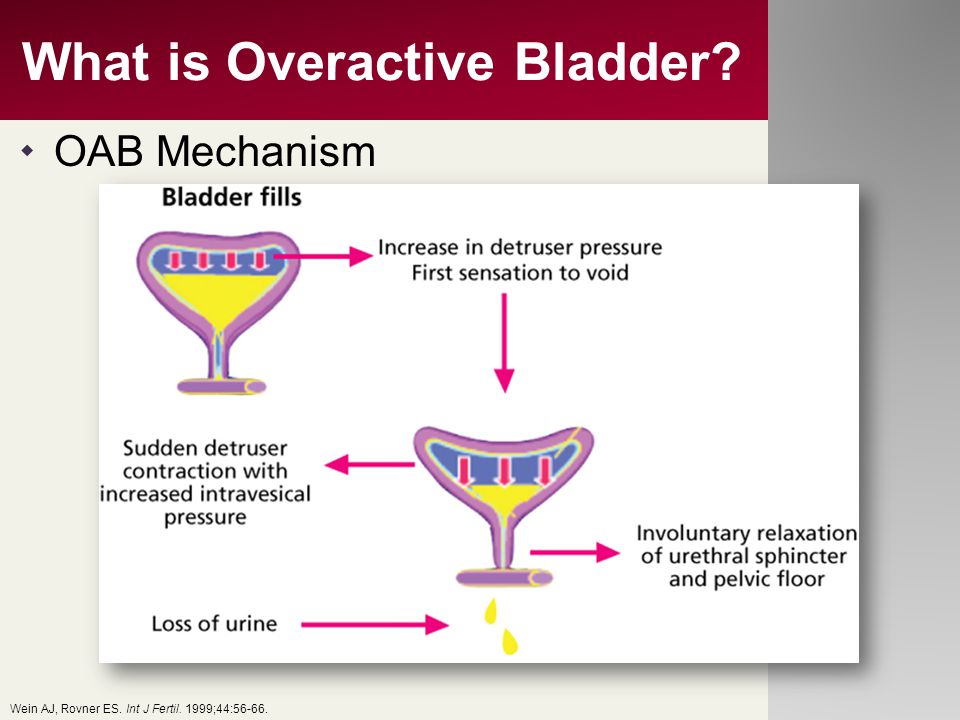
In certain cases, a woman may use a pessary, a device to block the urethra or to strengthen the pelvic muscles. In addition, medications also can be helpful in controlling muscle spasms in the bladder or strengthening the muscles in the urethra. Some drugs can help to relax an overactive bladder.
What Are Kegel Exercises?
Kegel exercises are another method that can be used to help control urinary incontinence. These exercises help tighten and strengthen the muscles in the pelvic floor. Strengthening the pelvic floor muscles can improve the function of the urethra and rectal sphincter.
One way to find the Kegel muscles is to sit on the toilet and begin urinating. Then stop urinating mid-stream. The muscles that you use to stop the flow of urine are the Kegel muscles. Another way to help locate the Kegel muscles is to insert a finger into the vagina and try to make the muscles around your finger tighter.
To perform Kegel exercises, you should:
- Keep your abdominal, thigh, and buttocks muscles relaxed.

- Tighten the pelvic floor muscles.
- Hold the muscles until you count to 10.
- Relax the pelvic floor muscles until you count to 10.
Do 10 Kegel exercises in the morning, afternoon, and at night. They can be done anytime -- while driving or sitting at your desk. Women who do Kegel exercises tend to see results in four to six weeks.
When Should You See a Health Care Professional About Incontinence?
Talk to your doctor if you still have bladder problems six weeks after delivery. Accidental leaking of urine may mean that you have another medical condition. The loss of bladder control should be treated or it can become a long-term problem.
Risk factors for urinary incontinence during pregnancy and postpartum in pregnant women with overactive bladder
HEALTH OF WOMAN. 2018.3(129):80–82
Kostyuk I.
Vinnitsa National Medical University H . and . Pirogov a M Z Ukraine
Since many factors can affect the manifestation of urinary disorders in an individual woman at different periods of life, some of them can cause urinary incontinence, influence the choice of method and the success of treatment.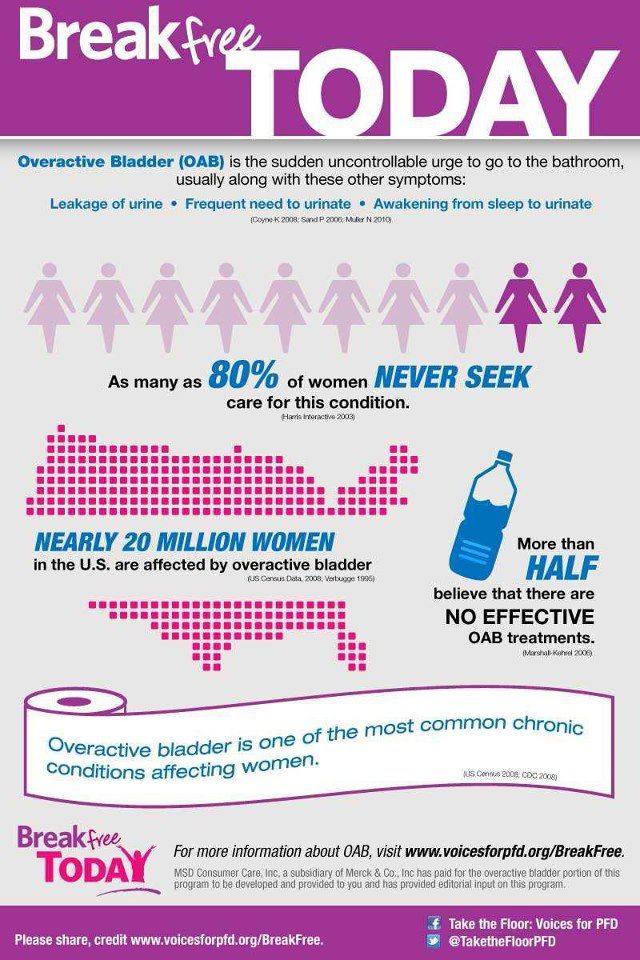 The obtained research results indicate that the treatment of diseases such as overactive bladder syndrome requires an integrated approach through careful collection of data on the socio-economic status, style and quality of life, extragenital diseases, family, obstetric-gynecological and hereditary history, as well as about the sexual function of women during the reproductive period. The results of this study should be taken into account in the development of a diagnostic algorithm for women with overactive bladder syndrome during pregnancy and after childbirth in order to avoid or reduce the clinical manifestations and severity of this syndrome among the female population in the future.
The obtained research results indicate that the treatment of diseases such as overactive bladder syndrome requires an integrated approach through careful collection of data on the socio-economic status, style and quality of life, extragenital diseases, family, obstetric-gynecological and hereditary history, as well as about the sexual function of women during the reproductive period. The results of this study should be taken into account in the development of a diagnostic algorithm for women with overactive bladder syndrome during pregnancy and after childbirth in order to avoid or reduce the clinical manifestations and severity of this syndrome among the female population in the future.
Key words: urination disorders, urinary incontinence, overactive bladder.
BIBLIOGRAPHY
1. Abrams P., Cardozo L., Fall M. et al. The Standardization of Terminology of Lower Urinary Tract Function Neurourol. Urodyne 2002; 21:167-78. https://doi.org/10.1002/nau.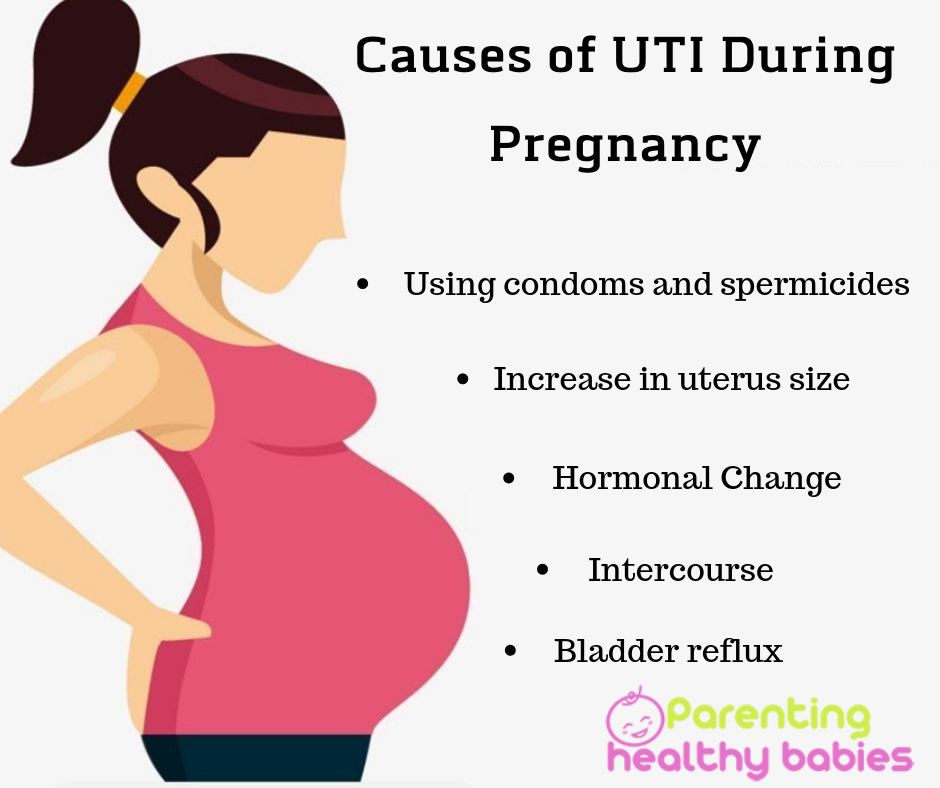 10052; PMid:11857671
10052; PMid:11857671
2. Abrams R., Blaivas J.G., Stanton S.L. Andersen J.T. The standardization of terminology of lower urinary tract function recommended by International Continence Society. Int Urogynec J 1990; 1:45.
3. Hunskaar S., Lose G., Sykes D., Voss S. The prevalence of urinary incontinence in women in four European countries. BJU Int 2004; 93(3):324–330. https://doi.org/10.1111/j.1464-410X.2003.04609.x; PMid:14764130
4. A new aethiology for OAB: intracellular bacterial colonization of urothelial cells / R.K. Khasriya, S. Ismail, M. Wilson, J. Malonee-Lee // International Journal of Urogynecology. - 2011. - Vol. 22 (suppl 1). – P. 141–142.
5. Association of Toll-like receptor 4 gene polymorphism and expression with urinary tract infection types in adults / Y. Xiaolin, H. Tianwen, L. Ying et al. //PLOS ONE. - 2012. - Vol. 5 (12). – e14223.
6. Evaluation of the impact of overactive bladder on sexual health in women: what is relevant? / K. S. Coyne, M.K. Margolis, J. Brewster - Jordan et al. // The Journal of Sexual Medicine. - 2007. - No. 4 (1). - P. 124-136. https://doi.org/10.1111/j.1743-6109.2006.00315.x; PMid:17034411
S. Coyne, M.K. Margolis, J. Brewster - Jordan et al. // The Journal of Sexual Medicine. - 2007. - No. 4 (1). - P. 124-136. https://doi.org/10.1111/j.1743-6109.2006.00315.x; PMid:17034411
7. Felde G. Anxiety and depression associated with incontinence in middle – aged women: a large Norwegian cross – sectional study / G. Felde, I. Bjelland, S. Hunskaar // International Urogynecology Journal. - 2012. - Vol. 23. – No. 3. – P. 299–306. https://doi.org/10.1007/s00192-011-1564-3; PMid:22068320
8. Hopkins W.J. Evaluation of a familial predisposition to recurrent urinary tract infections in women / Hopkins W.J., Uehling D.T., Wargovski D.S. / American Journal of Medical Genetics. - 1999. - Vol. 83.–P. 422–424. https://doi.org/10.1002/(SICI)1096-8628(19990423)83:5<422::AID-AJMG16>3.0.CO;2-1
9. Impact of overactive bladder and lower urinary tract symptoms on sexual health in Japanese women / T. Sako, M. Inoue, T. Watanabe et al. // International Journal of Urogynecology.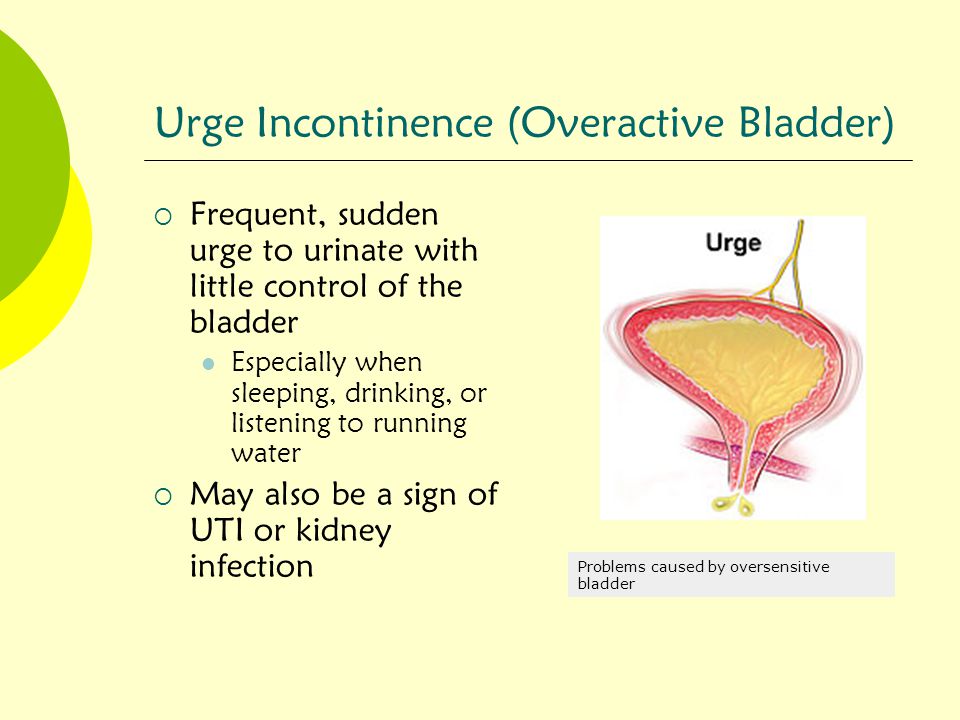 - 2011. - Vol. 22. – P. 165–169. https://doi.org/10.1007/s00192-010-1250-x; PMid:20798921
- 2011. - Vol. 22. – P. 165–169. https://doi.org/10.1007/s00192-010-1250-x; PMid:20798921
10. Incontinence severity and major depression in incontinent women / J.L. Melville, K. Delaney, K. Newton, W. Katon // Obstetrics and gynecology. - 2005. - Vol. 106.–P. 585–592. https://doi.org/10.1097/01.AOG.0000173985.39533.37; PMid:16135592
11. Overactive bladder: prevalence, risk factors and relation to stress incontinence in middle-aged women / P.M. Teleman, J. Lidfeldt, C. Nerbrand, G. Samsioe, A. Mattiasson, WHILA study group // BJOG. - 2004. - Vol. 111. – P. 600. https://doi.org/10.1111/j.1471-0528.2004.00137.x; PMid:15198789
Overactive bladder - symptoms, diagnosis and treatment in St. Petersburg
Symptoms of an overactive bladder
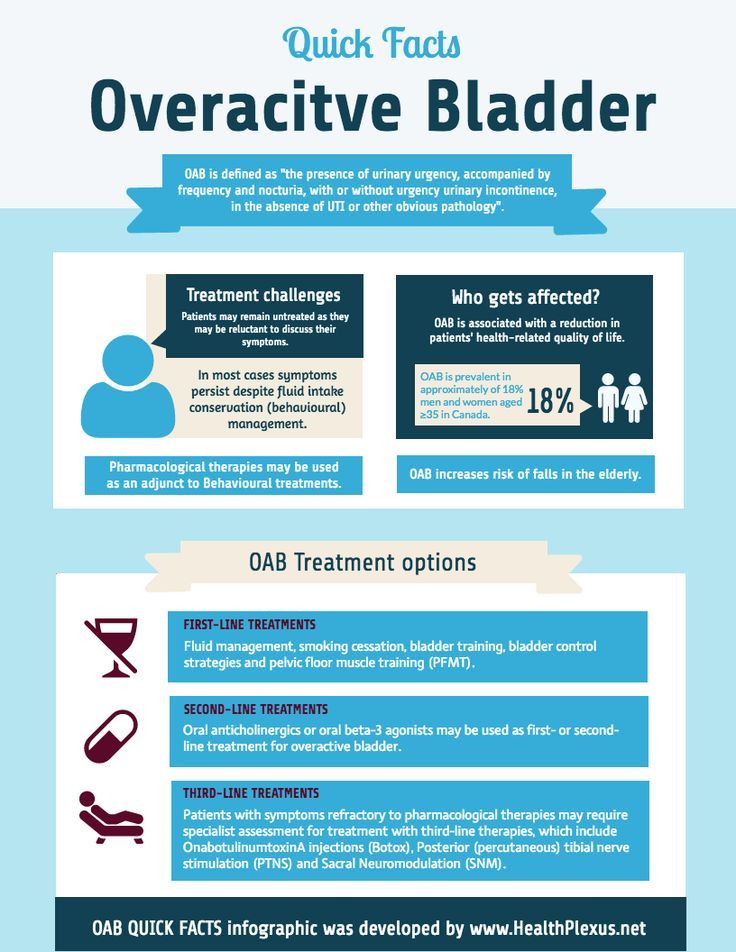
OAB (overactive bladder) is characterized by an imperative urge to urinate. It appears suddenly and gradually increases, making it impossible to postpone going to the toilet until a more convenient time. With the disease, urination occurs at least eight times a day, including during a night's sleep. Nighttime urge to urinate often interferes with proper rest and gives the patient some discomfort.
Nighttime urge to urinate often interferes with proper rest and gives the patient some discomfort.
However, not all patients with corresponding symptoms are diagnosed with OAB. Signs of an overactive bladder may indicate the presence of urinary tract infections, metabolic disorders, or cancer.
People suffering from OAB develop a certain mechanism of behavior. They tend to immediately look for a toilet room in any unfamiliar place in order to use it if necessary. There may also be frequent emptying of the bladder in advance, even if this is not necessary.
Possible causes of the development of the disease
Prerequisites for the development of OAB can be both neurogenic and physiological causes. These include:
- benign and malignant tumors of the prostate that cause narrowing of the urethra;
- pathologies of the spinal cord: neoplasms, hernias, mechanical damage as a result of injuries, consequences of unsuccessful surgical intervention;
- diseases of the brain: sclerosis, Parkinson's or Alzheimer's disease;
- stroke;
- traumatic brain injury;
- diabetes mellitus;
- alcoholic and diabetic neuropathy;
- congenital pathologies of the genitourinary system;
- hormonal imbalance;
- age-related changes;
- urinary tract infections; poisoning with alcohol, drugs or other toxic substances;
- severe stress;
- pregnancy.
Risk factors that contribute to the development of overactive bladder syndrome include smoking, drinking alcoholic and caffeinated beverages, being overweight, not taking enough vitamins (fresh vegetables and fruits), and a large amount of preservatives in food
Diagnosis of the disease
When diagnosing OAB, it is important to exclude other diseases that may cause symptoms, especially infections of the genitourinary system. The main diagnostic measures include:
- taking an anamnesis and talking with the patient: finding out the time and circumstances of the onset of the first symptoms, monitoring the frequency of urination and keeping a special diary;
- elucidation of hereditary factors that may affect the development of the disease;
- general and biochemical analysis of urine;
- analysis of samples according to Nechiporenko;
- culture for bacteria and fungi;
- Ultrasound of the kidneys and bladder, ultrasound of the prostate;
- MRI;
- physical examination of the urethra with a cytoscope; x-ray examination using a contrast agent;
- urodynamic examinations.

The necessary diagnostic method is selected by the attending physician on an individual basis, based on complaints and the current state of the patient.
Methods of treatment
Treatment of pathology may include drug therapy, non-drug therapy and surgery. The first two types of treatment are considered the least traumatic.
Non-drug treatment consists of bladder training: observance of the urinary schedule, a set of exercises to train the pelvic muscles, physiotherapy to reduce urinary tract activity and sensitivity.
The combination of non-pharmacological methods with pharmacotherapy gives a stable effect, which can be prolonged with the help of concomitant measures. Medicamentous therapy on average takes about three months. At the same time, it is important to strictly follow the recommendations of the attending physician and regularly visit a specialist to monitor progress in treatment. If the first course did not give a positive result and there was a relapse of the disease, the question of the advisability of surgical intervention is considered.












